How to calculate child medicine dosage
Pediatric Dose Calculator
Created by Łucja Zaborowska, MD, PhD candidate
Reviewed by Bogna Szyk and Steven Wooding
Based on research by
Pan SD, Zhu LL, Chen M, Xia P, Zhou Q. “Weight-based dosing in medication use: what should we know?“ Patient Prefer Adherence (2016)
Last updated: Aug 06, 2022
Table of contents:- How to use the pediatric dose calculator?
- Dose frequency abbreviations
- How do you calculate pediatric doses?
- Child dose calculations examples
The pediatric dose calculator is a simple tool for computing the pediatric dosage for a child of a given weight. 👶
Our calculator allows you to convert values in mg or μg to a precise volume of the medication, using a wide range of units.
The article below is an essential part of our peds dosing calculator - keep on reading to discover all the necessary medical abbreviations, information on pediatric medication dosing, and tips on how to calculate the pediatric dose on your own.
Disclaimer: We try our best to make our Omni Calculators as precise and reliable as possible. However, this tool can never replace professional medical advice.
How to use the pediatric dose calculator?
Pediatric dosage is a complicated matter - we can't deny it. We decided to make things easier for you and explain step-by-step all the actions you need to take to receive the most accurate results.
| 💡 Our mg per kg dosage calculator works both ways; you may convert medication's weight to volume and the other way around. |
-
Decide whether your dose is given in mg or μg.
Milligrams (mg) are 1000 times greater unit than micrograms (μg) - 1 mg = 1000 μg.
-
Find out your type of dosage.
Your dose in mg/μg might be given:
-
per kilogram per day (e.
 g., mg/kg/day) - the most popular option
g., mg/kg/day) - the most popular option -
per kilogram per dose (e.g., mg/kg/dose)
-
per day (e.g., mg/day)
-
per dose (e.g., mg/dose)
The calculator will display the chosen dosage type underneath.
Dosage type has a crucial impact on the value of the dosage!
Only the first two types use the dosage calculator by weight; two latter ones rely on a predetermined amount of medication.
-
Finally, enter your dose amount in mg or μg.
Double-check all the settings - you want to make sure that the pediatric drug dose calculator is computing exactly what you want it to calculate.
-
Choose the frequency. - check the section below.
-
Choose the weight of your child and a proper unit.
-
Enter your drug concentration.
Choose the mass of the drug per given volume of the medication.
The calculator will display the chosen concentration underneath.
| 💡 Our calculator can also compute the number of tablets needed. To calculate that, enter 1 into the volume field. 💊 |
- Yay! Your results are here - it wasn't that hard, was it? 🎉
If you've already found out everything you need to know, you may as well try and discover our other child dose calculations:
- Ibuprofen dosage
- Paracetamol dosage calculator
- Simple dosage calculator
- Epinephrine dose for kids
Dose frequency abbreviations
Dose frequency might be quite misleading since all the abbreviations originate from the Latin language. Here we present a short, useful medical dictionary:
- dQ - once per day
- BID - twice per day
- TID - three times per day
- QID - four times per day
- q4 hr - once every four hours (6 times per day)
- q3 hr - once every three hours (8 times per day)
- q2 hr - once every two hours (12 times per day)
- q1 hr - once every hour (24 times per day)
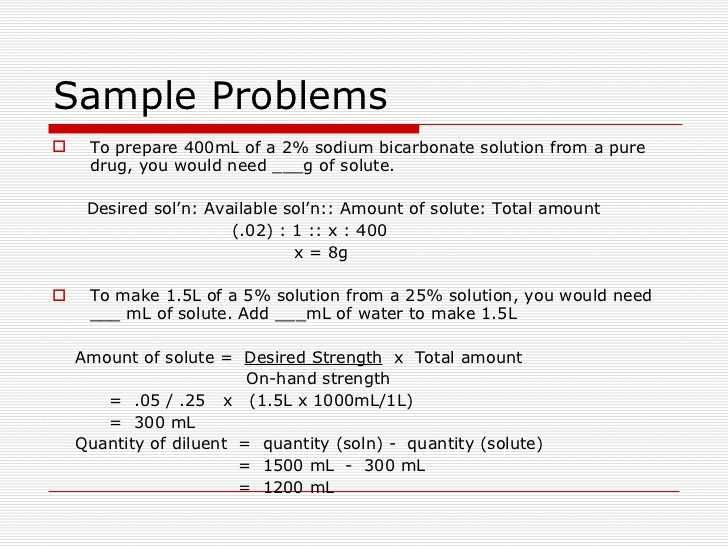
How do you calculate pediatric doses?
There's one primary dose calculation formula for children:
▪️ mg/μg per kilogram per day
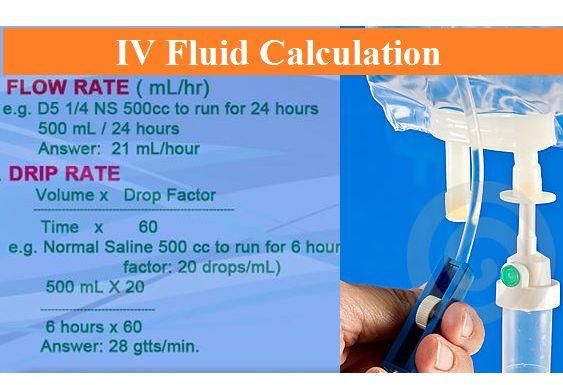
dose (volume) = (dose (mg/μg) * child's weight) / (concentration * frequency)
where:
concentrationis usually given in mg/mLchild's weightis given in kgfrequencymeans the number of times a chosen medication is given per day.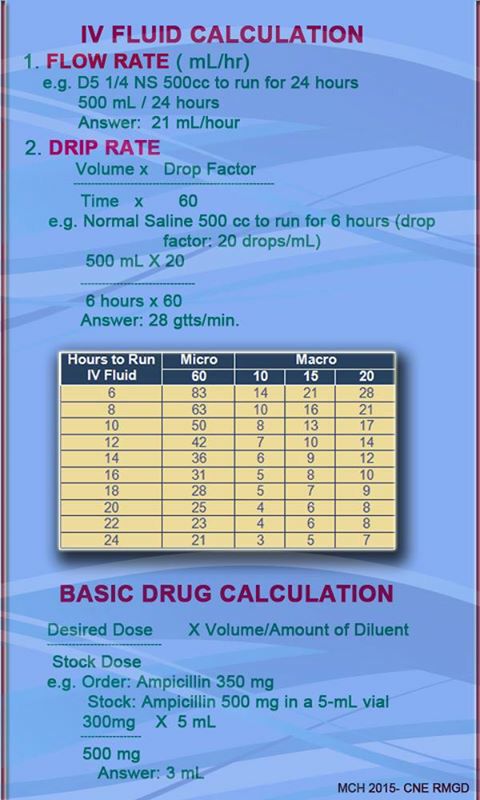 E.g., q1 hr frequency has a value of 24.
E.g., q1 hr frequency has a value of 24.
However, this equation still has to be modified for every other type of dosage! Below, we enumerated all the available pediatric dosage calculations formulas:
▪️ mg/μg per kilogram per dose
dose (volume) = (dose (mg/μg) * child's weight) / concentration
▪️ mg/μg per day
dose (volume) = dose (mg/μg) / (concentration * frequency)
▪️ mg/μg per day
dose (volume) = dose (mg/μg) / concentration
Hey, how about discovering our other professional pediatric tools:
- Maintenance fluids 🚰
- Blood volume 💉
- Blood transfusion 💉
- Growth charts 📈
Child dose calculations examples
Our baby has a fever! 🤒🌡️👶
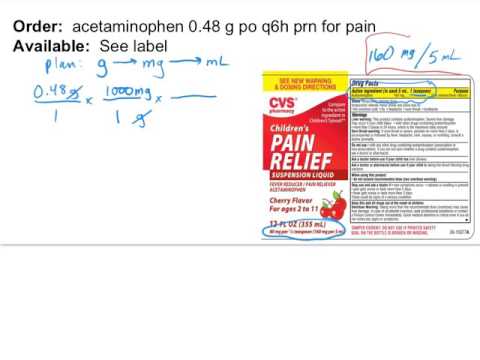
Still not sure how to calculate pediatric doses? We're going to focus on an mg/kg/day formula since it's the most complex one. Carefully follow the example below:
Carefully follow the example below:
- We bought some paracetamol to lower the fever - its container states that this syrup's concentration is equal to 120 mg /5 mL. Our prescribed peds dose is 10 mg/kg. Our kid's 4.5 years old and weights 20 kg. We need two doses of paracetamol per day.
How much mL of paracetamol syrup do we need per day?
Let's use the following formula:
dose (volume) = (dose (mg/μg) * child's weight) / (concentration * frequency)
First, let's boil down the concentration:
120 mg/5 mL / 5 = 24 mg / 1 mL = 24 mg/mL
Then come back to the equation itself:
dose (volume) = (10 mg/kg * 10 kg) / (24 mg/mL * 2)
dose (volume) = 100 mg / 48 mg/mL
dose (volume) = 2.083 ≈ 2.1 mL - we need 2.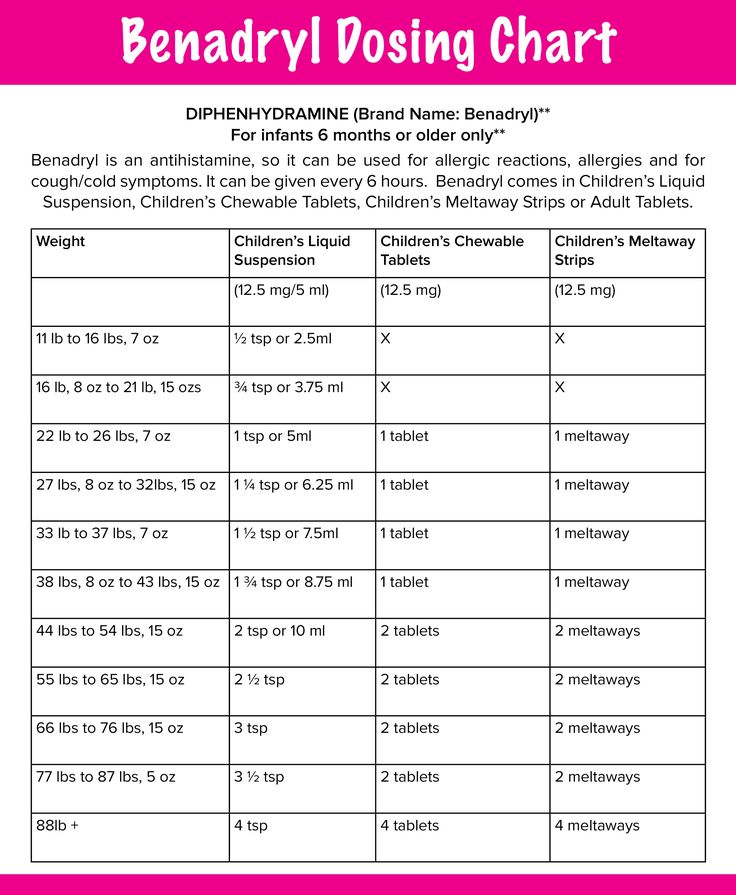 1 mL of paracetamol per dose, twice per day.
1 mL of paracetamol per dose, twice per day.
Yay, we got it! You're becoming the true pediatric dose master.
Łucja Zaborowska, MD, PhD candidate
Dosage (weight)
Dosage type
Frequency
Weight
Drug concentration
Dosage (volume)
Dosage
per dose
per 24h
Check out 16 similar pediatric calculators 🧒
Adjusted ageAmoxicillin pediatric dosageAPGAR score… 13 more
Clark's Rule - StatPearls - NCBI Bookshelf
Benjamin J. Delgado; Anthony O. Safadi; Tushar Bajaj.
Author Information
Last Update: July 5, 2022.
Definition/Introduction
Clark's rule is an equation used to calculate pediatric medication dosage based on the known weight of a patient and a known adult dose of medication to be used. Clark's rule equation is defined as the weight of the patient in pounds divided by the average standard weight of 150 pounds (68 kg) multiplied by the adult dose of a drug equals the pediatric medication dose, as is demonstrated below:
(Weight* divided by 150 lbs.
 ) x Adult Dose** = Pediatric Dosage
) x Adult Dose** = Pediatric Dosage(Weight*** divided by 68 kg) x Adult Dose** = Pediatric Dosage
*Weight of pediatric patient in pounds (lbs.)
**Adult dose is the recommended dosage for adult medication use
***Weight of pediatric patient in kilograms (kg)
Clark's rule is one of the known pediatric medication dosing rules described in the medical literature that utilizes the patient's weight to calculate medication dosage. Other equations that utilize pediatric weight to calculate medication dosing include Salisbury's rule, Penna's rule, and the Body Surface Area rule. Other methods besides Clark's rule that also utilize pediatric age to calculate radiopharmaceutical medication dosages used in nuclear imaging include Young's rule, Webster's rule, and Fried's rule.[1][2]
Issues of Concern
Pediatric Obesity and Medication Dosing
Data from 2011 to 2014 showed the prevalence of obesity among children and adolescents 2 to 19-year-old of age to be 17% in the United States and continues to increase. [3] In addition to the known numerous health complications and the development of comorbidities associated with pediatric obesity, this epidemic has created challenges to weight-based medication dosing because of the pharmacokinetic changes associated with obesity. For medication distribution, excess adipose tissue in obese pediatric patients has been described to affect a medication's volume distribution (the amount of medication in the body compared to plasma concentration). Lipophilic medications are more likely to have higher volume distribution into adipose tissue when compared to normal-weight pediatric patients. In contrast, hydrophilic medications may have increased or decreased volume distributions, altering the medication loading dose.[4]
[3] In addition to the known numerous health complications and the development of comorbidities associated with pediatric obesity, this epidemic has created challenges to weight-based medication dosing because of the pharmacokinetic changes associated with obesity. For medication distribution, excess adipose tissue in obese pediatric patients has been described to affect a medication's volume distribution (the amount of medication in the body compared to plasma concentration). Lipophilic medications are more likely to have higher volume distribution into adipose tissue when compared to normal-weight pediatric patients. In contrast, hydrophilic medications may have increased or decreased volume distributions, altering the medication loading dose.[4]
Due to the alterations in medication loading doses, obese pediatric patients may be at risk for either medication toxicity or sub-therapeutic medication therapy. Studies have described the use of ideal body weight for the calculation of hydrophilic medication loading dose, total body weight for lipophilic medications loading dose, and adjusted body weight for a partially lipophilic medication loading dose.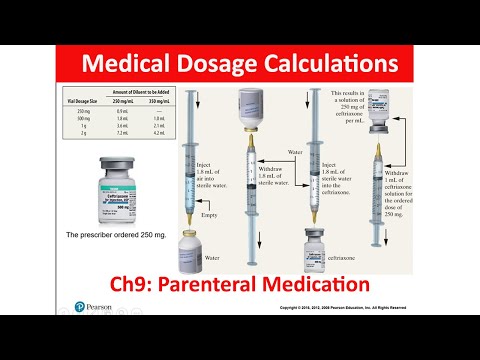 [5][6] Pediatric obesity's effects on pharmacokinetic changes in medication absorption, metabolism, and excretion remain an area in need of further research.[4]
[5][6] Pediatric obesity's effects on pharmacokinetic changes in medication absorption, metabolism, and excretion remain an area in need of further research.[4]
Clinical Significance
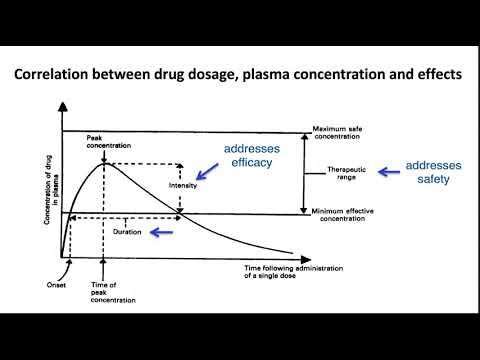
Medication dosing for pediatric patients is described to use either the following methods for medication dosing: age-based dosing, allometric scaling, body surface area-based dosing, and weight-based dosing; neither method is to be more superior to the other and varies based on a medication's chemical properties and the age of the patient.[7] Weight-based dosing is the most commonly used method for calculating recommended medication doses in pediatric clinical practice.[8] Some have thought that adult medication dosages are universally applied to pediatric patients when in fact, this is a misconception. Pediatric patient pharmacokinetics and pharmacodynamics vary in age, body weight, body surface area, and developmental growth and function of various organ systems compared to adults.[7]
The absence of deliberate practice in correct pediatric medication dosing can have potential effects such as exposing the patient to suboptimal medication dosages and severe systemic toxicity, which may even result in fatalities.
Nursing, Allied Health, and Interprofessional Team Interventions
Nursing and pharmacy should be familiar with Clark's rule since they will be preparing/dispensing and administering the medications to infants and children. This way, they can add another layer of safety when administering drugs to children and reach out to the prescribing or ordering clinician if they suspect an incorrect dose when using Clark's rule. This interprofessional system of checks and balances can optimize patient outcomes. [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Elias GP, Antoniali C, Mariano RC. Comparative study of rules employed for calculation of pediatric drug dosage. J Appl Oral Sci. 2005 Jun;13(2):114-9. [PubMed: 20924533]
- 2.
Accorsi R, Karp JS, Surti S. Improved dose regimen in pediatric PET. J Nucl Med. 2010 Feb;51(2):293-300.
 [PubMed: 20080887]
[PubMed: 20080887]- 3.
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988-1994 Through 2013-2014. JAMA. 2016 Jun 07;315(21):2292-9. [PMC free article: PMC6361521] [PubMed: 27272581]
- 4.
Kendrick JG, Carr RR, Ensom MH. Pharmacokinetics and drug dosing in obese children. J Pediatr Pharmacol Ther. 2010 Apr;15(2):94-109. [PMC free article: PMC3018176] [PubMed: 22477800]
- 5.
Kendrick JG, Carr RR, Ensom MH. Pediatric Obesity: Pharmacokinetics and Implications for Drug Dosing. Clin Ther. 2015 Sep 01;37(9):1897-923. [PubMed: 26361823]
- 6.
Matson KL, Horton ER, Capino AC., Advocacy Committee for the Pediatric Pharmacy Advocacy Group. Medication Dosage in Overweight and Obese Children. J Pediatr Pharmacol Ther. 2017 Jan-Feb;22(1):81-83. [PMC free article: PMC5341538] [PubMed: 28337087]
- 7.
Bartelink IH, Rademaker CM, Schobben AF, van den Anker JN. Guidelines on paediatric dosing on the basis of developmental physiology and pharmacokinetic considerations. Clin Pharmacokinet. 2006;45(11):1077-97. [PubMed: 17048973]
- 8.
Pan SD, Zhu LL, Chen M, Xia P, Zhou Q. Weight-based dosing in medication use: what should we know? Patient Prefer Adherence. 2016;10:549-60. [PMC free article: PMC4835122] [PubMed: 27110105]
Children's dosage: measure correctly - Letidor
Despite the fact that the dosages are indicated in the instructions for the drug, the question: "How to calculate the amount of medicine for a child?" - I hear it very often. And this is good. It is much worse if the mother does not think about it and gives the baby an extra second or even third pill to enhance the effect.
But even if parents understand the meaning of children's dosage, they do not always know the practical details. For example, not all tablets can be cut in half, and not all teaspoons are equally useful in measuring five milliliters.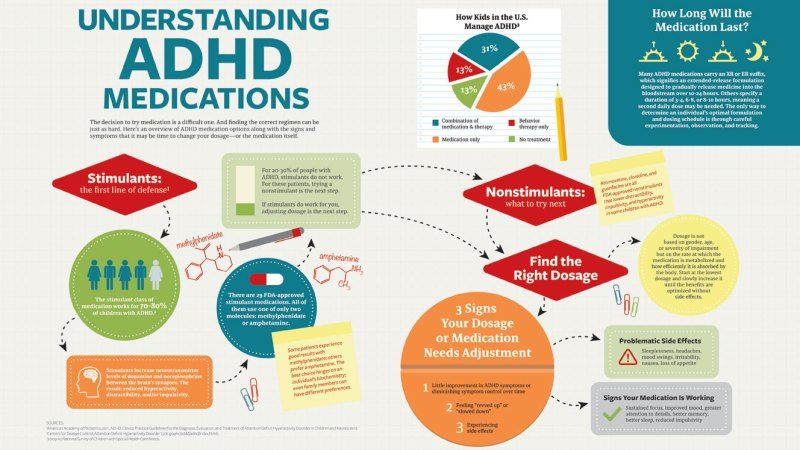
Limits of the norm
There are two main doses for any drug:
Maximum single dose - how much you can drink at one time.
Maximum daily is the total amount of medication per day.
They are especially important for over-the-counter products, the instructions for which parents rarely read, considering them harmless. Which is not true at all. These doses should not be exceeded in any case, the consequences can be varied, but always unpleasant, sometimes even downright dangerous. From the instructions, you can generally learn a lot of interesting things, for example, that acetylsalicylic acid should not be given to children under 12 years old.
Under 16 and over
Children's doses are calculated based on body weight. Age also matters, but if a too well-developed girl weighs 40 kg at 10 years old, she will need the same amount of the drug as a 15-year-old asthenic boy with the same weight.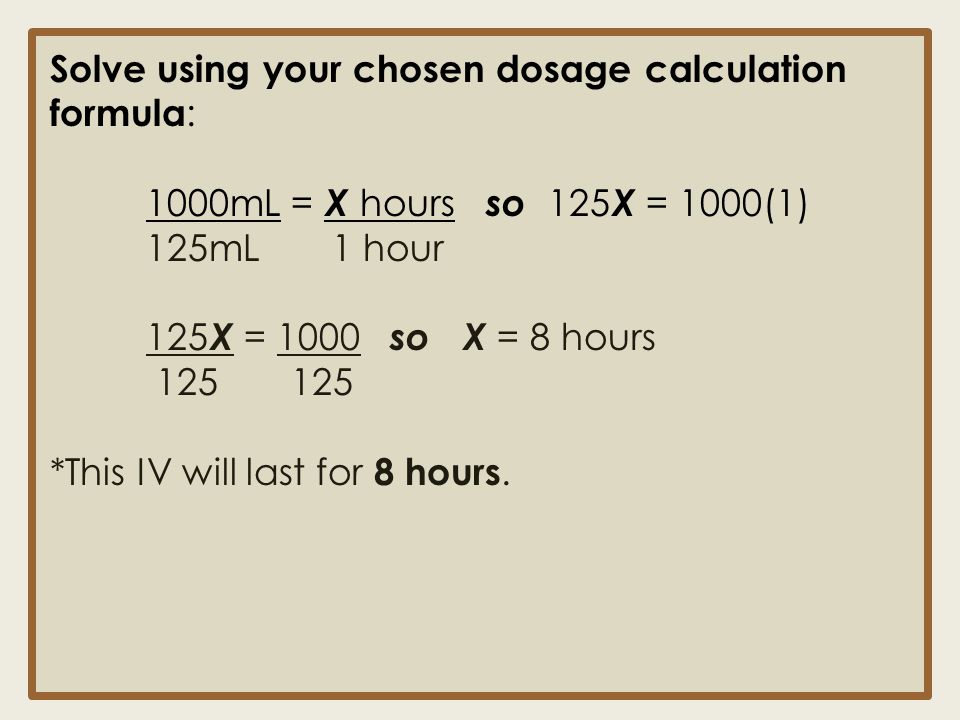 That is why all instructions indicate not only the age, but also the weight category of the child.
That is why all instructions indicate not only the age, but also the weight category of the child.
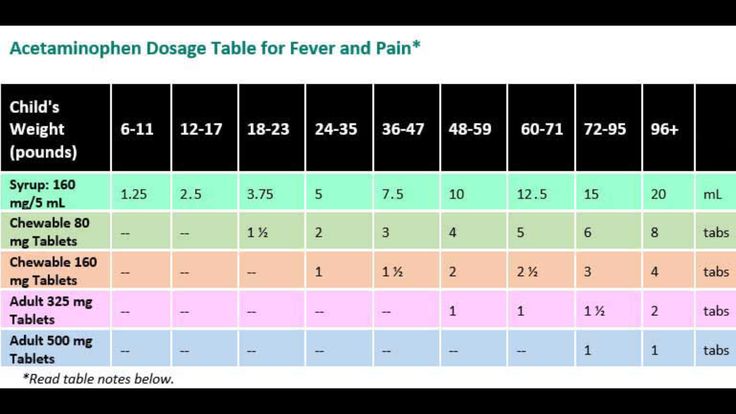
Example: Maximum daily doses of paracetamol (do not forget to count ALL paracetamol included in hot drinks, syrups, suppositories, etc.).
- up to 6 months (up to 7 kg) - 350 mg
- from 6 months to a year (up to 10 kg) - 500 mg
- 1-3 years (up to 15 kg) - 750 mg
- up to 22 kg) — 1 g
- 6–9 years (up to 30 kg) — 1.5 g
- 9–12 years (up to 40 kg) — 2 g
Important! There are no universal rules for calculating the dose that could guarantee the effectiveness and safety of the use of drugs in children, especially newborns. The pediatrician should correctly prescribe the drug.
Indivisible whole
Many people think that it is enough to split a tablet in half and the required dosage will be observed! You can break it only if there is a special groove.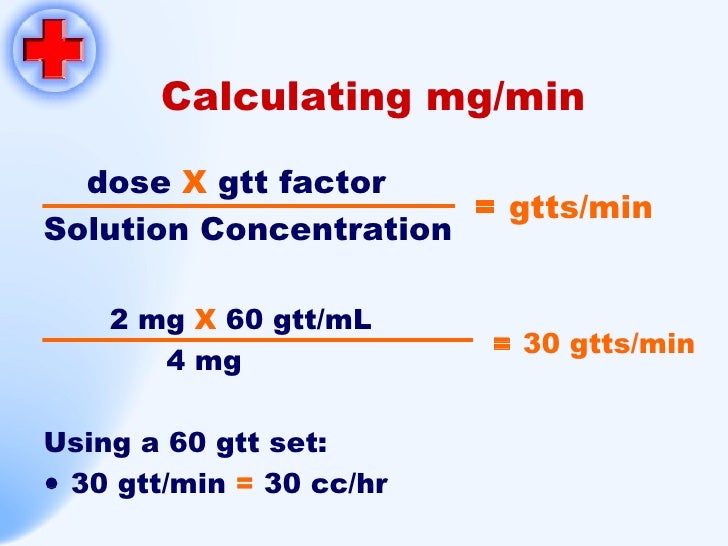 In other cases, special medicines with multiple doses are required. Why is it so?
In other cases, special medicines with multiple doses are required. Why is it so?
Firstly, during production it is almost impossible to mix the mass to a homogeneous state and make sure that exactly 50% of the necessary ingredients are in the half. Studies have shown that this percentage ranges from 20 to 80. And the spread of dosages will be the higher, the more components in the drug.
Secondly, in addition to the main active ingredient in the tablet, there is also a lot of auxiliary, added not at all in a 1:1 ratio. And when dividing them, it will turn out less than what is required for the correct "work" of the medicine.
_ Important! Never replace "baby" doses with half or quarter "adult" doses. This is fraught with an overdose, especially in young children. _
A spoon for mother
Liquid dosage forms are sometimes measured incorrectly. Most people are sure that a teaspoon is 5 ml, a dessert spoon is 10 ml, and a tablespoon is 15 ml. But firstly, there are tablespoons and 20 ml each, and teaspoons - 7.5 ml each. Secondly, not everyone fills even a standard spoon exactly to the brim.
But firstly, there are tablespoons and 20 ml each, and teaspoons - 7.5 ml each. Secondly, not everyone fills even a standard spoon exactly to the brim.
American scientists from Cornell University conducted a study, and it turned out that when using medium-sized spoons, patients receive 8.4% less of the drug, and when measuring the remedy with large spoons, 11.6% more. At the same time, every fifth participant in the experiment was sure that in both cases the medicine would give the same effect.
The consequences of a single over- or underdose are insignificant, but for people who have to take the medicine every 4-8 hours for several days, this difference between the recommended and actual dose can be significant.
_ Important! Use cutlery only if the medicine does not come with a special measuring container - a cap or a spoon. _
Herbs for the baby
The most difficult situation is with the use of medicinal plants in children. Unfortunately, the recommendations on the packages, as a rule, apply only to adult patients. Many mothers brew herbs for a child “as written on the pack”, that is, an adult dose, and at the same time receive an overdose of a medicinal substance, which can result in allergic, toxic reactions, and deterioration in well-being. But the herbs will be completely innocent! So that they give only strength and health, we present the most commonly used children's dosages.
Unfortunately, the recommendations on the packages, as a rule, apply only to adult patients. Many mothers brew herbs for a child “as written on the pack”, that is, an adult dose, and at the same time receive an overdose of a medicinal substance, which can result in allergic, toxic reactions, and deterioration in well-being. But the herbs will be completely innocent! So that they give only strength and health, we present the most commonly used children's dosages.
Dosages of herbs and herbs (based on 2 days): - 8-10 years - 0.5 l heaping tablespoon Since the activity of plant biological substances is preserved in solution for up to 2 days, it is very convenient to prepare a medicinal infusion immediately for 2 days. Store it in the refrigerator and warm up to room temperature before use. The child should drink half of the prepared dose per day (about a glass on average). Divide it into 3-5 doses. Up to 3 years old - from 1 to 3 tablespoons per dose, over 3 years old - about 1/3 cup. It is desirable to vary the daily dose depending on the constitution and weight of the children. For thin people, we reduce it by about 1/5. We increase the "dumplings" by the same amount. Usually these variations come down to the presence or absence of a slide in a spoonful of dry grass. If you use medicinal plants and fees in filter bags, be guided by such children's dosages (based on 2 days): Restrictions on the use of herbs in children of the first year of life are mainly due to the immaturity of most enzyme systems. They are not always able to provide an adequate response to the intake of new chemicals into the body, so an allergic or toxic reaction may develop, explains _ Olga DANILYUK , phytotherapeutist, candidate of medical sciences, assistant of the Department of Phytotherapy of the FPCMR PFUR. For example, the younger the baby , the higher the risk of toxic effects of peppermint and menthol essential oils on the central nervous system. With their overdose, convulsions and vomiting are possible, especially in children of the first 6 months of life. Mint is not prescribed for children of the first year of life. With age, the threat of poisoning with peppermint oils or menthol decreases markedly, and after 3 years there is no danger anymore. Caution should also be taken with celandine. It contains potent substances that can have a toxic effect on an infant. A direct contraindication to its use is convulsive readiness or past convulsions. Before 3 months, it is better not to use celandine at all. It is better not to give alcohol tinctures to children under 5–7 years old (as well as pregnant women), replacing them with non-alcoholic analogues. If there is no way out, you will have to expel ethanol from the herbal remedy at home. If there is nowhere to hurry, then it is possible without boiling, for a day at room temperature, and this option is preferable. Please note that the medicine spoils quickly in this form, so you need to store it in the refrigerator. Alcohol tinctures are usually dosed at the rate of a drop for the current year of life. For example, a child is 3 years and 4 months old, which means that the 4th year of life has already begun, so we give 4 drops of tincture 2-3 times a day. When a child has a high temperature, we usually take out Nurofen or Paracetamol for children from the medicine cabinet and do not think about the fact that there should be some special dosage of Nurofen syrup for a child according to his weight (well, or the dosage of Paracetamol). You might be interested in reading: If your child is often sick: 3 ways to boost immunity However, this approach is not always effective. As an example, after taking the syrup, the baby's temperature drops badly and soon rises again. Which forces us to give the child an antipyretic again. Before using the medicines listed in this article, you should consult with your pediatrician. Let me remind you that I am not a doctor. And just a mother who shares her observations and experiences. Therefore, this text can be considered only as another source of information on this topic, and not as a guide to action. Well, I think we understood each other) Content of the article: Alice was 9 or 10 months old (I don't remember exactly) when she had a high temperature for several days. In general, if you still use a mercury thermometer, I strongly advise you to take a closer look at its non-contact counterpart. Yes, I know, some mothers are wary of this device. And some of the owners, perhaps, even had time to be disappointed. But, I'll tell you - this is not a reason to refuse such a necessary and very convenient device) You can read about why an infrared thermometer often lies and how to measure the temperature with it correctly, you can read in my article: Non-contact thermometer for a child - a convenient device that lies? So, back to our story. "How do you calculate the dose of antipyretic?" the doctor asked me. So, what does it turn out to be? Take, for example, the instructions for Nurofen syrup. And, we see that for a child aged 3 months. up to 12 months a single dose of syrup is 2.5 ml. It is also worth mentioning the fact that children of the same age may have different weights. Some kids are overweight and some are underweight. One child weighs 5 kg at 3 months, and the other, of the same age, 8 kg. In order for the syrup to work effectively, we need to calculate its maximum allowable SINGLE dose. Carefully read the instructions for Nurofen: "The maximum DAILY dose should not exceed 30 mg/kg of the child's body weight with intervals between doses of the drug 6-8 hours. Usually, children under one year of age are weighed every month at the clinic during a preventive examination. Of course, there is always an error on such scales (however, as on any scales), so it is better to round the result down a little. Now, let's solve a mathematical problem. The maximum single dose of syrup, as we have already found out, is 10 mg/kg of the child's weight. It is necessary to calculate a single dose of Nurofen syrup in milliliters for a child weighing 8.5 kg. Let us first calculate a single dose of Nurofen in mg: In 5 ml - 100 mg of ibuprofen, and in x? ml - 85 mg. Why am I describing all this here? But because on a decree from such a seemingly easy example, the brain can melt even for mothers-mathematicians) Therefore, swearing, when once again I had to surf the Internet and remember those damned proportions, I gave my word to make things easier for myself. And I made an online calculator, where I entered the formula for calculating the SINGLE dosage of Nurofen syrup for a child by weight. So, you just need to enter the weight of the child in kg. in the specified field. Enter the child's weight in kg. A single dose of syrup will be: 0 ml. ATTENTION!!! IMPORTANT! Subscribe to the blog "MamaNastya" by e-mail : Email address
 _
_
Removing alcohol 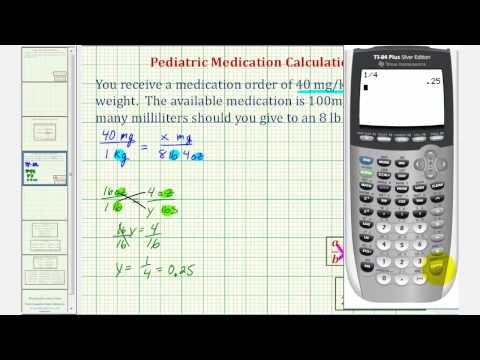 If it is urgent, you can pour the prepared liquid into a dish with a wide mouth and hold it for 5-7 minutes without a lid in a boiling water bath.
If it is urgent, you can pour the prepared liquid into a dish with a wide mouth and hold it for 5-7 minutes without a lid in a boiling water bath. Nurofen syrup dosage for a child by weight + calculator
We simply look at the instructions for these drugs and give the child the exact amount of suspension indicated in it, based on his age.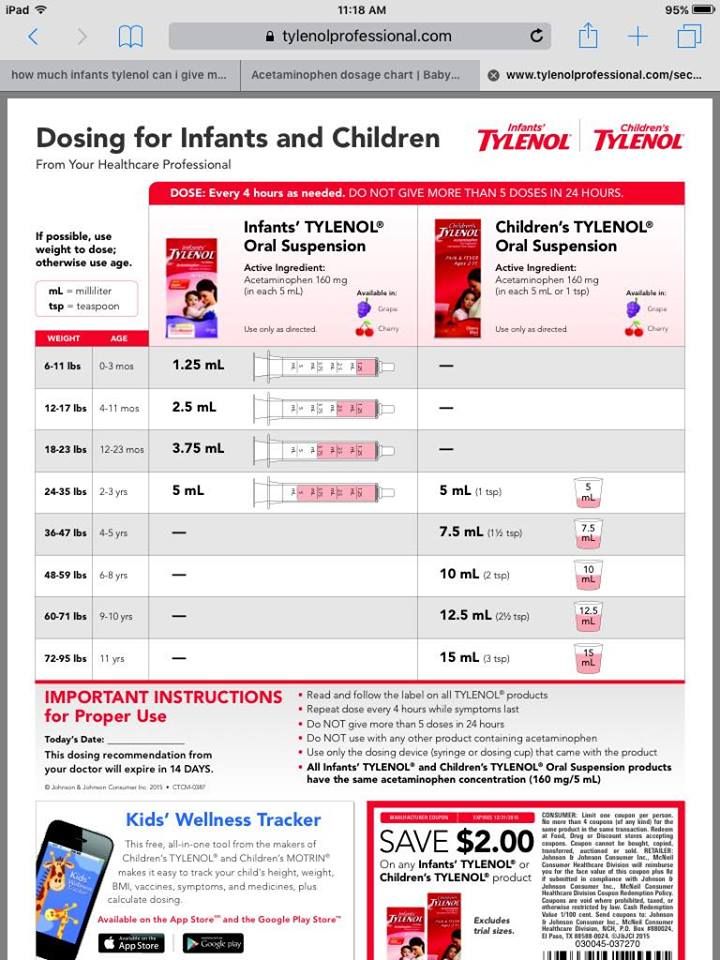
Why this happens and how it can be avoided will be discussed in this article.
Background 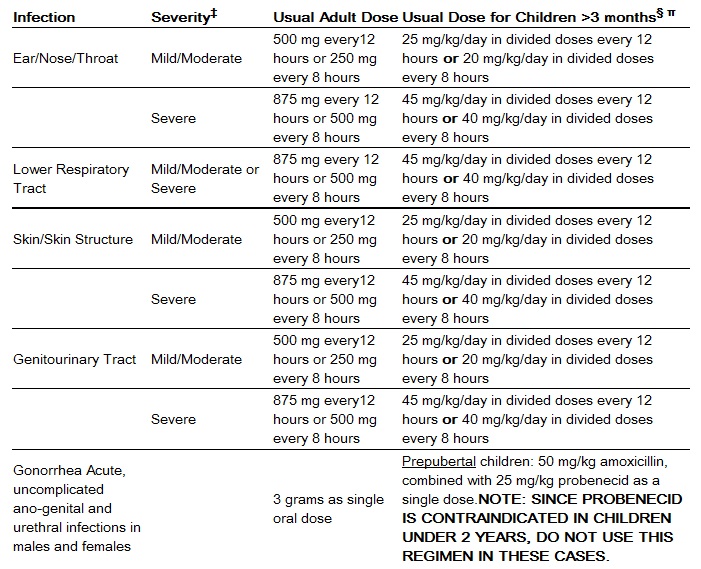 Which didn't crash.
Which didn't crash.
More precisely, after taking the antipyretic, the temperature dropped slightly, but then quickly rose again.
I, on the advice of our local pediatrician, alternated Nurofen and Paracetamol syrups, as well as suppositories.
But, one night, we even had to call an ambulance, because. in the evening, despite taking antipyretics, Alice's temperature remained at the same level.
I remember she was sleeping, and I measured her sleeping temperature probably every 20 minutes. It is good that a non-contact thermometer was used for this purpose. I can't imagine how you can monitor the temperature of a sleeping child with an ordinary thermometer... 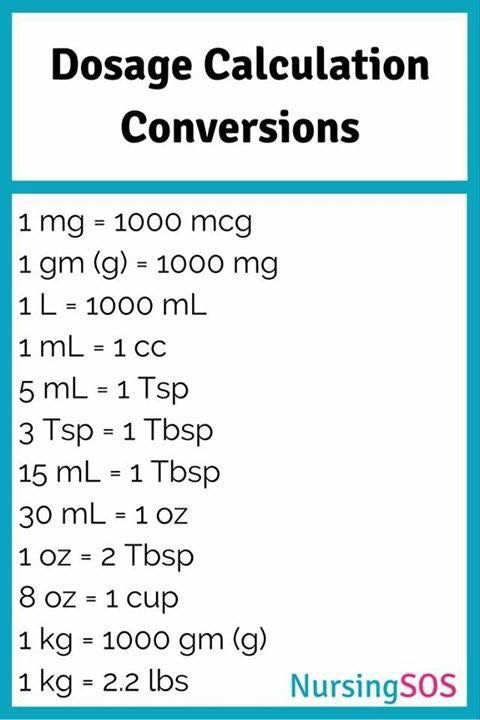 The ambulance arrived only 2 hours after the call. And just by that time, thank God, my daughter's temperature dropped to 38.
The ambulance arrived only 2 hours after the call. And just by that time, thank God, my daughter's temperature dropped to 38.
Of course, the ambulance doctor did not give any injections, because the temperature has already dropped.
In response to the doctor's question about our complaints, I told him about a badly fluctuating temperature.
“I give according to the instructions, of course. According to our age,” I replied.
“Didn't you know that the instructions contain general recommendations, average doses are indicated? The specific dose must be calculated individually according to the weight of your child. If you gave 2.5 ml, then this is not enough for your weight, ”the ambulance doctor said and left.
No, I didn't know that. For me, the words of the ambulance doctor became news. How is it to calculate the antipyretic according to the weight of the child? And I climbed to enlighten on this topic on the Internet.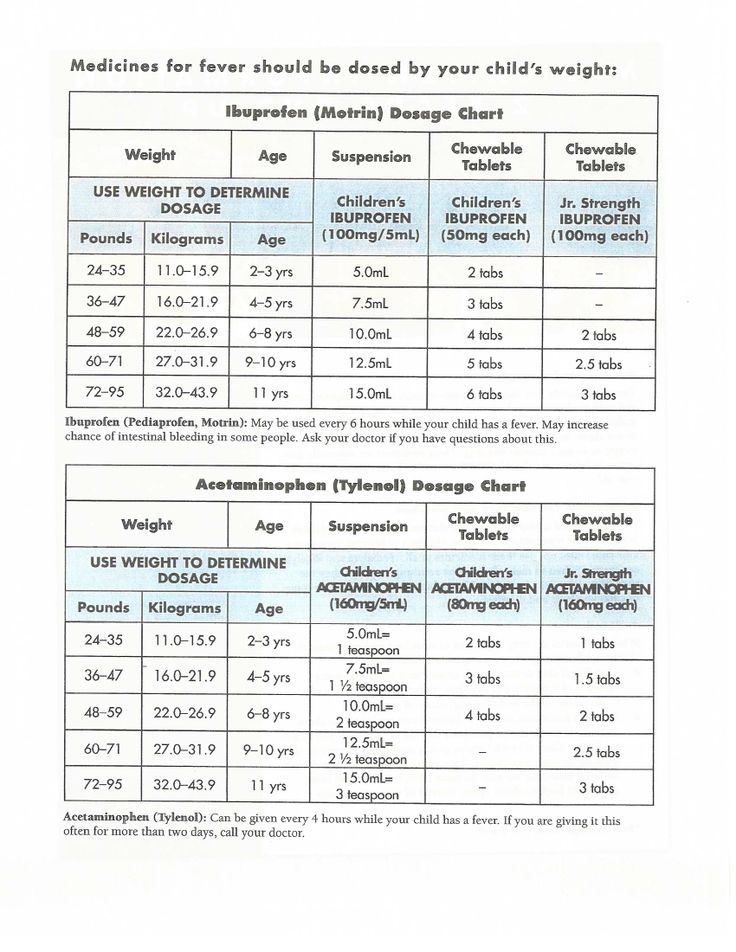
Why it is necessary to calculate the dose of antipyretic syrups for a child according to his weight
And the fact that, according to pediatricians, in the overwhelming majority of cases, the reason for the high “irreducible” temperature is the WRONG dosage of the antipyretic drug.
Indeed, the calculation of the dose of antipyretics should be made depending on the weight of the child, and not his age.
Only, up to 6 months. this syrup can be given only three times a day.
A from 6 months. up to 12 months - It is permissible to give already 4 times a day.
As a result, nevertheless, it turns out that the SINGLE dose for a three-month-old baby and a ten-month-old baby is the SAME.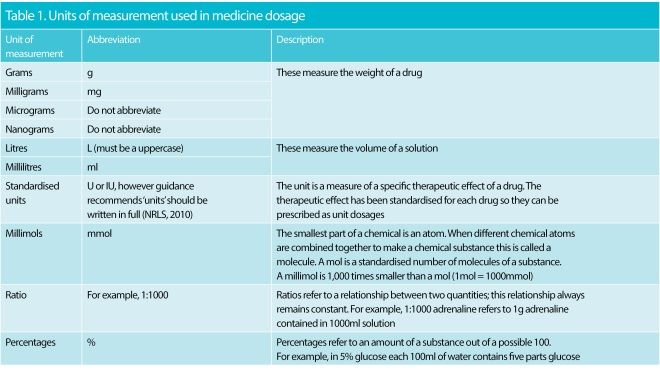
But, after all, the weight of a three-month-old and a ten-month-old child can differ by half!
And it becomes completely unsurprising that a single dose of 2.5 ml. Nurofen, which is enough to reduce the temperature of a three-month-old baby weighing 5 kg, for a 10-month-old baby weighing 9 kg. - is no longer sufficient.
Therefore, it is so important to calculate the dose of antipyretic syrups for a child precisely by his weight, and not by age.
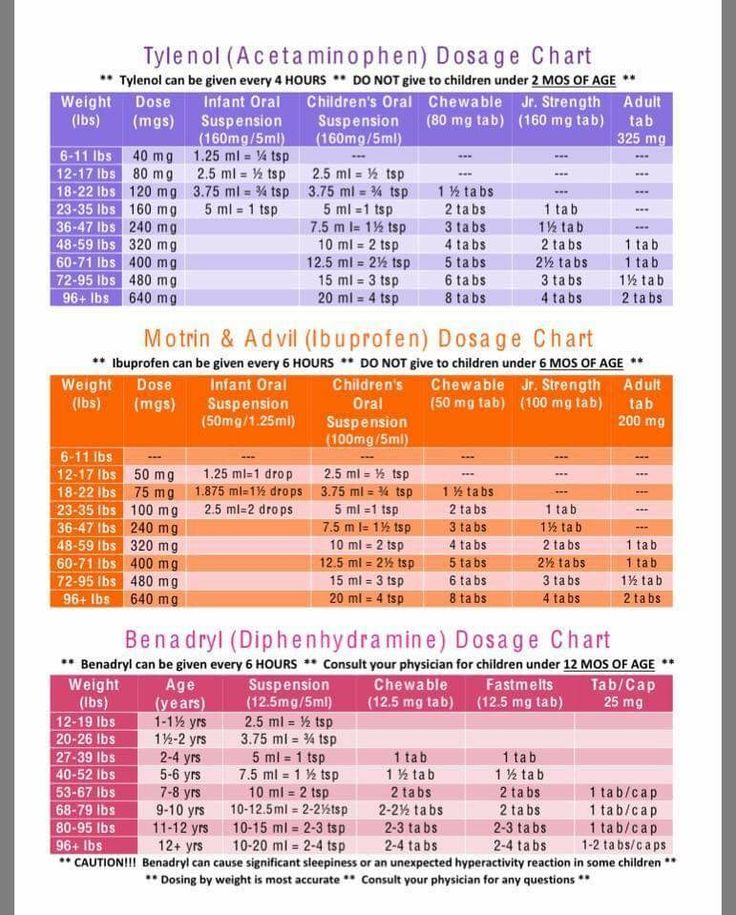
Dosage of Nurofen syrup for a child by weight
How to calculate the maximum allowable single dose of Nurofen syrup
 "
"
From this it follows that the maximum SINGLE dose of Nurofen syrup is 10 mg/kg of the child's weight.
Now, we need to know the baby's weight.
How to find out the weight of a child
Also, many houses have bathroom scales. A small child can also be weighed on them)
For example, I do it this way. I take the child in my arms, I stand with him on the scales. For an accurate measurement, the child must be calm at this moment. I write down our total weight with the child.
Next, I let the child play and stand on the scales alone.
Weighed - recorded.
Then I simply subtract my weight from our total weight with the child. We get a net child's weight) 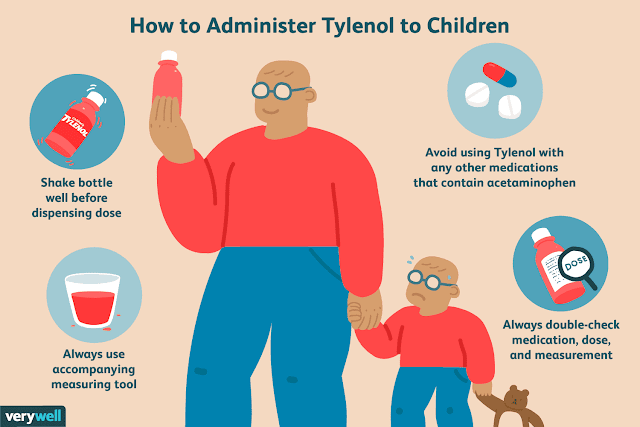
Especially if the child was weighed in clothes and in a diaper (here you can safely deduct 200-300 gr).
If, say, the weight of a child in clothes and in a diaper when weighed on floor scales turned out to be 8,750, it is better to take the figure 8,500 (8.5) for calculations.
An example of calculating a single dose of Nurofen syrup
Let's take a child weighing 8.5 kg as an example.
Look at the instructions for Nurofen: 5 ml. the drug contains 100 mg. the active ingredient is ibuprofen.
8.5 x 10 mg/kg = 85 mg - a single dose of suspension. 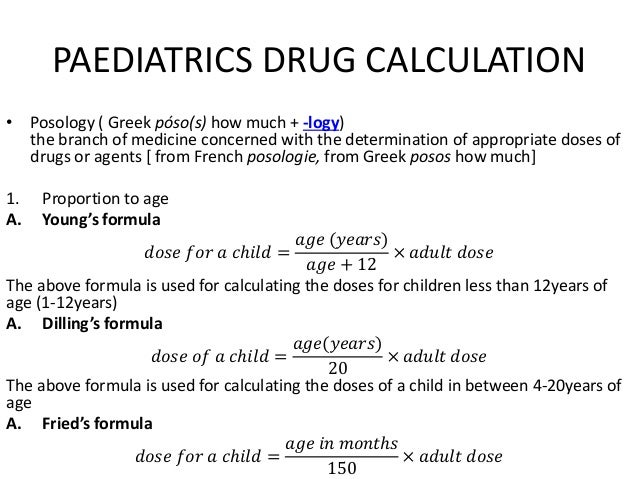
Using the proportion method, we derive a single dose of Nurofen syrup: (5*85/100) = 4.25 ml. Round up to 4.3 ml.
That's it, we have calculated the maximum single dose of Nurofen. We do not exceed this single dose, i.e. we give it no more than 3 times a day.
I'm already silent about the humanities moms, to which I also belong.
Maybe my children rarely get sick (pah-pah-pah!!!), so I don't remember by heart all these milliliters, milligrams and proportions. I will say one thing - when my daughters get sick, I have no time for calculations. But, it has to. 
If you, like me, are too lazy to remember and calculate the dosage of antipyretic syrup every time, you can also use it.
If the number is not round, enter through a comma or a dot, for example, 8.5 (or 8.5) and see the result in the lower right corner (syrup 100 mg/5 ml) for a child by weight
Cool, right? ))) And no problems with calculations)
Sometimes, for technical reasons and due to high traffic to this page, calculators may be temporarily unavailable for calculations.
If you plan to repeatedly use calculators and want to have quick access to them, I recommend subscribing to my blog
Dosage of paracetamol syrup for a child by weight Different syrups - different dosages
I want to warn - on sale there are several types of antipyretic syrups with active substance paracetamol.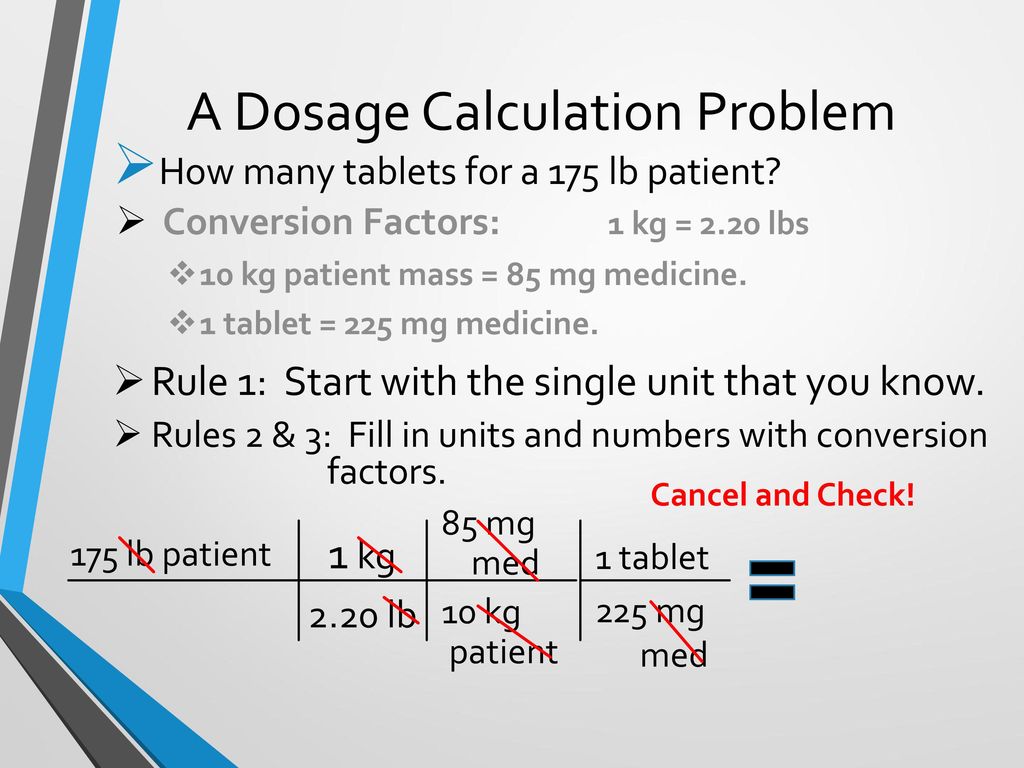 For example, there are syrups with the same name Paracetamol, there is Panadol syrup and there is Efferalgan. Maybe some more Yes, I just know these.
For example, there are syrups with the same name Paracetamol, there is Panadol syrup and there is Efferalgan. Maybe some more Yes, I just know these.
The dosages of these syrups may vary! Be careful! Be sure to check the instructions for how much active ingredient (paracetamol) your syrup contains.
For example, in 1 ml syrup "Efferalgan" contains 30 mg of paracetamol. I warn you right away if you have Efferalgan, the calculations below and the calculator are NOT for this suspension. count dosage yourself.
The instructions for Panadol syrup indicate that in 5 ml. The drug contains 120 mg. paracetamol.
We also had a syrup with the same name "Paracetamol", with the same amount of active ingredient as "Panadol". That is, there is also 5 ml. syrup contains 120 mg. paracetamol.
This ratio is exactly 5 ml/120 mg. in syrups with the active ingredient "Paracetamol" is considered the most popular.
But, I repeat once again - be sure to look at the composition of the suspension!
Personally, I don't want to get confused and now I always buy Panadol Baby syrup.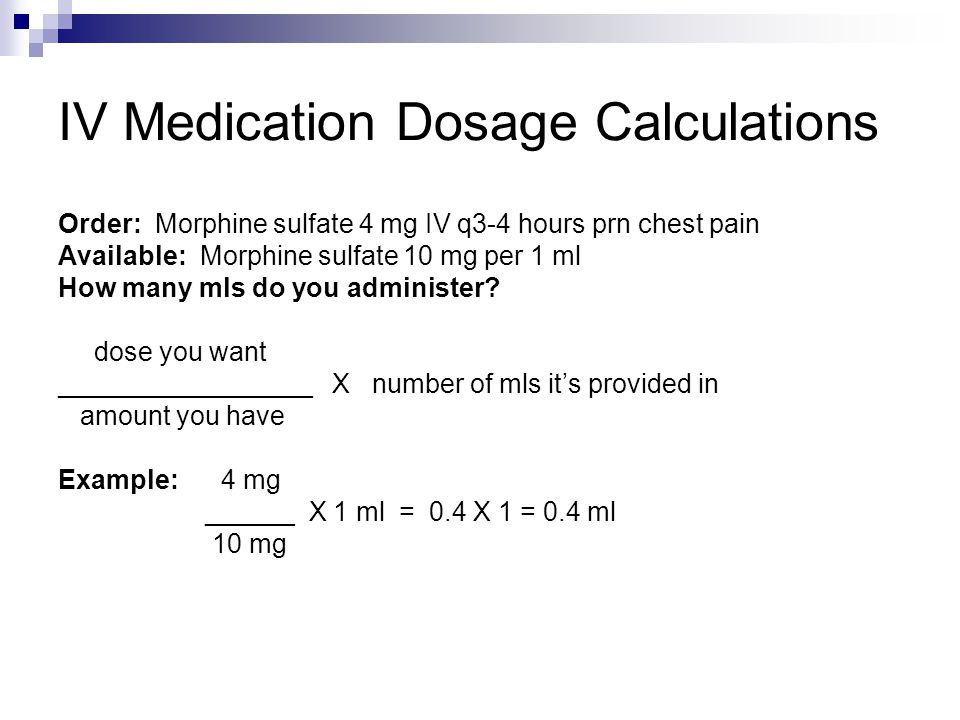 A syrup with this name is popular; it is on sale in any pharmacy. And, importantly, it comes with a measuring syringe.
A syrup with this name is popular; it is on sale in any pharmacy. And, importantly, it comes with a measuring syringe.
I remember the cheaper syrup called Paracetamol only came with a scoop. I can’t and don’t like to give syrup from a spoon. It seems to me that only a syringe can measure the exact amount of suspension. That's why I prefer Panadol.
By the way, I prefer to buy antipyretic syrups, as well as other important preparations for a child's first aid kit, in advance. And the Internet service zdravcity.ru
helps me in this If you are not familiar with this very convenient and profitable service, you can read my review article:
Why do we choose the Zdravcity service
An example of calculating a single dose of Paracetamol syrup
So, I have Panadol syrup, 5 ml. which contains 120 mg. the active substance is paracetamol.
For calculating one-time dosages, we read the instructions, which already indicate the maximum SINGLE dose - 15 mg/kg.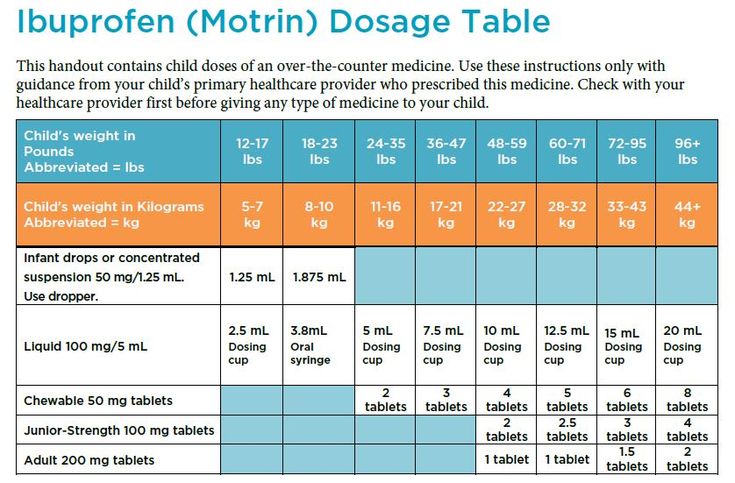 child's weight.
child's weight.
For example, let's take the same weight of a child - 8.5 kg.
Let us first calculate a single dose of "Panadol" in mg:
8.5 x 15 mg / kg = 127.5 mg - a single dose of Panadol.
But, we need a single dose in milliliters.
In 5 ml - 120 mg of paracetamol, and in x? ml - 127.5 mg.
Using the proportion method, we derive a single dose of Panadol syrup:
(5 * 127.5 / 120) = 5.3 ml. - this is the maximum single dose of Panadol syrup, which can be given up to 4 times a day, not more than . So that the daily dose does not exceed the figure indicated in the instructions of 60 mg / kg. child's weight.
I painted everything tediously again, didn't I? )))
And why))) When you can just enter the weight of the child here and the calculator will calculate everything for us:
Calculator "Paracetamol syrup dosage for a child by weight"
child by weight
Enter the child's weight in kg.