How to relieve headaches when pregnant
Headache and migraine remedies that are safe during pregnancy | Your Pregnancy Matters
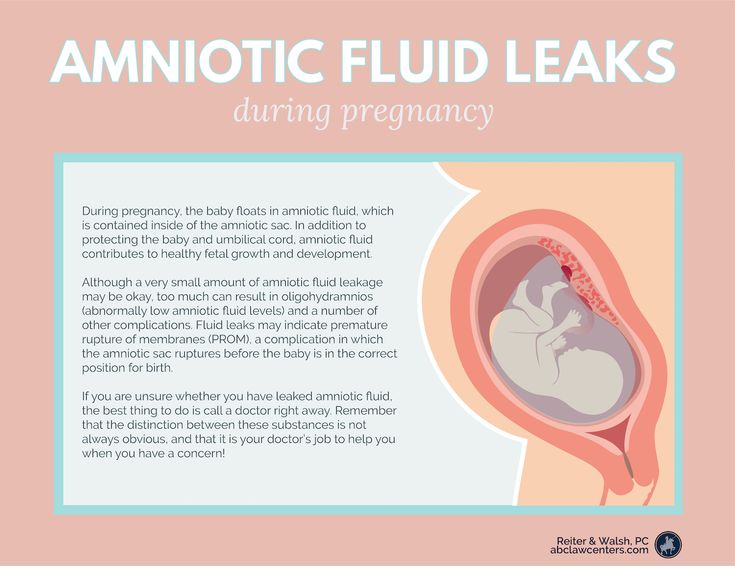
Occasional, mild headaches during pregnancy usually are nothing to worry about.Most women deal with headaches at some point in their lives. Data from the Centers for Disease Control and Prevention suggest that one in five women had a severe acute headache or migraine in the previous three months. Additionally, migraines are more common in women than men – approximately 18 percent of women have them compared to 6.5 percent of men.
Because headaches and migraines are so common, it’s probably no surprise that many women deal with them during pregnancy. For the majority of pregnant women, occasional headaches or migraines are no cause for alarm, and most standard treatments are safe. However, suffering a severe headache at key times during or after pregnancy can indicate a serious medical emergency.
Common types of headaches and treatment options
Primary headaches
Primary or acute headaches arise once in a while and typically pass after a few hours. Tension headaches are the most common type and are characterized by muscle tightness and localized pain in the head and neck.
Primary headaches in pregnant women usually can be treated at home. Rest, a neck or scalp massage, hot or cold packs, and over-the-counter anti-inflammatory drugs such as Tylenol, aspirin, or ibuprofen can reduce the pain. However, if you start to have frequent or severe headaches, talk to your doctor to determine the cause.
Migraines
Migraines tend to be episodic (frequent and long-lasting) and typically cause additional neurological symptoms, such as:
● Blurred or tunnel vision
● Hallucinations
● Light sensitivity
● Nausea and vomiting
Studies have shown that migraines can be triggered by hormonal changes, including right before your period or as a result of taking oral contraceptives.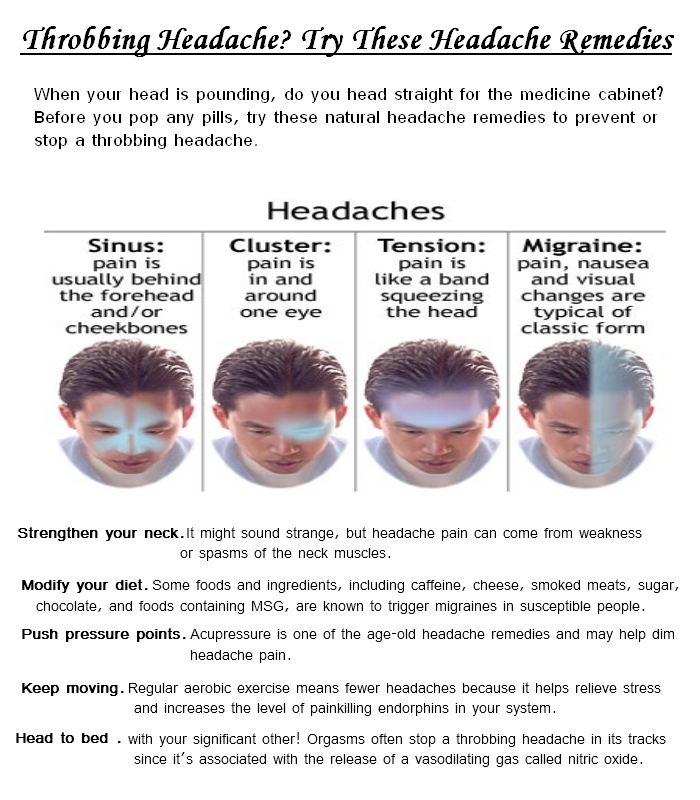 Interestingly, some women who have migraines find that the frequency or intensity of their symptoms decreases during pregnancy. Research does not suggest, however, that pregnancy triggers the onset of migraines – if you have your first migraine during pregnancy, it’s likely coincidental.
Interestingly, some women who have migraines find that the frequency or intensity of their symptoms decreases during pregnancy. Research does not suggest, however, that pregnancy triggers the onset of migraines – if you have your first migraine during pregnancy, it’s likely coincidental.
Treatment during pregnancy is fairly similar to standard treatment. Anti-inflammatory drugs are generally safe and effective during pregnancy when used in a limited manner. Midrin is a commonly prescribed headache medication that contains acetaminophen along with a mild sedative. Midrin also has vasoconstrictive properties, which means it narrows the blood vessels, thereby reducing blood flow and pain.
Sumatriptan, commonly known as Imitrex, is another medication that reduces blood flow to the brain. It works best to stop a migraine if it’s taken as soon as symptoms present. Most nausea medications prescribed to women with migraines are safe to use during pregnancy, but I suggest reviewing the medications you take for migraine relief with your obstetrician at your first prenatal visit, just to be safe.
Certain drugs called ergotamines have a stronger vasoconstrictive effect and can adversely affect fetal growth. They also can stimulate uterine activity. Because of this, they absolutely should not be used during pregnancy.
Severe migraines might require hospitalization so you can receive fluids, pain medication, or anti-nausea medication through an IV if you are unable to keep medications down.
"Most women don’t require special care for headaches and migraines during pregnancy, and most standard remedies are safe. However, certain types of headaches require immediate medical attention to avoid potentially harmful health issues."
– Robyn Horsager-Boehrer, M.D.
When headaches are secondary to other problems
Headaches can result from other conditions, some of which are life-threatening:
● Stroke: Sudden and severe headaches might be a sign of a stroke. Women who have strokes during pregnancy or after delivery typically describe the pain as the worst headache of their lives. They also might report other symptoms, such as speech problems, vision issues, or functional problems on one side of the face or body. At the emergency room, the doctor will evaluate you for stroke symptoms, such as visual changes, facial drooping, and arm or leg weakness. If you are having or had a stroke, we will get you emergency treatment at our Advanced Comprehensive Stroke Center.
Women who have strokes during pregnancy or after delivery typically describe the pain as the worst headache of their lives. They also might report other symptoms, such as speech problems, vision issues, or functional problems on one side of the face or body. At the emergency room, the doctor will evaluate you for stroke symptoms, such as visual changes, facial drooping, and arm or leg weakness. If you are having or had a stroke, we will get you emergency treatment at our Advanced Comprehensive Stroke Center.
● Preeclampsia: A headache with preeclampsia (a pregnancy complication characterized by high blood pressure) can indicate a dangerous spike in blood pressure. The doctor will assess you and might admit you to the hospital for management of blood pressure and treatment to prevent seizures.
● Spinal fluid leak: A headache after an epidural or spinal block can indicate a spinal fluid leak, especially if it worsens when you sit or stand up. The most effective treatment is an epidural blood patch, in which the doctor injects a sample of your blood into the leaking area, essentially plugging the hole. This therapy provides dramatic relief right away.
This therapy provides dramatic relief right away.
Occasional mild headaches are common in women. The vast majority are no cause for alarm and can be treated at home, with guidance from your doctor. However, if your symptoms are severe or something just doesn’t seem right, it’s much better to seek care and be safe rather than sorry.
Stay on top of health care news. Subscribe to our blog today.
Migraines & Headaches During Pregnancy: Causes and Treatment
Written by Rebecca Buffum Taylor
In this Article
- Causes of Migraine Headaches
- Tracking Triggers With a Migraine Diary
- Tests for Migraines
- Self-Care of Migraines
- Medications for Migraines
- Acute Migraine Treatment
- Preventive Migraine Treatment
If you're pregnant, you're no doubt experiencing new aches and pains. If you're also one of the millions of pregnant women who experience migraines, you might be glad to know that pregnancy eases migraine headache symptoms for many women.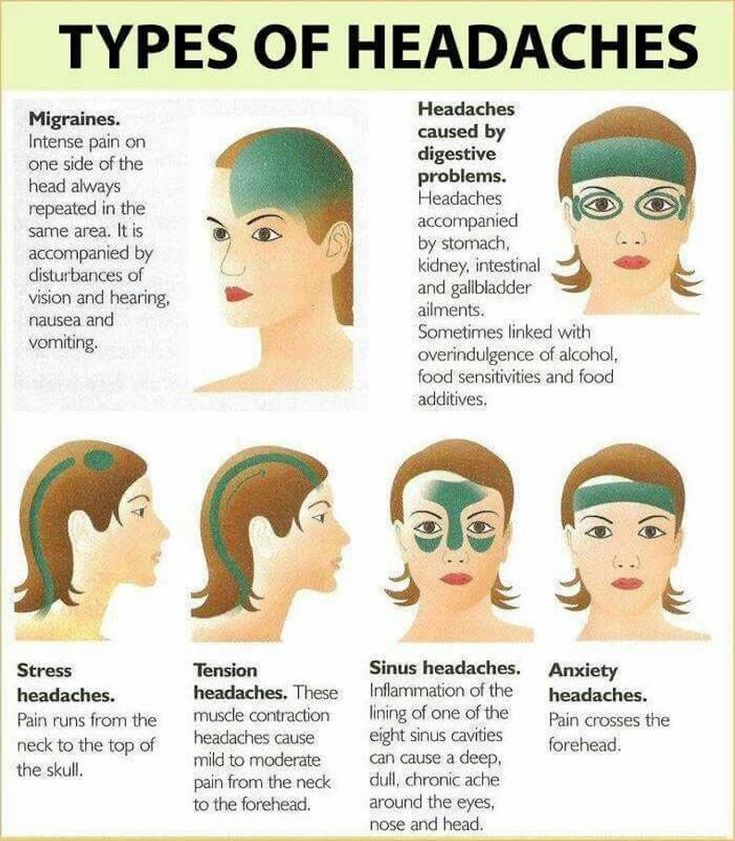 But even if it doesn't for you, the information in this article can help you cope.
But even if it doesn't for you, the information in this article can help you cope.
Causes of Migraine Headaches
Exactly what causes migraine headaches isn't known. But migraines appear to involve changes in nerve pathways, neurochemicals, and blood flow in the brain.
Researchers believe that overly excited brain cells stimulate a release of chemicals. These chemicals irritate blood vessels on the brain's surface. That, in turn, causes blood vessels to swell and stimulate the pain response.
Estrogen is thought to play a role in migraines. That's why pregnancy, menstruation, and menopause often change a woman's pattern of migraine headaches.
The neurotransmitter serotonin also appears to have a key role in migraines.
Tracking Triggers With a Migraine Diary
Hormone changes during pregnancy are not the only thing that can trigger migraine headaches. Most women have a combination of triggers. For instance, stress, skipped meals, and lack of sleep may all trigger a migraine. And something that triggers a migraine one day may not bother you at all the next.
And something that triggers a migraine one day may not bother you at all the next.
Some migraines last a few hours. Others, if left untreated, could last a couple of days. Migraines are quite unpredictable. So while pregnancy may make them worse for one woman, they might completely disappear for another.
A headache diary can let you track your particular triggers. This will help your doctor decide on what treatment will work best to relieve your specific symptoms. It may also help you recognize a pattern that tells you which triggers to avoid while you're pregnant.
Each time you have a headache, write down:
- Your specific symptoms: where you feel the pain, what the pain feels like, and any other symptoms such as vomiting or sensitivity to noise, smells, or bright light
- The time your headache started and ended
- Food and beverages you had during the 24 hours before the migraine
- Any change in your environment, such as traveling to a new place, a change in weather, or trying new kinds of food
- Any treatment you tried, and whether it helped or made the headache worse
Common headache triggers include:
- Chocolate
- Caffeine
- Foods that contain the preservatives MSG (monosodium glutamate) and nitrates
- Aspartame, the sweetener in NutraSweet and Equal
Tests for Migraines
Headaches can be caused by a pregnancy complication called preeclampsia. So your doctor may evaluate you for that condition before making a diagnosis of migraine. Be sure to tell your doctor about all the medications you're taking, including over-the-counter products and natural supplements. Also let your doctor know whether anyone in your family has had migraines.
So your doctor may evaluate you for that condition before making a diagnosis of migraine. Be sure to tell your doctor about all the medications you're taking, including over-the-counter products and natural supplements. Also let your doctor know whether anyone in your family has had migraines.
The doctor often can diagnose migraine from a headache diary and your medical history. CT scans and other radiology tests to rule out other causes of your headaches aren't usually advised in pregnancy. That's because of the potential risks to the fetus.
Self-Care of Migraines
Your first line of defense against migraine headaches is a healthy lifestyle and self-care. Here are some tips to help you manage migraines during pregnancy:
- Avoid your known triggers, such as specific foods, as much as possible.
- Keep a predictable schedule of meals and snacks.
- Drink plenty of water.
- Get plenty of rest.
- Consider taking a class in biofeedback or other relaxation techniques.

- When pain strikes, try ice packs, massage, and resting in a quiet, darkened room.
Medications for Migraines
If you're pregnant -- or planning to get pregnant soon -- your doctor will generally advise you to stay off medications unless they're absolutely needed. Together, you'll have to weigh the potential effects of a drug on your unborn baby. In some cases, a decision will need to be made based on scant or inconclusive research into a particular drug.
Many of the anti-migraine medications to treat or prevent migraine headache and its symptoms should be avoided during pregnancy. Some have been linked to birth defects in babies. Other medications are associated with pregnancy complications. For instance, some have been associated with bleeding, miscarriage, or intrauterine growth restriction (IUGR), a condition in which the uterus and fetus don't grow normally.
Acute Migraine Treatment
Acute treatment aims to stop a migraine attack after its first signs appear.
Pain relievers, also called analgesics, may help ease the intense pain of migraines. These general pain-relieving drugs, though, aren't specific to the migraine pain pathway:
- Acetaminophen is generally considered low-risk during pregnancy.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, may carry a risk of bleeding and miscarriage if taken in early pregnancy. There is also a possible risk of heart complications in the baby if they are taken in the third trimester. Aspirin taken near delivery may lead to excess blood loss in mothers during birth.
- Most NSAIDs, including ibuprofen -- sold over the counter under the brand names Advil and Motrin -- and naproxen -- sold as Aleve, Naprosyn and other brands -- don't have enough controlled human research studies to assess all their risks in pregnancy.
- Narcotic pain relievers should generally be avoided. There is a dual risk of addiction in both mothers and babies if they are used for prolonged periods of time.
Ergotamines work specifically for migraine pain. But doctors advise against taking these drugs during pregnancy. They carry a risk of birth defects, especially if taken in the first trimester. These drugs may also stimulate labor contractions and premature birth.
Triptans work specifically on the migraine pain pathway. Triptans aren't known to cause birth defects. But most research to date has focused on animals, not humans. Your doctor can help you decide is it is safe for you and your unborn baby.
Other medications may be prescribed for relief of specific symptoms of a migraine during pregnancy. For instance, antiemetics help soothe the vomiting and nausea that can accompany a migraine. But many of the drugs typically used for migraine haven't been adequately studied in pregnancy, so their safety or risk to the fetus has not been determined.
Preventive Migraine Treatment
If you have severe, recurring attacks, preventive treatment may stop future attacks or reduce their severity. Many of the drugs used for prevention were originally used for other conditions, such as high blood pressure.
Many of the drugs used for prevention were originally used for other conditions, such as high blood pressure.
See a neurologist experienced with treating pregnant women. They'll prescribe a medicine in the lowest dose needed to help you and likely recommend some kind of talk therapy. Relatively safe medications for migraines include beta-blockers, such as metoprolol (Lopressor, Toprol XL) and propranolol (Inderal LA, Inderal XL, InnoPran XL)
When you're pregnant, always talk with your doctor before taking any drug, herbal product, or natural medicine.
If you can't take medications or wish not to, there are some devices which might be worth considering. Cefaly is a portable headband-like device that gives electrical impulses on the skin at the forehead. This stimulates a nerve associated with migraine headaches. Cefaly is used once a day for 20 minutes, and when it's on you'll feel a tingling or massaging sensation.
SpringTMS is a magnet placed on the back of the head at the first sign of a headache. It gives off a split-second magnetic pulse that stimulates part of the brain. It usually has no side effects. Also, gammaCore is a hand-held portable device which is a noninvasive vagus nerve stimulator (nVS). When placed over the vagus nerve in the neck, it releases a mild electrical stimulation to the nerve's fibers to relieve pain.
It gives off a split-second magnetic pulse that stimulates part of the brain. It usually has no side effects. Also, gammaCore is a hand-held portable device which is a noninvasive vagus nerve stimulator (nVS). When placed over the vagus nerve in the neck, it releases a mild electrical stimulation to the nerve's fibers to relieve pain.
If you're seeing a headache specialist, double-check with your obstetrician or certified midwife about the safety of any medications ordevices during pregnancy. While migraine pain may be excruciating, taking a risk with your baby's health could cause lifelong health problems for your child.
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, as:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.

Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraine during pregnancy either remains unchanged or worsens. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman throughout the entire period of pregnancy and after childbirth too.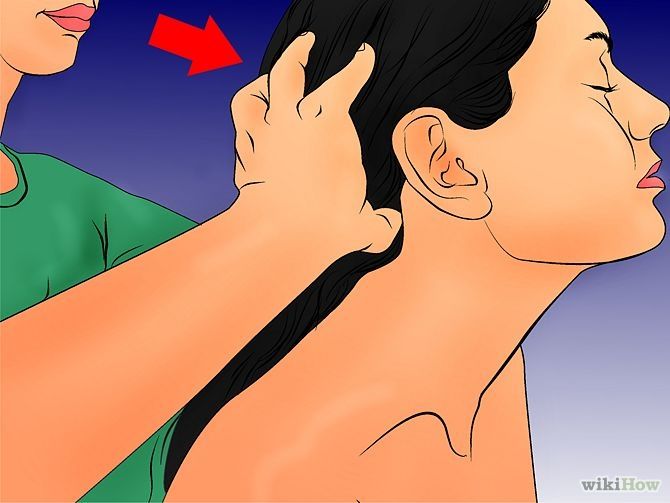
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink enough fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations. This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make attacks less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods.
 Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfere with your life, then under the supervision of a specialist, you can resort to drug therapy.
PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted.
 However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.
When to see a doctor:
-
migraine occurred for the first time during pregnancy;
-
if migraine attacks suddenly become more frequent and stronger;
-
if the aura became longer or appeared for the first time;
-
if the headache is rapidly increasing and has an unusual character;
-
if the pressure rises during the headache.
Follow our Instagram to read the latest materials on the diagnosis and treatment of headaches!
cluster headache. Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Pregnancy: how to beat a headache without pills | 74.ru
All newsTake it out correctly: how much money you can take with you abroad and how to pay there
They promised not to call. How mobilization affected the labor market in the Chelyabinsk region
The multifunctional center under construction on Universitetskaya Embankment may rise in price for the second time
Shelling of cities and a terrorist attack on a training ground in the Belgorod region: news around the SVO for October 16
Traktor beat Ak Bars
“Spring flowers under leaden October clouds”: snowdrops bloomed in the Chelyabinsk region in autumn
I was driving with special signals on red: in Chelyabinsk, an ambulance with a patient got into an accident at a busy intersection
A loud theater scandal in Novosibirsk got into a new novel by the author of Harry Potter — we asked JK Rowling about it
In Chelyabinsk, a female driver and two children were injured in a collision of two foreign cars
“The most dangerous time for everyone”: Pavel Globa — about what awaits Russia and the world from October 25 to November 8
35 years old, second grade, was discharged from the army. The story of a mobilized single father
The story of a mobilized single father
"Day and night we look out the window - it will crash there, then there." A report from Belgorod, which lives under daily shelling
The police are looking for the owner of the Alabai, who attacked a child and killed several dogs in Chelyabinsk
Beets for the winter: from dressing for borscht to caviar - 5 simple and incredibly tasty recipes for preparations
mobilized South Ural residents in Chebarkul
The authorities of Donetsk reported about the shelling of the city administration
Doctors told what foods make you want to eat even more
Do we have no future? Independent demographer - about what will happen to the birth rate in the country in the coming years 11 people died
"The only man was stolen." How the village of Mogilnoye was mobilized, depriving the chance of survival
An oil depot caught fire in Belgorod, and Lukashenka called for peace: news around the SVO for October 15
A triple volley and a Shaman's song: two mobilized people who died in a special operation were buried in the Chelyabinsk region
He lived in a hut, and now he is renting a one-room apartment: the story of the most decent beggar
In the Chelyabinsk region, a teacher was fined 40,000 under the article on discrediting the Russian Armed Forces
Buckwheat drenched in kefir: a simple and cheap recipe that will help you lose up to 5 kg per week - for whom it suits
A completely blind woman creates masterpieces by touch - take a look at her work
Auto No matter what! We show the anti-crisis Lada Granta at a price of 680,000
Chelyabinsk region says goodbye to those mobilized who died in a special operation
Difficulties with renting housing and delicious food: what you need to know before traveling to Istanbul
Forecasters warned South Ural residents about the approaching wet snow
"Come on, surprise people": check what you remember about the "Star Factory"
Are Russian doctors forbidden to leave the country? What to expect next for doctors and whether restrictions are legal
Pardon for heroism: the Federation Council has prepared a bill on the participation of convicts in hostilities
“They say we hide behind children.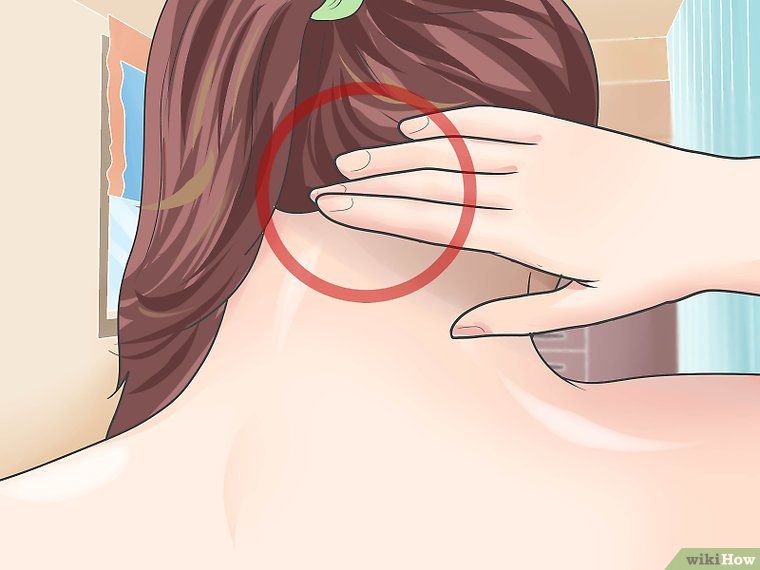 And we are like on a swing”: monologues of fathers with many children (not) subject to mobilization
And we are like on a swing”: monologues of fathers with many children (not) subject to mobilization
When will partial mobilization end: news around the SVO for October 14
Electric substation caught fire after shelling in Belgorod
a wave of "mining" in Chelyabinsk
Partial mobilization and strikes against Ukraine: main statements from Putin's press conference
Putin said that massive strikes against Ukraine are not necessary
All news
Share
Share
trimester) is a headache. Every fifth expectant mother suffers from this disease. The causes of pain can be so different that it is not always possible to immediately make a diagnosis. In addition, such a pattern was revealed: in the early stages of pregnancy, as a rule, blood pressure decreases, which may well provoke headaches and dizziness. Pregnant women often react sharply to weather changes - increased meteosensitivity can also be the cause of ailments.
A common cause of headache is migraine, in which attacks develop due to changes in the tone of the head vessels. It just so happened that in women this disease is much more common than in men, however, it should be noted that the frequency and severity of migraine decreases with the onset of pregnancy, especially in the second half, which is associated with changes in hormonal levels. Usually, with this ailment, it “aches in the temples”, a throbbing headache may be accompanied by nausea, vomiting. In the classic form of migraine, headaches are usually preceded by "flies" or flashes before the eyes.
Headache of moderate intensity is common, covering the head, squeezing it like a hoop, or pulling. It is usually associated with stress, physical or emotional strain. In some cases, it may be associated with muscle strain: in particular, the muscles of the neck and upper shoulder girdle during prolonged work in an uncomfortable position.
In addition to hypotension (low blood pressure), headache can also be caused by hypertension (high blood pressure), which is one of the symptoms of a serious pathology of pregnancy - late toxicosis (preeclampsia). In this case, edema and protein in the urine are often added to the pain.
In this case, edema and protein in the urine are often added to the pain.
The treatment of headache during pregnancy is very limited, as most drugs have a negative effect on the course of pregnancy, the formation of the fetus.
Lie in a comfortable position in a dark, ventilated room, in silence. Usually the pain goes away after a short sleep. Head massage can also help: make circular movements with your fingertips, while trying to relax as much as possible. Another simple but very effective way is washing your hair with warm water or a cold compress applied to the temporal or occipital region.
Decoctions of mint, rosehip, chamomile can be used to relieve headaches. They have a calming and analgesic effect. With reduced pressure, strong sweet tea helps. Before pregnancy, did a cup of coffee help with pain? Most likely, now this method will have to be abandoned: doctors do not recommend strong coffee to pregnant women.
Try to eat fractionally and in small portions. Feeling hungry can also trigger a headache. Snack not on chocolates and chips, but on dried fruits, cookies or an apple.
Feeling hungry can also trigger a headache. Snack not on chocolates and chips, but on dried fruits, cookies or an apple.
Do not forget that good sleep is very important for a pregnant woman. However, a significant increase in sleep time can also trigger a headache.
Try to walk more, breathe fresh air. If you work at a computer, remember to get up every 30 minutes, do some light exercise, or just walk down the hallway.
Be sure to remember: it is important to know and believe that you can and should cope with a headache without pills. This is very important not only for you, but also for the baby. Be healthy!
Galina KIM
- LIKE83
- LAUGHTER5
- SURPRISE6
- ANGER10
- SAD23
Select a fragment and press Ctrl+Enter
COMMENTS23
Read all comments
registration
What can I do if I log in?
COMMENT RULES
0 / 1400 This site is protected by reCAPTCHA and Google.