How to stop post nasal drip in child
Pediatric Post Nasal Drip - Coastal Ear Nose & Throat
Insight Into Treating a Runny Nose:
- What is Post-Nasal Drip?
- How is Swallowing Affected?
- How is Post-Nasal Drip Treated?
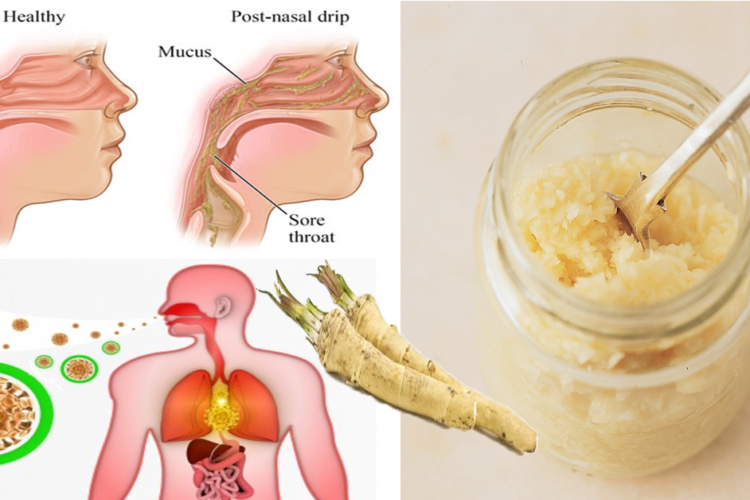
Glands in your nose and throat continually produce mucus (one to two quarts a day). Mucus moistens and cleans the nasal membranes, humidifies air, traps and clears inhaled foreign matter, and fights infection. Although it is normally swallowed unconsciously, the feeling of it accumulating in the throat or dripping from the back of your nose is called post-nasal drip. This sensation can be caused by excessively thick secretions or by throat muscle and swallowing disorders.
What Causes Abnormal Secretions?
Thin Secretions:
Increased thin clear secretions can be due to colds and flu, allergies, cold temperatures, bright lights, certain foods/spices, pregnancy, and other hormonal changes. Various drugs (including birth control pills and high blood pressure medications) and structural abnormalities can also produce increased secretions. These abnormalities might include a deviated or irregular nasal septum (the cartilage and bony dividing wall that separates the two nostrils).
Thick Secretions:
Increased thick secretions in the winter often result from dryness in heated buildings and homes. They can also result from sinus or nose infections and allergies, especially to foods such as dairy products.
If thin secretions become thick, and turn green or yellow, it is likely that a bacterial sinus infection is developing. In children, thick secretions from one side of the nose can mean that something is stuck in the nose such as a bean, wadded paper, or piece of toy. If these symptoms are observed, seek a physician for examination.
How is Swallowing Affected by Post Nasal Drip?
Swallowing problems may result in an accumulation of solids or liquids in the throat that may complicate or feel like post-nasal drip. When the nerves and muscles in the mouth, throat, and food passage (esophagus) aren’t interacting properly, overflow secretions can spill into the voice box (larynx) and breathing passages (trachea and bronchi), causing hoarseness, throat clearing, or coughing.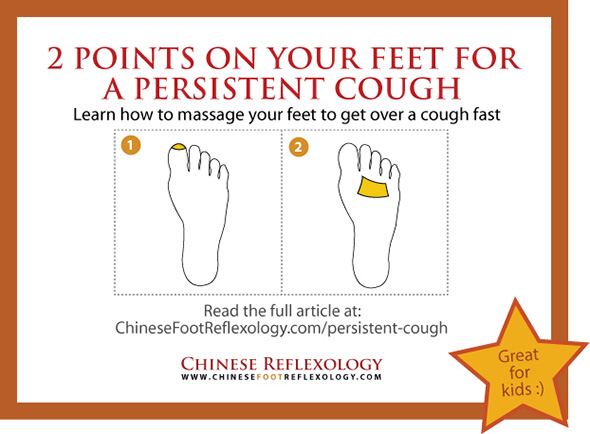
Several factors contribute to swallowing problems:
- With age, swallowing muscles often lose strength and coordination, making it difficult for even normal secretions to pass smoothly into the stomach.
- During sleep, swallowing occurs much less frequently, and secretions may gather. Coughing and vigorous throat clearing are often needed upon waking.
- When nervous or under stress, throat muscles can trigger spasms that make it feel as if there is a lump in the throat. Frequent throat clearing, which usually produces little or no mucus, can make the problem worse by increasing irritation.
- Growths or swelling in the food passage can slow or prevent the movement of liquids and/or solids.
Swallowing problems may also be caused by gastroesophageal reflux disease (GERD). This is a backup of stomach contents and acid into the esophagus or throat. Heartburn, indigestion, and sore throat are common symptoms. GERD may be aggravated by lying down, especially following eating. Hiatal hernia, a pouch-like tissue mass where the esophagus meets the stomach, often contributes to the reflux.
Hiatal hernia, a pouch-like tissue mass where the esophagus meets the stomach, often contributes to the reflux.
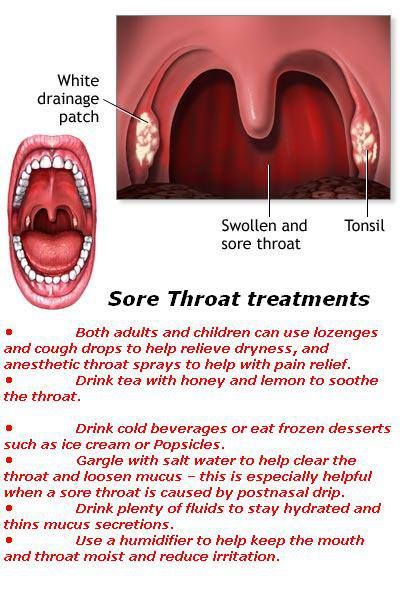
How is the Throat Affected by Post-Nasal Drip?
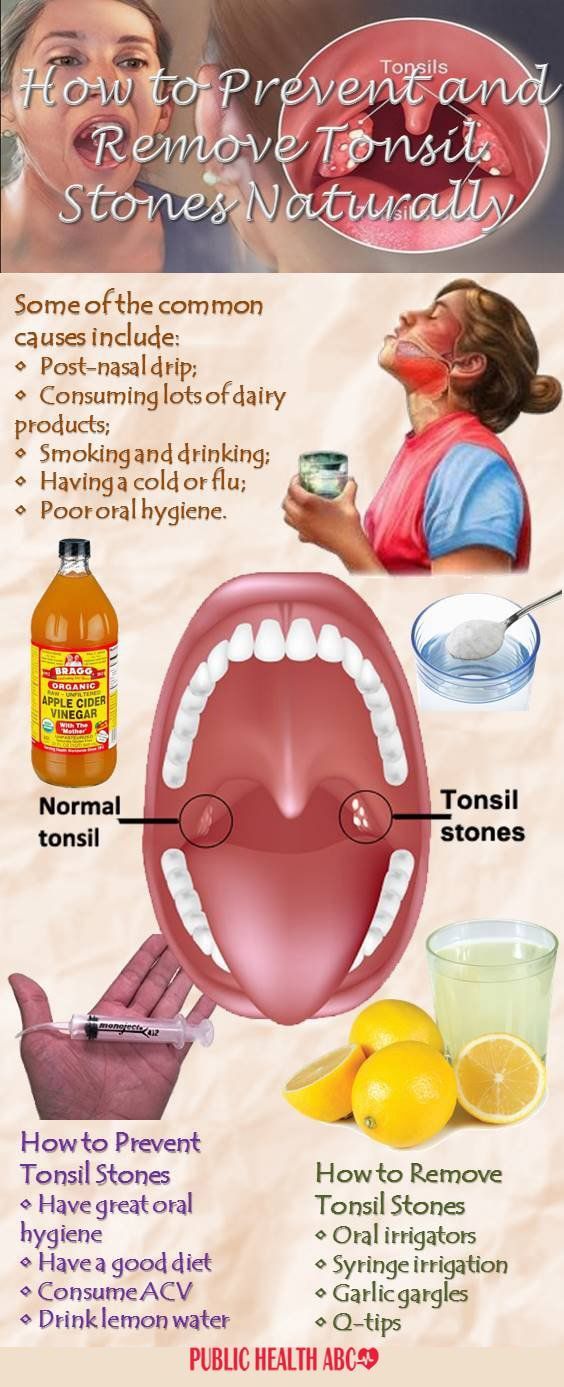
Post-nasal drip often leads to a sore, irritated throat. Although there is usually no infection, the tonsils and other tissues in the throat may swell. This can cause discomfort or a feeling that there is a lump in the throat. Successful treatment of the post-nasal drip will usually clear up these throat symptoms.
How is Post-Nasal Drip Treated?
A correct diagnosis requires a detailed ear, nose, and throat exam, and possibly laboratory, endoscopic (procedures that use a tube to look inside the body), and x-ray studies. Treatment varies according to the following causes:
- Bacterial infections are treated with antibiotics. These drugs may only provide temporary relief. In cases of chronic sinusitis, surgery to open the blocked sinuses may be required.
- Allergies are managed by avoiding the causes.
 Antihistamines and decongestants, cromolyn and steroid (cortisone type) nasal sprays, and other forms of steroids may offer relief. Immunotherapy, either by shots or sublingual (under the tongue drops) may also be helpful. However, some older, sedating antihistamines may dry and thicken post-nasal secretions even more; newer nonsedating antihistamines, available by prescription only, do not have this effect. Decongestants can aggravate high blood pressure, heart, and thyroid disease. Steroid sprays may be used safely under medical supervision. Oral and injectable steroids rarely produce serious complications in short-term use. Because significant side-effects can occur, steroids must be monitored carefully when used for more than one week.
Antihistamines and decongestants, cromolyn and steroid (cortisone type) nasal sprays, and other forms of steroids may offer relief. Immunotherapy, either by shots or sublingual (under the tongue drops) may also be helpful. However, some older, sedating antihistamines may dry and thicken post-nasal secretions even more; newer nonsedating antihistamines, available by prescription only, do not have this effect. Decongestants can aggravate high blood pressure, heart, and thyroid disease. Steroid sprays may be used safely under medical supervision. Oral and injectable steroids rarely produce serious complications in short-term use. Because significant side-effects can occur, steroids must be monitored carefully when used for more than one week. - Gastroesophageal reflux is treated by elevating the head of the bed six to eight inches, avoiding foods and beverages for two to three hours before bedtime, and eliminating alcohol and caffeine from the daily diet. Antacids such as Maalox®, Mylanta®, Gaviscon®, and drugs that block stomach acid production such as Zantac®, Tagamet®, or Pepcid®) may be prescribed.
 If these are not successful, stronger medications can be prescribed. Trial treatments are usually suggested before x-rays and other diagnostic studies are performed.
If these are not successful, stronger medications can be prescribed. Trial treatments are usually suggested before x-rays and other diagnostic studies are performed.
General measures that allow mucus secretions to pass more easily may be recommended when it is not possible to determine the cause of post-nasal drip. Many people, especially older persons, need more fluids to thin out secretions.
Drinking more water, eliminating caffeine, and avoiding diuretics (medications that increase urination) will help. Mucous-thinning agents such as guaifenesin (Humibid®, Robitussin®) may also thin secretions. Nasal irrigations may alleviate thickened secretions. These can be performed two to four times a day either with a nasal douche device or a Water Pik® with a nasal irrigation nozzle.
Warm water with baking soda or salt (½ to 1 tsp. to the pint) or Alkalol®, a nonprescription irrigating solution (full strength or diluted by half warm water), may be helpful. Finally, use of simple saline (salt) nonprescription nasal sprays(e.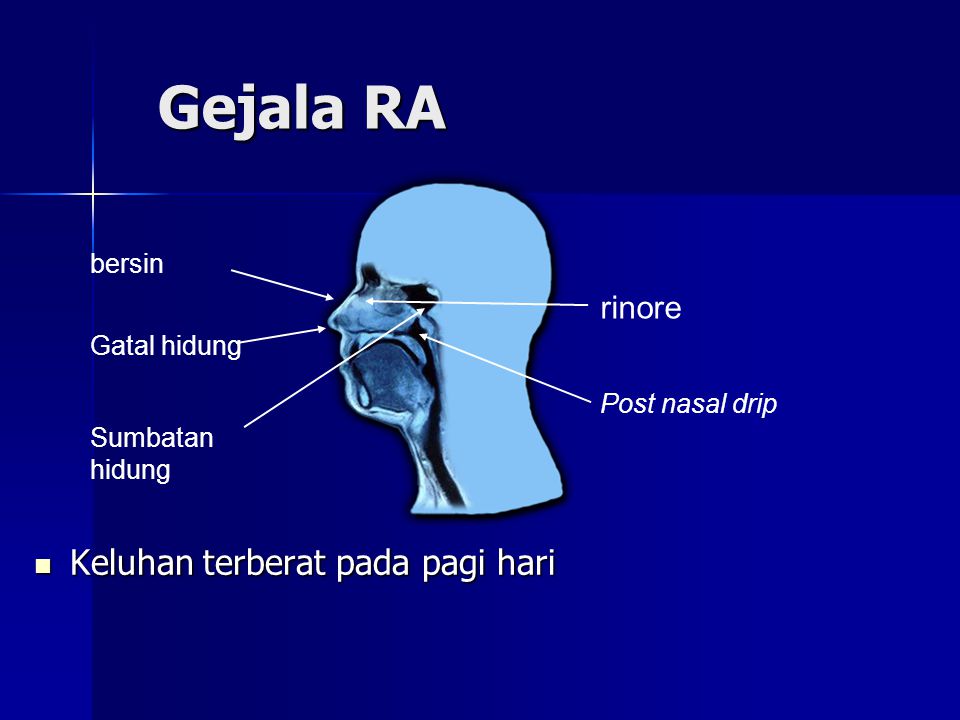 g., Ocean®, Ayr®, or Nasal®) to moisten the nose is often very beneficial.
g., Ocean®, Ayr®, or Nasal®) to moisten the nose is often very beneficial.
Sinus Conditions
Sinuses are air-filled cavities in the skull. They drain into the nose through small openings. Blockages in the openings from swelling due to colds, flu, or allergies may lead to acute sinus infection. A viral cold that persists for 10 days or more may have become a bacterial sinus infection. This infection may increase post-nasal drip. If you suspect that you have a sinus infection, you should contact your physician to see if it needs antibiotic treatment.
Chronic sinusitis occurs when sinus blockages persist, causing the lining of the sinuses to swell further. Polyps (growths in the nose) may develop with chronic sinusitis. Patients with polyps tend to have irritating, persistent post-nasal drip. Evaluation by an otolaryngologist may include an exam of the interior of the nose with a fiberoptic scope and CAT scan x-rays. If medication does not relieve the problem, surgery may be recommended. Vasomotor Rhinitis describes a nonallergic “hyperirritable nose” that feels congested, blocked, or wet..
Vasomotor Rhinitis describes a nonallergic “hyperirritable nose” that feels congested, blocked, or wet..
How To Treat A Post Nasal Drip Cough
Understanding Post Nasal Drip Cough
Written by Adam Partridge, PA-C - Genexa Healthcare Provider & Partner on June 1, 2021
Postnasal drip is extremely annoying, and when your child is dealing with this symptom they might be feeling pretty uncomfortable… and that’s when it isn’t accompanied by other symptoms.
When postnasal drip causes a cough, the coughing can be constant and your kiddo’s symptoms may leave them in a pretty dismal state of mind. Luckily, postnasal drip, and all of its accompanying symptoms, can be pretty easily treated right at home.
Home remedies and OTC medicine can make a world of difference when it comes to easing symptoms, and your doctor will be able to recommend methods of treatment if further guidance is needed.
Why Does Post Nasal Drip Cause a Cough?
Postnasal drip happens when your body produces too much mucus, like as a response to illness or infection, and the excess mucus drips down the back of your throat instead of being flushed out through the nose.
Postnasal drip can cause symptoms like:
- Frequent throat clearing
- Sore throat
- Raspy voice
- Cough
- A feeling of mucus draining down your throat
Postnasal drip can sometimes cause a cough because of all the mucus traveling down the throat and through the airways. Typically, treating the illness or infection that caused postnasal drip in the first place will eventually clear up any kind of cough or other symptoms happening as a result.
Postnasal drip can be caused by a multitude of illnesses and infections, but it can also be caused by things like allergies.
The main causes of postnasal drip include:
- Bacterial infections, like strep throat
- Allergies or hay fever
- Nonallergic rhinitis, which can be understood as an overly sensitive nose
- Gastroesophageal reflux
How Can I Ease My Child’s Symptoms at Home?
When postnasal drip causes a cough, the symptoms can be really unpleasant, but they are generally highly treatable… which means your kiddo can get some relief pretty quickly.
There are plenty of home remedies that can ease the symptoms caused by postnasal drip.
Remedies that can be used to treat most of the symptoms associated with post nasal drip include:
Add Moisture To The Air
There are a couple of ways you can approach this method of treatment. One method is to run a hot shower and allow your child to sit in the steam for a while. The steam can help soothe an irritated throat and irritated airways, thus helping to relieve the nagging cough that can be caused by postnasal drip. When your child is having a coughing fit, the shower method is a great option.
When your child is having a coughing fit, the shower method is a great option.
Another approach is to use a humidifier to add some moisture to the air since dry air can aggravate symptoms. You can also fill the sink with hot water and then have your child lean over it with a towel covering their head to keep the steam near their face.
Stay hydrated
When your kiddo is struggling with post nasal drip, making sure they are drinking plenty of fluids can help ease some of the discomfort. Staying well-hydrated is a great way to get rid of a pesky cough.
Prop your child’s head up at night.
When your child goes to sleep at night, using an extra pillow to prop their head up a little bit higher can ease symptoms by preventing any excess mucus from collecting in the back of their throat and making them cough.
Sleep, and rest in general, is also a critical part of recovery, so this method may also be great in terms of helping your child sleep through the night while they are under the weather.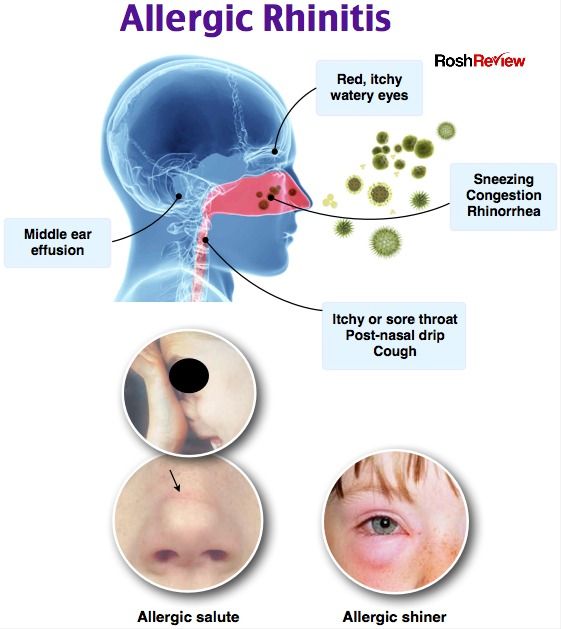
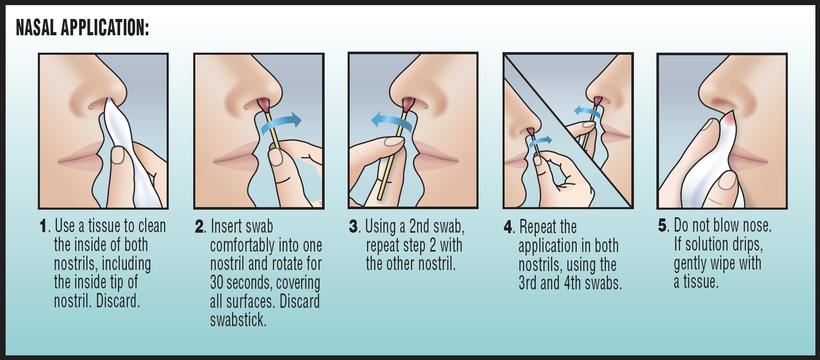
Saline nasal irrigation.
Using saline solution or drops to help flush out your child’s nasal passages may help thin and loosen the mucus in their nose, thus reducing symptoms.
When it comes to a cough specifically, these remedies may come in handy as well:
- Tea with lemon and honey can make a great remedy for a pesky cough, and may also help with relentless coughing fits. Warm liquids help soothe the throat and break up mucus, and honey offers a coating for the throat that can work against irritation.
- Keeping cough drops on hand is another great idea because these work very well during coughing fits and are easy to keep around. Just be careful, because it is easy to choke on cough drops, and if your child is under 6 years old this method is not highly recommended.
In some cases, your little one’s symptoms just might be too uncomfortable to respond to these kinds of remedies. When this happens, over-the-counter cough or cold medicine might do the trick.
Genexa’s Kids’ Cough & Chest Congestion oral suspension medication works hard to thin and loosen mucus, control a cough, and relieve chest congestion, making it a great choice when your kid has a postnasal drip cough. Additionally, Genexa’s Kid’s Honey Cough Syrup is a helpful remedy that soothes coughs associated with dry throat and irritation while supporting immunity.
Genexa is the first clean medicine brand, meaning that they make medicine with the active ingredients you need and without the artificial inactive ingredients you don’t need. They are working hard to revolutionize the world of medicine one product at a time, and are committed to making real, clean medicine that you can trust. Any inactive ingredients that you find in Genexa’s products are non-GMO, gluten-free, and certified vegan. Genexa was founded by two dads who know what it is like to constantly be on the hunt for the best when it comes to their kid's health, and this is why they are determined to offer you a clean medicine option.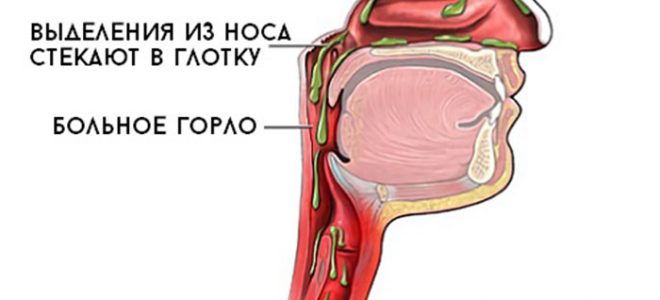 Clean medicines is made with the same effective ingredients you need, but without the artificial inactive ones you don’t.
Clean medicines is made with the same effective ingredients you need, but without the artificial inactive ones you don’t.
How Do I Know If I Should Consult a Doctor About My Child’s Symptoms?
Postnasal drip will almost always be nothing to worry about, but it might be easy to mistake something more serious for postnasal drip… and this is when problems happen.
Sometimes, more concerning symptoms will present themselves that indicate that your child needs to see a doctor.
Symptoms you should keep your eyes peeled for include:
- An unexplained fever, especially if it is high
- Bloody mucus from the nose, or bloody mucus being coughed up
- Wheezing or shortness of breath
- Foul-smelling nose drainage or heavy drainage that only comes from one nostril
- Persistent symptoms that do not respond to treatment
One key thing to be especially mindful of here is if your child’s symptoms do not respond to medicine and other treatment. This is a huge sign that there may be something bigger going on and your kiddo may need prescription medication in order to feel better.
This is a huge sign that there may be something bigger going on and your kiddo may need prescription medication in order to feel better.
If your child’s symptoms do not get better with treatment or if they continue to persist after a week or so, it is important to get in touch with your doctor or pediatrician in order to get to the bottom of it.
Even if these more concerning symptoms do not appear, it still doesn’t hurt to contact your pediatrician and talk about your kiddo’s symptoms. Doctors can make great recommendations when it comes to managing symptoms at home, and they can also offer guidance as to whether or not it would be helpful for your child to be brought in for an exam. There is no shame in playing it safe when your child is not feeling quite right, and a doctor can put any questions or concerns to rest.
Postnasal Drip Cough: Outlook
Though it can be pesky, uncomfortable, and all-around annoying, a cough caused by postnasal drip usually does not last too long and is fairly easy to treat. This kind of cough is caused by excess mucus that drips down the back of the throat, so treatment methods aimed at thinning and loosening mucus tend to work best when it comes to finding relief.
This kind of cough is caused by excess mucus that drips down the back of the throat, so treatment methods aimed at thinning and loosening mucus tend to work best when it comes to finding relief.
Drinking more fluids, getting some rest, and inhaling steam are three highly effective methods of calming the nagging cough caused by postnasal drip, but over-the-counter medicine is another option if these types of home remedies don’t cut it.
If your child’s symptoms do not respond to treatment, whether it be over-the-counter medicine or prescription medication, it is important to consult a doctor, as this is a major indication that something more serious is going on and your child may need a new treatment plan.
Additionally, symptoms that persist for more than a week or so should be discussed with a doctor. Your doctor will always be able to answer any questions you may have, and they can also offer guidance when it comes to medication dosages, treatment recommendations, and the amount of time it should take for your child to start feeling a little bit better.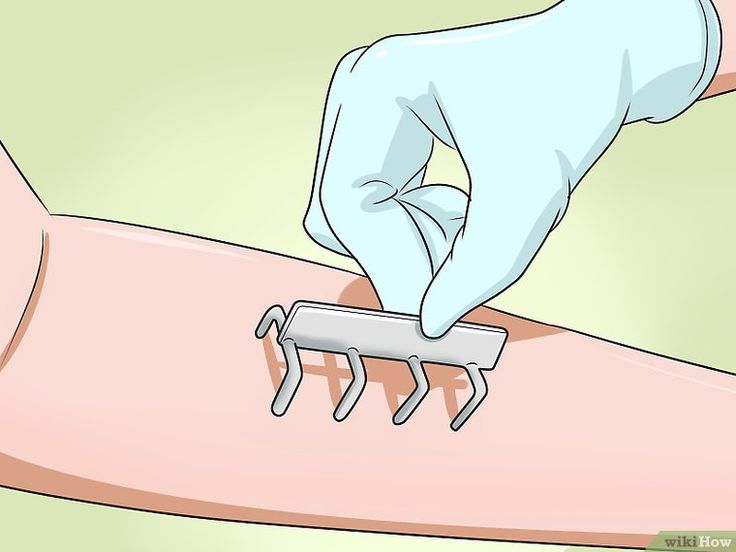
When in doubt, consult a doctor.
Sources:
https://www.enthealth.org/conditions/post-nasal-drip/
https://www.health.harvard.edu/staying-healthy/treatments-for-post-nasal-drip
https://www.seattlechildrens.org/conditions/a-z/coughs-meds-or-home-remedies/
Related Articles
Continue to Article
Continue to Article
All Articles
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Continue to Article
Proper treatment of the common cold in children
A common cold usually takes 7-10 days or more to develop, depending on the type of illness that provoked it.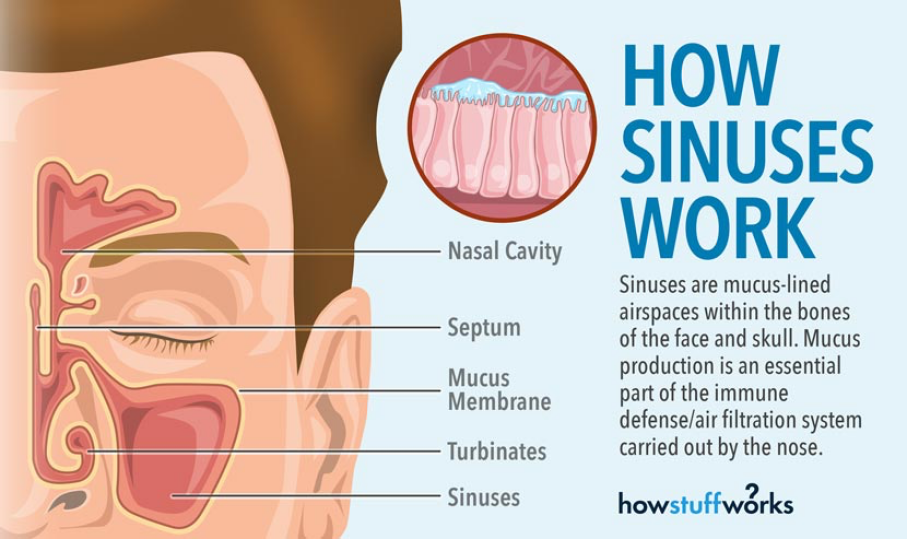 Serious illnesses, such as some types of acute respiratory viral infections (ARVI), as well as chronic rhinitis caused by specific infections (syphilis, tuberculosis, gonorrhea) are treated simultaneously with the underlying disease in specialized medical centers.
Serious illnesses, such as some types of acute respiratory viral infections (ARVI), as well as chronic rhinitis caused by specific infections (syphilis, tuberculosis, gonorrhea) are treated simultaneously with the underlying disease in specialized medical centers.
In this article we will talk about how to properly treat a simple infectious rhinitis in newborns, infants and older children. It is important that parents caring for sick children have some knowledge of how to properly care for a child with a cold and why this is important. nine0003
How to properly treat a runny nose in a child?
First aid
In all cases of a cold in a child, before starting any medical treatment (i.e. drug treatment), you should try to alleviate the child's condition with available means:
1. Raise the head of the bed on which the child is lying. To do this, a pillow can be placed under the shoulders of the child, so that the head and upper body of the child are located in relation to the body at an angle of 40–45? (make sure the child is comfortable in this position). This will make the phlegm that forms in your nose easier to pass and you may not need to use any medication. nine0003
This will make the phlegm that forms in your nose easier to pass and you may not need to use any medication. nine0003
2. If a newborn or infant has a very stuffy nose with phlegm, you can try to suck out the mucus from the nasal passages with a rubber bulb or a regular syringe. In general, sputum suction is used to help children who cannot blow their nose on their own. To suck out sputum, you can use a regular rubber bulb with a fairly thin tip or a regular syringe without a needle. The tip of a pear or syringe should be inserted into the nasal passage of a child with a runny nose carefully, so as not to injure the mucous membrane. Mucus is sucked out first from one, and then from the other nasal passage. This procedure can be repeated as often as needed. nine0003
Do not let the sputum dry out!
The easiest way is to put a saline solution into a child's nose: In the case of a cold in newborns or infants, as well as a cold in older children, it is important not to allow mucus to dry in the nasal passages - this can completely upset nasal breathing.
In order to prevent mucus from drying up in the nasal passages, wetting the nasal passages with saline solution is recommended. To do this, you can use ordinary saline, or you can just use a solution of ordinary table salt in water. nine0003
Saline solution instilled 3-4 drops into each nostril. It is desirable that at this time the child lies with his head thrown back. The first entry of fluid into the nose can be very unpleasant, causing coughing, sneezing, or even the urge to vomit. However, after several instillation procedures, such sensitivity of the nasal and pharyngeal mucosa disappears. The procedure can be repeated every 30-60 minutes. It is important to ensure that the mucus in the nose does not dry out. The saline solution helps thin the sputum and make it easier to excrete from the nose of a child with a runny nose. nine0003
Instead of saline, some experts recommend using oily liquids, such as vitamin A or vitamin E oil, available from pharmacies. Such liquids not only prevent sputum from drying out, but also moisturize the nasal mucosa, relieve irritation, and have a regenerating effect.
Medications to relieve nasal breathing
In some sources, of course, you can read about the "danger" or "inappropriateness" of the use of decongestants (the so-called all types of drugs that, when instilled into the nose or when taken by mouth, facilitate nasal breathing) in treatment of acute rhinitis in newborns, infants and older children. nine0003
We must give credit to our colleagues for noting that such drugs can indeed cause some complications and that, if used incorrectly, they can aggravate the child's condition. We note right away that the complications of the common cold do not arise because of the drugs themselves, but because of their illiterate use. It is absolutely unacceptable to treat children with decongestants intended for adults and give the child medicine when it pleases.
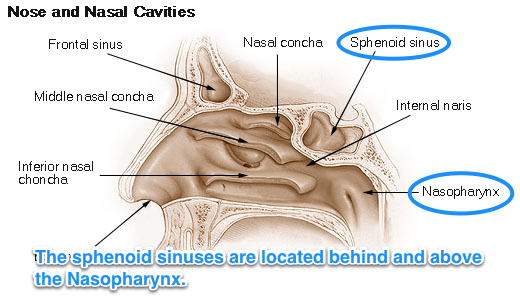
Below we will review some of the drugs recommended for the treatment of the common cold in children, but first we note that failure to treat modern decongestants can cause complications such as sinusitis. The fact is that all nasal sinuses (two maxillary, two frontal, ethmoid and sphenoid) open with small openings into the nasal cavity. Microbes are expelled from the sinuses through these openings. With a runny nose, children develop severe swelling of the nasal mucosa, which leads to complete closure of the holes that communicate the nasal cavity with the cavities of the paranasal sinuses. As a result, microbes accumulate in the sinuses, which eventually cause sinusitis - inflammation of the sinuses. nine0003
The fact is that all nasal sinuses (two maxillary, two frontal, ethmoid and sphenoid) open with small openings into the nasal cavity. Microbes are expelled from the sinuses through these openings. With a runny nose, children develop severe swelling of the nasal mucosa, which leads to complete closure of the holes that communicate the nasal cavity with the cavities of the paranasal sinuses. As a result, microbes accumulate in the sinuses, which eventually cause sinusitis - inflammation of the sinuses. nine0003
How do nasal breathing medicines work?
There are two large groups of drugs that facilitate nasal breathing: local (topical) and systemic decongestants. Both those and other types of cold medicine act in the same way: they constrict the vessels of the nasal mucosa. Due to the narrowing of the vessels, the swelling of the nasal mucosa decreases and nasal breathing is partially or completely restored. It also opens the communication channels between the nasal cavity and the paranasal sinuses, thereby reducing the risk of developing sinusitis. nine0003
nine0003
What medicines are used to treat the common cold in children?
First, let's draw the attention of parents to the specifics of drug production: the same drug is produced by different companies under different names. However, on the packaging of the drug or in the instructions for its use, the active substance is always indicated, which is the same in all drugs of this type. Therefore, when buying a medicine, pay attention not to the commercial name, but to the name of the active substance that is part of the medicine, as well as to the concentration of the active substance in the preparation. Below we present several such examples. nine0047
|
Runny nose in children - how to treat, how to wash the nose if the child is sick
Author, editor and medical expert - Klimovich Elina Valerievna. nine0003
Editor and medical expert - Harutyunyan Mariam Harutyunovna.
Last updated: 12/28/2022
Number of views: 412,749.
Content:
Stages of development
Features of the disease in children under one year old
Allergic rhinitis
Chronic rhinitis in children
How to treat correctly?
Vasoconstrictors for the common cold for children
Quite often, mothers bring their children to ENT doctors with snot, and often the situations are neglected. Everything about rhinitis, about what a runny nose can be dangerous for a child and how to properly treat it in order to prevent complications - in our article.
Everything about rhinitis, about what a runny nose can be dangerous for a child and how to properly treat it in order to prevent complications - in our article.
The term rhinitis (Latin for rhinitis) comes from the Greek rhinos, nose, and the suffix "it" which doctors use to denote inflammation. In Russian, the disease is called a runny nose, which also implies inflammation of the mucous membrane of the nasal cavity. nine0003
What is it like?
Depending on the causes and characteristics of the runny nose, a child may have 1.2 :
1. Acute
- Infectious : viral, bacterial, fungal or mixed. Of the viruses, adenoviruses, rhinoviruses, influenza and parainfluenza viruses are more often the cause of the disease - in total more than 90 different pathogens 1 .
Of the bacteria, pneumococci, streptococci, staphylococci are more common - those that usually live in the respiratory tract of healthy people and show aggression when immunity is reduced. nine0003
nine0003
- Allergic - arising as a manifestation of intolerance of the body, for example, during the flowering season of certain plants.
- Traumatic - developing after inhalation of dust and smoke, with thermal burns, ingress of foreign bodies and substances, after surgical interventions.
Important! A foreign body may be the cause of airway obstruction 1.4 . The baby can shove it so deep that nothing will be visible during external examination. Therefore, a runny nose without fever in a child under three years old is a reason for mandatory medical visits.
2. Chronic (Protracted)
It can also be:
- infectious;
- allergic: year-round, for example, in case of allergy to house dust or seasonal, in case of allergy to plant pollen;
- vasomotor - arising as a result of an inadequate response to signals from the nervous system, often against the background of problems with the thyroid gland 1 .
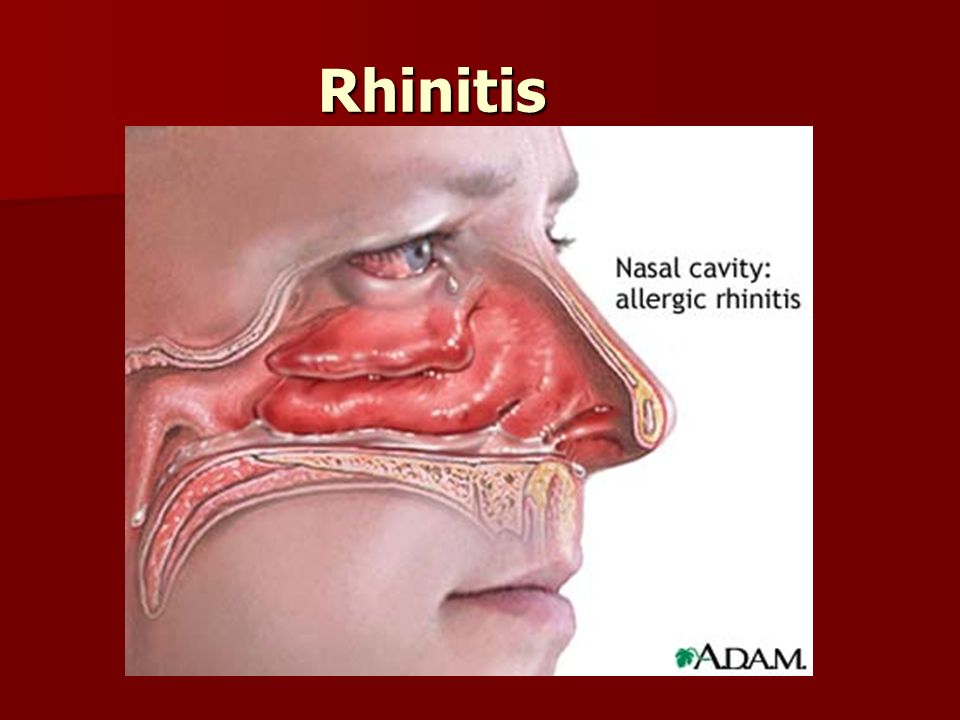
More often chronic rhinitis is accompanied by proliferation ( hypertrophy ) of the turbinates, which requires surgical treatment 1.4 . An atrophic variant, in which thinning of the mucosa is observed, is extremely rare in children and occurs mainly on the background of dependence on vasoconstrictor drugs 1,2,4 .
Stages of development
Let's analyze the disease on the example of its acute infectious variant occurring in three successive stages 1,2,3 .
1. The first stage of irritation, or "dry"
The mucous membrane is the first barrier to airborne viruses. The viruses that settle on its surface penetrate the cells and begin to multiply intensively. This causes flushing and swelling, narrowing of the nasal passages, and difficulty breathing.
There is dryness, itching and burning in the nose, the baby starts to sneeze. The first signs of general intoxication make themselves felt: malaise, headache and chills. Body temperature rises according to the type of infection. nine0003
Body temperature rises according to the type of infection. nine0003
How quickly does a runny nose in children progress to the next stage? More often this happens within a few hours, sometimes - days 1.2 .
2. Second - serous stage
It lasts up to 1 to 3 days 1.2 .
The action of viruses causes an increase in mucus secretion. Liquid transparent foamy discharge from the nasal passages makes breathing even more difficult, reduces sensitivity to odors, irritates the skin of the upper lip, causes redness and cracks on it. nine0003
Lachrymation worsens. The baby becomes lethargic, restless, inattentive, sleeps and eats poorly.
Swelling of the inner lining of the nasal cavity hinders the outflow of contents from the paranasal sinuses and middle ear 1.2 . If a bacterial infection enters the sinuses and ears, the situation is complicated by sinusitis or otitis media 1.2 .
3. Stage of purulent discharge
It starts on the 4-5th day 1.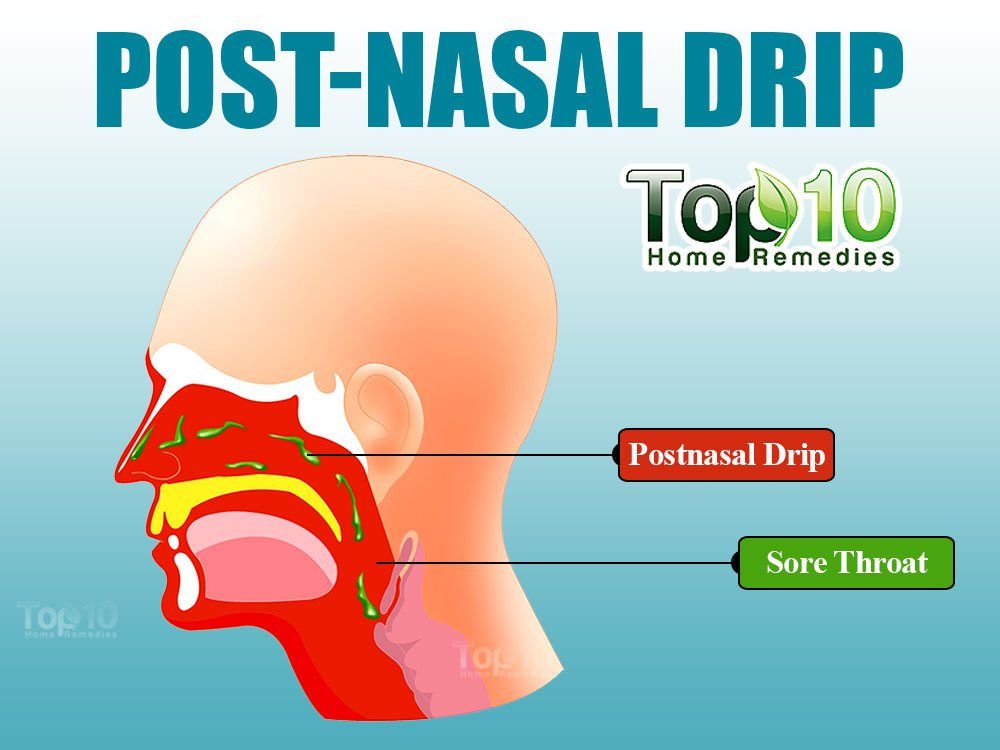 2 .
2 .
Viruses reproducing inside cells cause their death. Dead cells are exfoliated, and wounds appear on the surface of the mucosa, which become easy prey for bacteria - bacterial inflammation develops. nine0003
At this stage of the common cold, the child's snot turns yellow or yellow-green 1.2 . Their number is decreasing. They become thick and dry out, forming crusts.
Gradually, the discharge becomes less and less. Sneezing, lacrimation stops. Recovery is coming.
Total duration of rhinitis in children - 1-2 weeks 1.2 .
Recovery can occur much earlier - in 2-3 days, if the microbes that caused the illness are weak and the baby's immunity is strong 1.2 .
A prolonged runny nose in a child lasting up to 3-4 weeks can often indicate a weakened body and the development of complications 1.2 :
- sinusitis;
- otitis;
- pharyngitis, laryngitis, tracheitis;
- bronchitis and pneumonia.

Important! Fever, cough, runny nose in a child should not be self-treated. Due to the characteristics of the child's body, the risk of pneumonia is high. Calling a doctor at home is a must! nine0003
Peculiarities of the disease in children under one year old
Up to 2.5 months, the nose of a newborn may be blocked for physiological reasons. If there is no discharge, no treatment is required 2.3 .
Sometimes problems are associated with frequent regurgitation and vomit in the nose. You also need to pay attention to this 2,3 .
The main features of infectious rhinitis in infants 2.3 :
- It proceeds as a general infection with fever, lethargy, sleep disturbance, constant crying, refusal to eat. nine0283
- Sucking is disturbed, the baby may refuse to breastfeed, stop gaining weight and even lose weight.
- Swallowing air provokes regurgitation, bloating, colic, stunting 2 .

- Difficulty breathing can sometimes cause increased intracranial pressure, irritation of the meninges 3 . The tension of the fontanelles increases, the baby throws back his head and arches his back in an arc 2.3 .
- Inflammation rapidly spreads to the underlying airways leading to bronchitis and pneumonia 3 .
Important! Any rhinitis in a baby is a reason to call a doctor at home.
Allergic rhinitis
It is caused by allergens. Most often, doctors have to deal with pollinosis - an allergy to plant pollen 1.4 . Tree pollen is considered the most aggressive, its maximum concentration in the air occurs in spring, as well as pollen of cereals and wild grasses 1.4 - in this case, allergies occur mainly in late summer and early autumn. Since the symptoms are seasonal, this runny nose is called chronic seasonal.
Chronic allergic form of the disease also occurs with intolerance to house dust, pets, indoor plants, fungi and other allergens, contact with which occurs constantly or in a certain season 1.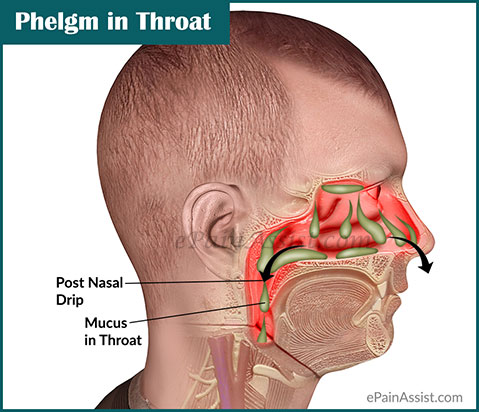 4 .
4 .
It all starts with the contact of the allergen with the membrane of the nasal cavity and the activation of immune blood cells. Absorbing the allergen, immune cells are destroyed. This leads to the release of histamine in them, which causes the expansion of the blood vessels of the mucosa and its swelling, difficulty in breathing and increased secretion of mucus. nine0003
Prolonged course of the disease often leads to bronchial asthma, hearing loss, chronic headaches 1.4 .
The diagnosis of is confirmed by the results of skin tests with various allergens and blood tests for specific IgE - antibodies produced to certain types of allergens.
Chronic rhinitis in children
Chronic course of the disease may differ from acute 1.4 :
- Exacerbations with copious liquid discharge from the nose, followed by a period of calm, when the symptoms become less pronounced. The snot becomes smaller, they can dry out, forming crusts; nasal congestion is not tight - alternately lays one or the other nostril; nine0283
- The child often snores at night, sleeps anxiously and wakes up unrested;
- Continuous mouth breathing causes dryness and bad breath;
- Voice becomes nasal;
- Due to the lack of oxygen in the brain, progress is reduced, exercise tolerance is reduced, and development is slowed down.
In order to prevent a chronic process, it is necessary to properly treat acute rhinitis.
How to treat correctly?
Most often, parents have to treat a runny nose in a child at home. The main task is to clean the nose in time and correctly and prevent the mucus from drying out and the formation of crusts 5 :
- Room should be cool and humid . Ventilate it, carry out wet cleaning, use humidifiers 5 .
- Let your baby drink more. Drinking plenty of fluids is necessary to maintain increased secretion of mucus and eliminate toxins formed during inflammation 4.5 .
- Clean the spout of the baby with the special aspirator and be sure to wash it with soap and water after each use 2.4.5 .
- Teach an older child how to blow your nose . Ask the child to exhale sharply through the nose, alternately pinching one and then the other nostril 5 .
- It is easier to remove mucus from the back sections by “sniffing” through the nose , that is, by sharply inhaling one and then the other nostril 5 .
- Only use disposable tissues for spitting mucus and blowing your nose - cloth quickly becomes a breeding ground for infection 1 .
- Inhalations with the nebulizer can be performed on children from 10 months 2 . It is best to use normal saline for them, in the third stage of inflammation, the doctor may prescribe an antiseptic solution, and in case of allergies, an antiallergic and bronchodilator 2.4 .
- Use vasoconstrictor drops wisely to help your baby feel better and prevent complications 3.4 .
Children's vasopressors for the common cold
Vasoconstrictors reduce swelling and mucus within minutes 3 . They quickly restore breathing, improve sleep and facilitate feeding, open the ducts of the paranasal sinuses and the Eustachian tube, thereby reducing the risk of developing sinusitis and otitis media 3 .
They quickly restore breathing, improve sleep and facilitate feeding, open the ducts of the paranasal sinuses and the Eustachian tube, thereby reducing the risk of developing sinusitis and otitis media 3 .
When is it necessary to use vasoconstrictor drugs 5 :
- Before going to bed, so that the baby can breathe and the mucus does not dry out.
- If your ear hurts.
- When there are problems with eating in children older than one year and always before feeding the baby.
It is very important for children to use children's products 3,4,5 . They have a special dosage of 3,4,5 . Children from 2 to 6 years old can use spray TIZIN ® Expert 6 0.05% or 0.1% based on xylometazoline hydrochloride. Due to the fine "spray" the drug is distributed evenly over the entire surface of the nasal cavity, which contributes to its action. nine0003
The hyaluronic acid contained in the preparation helps to moisturize the mucous membranes and reduce dryness in the nose 6 .
 025%
025%  1%
1% 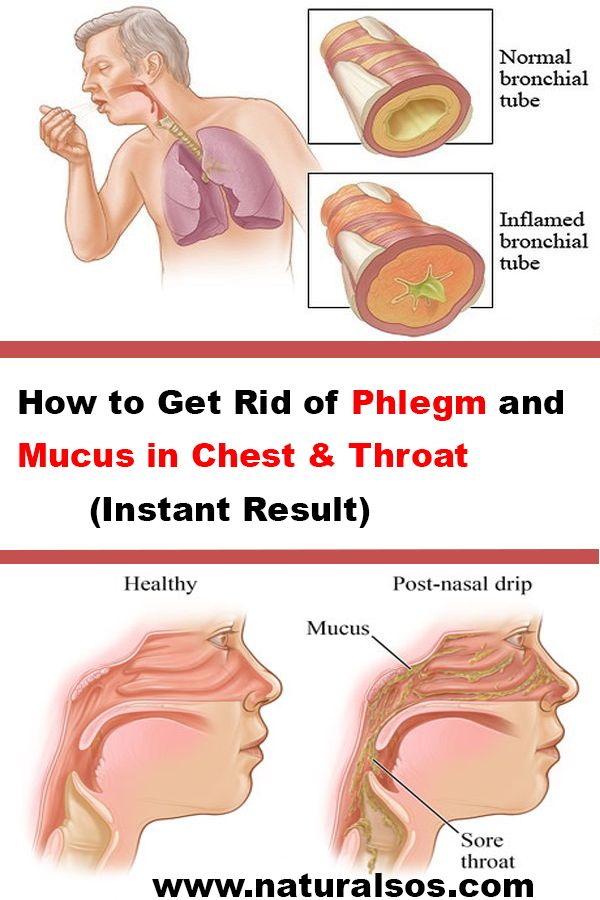 05%
05%