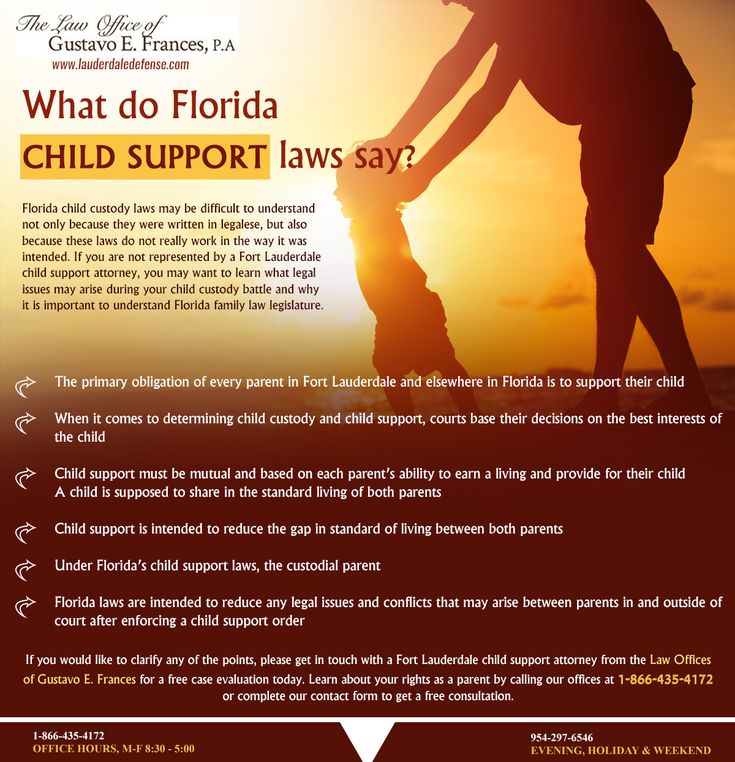
How to treat vulvovaginitis in child
Pediatric Vulvovaginitis | Children's Hospital Colorado
How is pediatric vulvovaginitis treated?
The good news is that most girls will get better after making the following changes:
- Wear only plain white, cotton underpants. Wash them with a tiny amount of unscented detergent and rinse twice to remove any remaining irritants from the detergent. Avoid fabric softeners or any extra cleaning or "freshening" products on underwear and swimsuits.
- Wear a nightgown for sleeping. It's OK to sleep without undies. Avoid one-piece sleeper pajamas. Very loose, soft PJ pants or loose boxer shorts are another option.
- Avoid tights, one-piece leotards, tight jeans or leggings. Choose skirts and looser fitting pants. Find clothes that are comfy, allow air to circulate and don't cause extra rubbing or pressure.
- Take a bath every day. (We may recommend this more than once a day until your child is feeling better.) Make sure that the bathtub is rinsed free of bleach, cleaning products or any leftover soap or bubble bath.
- Soak in clean, warm water. No soap, vinegar or baking soda is needed. Plain, warm water is best to avoid irritation.
- Don't scrub the vulva with a washcloth. Just allow the water to gently wash over and soak the area.
- Only use a mild soap (like Dove) when and where it is really needed, like on skin with visible dirt. Use soap at the end of a bath and then wash it completely off. Soap is usually not needed in the genital area.
- Gently pat dry the genital area.
- Don't use bubble bath or perfumed soap. When your daughter is the right age, tell her not to use feminine sprays, douches, powders or other scented feminine products.
- If the vulvar area is swollen, tender or itchy, use a cool compress for a few minutes. Vaseline or A&D diaper ointment can also be used to help protect the skin.
- Talk about, and remind your child, how to wipe after a bowel movement. Wiping from the front to the back is important to keep the bacteria away from the vulva.
- After swimming, change into dry clothes right away.
When can we expect things to get better?
Using the self-care tips above, symptoms usually get better in one to two weeks.
What if things are not getting better?
If your child/teen's condition does not improve, or if you have new symptoms to report, please call Pediatric and Adolescent Gynecology at 720-777-2667.
Why choose Children's Colorado for your child's vulvovaginitis?
At Children's Colorado, we provide expert care for the diagnosis, treatment and management of health issues of the female reproductive organs in children and teens.
Our board-certified pediatric and adolescent gynecologists have specialized training in the reproductive health concerns of girls of all ages. And depending on your child/teen's needs and treatment plan, we provide both outpatient and inpatient surgical services.
Compassionate care for sensitive issues
Doctors at Children's Colorado understand that topics involving female reproductive organs can be stressful to address, which is why we're extra-sensitive to the mental and emotional needs of our patients and their families. We create a friendly environment for dialogue and encourage our patients to ask questions and talk openly with their care team.
We create a friendly environment for dialogue and encourage our patients to ask questions and talk openly with their care team.
Kids Health Information : Vulvovaginitis
This fact sheet is available in the following languages: Arabic, Assyrian, Burmese, Chinese (simplified), Chinese (traditional), English, Karen, Persian, Somali, Turkish and Vietnamese.
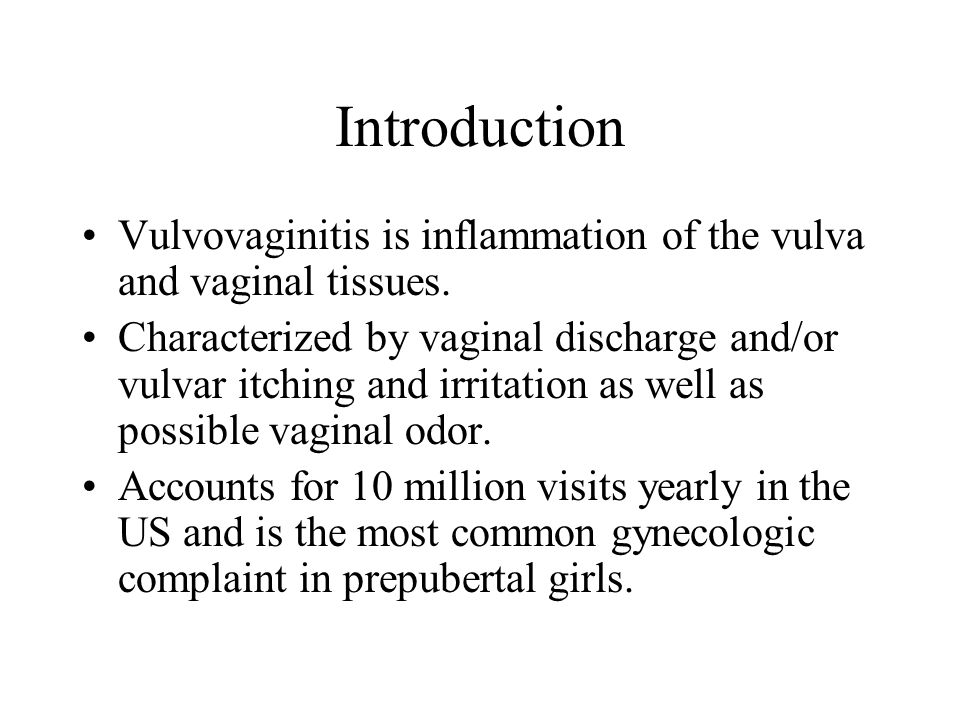
Vulvovaginitis (vul-vo-vaj-ee-night-is) is inflammation or irritation of the vagina and vulva (external female genital area). Mild vulvovaginitis is a very common problem, and some children will have vulvovaginitis many times. Once puberty has begun, vulvovaginitis usually occurs less often.
In most cases, vulvovaginitis is not a serious problem and it will usually improve with simple steps at home. Usually no medical treatment or tests are needed.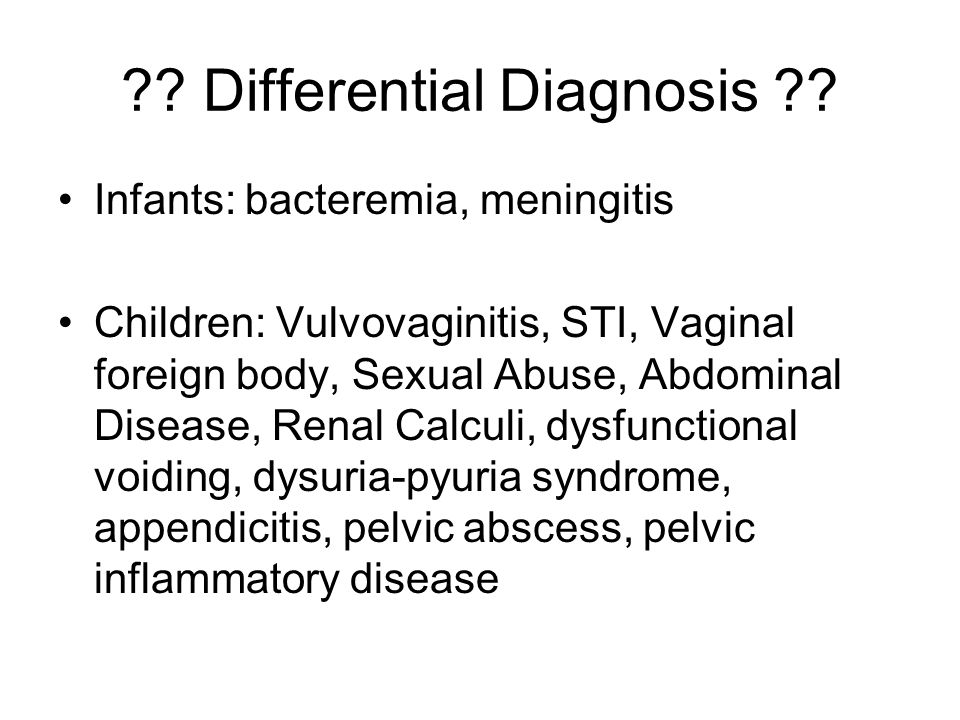
Signs and symptoms of vulvovaginitis
If your child has vulvovaginitis, they may have:
- itching in the vaginal area
- some discharge from the vagina
- redness of the skin between the labia majora (outside lips of the vagina)
- burning or stinging when they pass urine.
What causes vulvovaginitis?
While your child is young, the lining of the vagina and vulva can be quite thin and this can lead to it being easily irritated. Moisture or dampness around the vulva can also lead to vulvovaginitis – this is made worse by tight clothing or being overweight. Another cause of vulvovaginitis is irritants, such as soap residue, bubble baths and antiseptics.
Threadworms sometimes cause or worsen vulvovaginitis. Children with threadworms often scratch a lot at night. If itching is a major symptom, then you may want to treat your child for threadworms. See our fact sheet
Worms.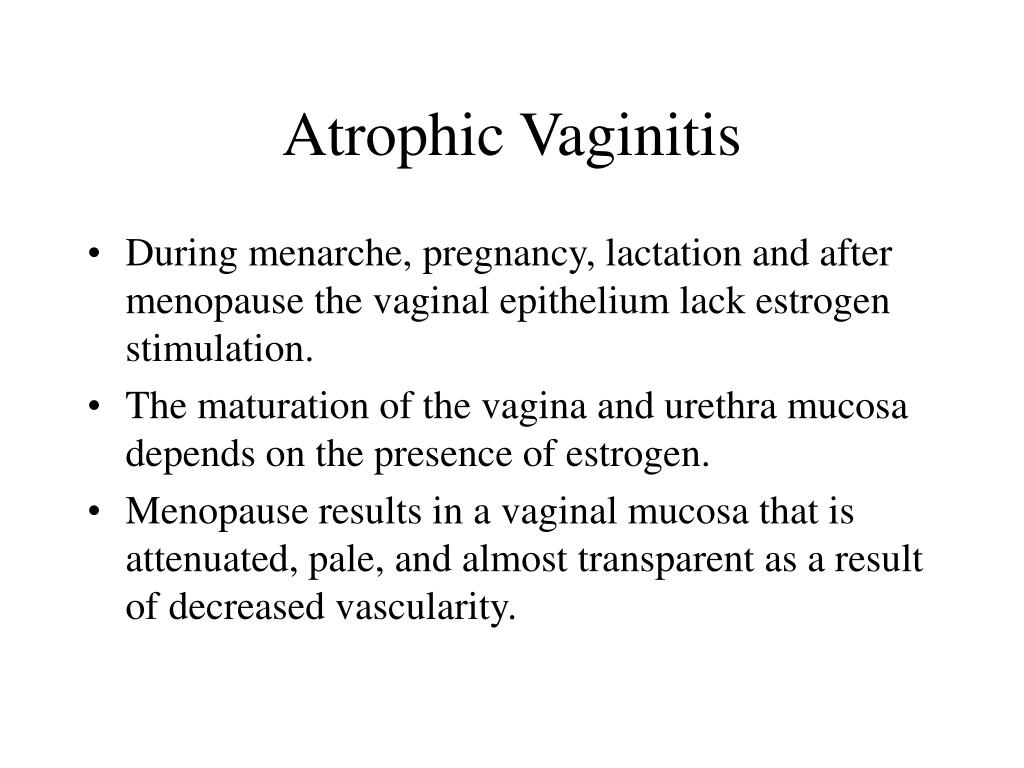
Care at home
In most mild cases of vulvovaginitis, you can care for your child at home without visiting a doctor. Reassure your child that they don’t need to worry, as vulvovaginitis is a common problem and a normal part of growing up.
Try avoiding the things that make vulvovaginitis worse:
- Wear loose cotton underwear and avoid tight jeans etc.
- If your child is overweight, seek advice on how to maintain a healthy weight with diet and exercise.
- Don't use a lot of soap in the bath or shower, and make sure any soap is well rinsed from the vulva. Avoid bubble baths and antibacterial products.
Some people find vinegar baths helpful: add half a cup of white vinegar to a shallow bath and soak for 10 to 15 minutes. Do this daily for a few days and see if it helps.
Soothing creams (for example, soft paraffin, nappy-rash creams) may help settle the soreness, as well as protect the skin from moisture or any discharge, which can be irritating.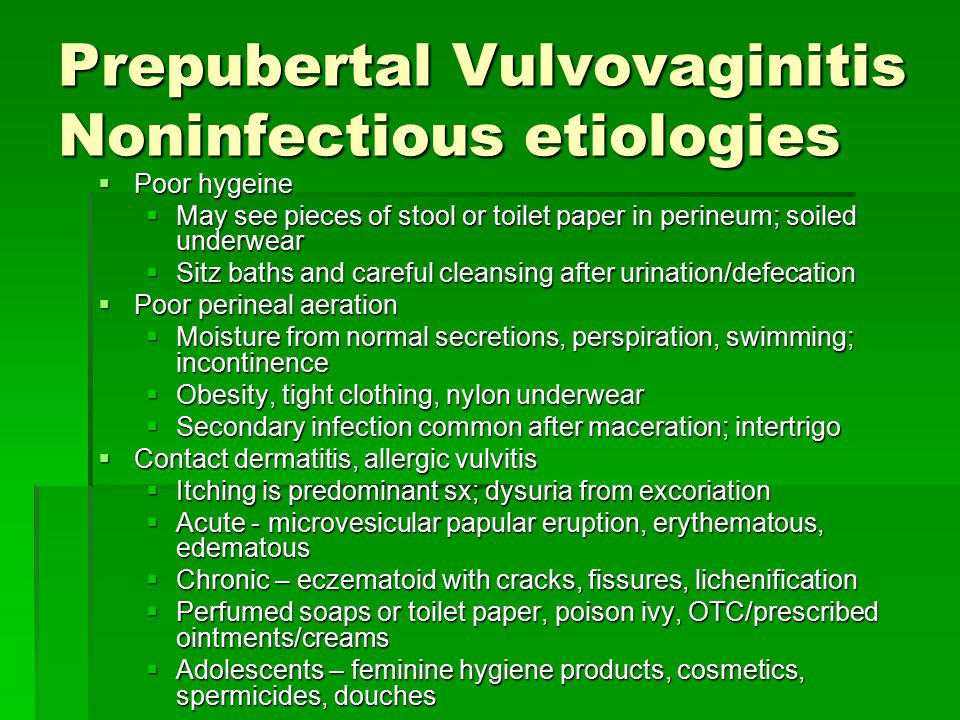
You may have to repeat these simple measures if the problem comes back.
When to see a doctor
Take your child to the GP if:
- The vulvovaginitis is bothering your child – the doctor may advise a swab of the area be taken for testing, but the results are not always helpful.
- Your child has a more severe case of vulvovaginitis, blood-stained discharge, or other skin problems – the doctor may refer them to a paediatrician or other specialist for further management.
- Your child has a fever and pain when passing urine – the doctor may want to test for a urinary tract infection (see our fact sheet Urinary tract infection).
Key points to remember
- Mild vulvovaginitis is a very common problem.
- It may recur now and then, but will improve as your child gets older.
- In most mild cases, no medical treatment or tests are necessary.
- Avoid the things that make vulvovaginitis worse, such as tight underwear and irritants like soap.
For more information
- Kids Health Info fact sheet: Worms
- Kids Health Info fact sheet: Vulval skincare for children
- Kids Health Info fact sheet: Vulval skincare for teenagers
- Kids Health Info fact sheet: Urinary tract infection
- Kids Health Info fact sheet: Nutrition – school-age to adolescence
- See your GP or paediatrician.
Common questions our doctors are asked
Can children get thrush? How do I know if my child has vulvovaginitis or thrush?
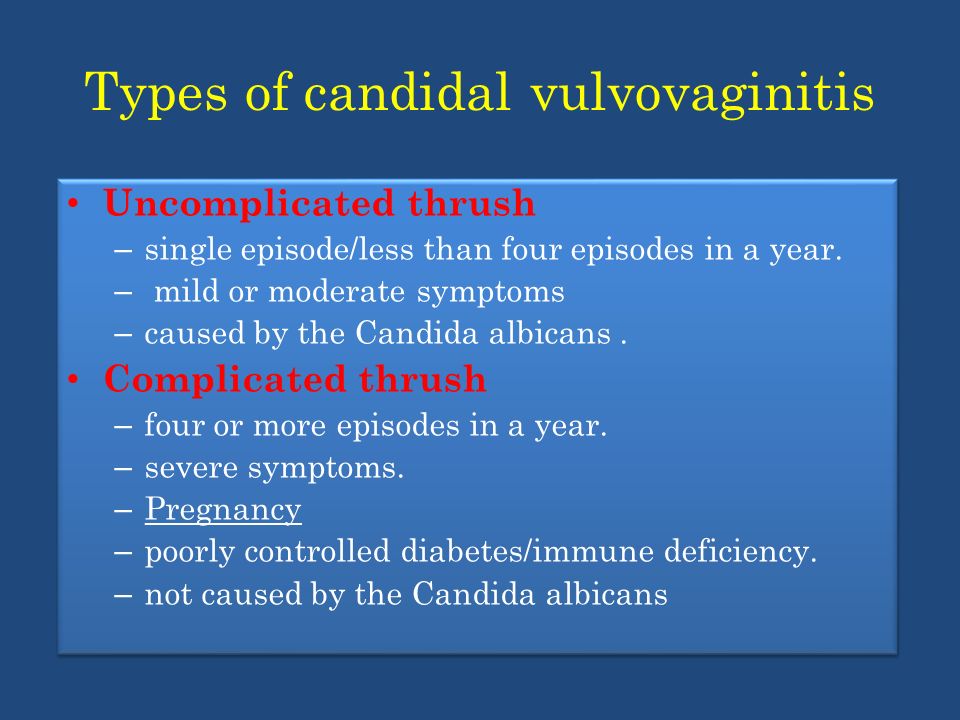
Vulvovaginitis is far more common in children who have not yet gone through puberty than thrush is.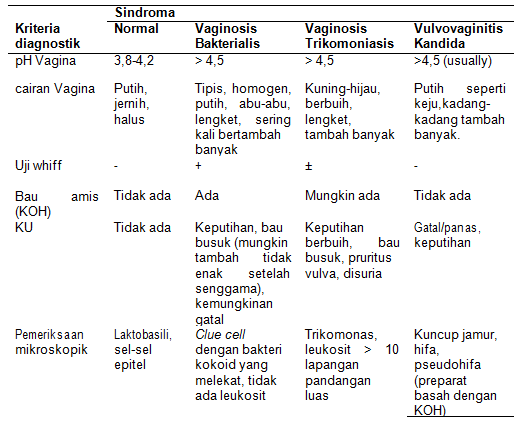 If your child has begun puberty, it is possible that they may have a vaginal yeast infection (thrush). It is important to discuss this with your child’s doctor, as the treatments are different.
If your child has begun puberty, it is possible that they may have a vaginal yeast infection (thrush). It is important to discuss this with your child’s doctor, as the treatments are different.
If my child has a burning feeling when she does a wee, is this vulvovaginitis or a UTI? Should I give her cranberry juice?
If your child is showing any symptoms of UTI, take her to the GP so a urine test can be carried out. Some of the symptoms of UTI overlap with vulvovaginitis. In any case, cranberry juice is not recommended as a treatment option for children for UTI or vulvovaginitis.
Developed by The Royal Children's Hospital General Medicine and Gynaecology departments. We acknowledge the input of RCH consumers and carers.
Reviewed February 2018.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit www.rchfoundation.org.au.
90,000 causes, prevention, treatment. / Useful information / About clinicDiagnostic and treatment center FAMILY CLINIC MEDA
- Home >
- About clinic >
- Useful information >
- Vulvovaginitis in children: causes, prevention, treatment.
Vulvovaginitis is one of the most common reasons mother and baby visit a pediatric gynecologist.
Vaginitis is an inflammation of the vagina, vulvitis is an inflammation of the vulva or external genital organs, that is, the perineum, labia majora and labia minora. Since these areas are close, often the disease occurs together, hence the name "vulvovaginitis".
Manifestations of vulvovaginitis
The girl complains to her mother about itching, pain, burning and discomfort, the mother notices that the child often pulls her hands to “the same place”, some discharge appeared on her panties (leucorrhea, cheesy, green), and the skin became bright red or pink, rashes or even scratching appeared. There are no other manifestations, such as a violation of the general condition, loss of appetite, pain in the abdomen or lower abdomen: they can appear only when inflammation spreads to other organs and tissues.
There are no other manifestations, such as a violation of the general condition, loss of appetite, pain in the abdomen or lower abdomen: they can appear only when inflammation spreads to other organs and tissues.
Causes of vulvovaginitis
The question arises, where does it come from, this vaginitis, in a small child?
There are many causes of vaginitis, but we will list the main ones:
- Allergic reaction
- Excessive efforts to wash the baby "to shine" - mothers wash away the natural protection of the vagina.
- Viral infections (SARS, rubella, chickenpox and many others), when the virus spreads through the blood and lymph throughout the girl's body, including entering the vagina. But it is worth noting that in such cases, vaginitis does not require treatment as such, since the elimination of the cause itself, that is, a viral infection, will also lead to the disappearance of the symptoms of vaginitis.
- Vaginitis often occurs as a result of swimming in pools with chlorinated water.
 In this case, chlorine acts as an irritant, and irritation appears in the genital area. This condition is observed not in all girls, but only in those who have a reaction to chlorine, therefore, in connection with this, it is not necessary to prohibit the child from visiting the pool.
In this case, chlorine acts as an irritant, and irritation appears in the genital area. This condition is observed not in all girls, but only in those who have a reaction to chlorine, therefore, in connection with this, it is not necessary to prohibit the child from visiting the pool. - Sea, public beaches, where there are a huge number of people per square meter
- Foreign body in the girl's vagina (bead, small toy, thread).
- Also, the reasons for the development of vaginitis in girls are reduced immunity and endocrine diseases.
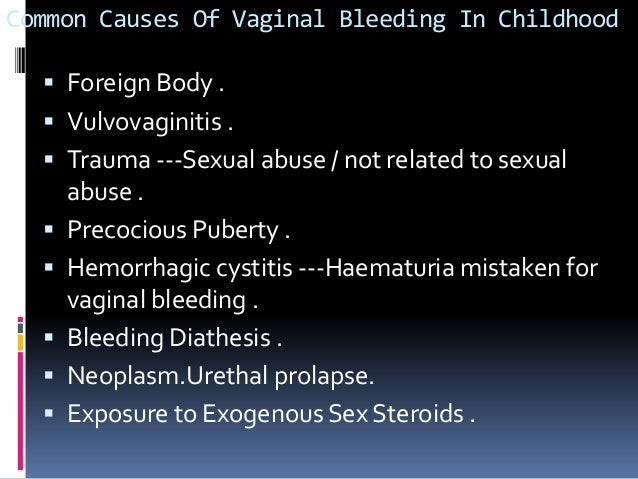
Vulvovaginitis in children is divided into specific, caused by an infectious agent - Trichomonas, chlamydia, tubercle bacillus and others, and non-specific, caused by viruses, yeast-like fungi and other agents that are conditionally pathogenic, that is, causing the development of infection under certain conditions.
Treatment of vulvovaginitis
Treatment of vaginitis depends on the causes that caused it.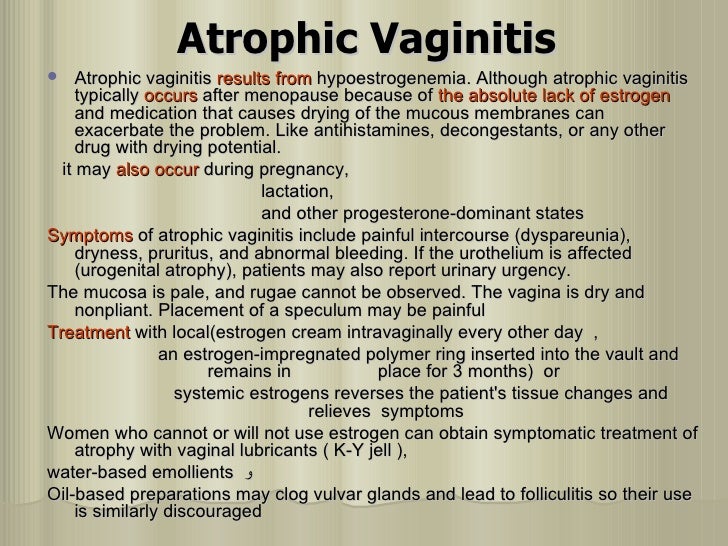
If it is a helminthic invasion, then antihelminthic therapy is prescribed.
In the presence of severe unbearable itching in the perineal area, sedatives (soothing) and antihistamines are prescribed.
In the event that Candida yeast-like fungi are detected during a laboratory examination in the analysis of a smear, antifungal drugs are prescribed in the form of ointments, creams.
There is such a thing as specific vulvovaginitis, that is, vaginitis caused by pathogenic microorganisms (gonococci, trichomonas, chlamydia). This disease requires the appointment of antibiotics, possibly the appointment of vaginal sticks and ointments.
In addition to drug therapy aimed at the destruction of the infectious agent, it is worth noting that the complex of treatment necessarily includes vitamins in the form of synthetic forms or products enriched with vitamins (fruits, vegetables, legumes). And, of course, the disease is considered cured when the microbiocenosis of the vagina is restored.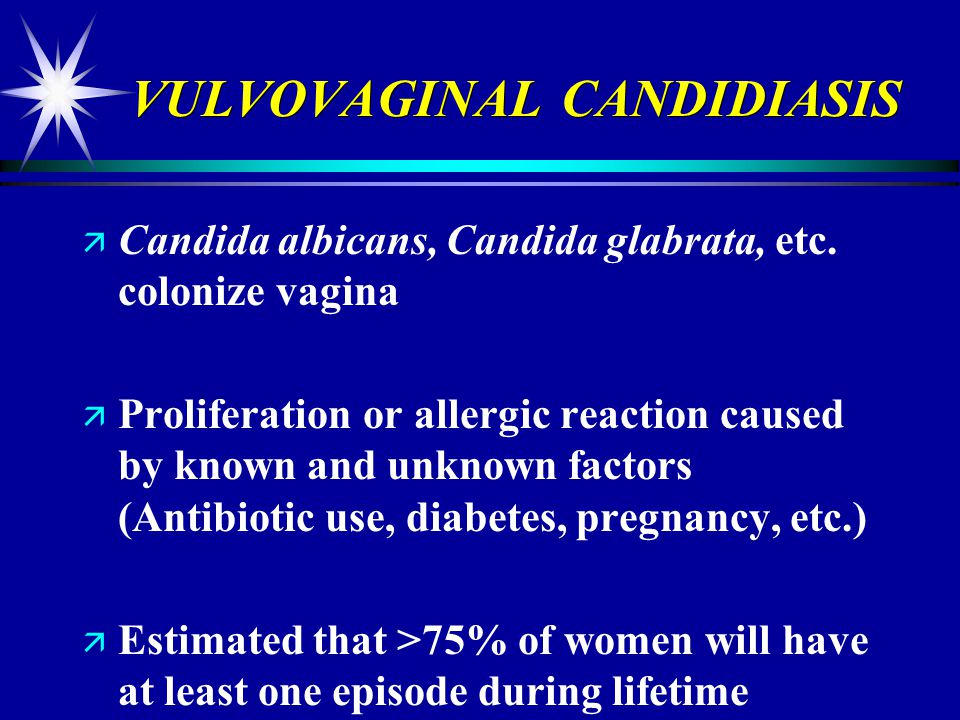
Restoration of microflora is carried out when taking probiotics (1st, 2nd, 3rd, 4th generations), prebiotics, eubiotics or fermented milk products
Prevention of vulvovaginitis
To prevent vulvovaginitis in girls it is important:
It is important to remember that vulvovaginitis of any etiology, if left untreated or self-treated, can cause serious damage to a girl's reproductive health.
BOOK YOUR APPOINTMENT
WE WILL CALL YOU BACK AS SOON
I give my consent to the processing of my personal data in accordance with Law
No. 152-FZ "On Personal Data" dated July 27, 2006 and accept the conditions
Vulvovaginitis is a problem for children and adolescents!
Vulvovaginitis is a disease often encountered in the practice of a pediatric gynecologist, and one of the most common among gynecological pathologies in girls of preschool age. Diseases account for 60 - 70% in the structure of gynecological morbidity in girls. This is due to some physiological features of the mucous membrane of the child's vagina and vulva, associated with a low level of estrogen in the blood.
Diseases account for 60 - 70% in the structure of gynecological morbidity in girls. This is due to some physiological features of the mucous membrane of the child's vagina and vulva, associated with a low level of estrogen in the blood.
As a rule, the child is disturbed by itching and burning sensations in the genital area, as well as swelling and overflow of blood vessels of the labia and surrounding skin, hyperemia of the skin of the perineum, vulvar mucosa, there may be rashes on the mucous membrane and skin of the labia, traces of scratching, thickening of the anal folds. Various vaginal discharges are observed. In vaginal smears, the number of leukocytes exceeds 30 per field of view, an abundance of flora is noted.
Infectious diseases are the main cause of the formation of the disease. They can be nonspecific or specific, which excite gonococci, chlamydia, mycobacterium tuberculosis, diphtheria bacillus and others. At an early age, the household route of transmission of the infection predominates (through household items, common areas, in violation of hygiene rules).
Classification of vulvovaginitis in girls
I. Infectious.
• Nonspecific vulvovaginitis.
• Specific vulvovaginitis: gonorrheal; tuberculosis; diphtheria.
II. Primarily non-infectious.
Vulvovaginitis caused by a foreign body in the vagina.
• Vulvovaginitis caused by worm infestation.
• Vulvovaginitis caused by onanism.
• Vulvovaginitis caused by changes in the body's reactivity:
- metabolic disorders;
- dysmetabolic nephropathy;
- allergic diseases;
- intestinal dysbacteriosis;
- diseases of the urinary tract;
- acute viral diseases;
- childhood infections.
History taking is the first step in diagnosing vulvovaginitis. It is necessary to find out the following points: the presence of concomitant diseases, provoking factors, such as a foreign body, wearing tight clothing, synthetic underwear, non-compliance with personal hygiene rules, the influence of various chemical detergents, and the onset of sexual activity.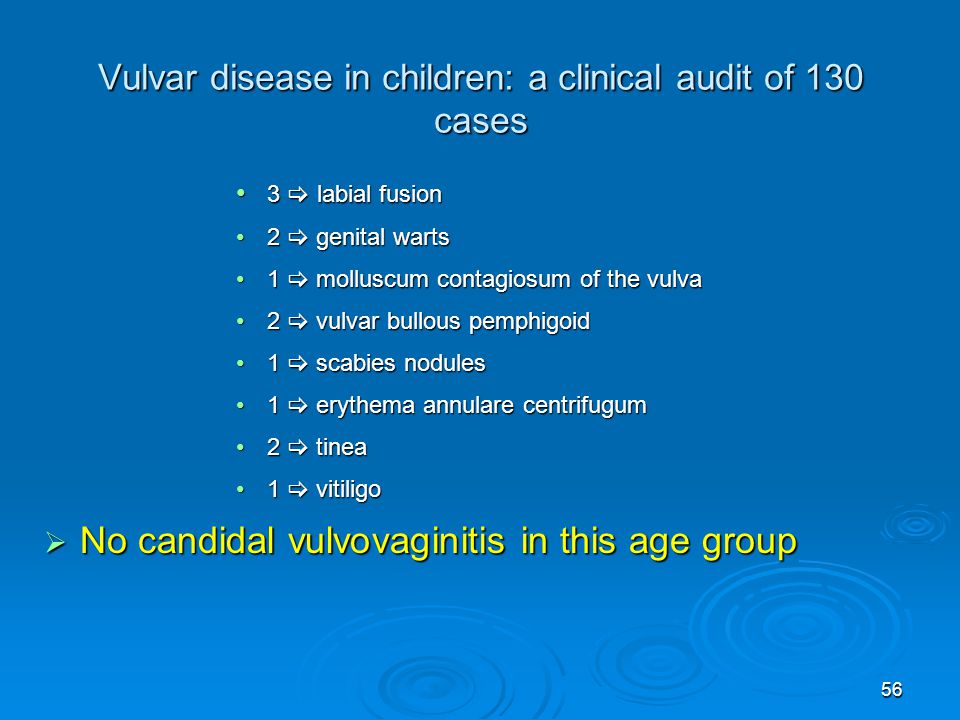 The data of the anamnesis allow to carry out the initial differential diagnosis, to determine the scope and sequence of the examination. This stage can cause some difficulties associated with the fear of a gynecological examination, especially in adolescents. In sexually active adolescents, the exclusion of STIs is mandatory. Vulvovaginitis can occur as an allergic reaction to various skin-contact chemicals and personal care products. This pathology often affects children who are not trained in appropriate personal hygiene skills. Of the laboratory tests, scraping from perianal folds for enterobiasis, fecal analysis for helminth eggs, serological blood testing for the presence of antiparasitic antibodies, as well as a clinical blood test, a general urinalysis, a Nechiporenko urinalysis and a bacteriological examination of urine with the determination of sensitivity to antibiotics are mandatory.
The data of the anamnesis allow to carry out the initial differential diagnosis, to determine the scope and sequence of the examination. This stage can cause some difficulties associated with the fear of a gynecological examination, especially in adolescents. In sexually active adolescents, the exclusion of STIs is mandatory. Vulvovaginitis can occur as an allergic reaction to various skin-contact chemicals and personal care products. This pathology often affects children who are not trained in appropriate personal hygiene skills. Of the laboratory tests, scraping from perianal folds for enterobiasis, fecal analysis for helminth eggs, serological blood testing for the presence of antiparasitic antibodies, as well as a clinical blood test, a general urinalysis, a Nechiporenko urinalysis and a bacteriological examination of urine with the determination of sensitivity to antibiotics are mandatory.
Trichomonas vulvovaginitis is more common in sexually active adolescent girls. Possible family infection of girls (if parents are sick), as well as infection of newborns (when the fetus passes through an infected birth canal).
Possible family infection of girls (if parents are sick), as well as infection of newborns (when the fetus passes through an infected birth canal).
Mycotic vulvovaginitis can occur at any age, more often in infancy, early childhood and puberty. The most common causative agent of the disease are fungi of the genus Candida. Predispose to the disease: immunodeficiency, hypovitaminosis, antibiotic treatment, endocrine disorders.
Bacterial (nonspecific) vulvovaginitis may begin acutely or have a torpid course with or without periods of exacerbation. Hyperemia of the vulva, skin of the perineum, labia, moderate vaginal discharge of a yellowish color are noted. On the skin of the thighs and around the labia there may be elements of pyoderma, on the walls of the vagina - foci of hyperemia.
Vulvovaginitis due to enterobiasis - introduction of intestinal flora into the vagina. The causative agent is Escherichia coli or Enterococcus. Careful questioning of parents helps to clarify the diagnosis. Parents note the restless sleep of the child, his complaints of itching of the skin of the perineum and external genitalia. Sometimes the child wakes up crying and screaming from pain in the vulva. Attentive parents can see the pinworm on the skin or in the feces of the child.
Careful questioning of parents helps to clarify the diagnosis. Parents note the restless sleep of the child, his complaints of itching of the skin of the perineum and external genitalia. Sometimes the child wakes up crying and screaming from pain in the vulva. Attentive parents can see the pinworm on the skin or in the feces of the child.
When examining the genitals, attention is drawn to the thickening of the anal folds, their hyperemia, traces of scratching around the anus. In such cases, it is advisable to take a scraping from the perianal folds on pinworm eggs.
Treatment. Daily washing of the vagina for 7 days, the toilet of the external genitalia and the anus and the introduction of suppositories with an antibiotic to which the pathogenic flora is sensitive. At the same time it is necessary to carry out the therapy of enterobiasis. For this purpose, pyrantel or other drugs that kill pinworms. Parents should pay attention to defects in the child's hygiene, to the possibility of enterobiasis affecting the whole family (in connection with which it is strongly recommended to treat enterobiasis to all family members), as well as to the daily toilet of the child's external genital organs.
Parents of girls with vulvovaginitis due to a foreign body of the vagina complain of profuse bloody-purulent discharge . Abundant discharge leads to maceration of the skin of the perineum and pyoderma. Recto-abdominal examination and vaginoscopy can detect inor one body of the vagina, usually surrounded by decaying granulations. Vaginoscopy or examination in children's vaginal mirrors is very important to clarify the diagnosis and conduct a differential diagnosis with vaginal sarcoma, which is usually observed in girls 2 to 4 years old and can be manifested by bloody-purulent discharge. However, with this severe malignant disease, grape-like growths are visible in the vagina, the decay of which causes sanious discharge.
Treatment - removal of a foreign body. After removing the foreign body, the vagina is washed with a disinfectant solution. The toilet of the vagina within 2 - 3 days usually leads to a cure for the inflammatory process.
Atopic vulvovaginitis observed in girls with exudative diathesis, with allergic manifestations. They may experience a sluggish, sometimes subsiding, sometimes exacerbating inflammatory process. When examining the genital organs, scanty leucorrhoea, thinning of the mucous membrane, "dryness", focal hyperemia of the vulva are noted. In the vagina, a diverse flora is determined, often conditionally pathogenic. Treatment. First of all, it is necessary to eliminate contact with the allergen, adjust the diet, exclude foods that cause diathesis. Antihistamines are prescribed. Local treatment includes baths of medicinal herbs (chamomile, oak bark, etc.), applying ointments to the area of the external genital organs.
They may experience a sluggish, sometimes subsiding, sometimes exacerbating inflammatory process. When examining the genital organs, scanty leucorrhoea, thinning of the mucous membrane, "dryness", focal hyperemia of the vulva are noted. In the vagina, a diverse flora is determined, often conditionally pathogenic. Treatment. First of all, it is necessary to eliminate contact with the allergen, adjust the diet, exclude foods that cause diathesis. Antihistamines are prescribed. Local treatment includes baths of medicinal herbs (chamomile, oak bark, etc.), applying ointments to the area of the external genital organs.
Chlamydia vulvovaginitis is characterized by a long course, often at the same time inflammation of the mucous membrane of the eyes and joints is detected in girls. The causative agent is detected by immunological methods and by examining the cells of vaginal smears for the presence of chlamydia. Antibiotics, interferon in suppositories, eubiotics are prescribed.
Personal hygiene of the girl and hygiene in the family, as well as timely and complete treatment of inflammatory diseases of the genital organs in spouses are very important. All this is an effective measure to preserve the health of children.
Treatment is aimed at eliminating the etiological factor causing vulvovaginitis, and should include both consultation of parents and the child regarding personal hygiene rules, and the appointment of adequate therapy. Treatment of nonspecific vulvovaginitis in children should be comprehensive and include several mandatory steps. The first stage is the sanitation of foci of extragenital infection. If necessary, treatment can be supplemented with the appointment of drugs for immunocorrection and desensitization. At the second stage, etiotropic antibiotic therapy is carried out, based on the sensitivity of the isolated microflora to antibiotics. To alleviate the symptoms of vulvitis, local therapy is prescribed in the form of irrigations and baths using broad-spectrum antibiotics, antiseptics (furatsilin, chlorhexidine), including herbal remedies based on calendula, chamomile, plantain, sage, 3% hydrogen peroxide solution.