How to deal with suicidal child
Teens and suicide: What parents should know
As a parent, you can approach suicide prevention in the same way you do other safety or health issues for your children. By educating yourself, you can learn what puts kids at greatest risk for suicide – and what protects them most strongly.
On this page
- Should parents be concerned about teen suicide?
- The facts
- Additional resources
- What can I do to protect my teen or tween from suicide risk?
- How can I tell if my child is behaving like a normal teenager – i.e. moody, etc. – or if there might be something wrong?
- How can I talk to my teen about mental health and suicide?
- Should I use the same approach for different age groups, i.e. tweens (ages 8 to 12) or teens (13 to 17)?
- What if they don’t want to talk?
- What if I’m concerned my child is thinking about suicide?
- What if my child knows someone who has taken their life? How do talk with them?
Sign up for email alerts
Receive updates from the American Foundation for Suicide Prevention
Should parents be concerned about teen suicide?
Suicide is in the news and in popular entertainment now more than ever, especially in regard to teens. You can play a role in building up your child’s mental health simply by becoming aware of the risk factors and warning signs that can lead to suicide, making yourself available to your child, knowing how to practice having a caring conversation, and being aware that help is always available.
The facts
There were approximately 100,000 teen (15-19 year-olds) suicide deaths over the 40 year period between 1975 through 2015, the most recent year covered by the study.
Boys take their lives at 3-4 times the rate of girls. The suicide rate for teen boys saw a rise that peaked in the late ‘80s and early ‘90s, then lowered in the late ‘90s and early 2000’s. This may be attributed to pediatricians increasingly taking on the role of treating depression. However, the rate has unfortunately been rising again since 2006.
The suicide rate for teen girls had a similar but less dramatic pattern. There has been an increase for girls over the last 10-12 years.
It’s worth noting there are fluctuations in suicide rates of all age groups over time. Youth rates remain significantly lower compared to every older age group.
Youth rates remain significantly lower compared to every older age group.
Additional resources
Risk factors and warning signs
While there is no single cause for suicide, there are risk factors and warning signs which may increase likelihood of an attempt. Learn what to look out for to keep your child or children safe.
Learn more
More Than Sad
The More Than Sad program shows you how to recognize signs of depression and other mental health problems, initiate a conversation about mental health with your child, and get help.
Learn more
Find a mental health professional
Who is a mental health professional, and how can they help? Find mental health providers in your area.
Learn more
LGBTQ crisis and support resources
LGBTQ crisis hotlines and support resources.
Learn more
What can I do to protect my teen or tween from suicide risk?
As a parent, you can teach and model healthy habits for mental health just as you would with physical health. Taking care of your own mental health, talking about it openly, and seeking therapy when warranted is one way to model healthy practices.
If your child sees you approaching your own challenges and learning for your own mistakes in an open way, they will understand that it’s okay to struggle and to learn from mistakes. They may develop flexibility and compassion for their own missteps — possibly even empathy for others, seeing how you navigate challenging times. They will also understand that life is messy and challenging for everyone at different times.
Check in with your child regularly, beyond just day-to-day tasks such as homework. You can learn how to invite deeper conversations through further guidance listed on this page.
You can learn how to invite deeper conversations through further guidance listed on this page.
If your child has a history of depression, anxiety, suicidal thoughts, self-harm or substance use, you should monitor them more closely, and consider involving a professional, either at key times, or for the longer term for more chronic conditions.
How can I tell if my child is behaving like a normal teenager – i.e. moody, etc. – or if there might be something wrong?
When children hit puberty, there are changes in their body and brain that can and do lead to behavioral changes. But there is a normal range which can manifest as moodiness, irritability, and pushing you away. This is a natural part of adolescent development. What should be concerning is if you notice indications of hopelessness or worthlessness, a withdrawal from friends and activities, or suicidal thinking or behavior. These are not typical manifestations for teenage angst.
But there is a normal range which can manifest as moodiness, irritability, and pushing you away. This is a natural part of adolescent development. What should be concerning is if you notice indications of hopelessness or worthlessness, a withdrawal from friends and activities, or suicidal thinking or behavior. These are not typical manifestations for teenage angst.
You know your child. You know their usual patterns, their common reactions to frustration and challenges, and what their good days and bad days look like. Trust your instincts if their behavior goes beyond these usual patterns of behavior. It could be just the tip of the iceberg of possible changes in their physical or mental health. It’s worth engaging them in conversation to get a fuller understanding of what they are experiencing so you can provide support, and get a better sense of how severe it is.
If your teen or tween’s sleep, energy, appetite, motivation, substance use, and frustration aren’t bouncing back to normal after a few days, have them see their pediatrician or a mental health practitioner.
How can I talk to my teen about mental health and suicide?
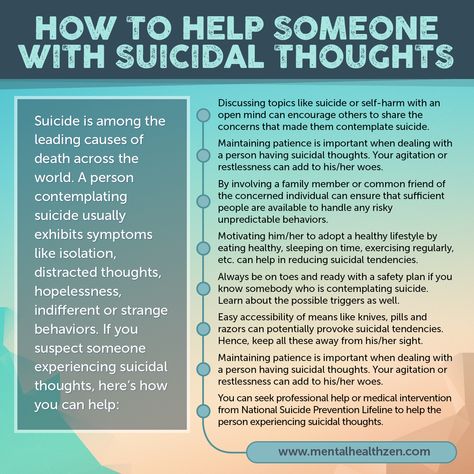
Don’t be afraid to have a conversation with your child about mental health and suicide. Ask your child how they’re doing, what’s happening in their world these days, and what their concerns are. It can start simply by asking, “Are you okay?”
Listen intently and without judgment. Ask open-ended questions, i.e. those that cannot be answered with a simple yes or no. Resist the urge to offer quick fixes or solutions to their challenges, which tends to shut down further dialog. Validate and support their feelings.
Follow their cues, and say things like, “Tell me more about that. I’d love to understand more about what that’s like for you. When he said that/did that to you, how did that make you feel?”
Should I use the same approach for different age groups, i.e. tweens (ages 8 to 12) or teens (13 to 17)?
The approach is very similar for tweens and teens, but with changes in language based on their level of sophistication and self-awareness.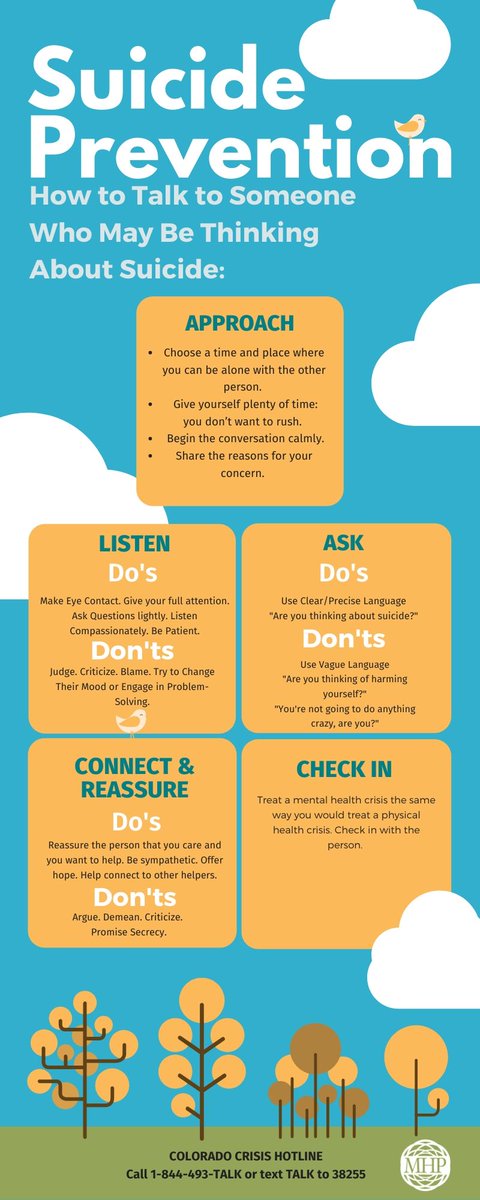 Use language that makes sense to your child, given their age, development, and what you know of how they think about things.
Use language that makes sense to your child, given their age, development, and what you know of how they think about things.
For a young child, you can ask about physical symptoms like stomach aches, and changes in feelings like getting upset or angry more lately. If it seems to you that they feel hopeless, trapped or overwhelmed – then ask if they ever think about hurting themselves or ending their life.
For older children, or kids who have demonstrated they are aware of their own thoughts and feelings, ask about their perceptions, as well as other symptoms like sleep problems, mood changes, and feelings of hopelessness, or of feeling trapped or overwhelmed.
What if they don’t want to talk?
If your child isn’t ready to talk, leave the invitation open for later by saying, “Whenever you want to talk, I’m here to listen and support you.” You could add “I won’t judge, and I’ll never stop supporting you, no matter what challenges you face.”
The likelihood is that your child will open up when you least expect it, sitting side-by-side rather than face-to-face, in the car or engaged in some other activity together.
When your teen starts to open up, be careful not to fall into the trap of jumping in with a solution or by saying, “You should…” or “Why didn’t you…”
What if I’m concerned my child is thinking about suicide?
If your child is talking about any level of distress, do not hesitate to ask them whether they’re feeling changes in their mood or level of stress, or having suicidal thoughts. Asking your child directly about suicide will not increase their risk, or plant the idea. It will create an opportunity to offer support, and let them know you care enough to have the conversation.
It will create an opportunity to offer support, and let them know you care enough to have the conversation.
You can say, “It sounds like you’ve been dealing with a lot lately. Does it ever get so tough that you think about ending your life?”
If your child gives any indication they have been thinking about suicide (unless they are in the act of self-harming) take them seriously. Continue to listen and engage in a caring, concerned, supportive manner. You can say things like, “Can you say more about that? I’m so sorry you’ve been feeling this way. I want to understand more about your perspective. I’m here for you no matter what. There is no problem too big that we as a family can’t get through. I’m going to keep supporting you and will also make sure you get the help you need to feel yourself again.”
Talk with your child about how to seek help. If you fear they may be at risk, get professional help right away.
Let them know you’ll be there for them no matter what, that your love is unconditional, and that you’ll help them get the support they need to get through this challenging time.
In a crisis situation, call the National Suicide Prevention Lifeline at 1-800-273-TALK or text the Crisis Text Line by texting ‘TALK’ to 741741 to speak or text with a trained counselor who can provide guidance on the most appropriate next steps and resources. Calling 911 is best for situations when self-harm is occurring or is about to occur.
For help finding a Mental Health Professional, consult with your child’s pediatrician, call your insurance, or use this treatment finder.
What if my child knows someone who has taken their life? How do talk with them?
It is important as a parent to be there for your child if a friend or a classmate has died by suicide. You can find specific guidance in AFSP’s Children, Teens, and Suicide Loss booklet, written in partnership with the Dougy Center, The National Center for Grieving Children & Families.
The booklet can be viewed online here.
Connection makes a difference
Find a chapter12 Things Parents Can Do to Help Prevent Suicide
As children grow into pre-teens and teenagers, it becomes more challenging for parents to know what they are thinking and feeling. When do the normal ups and downs of adolescence become something to worry about?
Parents and family members can help pre-teens and teens cope when life feels too difficult to bear. Learn about the factors that can increase your child's risks for suicide and explore the 12 suggestions below. These steps can help you feel better prepared to offer the caring, non-judgmental support your child needs.
1. If you see signs that your child's mental health is under threat, tune in.
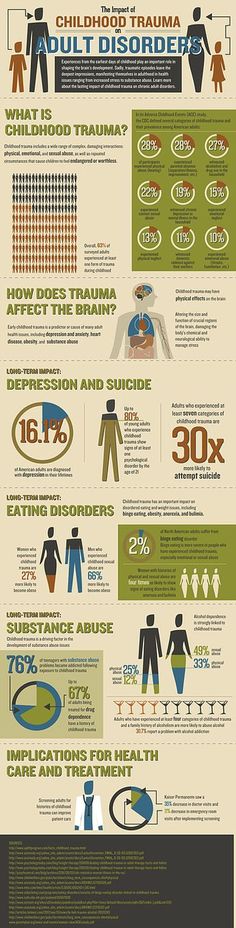
Maybe your child is just having a bad day, but when signs of mental health troubles last for weeks, don't assume it's just a passing mood. Studies show that 9 of 10 teens who took their own lives were struggling with mental health conditions such as anxiety. But keep in mind:
Teens who haven't been diagnosed with any mental health condition may still be at risk. In part, this is because it can be hard to pinpoint mental health issues at early ages.
Many teens who attempt suicide do not have underlying mental health issues, but in most cases, they will give signs that they're considering ending their own lives.
Your goal should be to remain calm, alert and ready to speak with your teen. Don't wait for them to come to you. You might start by saying,
"You seem sad. I'm open to talking about this, because I love you and I care what happens to you. " Here are more tips for
opening mental health conversations with your child.
" Here are more tips for
opening mental health conversations with your child.
2. Listen—even when your child is not talking.
Don't be surprised if your teen turns away when you first raise the subject of mental health or suicide. Keep in mind that, even if your child is silent at first, actions may speak even more loudly than words.
Watch for major changes in your child's sleep patterns, appetite, and social activities. Self-isolation, especially for kids who usually enjoy hanging out with friends or playing sports, can signal serious difficulties. If your child is struggling more than usual with schoolwork, chores and other responsibilities, these are additional signs you shouldn't ignore.
3. Realize that your child might be facing suicide risks you haven't considered yet.
Many parents wonder: Could this really happen to my child? Unfortunately, the answer is yes. Young people of all races, ethnicities, gender identities, sexual orientations, income levels, and community backgrounds die by suicide every year. In fact, suicide is the second leading cause of death among young people 10 to 24 years old.
In fact, suicide is the second leading cause of death among young people 10 to 24 years old.
Here are some things that can cause young people to think about ending their lives:
Loss of a loved one to death, divorce, deployment, deportation or incarceration
Bullying (in person or online)
Discrimination, rejection or hostility due to gender identity or sexual orientation
Racism, discrimination and related inequities and stressors
Family history of suicide or mental health difficulties
Stigma (the belief that it's wrong or shameful to talk about mental health or suicide)
Easy access to firearms or other life-threatening tools and substances
Witnessing or suffering violence or domestic abuse
Financial instability that causes worry and insecurity
Suicide in their school or friend group
Get more perspective on your child's specific risks
here.
4. Try not to dismiss what you're seeing as "teenage drama."
Never assume your child is exaggerating or playing games if they say or write:
"I want to die."
"I don't care anymore."
"Nothing matters."
"I wonder how many people would come to my funeral?"
"Sometimes I wish I could just go to sleep and never wake up."
"Everyone would be better off without me."
"You won't have to worry about me much longer."
Many kids who attempt suicide will tell their parents ahead of time (though others do not). These words indicate an urgent need for help.
Don't risk being wrong about this. Take every statement about suicide seriously.
5. Respond with empathy and understanding.
When your child talks or writes about suicide, you may feel shocked, hurt, or angry. You may even want to deny what you're seeing or argue with your child. These feelings are natural and valid, but it's essential to focus on your child's needs first and foremost. Your goal is to create a safe space where your teen can trust you to listen and express concern, but without judgment or blame.
You may even want to deny what you're seeing or argue with your child. These feelings are natural and valid, but it's essential to focus on your child's needs first and foremost. Your goal is to create a safe space where your teen can trust you to listen and express concern, but without judgment or blame.
Instead of reacting this way:
"That's a ridiculous thing to say."
"You have a great life – why would you end it?"
"You don't mean that."
"I can't believe what I'm hearing!"
Manage your own feelings so you can respond with empathy:
"It sounds like you're in tremendous pain and you can't see a way out."
"Maybe you're wondering how life got this complicated and difficult."
"Right now, you're not sure of the answers to the problems you're facing.
 "
""You must really, really be hurting inside to consider ending your life."
6. Get professional help right away.
If your teen is self-harming, or you sense they're at risk for attempting suicide, take them to the emergency department of your local hospital. Fast action is crucial when things have reached a crisis point.
If you see signs of suicidal thoughts but don't sense an immediate crisis, you still need to take action. Reach out to your pediatrician or local mental health providers who treat children and teens. Explain what you're seeing and hearing and schedule a mental health evaluation.
Health care providers can help you and your teen create a safety plan that covers:
Warning signs or triggers your teen feels will lead to suicidal thoughts
Possible steps to help them cope when they feel triggered
Sources of support: family, friends, teachers, mentors and others
Emergency contacts and steps to take if things get worse
7.
 Remove or secure guns you have at home. Do the same with other lethal tools and substances.
Remove or secure guns you have at home. Do the same with other lethal tools and substances.Half of youth suicides occur with firearms—and suicide attempts with firearms are almost always fatal. By far, the safest option is to remove guns and ammunition from your home while your teen is struggling with thoughts of suicide. Many families turn guns over to relatives or other trusted individuals to help safeguard their teen during a vulnerable time.
Safe home storage is the second-best option. Locking and unloading all guns, with ammunition stored and locked in a separate space, does reduce the risk of tragedy – but only if your teen doesn't know the combination to the lock or where the key is hidden. Disassembling guns and storing the components separately and locked is another option.
Of course, guns are not the only means of suicide your child might seek out. Prescription medications and over-the-counter drugs can pose hazards during a suicidal crisis. Families should keep medications locked away and, whenever possible, reduce the volume of medications on hand. Also consider buying over-the-counter medications in blister packs instead of bottles, to slow down access to pills.
Families should keep medications locked away and, whenever possible, reduce the volume of medications on hand. Also consider buying over-the-counter medications in blister packs instead of bottles, to slow down access to pills.
Other potentially lethal tools and substances you should consider locking away include:
Alcohol
Illicit drugs
Household cleaners and other poisonous products
Canned dusting products
Inhalants
Antifreeze
Knives, razors, or other weapons
Ropes, belts, or plastic bags
The work of removing or locking up these objects and substances may seem daunting, but your child's safety is at stake. Suicide attempts are often impulsive, and a moment of crisis can escalate very quickly. Making sure your teen cannot lay hands on lethal means at the wrong time is critical.
8. As your child enters treatment, focus on creating hope.

Your child's care team will likely recommend a combination of steps to reduce mental health symptoms and thoughts of suicide. Medications, talk therapy, and stress-reducing techniques such as yoga, meditation or journaling may be part of the plan.
Provide realistic reassurance for your child along the way. Remind them (and yourself) that difficult times don't last forever. People do feel better when they receive effective treatment and support.
If your child expresses feelings of stigma or shame, you can remind them that 1 in 5 people have mental health symptoms at some point in their lives. Mental health is part of total health—and seeking help is a sign of self-respect and maturity.
9. Encourage them to see family and friends.
Your child may feel reluctant to spend time with other people, but you can explain that social support will help them feel better. Though more quiet time might be needed at first, gentle encouragement to hang out with family, friends and neighbors will be helpful. Avoid power struggles around specific events or invitations, since your goal is to respect your child's needs and minimize stress.
Avoid power struggles around specific events or invitations, since your goal is to respect your child's needs and minimize stress.
10. Suggest exercise.
Physical activity eases mental health symptoms and supports your child's wellness plan. Whether it's getting outside to take a daily walk, a gym workout, an online exercise class or something else, exercise will:
Elevate your teen's mood by stimulating the production of endorphins (natural substances in the brain and body that help balance out stress and manage pain).
Support higher levels of serotonin, another brain-body substance that leads to positive moods and restful sleep.
Experts recommend working out 30 to 40 minutes between 2 and 5 times per week. Any form of exercise is fine. What matters most is that your teen enjoys this activity and feels motivated to do it regularly.
11. Encourage balance and moderation.
Teens in crisis need to go easy on themselves. This means adopting a realistic pace and avoiding experiences that could prove overwhelming.
This means adopting a realistic pace and avoiding experiences that could prove overwhelming.
Reassure your teen that self-care is never a sign of weakness. Everything we do in life is affected by our health, so giving ourselves time to heal is essential. Big tasks can be divided into smaller, more manageable ones, and gradually, as your child's confidence and strength grows, they'll feel ready to take on more.
12. Remind each other that this will take time.
You and your child will benefit from knowing that progress will come at its own pace. Setbacks may happen—they're part of the healing process, too. Encourage your child to be patient and self-forgiving. They've been through a lot, but with the right care and support, you will both see improvement.
Remember
If your child is considering suicide, call or text 988 or chat on 988lifeline.org right away.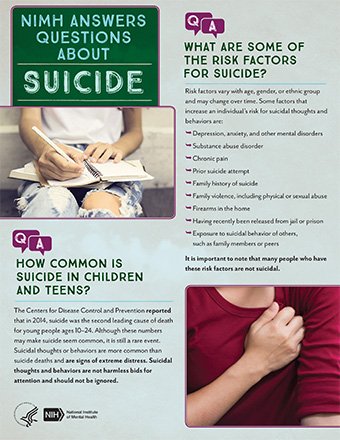 The Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones.
The Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones.
Ask your teen's care team for other resources you should know about. The National Alliance on Mental Illness has great information.
Parents of LGBTQ2S+ children can visit the Trevor Project website for focused resources. Parents and teens facing racial stress can benefit from these strategies and tools offered by the American Psychological Association.
You can also visit the American Academy of Pediatrics Blueprint for Youth Suicide Prevention for information about ways to prevent suicide in your community or school.
More information
-
Teen Suicide Risk: What Parents Should Know
- How to Talk About Mental Health With Your Child And Their Pediatrician
-
Mental Health & COVID-19: Signs Your Child May Need More Support
- 988 Suicide & Crisis Lifeline
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Get help & support for suicide
If you’re in emotional distress or suicidal crisis, find help in your area with Find a helpline.
If you believe that someone else is in danger of suicide and you have their contact information, contact your local law enforcement for immediate help. You can also encourage the person to contact a suicide prevention hotline using the information above.
Learn more about personal crisis information with Google Search.
Google’s crisis information comes from high-quality websites, partnerships, medical professionals, and search results.
Important: Partnerships vary by country and region.
| Country | Hotline organization | Website | Phone number |
|---|---|---|---|
| Argentina | Centro de Asistencia al Suicida | www. asistenciaalsuicida.org asistenciaalsuicida.org | (011) 5275-1135 |
| Australia | Lifeline Australia | www.lifeline.org | 13 11 14 |
| Austria | Telefon Seelsorge Osterreich | www.telefonseelsorge.at | 142 |
| Belgium | Center de Prevention du Suicide | www.preventionsuicide.be | 0800 32 123 |
| Belgium | CHS Helpline | www.chsbelgium.org | 02 648 40 14 |
| Belgium | Zelfmoord 1813 | www.zelfmoord1813.be | 1813 |
| Brazil | Centro de Valorização da Vida | www.cvv.org | 188 |
| Canada | Crisis Services Canada | crisisservicescanada. ca ca | 833-456-4566 |
| Chile | Ministry of Health of Chile | www.hospitaldigital.gob | 6003607777 |
| China | Beijing Suicide Research and Prevention Center | www.crisis.org | 800-810-1117 |
| Costa Rica | Colegio de Profesionales en Psicologia de Costa Rica | psicologiacr.com/aqui-estoy | 2272-3774 |
| France | SOS Amitié | www.sos-amitie.org | 09 72 39 40 50 |
| Germany | Telefon Seelsorge Deutschland | www.telefonseelsorge.de | 0800 1110111 |
| Hong Kong | Suicide Prevention Services | www.sps.org | 2382 0000 |
| India | iCall Helpline | icallhelpline. org org | 9152987821 |
| Ireland | Samaritans Ireland | www.samaritans.org/how-we-can-help | 116 123 |
| Israel | [Eran] ער"ן | www.eran.org | 1201 |
| Italy | Samaritans Onlus | www.samaritansonlus.org | 06 77208977 |
| Japan | Ministry of Education, Culture, Sports, Science and Technology | www.mext.go.jp | 81-0120-0-78310 |
| Japan | Ministry of Health, Labor and Welfare of Japan | www.mhlw.go | 0570-064-556 |
| Malaysia | Befrienders KL | www.befrienders.org | 03-76272929 |
| Netherlands | 113Online | www. 113.nl 113.nl | 0800-0113 |
| New Zealand | Lifeline Aotearoa Incorporated | www.lifeline.org | 0800 543 354 |
| Norway | Mental Helse | mentalhelse.no | 116 123 |
| Pakistan | Umang Pakistan | www.umang.com.pk/ | 0311-7786264 |
| Peru | Linea 113 Salud | www.gob.pe/555-recibir-informacion-y-orientacion-en-salud | 113 |
| Philippines | Department of Health - Republic of the Philippines | doh.gov.ph/NCMH-Crisis-Hotline | 0966-351-4518 |
| Portugal | SOS Voz Amiga | www.sosvozamiga.org | 213 544 545 963 524 660 912 802 669 |
| Russia | Fund to Support Children in Difficult Life Situations | www. ya-parent.ru ya-parent.ru | 8-800-2000-122 |
| Singapore | Samaritans of Singapore | www.sos.org | 1-767 |
| South Africa | South African Depression and Anxiety Group | www.sadag.org | 0800 567 567 |
| South Korea | Korea Suicide Prevention Center중앙자살예방센터 | www.spckorea.or | 1393 |
| Spain | Telefono de la Esperanza | www.telefonodelaesperanza.org | 717 003 717 |
| Switzerland | Die Dargebotene Hand | www.143.ch | 143 |
| Taiwan | 国际生命线台湾总会 [International Lifeline Taiwan Association] | www.life1995.org | 1995 |
| Ukraine | Lifeline Ukraine | lifelineukraine. com com | 7333 |
| United Kingdom | Samaritans | www.samaritans.org/how-we-can-help | 116 123 |
| United States | 988 Suicide & Crisis Lifeline | 988lifeline.org | 988 |
How can we improve it?
Ask the Help Community
Get answers from community expertsTransfers
home
Parents
Helpline
Information about the unified all-Russian children’s helpline
0446 8-800-2000-122 .
When calling this number in any locality of the Russian Federation from fixed or mobile phones, children in difficult life situations, adolescents and their parents, other citizens can receive emergency psychological assistance, which is provided by specialists of services already operating in the constituent entities of the Russian Federation that provide services for telephone counseling and connected to a single all-Russian number of children's helpline.
Confidentiality and free of charge are the two main principles of the children's helpline. This means that every child and parent can anonymously and free of charge receive psychological assistance and the secrecy of his call to the helpline is guaranteed.
Working hours of the children's helpline in the constituent entities of the Russian Federation
(as of October 1, 2013)
| Name of the subject of the Russian Federation 9Arkhangelsk region 09.00-22.00 | |||
| 22 | with Nenets Autonomous Okrug | daily 09.00-17.30 | |
| 23 | Vologda region | around the clock | |
| 24 | Kaliningrad region | daily0039 | around the clock |
| 35 | Chechen Republic 08.30-20.00 | ||
| South Federal District | |||
| 37 | Republic of Adygea | ||
| Kalmykia | Pon-Pip. 8.00-17.00 8.00-17.00 | ||
| 3 | |||
| 80 | Magadan region | Pon.-Pon. 10.00.22.00 | |
| 81 | Sakhalin Region | ||
| 900 | |||
| 83 | Chukotka AO | Mon-Fri 09.00-22.00, closed 16.00-22.00 | |
Infographics. The principle of operation of a single federal helpline number for children, adolescents and their parents
Information from the regions about the work of the children's helpline
12/28/2016
What to do when there is a problem, but there is no one to tell about it?
12/28/2016
Online psychologists are ready to save children from bullying
12/28/2016
What problems do residents of the Irkutsk region call the helpline
09.1 for children1.2016
3
3
09.