Allergic reaction baby milk allergy rash pictures
Allergic reaction in baby: Treatment and pictures
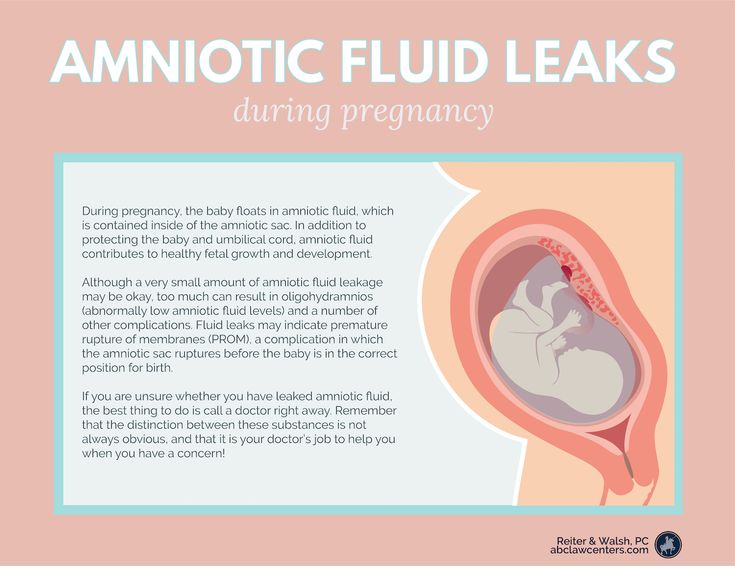
A baby can have an allergic reaction for a variety of reasons. An allergic reaction occurs when the body has an adverse response to a usually harmless substance, such as a soap or a specific food.
Babies have sensitive skin, which makes them more likely than adults to develop a rash. Even a slight irritation to a baby’s skin may be enough to trigger a rash.
Identifying the cause of the allergic reaction or sensitivity can help parents and caregivers to prevent and treat any future reactions.
Babies can have several different types of skin rash, which have a range of causes. Some allergic reactions can also lead to additional symptoms, such as nausea and vomiting.
Common types of allergic reactions in infants include the following:
Eczema
Share on PinterestIrritating fabrics, soaps, and heat can lead to eczema outbreaks in babies.Eczema is one of the most common skin conditions in babies. There are different types of eczema, but atopic eczema is one of the most likely to affect babies and small children.
An eczema rash may consist of tiny red bumps, or it may look like scaly, dry skin.
Doctors do not know why some people develop eczema while others do not, but it may be due to a combination of genetic and environmental factors.
Common triggers of eczema outbreaks in babies include irritating fabrics, soaps, and heat.
An eczema rash may look slightly different in older infants. According to the National Eczema Association, babies younger than 6 months tend to develop eczema-type rashes on the scalp, face, and forehead.
In babies aged between 6 months and 1 year, the rash often appears on the knees and elbows.
Papular urticaria
Papular urticaria is a localized allergic reaction to a bug bite. Bites from various insects, including mosquitoes, mites, and bedbugs, can cause the reaction.
Although it usually affects children aged 2–6 years, papular urticaria can also occur in infants.
Papular urticaria resembles small clusters of red bumps or bug bites. Some of the bumps may be fluid-filled. Papular urticaria can last for several days or even weeks.
Some of the bumps may be fluid-filled. Papular urticaria can last for several days or even weeks.
Hives
When the body is allergic to a substance, it releases a chemical called histamine that can lead to the development of hives and other allergy symptoms.
Hives are itchy, raised patches on the skin. They can range in size and shape but are usually pink or red with a thin red border.
Hives can develop anywhere on the body and often appear in clusters.
Share on PinterestA baby can develop hives as the result of a food allergy.
According to the American Academy of Allergy, Asthma & Immunology, about 6 percent of children aged 2 and under have food allergies.
Signs of a food allergy can include skin reactions and respiratory or intestinal symptoms, such as:
- hives
- itching
- coughing
- vomiting
- diarrhea
- blood in the stool
Occasionally, it is even possible for babies to have allergic reactions to foods before they start eating them.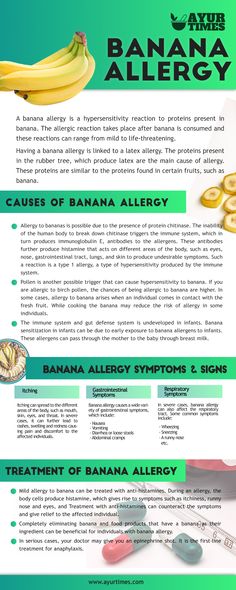 This is because they can develop allergies to the foods that the person who is breast-feeding them eats.
This is because they can develop allergies to the foods that the person who is breast-feeding them eats.
The foods that children are most likely to be allergic to are:
- milk and dairy products
- peanuts
- shellfish
Once they start eating solid foods, babies may show signs of additional allergies.
Doctors often recommend that parents and caregivers introduce new foods to a baby one at a time. This way, if an allergy does develop, it is easier to determine which food is responsible for the reaction.
Not all reactions in babies require treatment. For example, a mild rash is likely to fade within a few hours and may not trouble the baby in that time.
However, if the symptoms of a reaction are causing visible discomfort, treatment may be necessary.
The treatment can vary according to the type of rash or reaction. In general, the following treatments may help:
- Avoiding triggers: Soaps, detergents, and scented lotions can often irritate a baby’s skin, so it may be best to avoid using chemical cleaners and to choose hypoallergenic products instead.
- Washing with a fragrance-free cleanser: After using a mild, scent-free soap, pat the baby’s skin dry and avoid rubbing too hard, as this can irritate the skin.
- Applying a moisturizer: Using a hypoallergenic moisturizer after a baby’s bath can help to prevent dry skin. Moisturizers also provide a barrier to protect the skin from irritants.
- Using 1-percent hydrocortisone cream: Hydrocortisone cream can treat skin rashes relating to eczema or other allergic reactions. Although it is usually safe to use for infants for short periods, it is essential to speak to a doctor first.
- Considering scratch mitts: Scratch mitts prevent a baby from scratching a rash with their fingernails. Too much scratching can injure the skin and lead to an infection.
It is not possible to prevent all allergic reactions in babies, but there are steps that parents and caregivers can take to reduce the risk. These include:
These include:
- washing the baby’s clothes in hypoallergenic detergent
- using fragrance-free shampoo, lotions, and soap
- washing the baby’s bedding in hot water every week to reduce the chance of dust mites
- vacuuming frequently
- introducing new foods one at a time
If a baby has an allergic reaction after breast-feeding, it might be beneficial to keep a food diary to try to determine the underlying cause. Dairy is a very common culprit, especially before the infant reaches 1 year in age.
After identifying the allergen, it may help to avoid eating this food while breast-feeding. However, it is best to speak to a doctor before making changes to the diet.
Share on PinterestSeek medical advice if a rash worsens over time.
People can often treat allergic reactions in babies at home. However, in some cases, it is best to see a doctor.
If the rash spreads or worsens over time, a person should consult a doctor. It is also essential to seek medical advice if the skin shows signs of an infection, such as blistering, bleeding, or seeping fluid.
In some cases, a rash can signify another illness. If a rash appears alongside the symptoms below, people should consult a doctor:
- fever
- lethargy
- poor feeding
- coughing
- excessive crying
Babies who develop allergic reactions that include wheezing, swelling of the lips or tongue, or trouble breathing will require immediate medical attention. They may be having an anaphylactic reaction, which can be severe.
Allergic reactions and sensitivities are common in babies, in part because they have such sensitive skin.
In most cases, these reactions are mild, and parents or caregivers can treat them at home.
Identifying the allergen can help to prevent future reactions. Many babies will grow out of their allergies, but others will develop new allergies as they get older.
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP to discuss your concerns.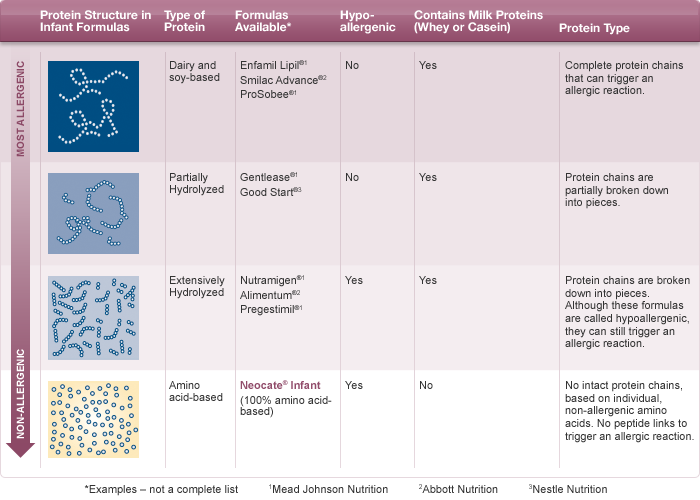
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it by the age of 5.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as a red itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction, or anaphylaxis, is a medical emergency – call 999 or go immediately to your local hospital A&E department.
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed every 6 to 12 months to see if they have grown out of their allergy.
Read more about cows' milk allergy.
Could it be lactose intolerance?
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance in children.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- When should I start giving my baby solids?
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 12 July 2019
Next review due: 12 July 2022
Allergy to cow's milk protein in children
Food allergy is a food-induced adverse (pathological) reaction based on immune mechanisms. In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
A distinction is made between cow's milk protein allergy and cow's milk protein intolerance. In the first case immune mechanisms are involved, in the second - the baby simply does not have enough enzymes to digest cow's milk protein (for example, lactase deficiency).
There are only 36 cow's milk protein allergens, but 4 of them most often cause food allergies.
Casein is 80% BCM, it is heat stable (does not break down when boiled) and is not a species-specific protein. This means that if you are allergic to it, you may be allergic to the milk of other animal species.
β - lactoglobulin has the highest allergenic activity, species-specific, not destroyed by boiling. This protein is not found in human milk.
α - lactalbumin is destroyed by boiling, species-specific.
Bovine serum albumin is not destroyed by boiling, if an allergy to this cow's milk protein is detected, the child may also react to beef and veal meat.
It should be noted that mainly children who are formula-fed formulas based on cow's milk protein suffer from allergy to cow's milk protein.
This type of allergy can also develop in children who are breastfed - if the diet of a nursing mother contains products containing cow's milk protein (milk, cheese, cottage cheese, sour cream, butter, fermented milk products), especially in large quantities.
What symptoms suggest that the baby may be allergic to CMP:
- Skin manifestations (dry skin, dry nummular rashes, skin itching).
- Gastrointestinal manifestations (bloating, regurgitation, vomiting, loose stools, possibly mucus and blood-streaked stools).
- Respiratory manifestations (itchy eyes, cough, nasal congestion and even urticaria and Quincke's edema).
 These symptoms are rare in toddlers, but still possible.
These symptoms are rare in toddlers, but still possible.
Diagnosis
I must say that if the first manifestations of a food allergy in a baby appeared after switching to artificial feeding with a "regular" adapted formula based on cow's milk, then this is a reason to suspect cow's milk proteins as an allergen.
The next thing is correct history taking : the doctor will definitely find out if anyone in your family suffers from allergic diseases (bronchial asthma, allergic rhinitis, atopic dermatitis, hay fever). If the family has these diseases, the risk of developing allergies in the baby increases.
At the discretion of the doctor, it is possible to take blood from a child for the presence of immunoglobulin E (IgE) antibodies to cow's milk proteins, which were mentioned above. In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy. Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
And the simplest, most important and affordable method is the diagnostic diet with the exclusion of products from the child's diet (or from the mother's diet during breastfeeding) containing CMP. The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
If the child's condition improves, you may need challenge test . This means the introduction of dairy products into the child's diet again. And if the manifestations of allergies return, this will prove an allergy to BCM. This test is carried out under strict medical supervision.
In children who are fed exclusively with breast milk, it is necessary to exclude from the diet of mothers products containing CMP.
There are 3 types of mixtures:
- based on the hydrolysis of whey proteins;
- based on the hydrolysis of the casein fraction;
- based on amino acids.
Allergy is possible for the first two options, the reaction is very unlikely for the third option.
If the baby is bottle-fed, then he must be transferred to amino acid blend or highly hydrolyzed blend. Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Usually, allergists first transfer children to mixtures based on complete hydrolysis of BCM or casein, if there is no proper effect within 2-3 weeks, it is recommended to transfer the baby to an amino acid mixture.
Perhaps, if the child has severe manifestations of food allergies, the doctor will advise you to immediately transfer the baby to an amino acid mixture. By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
Amino acid mixtures are more easily tolerated by children with various forms of food allergies, as they do not have the bitter taste characteristic of mixtures with a high degree of protein hydrolysis.
Amino acid mixtures can be used both for the short term diagnosis of CMP allergy and as a dietary base for long term use in children with food allergies.
Diet duration — at least 6 months . Then the issue of transferring the baby to a hypoallergenic mixture is decided. In case of recurrence of symptoms, the introduction of dairy products is postponed for another 6 months.
The prognosis for CMP allergy in infants and young children with the correct management of patients is favorable.
Approximately 50% of children by the age of 1 year can be introduced into the diet of foods that include CMP. More than 75% of children by age 3 or older 90% of children by the age of 6 do not show allergic reactions to CMP.
More than 75% of children by age 3 or older 90% of children by the age of 6 do not show allergic reactions to CMP.
Food allergies in children - symptoms, treatments, diet or its individual components. What are its causes, what are the risk factors, and what food to choose in case of an allergic reaction - read in this material.
Food allergy symptoms
The causes of food intolerances are due to the fact that the immune system "incorrectly" recognizes them as potentially dangerous, and produces protective antibodies in excess. Excessively violent reaction leads to the fact that the child develops an allergy to certain types of food. 1.3
Symptoms of food allergy in children are different. But most often, food allergies manifest themselves on the part of the skin - itching, a feeling of tightness and dryness. Local swelling may occur on the skin, a rash (urticaria), redness, blisters may appear. In second place in terms of frequency of manifestation - reactions from the respiratory system. Runny nose, nasal congestion, sore throat, cough of varying intensity. Also, reactions from the organs of the gastrointestinal tract can indicate food allergies. A very young child begins to be disturbed by colic, dyspepsia, stool disorders from diarrhea to constipation. Older children complain of nausea, vomiting, abdominal pain, a feeling of scratching in the throat, behind the sternum.
Runny nose, nasal congestion, sore throat, cough of varying intensity. Also, reactions from the organs of the gastrointestinal tract can indicate food allergies. A very young child begins to be disturbed by colic, dyspepsia, stool disorders from diarrhea to constipation. Older children complain of nausea, vomiting, abdominal pain, a feeling of scratching in the throat, behind the sternum.
Do not forget about the general symptoms of food allergies: the child becomes lethargic, capricious, sleeps poorly, does worse in school (or psycho-emotional development), is prone to daytime sleepiness. 2.3
Causes of food allergies
Newborns and young children, if predisposed, may suffer from allergies due to their physiological characteristics. The fact is that a child is born with an immature gastrointestinal tract, the intestinal walls are permeable to many substances, the enzyme system is still imperfect. Therefore, it is difficult for the body to cope with the digestion of proteins. The body seems to be in a state of constant "combat readiness" and the ingestion of even a small amount of allergens leads to a response from the immune system and the development of a violent allergic reaction. 1.2
The body seems to be in a state of constant "combat readiness" and the ingestion of even a small amount of allergens leads to a response from the immune system and the development of a violent allergic reaction. 1.2
In older children, many internal and external conditions become risk factors. For example, heredity - after all, if one of the child's parents suffered from an allergic disease, then with a high degree of probability the child will also be given a tendency to it. Unfavorable environmental factors influence - polluted atmosphere, car exhausts, lack of green plants in cities. Very often, a violation of the immune system in the form of an allergic reaction occurs in children with a labile, mobile psyche, with sharp transitions from friendliness and calmness to crying and back. Finally, bad habits, both in children and mothers during pregnancy, become an important factor. This is incorrectly introduced complementary foods and early introduction of potentially allergenic foods into the child's diet: citrus fruits, nuts, chocolate, berries, honey, and, of course, the habit of children to eat only something tasty (usually unhealthy; chocolate, carbonated drinks, fast food ) 2,3,4
List of products that provoke allergies
Due to the extreme individuality of the immune system, it is almost impossible to predict its reaction. However, there is a rough list of foods classified into groups depending on their allergenicity - that is, the ability to cause a sharp reaction from the immune system and allergy symptoms. It is important to remember that it is not at all necessary that any product from the first column will cause a reaction. Like any low allergenic product, in some cases, it can cause an overreaction to it. 2,3,4
However, there is a rough list of foods classified into groups depending on their allergenicity - that is, the ability to cause a sharp reaction from the immune system and allergy symptoms. It is important to remember that it is not at all necessary that any product from the first column will cause a reaction. Like any low allergenic product, in some cases, it can cause an overreaction to it. 2,3,4
Examples of the most typical exoallergens
| Highly allergenic products | Foods of average allergenicity | Low Allergy Products | |
| all citrus fruits, strawberries, strawberries, raspberries, blackberries, pineapples. | peaches, cranberries, lingonberries, cherries, blueberries, black currants. | pears, gooseberries, dried apricots, plums, white currants, apples and pears. | |
carrots, tomatoes, bell peppers, radishes. | potatoes, beets, peppers, peas, corn. | broccoli, green peas, zucchini, squash, white and cauliflower, cucumbers, pumpkin. | |
| eggs, sausages and sausages, chicken, sea fish. | beef, rabbit, pork. | lamb. | |
| whole cow's milk, cheeses, yoghurts with additives. | fermented milk products. | ||
| wheat, rye. | buckwheat, oats, rice, peas, beans. | barley, millet. | |
| coffee, cocoa, chocolate, nuts, honey. | xylitol, fructose | ||
| mushrooms, carbonated drinks, packaged juices. | vegetable oil. |
Diagnosis established
The diagnosis of this allergy, as well as the search for the causes that caused it, requires a careful and serious approach on the part of parents. The younger the child, the easier it is to find foods that cause illness. For this, two conditions must be met.
For this, two conditions must be met.
The first thing is to put a child or mother on a hypoallergenic diet if she is breastfeeding - a detailed nutrition plan will be helped by an allergist together with a pediatrician. Please note that during an exacerbation, the diet will be extremely strict, the so-called elimination diet - aimed at removing the allergen and reaction products to it with the complete elimination of potential and cross allergens. The duration of such a diet is determined by the doctor. When the exacerbation fades, the diet gradually expands due to safe foods. 3.4
And the second thing is to start keeping a special food diary in which to record everything that was eaten and drunk by the child during the day, as well as what was cooked and how. At the first sign of an allergic reaction, suspicious foods should be eliminated one at a time (or from the mother's diet if the baby is breastfed). After elimination, within a few days, it is worth observing the reaction, if the manifestations of allergies decrease, then the product is really not suitable for the child - it should be avoided. If the child is very small, then the diary is kept according to the opposite principle: all foods that are introduced as complementary foods are recorded in it. The name of the product, the quantity, the time of eating and the reactions of the body are recorded over the next few days (the attending physician will determine the specific timing of observation). Next, the doctor will need to check and confirm the preliminary diagnosis by conducting special tests and analyzes.
If the child is very small, then the diary is kept according to the opposite principle: all foods that are introduced as complementary foods are recorded in it. The name of the product, the quantity, the time of eating and the reactions of the body are recorded over the next few days (the attending physician will determine the specific timing of observation). Next, the doctor will need to check and confirm the preliminary diagnosis by conducting special tests and analyzes.
Food allergy emergency
The first step is to evaluate the severity of the food allergy.
For any symptoms, the first step is to avoid contact with a specific familiar allergen or any suspicious food or drink.
If the symptoms of allergy are mild - itching, redness of the skin, then you can give the child an antihistamine, which was previously recommended by the doctor for such cases. In addition, you must also call the local pediatrician and carefully monitor the condition of the child.