How to diagnose bipolar disorder in a child
NIMH » Bipolar Disorder in Children and Teens
Does your child go through extreme changes in mood and behavior? Does your child get much more excited or much more irritable than other kids? Do you notice that your child goes through cycles of extreme highs and lows more often than other children? Do these mood changes affect how your child acts at school or at home?
Some children and teens with these symptoms may have bipolar disorder, a brain disorder that causes unusual shifts in mood, energy, activity levels, and day-to-day functioning. With treatment, children and teens with bipolar disorder can get better over time.
What is bipolar disorder?
Bipolar disorder is a mental disorder that causes people to experience noticeable, sometimes extreme, changes in mood and behavior. Sometimes children with bipolar disorder feel very happy or “up” and are much more energetic and active than usual. This is called a manic episode. Sometimes children with bipolar disorder feel very sad or “down” and are much less active than usual. This is called a depressive episode.
Bipolar disorder, which used to be called manic-depressive illness or manic depression, is not the same as the normal ups and downs every child goes through. The mood changes in bipolar disorder are more extreme, often unprovoked, and accompanied by changes in sleep, energy level, and the ability to think clearly. Bipolar symptoms can make it hard for young people to perform well in school or to get along with friends and family members. Some children and teens with bipolar disorder may try to hurt themselves or attempt suicide.
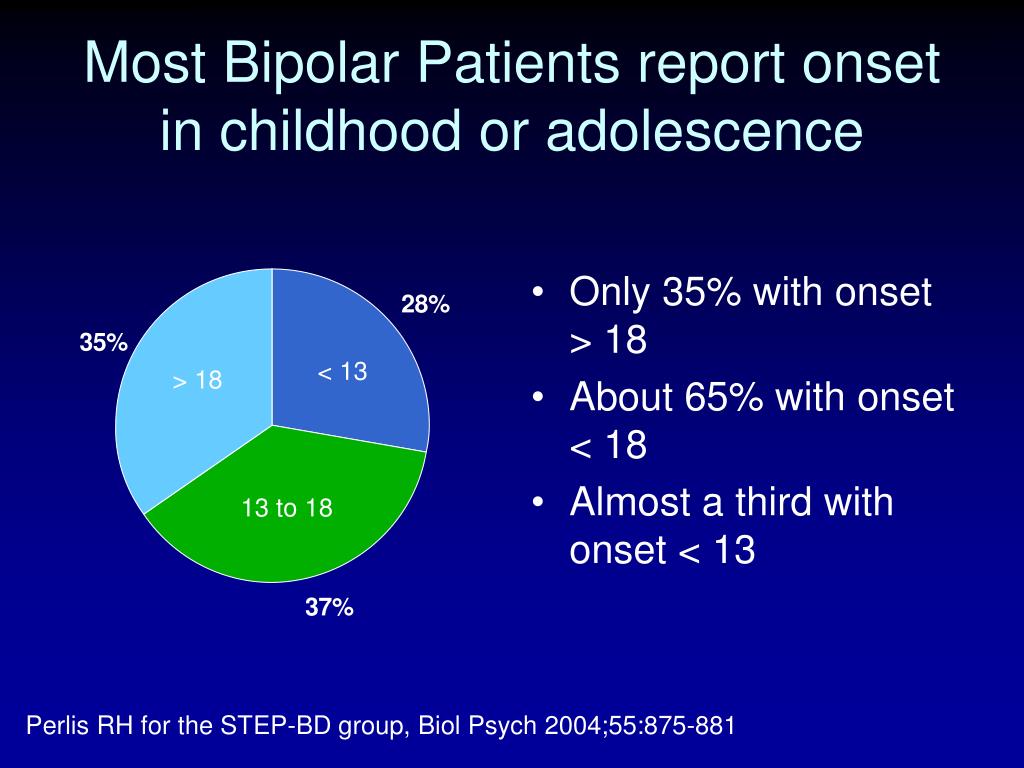
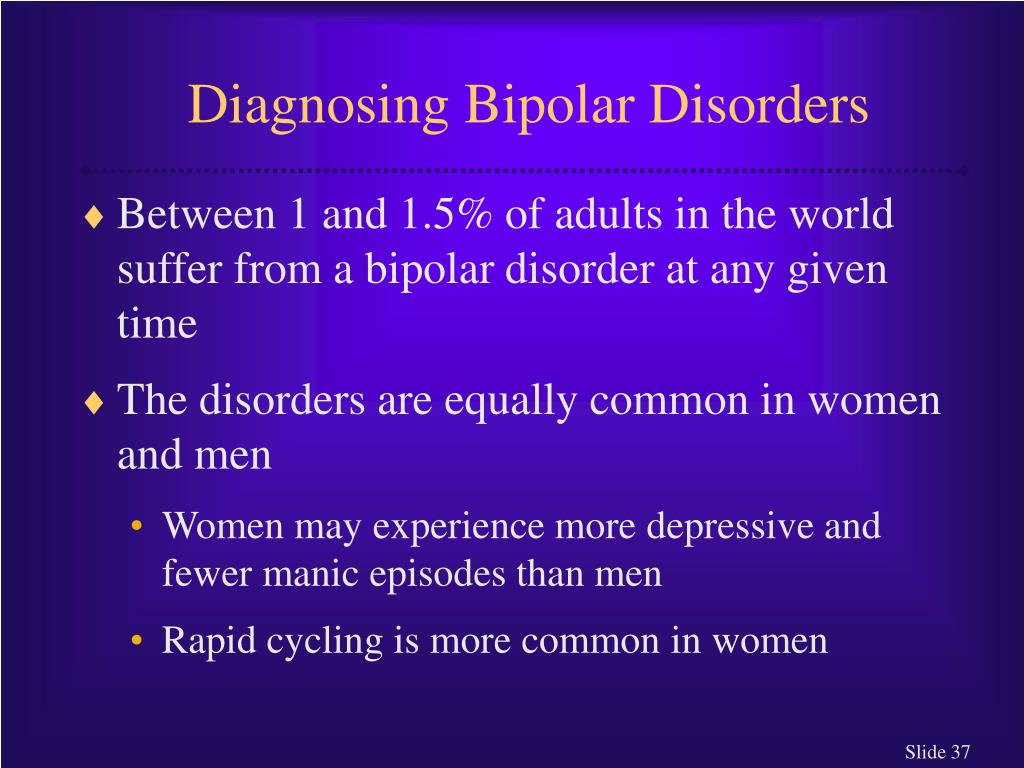
Most people are diagnosed with bipolar disorder in adolescence or adulthood, but the symptoms can appear earlier in childhood. Bipolar disorder is often episodic, but it usually lasts a lifetime.
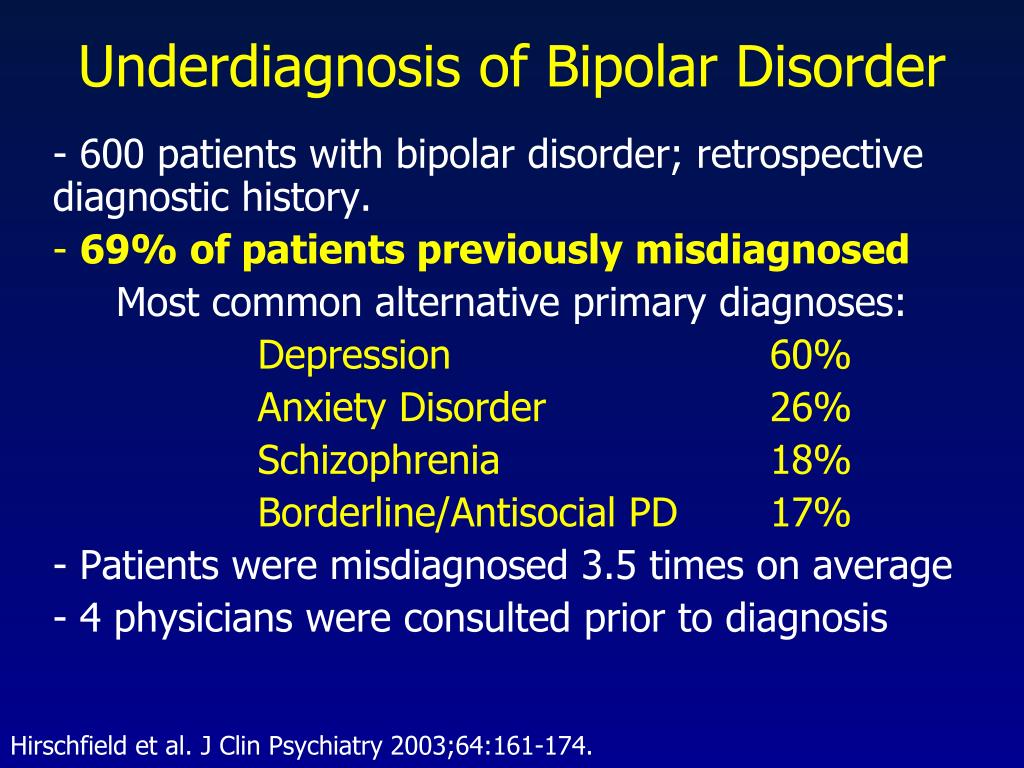
Signs and symptoms of bipolar disorder may overlap with symptoms of other disorders that are common in young people, such as attention-deficit/hyperactivity disorder (ADHD), conduct problems, major depression, and anxiety disorders. Diagnosing bipolar disorder can be complicated and requires a careful and thorough evaluation by a trained, experienced mental health professional.
Diagnosing bipolar disorder can be complicated and requires a careful and thorough evaluation by a trained, experienced mental health professional.
With treatment, children and teens with bipolar disorder can manage their symptoms and lead successful lives.
What causes bipolar disorder?
The exact causes of bipolar disorder are unknown, but several factors may contribute to the illness.
For example, researchers are beginning to uncover genetic mechanisms that are linked to bipolar disorder and other mental disorders. Research shows that people’s chance of having bipolar disorder is higher if they have a close family member with the illness, which may be because they have the same genetic variations. However, just because one family member has bipolar disorder, it does not mean that other members of the family will have it. Many genes are involved in the disorder, and no single gene causes it.
Research also suggests that adversity, trauma, and stressful life events may increase the chances of developing bipolar disorder in people with a genetic risk of having the illness.
Some research studies have found differences in brain structure and function between people who have bipolar disorder and those who do not. Researchers are studying the disorder to learn more about its causes and effective treatments.
What are the symptoms of bipolar disorder?
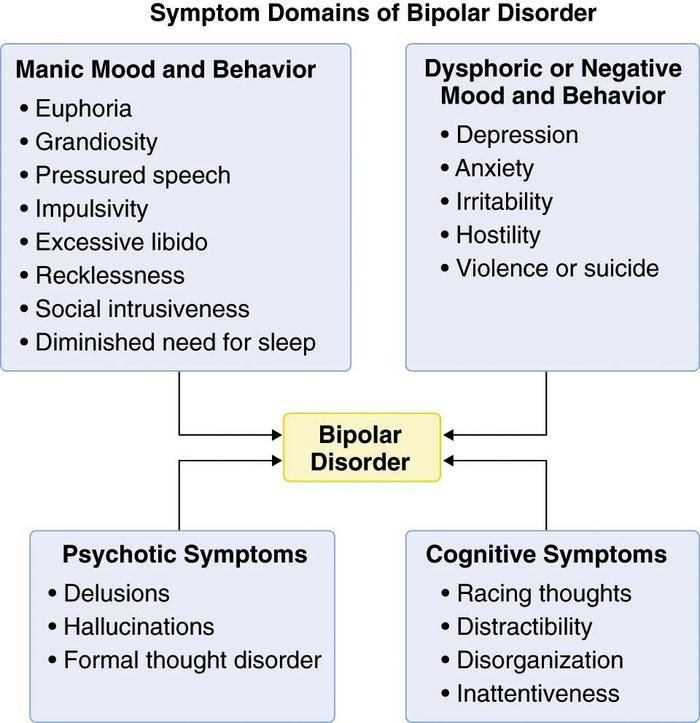
Mood episodes in bipolar disorder include intense emotions along with significant changes in sleep habits, activity levels, thoughts, or behaviors. A person with bipolar disorder may have manic episodes, depressive episodes, or “mixed” episodes. A mixed episode has both manic and depressive symptoms. These mood episodes cause symptoms that often last for several days or weeks. During an episode, the symptoms last every day for most of the day.
These mood and activity changes are very different from the child’s usual behavior and from the behavior of healthy children and teens.
Children and teens having a manic episode may:
- Show intense happiness or silliness for long periods of time.
- Have a very short temper or seem extremely irritable.
- Talk fast about a lot of different things.
- Have trouble sleeping but not feel tired.
- Have trouble staying focused, and experience racing thoughts.
- Seem overly interested or involved in pleasurable but risky activities.
- Do risky or reckless things that show poor judgment.
Children and teens having a depressive episode may:
- Feel frequent and unprovoked sadness.
- Show increased irritability, anger, or hostility.
- Complain a lot about pain, such as stomachaches and headaches.
- Have a noticeable increase in amount of sleep.
- Have difficulty concentrating.
- Feel hopeless and worthless.
- Have difficulty communicating or maintaining relationships.
- Eat too much or too little.
- Have little energy and no interest in activities they usually enjoy.
- Think about death, or have thoughts of suicide.
Can children and teens with bipolar disorder have other problems?
Young people with bipolar disorder can have several problems at the same time. These include:
- Misuse of alcohol and drugs. Young people with bipolar disorder are at risk of misusing alcohol or drugs.
- Attention-deficit/hyperactivity disorder (ADHD). Children and teens who have both bipolar disorder and ADHD may have trouble staying focused.
- Anxiety disorders. Children and teens with bipolar disorder also may have an anxiety disorder.
Sometimes extreme behaviors go along with mood episodes. During manic episodes, young people with bipolar disorder may take extreme risks that they wouldn’t usually take or that could cause them harm or injury. During depressive episodes, some young people with bipolar disorder may think about running away from home or have thoughts of suicide.
If your child shows signs of suicidal thinking, take these signs seriously and call your child’s health care provider.
If you think your child is in crisis and needs immediate help, call 911. You also can call the National Suicide Prevention Lifeline (Lifeline) at 1‑800‑273‑TALK (8255), or text the Crisis Text Line (text HELLO to 741741). These services are confidential, free, and available 24/7.
How is bipolar disorder diagnosed?
A health care provider will ask questions about your child’s mood, sleeping patterns, energy levels, and behavior. There are no blood tests or brain scans that can diagnose bipolar disorder. However, the health care provider may use tests to see if something other than bipolar disorder is causing your child’s symptoms. Sometimes health care providers need to know about medical conditions in the family, such as depression or substance use.
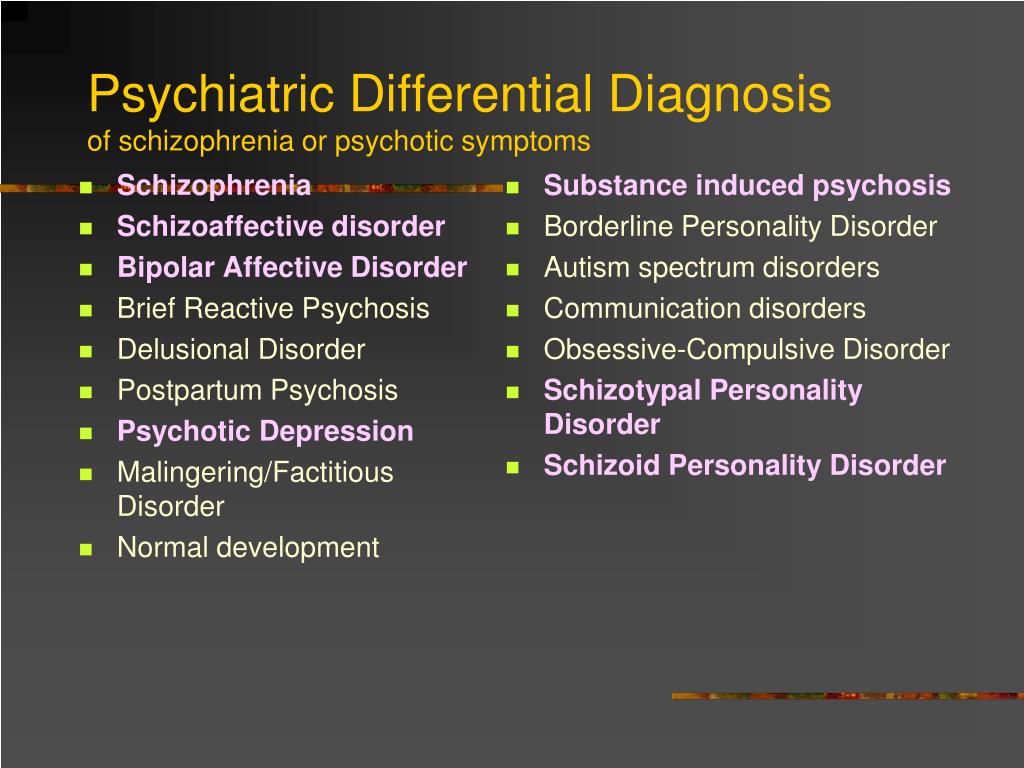
Other disorders have symptoms like those of bipolar disorder, including ADHD, disruptive mood regulation disorder, oppositional defiant disorder, conduct disorder, and anxiety disorders.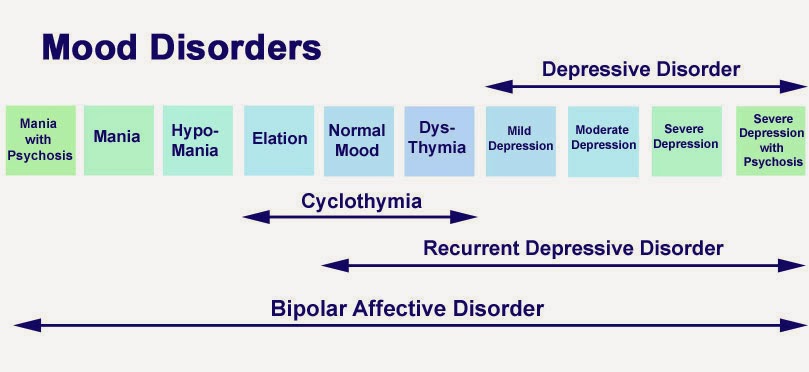 It also can be challenging to distinguish bipolar disorder from depression that occurs without mania, which is referred to as “major depression.” A health care provider who specializes in working with children and teens can make a careful and complete evaluation of your child’s symptoms to provide the right diagnosis.
It also can be challenging to distinguish bipolar disorder from depression that occurs without mania, which is referred to as “major depression.” A health care provider who specializes in working with children and teens can make a careful and complete evaluation of your child’s symptoms to provide the right diagnosis.
How is bipolar disorder treated?
Children and teens can work with their health care provider to develop a treatment plan that will help them manage their symptoms and improve their quality of life. It is important to follow the treatment plan, even when your child is not currently experiencing a mood episode. Steady, dependable treatment works better than treatment that starts and stops.
Treatment options include:
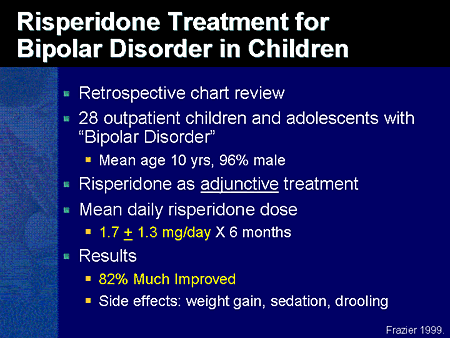
- Medication. Several types of medication can help treat symptoms of bipolar disorder. Children respond to medications in different ways, so the right type of medication depends on the child.
 This means children may need to try different types of medication to see which one works best for them. Some children may need more than one type of medication because their symptoms are complex. Children should take the fewest number of medications and the smallest doses possible to help their symptoms. A good way to remember this is “start low, go slow.” Medications can cause side effects. Always tell your child’s health care provider about any problems with side effects. Do not stop giving your child medication without speaking to a health care provider. Stopping medication suddenly can be dangerous and can make bipolar symptoms worse.
This means children may need to try different types of medication to see which one works best for them. Some children may need more than one type of medication because their symptoms are complex. Children should take the fewest number of medications and the smallest doses possible to help their symptoms. A good way to remember this is “start low, go slow.” Medications can cause side effects. Always tell your child’s health care provider about any problems with side effects. Do not stop giving your child medication without speaking to a health care provider. Stopping medication suddenly can be dangerous and can make bipolar symptoms worse. - Psychosocial Therapy. Different kinds of psychosocial therapy can help children and their families manage the symptoms of bipolar disorder. Therapies that are based on scientific research—including cognitive behavioral approaches and family-focused therapy—can provide support, education, and guidance to youth and their families.
 These therapies teach skills that can help people manage bipolar disorder, including skills for maintaining routines, enhancing emotion regulation, and improving social interactions.
These therapies teach skills that can help people manage bipolar disorder, including skills for maintaining routines, enhancing emotion regulation, and improving social interactions.
What can children and teens expect from treatment?
With treatment, children and teens with bipolar disorder can get better over time. Treatment is more effective when health care providers, parents, and young people work together.
Sometimes a child’s symptoms may change, or disappear and then come back. When this happens, your child’s health care provider may recommend changes to the treatment plan. Treatment can take time, but sticking with the treatment plan can help young people manage their symptoms and reduce the likelihood of future episodes.
Your child’s health care provider may recommend keeping a daily life chart or mood chart to track your child’s moods, behaviors, and sleep patterns. This may make it easier to track the illness and see whether treatment is working.
How can I help my child or teen?
Help begins with the right diagnosis and treatment. Talk to your family health care provider about any symptoms you notice.
If your child has bipolar disorder, here are some basic things you can do:
- Be patient.
- Encourage your child to talk, and listen to your child carefully.
- Pay attention to your child’s moods, and be alert to any major changes.
- Understand triggers, and learn strategies for managing intense emotions and irritability.
- Help your child have fun.
- Remember that treatment takes time: sticking with the treatment plan can help your child get better and stay better.
- Help your child understand that treatment can make life better.
How does bipolar disorder affect caregivers and families?
Caring for a child or teenager with bipolar disorder can be stressful for parents and families. Coping with a child’s mood episodes and other problems—such as short tempers and risky behaviors—can challenge any caregiver.
Coping with a child’s mood episodes and other problems—such as short tempers and risky behaviors—can challenge any caregiver.
It is important that caregivers take care of themselves, too. Find someone you can talk to or consult your health care provider about support groups. Finding support and strategies for managing stress can help you and your child.
Where do I go for help?
If you’re not sure where to get help, your doctor, pediatrician, or other family health care provider is a good place to start. A health care provider can refer you to a qualified mental health professional, such as a psychiatrist or psychologist, who has experience treating bipolar disorder and can evaluate your child’s symptoms.
You can learn more about getting help and finding a health care provider on the National Institute of Mental Health website. Hospital health care providers can help in an emergency. The Substance Abuse and Mental Health Services Administration (SAMHSA) has an online tool to help you find mental health services in your area.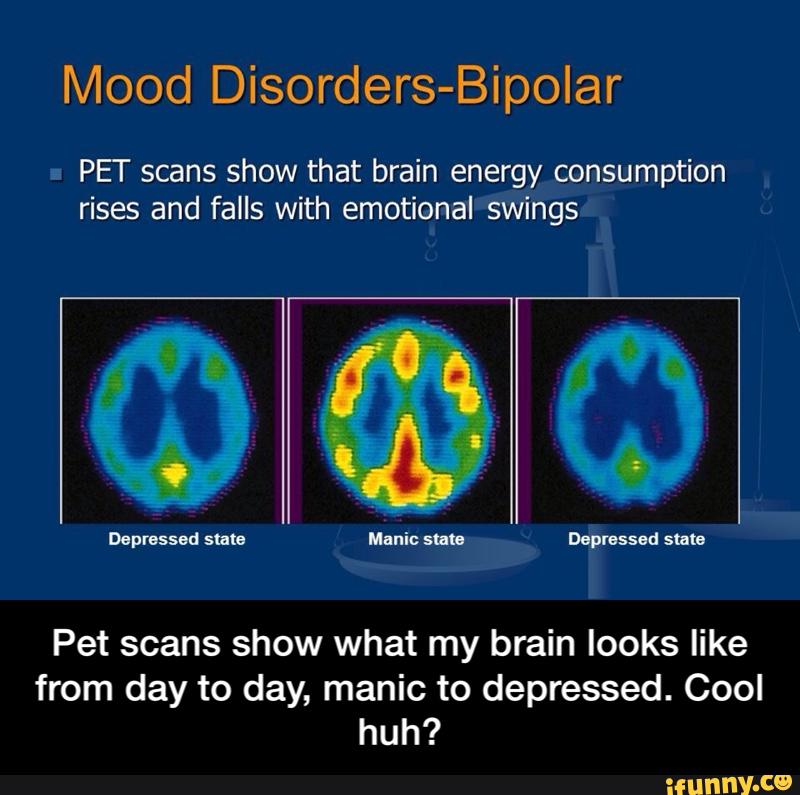
I know someone who is in crisis. What do I do?
If you know someone who might be thinking about hurting themselves or someone else, get help quickly.
- Do not leave the person alone.
- Call 911 or go to the nearest hospital emergency room.
- Call the toll-free National Suicide Prevention Lifeline at 1-800-273-TALK (8255) or the toll-free TTY number at 1-800-799-4TTY (4889). You also can text the Crisis Text Line (text HELLO to 741741) or go to the National Suicide Prevention Lifeline website.
What should I know about clinical trials?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct clinical trials with patients and healthy volunteers. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information, visit the NIMH Clinical Trials webpage.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. Citation of NIMH as a source is appreciated. To learn more about using NIMH publications, please contact the NIMH Information Resource Center at 1-866‑615‑6464, email [email protected], or refer to our reprint guidelines.
For More Information
MedlinePlus (National Library of Medicine) (En español)
ClinicalTrials.gov (En español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 20-MH-8081
Revised 2020
Pediatric Bipolar Disorder - CHADD
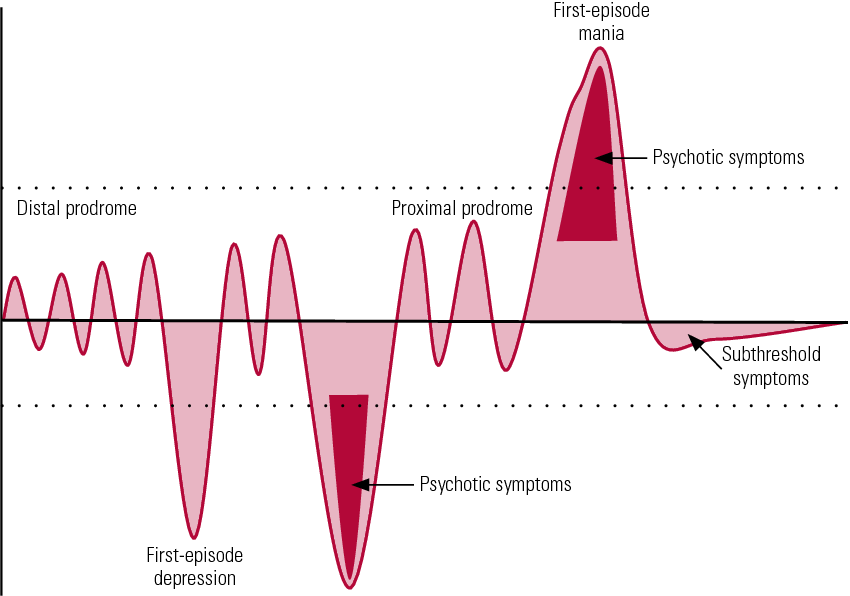
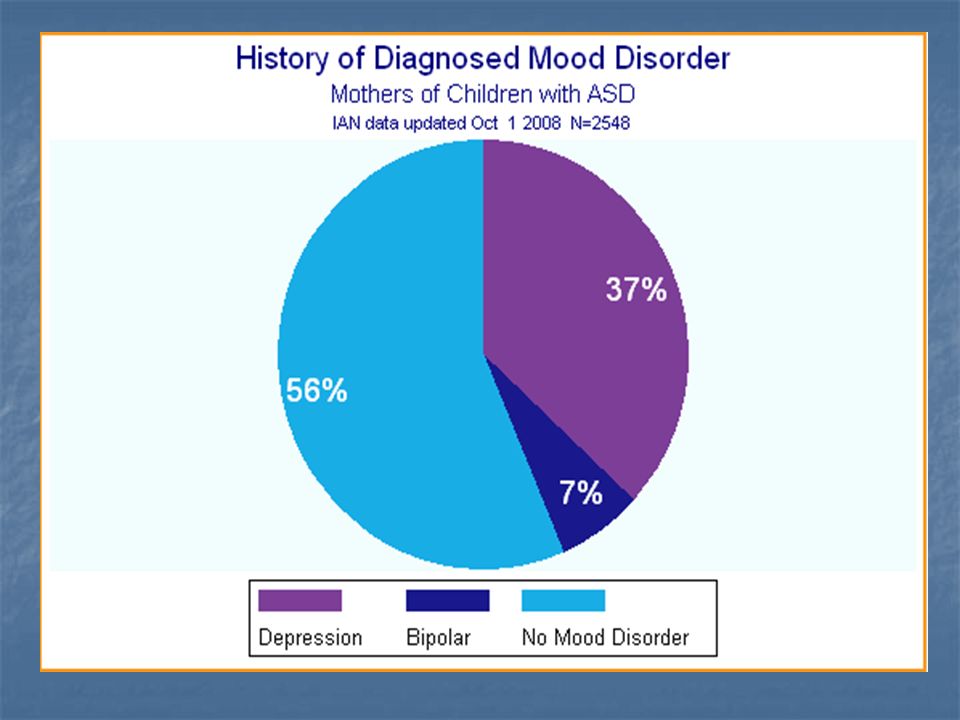
The existence of a mood disorder in adults involving severe mood swings from states of deep depression to states of elation has been recognized now for over a century. This disorder is commonly referred to as manic-depression but is now formally referred to as bipolar disorder, referring to the two “poles” of depression and mania. Until recently, however, youth were rarely diagnosed with this disorder. Bipolar disorder has also become a controversial area within the field of children’s mental health. There is little disagreement about whether it exists. The disagreement is about the symptoms of bipolar disorder in youth and how they differ from those in adults.
This disorder is commonly referred to as manic-depression but is now formally referred to as bipolar disorder, referring to the two “poles” of depression and mania. Until recently, however, youth were rarely diagnosed with this disorder. Bipolar disorder has also become a controversial area within the field of children’s mental health. There is little disagreement about whether it exists. The disagreement is about the symptoms of bipolar disorder in youth and how they differ from those in adults.
First, some definitions
Bipolar disorder involves episodes of both major depression and mania. (To clarify, major depression is another, separate mood disorder involving these same symptoms of depression but without the occurrence of symptoms of mania). The diagnostic manual used by mental health professionals is based on the diagnosis of bipolar disorder in adults. The following lists consist of behaviors observed by parents of children diagnosed with bipolar disorder.
Behaviors connected to major depressive episodes:
- marked decrease in interest in or pleasure from life, sometimes expressed by boredom
- agitation and irritability
- sleeping too much or inability to sleep
- significant change in appetite
- change in observed activity level (usually slowed down or dragging)
- loss of energy
- inability to concentrate
- frequent sadness or crying
- feelings of worthlessness or guilt
- thoughts of death or suicide or self-destructive behavior
Behaviors connected to mania:
- elevated, expansive or irritable mood
- inflated self esteem or grandiosity (an unrealistic sense of one’s capabilities)
- significantly decreased need for sleep
- much more talkative or pressured speech (speech so rapid that the words bump into and overrun each other)
- racing thoughts or flight of ideas (completely disconnected thoughts)
- distractibility
- excessive involvement in multiple projects and activities
- highly risky pursuit of pleasurable activities (for example, activities involving drugs, alcohol or sex)
The combination of episodes of mania and major depressive episodes is what constitutes classic bipolar disorder.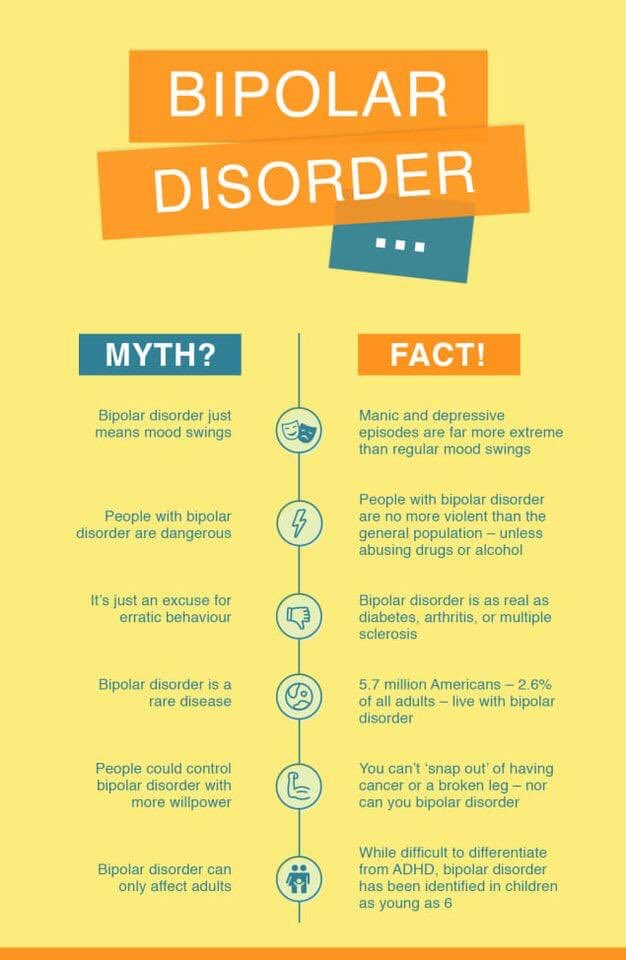 However, more than one type of bipolar disorder exists.
However, more than one type of bipolar disorder exists.
The controversy
As mentioned earlier, mental health practitioners disagree about the symptoms of bipolar disorder in youth and how they differ from those in adults. In adolescents, where the presentation of the disorder more closely resembles that seen in adults, there is much less controversy.
More controversy exists in children when there appears to be a more chronic course, including more irritability and unstable moods, including severe temper outbursts. In short, where does a child with ADHD, oppositional behaviors, and a fair degree of crankiness/moodiness end, and where does a child with bipolar disorder begin.
While no one has the definitive answers to these questions, there are competing schools of thought on this issue. Some experts feel that children with severe irritability, emotional instability, and severe temper outbursts are, in fact, suffering from bipolar disorder as it appears in childhood and should be treated accordingly. Other experts feel this approach will lead to the overdiagnosis of children who in fact suffer from disorders other than bipolar disorder. These experts argue for a narrower definition of bipolar disorder which includes episodic mood swings, elevated or expansive mood—not just irritable mood—and grandiosity or inappropriate euphoria (extreme joyfulness).
Other experts feel this approach will lead to the overdiagnosis of children who in fact suffer from disorders other than bipolar disorder. These experts argue for a narrower definition of bipolar disorder which includes episodic mood swings, elevated or expansive mood—not just irritable mood—and grandiosity or inappropriate euphoria (extreme joyfulness).
These experts clearly recognize that this definition excludes a number of children with episodes of mood instability, explosive rage episodes, extreme irritability and agitation. There is no disagreement that children with these symptoms are impaired. However, experts differ on whether or not such children should be diagnosed with bipolar disorder. Experts also differ on what would be the most appropriate and effective treatment for them.
There are also other factors that can seriously complicate the diagnosis of bipolar disorder in children. A history of severe emotional trauma such as physical or sexual abuse can lead to mood swings, emotional outbursts, hallucinations, and extremely severe behavioral problems, including sexualized behaviors that can resemble bipolar disorder.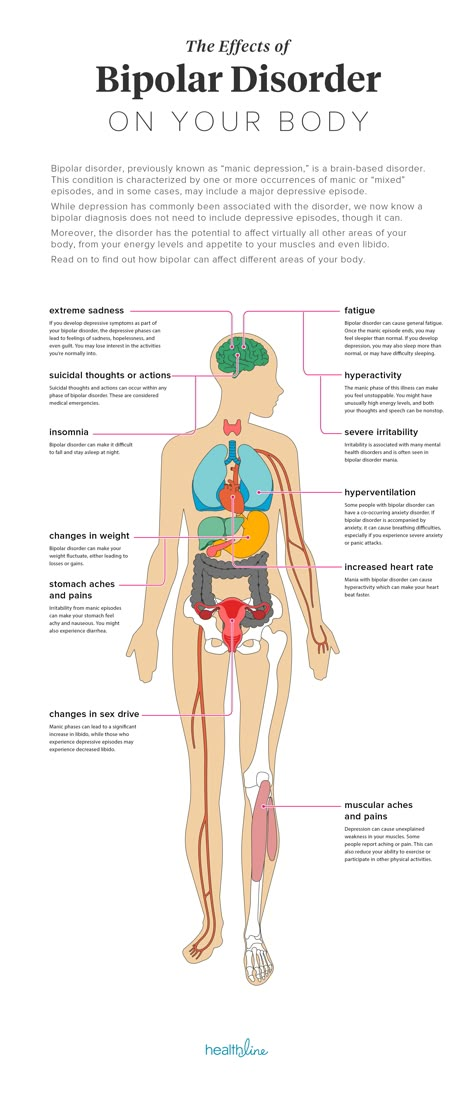 Improving our understanding of all of these issues depends on further research into these disorders as they appear in children and adolescents. Fortunately, some of this research is currently underway and holds the promise of better answers to these important questions in the future.
Improving our understanding of all of these issues depends on further research into these disorders as they appear in children and adolescents. Fortunately, some of this research is currently underway and holds the promise of better answers to these important questions in the future.
Bipolar disorder in children and adolescents
In adults, bipolar disorder commonly involves separate episodes of major depression, alternating with separate episodes of mania. In children mixed states (a mix of mania and depression) and rapid cycling (mood swings) may be much more common. This can make the diagnosis of bipolar disorder much more challenging in these age groups.
Many clinicians have observed that the symptoms of bipolar disorder appear to change as children develop, though these observations have not been confirmed by long-term studies. In younger children chronic irritability and mood instability without classic mood swings may predominate. These symptoms most closely resemble a mixed state of the disorder. In older children and adolescents, episodes including euphoria, grandiosity and paranoia may predominate. In all age groups hyperactivity, distractibility and pressured speech are seen. In general, the older the individual, the more the symptoms may resemble those seen in adults.
In older children and adolescents, episodes including euphoria, grandiosity and paranoia may predominate. In all age groups hyperactivity, distractibility and pressured speech are seen. In general, the older the individual, the more the symptoms may resemble those seen in adults.
Bipolar disorder and ADHD
As any parent of a child with ADHD has probably already noted, there is a significant overlap in the symptoms of mania, and to a lesser extent depression, and the symptoms of ADHD. ADHD, mania and depression may all involve inability to concentrate and problems with distractibility. Mania and ADHD may both involve hyperactivity and impulsivity. Though the symptom overlap is significant there are several factors that can help to distinguish these disorders.
ADHD in children usually does not involve mood symptoms such as depression and euphoria to the extent seen in bipolar disorder. ADHD symptoms usually first appear early in childhood while the onset of bipolar disorder appears to occur later in childhood or adolescence (4). ADHD also usually involves normal sleep, at least once a child has settled down in bed and is ready for sleep. Mania, in contrast, involves decreased need for sleep with the individual still “raring to go” the next day despite little sleep. The family history can be helpful, as both disorders appear to run in families.
ADHD also usually involves normal sleep, at least once a child has settled down in bed and is ready for sleep. Mania, in contrast, involves decreased need for sleep with the individual still “raring to go” the next day despite little sleep. The family history can be helpful, as both disorders appear to run in families.
Depression and bipolar disorder
People who suffer from depression, including those who suffer from major depressive disorder, may also eventually exhibit symptoms of bipolar disorder. It is harder to tell the difference between depression and bipolar disorder in children than in adults. Children with depression more often appear irritable than sad. This presents another overlap with the irritability seen in bipolar disorder. Children and adolescents are also by their nature prone to some degree of unstable mood. Determining where this type of moodiness ends and bipolar disorder begins in a depressed young person can present a challenge. Looking for the presence of other symptoms of mania or elevated mood, including the presence of euphoria or grandiosity at some point, is important in making this diagnostic distinction.
Further complicating the picture is the fact that both adults and younger people who initially exhibit symptoms only of depression may later develop bipolar disorder. The risk of depression turning into bipolar disorder is estimated at 10 percent or less in adults but appears to be as high as 20–40 percent in children and adolescents. Several risk factors for the eventual development of bipolar disorder in addition to early onset of depression have been identified, including psychosis, sudden onset, severely slowed or retarded movement, antidepressant-induced mania or elevated mood, and family history of bipolar disorder.
Treatment
Bipolar disorder is a serious disorder that can cause significant problems in school, the family, and the community. Untreated bipolar disorder can lead to hospitalization, drug abuse, accidents, or suicide. Parents who suspect that their child has bipolar disorder should find a child psychiatrist or psychologist who can evaluate the child.
The comprehensive treatment of bipolar disorder, like all other mental illnesses in children and adolescents, involves a multi-modal approach. Of course the first step in treatment is a comprehensive diagnostic evaluation performed by a child psychiatrist or psychologist with experience in the diagnosis of bipolar disorder in children and adolescents. Once the diagnosis is established ongoing treatment can begin. Medications form the foundation of this treatment. These medications have been found effective in adults and are currently being tested in children. At this point medication treatment of bipolar disorder involves the use of a mood stabilizer, which helps to prevent symptoms of mania while also hopefully improving symptoms of depression. In cases where depression remains a problem, the physician may consider prescribing an antidepressant as well as a mood stabilizer. Antidepressants in bipolar patients must be used cautiously, however, as they may cause a manic state.
Some clinicians are reluctant to prescribe stimulant medication for children who meet criteria for ADHD but who also have, or may have, bipolar disorder, because of a concern that bipolar symptoms might become worse.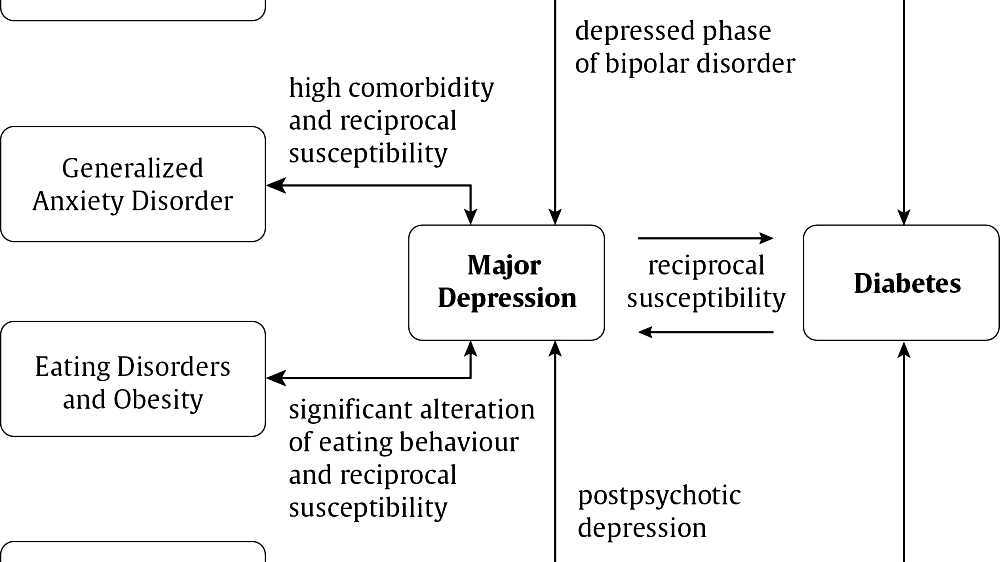 Currently, there is not evidence that this is the case, and research suggests that in general, children who have both ADHD and bipolar disorder can benefit from stimulant medication. However, it is important to be extremely careful in monitoring these children’s response to medication.
Currently, there is not evidence that this is the case, and research suggests that in general, children who have both ADHD and bipolar disorder can benefit from stimulant medication. However, it is important to be extremely careful in monitoring these children’s response to medication.
Other treatments are also very important in the management of this illness. They include measures to try to ensure regular sleep, which helps to keep mood stable. Therapy that educates the child about the importance of taking medication is also important. This is especially true for adolescents where any chronic illness can make it more difficult to achieve independence. Additionally, the family will benefit from comprehensive education and support as they help their child to deal with this very challenging illness. Academic interventions may also be needed (see Education). Finally, coexisting illnesses (other illnesses also present) including ADHD need to be treated.
The “classic” combination of mania and major depressive episodes is now referred to as Bipolar I Disorder.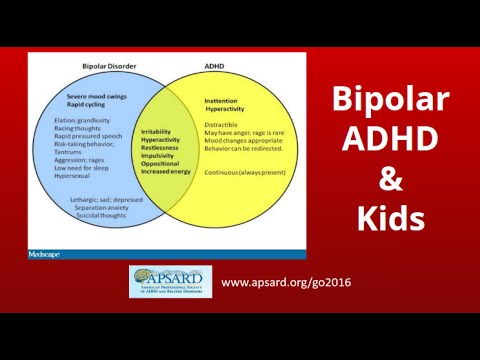 Major depressive episodes combined with a less severe expression of manic symptoms (called hypomania) is referred to as Bipolar II Disorder. Hypomania combined with a less pronounced and more longstanding form of depression (known as Dysthymia) is referred to as Cyclothymia. Symptoms of mania and a major depressive episode may also occur in combination simultaneously, this is called a Mixed State of Bipolar disorder. Finally, though episodes of mania and major depression classically occur in well-defined episodes, some people suffer from rapid swings between the two mood states that is referred to as Rapid Cycling. Bipolar I Disorder, Bipolar II Disorder, Cyclothymia, Mixed States and Rapid Cycling States are all considered to be bipolar spectrum disorders.
Major depressive episodes combined with a less severe expression of manic symptoms (called hypomania) is referred to as Bipolar II Disorder. Hypomania combined with a less pronounced and more longstanding form of depression (known as Dysthymia) is referred to as Cyclothymia. Symptoms of mania and a major depressive episode may also occur in combination simultaneously, this is called a Mixed State of Bipolar disorder. Finally, though episodes of mania and major depression classically occur in well-defined episodes, some people suffer from rapid swings between the two mood states that is referred to as Rapid Cycling. Bipolar I Disorder, Bipolar II Disorder, Cyclothymia, Mixed States and Rapid Cycling States are all considered to be bipolar spectrum disorders.
References
- Weller, E.B.; Weller, R.A.;and Fristad, M.A. (1995). “Bipolar disorder in children: misdiagnosis, underdiagnosis and future directions,” Journal of the American Academy of Child and Adolescent Psychiatry34:709–714, 1995.
- Weller, E.B.; Weller, R.A.; Danielyan, A.K. (2004) “Mood disorders in prepubertal children.” In Wiener, J.M., Dulcan, M.D. (editors). Textbook of child and adolescent psychiatry. Washington, D,C.: American Psychiatric Publishing: 418.
- Akiskal, H.S. (1995). “Developmental pathways to bipolarity: are juvenile onset depressions pre-bipolar “Journal of the American Academy of Child and Adolescent Psychiatry . 34:754–763.
- Strober, M.; and Carlson, G. (1982). “Bipolar illness in adolescents with major depression: clinical, genetic and psychopharmacologic predictors in a three-to-four year prospective follow-up investigation,” Archives of General Psychiatry 39:549–555, 1982.
- Carlson, G.A.; Loney, J.; Salisbury, H.; Kramer, J.R.; Arthur, C. (2000). “Stimulant treatment in young boys with symptoms suggesting childhood mania: A report from a longitudinal study.” Journal of Child and Adolescent Psychopharmacology 10(3): 175–184.
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. These may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
These may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.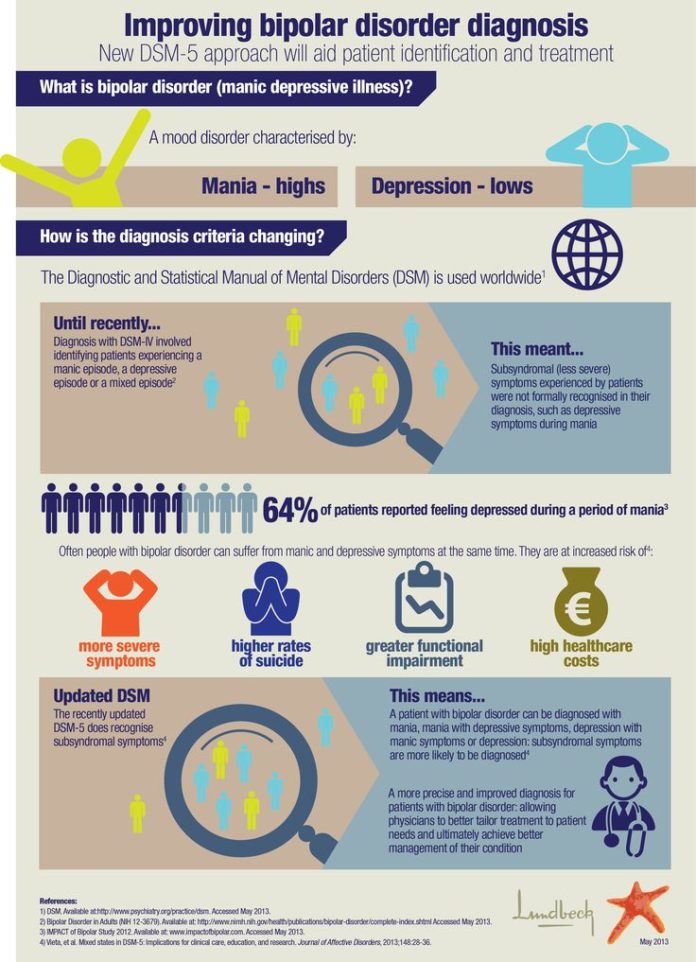 The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships.
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Differential diagnosis of bipolar disorder in children and adolescents
G.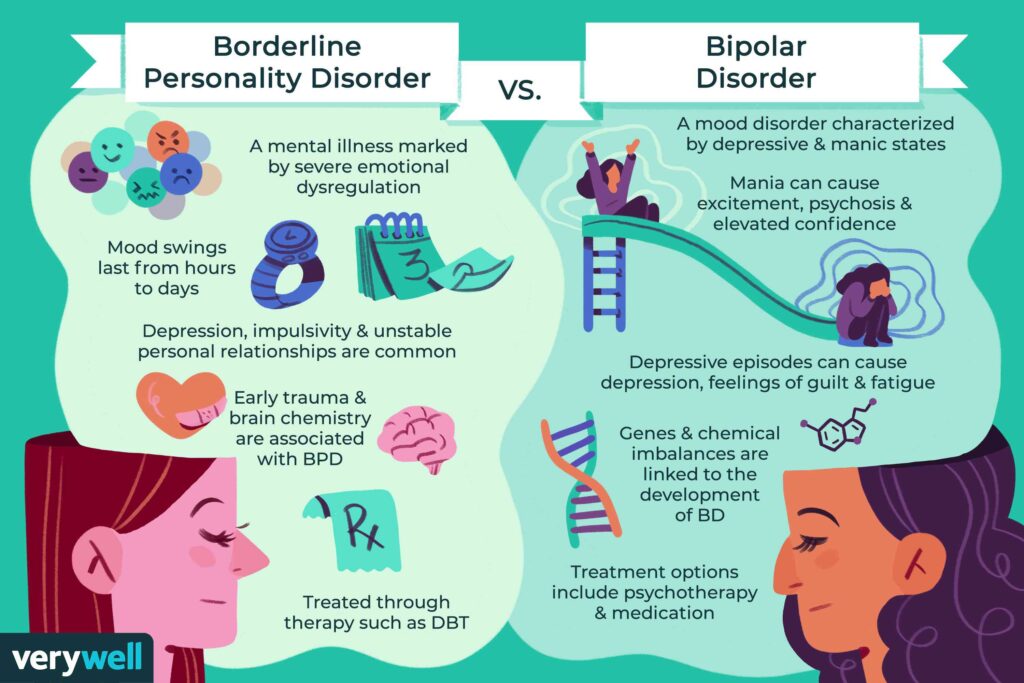 A. Carlson 1
A. Carlson 1
The differential diagnosis of bipolar affective disorder (BAD) in children and adolescents is a complex problem. The diagnosis of mania in BAD type I cannot be made without long-term follow-up. This disease leads to disability, but it must be distinguished from other similar pathologies. Having a family history of bipolar disorder may increase the risk of certain symptoms and behaviors that are characteristic of the onset of the disease, but a diagnosis should not be made on the basis of the history alone. Until there are biomarkers to confirm the diagnosis and targeted treatments for the disease, it makes sense to make a diagnosis of bipolar disorder in children and adolescents only temporarily, with the expectation that they will need to be re-examined in the future.
There are at least five challenges to the differential diagnosis of bipolar disorder in children and adolescents, which are discussed below.
- How to determine the subtype of bipolar disorder (differential diagnosis between mania and depression, between type I bipolar disorder and unspecified bipolar disorder)?
- The age of the child and the onset of the disease.
- Should we consider only those episodes of illness when mood changes and impaired functioning are clearly visible in comparison with the premorbid background, or should we consider, for example, outbursts of anger and severe irritability already as a change in mood?
- Who should provide information about symptoms of illness during mania, and when should data be collected after an attack or in the middle of an illness when it is easier to study?
- Influence of family history on diagnosis.
Not all children and adolescents can clearly tell about their lives, they do not always understand such abstract concepts as euphoria or a leap of ideas. Parents may underestimate or misinterpret the experiences of their children. Children spend most of their time at school, therefore, if a child is in a certain mood for most of the day every day, the teacher can notice changes in his behavior and mood, regardless of whether he / she has an idea of mania or depression and other diseases.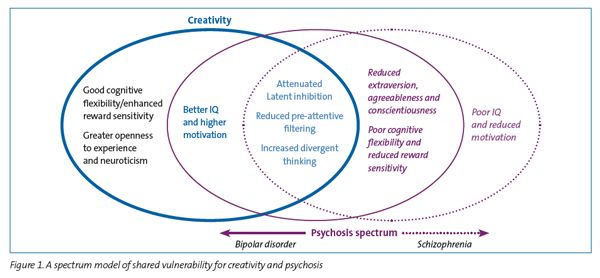
This article will focus mostly on mania and the differences between children and adolescents. An attempt will be made to describe a comprehensive approach to diagnosing a disease and to discuss the impact of different ways of providing information on making a diagnosis.
Post-puberty mania
Jeffrey was 14 years old when he first came to the attention of doctors. He is a sociable, energetic, purposeful, creative young man, at the same time he has many hobbies that he does not give up halfway, he approaches all his activities diligently and responsibly. However, in recent months, the guy has problems with concentration; at night he began to swim unannounced in a neighbor's pool, tried to reach President Bush in order to advise on further tactics for the war in Iraq, became short-tempered and implacable with his parents when they tried to put him to sleep. Following this period, which lasted several weeks, Geoffrey became physically weak, exhausted, lost interest in socializing with friends, in hobbies, practically stopped eating and felt extremely depressed.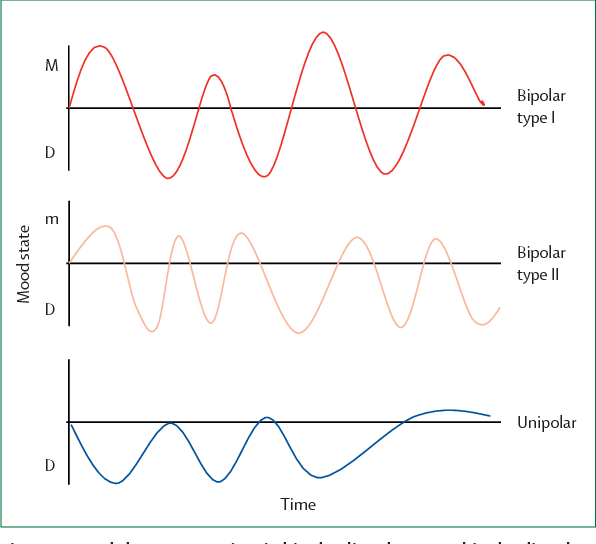 Upon further questioning, it was possible to find out other symptoms indicating mania without signs of depressive episodes in history. The task of the doctor was to find out what it is: "adolescent behavior" or psychopathology. The difficulty was that two weeks before the change in behavior, Jeffrey had suffered a head injury in football training without losing consciousness, and this may have affected the development of painful symptoms. Although it is clear that Geoffrey suffered a classic symptomatic episode of mania, some questions still need to be clarified.
Upon further questioning, it was possible to find out other symptoms indicating mania without signs of depressive episodes in history. The task of the doctor was to find out what it is: "adolescent behavior" or psychopathology. The difficulty was that two weeks before the change in behavior, Jeffrey had suffered a head injury in football training without losing consciousness, and this may have affected the development of painful symptoms. Although it is clear that Geoffrey suffered a classic symptomatic episode of mania, some questions still need to be clarified.
- How big is the contribution of Jeffrey's initially hyperthymic character traits to further behavior change [2]? A person with a hyperthymic character is usually cheerful, ebullient, talkative, playful, too optimistic, relaxed, carefree, energetic, full of short-term plans, often changes his circle of interests, interferes in everything, becoming annoying. All this applied to Geoffrey. Has he crossed the line of hypomania or even a manic episode? If he had been a quiet, modest person by nature before the excitement began, the issue would have been easily resolved in a positive direction.
 At the same time, such violations and subsequent depression do not fit only into the framework of character traits.
At the same time, such violations and subsequent depression do not fit only into the framework of character traits. - Did the head injury matter? There is evidence of an association between brain injury and the onset of mania [3]. There is also a condition called "personality change after traumatic brain injury", which describes patients with disinhibited behavior [4]. In early versions of the DSM, this was the term "organic affective disorder".
- Is there any evidence of Jeffrey's substance abuse? In adolescents, a first episode of mood disturbance raises questions about the presence of alcohol or drug dependence [5]. So, with the abuse of marijuana, alcohol and other drugs, they may develop psychotic or affective symptoms. Although a positive test for toxic substances in the body helps to confirm the fact of drug use, a negative result does not at all indicate the absence of addiction. Moreover, manic symptoms may continue for weeks after the patient has stopped taking the substances.
 Sometimes it is difficult to figure out how big the role of drug use in the occurrence of mood changes is, whether it brings the onset of the disease closer and whether it prolongs its course, because it could proceed faster, or whether this is completely insignificant [6].
Sometimes it is difficult to figure out how big the role of drug use in the occurrence of mood changes is, whether it brings the onset of the disease closer and whether it prolongs its course, because it could proceed faster, or whether this is completely insignificant [6].
11-27% of adolescents admitted to hospital for their first psychotic episode were previously diagnosed with type I bipolar disorder [7]. However, during the first episode, it is extremely difficult to accurately determine the diagnosis due to the confusion and variability of symptoms over time. Example: Dennis is 16 years old, he has not slept for three days, he has a feeling that he can rule the world; the boy wrote notes in which he argued that all objects around had their own purpose and connection with each other, including the German swastika, the Egyptian pyramids and the dove of peace. He experienced physical arousal, was verbose, paranoid thoughts grew that the psychiatrist wanted to harm him. Over the next 6 months, on antipsychotic and lithium therapy, the affective symptoms subsided, but a sense of thought transmission and related thinking disorders appeared, which were persistent. After 10 years, she was diagnosed with schizoaffective disorder due to chronic thought disorder and persistent psychotic symptoms. The medication improved the patient's mood but did not affect the negative symptoms.
Over the next 6 months, on antipsychotic and lithium therapy, the affective symptoms subsided, but a sense of thought transmission and related thinking disorders appeared, which were persistent. After 10 years, she was diagnosed with schizoaffective disorder due to chronic thought disorder and persistent psychotic symptoms. The medication improved the patient's mood but did not affect the negative symptoms.
Despite the fact that almost 70% of patients with a first manic psychotic episode are diagnosed with bipolar disorder (sometimes as an intermediate) within 10 years after the onset of the disease, in this case, the presence of symptoms of the first rank according to Schneider, as well as premorbid decline in social functioning [8]. Harbingers of an unfavorable prognosis are also considered to be depressive manifestations, childhood psychopathology, and early onset of the disease [9].
Mania in children
The diagnosis of mania before the age of 10 years is much more controversial than in adolescents [10].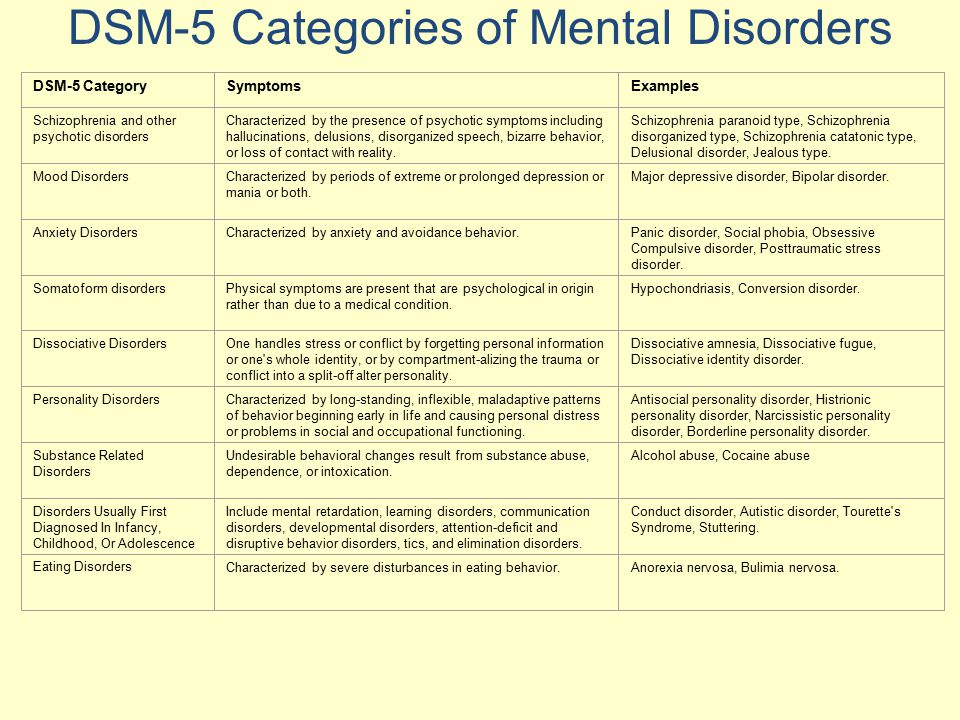 In order to apply the criteria for bipolar disorder to children, the DSM-IV-TR has updated the list of symptoms of mania to include the most common manifestations of the disease in young children. The unresolved question remains whether these children grow up healthy until the first episodes of depression or mania (as in the case of Jeffrey: acute onset of mania, isolated episodes, no comorbid pathology), or whether these are continuous mood swings against the background of depression - close to those observed in patients enrolled in the Bipolar Disorder Systematic Care Program (STEP-BD) study [11]? Or perhaps their prognosis is completely different - patients grow up and do not experience any episodes of altered mood in the future [12]?
In order to apply the criteria for bipolar disorder to children, the DSM-IV-TR has updated the list of symptoms of mania to include the most common manifestations of the disease in young children. The unresolved question remains whether these children grow up healthy until the first episodes of depression or mania (as in the case of Jeffrey: acute onset of mania, isolated episodes, no comorbid pathology), or whether these are continuous mood swings against the background of depression - close to those observed in patients enrolled in the Bipolar Disorder Systematic Care Program (STEP-BD) study [11]? Or perhaps their prognosis is completely different - patients grow up and do not experience any episodes of altered mood in the future [12]?
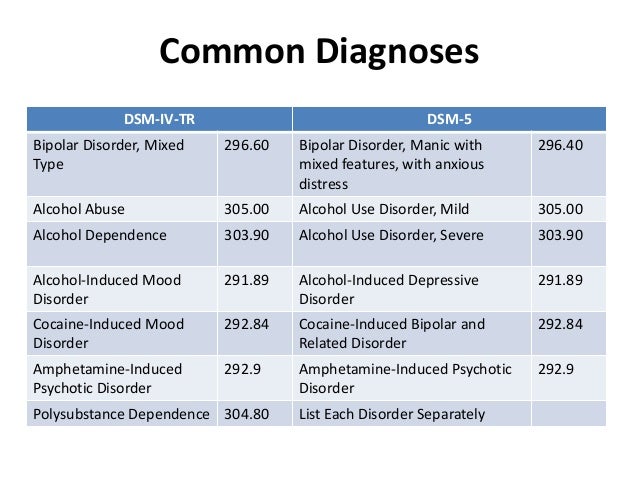
The insidiousness and complexity of diagnosing early forms of bipolar disorder lies in the different interpretation of the criteria. In the "classic" cases of mania, there are practically no contradictions: the onset of the disease is clearly monitored, and manic symptoms, consistently manifesting themselves, do not allow mania to be confused with another psychopathology.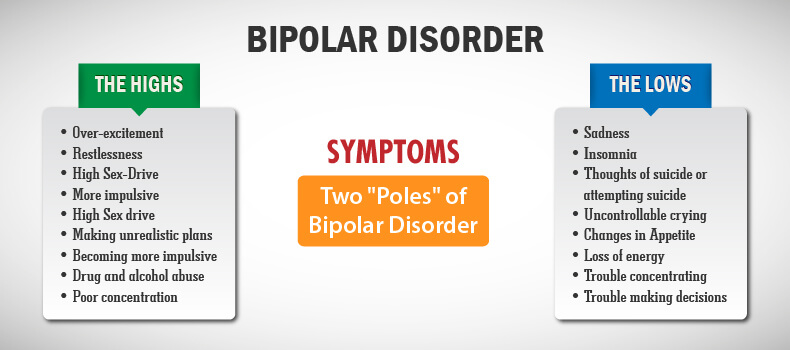 In the course of the disease in a less “classical way”, much more discrepancies appear [13]. The criteria may be reliable for a certain category of patients, but do not guarantee accuracy and do not apply to other groups. According to the DSM-IV-TR, a manic episode is defined as a distinct time span of the presence of a characteristic set of symptoms. Unfortunately, there is no agreement in understanding the boundaries of this time period [14]. Therefore, the criteria for mania will be subject to some changes in the next version of the DSM-5 (see www.dsm5.org). The document states that "doctors have not been able to agree on what is still considered an episode of mania, especially a lot of controversy in the literature in the field of child psychiatry."
In the course of the disease in a less “classical way”, much more discrepancies appear [13]. The criteria may be reliable for a certain category of patients, but do not guarantee accuracy and do not apply to other groups. According to the DSM-IV-TR, a manic episode is defined as a distinct time span of the presence of a characteristic set of symptoms. Unfortunately, there is no agreement in understanding the boundaries of this time period [14]. Therefore, the criteria for mania will be subject to some changes in the next version of the DSM-5 (see www.dsm5.org). The document states that "doctors have not been able to agree on what is still considered an episode of mania, especially a lot of controversy in the literature in the field of child psychiatry."
According to the Mood Disorders Research Group, the language in the DSM-IV regarding the criteria for mania and hypomania has only led to confusion. Therefore, the goal of the DSM change proposal would be to provide more clarity to ensure more accurate, consistent diagnosis.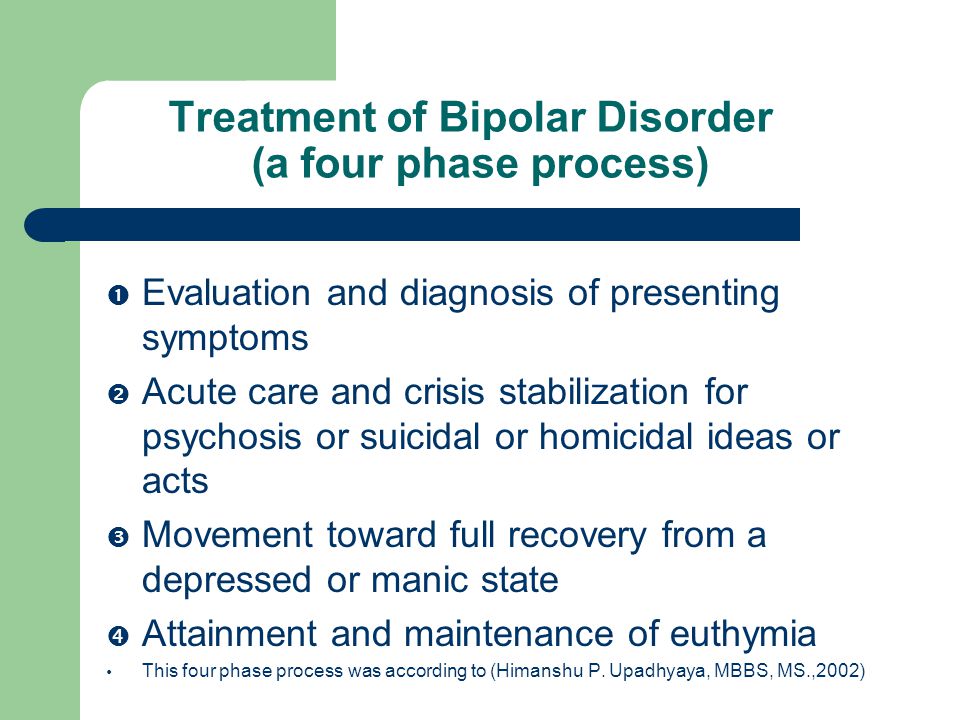 At the same time, it is necessary to rely on the experience of previous versions of the DSM, taking into account the modern dynamic characteristics of the disease. Criterion A would be: Unusual and persistent high spirits, expansiveness, irritability, unaccustomed and persistent energy, elation, lasting at least 1 week and lasting almost daily for most of the day (duration is not important if hospitalization is necessary) for a certain period of time.
At the same time, it is necessary to rely on the experience of previous versions of the DSM, taking into account the modern dynamic characteristics of the disease. Criterion A would be: Unusual and persistent high spirits, expansiveness, irritability, unaccustomed and persistent energy, elation, lasting at least 1 week and lasting almost daily for most of the day (duration is not important if hospitalization is necessary) for a certain period of time.
An accurate understanding of the symptoms is essential when discussing the differential diagnosis of mania. While it is recognized that depressive symptoms may occur independently of a depressive episode or clinical depression, manic symptoms have hardly been assessed in this way. Previously published results of a study in 1988 [15], as well as a number of other studies, confirmed that the symptoms of mania occur much more often than the manic episode itself, and cause serious damage to health. However, these symptoms are nonspecific and occur in various pathologies [16, 17].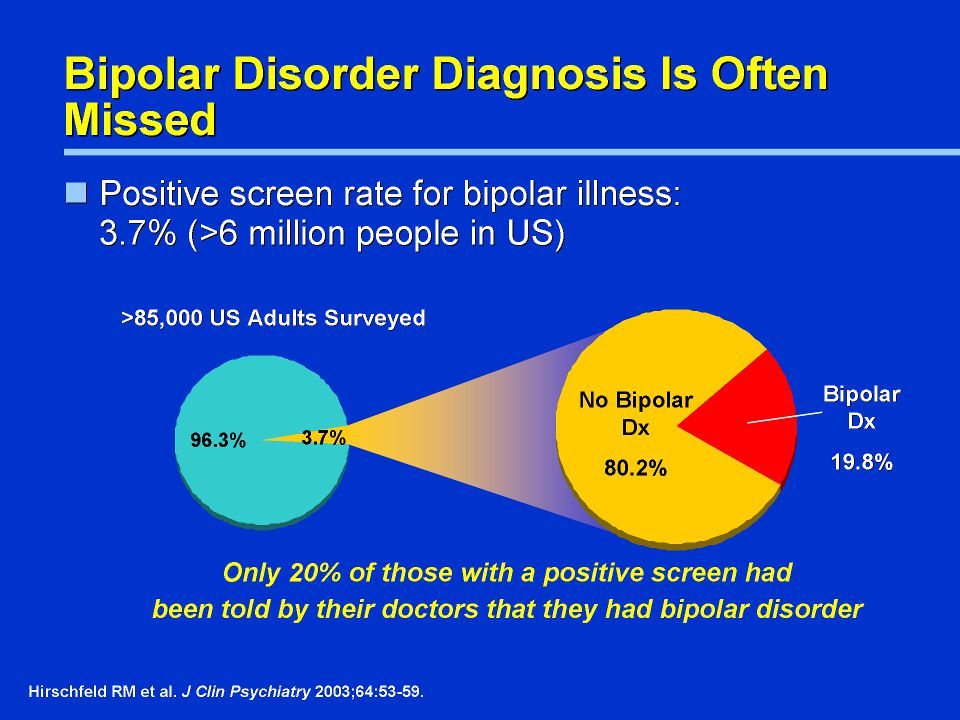 Without knowing exactly whether an episode occurred or not (the time of onset and end of changes in the patient's "habitual behavior"), without data on early childhood, about what this "habitual behavior" was, it is extremely difficult to distinguish mania from other childhood illnesses that occur with irritability and agitation. Attention Deficit Hyperactivity Disorder (ADHD) is a disease that is most often confused with mania in children. A significant part of the symptoms are the same: in both conditions there are distractibility, impulsiveness, hyperactivity, accelerated and excessive speech [19]. Yet children with mania have more symptomatic symptoms than those with uncomplicated ADHD. In such children, as a rule, the violations are deeper; another pathology (comorbid conditions) is necessarily found according to the criteria [20, 21]. Curiously, when comparing children with symptoms of mania and children with ADHD, complicated in both cases by a similar comorbid pathology, all differences disappear [22, 23].
Without knowing exactly whether an episode occurred or not (the time of onset and end of changes in the patient's "habitual behavior"), without data on early childhood, about what this "habitual behavior" was, it is extremely difficult to distinguish mania from other childhood illnesses that occur with irritability and agitation. Attention Deficit Hyperactivity Disorder (ADHD) is a disease that is most often confused with mania in children. A significant part of the symptoms are the same: in both conditions there are distractibility, impulsiveness, hyperactivity, accelerated and excessive speech [19]. Yet children with mania have more symptomatic symptoms than those with uncomplicated ADHD. In such children, as a rule, the violations are deeper; another pathology (comorbid conditions) is necessarily found according to the criteria [20, 21]. Curiously, when comparing children with symptoms of mania and children with ADHD, complicated in both cases by a similar comorbid pathology, all differences disappear [22, 23]. A diagnostic question arises: either children with symptoms of mania suffer from bipolar disorder in combination with ADHD, or ADHD occurs against a background of increased emotional or protest isolation.
A diagnostic question arises: either children with symptoms of mania suffer from bipolar disorder in combination with ADHD, or ADHD occurs against a background of increased emotional or protest isolation.
Emotional/protest behavior in ADHD is considered among the "associated symptoms" in the DSM-III/IV. The DSM-IV-TR states that the emotional component of the illness includes low frustration tolerance, irritability, temper tantrums, mood swings, dysphoria, and low self-esteem. All symptoms fit within the framework of mood. The emotional component is present in both manifestations of ADHD - impaired attention and hyperactivity. The symptoms of ADHD caused by impaired attention may be initially associated with a defect in the sphere of regulation and control, while the symptoms of hyperactivity and impulsivity may arise from disturbances in the emotional sphere [24]. It is only obvious that in children with both bipolar disorder and ADHD complicated by emotional disorders, disorders are much more clearly manifested, which was verified by comparing them with cases of ADHD without complications in the course of cross-sectional and longitudinal studies [20, 25].
ADHD and bipolar disorder often coexist. A recently published study titled Longitudinal Mania Symptom Study explores the issue of ADHD and bipolar disorder in great detail [16, 20]. Researchers compared children aged 6 to 12 years (n = 621) whose parents tested positive for manic symptoms on the General Behavior Questionnaire with children whose parents did not score enough (n = 86) [26]. Of the total number of children (n = 707), the majority (59.5%) had ADHD, 6.4% had a bipolar disorder without ADHD, 16.5% had both, and 17.5% were healthy. The spectrum of bipolar disorders evenly consisted of cases of type I bipolar disorder and unspecified bipolar disorder, there was also a small number of type II bipolar disorder. As in previous studies [1, 15], children with symptoms of mania were not found to have bipolar spectrum disorders. Of 162 children with bipolar spectrum disorders, the majority (72.2%) also had ADHD. According to the results of a survey of parents, it turned out that in the presence of a combination of these diseases, the symptoms are richer than in the case of each of the pathologies separately.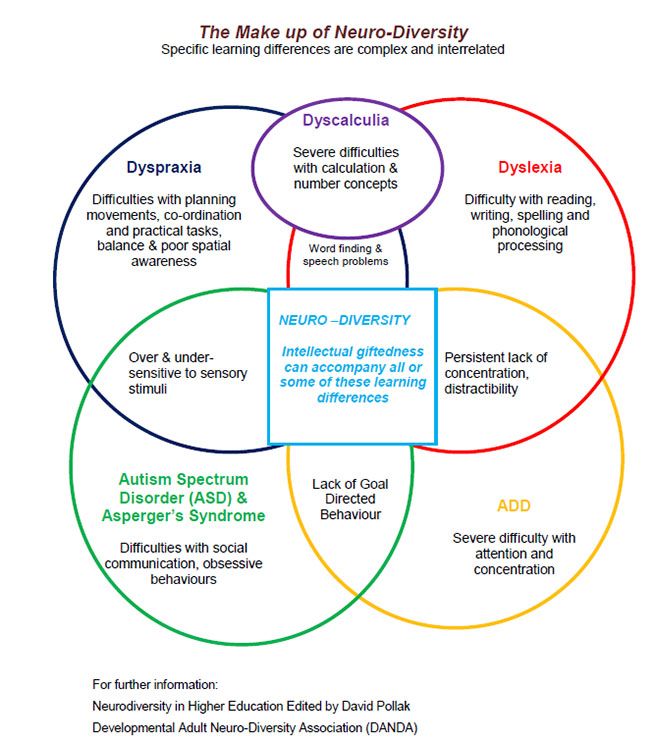 The diagnosis was made according to the children's diagnostic scale for affective disorders and schizophrenia [27]. Although the authors did not specify, some believe that the data were based more on parental responses, as teachers often disagreed with the results [20]. Yet much attention has been paid to distinguishing chronic symptoms from acute or intermittent ones. It is this approach that helps in differentiating mania and ADHD from the joint course of these diseases. In addition to taking an anamnesis, which may include episodes, a scrupulous examination of all overlapping symptoms is necessary. The symptoms of mania and ADHD, mixed together, can give the following picture:
The diagnosis was made according to the children's diagnostic scale for affective disorders and schizophrenia [27]. Although the authors did not specify, some believe that the data were based more on parental responses, as teachers often disagreed with the results [20]. Yet much attention has been paid to distinguishing chronic symptoms from acute or intermittent ones. It is this approach that helps in differentiating mania and ADHD from the joint course of these diseases. In addition to taking an anamnesis, which may include episodes, a scrupulous examination of all overlapping symptoms is necessary. The symptoms of mania and ADHD, mixed together, can give the following picture:
- goofy, disinhibited behavior in a child with ADHD who tries to be funny without regard to the circumstances, or is simply high spirits;
- impulsiveness or desire to enjoy without considering the consequences;
- refusal to go to bed on time or simply reduced need for sleep;
- worsening of subtle symptoms of ADHD due to increased workload in primary or secondary school, or the onset of mood disturbances;
- exacerbation of ADHD symptoms, including greater protest, irascibility, stupid behavior, as part of poor relationships within the family and school circles, among peers;
- intrusive, slurred, or bizarre speech in children with ADHD or autism spectrum disease speech problems may resemble the thought jitters or thought disturbances of mania;
- "hallucinations" in highly anxious children, or symptoms incongruent to affect in mania.
Children with RSA due to impaired emotional control can be confused with those with mania [28]. And it's not just their impulsiveness and excessive activity. Speech disorders may also look like a thought disorder, especially for a clinician with little experience in differential diagnosis [29]. As in the case of ADHD, a good history can help distinguish which symptoms are chronic and which first appeared as part of an altered state. Interestingly, children with autism and bipolar disorder (including the most classic episodic variants of bipolar disorder) have always been considered together [30], while children with a general developmental disorder have almost always been overlooked in the studies.
Dysregulation of mood
At the age of 11, Linda was brought to the doctor by her parents due to mood swings, namely frequent outbursts of anger [13].
From early childhood she suffered from ADHD, the symptoms of which were almost continuous during treatment with stimulants. By the 5th grade, the girl became irritable, disobedient, spiteful towards her parents, ignoring their concern about her school grades. There was a feeling of grandiosity with ideas about the uselessness of study. Linda visited porn sites and stayed up late in front of the computer supposedly with online friends, lagged behind in her studies and shunned her peers. Temper at school did not manifest itself, but the symptoms of ADHD were evident. Parents during the history taking confirmed the presence of symptoms resembling mania. Linda herself complained of dysphoria, irritability, trouble concentrating, low self-esteem, and occasional suicidal thoughts. Among other things, there were serious quarrels at home, but without violence. Linda's differential diagnosis based on DSM-IV criteria would include ADHD and incipient oppositional conduct disorder, major depressive disorder, secondary adjustment disorder with impaired social, academic and home connections, and an episode of mixed mania.
By the 5th grade, the girl became irritable, disobedient, spiteful towards her parents, ignoring their concern about her school grades. There was a feeling of grandiosity with ideas about the uselessness of study. Linda visited porn sites and stayed up late in front of the computer supposedly with online friends, lagged behind in her studies and shunned her peers. Temper at school did not manifest itself, but the symptoms of ADHD were evident. Parents during the history taking confirmed the presence of symptoms resembling mania. Linda herself complained of dysphoria, irritability, trouble concentrating, low self-esteem, and occasional suicidal thoughts. Among other things, there were serious quarrels at home, but without violence. Linda's differential diagnosis based on DSM-IV criteria would include ADHD and incipient oppositional conduct disorder, major depressive disorder, secondary adjustment disorder with impaired social, academic and home connections, and an episode of mixed mania.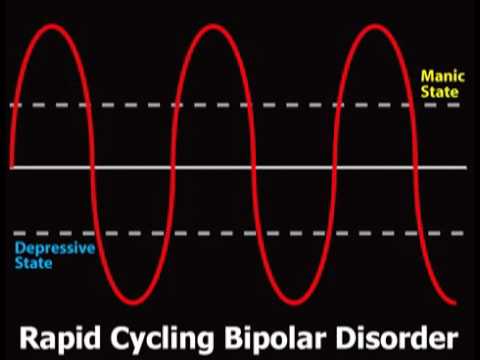
Mood disturbances/lability are present in many cases as an important component of a number of conditions [31]. Non-professionals often use the term "bipolar" to describe mood swings, that is, sudden changes that are inexplicable to an outsider. We are talking about the sudden onset of a bad mood as a cause of irritability. When experiencing a manic episode, both adults and children are often irritable. However, the question remains: do extremely irascible children suffer from mania, or is it a character (irritability as a trait), which casts doubt on the diagnosis of such conditions as depression, anxiety, schizophrenia, etc., in which the symptom of irritability plays a significant role [32].
Depressive and Anxiety Disorders
Irritability as a symptom is of course important not only in mania, but also in depression (equally in major depression and dysthymia) and anxiety disorders (including post-traumatic stress disorder, obsessive-compulsive disorder, social phobia, avoidance and generalized anxiety disorder). As with ADHD, the question "is it depression or anxiety?" not worth it, rather a combination of both. Of particular difficulty is how to distinguish between mixed mania, or "rapid" cycles, and agitated depression. Some view agitated depression as a bipolar disorder [33]. Longitudinal pro- and retrospective trials show that the predominantly depressive course of the disease from the bipolar spectrum is more likely to become chronic and more difficult to treat than manic [9, 34, 35]. The question that arises in the course of a prospective study of a group of children is this: how many children "outgrow" mania and go into depression or even remission [12, 36]?
As with ADHD, the question "is it depression or anxiety?" not worth it, rather a combination of both. Of particular difficulty is how to distinguish between mixed mania, or "rapid" cycles, and agitated depression. Some view agitated depression as a bipolar disorder [33]. Longitudinal pro- and retrospective trials show that the predominantly depressive course of the disease from the bipolar spectrum is more likely to become chronic and more difficult to treat than manic [9, 34, 35]. The question that arises in the course of a prospective study of a group of children is this: how many children "outgrow" mania and go into depression or even remission [12, 36]?
Irritability and hyperactivity are also inherent in anxiety. In adults and adolescents, bipolar disorder is often accompanied by painful anxiety. In adults, the presence of anxiety symptoms reduces the likelihood of recovery from bipolar depression, prolongs the course of the disease, and increases the likelihood of a relapse [37].
In children, anxiety disorder often precedes the onset of mania, in which case the manic episode would be considered a comorbid disorder. If anxiety has not previously arisen, it is quite acceptable to consider it within the framework of a manic episode, not considering it as a comorbid disorder [38]. In children and adolescents, anxiety is most often associated with type II bipolar disorder. These patients often have parallel longer and more severe episodes of depression, and a richer family history of depression than children and adolescents without anxiety symptoms as a comorbid pathology [38].
Mood regulation disorder with disruptive features
Leibenluft and the National Institute of Mental Health (NIMH) Intramural Program on Mood Disorders in an attempt to better understand the similarities and differences between chronic, severe irritability and It was proposed to single out such a condition as “severe mood regulation disorder” (SMDD) as a more classic, episodic course, bipolar disorder [32]. This condition is characterized by persistent irritability with frequent outbursts of anger and is more commonly referred to as mania, schizophrenia or schizophrenia spectrum disorder, general developmental disorder, post-traumatic stress disorder, substance abuse, organic or neurological disorder. In a sample of 146 children, 75% had ADHD and oppositional disorder as a comorbid disorder, and more than half (58%) had an episode of anxiety disorder at least once in their lives. Although prospective studies have not been conducted in children with CCHD, extrapolating data from other studies [39-41], it can be assumed that depression is the basis of such behavioral disorders. Thus, the DSM-5 Mood Disorders Study Group is using data from these studies to add HDD to the new guidelines under mood disorders. This condition has been termed Mood Disorder with Disruptive Traits (MDD) (see www.dsm5.org).
This condition is characterized by persistent irritability with frequent outbursts of anger and is more commonly referred to as mania, schizophrenia or schizophrenia spectrum disorder, general developmental disorder, post-traumatic stress disorder, substance abuse, organic or neurological disorder. In a sample of 146 children, 75% had ADHD and oppositional disorder as a comorbid disorder, and more than half (58%) had an episode of anxiety disorder at least once in their lives. Although prospective studies have not been conducted in children with CCHD, extrapolating data from other studies [39-41], it can be assumed that depression is the basis of such behavioral disorders. Thus, the DSM-5 Mood Disorders Study Group is using data from these studies to add HDD to the new guidelines under mood disorders. This condition has been termed Mood Disorder with Disruptive Traits (MDD) (see www.dsm5.org).
In the absence of an episodic course, differentiation of RRND from mania should not be difficult. In addition, the onset of the disease most often occurs between the ages of 6 and 10, which makes it possible to protect temperamental preschoolers from making a “serious diagnosis” and at the same time regard the disorder as childish. It is the chronic course of the disease (that is, the symptoms last at least 1 year) that does not allow children to be diagnosed with RRND. These are the children who respond to acute stress and could be diagnosed with an adjustment disorder with behavioral or mood disturbances. The diagnosis of RRND, when correctly made, usually means a serious condition and loss or decrease in working capacity [31].
In addition, the onset of the disease most often occurs between the ages of 6 and 10, which makes it possible to protect temperamental preschoolers from making a “serious diagnosis” and at the same time regard the disorder as childish. It is the chronic course of the disease (that is, the symptoms last at least 1 year) that does not allow children to be diagnosed with RRND. These are the children who respond to acute stress and could be diagnosed with an adjustment disorder with behavioral or mood disturbances. The diagnosis of RRND, when correctly made, usually means a serious condition and loss or decrease in working capacity [31].
The main diagnostic difficulty in the case of RRND is the fact that irritability and irascibility are nonspecific signs [42]. Children who constantly show temper tantrums (whether chronically irritable or not) end up in emergency hospitals, psychiatric and other supervised and special educational institutions. The need for diagnosis is dictated by the need to count such patients, provide them with proper treatment and inclusion in the insurance list. Typically, these short-tempered children fall into the category of oppositional disorder or conduct disorder, and both categories are not included in the insurance list of illnesses, as they are considered within the framework of "family" or "social" problems. Due to the lack of a reliable and accurate coding for such outbursts of anger, doctors are forced to assign them the category BAD, which in turn prevents a serious understanding of the nature of these outbursts [43].
Typically, these short-tempered children fall into the category of oppositional disorder or conduct disorder, and both categories are not included in the insurance list of illnesses, as they are considered within the framework of "family" or "social" problems. Due to the lack of a reliable and accurate coding for such outbursts of anger, doctors are forced to assign them the category BAD, which in turn prevents a serious understanding of the nature of these outbursts [43].
The question arises whether temper tantrums are a subset or more severe manifestation of mood swings (tantrums) in early childhood patients [44, 45]? Interestingly, both states are generally similar, differing only in duration (20 and 5 minutes, respectively), as well as in more rude behavior (children can kick, hit, throw, spit) and the degree of harm that a child in a tantrum state can cause, due to that these children are older (from 7 to 17 years). There are no data describing the characteristics of outbursts of anger in various pathologies, that is, the anger that occurs during a panic attack is outwardly similar to that in a manic episode, oppositional disorder, depression, etc. [46]. Many clinicians worry that this diagnosis will be misused to the same extent as the diagnosis of bipolar disorder [43]. Mistakes can be avoided by following the algorithm correctly, for example, if you take outbursts of anger as a key and distinguishing feature for a number of conditions where they are present, just as types of catatonia allow you to distinguish between a number of pathologies. For example, the diagnosis of "ADHD with outbursts of anger" - the key ones in this case, could be regarded as an independent diagnosis of "outbursts of anger", which would allow for more complete treatment.
[46]. Many clinicians worry that this diagnosis will be misused to the same extent as the diagnosis of bipolar disorder [43]. Mistakes can be avoided by following the algorithm correctly, for example, if you take outbursts of anger as a key and distinguishing feature for a number of conditions where they are present, just as types of catatonia allow you to distinguish between a number of pathologies. For example, the diagnosis of "ADHD with outbursts of anger" - the key ones in this case, could be regarded as an independent diagnosis of "outbursts of anger", which would allow for more complete treatment.
Interview discrepancy
A mandatory minimum in child and adolescent psychiatry is the history taking of the parent/guardian and the child. In the case of behavioral disorders, as in ADHD, it is also important to seek the opinion of teachers. Unfortunately, it turned out that the coincidences in the survey data are very small. The measure of kappa correspondence between the words of the child and the parent in the case of mania or depressive symptoms is usually below 0.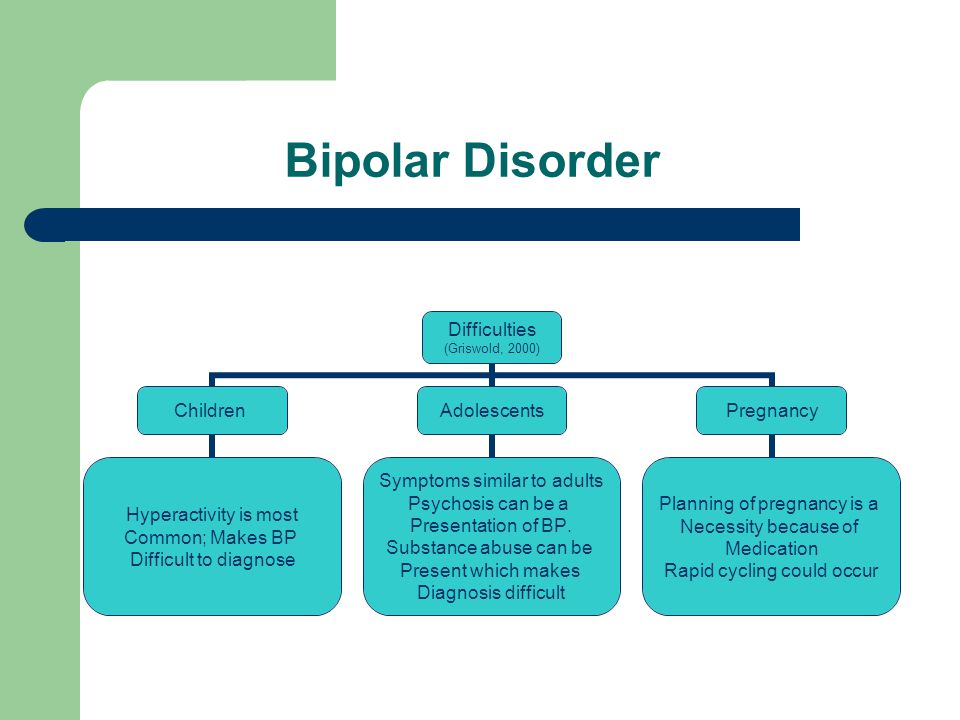 2.
2.
At the same time, Biederman et al. found that in 62.7% of cases of mania, both parent and child admitted to having manic symptoms [47]. Data from Tillman et al. differed a little - 49.5% [48]. However, Tillman in the study showed that the highest compliance rates of the survey results are characteristic of ADHD symptoms (80% for accelerated speech, 91.4% for hyper-energy, 85.9% for motor activity), 75.8% for irritable mood, scores were significantly lower for other symptoms of mania (42.2% elevated mood, 32.5% sense of grandeur, 35.8% thought racing, 34.4% disinhibited behavior, 16.2% reduced need for sleep, 21.4% - psychotic phenomena). In addition, children were much less likely to admit to specific symptoms of mania than their parents. Hence the simple explanation for such frequent disputes over the diagnosis: mania or ADHD, since, for the most part, when assessing the mental state of a child, specialists are guided by the interpretation of parents.
In the study of bipolar disorder, researchers have never set out to determine the value of any other sources of information about the child's manic behavior, other than parents.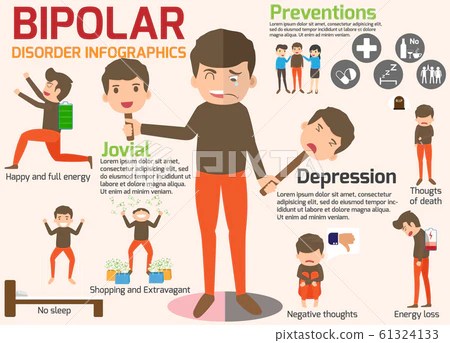
The correlation of data received from parents and teachers approaches r = 0.3 [49]. Carlson and Blader report that where teacher and parental indications of mania symptoms (as measured by the Childhood Mania Rating Scale) were highly consistent, logistic regression revealed a 10-fold prevalence of other diagnoses associated with exogenous disorders (ADHD). , oppositional disorder, behavioral disorder, or a combination of these diseases) [1, 50]. And in children with bipolar spectrum disorders, the degree of agreement between parents and teachers was higher. In contrast, in the spectrum of endogenous diseases (anxiety and depressive disorders), there was a 3.7 times greater discrepancy between the information received from teachers and parents using the children's mania rating scale.
This study used a more advanced system for evaluating information from parents, children, and teachers, in addition to a simple survey, often without a specific structure, in making a diagnosis.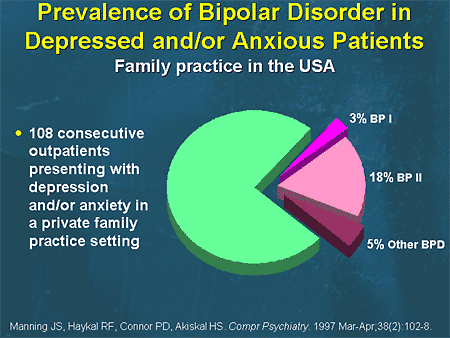 More research is needed to explain why a child's severe condition lasting weeks is noticed by parents but not by teachers.
More research is needed to explain why a child's severe condition lasting weeks is noticed by parents but not by teachers.
Family history
Obviously, bipolar disorder has a hereditary component [51]. A long-published meta-analysis of studies has shown that children of parents with bipolar disorder are 2.7 times more likely to develop a mental disorder and 4 times more likely to have a mood disorder than children of healthy parents [52]. Recent trials have confirmed these figures [53]. However, it is interesting that the risk of developing general psychopathological disorders turned out to be much higher than type I bipolar disorder. For example, Hillegers et al. found that by the age of 21, among Dutch teenagers at high risk, 3% had type I bipolar disorder, 10% had bipolar disorder, but 59% had some kind of psychopathology [54]. Although high-risk children with mood disorders are more likely than healthy children to develop bipolar disorder in adulthood, they are also at significant risk of developing a wide range of other diseases [55].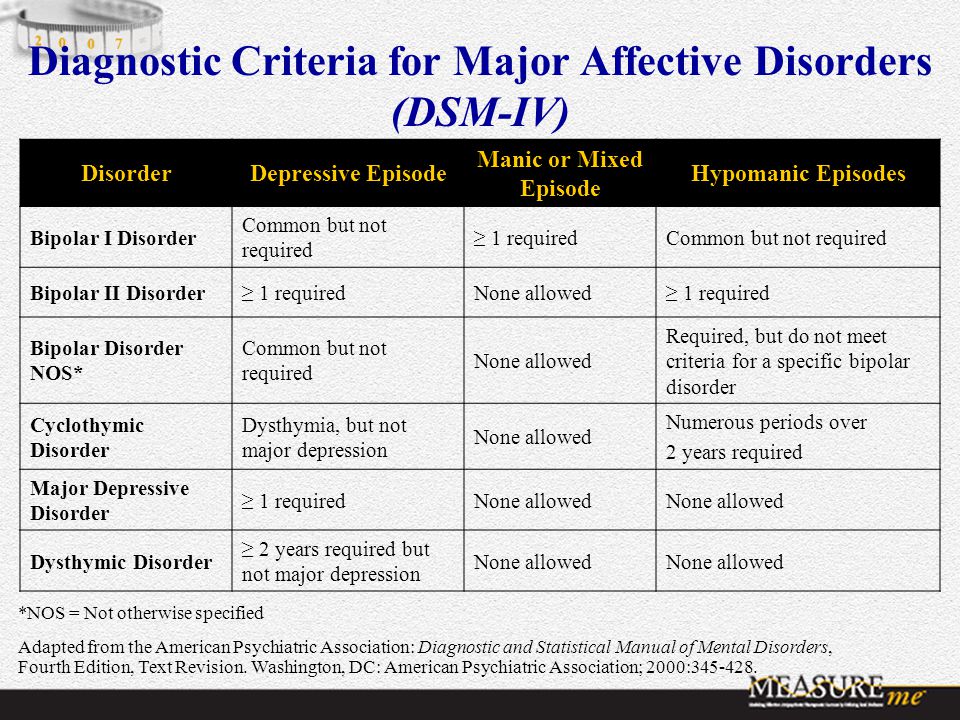
Many studies focusing on high-risk groups compare children of parents with bipolar disorder with those of a control group whose parents do not have a mental disorder, indicating a difference in risk. However, children from families with any other mental illness, such as ADHD, autism, learning disabilities, other mood disorders and schizophrenia, also come to the attention of doctors. It is believed that children whose parents responded well to lithium therapy have a milder disease course than those whose parents are resistant to lithium [56]. This could help in the selection of therapy in the case of a diagnosis of type I bipolar disorder. And yet, the presence of a diagnosis in the parents does not mean the presence of the disease in the child.
Finally, the age at risk for bipolar disorder is significantly stretched. In a Danish population study that included a group of children whose parents had at least once been hospitalized with bipolar disorder, it was found that by the age of 53, among "children" with a parent who was ill, the risk was 4.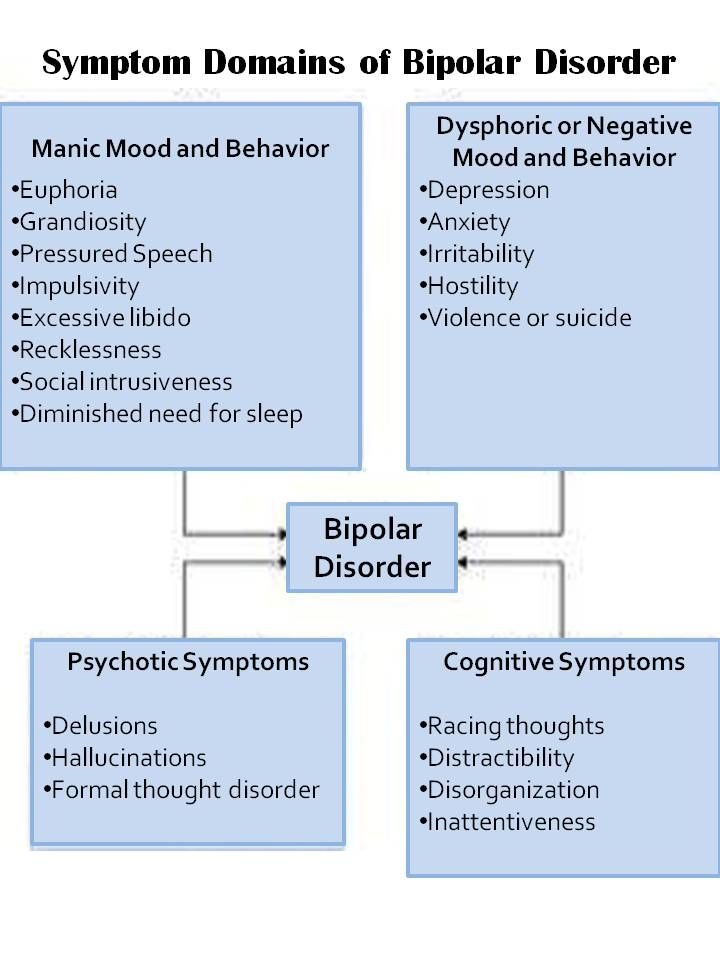 4% compared with a 0.48% risk in those who had parents without bipolar disorder. The difference in risk among children under 20 years of age is negligible [57]. From these indicators, it follows that suspicions about bipolar disorder are increasing, but the fact of a family history cannot be taken as an absolute criterion for making such a diagnosis, especially if the child does not have other diagnostic components of the disease.
4% compared with a 0.48% risk in those who had parents without bipolar disorder. The difference in risk among children under 20 years of age is negligible [57]. From these indicators, it follows that suspicions about bipolar disorder are increasing, but the fact of a family history cannot be taken as an absolute criterion for making such a diagnosis, especially if the child does not have other diagnostic components of the disease.
Conclusions
Although Type I mania/BAD often begins at an early age, it is better to delay diagnosis for more than one year. This is a serious condition that reduces the ability to work, but there are other diseases from which it should be able to distinguish. Psychosis, substance abuse, and agitated unipolar depression present great difficulties in making a differential diagnosis in adolescents. Defining executive dysfunctions in children is also challenging. A multilateral survey increases the chances of a correct diagnosis, although it is necessary to clearly understand the difference and correctly compare the answers of parents, teachers and the child himself. Having a family history of illness may increase the risk of certain symptoms and behavioral problems associated with the onset of bipolar disorder, but the diagnosis should not be made based on the history. In addition, difficult children are most often from difficult families.
Having a family history of illness may increase the risk of certain symptoms and behavioral problems associated with the onset of bipolar disorder, but the diagnosis should not be made based on the history. In addition, difficult children are most often from difficult families.
Until biomarkers are identified to accurately confirm the diagnosis and drugs that are exclusively specific for this pathology, it makes sense to diagnose bipolar disorder in children and adolescents only temporarily, with the expectation of the need for re-examination in the future [58]. The assertion that a child is ill for life requires more evidence than we have.
Literature
- Carlson G.A., Blader J.C. Diagnostic implications of informant disagreement for manic symptoms // J Child Adolesc Psychopharmacol. - 2011. - 21. - R. 399-405.
- Akiskal H.S., Khani M.K., Scott-Strauss A. Cyclothymic temperamental disorders // Psychiatr Clin North Am. - 1979. - 2. - R. 527-554.
- Jorge R.
 E., Robinson R.G., Starkstein S.E. et al. Secondary mania following traumatic brain injury // Am J Psychiatry. - 1993. - 150. - R. 916-921.
E., Robinson R.G., Starkstein S.E. et al. Secondary mania following traumatic brain injury // Am J Psychiatry. - 1993. - 150. - R. 916-921. - Max J.E., Robertson B.A., Lansing A.E. The phenomenology of personality change due to traumatic brain injury in children and adolescents // J Neuropsychiatry Clin Neurosci. - 2000. -13. - R. 161-170.
- Wilens T.E., Biederman J., Millstein R.B. et al. Risk for substance use disorders in youths with child- and adolescent-onset bipolar disorder // J Am Acad Child Adolesc Psychiatry. - 1999. - 38. - R. 680-685.
- Carlson G.A., Bromet E.J., Lavelle J. Medication treatment in adolescents vs. adults with psychotic mania // J Child Adolesc Psychopharmacol. - 1999. - 9. - R. 221-231.
- Carlson G.A., Naz B., Bromet E.J. Phenomenology and assessment of adolescent-onset psychosis: observations from a first admission psychosis project. In: Findling R.L., Schultz S.C. (eds). Juvenile onset schizophrenia. - Baltimore: Johns Hopkins University Press, 2005.
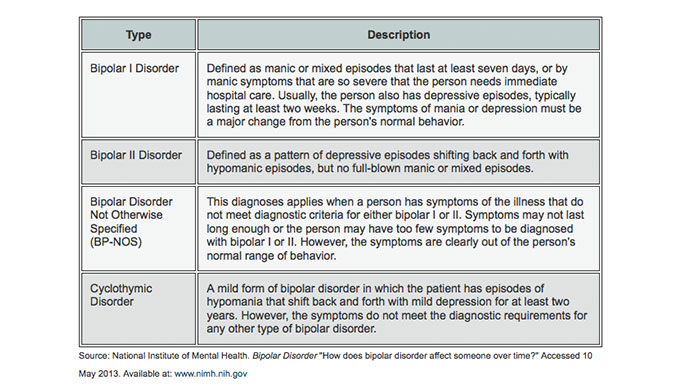 - R. 1-38.
- R. 1-38. - Bromet E.J., Kotov R., Fochtmann L.J. et al. Diagnostic shifts during the decade following first admission for psychosis // Am J Psychiatry. - 2011. - 168. - R. 1186-1194.
- Carlson G.A., Kotov R., Chang S.W. et al. Early determinants of four-year clinical outcomes in bipolar disorder with psychosis // Bipolar Disord. - 2012. - 14. - R. 19-30.
- Carlson G.A., Jensen P.S., Findling R.L. et al. Methodological issues and controversies in clinical trials with child and adolescent patients with bipolar disorder: report of a consensus conference // J Child Adolesc Psychopharmacol. - 2003. - 13. - R. 13-27.
- Nierenberg A.A. Lessons from STEP-BD for the treatment of bipolar depression // Depress Anxiety. - 2009. - 26. - R. 106-109.
- Cicero D.C., Epler A.J., Sher K.J. Are there developmentally limited forms of bipolar disorder? // J Abnorm Psychol. - 2009. - 118. - R. 431-447.
A complete list of references, including 57 items, is under revision.