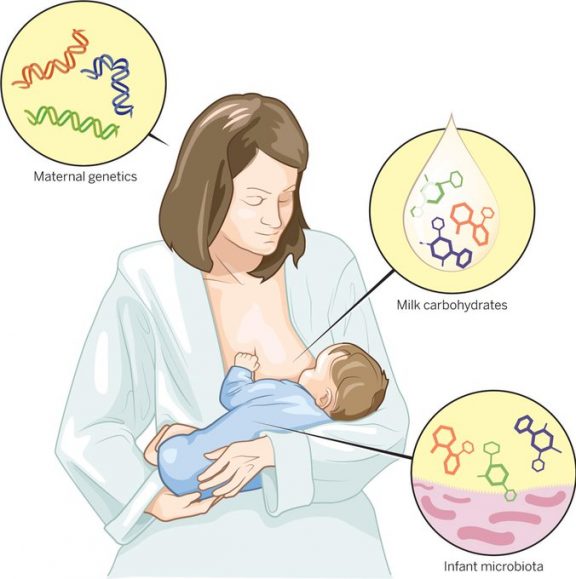
How to create an oversupply of breast milk
Breast Milk Oversupply | Advice for New Parents
Many women naturally make more milk than their infant needs. Sometimes an oversupply is created by over stimulating the breasts doing both breastfeeding and pumping. Having an oversupply of breast milk can be uncomfortable for both mother and her infant.
Signs of Oversupply - Mom
The following are signs of oversupply in the mom:
- Leaking a lot of milk
- Breast pain from feeling overly full
- Nipple pain usually from infant biting, chewing or clenching down to slow a very fast let down
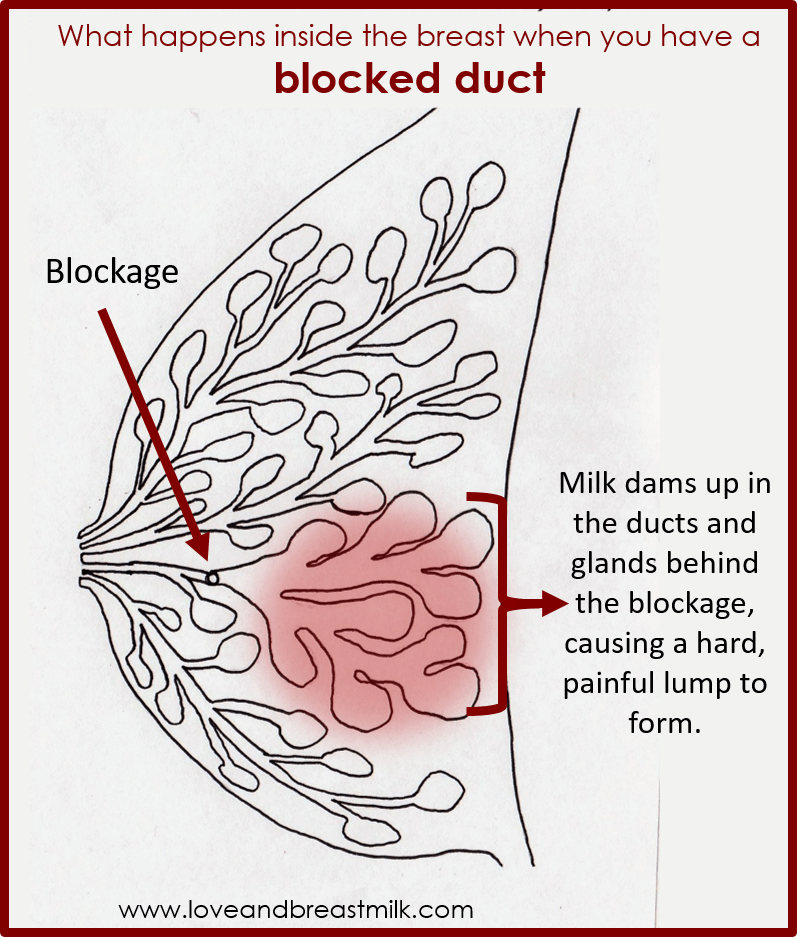
- Recurring plugged ducts or mastitis
Signs of Oversupply - Infant
The following are signs of oversupply in the infant:
- Gulping, coughing, choking or sputtering during feedings
- Frequently detaching from the breast during feedings
- Fussiness between feedings and/or cuing to feed all the time (even after drinking plenty of milk)
- Frequently spitting up
- Passing lots of gas
- Explosive, green, frothy or watery stools; maybe even mucus or blood in the stool
- Overly fast weight gain
- May be diagnosed with “reflux”, “colic”, “lactose intolerance”, or even “failure to thrive”
Since most mothers and infants have symptoms, treatment is often a two-step process.
- Feedings at the breast must be more comfortable for mother and infant.
- A small decrease in milk production will make feedings more enjoyable for mother and infant.
Suggestions for making a little less milk
The following are suggestions on how to make less milk:
- Use only one side for a three hour block of time, returning to the same breast if your infant cues to feed again in that time frame. Express a minimum amount from the other breast only as needed for comfort, until the next three hour block.
- Gradually increase the time blocks up to 12 hours per breast, as needed.
- There are medications and herbs that can be used if these strategies do not work for you. Call your lactation consultant or The Center for Breastfeeding Medicine at 513-636-2326 for guidance.
Stop these strategies as you decrease your milk supply and feeds become more comfortable.
Suggestions for managing feedings with a very fast milk flow
Here are suggestions for managing feedings with a very fast milk flow:
- Try feeding when your infant is drowsy
- Offer the breast before it gets overly full
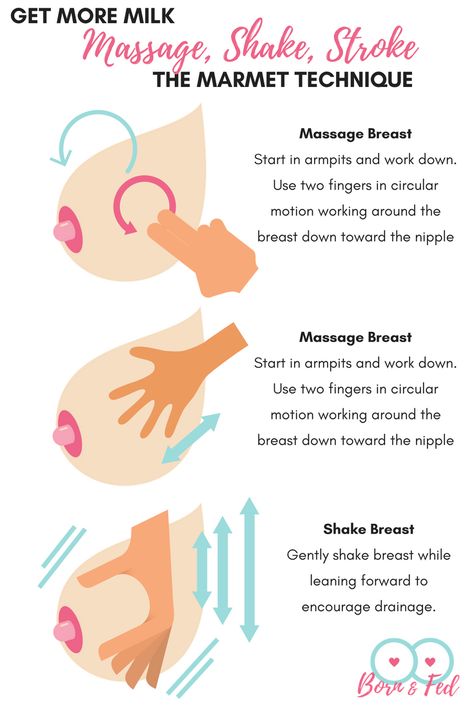
- If your breast is overfull, hand express or pump just the initial fast flow of milk and then latch your infant
- Try feeding positions that use gravity to slow the flow of milk, such as a laid back nursing position
- Burp frequently and give your infant breaks to pace him/herself
- Firmly press the pinky side of your hand into your breast (like a karate chop) during the initial fast let down to slow the flow of milk. As your infants sucking slows down, release your hand to allow milk flow.
Last Updated 03/2020
Reviewed by Barb Chaney, MSN, RN, IBCLC
Contact us or refer a patient.
Oversupply of breastmilk | Pregnancy Birth and Baby
beginning of content4-minute read
Listen
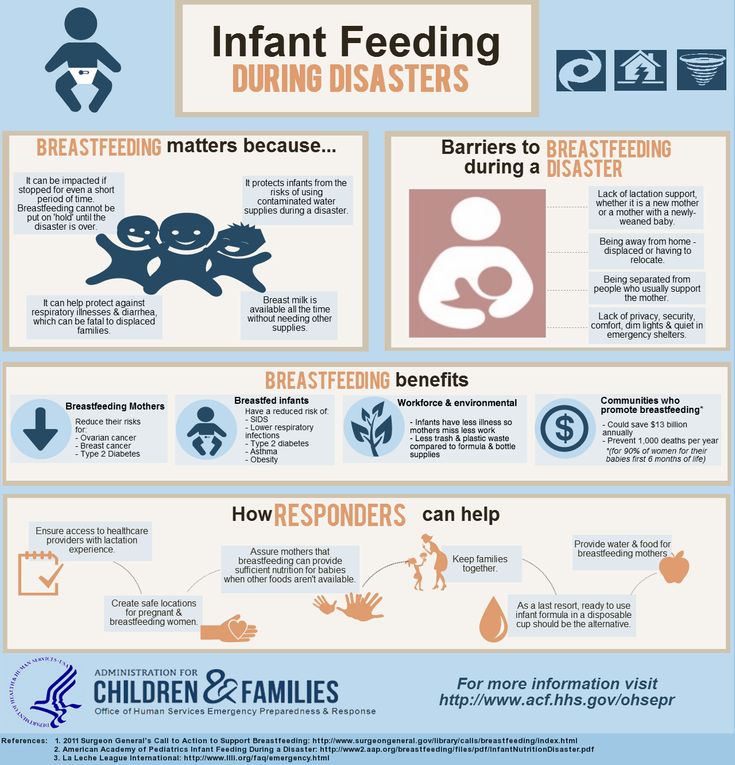
A mother’s milk supply usually adjusts to her baby’s needs after about 4 weeks of breastfeeding. Some mothers continue to make more milk than the baby requires, and this is known as ‘oversupply’.
Oversupply can make breastfeeding difficult for both mother and baby.
What are the causes of oversupply?
Breastmilk oversupply that continues after the first 4 weeks or so can have many causes. Feeding patterns may cause the oversupply, such as:
- feeding the baby on a set schedule rather than according to need
- pumping too much before a feed to make the breast soft and easier for the baby to latch onto
- the baby preferring to feed mainly from 1 breast
Other causes of oversupply include:
- an excess of the milk production-stimulating hormone prolactin in your blood (hyperprolactinemia)
- a congenital predisposition
How breastmilk oversupply affects your baby
Your baby may be unsettled or distressed during and after feeding, and it can be hard to know whether they are still hungry or are getting too much milk too fast. Your baby may:
Your baby may:
- choke and splutter at the breast due to the high rate of milk flow
- have trouble latching onto the breast
- feed for only short periods of time leading to ‘lactose overload’
- have a lot of urine (more than 10 wees a day) or diarrhoea with green, frothy poos and nappy rash
- have excessive wind, causing unsettled, colicky behaviour
- bring up a lot of milk after breastfeeding
- put on weight quickly
How breastmilk oversupply affects you
Oversupply can also cause problems for you.
You might feel your breasts refill very quickly after feeding your baby. They might feel lumpy and tight after breastfeeding. You might also leak more than usual or have an explosive milk-ejection reflex, which makes it difficult to feed in public, and can cause difficulties for your baby at the beginning of feeding.
You could develop blocked milk ducts or mastitis and breast abscesses.
Oversupply can make breastfeeding a less pleasurable experience for you or your baby. Some mothers think about early weaning if oversupply is not diagnosed and managed well.
Some mothers think about early weaning if oversupply is not diagnosed and managed well.
How is breastmilk oversupply diagnosed?
It is essential to have a health professional such as a lactation consultant, breastfeeding counsellor, doctor or child health nurse watch your baby breastfeed to diagnose true oversupply. It can easily be confused with breast engorgement or a fast ‘let-down’ reflex.
For help with the diagnosis and treatment of oversupply, contact a health professional, such as a lactation consultant, breastfeeding counsellor, or child health nurse, or call Pregnancy Birth and Baby on 1800 882 436.
How is breastmilk oversupply treated?
The aim of treatment is to reduce your milk production. This is best done while you are being supported by a lactation consultant, breastfeeding counsellor, or child health nurse.
‘Block feeding’ is a method that can help reduce milk supply in just a few days:
- Choose a time frame, usually from 3 to 4 hours, and feed your baby from only 1 breast during that time.
- Then change to the other breast for the same time period.
- Continue this pattern for a few days.
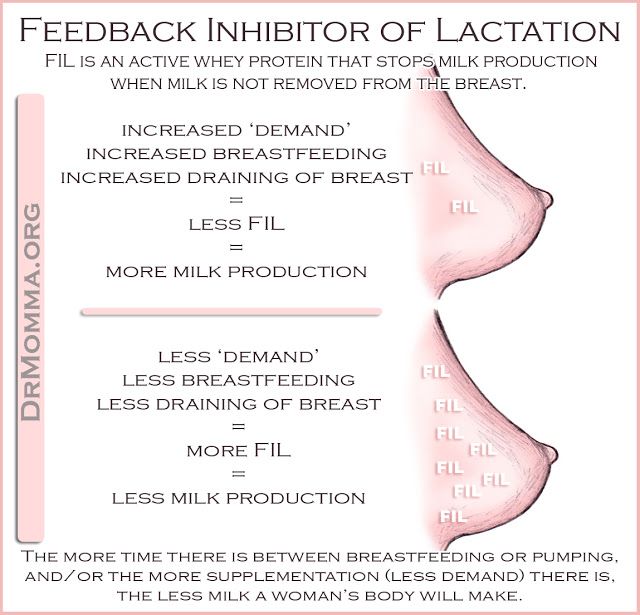
- You might need to hand express a small amount from the unused breast to relieve pressure or discomfort, but don’t empty it — the residual milk in the unused breast triggers the reduction in milk production.
Block feeding ensures that 1 breast always contains residual milk. This will trigger both breasts to reduce milk production, and should gradually resolve oversupply of milk. How long it takes depends on your situation.
Block feeding will also help to reduce the amount of thinner foremilk consumed by your baby. As your baby gets to drink more of the creamy hindmilk, you’ll see your baby’s stools get thicker. This tells you that you are on the way.
If your milk supply does not respond to block feeding, talk to your doctor.
The Australian Breastfeeding Association website has more tips about managing oversupply.
Sources:
Australian Breastfeeding Association (Too much milk), Australian Breastfeeding Association (Lactose overload in babies), Raising Children Network (Oversupply of breastmilk and engorgement), King Edward Memorial Hospital Obstetrics & Gynaecology (Clinical Practice Guideline: Breastfeeding challenges: oversupply/hyperlactation), Breastfeeding USA (Oversupply: Symptoms, causes, and what to do if you have too much milk))Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2021
Back To Top
Related pages
- Breastfeeding your baby
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Too much milk? Reduced lactation
Sometimes you may feel like you are producing too much milk, especially in the first weeks of breastfeeding. After reading our article, you will find out if you really have too much milk, and what can be done to reduce it.
Share this information
Breast milk is very healthy, so it's good to have a lot of it, right? However, this is not always the case. Babies can sometimes have a hard time coping with the rapid rush of milk that usually accompanies excess lactation. And mothers who have too much milk often experience discomfort due to the constant leakage of milk and often suffer from mastitis.
Fortunately, there are a number of ways to help in this situation. But before you use them, answer two important questions:
Do I really have too much milk?
Some of the symptoms of over-lactation (listed below) may occur for very different reasons. You should not try to reduce the production of breast milk, if you are not sure that it is the overabundance of it that is the main problem. Otherwise, this can lead to the fact that your baby will produce less milk than your baby needs, especially in the critical first month when production is just being established.
Is being overweight a problem for me or my baby?
If you are sure that you have an excess of milk, but this does not cause problems for you and your baby, you do not need to do anything. In most cases, everything returns to normal within the first few months. As the baby grows, he will learn to better cope with the rapid flow of milk and will feed with pleasure.
Leakage is not always a sign of too much milk
During the first four to six weeks of your baby's birth, the level of prolactin, the hormone responsible for milk production, will rise each time the breast is emptied. In these first weeks, the breast learns to produce milk in the amount that the baby needs, depending on the time of day. Therefore, excessive leakage, rapid filling of the breast, and even splashing of milk during a rush are the norm. 1
At the same time, your baby is learning to suck and swallow milk, so you shouldn't be surprised if he suddenly coughs or chokes when he suckles.
After about four to six weeks, the spikes in prolactin levels will begin to fade and milk production will become more balanced, adjusting to your baby's needs on a supply and demand basis. 2 However, given the many hormonal changes that occur in the body of a young mother, such a restructuring may take some time. In some mothers, milk production is established quickly, in others a little longer.
Behavior of the child, which may indicate an excess of milk
When overproduced, milk is usually released very quickly, especially during the first flush. As a result, the baby may cough or choke at the beginning of a feed, push back, or hold the breast loose in the mouth. The baby may pull away from the chest, frightened by a quick rush, and then cry because he hasn’t eaten. He can swallow milk in large volumes and with a lot of air, and after that he will spit up a lot. Try to be as careful as possible when you help him burp - sudden movements combined with a full tummy can cause the baby to vomit and scare him even more.
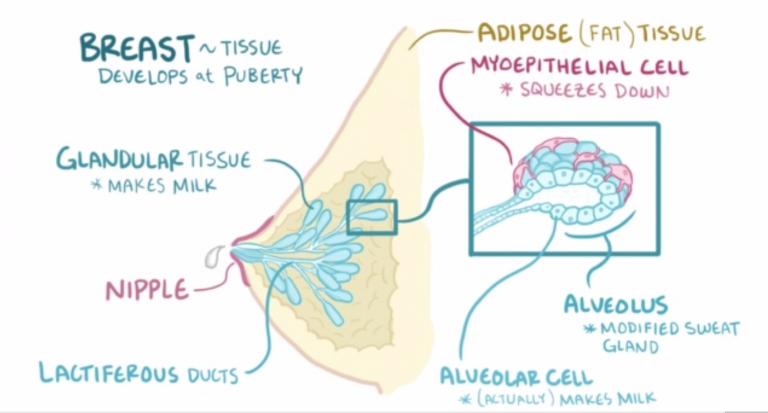
At the start of a feed, milk is relatively low in fat and consists mainly of lactose (sugar) and proteins. As the breast is fed and emptied, the fat content constantly increases. In the case of excess milk production, your baby may feel full before he completely empties his breast. This means that he will get a lot of lactose-rich milk, but not enough fat-rich milk that comes towards the end of a feed. Excess lactose instead of a balanced diet can make digestion difficult and cause hard, frothy, and greenish stools.
Excess lactose instead of a balanced diet can make digestion difficult and cause hard, frothy, and greenish stools.
Oddly enough, in such a situation, the baby may constantly want to eat and behave restlessly between feedings. Despite the high calorie content, the low fat content of milk prevents it from being fully satiated. It is the fat contained in food that gives us a feeling of satiety. What happens if you eat a few dozen rice crackers or a slice of cheese with a cookie instead? You will fill up on cheese faster, as it is more saturated with fats.
However, all these symptoms can be caused by completely different problems, such as reflux, allergies, or even vice versa, insufficient milk production. An excess of breast milk can indeed cause these symptoms, but only if they are accompanied by excessive weight gain. Children usually dial around 900 g per month, but in the case of an excess of milk, they can gain much more, often almost twice as much. 1 If you feel like you are having too much milk but your baby is gaining weight normally, contact your lactation consultant or your healthcare provider.
Symptoms that may indicate an excess of milk in mothers
Mothers with an excess of breast milk often experience swelling and tightness in the breast, which constantly seems full. 3 As already noted, the leakage of breast milk in the first six weeks does not indicate its excess. However, if this continues at every feeding and after this period, it may be that the problem is in the overabundance.
A baby cannot always empty a full breast, so when there is an excess of breast milk, blockage of the milk ducts or periodic bouts of mastitis often occur. However, these problems can also be caused by other reasons.
How to reduce milk production
If you have found that you have too much breastmilk and this is causing you concern, here are a few simple things that can help. For some mothers, they are enough.
- Try feeding in a relaxed position. Reclining or lying down feeding will allow the baby to better control the process.
 In this position, the baby sets the rhythm of feeding himself and can always raise his head to take a break if the milk is released too quickly. Don't forget to put a towel over to soak up spilled milk.
In this position, the baby sets the rhythm of feeding himself and can always raise his head to take a break if the milk is released too quickly. Don't forget to put a towel over to soak up spilled milk. - Release pressure. If full breasts make you uncomfortable, try expressing some milk by hand or with a breast pump, but try to express as little milk as possible. Every time you empty your breast, you send a signal to her to produce even more milk. Therefore, pumping provides short-term relief, but with prolonged use, it can only aggravate the situation. If you need to express and store milk to feed your baby when you are not around, it is best to address the problem of excess production first.
- Try bra pads. If you have milk leaks, put special pads or pads in your bra to collect milk* to keep your underwear dry. If your milk leakage is moderate and already decreasing, or your breasts leak slightly during pregnancy, ultra-thin disposable pads will help you feel confident in any life situation.

- Avoid teas and lactation supplements. If you have been drinking teas, eating special biscuits, or taking supplements to improve breast milk production, this should be stopped now to resolve the problem.
"Breast Watch" to reduce milk production
If all the above methods fail, you can try a technique called "Breast Watch", which allows you to better control milk production. However, before trying this method, check with a lactation consultant or healthcare provider.
On breastfeeding, you feed your baby on demand, but only on one breast for four hours. The second breast during this time is strongly filled. Since breast milk contains what is known as a "feedback lactation inhibitor", due to overfullness, the body sends a signal to that breast to slow down milk production. This is a natural way to protect the breast from endless filling.
This technique must be applied for 24 hours, changing breasts every four hours. If the milk does not become less, try increasing the duration of the "watch" to six hours.
Complete emptying and “breast duty” technique
If after another day there is still a lot of milk produced,
you can try another version of this technique, which is recommended in cases of extreme overabundance. It is called "complete emptying and duty of the breast." 3
In this method, both breasts must be completely emptied in the morning with an electric breast pump and breastfeeding should be started immediately. The flow of milk will be weaker and allow the baby to eat calmly. In addition, he will get more fat-rich milk, which comes at the end of feeding, which means he will feel more full.
After that, you can continue the "breast watch" for four hours, as described above. If that doesn't help, try increasing the interval to six, eight, or twelve hours the next day, depending on the extent of the problem. Before using this technique, be sure to consult with your doctor.
You may not need to completely empty your breasts after the first use of this technique, but some mothers have to do this once or twice. Improvement usually occurs within the first two days or a little later, but in no case should "breast watch" be used for more than five days.
Improvement usually occurs within the first two days or a little later, but in no case should "breast watch" be used for more than five days.
Literature
1 Morbacher N. Breastfeeding answers made simple. Amarillo TX , USA : Hale Publishing ; 2010. - Morbacher N., "Simple answers to questions about breastfeeding." Amarillo, Texas, USA: Publishing Hale 0106 et al . Blood and milk prolactin and the rate of milk synthesis in women. Exp Physiol. 1996;81(6):1007-1020. - Cox D.B. et al., Effects of blood and milk prolactin on milk production in women. Exp Physiol. 1996;81(6):1007-1020.
3 van Veldhuizen-Staas CG. Overabundant milk supply: an alternative way to intervene by full drainage and block feeding. Int Breastfeed J . 2007;2(1):11. - van Velhusen-Staas SJ, "Milk Overabundance: An Alternative Countermeasure by Total Drying and Blocking of Feeds." Int Brestfeed J (International Journal of Breastfeeding). 2007;2(1):11.
2007;2(1):11. - van Velhusen-Staas SJ, "Milk Overabundance: An Alternative Countermeasure by Total Drying and Blocking of Feeds." Int Brestfeed J (International Journal of Breastfeeding). 2007;2(1):11.
Read instructions before use. Consult a specialist about possible contraindications.
* RC № FZZ 2010/07352 dated 19.07.2010
Six first week breastfeeding solutions
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: for some mothers, the nipples crack, bleed or blister. This is, of course, very annoying.
Solutions 3
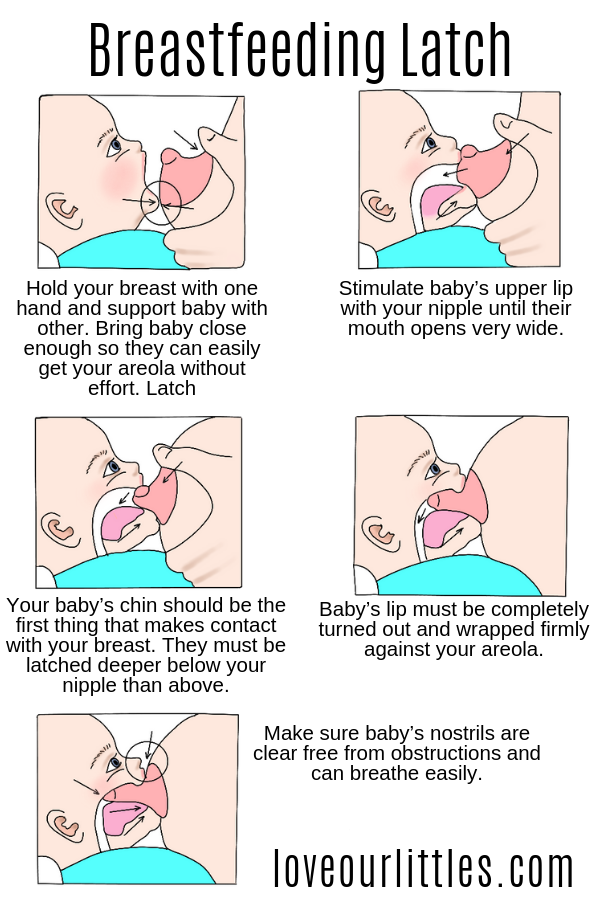
- Check how the baby latch on. An incorrect latch is one of the most common causes of pain during breastfeeding.
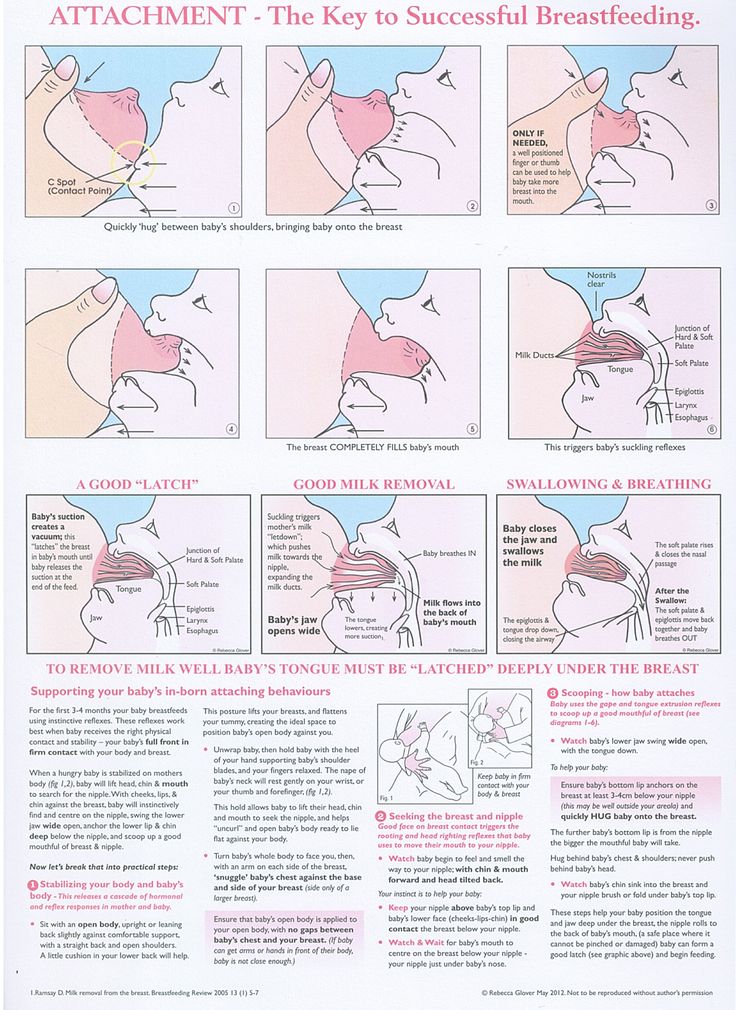 A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue. - Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.
- Gently wipe soaked nipples with water-dampened cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or pat dry with a clean, soft muslin or flannel cloth to prevent bacterial growth in humid environments. Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
- Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. Inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not improve after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.
Problem #2. Baby doesn't latch on properly
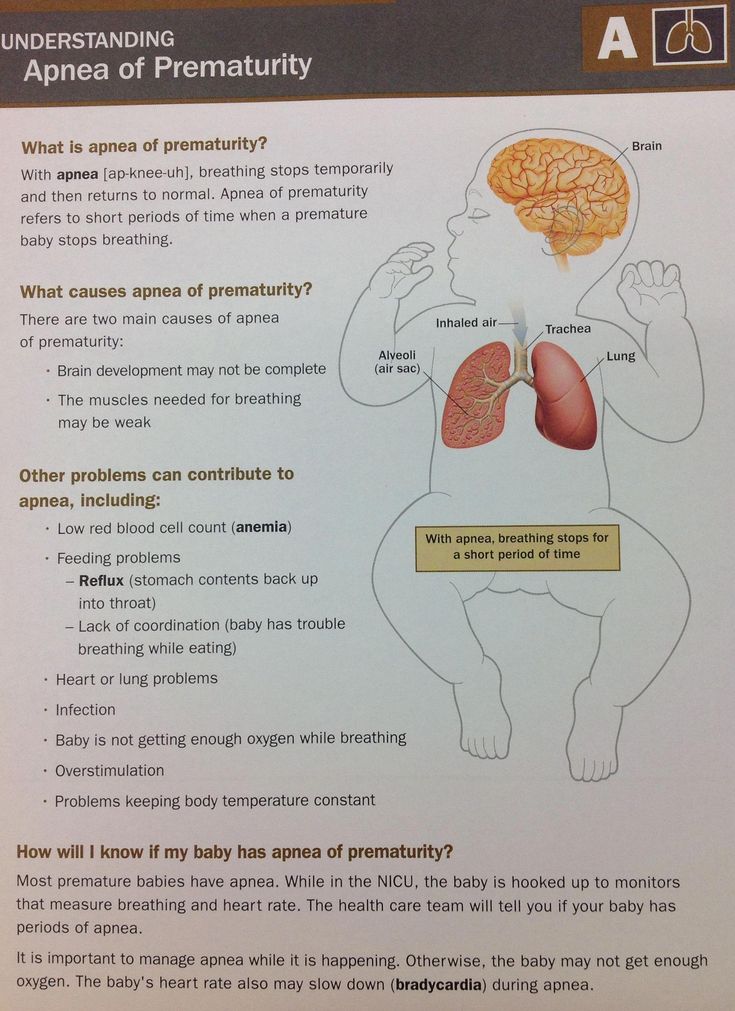
Some newborns do not immediately latch on properly. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
- When feeding, try to find the optimal position.
 Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional. - Use nursing pads. If your baby is having trouble latching on, a lactation consultant or healthcare professional may suggest trying nursing pads*. A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you are having problems with milk production. The sooner you do this, the better.
- Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night. Such frequent feeding helps to establish the production of breast milk.
- Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4. Breast full and heavy
Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.
Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away. Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the start of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk. The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you.
- Be gentle and patient. Let your baby rest and digest milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s Health 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding.