How to stop my child constantly coughing
Home Treatments and Seeking Help
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Coughing in toddlers
Colds and coughs are common in young children. Exposure to germs and fighting them helps kids develop their immune systems. Helping your child to feel comfortable and manage their symptoms can help them get the rest they need to help them recover.
A regular cough can last up to two weeks. Many coughs are due to common viruses that have no cure. Unless a cough is extreme or comes with other, serious symptoms (see our list below), the best solution is to offer comfort measures at home.
Cough treatment should aim to keep your child hydrated, relaxed, and sleeping well. It’s not important to try to stop the coughing itself.
Read on to discover toddler cough remedies you can try at home, plus learn how to identify the signs that your child needs to see a doctor.
8 Home remedies
Pay attention to the sound of your child’s cough to help you pick the best home remedy and so that you can properly explain the cough to a doctor. For example:
- Deep cough coming from the chest. It’s likely due to mucus in the airways.

- Tight cough coming from the upper throat. It may be due to an infection and swelling around the larynx (voice box).
- Mild cough with sniffing. It could be due to post-nasal drip from the back of your child’s throat.
1. Use saline nasal drops
You can buy these over-the-counter nasal drops at a pharmacy. Used with a nasal syringe or nose blowing, saline drops can soften mucus to help remove it.
Follow the instructions on the bottle to administer the nasal drops safely.
If it’s impossible to get these little drops in your toddler’s nose, sitting in a warm bath can also clear nasal passages and soften mucus. This helps prevent post-nasal drip.
You may especially want to use saline drops before bed or in the middle of the night if your toddler wakes up coughing.
Saline nasal drops are generally considered safe.
2. Offer fluids
Staying hydrated is especially important when your child is sick. Water helps the body fight illness and keeps airways moist and strong.
Water helps the body fight illness and keeps airways moist and strong.
One way to make sure your child is getting enough water is to have them to drink one serving of water (8 ounces or 0.23 liters) for each year of their life. For example, a one-year-old needs a minimum of one serving of water per day. A two-year-old needs two servings per day.
If they’re refusing their usual milk or not eating much, younger children may need more water. Offer water freely (at least every hour or two), but don’t push them to drink it.
In addition to enough water, you can offer popsicles to increase fluids and soothe a sore throat.
3. Offer honey
Honey is a natural sweetener that can help soothe a sore throat. Honey also has antibacterial properties and may help fight infection.
Honey isn’t safe for children who are under one year of age because there’s a risk of botulism.
For toddlers over one, you can give a spoonful of honey as often as you like, but be aware of the sugar intake that comes with it.
You can also try mixing the honey in warm water to make it easier for your child to consume the honey. This has the added benefit of helping to hydrate your child, too.
4. Elevate your child’s head when sleeping
Babies under one-and-a-half years old should not sleep with any pillows.
Getting your older toddler to fall asleep with their head on one or more pillows can be difficult, especially if your child is prone to moving around a lot while they’re asleep.
An option other than using pillows in the crib or bed to elevate your toddler’s head, is to try elevating one end of the mattress. You can do this by placing a rolled-up towel under the mattress on the end where your child’s head rests.
However, you should ask your pediatrician before attempting this.
5. Add moisture with a humidifier
Adding moisture to the air helps keep your child’s airways from drying out and loosens mucus. This may ease coughing and congestion.
When purchasing a humidifier, choose a cold air humidifier. Cold air humidifiers are safer for children and as effective as warm air humidifiers. If possible, use purified or distilled water to slow down mineral buildup inside the humidifier.
Cold air humidifiers are safer for children and as effective as warm air humidifiers. If possible, use purified or distilled water to slow down mineral buildup inside the humidifier.
Run a humidifier all night in the room where your toddler sleeps. During the day, run it in whatever room they’ll be spending the most time in.
If you don’t have a humidifier, you can try running a hot shower and blocking the crack under the bathroom door with a towel. Sit in the steamy bathroom to provide your child with some temporary relief.
6. Talk a walk in cold air
If it’s cold outside, you can try this folk remedy that uses the power of fresh air and exercise to relieve cough symptoms.
Bundle your child up for a walk in cold weather and aim for just a few minutes outside. You don’t want to exhaust your toddler, but there are many anecdotal stories of this helping coughs and shortening the length of a common cold.
Some parents even try opening the freezer door and standing their toddler in front of it for a few minutes if the child wakes up to a coughing fit in the middle of the night.
7. Apply vapor rub
It’s controversial whether vapor rubs that contain camphor or menthol are beneficial. Caretakers have been rubbing this balm on children’s chest and feet for generations, but one animal study suggested it may actually increase mucus, which can dangerously block tiny toddler airways.
Ask your pediatrician before using any vapor rub. If you do use a vapor rub, applying it to your child’s feet may be safer than on the chest where toddlers might touch it and then get it in their eyes.
Never use vapor rub on babies under two, and never put it on a child’s face or under their nose.
8. Use essential oils
These herbal products are gaining in popularity and some may be effective at easing a cough or muscle aches when applied on the skin or diffused into the air.
But always talk with your doctor before using essential oils. Not all oils are safe for toddlers, and dosage isn’t regulated.
Can you offer cough medicine?
Cough medicine isn’t recommended for toddlers or any child under six. It’s also not safe for young children, and it’s usually not effective at relieving their symptoms.
It’s also not safe for young children, and it’s usually not effective at relieving their symptoms.
Any combination medicine for treating more than one symptom is likely to give kids more side effects and increase the risk of overdose.
Only offer cough drops to children four years old and older due to choking risks.
For children over the age of one, you can try a homemade cough recipe of honey dissolved in warm water and lemon juice.
Treatments from the doctor
In some cases, you may need to see a doctor to treat your child’s cough.
If your child has croup, their pediatrician may prescribe a steroid to decrease inflammation. Croup causes a tight, barking cough that tends to occur along with a fever.
The cough is usually worse at night. Steroids work best when given right away and they can be given to even very young toddlers.
If your doctor determines that your toddler has a bacterial infection, they may prescribe antibiotics. It’s important to give your child the full treatment: don’t stop antibiotics just when symptoms go away.
Does my toddler need to see a doctor?
If you’ve been treating your child’s cough at home for a few days and it’s getting worse, call your pediatrician’s office. The on-call nurse can give you more treatment ideas and help you decided whether or not to come in for a visit.
Asthma and allergies can cause chronic coughs and need to be treated by a doctor. Make an appointment if you think your toddler’s cough is due to either asthma or allergies.
Signs that your child should see a doctor include:
- cough that lasts more than 10 days
- fever over 100.4˚F (38˚C) for more than 3 days
- labored breathing
- chest pain
- muscles pulling in around the neck or rib cage when breathing
- tugging on the ears, which may be a sign of ear infection
The doctor will observe your child’s breathing and, in some cases, may use an X-ray to get a diagnosis.
Go to an emergency room if your child:
- is lethargic or seems very ill
- showing signs of dehydration
- has rapid breathing or can’t catch their breath
- develops a blue tinge on the lips, nails, or skin, which is a sign of a lack of oxygen
The takeaway
Coughing is a common symptom in toddlers and can last for weeks.
Coughs may sound serious and can interrupt sleep, but unless your child is having difficulty breathing, showing signs of croup, or looking seriously sick, you can usually treat coughs at home.
Coughing (for Parents) - Nemours KidsHealth
What Are Coughs?
Coughs are one of the most common symptoms of childhood illness. A cough can sound awful, but usually isn't a sign of a serious condition. In fact, coughing is a healthy and important reflex that helps protect the airways in the throat and chest.
What Are the Different Types of Coughs?
Sometimes, though, a cough needs a doctor's care. Understanding the different types of cough can help you know when to handle them at home and when to call your doctor.
The most common types of coughs are:
- "barky" cough
- whooping cough
- cough with wheezing
- nighttime cough
- daytime cough
- cough with a fever
- cough with vomiting
- persistent cough
"Barky" Cough
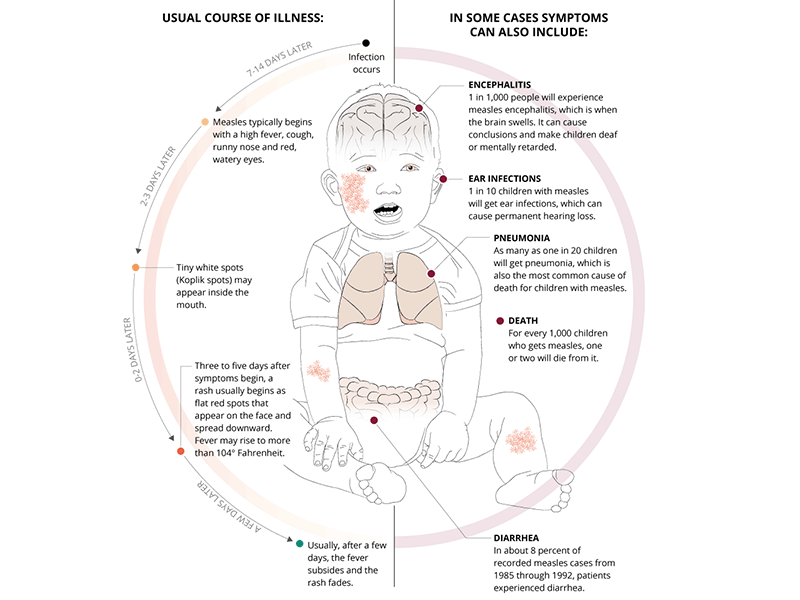
Barky coughs are usually caused by swelling in the upper airway. Most of the time, a barky cough comes from croup, a swelling of the larynx (voice box) and trachea (windpipe). Younger children have smaller airways that, if swollen, can make it hard to breathe. Kids younger than 3 are most at risk for croup because their airways are so narrow.
Most of the time, a barky cough comes from croup, a swelling of the larynx (voice box) and trachea (windpipe). Younger children have smaller airways that, if swollen, can make it hard to breathe. Kids younger than 3 are most at risk for croup because their airways are so narrow.
A cough from croup can start suddenly, often in the middle of the night. Most kids with croup will also have stridor, which is a noisy, harsh breathing that happens when the child inhales (breathes in).
Whooping Cough
Whooping cough (pertussis) is an infection of the airways caused by the
bacteriaBordetella pertussis. Kids with pertussis will have spells of back-to-back coughs without breathing in between. At the end of the coughing, they'll take a deep breath in that makes a "whooping" sound. Other symptoms are a runny nose, sneezing, mild cough, and a low-grade fever.
Whooping cough can happen at any age, but is most severe in infants under 1 year old who did not get the pertussis vaccine, which is part of the DTaP vaccine (diphtheria, tetanus, acellular pertussis). It's very contagious, so all kids should get the pertussis shot at 2 months, 4 months, 6 months, 15 months, and 4–6 years of age.
It's very contagious, so all kids should get the pertussis shot at 2 months, 4 months, 6 months, 15 months, and 4–6 years of age.
Cough With Wheezing
If your child makes a wheezing (whistling) sound when breathing out (exhaling), this could mean that the lower airways in the lungs are swollen. This can happen with asthma or with the viral infection bronchiolitis. Wheezing also can happen if the lower airway is blocked by a foreign object. A child who starts to cough after inhaling something such as food or a small toy should see a doctor.
Nighttime Cough
Lots of coughs get worse at night. When your child has a cold, the mucus from the nose and sinuses can drain down the throat and trigger a cough during sleep. This is only a problem if the cough won't let your child sleep.
Asthma also can trigger nighttime coughs because the airways tend to be more sensitive and irritable at night.
Daytime Cough
Cold air or activity can make coughs worse during the daytime. Try to make sure that nothing in your house — like air freshener, pets, or smoke (especially tobacco smoke) — is making your child cough.
Try to make sure that nothing in your house — like air freshener, pets, or smoke (especially tobacco smoke) — is making your child cough.
Cough With a Fever
A child who has a cough, mild fever, and runny nose probably has a common cold. But coughs with a fever of 102°F (39°C) or higher can sometimes be due to pneumonia, especially if a child is weak and breathing fast. In this case, call your doctor immediately.
Cough With Vomiting
Kids often cough so much that it triggers their gag reflex, making them throw up. Also, a child who has a cough with a cold or an asthma flare-up might vomit if lots of mucus drains into the stomach and causes nausea. Usually, this is not cause for alarm unless the vomiting doesn't stop.
Persistent Cough
Coughs caused by colds due to viruses can last weeks, especially if a child has one cold right after another. Asthma, allergies, or a chronic infection in the sinuses or airways also might cause lasting coughs. If your child still has a cough after 3 weeks, call your doctor.
How Are Types of Coughs Diagnosed?
If you're concerned about your child's cough, call your doctor. Depending on the type of cough, other symptoms, and how long it's lasting, the doctor might want to see your child.
Many health care providers now offer telehealth visits, which can save parents a trip to the office (especially for a nighttime cough). "Video chatting" lets doctors see and hear a child cough, and often this is enough to make a diagnosis or rule out a serious problem. Hearing the cough will help the doctor decide whether (and how) to treat it.
How Are Coughs Treated?
Most coughs are caused by viruses and have to just run their course. Sometimes, this can take up to 2 weeks. Doctors usually don't prescribe antibiotics because these only work against bacteria.
Unless a cough won't let your child sleep, cough medicines are not needed. They might help a child stop coughing, but they don't treat the cause of the cough. If you do use an over-the-counter (OTC) cough medicine, call the doctor to be sure of the correct dose and to make sure it's safe for your child.
Do not use OTC combination medicines (like "Tylenol Cold") — they have more than one medicine in them, and kids can have more side effects than adults and are more likely to get an overdose of the medicine.
Cough medicines are not recommended for any children under 6 years old.
How Can I Help My Child Feel Better?
To help your coughing child feel better:
- For a "barky" or "croupy" cough, turn on the hot water in the shower in your bathroom and close the door so the room will steam up. Then, sit in the bathroom with your child for about 20 minutes. The steam should help your child breathe more easily. Try reading a book together to pass the time.
- A cool-mist humidifier in your child's bedroom might help with sleep.
- Sometimes, brief exposure to cool air outdoors can relieve the cough. Make sure to dress your child appropriately for the outdoor weather and try this for 10–15 minutes.
- Cool beverages like juice can be soothing and it is important to keep your child hydrated.
 But do not give soda or orange juice, as these can hurt a throat that is sore from coughing.
But do not give soda or orange juice, as these can hurt a throat that is sore from coughing. - You should not give your child (especially a baby or toddler) OTC cough medicine without first checking with your doctor.
- If your child has asthma, make sure you have an asthma action plan from your doctor. The plan should help you choose the right asthma medicines to give.
- Cough drops are OK for older kids, but kids younger than 3 years old can choke on them. It's better to avoid cough drops unless your doctor says that they're safe for your child.
When Should I Call the Doctor?
Always call your doctor if your child is coughing and:
- has trouble breathing or is working hard to breathe
- is breathing faster than usual
- has a blue or dusky color to the lips, face, or tongue
- has a high fever (especially if your child is coughing but does NOT have a runny or stuffy nose)
- has any fever and is younger than 3 months old
- is younger than 3 months old and has been coughing for more than a few hours
- makes a "whooping" sound when breathing in after coughing
- is coughing up blood
- has stridor (a noisy or musical sound) when breathing in
- has wheezing when breathing out (unless your doctor already gave you an asthma action plan)
- is weak, cranky, or irritable
- is dehydrated; signs include dizziness, drowsiness, a dry or sticky mouth, sunken eyes, crying with little or no tears, or peeing less often (or having fewer wet diapers)
Children's tics: symptoms, causes, treatment
Have you noticed that your child blinks more than usual, twitches his shoulders and coughs? Perhaps these are manifestations of tics. Why they arise and how to treat them correctly, Galina Anatolyevna Zueva, chief pediatric neurologist of the Ministry of Health of the Tver Region, will tell.
Why they arise and how to treat them correctly, Galina Anatolyevna Zueva, chief pediatric neurologist of the Ministry of Health of the Tver Region, will tell.
What are tics?
Tics are involuntary violent movements that occur in certain muscle groups.
Tics are most common in children aged 4 to 6 years . This is due to the maturation of the subcortical parts of the brain, which most often ends by the age of seven or eight.
If, for some reason, a little more activating (or, conversely, fewer inhibitory) neurons are produced in the child's body than required, and the mode of motor and other load is not observed, then he starts having problems. It can be attention deficit hyperactivity disorder, or sleep disturbances, or tics. nine0003
From the age of three or four, your baby begins to grow very actively and explore the world. In order for the cognitive function to be fast, for it to absorb a large amount of information, and for the brain to mature, the child needs a lot of activating neurotransmitters. He must have time to climb everywhere, jump, look, speak, speak, ask a bunch of questions, understand and assimilate everything he hears. If activating neurotransmitters are used correctly, then the child develops harmoniously: he is smart, but at the same time he can control himself, follow the rules, and show perseverance during kindergarten classes. It's perfectly normal that your child is active, inquisitive, fast. When a baby does not use these neurotransmitters for movement, communication, learning (for example, he sits at home all day, he is not allowed to walk outside), then various problems may arise: hyperactivity syndrome, sleep disturbance, behavior problems.
He must have time to climb everywhere, jump, look, speak, speak, ask a bunch of questions, understand and assimilate everything he hears. If activating neurotransmitters are used correctly, then the child develops harmoniously: he is smart, but at the same time he can control himself, follow the rules, and show perseverance during kindergarten classes. It's perfectly normal that your child is active, inquisitive, fast. When a baby does not use these neurotransmitters for movement, communication, learning (for example, he sits at home all day, he is not allowed to walk outside), then various problems may arise: hyperactivity syndrome, sleep disturbance, behavior problems.
So, in order for a child to develop properly, he must run a lot, climb, talk, learn about the world around him, experience various emotions. This forms spatial-figurative thinking, motor skills, synchrony of the work of the two hemispheres, develops the brain and at the same time correctly wastes all the developed neurotransmitters of activity. nine0009 At the age of 3-5 years, the child is smart, he quickly switches, but at the same time copes with his tasks: if he needs to sit, he will sit normally, study, do something. This is the standard development of the child, which should be.
nine0009 At the age of 3-5 years, the child is smart, he quickly switches, but at the same time copes with his tasks: if he needs to sit, he will sit normally, study, do something. This is the standard development of the child, which should be.
Types of tics in children
Most often, children aged 3-6 years have motor and vocal tics.
Motor are movement-related tics: blinking, blinking, squinting, nose twitching, pulling clothes, shouldering, etc. nine0003
Vocal - tics associated with breathing. These are all kinds of huffing, sniffing, coughing, whistling. By the way, a frequent case in my practice: a child coughs for a long time, they take him to the doctors, looking for the cause, but in fact he has a vocal tic, which needs to be treated by a neurologist. It doesn't have to be a tick, but it also happens and needs to be taken into account.
Quite often there are combinations of several ticks. For example, blinking, twitching the corners of the nose and the behavior of the shoulders at the same time. Tics can be more pronounced when certain muscle groups, the so-called segmental tics . There may be a combination of motor and vocal tics - for example, blinking eyes and grunting at the same time. At the same time, he can independently delay the manifestation of a tick for some time (up to several seconds) and repeat it on request. This is the so-called duplication, which is a distinctive feature of tics from other types of obsessive movements - hyperkinesis.
For example, blinking, twitching the corners of the nose and the behavior of the shoulders at the same time. Tics can be more pronounced when certain muscle groups, the so-called segmental tics . There may be a combination of motor and vocal tics - for example, blinking eyes and grunting at the same time. At the same time, he can independently delay the manifestation of a tick for some time (up to several seconds) and repeat it on request. This is the so-called duplication, which is a distinctive feature of tics from other types of obsessive movements - hyperkinesis.
A separate, most complex, case of generalized tics is Tourette's syndrome , when tic manifestations occur in multiple muscle groups, when the same child has several varieties of vocal tics. They are very pronounced and cause great inconvenience to the child. In this case, examination and treatment by a neurologist is strictly required. nine0003
Tics can be transient, i. e. appeared, were observed for some time in the child, and then passed. But if the tics continue for more than a year, then these are already chronic tics , so examination and treatment are required.
e. appeared, were observed for some time in the child, and then passed. But if the tics continue for more than a year, then these are already chronic tics , so examination and treatment are required.
Causes of tics in children
As we have already said, this is a lesion of the subcortical formations in the child's brain. It may be due to the peculiarities of the development of the brain or be damaged by some factor.
A sedentary lifestyle is one of the most common triggers for tics. When a child is not active enough, he does not consume all the neurotransmitters of activity. Muscles need to move, but they don't get it. As a result, tics occur. The child must definitely run, and it’s better not along a flat asphalt path, but along a forest path, where you need to crawl under a tree somewhere, run along a log, turn away from the root. All this better forms the nervous system, helps to develop spatial-figurative thinking. Can't go to the forest? In the park, get off the flat path and walk along the dirt path, just dress appropriately so that both you and your baby feel comfortable. nine0009 This is one of the most common mistakes parents make: they spend hours walking in parks, dressed up on paths, but this is of little use. It is much more useful for the child to be closer to nature, to study, to learn. And a lot of emotions that he receives at the same time correctly spend the energy inherent in him. When a child sits at home all day with a tablet, this energy accumulates in him, and then it pours out into fights, disobedience and tics as well.
nine0009 This is one of the most common mistakes parents make: they spend hours walking in parks, dressed up on paths, but this is of little use. It is much more useful for the child to be closer to nature, to study, to learn. And a lot of emotions that he receives at the same time correctly spend the energy inherent in him. When a child sits at home all day with a tablet, this energy accumulates in him, and then it pours out into fights, disobedience and tics as well.
Particularly susceptible to tics attention-deficit children . Due to illness, they already have a failure in the formation of neurotransmitters, and when we do not allow them to fully use all this energy, various problems appear: headaches, insomnia, tics.
Unfavorable psycho-emotional environment is another common cause of tics in children. For example, if a child really does not like going to kindergarten, which causes negative emotions in him and creates a lot of stress, and parents do not have time to discuss this situation with him, explain it, and agree.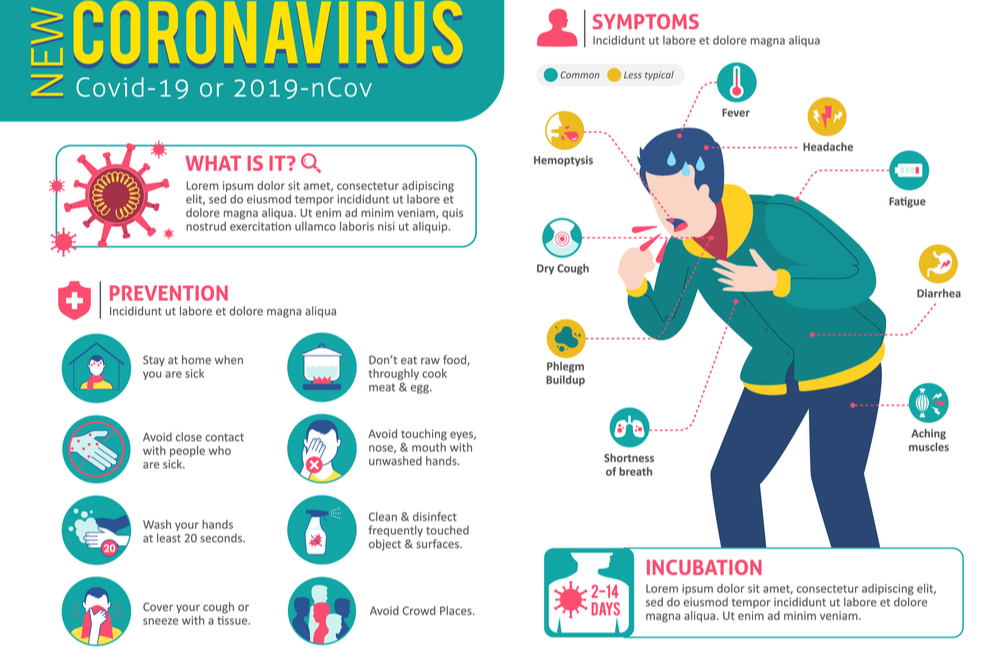 In this case, the child's nervousness can also get a side effect in the form of a tick. nine0003
In this case, the child's nervousness can also get a side effect in the form of a tick. nine0003
Some difficult situation in the family can also lead to stress , for example, when parents demand high results from a child in all subjects, forming the so-called excellent student syndrome. The kid is afraid not to cope, he has a great responsibility, as a result, neuroses, tics, most often vocal ones, arise. Moreover, they can persist for a long time, manifesting themselves in stressful situations.
A common cause of tics is divergence of views on raising a child in one family . When, for example, parents treat him strictly, and grandparents, on the contrary, indulge all whims. The child ceases to understand how to behave, and this leads to neurosis.
This is all about common tics in children aged 4 to 6 years. But there are also more difficult cases. If tics appear in children older than seven years , then the reason is no longer in the usual maturation of the body, but in some kind of pathology.
This may be a consequence of frequent angina, streptococcus , when an autoimmune process occurs that damages subcortical formations and malfunctions in the form of various tics or hyperkinesis. They must be treated.
Also the cause may be the effects of frequent mononucleosis , this virus also often affects the subcortical nuclei.
There are a number of hereditary diseases that cause tics. They are rare, but nonetheless. For example, diseases associated with a violation of the proper breakdown of copper and iron. Among them is Wilson-Konovalov's disease, in which copper begins to be deposited in the liver and other internal organs, including in the subcortical formations of the brain, and leads to various types of hyperkinesis, tics. These diseases are necessarily excluded in children with tics. nine0003
When should tics be treated in children?
If these are single simple motor tics in a child aged 4 to 6 years, they are rare and do not interfere with the baby's life, then most likely this is due to a slight overabundance of neurotransmitters. Such tics can be left untreated , they will go away on their own in a year or two.
Such tics can be left untreated , they will go away on their own in a year or two.
However, if the tics are frequent and prevent the child from concentrating, then, of course, this should be examined and treated .
Pay special attention to tics that appear in a child after 7-8 years . They must be examined and found out the cause of the occurrence.
I must say that tics are well treated . There are a lot of quality products out there now. It is important here that the doctor correctly selects the right medicine and dosage. For the treatment of tics, a special drug regimen is used, the dosage here is slightly higher than usual, but you should not worry about this - the drugs are well tolerated and will not harm the health of the child. Sometimes for chronic tics, medicines are given for the entire school year. nine0003
Prevention of tics in children
Follow these simple guidelines and your child will grow up healthy and happy.
Walk with your child as much as possible. It’s good if he runs not only around the yard or a flat path, but also along earthen paths with some small obstacles. To do this, it is enough to get off the main alley in the park and go to explore the lawns.
Study natural phenomena. Listen to the sounds of nature, teach your child to distinguish them, learn with him the laws of the world around him. All this will not only develop the baby's brain, but also help him use neurotransmitters to good use and cope with stress. nine0003
Play active games with your child. It is normal for a child between the ages of 2 and 5 to spend about 10 hours a day in active movement. Let's say he worked out, drew, then ran in the yard, played with the dog, went down the hill, explored something, met someone on the playground, talked, then rested and ran to play again. Then the neurotransmitters will be spent correctly and the child will not have problems with sleep, or with nervousness, or with behavior. nine0003
nine0003
Talk to your child. And this is a very important point. Something that many parents often forget about. Meanwhile, it is conversations with the baby that can solve many neurological problems. It is important not only to talk to the child, but also to listen to what he says to you in response. From the age of two, the baby has every right to make some decisions, to choose something - for example, in which T-shirt to go for a walk or what color to take a toy. Give him the opportunity to participate in family life, listen to his opinion. You need to understand that this opinion should be reasoned, that is, not just “I want”, but “I want, because ...” This will not only help you create and maintain a trusting relationship with your child, but also keep him healthy and save him from many behavioral problems. nine0003
Good luck to you and your children!
The child breathes through his mouth - what to do
St. Petersburg, Novocherkassky pr-t, 33, bld. Make an appointment
Make an appointment
Correction of bite Dentistry for teenagers
08/30/2021
Mouth breathing in children is not uncommon. This happens when there is not enough air coming through the nose.
There can be many reasons: a runny nose or inflamed adenoids, etc. The air passage is completely blocked or noticeably narrowed, and the body is forced to rebuild - for this, the mouth is involved. nine0003
Is it acceptable for children to breathe through their mouths? Yes. This breathing is not physiological - it is a "reserve airfield" for a cold. A week or two of such a regimen will not do harm. But if there is no runny nose, and the mouth is constantly open, this is already a cause for concern.
If a child breathes through his mouth all the time, a whole cascade of changes takes place.
Firstly, the width of the airways is still not enough for a normal supply of oxygen, hypoxia develops, which affects the general condition of the child: he becomes irritable and capricious, gets sick and tired more often, there is no success in sports, academic performance decreases. nine0003
nine0003
Secondly, there are noticeable metamorphoses at the physiological level: the lower jaw goes down and goes back, followed by the tongue.
Even posture suffers: the head is pulled forward, the person unconsciously begins to stoop. So the body tries to cope with the lack of oxygen. And it is completely useless to say "straighten up!". Correction must begin with a visit to the ENT doctor.
What happens to the bite when a child breathes frequently through an open mouth?
When breathing through the nose, the tip and front third of the tongue are in the correct position in the mouth. So the upper jaw receives the necessary stimulus for development. nine0003
But if the baby breathes deeply through the mouth, the tongue falls down along with the lower jaw, and the upper jaw does not receive enough pressure, does not develop and remains narrow. In this case, the lower part of the chin moves even more back. This is how the distal bite is formed.
In turn, the lips do not close and do not exert the necessary pressure on the dentition. As a result, the front teeth deviate forward. It looks ugly and increases the risk of injury.
As a result, the front teeth deviate forward. It looks ugly and increases the risk of injury.
All these changes are reflected in the appearance: the face is elongated, the chin moves back, a “second chin” appears, not associated with excess weight. nine0003
If the child began to constantly breathe through the mouth, dry mouth makes itself felt, and saliva ceases to protect the teeth. Therefore, in children with such a problem, caries spreads instantly.
How to wean a child to breathe through his mouth?
To solve this problem, it is important to work in a team with several doctors. The ENT corrects the patency of the nasopharynx, the osteopath corrects the posture, the dentist eliminates the foci of infection, the orthodontist expands the upper jaw and sets the lower jaw to a standard position. The speech therapist retrains the tongue to lie back where it is supposed to - at the top, restores the weakened tone of the lips and shows exercises for differentiating nasal and oral breathing.