How many people have o neg blood
Blood Types Explained - A, B, AB and O
How Blood Type Is Determined And Why You Need To Know
Blood types are determined by the presence or absence of certain antigens – substances that can trigger an immune response if they are foreign to the body. Since some antigens can trigger a patient's immune system to attack the transfused blood, safe blood transfusions depend on careful blood typing and cross-matching. Do you know what blood type is safe for you if you need a transfusion?
Discover what blood types are compatible with yours.
Get our guide to find out.
Download Guide
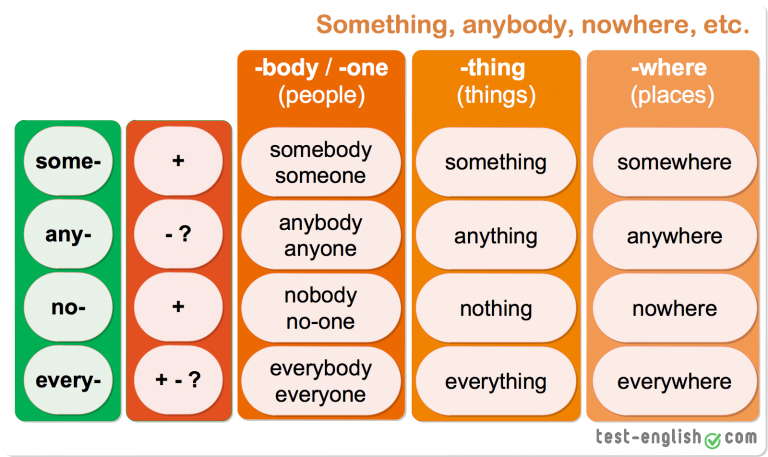
There are four major blood groups determined by the presence or absence of two antigens, A and B, on the surface of red blood cells. In addition to the A and B antigens, there is a protein called the Rh factor, which can be either present (+) or absent (–), creating the 8 most common blood types (A+, A-, B+, B-, O+, O-, AB+, AB-).
",xd="",yd="
",zd="",Ad='
There are very specific ways in which blood types must be matched for a safe transfusion. The right blood transfusion can mean the difference between life and death. Use the interactive graphic below to learn more about matching blood types for transfusions.
Also, Rh-negative blood is given to Rh-negative patients, and Rh-positive or Rh-negative blood may be given to Rh-positive patients. The rules for plasma are the reverse.
- The universal red cell donor has Type O negative blood.
- The universal plasma donor has Type AB blood.
There are more than 600 other known antigens, the presence or absence of which creates "rare blood types." Certain blood types are unique to specific ethnic or racial groups. That’s why an African-American blood donation may be the best hope for the needs of patients with sickle cell disease, many of whom are of African descent. Learn about blood and diversity.
Learn about blood and diversity.
Universal donors are those with an O negative blood type. Why? O negative blood can be used in transfusions for any blood type.
Type O is routinely in short supply and in high demand by hospitals – both because it is the most common blood type and because type O negative blood is the universal blood type needed for emergency transfusions and for immune deficient infants.
Approximately 45 percent of Caucasians are type O (positive or negative), but 51 percent of African-Americans and 57 percent of Hispanics are type O. Minority and diverse populations, therefore, play a critical role in meeting the constant need for blood.
Types O negative and O positive are in high demand. Only 7% of the population are O negative. However, the need for O negative blood is the highest because it is used most often during emergencies. The need for O+ is high because it is the most frequently occurring blood type (37% of the population).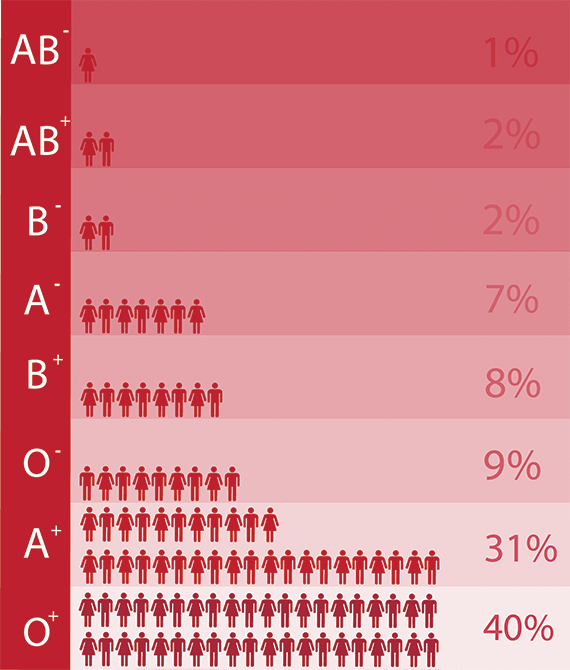
The universal red cell donor has Type O negative blood. The universal plasma donor has Type AB blood. For more about plasma donation, visit the plasma donation facts.
Nearly 16 million blood components are transfused each year in the U.S."
What is your blood type? Donate and find out.
Schedule Your Appointment
There are more than 600 other known antigens, the presence or absence of which creates "rare blood types." Your blood type is considered rare if you lack antigens that 99% of the people are positive for. If you somehow lack an antigen that 99.99% are positive for, your blood type is extremely rare.
It’s inherited. Like eye color, blood type is passed genetically from your parents. Whether your blood group is type A, B, AB or O is based on the blood types of your mother and father.
View all child parent pairings
* Note: If you have questions about paternity testing or about blood group inheritance, your primary care physician should be able to provide you with an appropriate referral. Testing difficulties can cause exceptions to the above patterns. ABO blood typing is not sufficient to prove or disprove paternity or maternity.
Testing difficulties can cause exceptions to the above patterns. ABO blood typing is not sufficient to prove or disprove paternity or maternity.
Make Your Appointment
The rarest and most common blood types by ethnicity
Blood types are a classification of blood based on the antigens present on red blood cells. Antigens are molecules that can trigger an immune system response. There are eight common blood groups but 36 human blood groups in total.
A blood transfusion is a procedure that restores blood to the body. It is essential that people undergoing the procedure receive the correct blood type, or it will trigger the immune system, causing sickness and complications.
According to the American Red Cross, roughly every 2 seconds, a person in the United States requires a blood transfusion. They also note that this procedure saves 4. 5 million lives each year.
5 million lives each year.
In this article, we discuss the rarest and most common blood types by ethnicity.
Share on PinterestA person’s blood type may fall into any of the 36 human blood groups. Getty ImagesPeople can define blood types using the ABO and Rhesus (Rh) blood group systems. These define blood types according to which antigens are present on red blood cells.
ABO system
This system classifies blood types as follows:
- Blood group A has A antigens on the red blood cells.
- Blood group B has B antigens.
- Blood group O has neither A nor B antigens.
- Blood group AB has both A and B antigens.
Rh system
Red blood cells may have another antigen called the Rh antigen on their surface. If it is present, the blood group is Rh-positive, but if it is absent, the blood group is Rh-negative.
Combining these two characteristics yields the eight most common blood types. Most people have one of these types:
Most people have one of these types:
- O-positive
- O-negative
- A-positive
- A-negative
- B-positive
- B-negative
- AB-positive
- AB-negative
The genes that a person inherits from their parents determine the mix of antigens and proteins in their blood.
These genetic factors tend to run in ethnic groups. As such, the American Red Cross suggests that when people, especially those with rare blood types, need blood, the best matches tend to come from people of the same race or ethnic background.
For this reason, some blood centers collect ethnic information from blood donors.
For some conditions, such as thalassemia and sickle cell disease, this matching is even more important because these conditions are more common among certain ethnic communities, and people may need frequent transfusions.
For example, only 2% of donors have a rare subtype of blood that doctors often use to treat sickle cell disease, but demand for it is increasing by 10–15% each year. The rarity of, and demand for, this type of blood emphasizes the importance of blood donors.
The rarity of, and demand for, this type of blood emphasizes the importance of blood donors.
Click here to learn more about blood types.
In the U.S., 38% of the population has O-positive blood, making it the most common blood type.
According to the American Red Cross, the following statistics show the most common blood types in the U.S. based on the donor population:
- African American: 47% O-positive, 24% A-positive, and 18% B-positive
- Latin American: 53% O-positive, 29% A-positive, and 9% B-positive
- Asian: 39% O-positive, 27% A-positive, and 25% B-positive
- Caucasian: 37% O-positive, 33% A-positive, and 9% B-positive
The least common blood type in the U.S. is AB-negative, with less than 1% of the population having this type.
Statistics from the American Red Cross show that the following are the most rare forms of the major eight blood types in the U. S. based on the donor population:
S. based on the donor population:
- African American: 0.3% AB-negative, 1% B-negative, and 2% A-negative
- Latin American: 0.2% AB-negative, 1% B-negative, and 2% both A-negative and AB-positive
- Asian: 0.1% AB-negative, 0.4% B-negative, and 0.5% A-negative
- Caucasian: 1% AB-negative, 2% B-negative, and 3% AB-positive
A and B antigens only represent two of approximately 600 other known antigens that can differentiate blood types. It is important to make a distinction between the rarest of the eight most common blood types and the extremely rare subtypes.
Having an antigen that most people do not have, or missing an antigen that most people do have, means that an individual has a rare blood type.
According to the International Society of Blood Transfusion, if only 1 in 500 people are missing the same antigen as an individual, their blood type is rare. If only 1 in 1,000 people lack it, the individual’s blood type is very rare.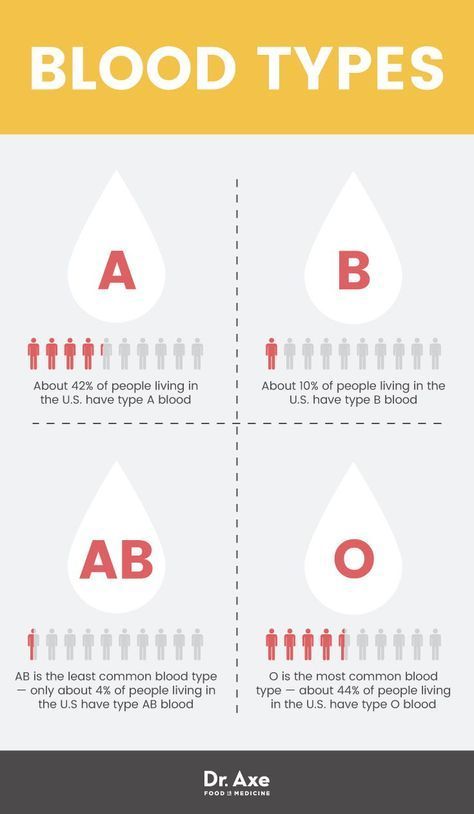
In addition, scientists have identified 36 different blood group systems, some of which can cause problems with blood transfusions.
Some of these rare blood types and blood group systems are distinctly more common in certain ethnic groups. The American Red Cross data below list the rare blood type and the ethnic group in which it is most common:
- African American: U-negative and Duffy-negative blood types
- Native American and Alaskan native: RzRz blood type
- Pacific Island and Asian: JKnull blood type
- Hispanic: Diego B-negative blood type
- East European and Russian Jewish: Drori A-negative blood type
- Caucasian: Kell B-negative and Vel-negative blood types
Experts base blood types on the different antigens and proteins present on red blood cells. To make sure that a transfusion supports an individual’s health instead of causing harm, there must be a good match between the donor’s blood type and that of the recipient.
As an individual’s genetic background influences their blood type, looking at the most common blood type by race or ethnicity can help healthcare professionals acquire and effectively use the most suitable blood and blood products for individuals requiring blood transfusions.
Information about blood and its components
REGIONAL BUDGETARY HEALTH INSTITUTION "KURSK REGIONAL CLINICAL BLOOD CENTER"
- You are here:
- Home
- Information about blood and its components
Questionnaires
School of Transfusiologist
Organizers of donation
Blood groups are genetically inherited traits that do not change during life under natural conditions. The blood group is a certain combination of surface antigens of erythrocytes (agglutinogens) of the ABO system. The definition of group affiliation is widely used in clinical practice in the transfusion of blood and its components, in gynecology and obstetrics in the planning and management of pregnancy.
Attempts to save a patient's life by transfusing another person's blood were made by doctors long before the concept of blood grouping appeared. Sometimes this saved the patient, and sometimes it had a negative effect, up to the death of the patient.
In 1901, a scientist from Austria, Karl Landsteiner, in the course of his experiments, noticed that mixing blood samples taken from different people, in some cases, leads to the formation of clots from clumped red blood cells.
As it turned out, the process of adhesion is caused by an immune reaction, while the immune system of one organism perceives the cells of another as foreign and seeks to destroy them.
In the course of his work, Karl Landsteiner was able to identify and divide people's blood into 3 different groups, which made it possible to select compatible blood and made the transfusion process safe for patients. In the future, the most rare, fourth group was also identified.
Karl Landsteiner was awarded the 1930 Nobel Prize for his work in medicine and physiology.
Group affiliation is formed in the process of intrauterine development and remains unchanged throughout life.
The ancestor of all blood groups is group 0 (I). Most of the people on the globe, about 45%, have this particular group, the rest were formed in the process of evolution, through gene mutations. The second place in prevalence is occupied by group A (II), about 35% of the population, mainly Europeans, have it. Approximately 13% of people are carriers of the third group. The rarest is AB (IV), it is inherent in 7% of the world's population.
Blood type has another important characteristic called the Rh factor.
In addition to antigens A and B, the shell of erythrocytes may contain another type of antigen, called the Rh factor. Its presence is denoted as RH+, its absence as RH-.
The vast majority of the world's population has a positive Rh factor. This antigen is absent only in 15% of Europeans and 1% of Asians.
Transfusion of blood from a non-RH- person from a RH+ person results in an immune defense response. In this case, Rh antibodies are produced and hemolysis and death of red blood cells occur.
In this case, Rh antibodies are produced and hemolysis and death of red blood cells occur.
Otherwise, if a person with a positive Rh factor is transfused with RH- blood, no negative consequences for the recipient occur.
© 2023 Regional budgetary health care institution "KURSK REGIONAL CLINICAL BLOOD CENTER"
Website development
About Blood Types - Blood Center
When a doctor talks about your blood type, he usually means two things: your ABO blood type and your Rh (rhesus factor).
A person's blood group is determined by antigens found on his red blood cells. An antigen is a structure on the surface of a cell. If it is foreign to the body, then the human defense system will react to it. Therefore, it is necessary to take into account blood groups when transfusing: the donor's blood group is determined at the Blood Center, and the patient's blood group is determined before transfusion.
AB0 system
The most important is the ABO blood group system, according to which blood is divided into groups A, B, O and AB.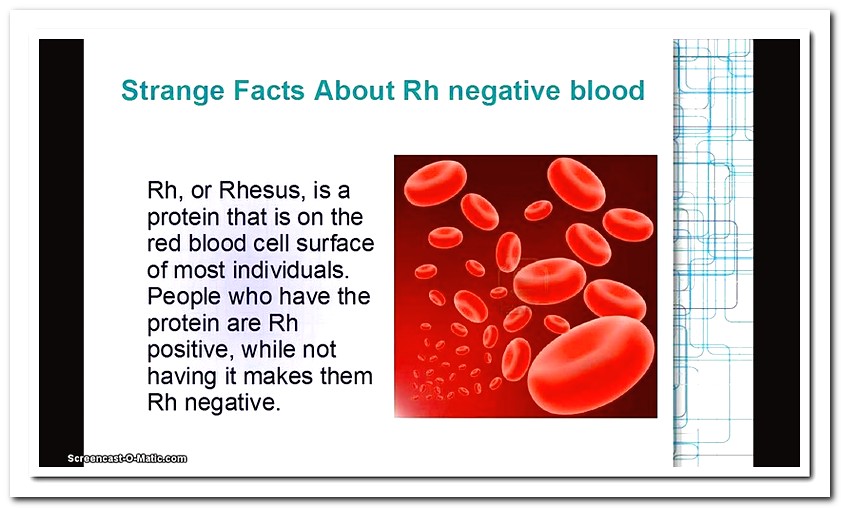 It is determined by two antigens located on the surface of red blood cells:
It is determined by two antigens located on the surface of red blood cells:
- group A - only antigen A is present on the surface of erythrocytes
- group B - only antigen B is present on the surface of erythrocytes
- group AB - both A and B antigens are on the surface of erythrocytes
- group O - on the surface of erythrocytes there is neither antigen A nor antigen B.
If a person has blood type A, B or 0, then in his blood plasma there are also antibodies that destroy those antigens that the person himself does not have. Examples: If you have type A blood, then you cannot be transfused with type B blood, because in this case there are antibodies in your blood that fight against B antigens. If you have blood type 0, then your blood contains antibodies that fight like against antigens A and against antigens B.
If a person has blood type AB, then he does not have such antibodies, so he can be transfused with blood of any group.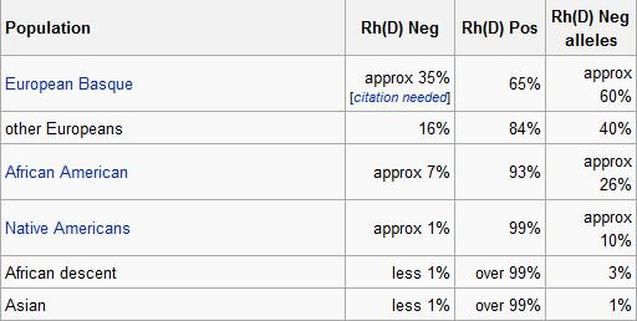 Therefore, a carrier of blood group AB can be called a universal patient .
Therefore, a carrier of blood group AB can be called a universal patient .
A carrier of blood type 0 with a negative Rh factor, in turn, is called a universal donor, , since his red blood cells are suitable for all patients.
Rhesus (Rh ) accessory
Rh factor (Rh) can be positive (+) and negative (-). It depends on the presence of the D antigen on the surface of the red blood cells. If the D antigen is present, the person is considered Rh-positive, and if the D antigen is absent, then the person is Rh-negative.
If a person is Rh negative, contact with Rh positive blood (for example, during pregnancy or blood transfusion) may form antibodies. These antibodies can cause pregnancy problems in an Rh-negative woman if she is carrying an Rh-positive baby.
In addition to the ABO and Rh systems, about thirty more blood group systems have been discovered to date. Clinically, the most important of these are the Kell, Kidd and Duffy systems. According to the Kell system, donor blood is also examined.
According to the Kell system, donor blood is also examined.
How is blood type determined?
To determine the blood type, it is mixed with a reagent containing known antibodies.
Three drops of blood taken from one person are applied to the base: the anti-A test reagent is added to one drop, the anti-B test reagent to the other, and the anti-D test reagent to the third, i.e. Rh test reagent. If blood clots form in the first drop, i.e. erythrocytes stick together (agglutination), then the person has antigen A. If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive.
Donor and recipient blood group compatibility is extremely important, otherwise the recipient may have dangerous reactions to the blood transfusion.
Blood group inheritance
A person inherits from his father and from his mother to the same extent. Therefore, the hereditary substance has a double structure: one part from the mother and the other from the father. Speaking about the inheritance of blood groups, it must be borne in mind that:
Therefore, the hereditary substance has a double structure: one part from the mother and the other from the father. Speaking about the inheritance of blood groups, it must be borne in mind that:
- Most of our genes exist in two copies
- Each parent gives (based on random selection) one of these copies to their children
- Genes occur in different versions (alleles)
- Some versions of the gene are stronger than others
| ABO system | Rh system | ||||||||||||||||||||||||||||||||||
In the AB0 system, antigens are presented in three versions A, B and 0. Given that the hereditary substance includes two parts, six different combinations can occur:
The stronger part appears, both equally or a combination of them.
Example: The mother has a combination of A0 genes in hereditary substance, and her blood type is A (at the same time, she is a carrier of the blood group 0 gene, and there is a possibility that she will pass it on to her child). The father's blood type has the designation 0, and in his hereditary substance there is a combination of genes 00. Accordingly, he can only pass 0 to the child, i.e. absence of antigens. Thus, their child may have an A (A0) or 0 (00) blood type. | |||||||||||||||||||||||||||||||||||
 In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows:
In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows: