How to treat uti in pregnancy
Urinary Tract Infections During Pregnancy
JOHN E. DELZELL, JR., M.D., AND MICHAEL L. LEFEVRE, M.D., M.S.P.H.
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2000;61(3):713-720
See related patient information handout on urinary tract infections during pregnancy, written by the authors of this article.
Urinary tract infections are common during pregnancy, and the most common causative organism is Escherichia coli. Asymptomatic bacteriuria can lead to the development of cystitis or pyelonephritis. All pregnant women should be screened for bacteriuria and subsequently treated with antibiotics such as nitrofurantoin, sulfisoxazole or cephalexin. Ampicillin should no longer be used in the treatment of asymptomatic bacteriuria because of high rates of resistance. Pyelonephritis can be a life-threatening illness, with increased risk of perinatal and neonatal morbidity. Recurrent infections are common during pregnancy and require prophylactic treatment. Pregnant women with urinary group B streptococcal infection should be treated and should receive intrapartum prophylactic therapy.
Urinary tract infections (UTIs) are frequently encountered in the family physician's office. UTIs account for approximately 10 percent of office visits by women, and 15 percent of women will have a UTI at some time during their life. In pregnant women, the incidence of UTI can be as high as 8 percent. 1,2 This article briefly examines the pathogenesis and bacteriology of UTIs during pregnancy, as well as patient-oriented outcomes. We review the diagnosis and treatment of asymptomatic bacteriuria, acute cystitis and pyelonephritis, plus the unique issues of group B streptococcus and recurrent infections.
1,2 This article briefly examines the pathogenesis and bacteriology of UTIs during pregnancy, as well as patient-oriented outcomes. We review the diagnosis and treatment of asymptomatic bacteriuria, acute cystitis and pyelonephritis, plus the unique issues of group B streptococcus and recurrent infections.
Pathogenesis
Pregnant women are at increased risk for UTIs. Beginning in week 6 and peaking during weeks 22 to 24, approximately 90 percent of pregnant women develop ureteral dilatation, which will remain until delivery (hydronephrosis of pregnancy). Increased bladder volume and decreased bladder tone, along with decreased ureteral tone, contribute to increased urinary stasis and ureterovesical reflux.1 Additionally, the physiologic increase in plasma volume during pregnancy decreases urine concentration. Up to 70 percent of pregnant women develop glycosuria, which encourages bacterial growth in the urine. Increases in urinary progestins and estrogens may lead to a decreased ability of the lower urinary tract to resist invading bacteria. This decreased ability may be caused by decreased ureteral tone or possibly by allowing some strains of bacteria to selectively grow.1,3 These factors may all contribute to the development of UTIs during pregnancy.
This decreased ability may be caused by decreased ureteral tone or possibly by allowing some strains of bacteria to selectively grow.1,3 These factors may all contribute to the development of UTIs during pregnancy.
Bacteriology
The organisms that cause UTIs during pregnancy are the same as those found in nonpregnant patients. Escherichia coli accounts for 80 to 90 percent of infections. Other gram-negative rods such as Proteus mirabilis and Klebsiella pneumoniae are also common. Gram-positive organisms such as group B streptococcus and Staphylococcus saprophyticus are less common causes of UTI. Group B streptococcus has important implications in the management of pregnancy and will be discussed further. Less common organisms that may cause UTI include enterococci, Gardnerella vaginalis and Ureaplasma ureolyticum.1,4,5
Diagnosis and Treatment of UTIs
UTIs have three principle presentations: asymptomatic bacteriuria, acute cystitis and pyelonephritis.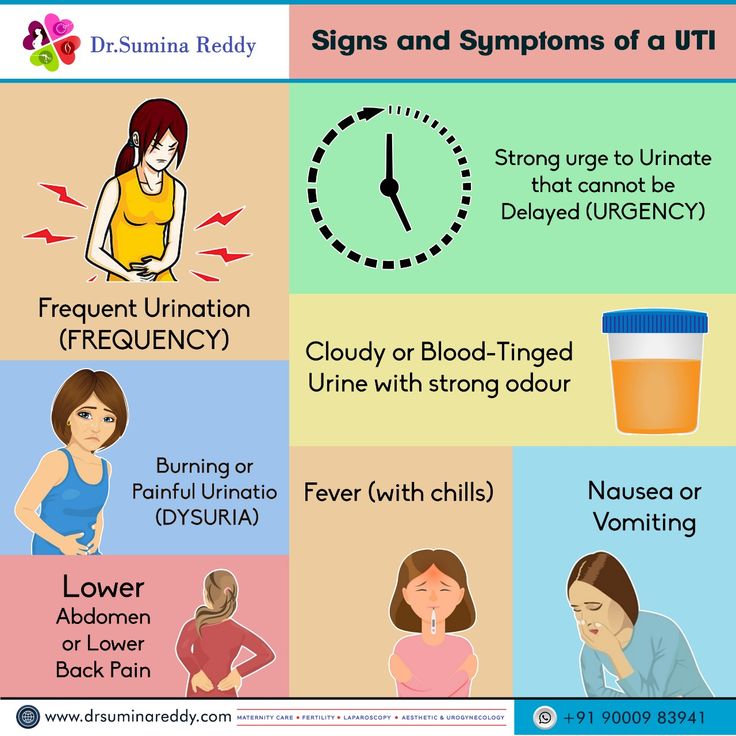 The diagnosis and treatment of UTI depends on the presentation.
The diagnosis and treatment of UTI depends on the presentation.
ASYMPTOMATIC BACTERIURIA
[ corrected] Significant bacteriuria may exist in asymptomatic patients. In the 1960s, Kass6 noted the subsequent increased risk of developing pyelonephritis in patients with asymptomatic bacteriuria. Significant bacteriuria has been historically defined as finding more than 105 colony-forming units per mL of urine.7 Recent studies of women with acute dysuria have shown the presence of significant bacteriuria with lower colony counts. This has not been studied in pregnant women, and finding more than 105 colony-forming units per mL of urine remains the commonly accepted standard. Asymptomatic bacteriuria is common, with a prevalence of 10 percent during pregnancy.6,8 Thus, routine screening for bacteriuria is advocated.
Untreated asymptomatic bacteriuria leads to the development of symptomatic cystitis in approximately 30 percent of patients and can lead to the development of pyelonephritis in up to 50 percent. 6 Asymptomatic bacteriuria is associated with an increased risk of intra-uterine growth retardation and low-birth-weight infants.9 The relatively high prevalence of asymptomatic bacteriuria during pregnancy, the significant consequences for women and for the pregnancy, plus the ability to avoid sequelae with treatment, justify screening pregnant women for bacteriuria.
6 Asymptomatic bacteriuria is associated with an increased risk of intra-uterine growth retardation and low-birth-weight infants.9 The relatively high prevalence of asymptomatic bacteriuria during pregnancy, the significant consequences for women and for the pregnancy, plus the ability to avoid sequelae with treatment, justify screening pregnant women for bacteriuria.
SCREENING
The American College of Obstetrics and Gynecology recommends that a urine culture be obtained at the first prenatal visit.10 A repeat urine culture should be obtained during the third trimester, because the urine of treated patients may not remain sterile for the entire pregnancy.10 The recommendation of the U.S. Preventative Services Task Force is to obtain a urine culture between 12 and 16 weeks of gestation (an “A” recommendation).11
By screening for and aggressively treating pregnant women with asymptomatic bacteriuria, it is possible to significantly decrease the annual incidence of pyelonephritis during pregnancy. 8,12 In randomized controlled trials, treatment of pregnant women with asymptomatic bacteriuria has been shown to decrease the incidence of preterm birth and low-birth-weight infants.13
8,12 In randomized controlled trials, treatment of pregnant women with asymptomatic bacteriuria has been shown to decrease the incidence of preterm birth and low-birth-weight infants.13
Rouse and colleagues14 performed a cost-benefit analysis of screening for bacteriuria in pregnant women versus inpatient treatment of pyelonephritis and found a substantial decrease in overall cost with screening. The cost of screening for bacteriuria to prevent the development of pyelonephritis in one patient was $1,605, while the cost of treating one patient with pyelonephritis was $2,485. Wadland and Plante15 performed a similar analysis in a family practice obstetric population and found screening for asymptomatic bacteriuria to be cost-effective.
The decision about how to screen asymptomatic women for bacteriuria is a balance between the cost of screening versus the sensitivity and specificity of each test. The gold standard for detection of bacteriuria is urine culture, but this test is costly and takes 24 to 48 hours to obtain results. The accuracy of faster screening methods (e.g., leukocyte esterase dipstick, nitrite dipstick, urinalysis and urine Gram staining) has been evaluated (Table 116). Bachman and associates16 compared these screening methods with urine culture and found that while it was more cost effective to screen for bacteriuria with the esterase dipstick for leukocytes, only one half of the patients with bacteriuria were identified compared with screening by urine culture. The increased number of false negatives and the relatively poor predictive value of a positive test make the faster methods less useful; therefore, a urine culture should be routinely obtained in pregnant women to screen for bacteriuria at the first prenatal visit and during the third trimester.10,11
The accuracy of faster screening methods (e.g., leukocyte esterase dipstick, nitrite dipstick, urinalysis and urine Gram staining) has been evaluated (Table 116). Bachman and associates16 compared these screening methods with urine culture and found that while it was more cost effective to screen for bacteriuria with the esterase dipstick for leukocytes, only one half of the patients with bacteriuria were identified compared with screening by urine culture. The increased number of false negatives and the relatively poor predictive value of a positive test make the faster methods less useful; therefore, a urine culture should be routinely obtained in pregnant women to screen for bacteriuria at the first prenatal visit and during the third trimester.10,11
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
TREATMENT
Pregnant women should be treated when bacteriuria is identified (Table 217,18). The choice of antibiotic should address the most common infecting organisms (i.e., gram-negative gastrointestinal organisms). The antibiotic should also be safe for the mother and fetus. Historically, ampicillin has been the drug of choice, but in recent years E. coli has become increasingly resistant to ampicillin.19 Ampicillin resistance is found in 20 to 30 percent of E. coli cultured from urine in the out-patient setting.20 Nitrofurantoin (Macrodantin) is a good choice because of its high urinary concentration. Alternatively, cephalosporins are well tolerated and adequately treat the important organisms. Fosfomycin (Monurol) is a new antibiotic that is taken as a single dose. Sulfonamides can be taken during the first and second trimesters but, during the third trimester, the use of sulfonamides carries a risk that the infant will develop kernicterus, especially preterm infants. Other common antibiotics (e.g., fluoroquinolones and tetracyclines) should not be prescribed during pregnancy because of possible toxic effects on the fetus.
The choice of antibiotic should address the most common infecting organisms (i.e., gram-negative gastrointestinal organisms). The antibiotic should also be safe for the mother and fetus. Historically, ampicillin has been the drug of choice, but in recent years E. coli has become increasingly resistant to ampicillin.19 Ampicillin resistance is found in 20 to 30 percent of E. coli cultured from urine in the out-patient setting.20 Nitrofurantoin (Macrodantin) is a good choice because of its high urinary concentration. Alternatively, cephalosporins are well tolerated and adequately treat the important organisms. Fosfomycin (Monurol) is a new antibiotic that is taken as a single dose. Sulfonamides can be taken during the first and second trimesters but, during the third trimester, the use of sulfonamides carries a risk that the infant will develop kernicterus, especially preterm infants. Other common antibiotics (e.g., fluoroquinolones and tetracyclines) should not be prescribed during pregnancy because of possible toxic effects on the fetus.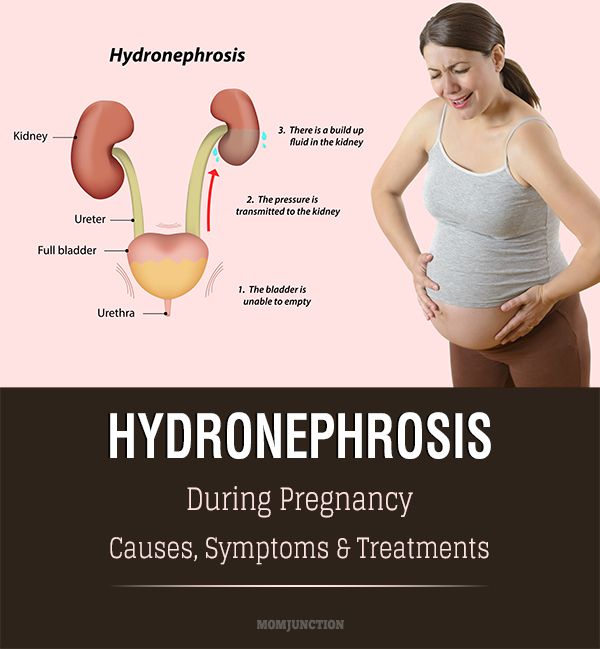
| Antibiotic | Pregnancy category | Dosage |
|---|---|---|
| Cephalexin (Keflex) | B | 250 mg two or four times daily |
| Erythromycin | B | 250 to 500 mg four times daily |
| Nitrofurantoin (Macrodantin) | B | 50 to 100 mg four times daily |
| Sulfisoxazole (Gantrisin) | C* | 1 g four times daily |
| Amoxicillin-clavulanic acid (Augmentin) | B | 250 mg four times daily |
| Fosfomycin (Monurol) | B | One 3-g sachet |
| Trimethoprim-sulfamethoxazole (Bactrim) | C† | 160/180 mg twice daily |
A seven- to 10-day course of antibiotic treatment is usually sufficient to eradicate the infecting organism(s). Some authorities have advocated shorter courses of treatment—even single-day therapy. Conflicting evidence remains as to whether pregnant patients should be treated with shorter courses of antibiotics. Masterton21 demonstrated a cure rate of 88 percent with a single 3-g dose of ampicillin in ampicillin-sensitive isolates. Several other studies have found that a single dose of amoxicillin, cephalexin (Keflex) or nitrofurantoin was less successful in eradicating bacteriuria, with cure rates from 50 to 78 percent.1,22–24 Fosfomycin is effective when taken as a single, 3-g sachet.
Some authorities have advocated shorter courses of treatment—even single-day therapy. Conflicting evidence remains as to whether pregnant patients should be treated with shorter courses of antibiotics. Masterton21 demonstrated a cure rate of 88 percent with a single 3-g dose of ampicillin in ampicillin-sensitive isolates. Several other studies have found that a single dose of amoxicillin, cephalexin (Keflex) or nitrofurantoin was less successful in eradicating bacteriuria, with cure rates from 50 to 78 percent.1,22–24 Fosfomycin is effective when taken as a single, 3-g sachet.
Other antibiotics have not been extensively researched for use in UTIs, and further studies are necessary to determine whether a shorter course of other antibiotics would be as effective as the traditional treatment length.1 After patients have completed the treatment regimen, a repeat culture should be obtained to document successful eradication of bacteriuria.10
Acute Cystitis
Acute cystitis is distinguished from asymptomatic bacteriuria by the presence of symptoms such as dysuria, urgency and frequency in afebrile patients with no evidence of systemic illness. Up to 30 percent of patients with untreated asymptomatic bacteriuria later develop symptomatic cystitis.6 Over a six-year period, Harris and Gilstrap25 found that 1.3 percent of obstetric patients who delivered at a single hospital developed acute cystitis with no symptoms of pyelonephritis.
Up to 30 percent of patients with untreated asymptomatic bacteriuria later develop symptomatic cystitis.6 Over a six-year period, Harris and Gilstrap25 found that 1.3 percent of obstetric patients who delivered at a single hospital developed acute cystitis with no symptoms of pyelonephritis.
TREATMENT
In general, treatment of pregnant patients with acute cystitis is initiated before the results of the culture are available. Antibiotic choice, as in asymptomatic bacteriuria, should focus on coverage of the common pathogens and can be changed after the organism is identified and sensitivities are determined. A three-day treatment course in nonpregnant patients with acute cystitis has a cure rate similar to a treatment course of seven to 10 days, but this finding has not been studied in the obstetric population.1 Patients treated for a shorter time frame are more likely to have a recurrence of the infection. In the pregnant patient, this higher rate of recurrence with shorter treatment periods may have serious consequences. Table 217,18 lists oral antibiotics that are acceptable treatment choices. Group B streptococcus is generally susceptible to penicillin, but E. coli and other gram-negative rods typically have a high rate of resistance to this agent.
Table 217,18 lists oral antibiotics that are acceptable treatment choices. Group B streptococcus is generally susceptible to penicillin, but E. coli and other gram-negative rods typically have a high rate of resistance to this agent.
Pyelonephritis
Acute pyelonephritis during pregnancy is a serious systemic illness that can progress to maternal sepsis, preterm labor and premature delivery. The diagnosis is made when the presence of bacteriuria is accompanied by systemic symptoms or signs such as fever, chills, nausea, vomiting and flank pain. Symptoms of lower tract infection (i.e., frequency and dysuria) may or may not be present. Pyelonephritis occurs in 2 percent of pregnant women; up to 23 percent of these women have a recurrence during the same pregnancy.26
Early, aggressive treatment is important in preventing complications from pyelonephritis. Hospitalization, although often indicated, is not always necessary. However, hospitalization is indicated for patients who are exhibiting signs of sepsis, who are vomiting and unable to stay hydrated, and who are having contractions. A randomized study of 90 obstetric inpatients with pyelonephritis compared treatment with oral cephalexin to treatment with intravenous cephalothin (Keflin) and found no difference between the two groups in the success of therapy, infant birth weight or preterm deliveries.27
A randomized study of 90 obstetric inpatients with pyelonephritis compared treatment with oral cephalexin to treatment with intravenous cephalothin (Keflin) and found no difference between the two groups in the success of therapy, infant birth weight or preterm deliveries.27
Further support for outpatient therapy is provided in a randomized clinical trial that compared standard inpatient, intravenous treatment to outpatient treatment with intramuscular ceftriaxone (Rocephin) plus oral cephalexin.28 Response to antibiotic therapy in each group was similar, with no evident differences in the number of recurrent infections or preterm deliveries.
Antibiotic therapy (and intravenous fluids, if hospitalization is required) may be initiated before obtaining the results of urine culture and sensitivity. Several antibiotic regimens may be used. A clinical trial comparing three parenteral regimens found no differences in length of hospitalization, recurrence of pyelonephritis or preterm delivery. 29 Patients in this trial were randomized to receive treatment with intravenous cefazolin (Ancef), intravenous gentamycin plus ampicillin, or intramuscular ceftriaxone.
29 Patients in this trial were randomized to receive treatment with intravenous cefazolin (Ancef), intravenous gentamycin plus ampicillin, or intramuscular ceftriaxone.
Parenteral treatment of pyelonephritis should be continued until the patient becomes afebrile. Most patients respond to hydration and prompt antibiotic treatment within 24 to 48 hours. The most common reason for initial treatment failure is resistance of the infecting organism to the antibiotic. If fever continues or other signs of systemic illness remain after appropriate antibiotic therapy, the possibility of a structural or anatomic abnormality should be investigated. Persistent infection may be caused by urolithiasis, which occurs in one of 1,500 pregnancies,30 or less commonly, congenital renal abnormalities or a perinephric abscess.
Diagnostic tests may include renal ultrasonography or an abbreviated intravenous pyelogram. The indication to perform an intravenous pyelogram is persistent infection after appropriate antibiotic therapy when there is the suggestion of a structural abnormality not evident on ultrasonography. 30 Even the low-dose radiation involved in an intravenous pyelogram, however, may be dangerous to the fetus and should be avoided if possible.
30 Even the low-dose radiation involved in an intravenous pyelogram, however, may be dangerous to the fetus and should be avoided if possible.
Group B Streptococcal Infection
Group B streptococcal (GBS) vaginal colonization is known to be a cause of neonatal sepsis and is associated with preterm rupture of membranes, and preterm labor and delivery. GBS is found to be the causative organism in UTIs in approximately 5 percent of patients.31,32 Evidence that GBS bacteriuria increases patient risk of preterm rupture of membranes and premature delivery is mixed.33,34 A randomized, controlled trial35 compared the treatment of GBS bacteriuria with penicillin to treatment with placebo. Results indicated a significant reduction in rates of premature rupture of membranes and preterm delivery in the women who received antibiotics. It is unclear if GBS bacteriuria is equivalent to GBS vaginal colonization, but pregnant women with GBS bacteriuria should be treated as GBS carriers and should receive a prophylactic antibiotic during labor.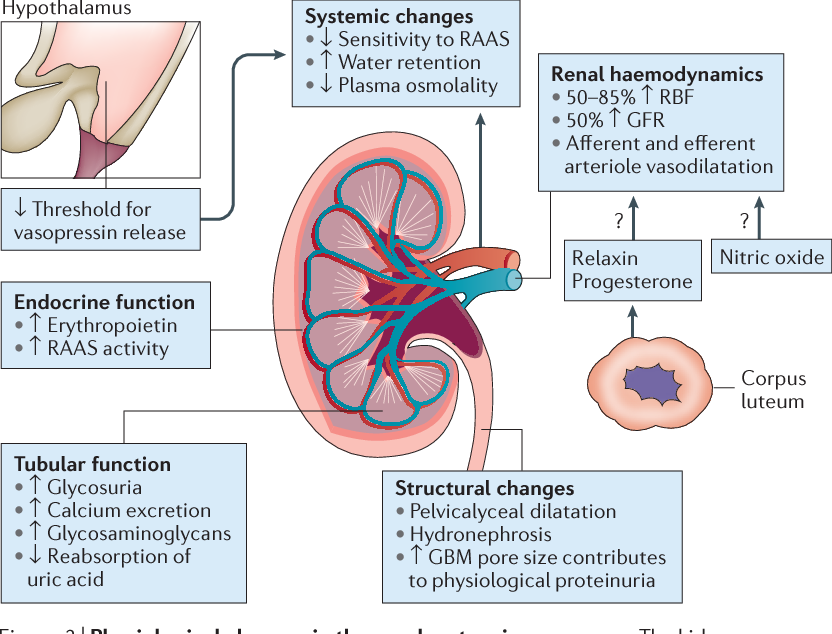 36
36
Recurrence and Prophylaxis
The majority of UTIs are caused by gastrointestinal organisms. Even with appropriate treatment, the patient may experience a reinfection of the urinary tract from the rectal reservoir. UTIs recur in approximately 4 to 5 percent of pregnancies, and the risk of developing pyelonephritis is the same as the risk with primary UTIs. A single, postcoital dose or daily suppression with cephalexin or nitrofurantoin in patients with recurrent UTIs is effective preventive therapy.37 A postpartum urologic evaluation may be necessary in patients with recurrent infections because they are more likely to have structural abnormalities of the renal system.26,30,38 Patients who are found to have urinary stones, who have more than one recurrent UTI or who have a recurrent UTI while on suppressive antibiotic therapy should undergo a postpartum evaluation.30,38
Outcomes
The maternal and neonatal complications of a UTI during pregnancy can be devastating. Thirty percent of patients with untreated asymptomatic bacteriuria develop symptomatic cystitis and up to 50 percent develop pyelonephritis.6 Asymptomatic bacteriuria is also associated with intrauterine growth retardation and low-birth-weight infants.9 Schieve and associates39 conducted a study involving 25,746 pregnant women and found that the presence of UTI was associated with premature labor (labor onset before 37 weeks of gestation), hypertensive disorders of pregnancy (such as pregnancy-induced hypertension and preeclampsia), anemia (hematocrit level less than 30 percent) and amnionitis (Table 337). While this does not prove a cause and effect relationship, randomized trials have demonstrated that antibiotic treatment decreases the incidence of preterm birth and low-birth-weight infants.13 A risk of urosepsis and chronic pyelonephritis was also found.40 In addition, acute pyelonephritis has been associated with anemia.
Thirty percent of patients with untreated asymptomatic bacteriuria develop symptomatic cystitis and up to 50 percent develop pyelonephritis.6 Asymptomatic bacteriuria is also associated with intrauterine growth retardation and low-birth-weight infants.9 Schieve and associates39 conducted a study involving 25,746 pregnant women and found that the presence of UTI was associated with premature labor (labor onset before 37 weeks of gestation), hypertensive disorders of pregnancy (such as pregnancy-induced hypertension and preeclampsia), anemia (hematocrit level less than 30 percent) and amnionitis (Table 337). While this does not prove a cause and effect relationship, randomized trials have demonstrated that antibiotic treatment decreases the incidence of preterm birth and low-birth-weight infants.13 A risk of urosepsis and chronic pyelonephritis was also found.40 In addition, acute pyelonephritis has been associated with anemia. 41
41
| Outcome | Odds ratio | 95% confidence interval | ||
|---|---|---|---|---|
| Perinatal | ||||
| Low birth weight (weight less than 2,500 g [5 lb, 8 oz]) | 1.4 | 1.2 to 1.6 | ||
| Prematurity (less than 37 weeks of gestation at delivery) | 1.3 | 1.1 to 1.4 | ||
| Preterm low birth weight (weight less than 2,500 g and less than 37 weeks of gestation at delivery) | 1.5 | 1.2 to 1.7 | ||
| Maternal | ||||
| Premature labor (less than 37 weeks of gestation at delivery) | 1.6 | 1.4 to 1. 8 8 | ||
| Hypertension/preeclampsia | 1.4 | 1.2 to 1.7 | ||
| Anemia (hematocrit level less than 30%) | 1.6 | 1.3 to 2.0 | ||
| Amnionitis (chorioamnionitis, amnionitis) | 1.4 | 1.1 to 1.9 | ||
Neonatal outcomes that are associated with UTI include sepsis and pneumonia (specifically, group B streptococcus infection).31,42 UTI increases the risk of low-birth-weight infants (weight less than 2,500 g [5 lb, 8 oz]), prematurity (less than 37 weeks of gestation at delivery) and preterm, low-birth-weight infants (weight less than 2,500 g and less than 37 weeks of gestation at delivery)39(Table 337).
Final Comment
UTIs during pregnancy are a common cause of serious maternal and perinatal morbidity; with appropriate screening and treatment, this morbidity can be limited. A UTI may manifest as asymptomatic bacteriuria, acute cystitis or pyelonephritis. All pregnant women should be screened for bacteriuria and subsequently treated with appropriate antibiotic therapy. Acute cystitis and pyelonephritis should be aggressively treated during pregnancy. Oral nitrofurantoin and cephalexin are good antibiotic choices for treatment in pregnant women with asymptomatic bacteriuria and acute cystitis, but parenteral antibiotic therapy may be required in women with pyelonephritis.
A UTI may manifest as asymptomatic bacteriuria, acute cystitis or pyelonephritis. All pregnant women should be screened for bacteriuria and subsequently treated with appropriate antibiotic therapy. Acute cystitis and pyelonephritis should be aggressively treated during pregnancy. Oral nitrofurantoin and cephalexin are good antibiotic choices for treatment in pregnant women with asymptomatic bacteriuria and acute cystitis, but parenteral antibiotic therapy may be required in women with pyelonephritis.
UTI During Pregnancy: How to Treat
UTI During Pregnancy: How to Treat- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Janine Kelbach, RNC-OB — By Chaunie Brusie on January 7, 2017
About halfway through my fourth pregnancy, my OB-GYN informed me that I had a urinary tract infection (UTI). I would need to be treated with antibiotics.
I would need to be treated with antibiotics.
I was surprised I’d tested positive for a UTI. I had no symptoms, so I didn’t think that I could have an infection. The doctor discovered it based on my routine urine test.
After four pregnancies, I had started to think that they were just making us preggos pee in a cup for fun. But I guess there’s a purpose to it. Who knew?
A UTI occurs when bacteria from somewhere outside of a woman’s body gets inside her urethra (basically the urinary tract) and causes an infection.
Women are more likely to get UTIs than men. The female anatomy makes it easy for bacteria from the vagina or rectal areas to get in the urinary tract because they are all close together.
UTIs are common during pregnancy. That’s because the growing fetus can put pressure on the bladder and urinary tract. This traps bacteria or causes urine to leak.
There are also physical changes to consider. As early as six weeks gestation, almost all pregnant women experience ureteral dilation, when the urethra expands and continues to expand until delivery.
The larger urinary tract, along with increased bladder volume and decreased bladder tone, all cause the urine to become more still in the urethra. This allows bacteria to grow.
To make matters worse, a pregnant woman’s urine gets more concentrated. It also has certain types of hormones and sugar. These can encourage bacterial growth and lower your body’s ability to fight off “bad” bacteria trying to get in.
Signs and symptoms of a UTI include:
- burning or painful urination
- cloudy or blood-tinged urine
- pelvic or lower back pain
- frequent urination
- feeling that you have to urinate frequently
- fever
- nausea or vomiting
Between 2 and 10 percent of pregnant women experience a UTI. Even more worrisome, UTIs tend to reoccur frequently during pregnancy.
Women who’ve had UTIs before are more prone to get them during pregnancy. The same goes for women who’ve had several children.
Any infection during pregnancy can be extremely dangerous for you and your baby. That’s because infections increase the risk of premature labor.
That’s because infections increase the risk of premature labor.
I found out the hard way that an untreated UTI during pregnancy can also wreak havoc after you deliver. After I had my first daughter, I woke up a mere 24 hours after coming home with a fever approaching 105˚F (41˚c).
I landed back in the hospital with a raging infection from an undiagnosed UTI, a condition called pyelonephritis. Pyelonephritis can be a life-threatening illness for both mother and baby. It had spread to my kidneys, and they suffered permanent damage as a result.
Moral of the story? Let your doctor know if you have any symptoms of a UTI during pregnancy. If you’re prescribed antibiotics, be sure to take every last pill to knock out that infection.
You can help prevent UTIs during your pregnancy by:
- emptying your bladder frequently, especially before and after sex
- wearing only cotton underwear
- nixing underwear at night
- avoiding douches, perfumes, or sprays
- drinking plenty of water to stay hydrated
- avoiding any harsh soaps or body wash in the genital area
Most UTIs during pregnancy are treated with a course of antibiotics. Your doctor will prescribe an antibiotic that is pregnancy-safe but still effective in killing off bacteria in your body.
Your doctor will prescribe an antibiotic that is pregnancy-safe but still effective in killing off bacteria in your body.
If your UTI has progressed to a kidney infection, you may need to take a stronger antibiotic or have an intravenous (IV) version administered.
Share on Pinterest
Last medically reviewed on January 8, 2017
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chen YK, et al. (2010). No increased risk of adverse pregnancy outcomes in women with urinary tract infections: A nationwide population‐based study. DOI:
10.3109/00016349.2010. 486826
486826 - Delzell JE, et al. (2000). Urinary tract infections during pregnancy.
aafp.org/afp/2000/0201/p713.html - Managing urinary tract infections in pregnancy. (2011).
bpac.org.nz/BPJ/2011/april/pregnant-uti.aspx - Matuszkiewicz-Rowinska J, et al. (2015). Urinary tract infections in pregnancy: Old and new unresolved diagnostic and therapeutic problems. DOOI:
10.5114/aoms.2013.39202 - Urinary tract infections (UTIs). (2015).
acog.org/~/media/For%20Patients/faq050.pdf/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Janine Kelbach, RNC-OB — By Chaunie Brusie on January 7, 2017
related stories
6 Home Remedies for Urinary Tract Infections (UTIs)
Infections in Pregnancy
When to Be Concerned by Pregnancy Cramps
8 Ways To Get Rid of UTIs Without Antibiotics
Can I Use Baking Soda to Treat a UTI?
Read this next
6 Home Remedies for Urinary Tract Infections (UTIs)
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COILearn about six home remedies that can help prevent UTIs (urinary tract infections).
READ MORE
Infections in Pregnancy
Medically reviewed by Nicole Galan, RN
Pregnancy can make women more prone to infection. Here’s a list of common complications and options for treatment.
READ MORE
When to Be Concerned by Pregnancy Cramps
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Normal stomach aches and pains are par for the course during pregnancy, but severe cramping can be dangerous. Here’s a look at when to be concerned.
READ MORE
8 Ways To Get Rid of UTIs Without Antibiotics
Medically reviewed by Alexandra Perez, PharmD, MBA, BCGP
Is treating a UTI without antibiotics possible? Because of antibiotic resistance, more and more people are seeking out alternative treatments for UTIs.

READ MORE
Can I Use Baking Soda to Treat a UTI?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Find out if baking soda can really help treat urinary infections, and learn why it may be dangerous.
READ MORE
Prenatal Care: Urinary Frequency and Thirst
Medically reviewed by University of Illinois
There are many symptoms that come with pregnancy. One is the seemingly never-ending urge to urinate – even if you’ve just gone a few minutes prior.
READ MORE
Irritable Uterus and Irritable Uterus Contractions: Causes, Symptoms, Treatment
Medically reviewed by Katie Mena, MD
Some women get regular contractions throughout pregnancy, meaning they have an irritable uterus. Here’s what’s normal and when to call your doctor.

READ MORE
Chronic Urinary Tract Infection (UTI)
Medically reviewed by Graham Rogers, M.D.
Chronic urinary tract infections (UTIs) are infections of the urinary tract that don’t respond to treatment.
READ MORE
Why Am I Experiencing Urinary Incontinence?
Medically reviewed by Matt Coward, MD, FACS
Urinary incontinence happens when you lose control of your bladder. Discover potential causes, treatments, prevention tips, and more.
READ MORE
UTIs in Adults: Everything You Need to Know
Learn about different types and treatments of urinary tract infections, the risk factors, and prevention for both men and women.
READ MORE
Bacteriuria, cystitis and pyelonephritis during pregnancy
The human urinary system consists of two kidneys that filter the blood plasma and remove part of the liquid and some substances dissolved in it into the urine, two ureters that conduct urine from the kidneys to the bladder, the bladder that serves as a reservoir for urine, and the urethra through which urine is excreted from the body.
During pregnancy, several changes occur in the urinary system that increase the risk of urinary tract infection. The acidity of urine changes, urine becomes more alkaline (its pH rises), and this creates a more favorable environment for the development of bacteria, slows down the passage of urine and creates conditions for reflux (reverse reflux) of urine, so that bacteria can be transported with urine from the underlying sections to the overlying ones. , to the renal pelvis. In addition, perfectly normal during pregnancy changes in the functioning of the immune system also reduce the body's ability to fight infection.
Thus, we see that pregnant women are more predisposed to developing urinary tract infections than their non-pregnant peers.
Asymptomatic bacteriuria
Asymptomatic bacteriuria is the presence of bacteria in the urine without signs of an inflammatory process.
Normally, our urine is sterile, and bacteria, even if they pass from the rectum to the bladder through the urethra, are washed out with the urine stream the next time we urinate. During pregnancy, very comfortable conditions are created for bacteria, and they can linger in the bladder, multiply, attach to the walls of the urinary tract, causing inflammation, and even throw into the renal pelvis. nine0003
During pregnancy, very comfortable conditions are created for bacteria, and they can linger in the bladder, multiply, attach to the walls of the urinary tract, causing inflammation, and even throw into the renal pelvis. nine0003
If bacteria and, in particular, nitrites, a product of the decomposition of urine urea by bacteria living in it, are detected in a general urine test during pregnancy, a urine culture is required to determine the pathogen, its amount (titer) and antibiotics to which it is sensitive.
Approximately thirty percent, that is, one in three pregnant women with asymptomatic bacteriuria without treatment, develop gestational (pregnancy-related) pyelonephritis during the same pregnancy. Therefore, asymptomatic bacteriuria during pregnancy always requires treatment. All urinary tract infections during pregnancy are treated antibacterial drugs.
Select drugs that are compatible with pregnancy and are safe enough for the fetus to be used at that time.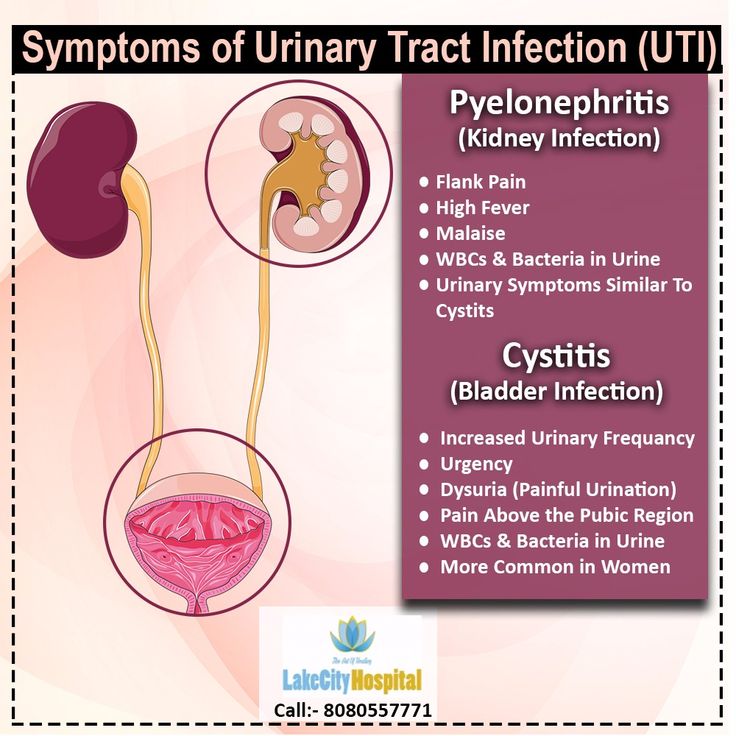 The sensitivity of the pathogen to the antibiotic is also taken into account. Phytotherapeutic drugs for the treatment of urinary tract infections during pregnancy should not be used.
The sensitivity of the pathogen to the antibiotic is also taken into account. Phytotherapeutic drugs for the treatment of urinary tract infections during pregnancy should not be used.
Cystitis
Cystitis (inflammation of the bladder wall) during pregnancy usually manifests itself in a more erased form than outside it, there is less often very severe pain, less often cystitis is hemorrhagic - that is, blood in the urine is less often detected. Cystitis can also serve as the first step to the subsequent development of pyelonephritis, so cystitis during pregnancy also requires treatment with antibacterial drugs, herbal medicine in this case should not be used. nine0003
Gestational pyelonephritis
Gestational pyelonephritis, in which the inflammatory process is localized in the pelvis of the kidney or both kidneys, is a rather formidable disease that can lead to abortion, stillbirth and even threaten the life of the pregnant woman herself.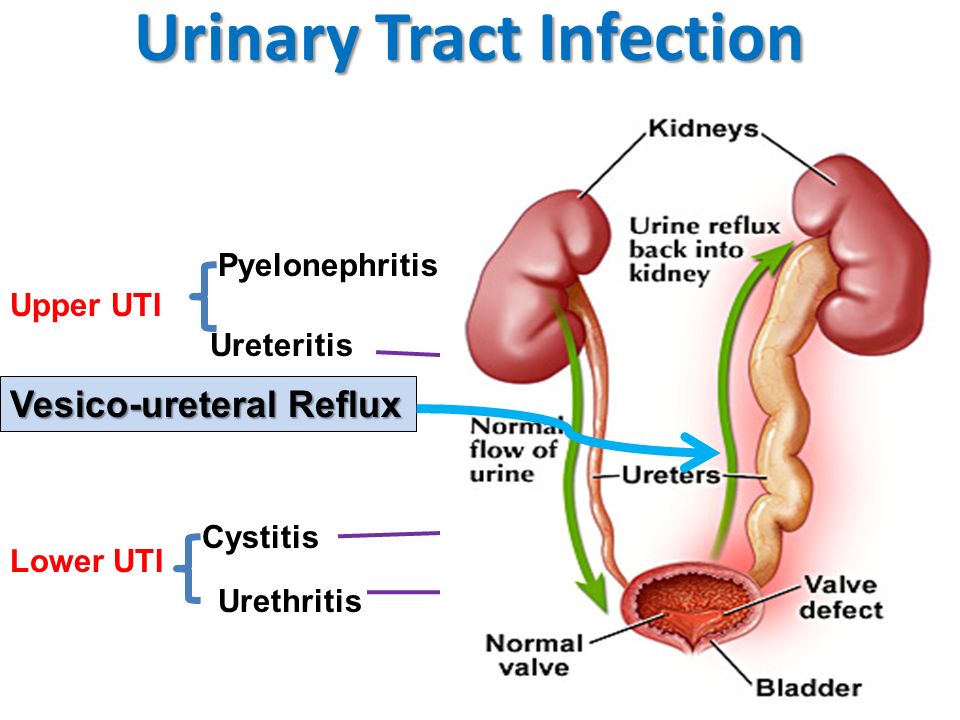 You can suspect it with an increase in temperature and pain in the lower back. With gestational pyelonephritis, hospitalization of a pregnant woman in the urological department for a short period of time and in the maternity hospital at a multidisciplinary hospital with the obligatory presence of a urological department is mandatory. Treatment is also with antibiotics. In the event that a clot of pus formed in the pelvis blocks the ureter and interferes with the outflow of urine, a special stent is installed in the ureter, restoring the patency of the ureter and saving the kidney from hydronephrotic transformation (stretching of the kidney with urine that does not drain, followed by the death of part of the kidney tissue). The stent may remain in place until delivery. nine0003
You can suspect it with an increase in temperature and pain in the lower back. With gestational pyelonephritis, hospitalization of a pregnant woman in the urological department for a short period of time and in the maternity hospital at a multidisciplinary hospital with the obligatory presence of a urological department is mandatory. Treatment is also with antibiotics. In the event that a clot of pus formed in the pelvis blocks the ureter and interferes with the outflow of urine, a special stent is installed in the ureter, restoring the patency of the ureter and saving the kidney from hydronephrotic transformation (stretching of the kidney with urine that does not drain, followed by the death of part of the kidney tissue). The stent may remain in place until delivery. nine0003
Make an appointment with a gynecologist
For more details, consult a qualified specialist at the Semeynaya clinic.
To find out prices for a gynecological appointment or other questions, follow the link below:
What causes urinary incontinence in pregnant women
One of the signs of pregnancy is frequent urination. In process of increase in term the phenomenon is expressed more often, especially at night. Unfortunately, this is often not the only change in the work of the expectant mother's urination organs. Against the background of metamorphoses occurring in the body of a woman, various disorders in the functioning of the kidneys and bladder appear. One of these troubles can be urinary incontinence in pregnant women. The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal. However, to rule out the presence of serious problems, it is worth consulting with your doctor. nine0003
In process of increase in term the phenomenon is expressed more often, especially at night. Unfortunately, this is often not the only change in the work of the expectant mother's urination organs. Against the background of metamorphoses occurring in the body of a woman, various disorders in the functioning of the kidneys and bladder appear. One of these troubles can be urinary incontinence in pregnant women. The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal. However, to rule out the presence of serious problems, it is worth consulting with your doctor. nine0003
Types of urinary incontinence during pregnancy
Most often, 3 types of urinary incontinence in a pregnant woman appear, and in each case there are characteristic signs.
- Stress. It manifests itself with the tension of the abdominal muscles and fluctuations of the diaphragm. That is, it is enough to sneeze, cough or laugh so that a couple of drops of urine appear on the linen. The condition is typical for the first trimester.
- Urgent. Symptoms are sudden urge to urinate. They arise so unexpectedly that the expectant mother simply does not have enough time to run to the bathroom. One of the causes of the condition lies in the irritation of the urinary canal. You can also blame the failure of the nervous system and overstretching of the muscles in the pelvis. The condition is typical for the last trimester, but also occurs after childbirth. nine0060
- Full bladder syndrome. The symptom is the inability to completely empty the bladder. A woman often feels an acute urge to urinate, and after leaving the toilet it seems that urine remains in the ureter. The reason may be hidden in the stretched and therefore sluggish walls of the bladder.

Regardless of the cause of urinary incontinence in a pregnant woman, the condition causes discomfort and stress. This is not a reason to panic, in fact, the situation is not so critical - most often, not the entire volume of urine from the bladder is released, but only a small amount. To calm down in such a difficult period, it is enough to consult a doctor and get an appointment if necessary. nine0003
Main causes of urinary incontinence in pregnancy
Given that it is not difficult to find an explanation for urinary incontinence in a pregnant woman, it should not cause much concern. It is only necessary to identify the causes and make sure that this is due to physiology, and not diseases of the genitourinary system. The doctor who leads the pregnancy will help dispel fears.
The main cause is weakened muscles in the pelvic area. Excessive stretching of muscle tissue leads to loss of tone. As a result, the sphincter that holds urine, the walls of the bladder, and other muscles are weakened. This is due to hormonal changes, as well as changes in the size of internal organs. For example, the growing uterus during pregnancy compresses the bladder. As a result, its volume decreases, and urination occurs more often. nine0003
This is due to hormonal changes, as well as changes in the size of internal organs. For example, the growing uterus during pregnancy compresses the bladder. As a result, its volume decreases, and urination occurs more often. nine0003
Another cause of urinary incontinence in a woman during pregnancy is the impact of a baby's foot on the bladder. This phenomenon does not happen to everyone. Doctors explain its severity by the position and size of the fetus, as well as the physical form of the expectant mother.
The number of previous pregnancies and births is also thought to increase the risk of urinary incontinence. Especially if the pregnancies go one after another, and the woman's muscles simply do not have time to recover. nine0003
Other factors associated with urinary incontinence during pregnancy are overweight and a sedentary lifestyle. A protracted birth process provokes a problem already in the postpartum period.
Healthy urinary retention occurs when the following conditions are met:
- when the bladder is in a normal position;
- immobility of the urethra;
- good work of the muscles surrounding the bladder and pelvic floor muscles; nine0060
- with the functional and anatomical integrity of the urethra and bladder closure apparatus.

What to do to deal with the problem
As mentioned above, urinary incontinence in women during pregnancy is most often associated with physiological changes, so no treatment is required. However, given the responsibility for the health of the baby during this period, you need to consult a doctor and, according to his appointment, take a urine test. This is necessary to exclude or identify urinary infections and diseases associated with them. nine0003
If the tests do not show deviations, it remains only to calm down and practice hygiene more often. The doctor will give recommendations on hygiene products - their choice and the frequency of changing underwear. But even without a specialist, we can say that the replacement of pads and panties is carried out as needed. Lingerie should fit the size, and it is better to choose a special cut for expectant mothers so that it does not press anywhere. Decorative details on underwear are not welcome, you should give preference to simple panties made of natural fabric.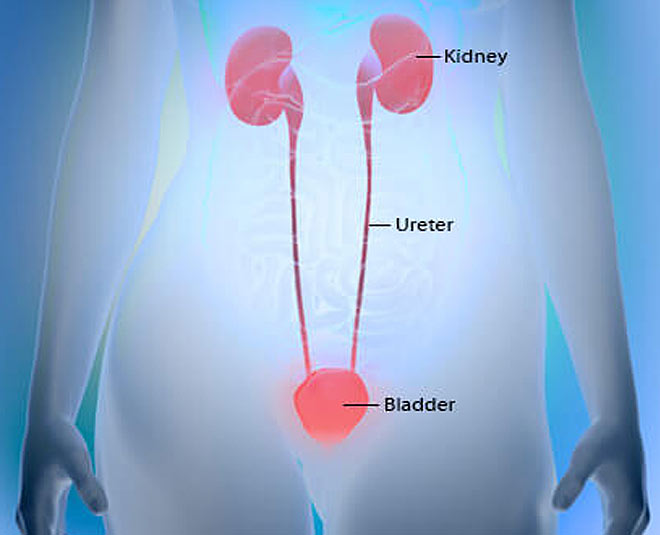 nine0003
nine0003
If there is a problem, you will often have to wash yourself, go to the toilet on time. Doctors advise you to lean forward slightly when urinating. This will allow the urethra to open completely. At the end, you need to push slightly (without fanaticism) to completely empty the bubble.
Reducing the pressure on the diaphragm can help reduce the risk of urine leakage when sneezing and coughing. To do this, you need to open your mouth, normalizing the pressure.
Examination and treatment
Before dealing with incontinence, it is imperative to establish its cause by contacting a doctor. The doctor, in turn, will prescribe the necessary examination. It usually consists of several stages:
- Urodynamic examination. With the help of it, the work of the upper and lower urinary tract is evaluated.
- Clinical examination. It includes a routine urine test and urine culture for flora, as well as a study in a gynecological chair - during an external examination, the doctor can assess the mobility of the bladder neck during a cough test or straining, assess the condition of the vaginal mucosa and skin, and also identify a possible genital prolapse.
 nine0060
nine0060 - Ultrasound examination. It is carried out to study the functioning of the renal system, the urethrovesical segment, the condition of the urethra in a pregnant woman with stress urinary incontinence, as well as to confirm the presence or absence of pathologies of the genitals.
In addition to tests and examinations, you will most likely be asked to keep a special diary in which for several days you will record several parameters of urination, such as the amount of urine released per urination, the number of urination per day, all cases of urinary incontinence, the number of used during the day pads and physical activity. nine0003
Only after the examination, conclusions are drawn about the methods of treatment, which are often necessary only in extreme cases. If no pathology or inflammatory processes are detected, then most likely no special treatment will be carried out, since after childbirth, incontinence most often goes away on its own or occurs less and less.
If incontinence is due to weakening of the pelvic floor muscles, then the situation can be significantly improved with the help of special exercises. Currently, there are a large number of complexes for intimate gymnastics. One of the most popular was developed by the American gynecologist and MD Arnold Kegel. The simplest and, perhaps, the most effective exercise that can be done several times a day is the repeated tension and relaxation of the "intimate muscles" (slow or intense, without delay). nine0003
It is important to know that if you have never strengthened intimate muscles before pregnancy, you need to do this with caution, in no case overdo it.
It is possible that the doctor will prescribe you some herbal preparation that supports the functioning of the bladder and has an antispasmodic, anti-inflammatory and antimicrobial effect.
Treatment with decoctions of herbs (rose hips, sage, dill, lingonberries) may also be recommended. They have not only preventive, but also curative properties.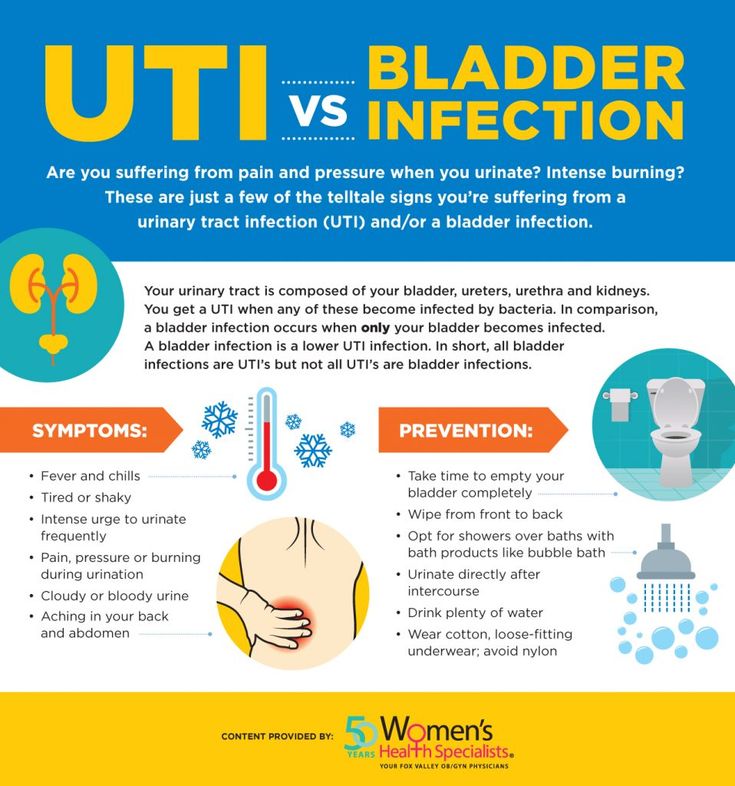 nine0003
nine0003
Pelvic (intimate) muscle training
To reduce the risk of urinary incontinence in a pregnant woman at night and during the day, doctors recommend doing special exercises. These are Kegel exercises that are useful not only for expectant mothers, but for all women, without exception, regardless of age. The bottom line is to alternate tension and relaxation of intimate muscles. It is not difficult to determine the zone for training - during urination, you need to interrupt the process for a couple of minutes. At this moment, those muscles that are involved in gymnastics will just tighten. You need to do exercises before childbirth, during pregnancy and after the baby is born. A simple and understandable set of exercises will reduce the risk of any problems with the urinary system. You can read more about gymnastics in another article. nine0003
How to ensure your comfort and peace of mind
So that urinary incontinence in pregnant women in the early, and especially in the later stages (38-39 weeks), does not cause increased discomfort, manufacturers of hygiene products produce special pads.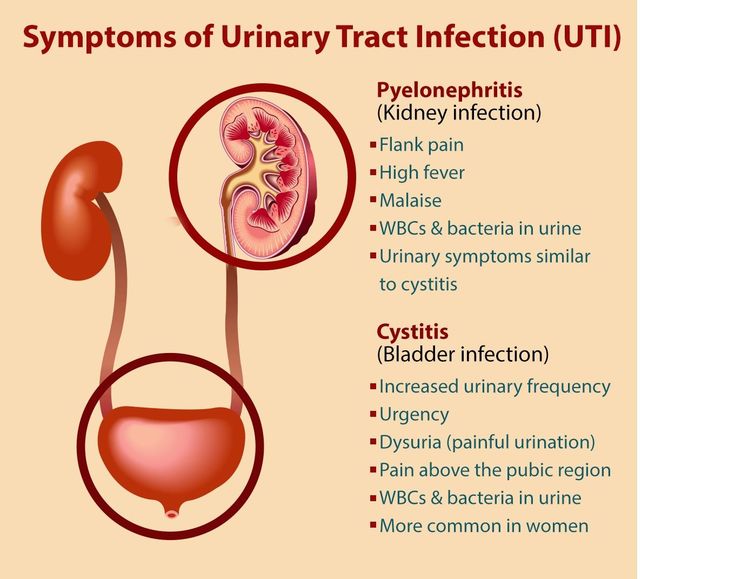 One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
- anatomically shaped to prevent urine from leaking out; nine0060
- absorbent layer that instantly absorbs liquid and odors;
- secure fit on underwear;
- small thickness so that the pad is not visible under clothing;
- safe even for sensitive skin;
- the ability to choose a product based on the amount of discharge.
If you need help choosing the right hygiene products, the PAUL HARTMANN Sp. z o.o. hotline will advise you. nine0003
How else can you help yourself
Go to the toilet as often as possible during the day. At the same time, you should not reduce your fluid intake. The expectant mother should drink as much as she wants. But you need to try not to drink large amounts of liquid an hour before bedtime.
Many women use disposable pads to avoid trouble.