How to help child with expressive language disorder
Strategies to support expressive language
Keep up to date with SEND: Get new post alerts!
Email Address
special needs, speech & language
By Helen Coleman SpeechBlogUK
In my most recent post on SNJ, I talked about how difficult it can sometimes be to identify when a child is having difficulty understanding and I offered some general principles for helping with comprehension, at home or in a classroom.
A child who is struggling with expressive language is not always so difficult to spot (though it can get harder as they get older and becomes better at hiding the problem!) However, just because it’s easier to see that a child is struggling to get their message across, it doesn’t mean that it’s always obvious how best to support them. How can we involve the child fully in conversation, without putting too much pressure on them? Here are a few ideas:-
Check that the child understands
Wait a minute – I just said that I was talking about expressive language! That’s true, but the two are often linked. A child who has difficulty finding the words they want to say, or structuring sentences, can sometimes struggle with understanding vocabulary and grammar as well. Make sure they understand what you’re talking about.
Take time
We all feel more pressured if we need to say something quickly. And if you’re anything like me, the time you need to convey something under pressure, is the time when you find that your mind goes blank, and you just can’t find a succinct way to explain what you mean. I’m sure I’m not the only one who has sat in an exam hall only to find myself struggling to answer a question that I know I could have answered the day before. Take time yourself over what you’re saying and pause lots. When possible, let the child know that there is no rush. You can do this either by directly saying it or just by letting your own voice and body language give the message. We all tend to imitate back the way that someone talks to us, so think about slowing your own rate of speech down just slightly to make the child feel less pressured.
When possible, let the child know that there is no rush. You can do this either by directly saying it or just by letting your own voice and body language give the message. We all tend to imitate back the way that someone talks to us, so think about slowing your own rate of speech down just slightly to make the child feel less pressured.
Comment, don’t question
This is a trap I still find myself falling into, as it’s so easily done. You really want to encourage a child to talk so you ask them questions: “What did you do?” “What’s this?”, “Where are you going?”…. That’s fine up to a point, but it can become a bit like an interview rather than a conversation and again, the child can feel quite under pressure to speak. This in turn can make a lot of children clam up. After all, who wants to be constantly made to do something they find difficult?! Often, a better way is just to comment on what’s happening instead. When a child is playing freely, give a simple commentary on what they’re doing eg “the train’s going over the bridge….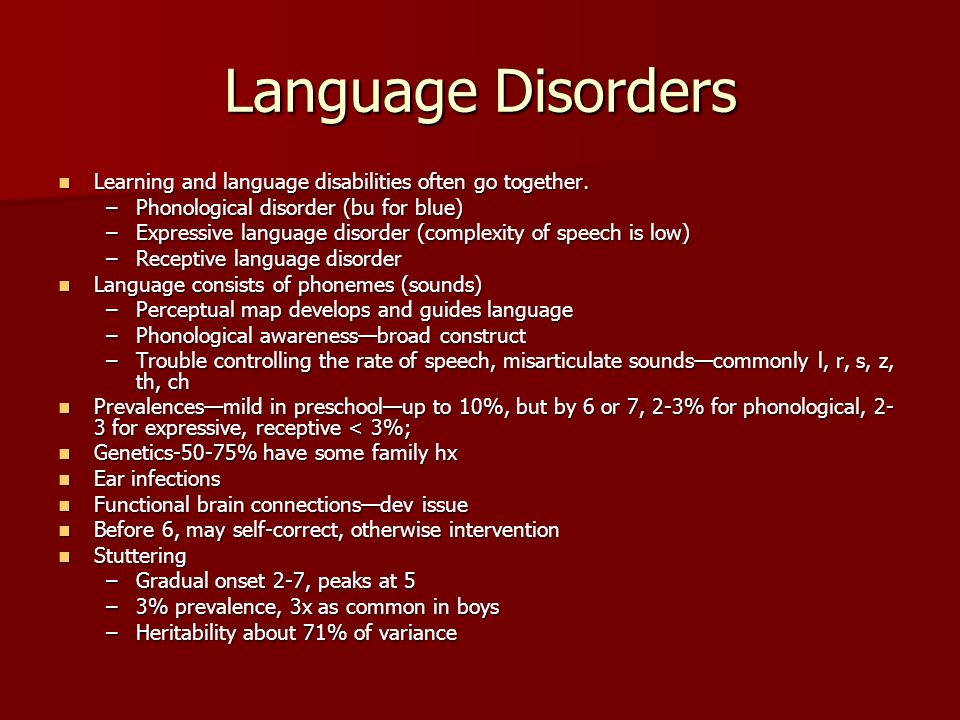 Choo choo…. Oh no, crash!” This works because you’re giving the child the words and phrases they might want to use in a far less pressured way as well as talking about what they’re interested in. Leave lots of pauses too and you may find the child soon starts to fill them.
Choo choo…. Oh no, crash!” This works because you’re giving the child the words and phrases they might want to use in a far less pressured way as well as talking about what they’re interested in. Leave lots of pauses too and you may find the child soon starts to fill them.
Advertisements
Model
This is one of those nice speech therapy words that I’m not sure make a lot of sense to other people sometimes. Certainly when I asked my husband to proof-read something for me that talked about modelling, he wondered why we were building models! What I mean is show your child how to say things. It’s usually best not to keep correcting them or telling them that what they have said is wrong, but (assuming that you understand what they meant) say it back to them with the errors corrected so that they can hear a good example. So if a child says “I goed to the park”, I might say “yes, you went to the park”.
Expand/add
This goes nicely with the “modelling”! When you’re saying a sentence back for a child to hear, add another word or two to what they said. It’s important not to go overboard with this – the idea is just to show them language one stage further on than what they are currently able to say. So, if a child says “sit on chair” I probably wouldn’t respond with “yes, that big teddy looks really comfy sitting on that soft chair”, but I might say “yes, teddy’s sitting on a chair”.
It’s important not to go overboard with this – the idea is just to show them language one stage further on than what they are currently able to say. So, if a child says “sit on chair” I probably wouldn’t respond with “yes, that big teddy looks really comfy sitting on that soft chair”, but I might say “yes, teddy’s sitting on a chair”.
Offer choices
Often when faced with a question, a child with a language difficulty knows the answer but can’t think of the words they want to say to respond. Offering a choice of two things reduces the options and helps to cue them in to the vocabulary they want. For example, it’s easier to answer “do you prefer ice-cream or chocolate?” than “what’s your favourite food?” (unless you’re me that is – I love them both!...)
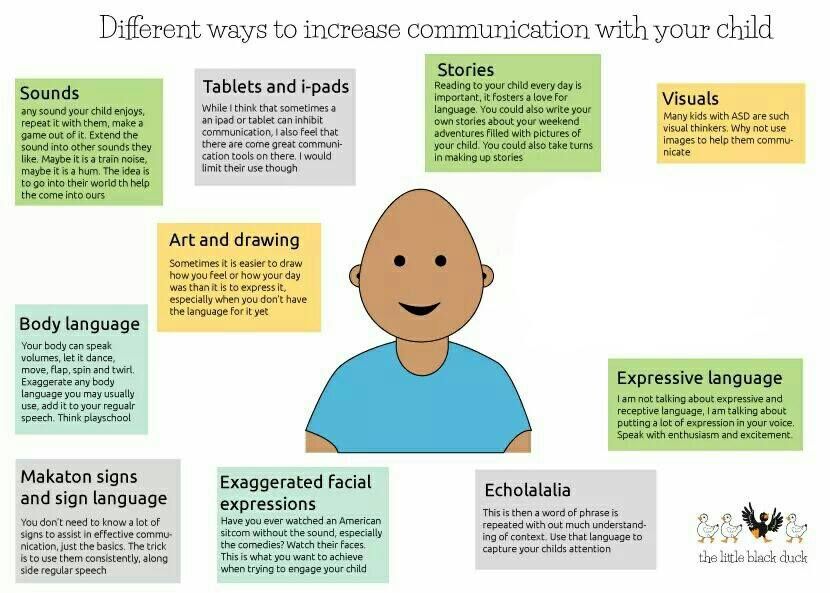
Use other ways to communicate as well as speech
Children who struggle to communicate verbally can often be really helped by using other ways to communicate as well as speech. This may include signing, gestures, pictures, communication books or other devices. Whatever method you are trying to encourage a child to use to supplement speech, the best way to encourage it is to use it yourself.
Whatever method you are trying to encourage a child to use to supplement speech, the best way to encourage it is to use it yourself.
Use context
Whatever language a child needs to learn, the best way to learn it is in context. If you’re teaching past tense verbs the best way to teach them is to talk about what has just happened. If you’re teaching idioms, the best way to teach them is to use them in an appropriate context and then explain what they mean. If you’re teaching new vocabulary, use the words as often as you can yourself in context. We all need to hear a new word lots of times before we remember it. This is even more true for children with speech and language difficulties. Use a new word, then use it again. Refer back to it later that day. Try to use it again a few days later. The more a child hears the word in context the more likely it is to be stored well in their brain and found more easily when they want to use it.
- About
- Latest Posts
Helen Coleman SpeechBlogUK
Speech & Language Therapist at Speech Blog UK
Helen is a speech and language therapist with more than 10 years' experience of working with children, families and schools. She is a regular columnist for Special Needs Jungle and also blogs jointly with Elizabeth Gunner at Speechbloguk.
She is a regular columnist for Special Needs Jungle and also blogs jointly with Elizabeth Gunner at Speechbloguk.
Latest posts by Helen Coleman SpeechBlogUK (see all)
SNJ is run by volunteer parents. Everything on SNJ is free to use, but if you like what we do, and you want us to keep doing it, a small donation towards running costs would be really appreciated.
Search SNJ
Search for:Recently on SNJ
- Is NHS England breaking a promise to roll out eye care for disabled children in all special schools?
October 14, 2022
- “Global wellbeing” is out of reach while children and vulnerable adults are routinely restrained in places of “safety”
October 10, 2022
- Parent-blaming to avoid professional accountability is a human rights issue
October 5, 2022
- 10 top tips for moving local authority with an EHCP
September 30, 2022
- New SEND Minister, Kelly Tolhurst: many responsibilities but none so important as disabled children’s futures
September 28, 2022
- Gendered misperceptions: Research shows girls with ADHD miss out on school support
September 22, 2022
- How will the government-funded RISE partnership improve local areas’ SEND provision?
September 13, 2022
- I’m a Dad with ASD and ADHD.
 Here’s why I’ll never give up fighting for my neurodiverse children’s educational rights
Here’s why I’ll never give up fighting for my neurodiverse children’s educational rightsSeptember 8, 2022
- What is “special educational provision” in law? How a case of electromagnetic hypersensitivity may help future appeals
September 6, 2022
- SNJ’s response to the EHCP Annual Review Timescales consultation
September 2, 2022
- An Employment Passport to young people with additional needs into paid work
August 23, 2022
- What influences the emotional wellbeing of young people with severe dyslexic difficulties?
August 17, 2022
- How The Wave Project makes surfing possible for disabled children
August 11, 2022
- Top tips for introducing a School Dog to help your students
August 5, 2022
- Helping Businesses Become More Inclusive with SEND Session Guides
August 1, 2022
- Why the Down Syndrome Act ‘call for evidence’ is also relevant for people with other genetic conditions
July 29, 2022
- Special Needs Jungle’s #SENDReview Consultation response
July 26, 2022
- Falling Through the Cracks: How children with SEND struggle to access early years education
July 20, 2022
- Using a different lens for neurodivergent children: Don’t treat them as younger, give them the tools to achieve
July 17, 2022
- #SENDReview: National standards plans are an assault on the rights and entitlements of children and young people with SEND
July 15, 2022
Help SNJ keep going!
Resource Listings
Reach North West
Expressive Language Disorder in Children
Expressive language disorder makes it hard for kids to express their thoughts and ideas. Kids understand what other people are saying, but they have trouble using language when they speak. That can have a big impact on their ability to make friends, socialize, and interact with other people.
Kids understand what other people are saying, but they have trouble using language when they speak. That can have a big impact on their ability to make friends, socialize, and interact with other people.
It can also affect them at school. Expressive language disorder can make it harder for kids to join classroom discussions or even write what they know. But with the right support, they can improve skills and build self-esteem.
You may not know yet if your child has this lifelong language disorder. But the more you understand the challenges, the better you can support your child.
Expressive language disorder is developmental, so it starts in childhood. The first thing most parents notice is that their child is late to talk or still speaks in single words as a toddler. But signs continue throughout childhood, and you may not recognize them at first.
If your child often uses the wrong word or says sentences that don’t make sense, you might suspect a problem with language. But some signs of expressive language disorder aren’t that clear. You may see behaviors that don’t seem directly related to language, or that could be a sign of many things.
But some signs of expressive language disorder aren’t that clear. You may see behaviors that don’t seem directly related to language, or that could be a sign of many things.
Here are some common signs of expressive language disorder in kids.
- Starting to talk later than most kids
- Frequently saying “um” and “huh”
- Having a limited vocabulary compared to kids the same age
- Using short phrases or sentences
- Not talking much, but understanding what’s said
- Having trouble finding the right words
- Using certain phrases over and over
- Avoiding social situations
- Not making or joining conversations
- Seeming withdrawn or not interested
It’s frustrating to not be able to communicate what you’re thinking. That’s why some kids with expressive language disorder avoid talking altogether. This can have a big impact on self-esteem, which might be why some kids withdraw.
Learn more about the signs of expressive language disorder.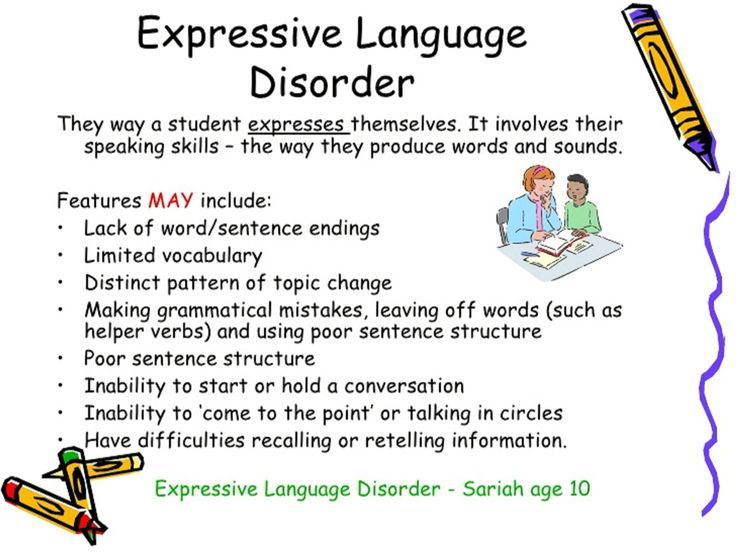
Finding out if your child has expressive language disorder
The people who diagnose expressive language disorder are speech-language pathologists (SLPs). They’re also known as speech-language therapists.
Your child can get a language evaluation for free at school. It’s often done as part of a full evaluation that looks at a wide range of learning skills.
Many kids who struggle with using language also have trouble understanding it. The combination is called mixed expressive-receptive language disorder. (Learn about receptive language disorder in children.)
Some SLPs work outside of school and do private language evaluations. Your child’s doctor may be able to give you a referral. These evaluations aren’t free. But colleges that train SLPs sometimes offer low-cost or free evaluations.
In the evaluation, the SLP will try strategies that might help your child build skills. The specialist may also interview you to get a better idea of what your child’s challenges look like at home.
How professionals can help with expressive language disorder
The main treatment for language disorders is speech-language therapy. The earlier kids start, the better. Kids get therapy at school as part of a special education plan called an IEP.
SLPs at schools work with kids one-on-one or in a small group of kids with similar challenges. They use strategies and activities that meet kids’ needs and interests. Kids with language challenges can also benefit from social skills groups.
Find out how speech-language therapy works.
How you can help with expressive language disorder
There are many fun ways you can help your child work on communication and conversation skills. You can read picture books together and name objects. Or name objects as you’re driving or walking.
Talk about characters in books or on TV and the plots. Ask your child to explain what happened in a movie you just watched. You can keep it simple—"What were the three most exciting parts?"
Role-playing is another great way to build conversation skills.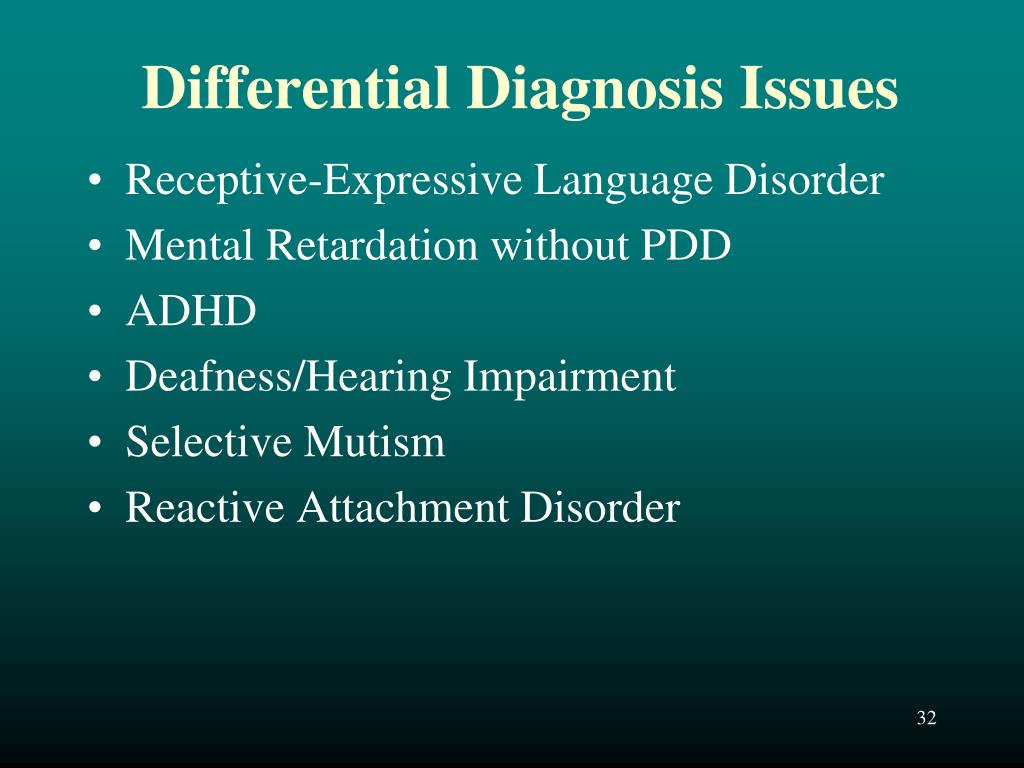 Act out a situation and switch parts midway. Or have your child play a news reporter doing an interview or a sportscaster describing a game.
Act out a situation and switch parts midway. Or have your child play a news reporter doing an interview or a sportscaster describing a game.
If your child says something that doesn’t make sense, or uses the wrong word, you can playfully point it out and ask your child to say it a different way.
It’s important to help your child improve language skills. But it’s just as important to help your child build self-esteem.
Struggling to get their thoughts out can make kids feel frustrated and ashamed. And even though it’s not a problem with intelligence, trouble using language can make them feel like they’re not smart.
Tell your child that everyone struggles with something, and that’s OK. Explain that with work, language skills can improve, and that you’ll be there to help. And be sure to celebrate successes large and small.
Download growth mindset worksheets to help your child stay motivated.
Related topics
Talking and understanding
Root causes
Speech delay | 1DMC
Medical examination in 1 month
Additional tests In order to undergo additional types of diagnostics, you need to get a referral…
Psychiatry
Vaccination
Orthopedics
general tips for preparing for an endoscopic examination depend on.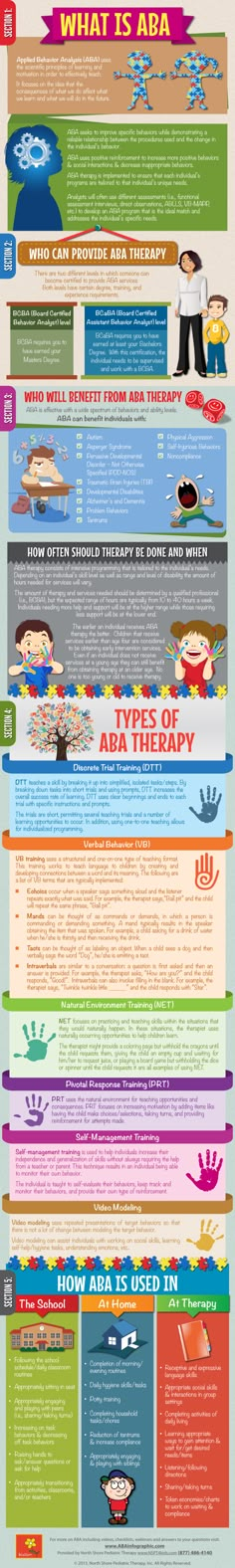 ..
..
Neurology
If you find any abnormalities, do not panic. However, put off going to a pediatric neurologist… Newborn jaundice - yellowish coloration of the whites of the eyes and skin ...
X-ray
Hematology
Stuttering: causes and forms
Stuttering in children is a speech disorder, a characteristic feature of which is frequent repetition or stretching ...
General Speech Underdevelopment
General Speech Underdevelopment (OHP) - disorders related to the formation of speech in children. This speech underdevelopment…
Voice disorder
Voice disorder is a group of speech disorders, manifested in complete or partial absence of phonation,…
Speech therapy
A speech therapist for children is a specialist who corrects speech disorders caused by both physical and…
Alalia
Alalia in children is a speech disorder characterized by a lack of development of speech skills (or…
Bradilalia
Bradilalia is a pathology of speech, which manifests itself in the form of a violation of the tempo and rhythm of speech. A person with such a speech…
A person with such a speech…
Dysarthria
Dysarthria is a pathology of speech in which there is an incorrect (distorted or difficult) pronunciation…
Dyslalia
Dyslalia is a violation of sound pronunciation in children with normal hearing and preserved innervation of the articulatory…
3 Rhinolalia is a speech disorder, manifested by a pronounced distortion of speech and incorrect pronunciation of individual ...
Laser treatment of skin pathologies
Your child's health should be entrusted to professionals. If you experience the first symptoms, contact…
Comprehensive examination of multifactorial diseases
Multifactorial diseases are diseases caused by different factors that require consultation…
Children’s cosmetology
Halotherapy
traditional therapeutic…
Issue of certificates and conclusions
In various situations, children need to issue medical certificates. First Children's Medical…
First Children's Medical…
Pulmonology
Obstructive syndrome in children You need to understand that without qualified and proper treatment of bronchitis ...
Therapeutic exercise
Physical activity is one of the important conditions for human life and development. It is a biological irritant…
Surgery
Pediatric Surgeon Choice The choice of a qualified doctor is important in pediatric surgery. Medical…
Laboratory
We offer a full range of traditional methods of general clinical and biochemical analysis. Laboratory…
Day hospital
On a day hospital basis in our Center we provide all types of infusion therapy, complex…
Annual follow-up program
Children's health - parents' peace of mind! Indeed, when children grow up healthy and strong, in a family…
Functional diagnostics
All equipment in the functional diagnostics room of our Center is digital (that is, working…
Physiotherapy
Physiotherapy is administered in courses. The duration of the course of treatment is 5-7 for some diseases, ... The development of many eye diseases can be prevented and stopped...
The duration of the course of treatment is 5-7 for some diseases, ... The development of many eye diseases can be prevented and stopped...
Otorhinolaryngology
Treatment of ENT diseases ENT of the First Children's Medical Center deals with diagnostics and treatment…
Nephrology
Dermatology
Treatment of skin diseases The skin is the most visible organ of the human body. Experienced and attentive…
Gynecology
It is important to help patients and their parents in a timely manner to identify and adequately deal with female problems…
Anesthesiology
Pediatric anesthesiologist in Saratov A pediatric anesthesiologist talks to the parents, as well as to the child himself…
Endocrinology
All this allows for timely and adequate treatment. If the child complies with the necessary ...
If the child complies with the necessary ...
Cardiology
After collecting an anamnesis and carrying out diagnostic measures, the pediatric cardiologist of the Center will draw up an individual…
Urology
If a child develops pulling pains in the lower abdomen, there is no need to self-medicate, let alone hope that…
Children Gastroenterology
less protected from diseases of the gastrointestinal tract than adults. Unbalanced…Pediatrics
Fast trace icon translate If your child often gets sick with acute respiratory ...
Allergology-immunology
Fast trace icon translate The main task of specialists in allergology and immunology is…
Speech developmental delays in children: causes, diagnosis and treatment
For citation.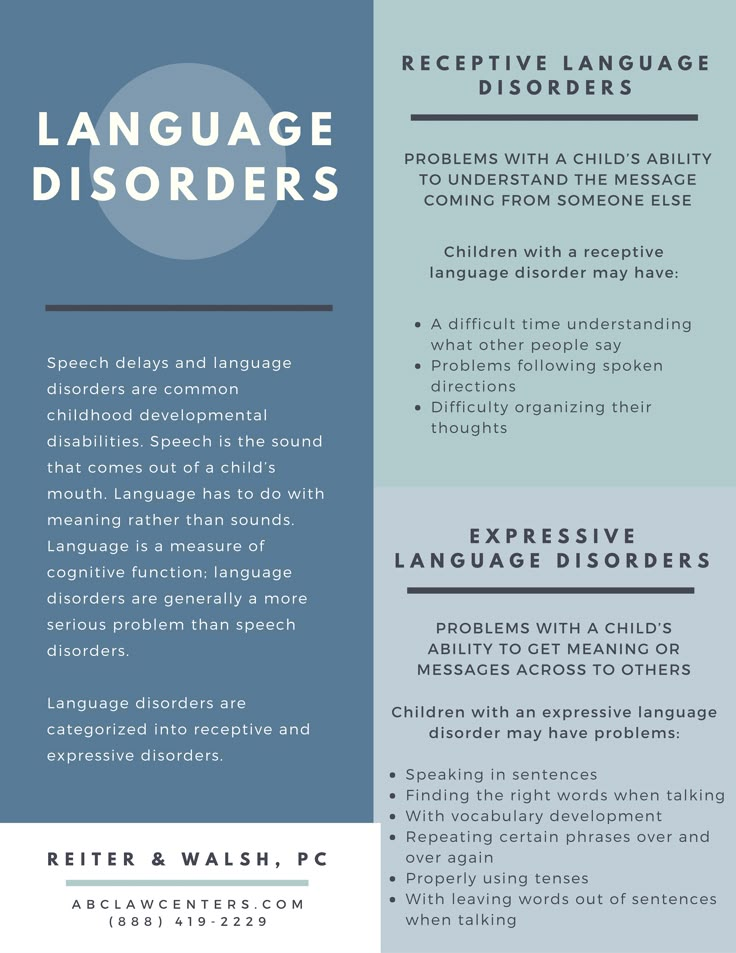 Zavadenko N.N., Suvorinova N.Yu. Delays in speech development in children: causes, diagnosis and treatment // RMJ. 2016. No. 6. S. 362–366.
Zavadenko N.N., Suvorinova N.Yu. Delays in speech development in children: causes, diagnosis and treatment // RMJ. 2016. No. 6. S. 362–366.
Delays in speech development are usually understood as a lag in the formation of speech from age standards in children under the age of 3–4 years. Meanwhile, this formulation implies a wide range of speech development disorders that have different causes.
The decisive period for the formation of speech is the period from the first year of life to 3-5 years. At this time, the brain and its functions are intensively developing. Any violations in the development of speech are a reason for an urgent appeal to specialists - a doctor (pediatrician, pediatric neurologist, ENT doctor, child psychiatrist), speech therapist, psychologist. This is all the more important because it is in the first years of life that deviations in the development of brain functions, including speech, are best corrected.
Speech and its functions. Speech is a special and most perfect form of communication, inherent only to man. In the process of verbal communication (communication), people exchange thoughts and interact with each other. Speech is an important means of communication between the child and the outside world. The communicative function of speech contributes to the development of communication skills with peers, develops the possibility of playing together, which is invaluable for the formation of adequate behavior, emotional-volitional sphere and personality of the child. The cognitive function of speech is closely related to the communicative one. The regulatory function of speech is formed already in the early stages of a child's development. However, the word of an adult becomes a true regulator of the activity and behavior of the child only by the age of 4–5, when the semantic side of speech is already significantly developed in the child. The formation of the regulatory function of speech is closely connected with the development of inner speech, purposeful behavior, and the ability for programmed intellectual activity.
Speech is a special and most perfect form of communication, inherent only to man. In the process of verbal communication (communication), people exchange thoughts and interact with each other. Speech is an important means of communication between the child and the outside world. The communicative function of speech contributes to the development of communication skills with peers, develops the possibility of playing together, which is invaluable for the formation of adequate behavior, emotional-volitional sphere and personality of the child. The cognitive function of speech is closely related to the communicative one. The regulatory function of speech is formed already in the early stages of a child's development. However, the word of an adult becomes a true regulator of the activity and behavior of the child only by the age of 4–5, when the semantic side of speech is already significantly developed in the child. The formation of the regulatory function of speech is closely connected with the development of inner speech, purposeful behavior, and the ability for programmed intellectual activity.
Disorders in the development of speech affect the general formation of the personality of children, their intellectual growth and behavior, make it difficult to learn and communicate with others [1, 2].
Forms of speech development disorders. Specific developmental speech disorders include those disorders in which normal speech development is impaired in the early stages. According to the ICD-10 classification [3], these include developmental disorders of expressive speech (F80.1) and receptive speech (F80.2). At the same time, violations appear without a previous period of normal development of speech. Specific disorders of speech development are the most widespread disorders of neuropsychic development; their frequency in the child population is 5–10% [1, 4].
Alalia (according to modern international classifications - "dysphasia" or "dysphasia of development") - systemic underdevelopment of speech, it is based on an insufficient level of development of the speech centers of the cerebral cortex, which can be congenital or acquired in the early stages of ontogenesis, in preverbal period. At the same time, the ability to speak first of all suffers in children, expressive speech is characterized by significant deviations, while speech understanding can vary, but, by definition, is much better developed [2]. The most common variants (expressive and mixed expressive-receptive disorders) are manifested by a significant delay in the development of expressive speech compared to the development of understanding. Due to difficulties in organizing speech movements and their coordination, independent speech does not develop for a long time or remains at the level of individual sounds and words. Speech is slow, poor, vocabulary is limited. There are many reservations (paraphasias), permutations, perseverations in speech. Growing up, children understand these mistakes, try to correct them.
At the same time, the ability to speak first of all suffers in children, expressive speech is characterized by significant deviations, while speech understanding can vary, but, by definition, is much better developed [2]. The most common variants (expressive and mixed expressive-receptive disorders) are manifested by a significant delay in the development of expressive speech compared to the development of understanding. Due to difficulties in organizing speech movements and their coordination, independent speech does not develop for a long time or remains at the level of individual sounds and words. Speech is slow, poor, vocabulary is limited. There are many reservations (paraphasias), permutations, perseverations in speech. Growing up, children understand these mistakes, try to correct them.
In modern literature, both terms - "specific developmental speech disorders" and "developmental dysphasia" - are used, while they refer to the same group of pediatric patients. But “developmental dysphasia” is considered a more accurate formulation of the diagnosis, since this term reflects both the neurological and evolutionary-age aspects of this disorder [2, 5].
Complete or partial loss of speech due to local lesions of the speech areas of the cerebral cortex is called aphasia. Aphasia is the disintegration of already formed speech functions, therefore such a diagnosis is made only after 3-4 years. With aphasia, there is a complete or partial loss of the ability to speak or understand someone else's speech.
Dysarthria - a violation of the sound-producing side of speech as a result of a violation of the innervation of the speech muscles. Depending on the localization of the lesion in the central nervous system (CNS), several variants of dysarthria are distinguished: pseudobulbar, bulbar, subcortical, cerebellar.
Depending on the leading disorders underlying speech disorders in children, L.O. Badalyan [6] proposed the following clinical classification.
I. Speech disorders associated with organic damage to the central nervous system. Depending on the level of damage, they are divided into the following forms:
1. Aphasia - the disintegration of all components of speech as a result of damage to the cortical speech zones.
Aphasia - the disintegration of all components of speech as a result of damage to the cortical speech zones.
2. Alalia - systemic underdevelopment of speech as a result of damage to the cortical speech zones in the pre-speech period.
3. Dysarthria - a violation of the sound-producing side of speech as a result of a violation of the innervation of the speech muscles. Depending on the localization of the lesion, several variants of dysarthria are distinguished.
II. Speech disorders associated with functional changes in the central nervous system (stuttering, mutism and deafness).
III. Speech disorders associated with defects in the structure of the articulatory apparatus (mechanical dyslalia, rhinolalia).
IV. Delays in speech development of various origins (with prematurity, severe diseases of internal organs, pedagogical neglect, etc.).
In the domestic psychological and pedagogical classification [7], alalia (dysphasia), along with other clinical forms of delayed speech development in children, is considered from the standpoint of general speech underdevelopment (ONR). This classification is built on the principle of "from particular to general". OHP is heterogeneous in terms of developmental mechanisms and can be observed in various forms of oral speech disorders (alalia, dysarthria, etc.). As common features, a late onset of speech development, a poor vocabulary, agrammatisms, pronunciation defects, and phoneme formation defects are noted [7]. Underdevelopment can be expressed in varying degrees: from the absence of speech or its babbling state to expanded speech, but with elements of phonetic and lexical and grammatical underdevelopment.
This classification is built on the principle of "from particular to general". OHP is heterogeneous in terms of developmental mechanisms and can be observed in various forms of oral speech disorders (alalia, dysarthria, etc.). As common features, a late onset of speech development, a poor vocabulary, agrammatisms, pronunciation defects, and phoneme formation defects are noted [7]. Underdevelopment can be expressed in varying degrees: from the absence of speech or its babbling state to expanded speech, but with elements of phonetic and lexical and grammatical underdevelopment.
The three levels of OHP are distinguished as follows: 1st - the absence of commonly used speech ("speechless children"), 2nd - the beginnings of common speech and 3rd - extended speech with elements of underdevelopment throughout the speech system. The development of ideas about OHP is focused on the creation of correction methods for groups of children with similar manifestations of various forms of speech disorders. The concept of OHP reflects the close interrelationship of all components of speech in the course of its abnormal development, but at the same time it emphasizes the possibility of overcoming this lag, the transition to qualitatively higher levels of speech development.
The concept of OHP reflects the close interrelationship of all components of speech in the course of its abnormal development, but at the same time it emphasizes the possibility of overcoming this lag, the transition to qualitatively higher levels of speech development.
However, the primary mechanisms of ONR cannot be elucidated without a neurological examination, one of the important tasks of which is to determine the location of the lesion in the nervous system, i.e., to make a topical diagnosis. At the same time, diagnostics is aimed at identifying the main disturbed links in the course of the development and implementation of speech processes, on the basis of which the form of speech disorders is determined. There is no doubt that when using the clinical classification of speech developmental disorders in children, a significant proportion of cases of ONR are associated with developmental dysphasia (alalia).
For the normal development of speech, it is necessary that the brain, and especially the cortex of its cerebral hemispheres, reach a certain maturity, the articulatory apparatus be formed, and hearing be preserved. Another indispensable condition is a full-fledged speech environment from the first days of a child's life.
Another indispensable condition is a full-fledged speech environment from the first days of a child's life.
The reasons for the lag in the development of speech may be the pathology of the course of pregnancy and childbirth, dysfunction of the articulatory apparatus, damage to the organ of hearing, a general lag in the mental development of the child, the influence of heredity and adverse social factors (insufficient communication and education). Difficulties in mastering speech are also characteristic of children with signs of a lag in physical development, who have suffered serious illnesses at an early age, are weakened, and receive malnutrition.
Hearing impairment is the most common cause of isolated speech delay [8]. It is known that even a moderately pronounced and gradually developing hearing loss can lead to a lag in the development of speech. Signs of hearing loss in toddlers include lack of response to sounds, inability to imitate sounds, and in older children excessive use of gestures and close observation of the lips of people who speak. However, the assessment of hearing based on the study of behavioral responses is insufficient and is subjective. Therefore, if partial or complete hearing loss is suspected in a child with an isolated speech delay, an audiological study should be performed. Reliable results are also given by the method of recording auditory evoked potentials. The sooner hearing defects are detected, the sooner it will be possible to start appropriate corrective work with the baby or provide him with a hearing aid.
However, the assessment of hearing based on the study of behavioral responses is insufficient and is subjective. Therefore, if partial or complete hearing loss is suspected in a child with an isolated speech delay, an audiological study should be performed. Reliable results are also given by the method of recording auditory evoked potentials. The sooner hearing defects are detected, the sooner it will be possible to start appropriate corrective work with the baby or provide him with a hearing aid.
The reasons for delay in the development of speech in a child may be autism or general mental retardation , which is characterized by a uniform incomplete formation of all higher mental functions and intellectual abilities. To clarify the diagnosis, an in-depth examination by a child psychoneurologist is carried out [9].
On the other hand, it is necessary to distinguish between tempo retardation of speech development due to a lack of stimulation of speech development under the influence of unfavorable social factors (insufficient communication and education). The speech of a child is not an innate ability, it is formed under the influence of the speech of adults and to a large extent depends on sufficient speech practice, a normal speech environment, on education and training, which begin from the first days of a child's life. The social environment stimulates speech development, represents a sample of speech. It is known that in families with meager speech impulses, children begin to speak late and speak little. The lag in speech development may be accompanied by general underdevelopment, while the natural intellectual and speech abilities of these children are normal.
The speech of a child is not an innate ability, it is formed under the influence of the speech of adults and to a large extent depends on sufficient speech practice, a normal speech environment, on education and training, which begin from the first days of a child's life. The social environment stimulates speech development, represents a sample of speech. It is known that in families with meager speech impulses, children begin to speak late and speak little. The lag in speech development may be accompanied by general underdevelopment, while the natural intellectual and speech abilities of these children are normal.
Neurobiological factors in the pathogenesis of speech developmental disorders. Perinatal pathology of the CNS plays a significant role in the formation of speech disorders in children. This is due to the fact that it is in the perinatal period that the most important events occur that have a direct and indirect impact on the processes of the structural and functional organization of the CNS. Taking this into account, it is advisable to identify risk groups for disorders of psychoverbal development as early as the first year of life [10]. The high-risk group should include children who, in the first 3 months. life as a result of the examination revealed structural changes in the CNS, premature (especially with extremely low body weight), children with analyzer disorders (auditory and visual), insufficiency of the cranial nerves (in particular V, VII, IX, X, XII), children with a delay in the reduction of unconditional automatisms, long-term violations of muscle tone [10].
Taking this into account, it is advisable to identify risk groups for disorders of psychoverbal development as early as the first year of life [10]. The high-risk group should include children who, in the first 3 months. life as a result of the examination revealed structural changes in the CNS, premature (especially with extremely low body weight), children with analyzer disorders (auditory and visual), insufficiency of the cranial nerves (in particular V, VII, IX, X, XII), children with a delay in the reduction of unconditional automatisms, long-term violations of muscle tone [10].
In premature newborns, especially those with a short gestational age, an important period of CNS development (interneuronal organization and intense myelination) occurs not in utero, but under difficult conditions of postnatal adaptation. The duration of this period can vary from 2-3 weeks. up to 2-3 months, and this period is often accompanied by the development of various infectious and somatic complications, which is an additional factor causing disorders of psychomotor and speech development in immature and premature babies. A negative role is played by one of the main consequences of prematurity - hearing loss [10]. Studies have shown that approximately half of very preterm children have a delay in speech development, and at school age - learning difficulties, problems with reading and writing, concentration of attention and behavior control [11].
A negative role is played by one of the main consequences of prematurity - hearing loss [10]. Studies have shown that approximately half of very preterm children have a delay in speech development, and at school age - learning difficulties, problems with reading and writing, concentration of attention and behavior control [11].
In recent years, the role of genetic factors in the formation of speech development disorders has also been confirmed [10].
The development of speech skills is normal. For timely and accurate diagnosis of speech disorders in children, it is necessary to take into account the patterns of normal speech development. Children pronounce their first words by the end of the first year of life, but they begin to train their speech apparatus much earlier, from the first months of life, so the age of up to one year is a preparatory period in the development of speech. The sequence in the development of pre-speech reactions is shown in Table 1.
So, in the first year of life, the child is preparing the speech apparatus for the pronunciation of sounds.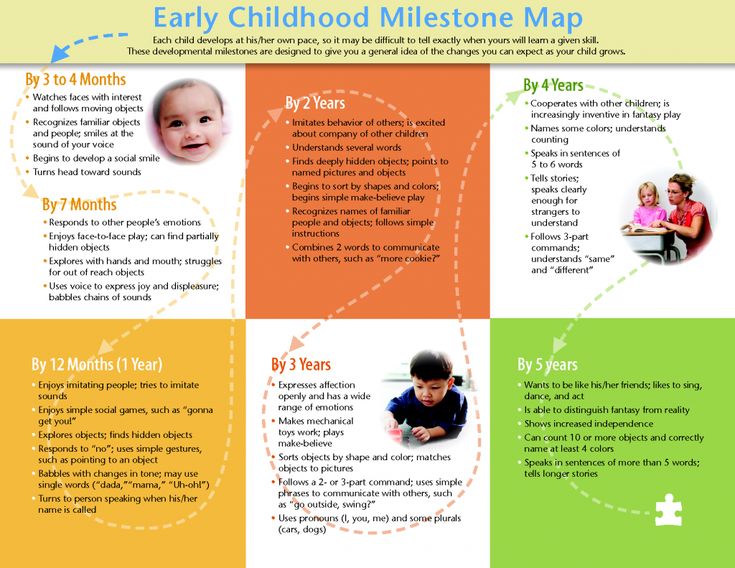 Cooing, “flute”, babble, modulated babble are a kind of game for the baby and give the child pleasure, for many minutes he can repeat the same sound, training in a similar way in the articulation of speech sounds. At the same time, there is an active formation of understanding of speech.
Cooing, “flute”, babble, modulated babble are a kind of game for the baby and give the child pleasure, for many minutes he can repeat the same sound, training in a similar way in the articulation of speech sounds. At the same time, there is an active formation of understanding of speech.
An important indicator of the development of speech up to one and a half to two years is not so much the actual pronunciation, but the understanding of addressed speech (receptive speech). The child should listen carefully and with interest to adults, understand well the speech addressed to him, recognize the names of many objects and pictures, and fulfill simple household requests-instructions. In the second year of life, words and sound combinations are already becoming a means of verbal communication, that is, expressive speech is being formed.
The main indicators of the normal development of speech from 1 year to 4 years:
• The appearance of clear, meaningful speech (words) - 9-18 months.
• At first (up to one and a half years), the child mainly learns to understand speech, and from 1.5–2 years old, active speech quickly develops, vocabulary grows. The number of words the baby understands (passive vocabulary) is greater than the number of words he can say (active vocabulary).
• The appearance of phrases from 2 words - 1.5-2 years, from 3 words - 2-2.5 years, from 4 or more words - 3-4 years.
• Volume of active dictionary:
- by the age of 1.5 years, children pronounce 5–20 words,
– 2 years – up to 150–300 words,
– 3 years – up to 800–1000 words,
- 4 years - up to 2000 words.
Early signs of trouble in speech formation. Children who are not trying to speak at 2–2.5 years of age should be of concern. However, parents may notice certain prerequisites for trouble in speech development even earlier. In the first year of life, the absence or weak expression of cooing, babbling, first words, reactions to adult speech and interest in it at the appropriate time should be alarming; at one year old - the child does not understand frequently used words and does not imitate the sounds of speech, does not respond to the speech addressed to him, and resorts only to crying to attract attention to himself; in the second year - lack of interest in speech activity, replenishment of the passive and active vocabulary, the appearance of phrases, inability to understand the simplest questions and show the image in the picture.
At 3–4 years of age, signs of dysfunctional speech formation should cause high alertness in comparison with the normal characteristics of its development, which are given in Table 2.
The lack of help at an early age for children with speech underdevelopment leads to the formation of a number of consequences: communication disorders and the resulting difficulties of adaptation in the children's team and contacts with other people, immaturity in the emotional sphere and behavior, insufficient cognitive activity. This is confirmed by the data of our study in order to assess the indicators of the age development of children with dysphasia [12].
We examined 120 patients aged 3 to 4.5 years (89 boys and 31 girls) with developmental dysphasia, a disorder in the development of expressive speech (F80.1 according to ICD-10 [3]) and a pattern of OHP of the 1st–2nd level. according to the psychological and pedagogical classification [7]. The study group excluded children whose speech development lag was due to hearing loss, mental retardation, autism, severe somatic pathology, malnutrition, as well as the influence of adverse social factors (insufficient communication and education).
The study of indicators of age development was carried out by us using the Developmental Profile 3 (DP-3) methodology [13] in five areas: motor skills, adaptive behavior, socio-emotional sphere, cognitive sphere, speech and communication skills.
A form was used for a structured survey conducted by a specialist with parents. Based on the data obtained, it was determined what age the child's development corresponds to in each of the areas and at what age interval he has a lag behind the normal indicators for his calendar age.
When examining the anamnesis, many parents indicated that already at an early age they paid attention to the absence or limitation of babbling in children. Parents noted silence, emphasized that the child understands everything, but does not want to speak. Instead of speech, facial expressions and gestures developed, which the children used selectively in emotionally charged situations. The first words and phrases appeared late. At the same time, parents noted that, in addition to the lag in speech, in general, children develop normally. The children had a meager active vocabulary, used babbling words, onomatopoeia, and sound complexes. There were many reservations in the speech, to which the children paid attention and tried to correct what was erroneously said. At the time of the survey, the volume of the active vocabulary (stock of spoken words) in children with OHP level 1 did not exceed 15-20 words, and with OHP level 2 - 20-50 words.
The children had a meager active vocabulary, used babbling words, onomatopoeia, and sound complexes. There were many reservations in the speech, to which the children paid attention and tried to correct what was erroneously said. At the time of the survey, the volume of the active vocabulary (stock of spoken words) in children with OHP level 1 did not exceed 15-20 words, and with OHP level 2 - 20-50 words.
Table 3 presents the results of the examination, showing the age interval for which there was a lag behind normal indicators in three groups of children with developmental dysphasia, divided by age: (1) from 3 years 0 months. up to 3 years 5 months; (2) from 3 years 6 months. up to 3 years 11 months; (3) from 4 years 0 months up to 4 years 5 months
It seems natural that the most significant was the lag in the formation of speech and communication skills, but the degree of this lag increased - from 17.3 ± 0.4 months. in the 1st group up to 21.2±0.8 in the 2nd and 27. 3±0.5 months. in the 3rd group. Along with an increase in the severity of differences from healthy peers in speech development, the lag in all other areas not only persisted, but also increased with each six-month age period. This testifies, on the one hand, to the significant influence of speech on other areas of the child's development, and on the other hand, to the close interconnection and inseparability of various aspects of individual development.
3±0.5 months. in the 3rd group. Along with an increase in the severity of differences from healthy peers in speech development, the lag in all other areas not only persisted, but also increased with each six-month age period. This testifies, on the one hand, to the significant influence of speech on other areas of the child's development, and on the other hand, to the close interconnection and inseparability of various aspects of individual development.
The main areas of complex therapy for developmental dysphasia in children are: speech therapy, psychological and pedagogical corrective measures, psychotherapeutic assistance to the child and his family, drug treatment. Since developmental dysphasia is a complex medical, psychological and pedagogical problem, the complexity of the impact and the continuity of work with children of specialists in various fields are of particular importance when organizing assistance to such children.
Speech therapy assistance is based on the ontogenetic principle, taking into account the patterns and sequence of speech formation in children. In addition, it has an individual, differentiated character depending on a number of factors: the leading mechanisms and symptoms of speech disorders, the structure of the speech defect, the age and individual characteristics of the child. Speech therapy and psychological-pedagogical corrective measures are a purposeful, complexly organized process that is carried out for a long time and systematically. Under these conditions, correctional work gives the majority of children with developmental dysphasia the means sufficient for verbal communication.
In addition, it has an individual, differentiated character depending on a number of factors: the leading mechanisms and symptoms of speech disorders, the structure of the speech defect, the age and individual characteristics of the child. Speech therapy and psychological-pedagogical corrective measures are a purposeful, complexly organized process that is carried out for a long time and systematically. Under these conditions, correctional work gives the majority of children with developmental dysphasia the means sufficient for verbal communication.
The most complete correction of speech development disorders is facilitated by the timely use of nootropic drugs. Their appointment is justified based on the main effects of this group of drugs: nootropic, stimulating, neurotrophic, neurometabolic, neuroprotective. One of these drugs is acetylaminosuccinic acid (Cogitum).
Kogitum is an adaptogenic and general tonic agent that normalizes the processes of nervous regulation and has immunostimulating activity. Kogitum contains acetylaminosuccinic acid (in the form of a dipotassium salt of acetylaminosuccinate) - a synthetic analogue of aspartic acid - a non-essential amino acid found mainly in the tissues of the central nervous system.
Kogitum contains acetylaminosuccinic acid (in the form of a dipotassium salt of acetylaminosuccinate) - a synthetic analogue of aspartic acid - a non-essential amino acid found mainly in the tissues of the central nervous system.
For pediatricians and pediatric neurologists, such properties of aspartic acid are important as participation in the synthesis of DNA and RNA, the effect on increasing physical activity and endurance, normalizing the balance between the processes of excitation and inhibition in the CNS, and immunomodulatory action (acceleration of antibody formation processes) [14]. Aspartic acid is involved in a number of metabolic processes, in particular, it regulates carbohydrate metabolism by stimulating the transformation of carbohydrates into glucose and the subsequent creation of glycogen stores; along with glycine and glutamic acid, aspartic acid serves as a neurotransmitter in the central nervous system, stabilizes the processes of nervous regulation, and has a psychostimulating activity [14]. In neuropediatric practice, the drug has been used for many years for such indications as delayed psychomotor and speech development, consequences of perinatal lesions of the central nervous system, neuroinfections and craniocerebral injuries, cerebrasthenic and astheno-neurotic syndromes.
In neuropediatric practice, the drug has been used for many years for such indications as delayed psychomotor and speech development, consequences of perinatal lesions of the central nervous system, neuroinfections and craniocerebral injuries, cerebrasthenic and astheno-neurotic syndromes.
Release form. Solution for oral administration in ampoules of 10 ml. 1 ml of the drug contains 25 mg of acetyl-aminosuccinic (aspartic) acid, and 1 ampoule (10 ml) - 250 mg. The composition of the drug includes: fructose (levulose) - 1.0 g, methyl parahydroxybenzoate (methyl-n-hydroxybenzoate) - 0.015 g, aromatic substances (banana flavor) - 0.007 g, distilled water - up to 10 ml per 1 ampoule. The drug does not contain crystalline sugar or its synthetic substitutes, therefore it is not contraindicated in diabetes mellitus.
Dosing regimens. The drug is given orally undiluted or with a small amount of liquid. For children aged 7-10 years, it is recommended to take 1 ampoule (250 mg) orally in the morning, for children over 10 years old - 1-2 ampoules (250-500 mg) in the morning.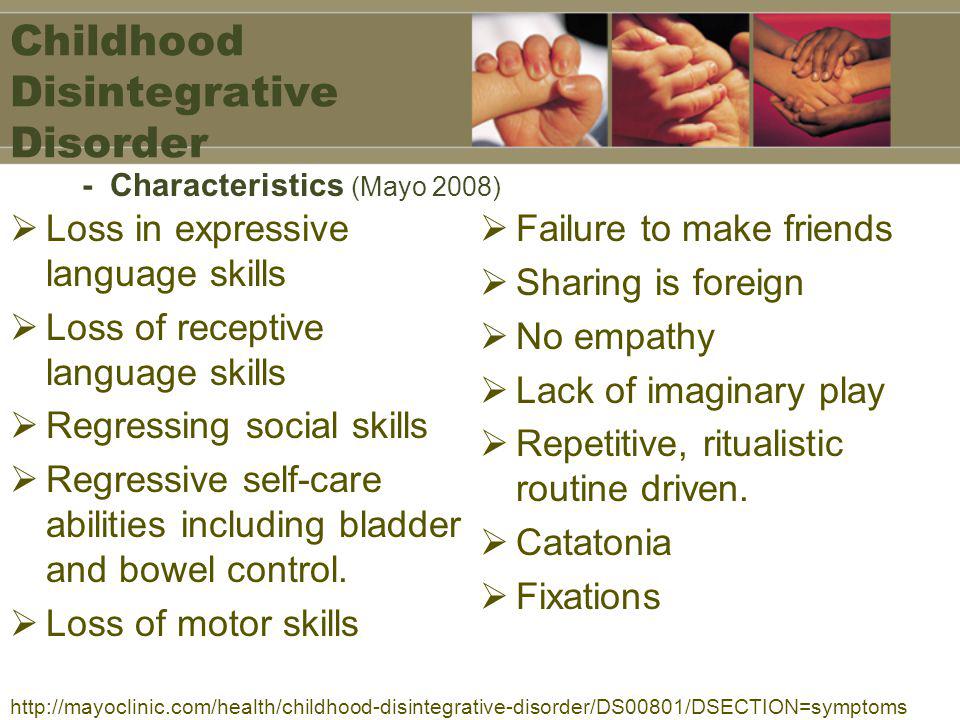 For patients from 1 to 7 years of age, the dose is determined by the doctor individually [14]. In our experience, it is preferable for children under 7 years of age to prescribe 5 ml (1/2 ampoules) 1 or 2 times a day. The duration of the course of treatment is usually 2-4 weeks. With a single dose, the drug is prescribed in the morning, with a double dose - the second dose no later than 16-17 hours. Before prescribing Kogitum, it is necessary to obtain written informed consent from parents / legal representatives for the treatment of a child with acetylaminosuccinic acid, indicating that they are familiar with the indications, contraindications and side effects and do not object to giving the drug to a child.
For patients from 1 to 7 years of age, the dose is determined by the doctor individually [14]. In our experience, it is preferable for children under 7 years of age to prescribe 5 ml (1/2 ampoules) 1 or 2 times a day. The duration of the course of treatment is usually 2-4 weeks. With a single dose, the drug is prescribed in the morning, with a double dose - the second dose no later than 16-17 hours. Before prescribing Kogitum, it is necessary to obtain written informed consent from parents / legal representatives for the treatment of a child with acetylaminosuccinic acid, indicating that they are familiar with the indications, contraindications and side effects and do not object to giving the drug to a child.
Side effects. Although hypersensitivity reactions (allergic reactions) to individual components of the drug are possible, they are rare. Overdoses of the drug are not reported in the literature.
If necessary, children with speech development delays may be prescribed repeated courses of treatment with nootropic drugs.