How long is the average induced labor
Induced labour | Pregnancy Birth and Baby
What is an induced labour?
Labour normally starts naturally any time between 37 and 42 weeks of pregnancy. The cervix softens and starts to open, you will get contractions, and your waters break.
In an induced labour, or induction, these labour processes are started artificially. It might involve mechanically opening your cervix, breaking your waters, or using medicine to start off your contractions — or a combination of these methods.
In Australia, about 1 in 3 women has an induced labour.
What are the differences between an induced and a natural labour?
An induced labour can be more painful than a natural labour. In natural labour, the contractions build up slowly, but in induced labour they can start more quickly and be stronger. Because the labour can be more painful, you are more likely to want some type of pain relief.
If your labour is induced, you are also more likely to need other interventions, such as the use of forceps or ventouse (vacuum) to assist with the birth of your baby. You will not be able to move around as much because the baby will be monitored more closely than during a natural labour.
You will only be offered induced labour if there is a risk to you or your baby's health. Your doctor might recommend induced labour if:
- you are overdue (more than 41 weeks pregnant)
- there is a concern the placenta is not working as it should
- you have a health condition, such as diabetes, kidney problems, high blood pressure or pre-eclampsia
- the baby is making fewer movements, showing changes in its heart rate, or not growing well
- your waters have broken, but the contractions have not started naturally
- you are giving birth to more than one baby (twins or multiple birth)
Not everyone can have an induced labour. It is not usually an option if you have had a caesarean section or major abdominal surgery before, if you have placenta praevia, or if your baby is breech or lying sideways.
Can I decide whether to have an induced labour?
If you are overdue, you might decide to wait and see if labour will start naturally. However, if there is a chance you or your baby are at risk of complications, you might need to consider induced labour before your due date.
However, if there is a chance you or your baby are at risk of complications, you might need to consider induced labour before your due date.
When making your decision, discuss the risks and benefits with your doctor. Do not be afraid to ask lots of questions, such as:
- Why do I need an induction?
- How will it affect me and my baby?
- What will happen if I do not have the induction?
- What procedures are involved and how will you care for me and my baby?
You might need to consider several other health concerns. For example, there is a higher risk of stillbirth or other problems if your baby is not born before 42 weeks, and an increased risk of infection if your waters break more than 24 hours before labour starts.
What can I expect with an induced labour?
During the late stages of your pregnancy, your healthcare team will carry out regular checks on your health and your baby's heath. These checks help them decide whether it is better to induce labour or to keep the baby inside. Always tell your doctor or midwife if you notice your baby is moving less than normal.
Always tell your doctor or midwife if you notice your baby is moving less than normal.
If they decide it is medically necessary to induce labour, first your doctor or midwife will do an internal examination by feeling inside your vagina. They will feel your cervix to see if it is ready for labour. This examination will also help them decide on the best method for you.
It can take from a few hours to as long as 2 to 3 days to induce labour. It depends how your body responds to the treatment. It is likely to take longer if this is your first pregnancy or you are less than 37 weeks pregnant.
What options are there to induce labour?
There are different ways to induce labour. Your doctor or midwife will recommend the best method for you when they examine your cervix. You may need a combination of different strategies. You will need to provide written consent for the procedure.
Sweeping the membranes
During a vaginal examination, the midwife or doctor makes circular movements around your cervix with their finger. This action should release a hormone called prostaglandins. You do not need to be admitted to hospital for this procedure and it is often done in the doctor's room. This can be enough to get labour started, meaning you will not need any other methods.
This action should release a hormone called prostaglandins. You do not need to be admitted to hospital for this procedure and it is often done in the doctor's room. This can be enough to get labour started, meaning you will not need any other methods.
Risks: This is a simple and easy procedure; however, it does not always work. It can be a bit uncomfortable, but it does not hurt.
Oxytocin
A synthetic version of the hormone oxytocin is given to you via a drip in your arm to start your contractions. When the contractions start, the amount of oxytocin is adjusted so you keep on having regular contractions until the baby is born. This whole process can take several hours.
Risks: Oxytocin can make contractions stronger, more frequent and more painful than in natural labour, so you are more likely to need pain relief. You will not be able to move around much because of the drip in your arm and you will also have a fetal monitor around your abdomen to monitor your baby.
Sometimes the contractions can come too quickly, which can affect the baby's heart rate. This can be controlled by slowing down the drip or giving you another medicine.
Artificial rupture of membranes ('breaking your waters')
Artificial rupture of membranes (ARM) is used when your waters do not break naturally. Your doctor or midwife inserts a small hook-like instrument through your vagina to make a hole in the membrane sac that is holding the amniotic fluid. This will increase the pressure of your baby's head on your cervix, which may be enough to get labour started. Many women will also need oxytocin to start their contractions.
Risks: ARM can be a bit uncomfortable but not painful. There is a small increased risk of a prolapsed umbilical cord, bleeding or infection.
Prostaglandins
A synthetic version of the hormone prostaglandins is inserted into your vagina to soften your cervix and prepare your body for labour. It can be in the form of a gel, which may be given in several doses (usually every 6 to 8 hours), or a pessary and tape (similar to a tampon), which slowly releases the hormone over 12 to 24 hours.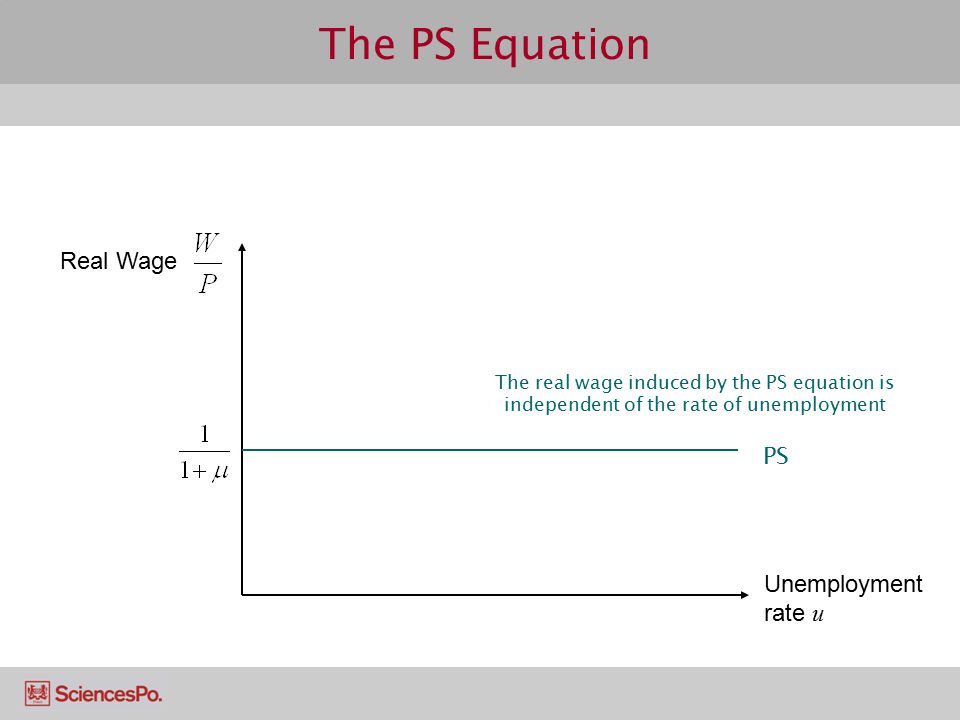 You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
Prostaglandins gel is often the preferred method of inducing labour since it is the closest to natural labour. Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
Risks: Some women find their vagina is sore after the prostaglandin gel, or they might experience nausea, vomiting or diarrhoea. These side effects are rare and there is no evidence that induction using prostaglandin is any more painful than a natural labour.
Very rarely, the contractions can come too strongly, which can affect the baby's heart rate. This can be controlled by giving you another medicine or removing the pessary.
You need to let your doctor or midwife know immediately if you start bleeding, or if your baby is moving less, because this could be a sign that something is wrong.
Cervical ripening balloon catheter
A cervical ripening balloon catheter is a small tube attached to a balloon that is inserted into your cervix. The balloon is inflated with saline, which usually puts enough pressure on your cervix for it to open. It stays in place for up to 15 hours, and then you will be examined again.
Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
You may also need ARM or oxytocin if you are using a cervical ripening balloon catheter.
Risks: Inserting the catheter can be a bit uncomfortable but not painful.
You also need to let your doctor or midwife know immediately if you start bleeding, or your baby is moving less, because this could be a sign that something is wrong.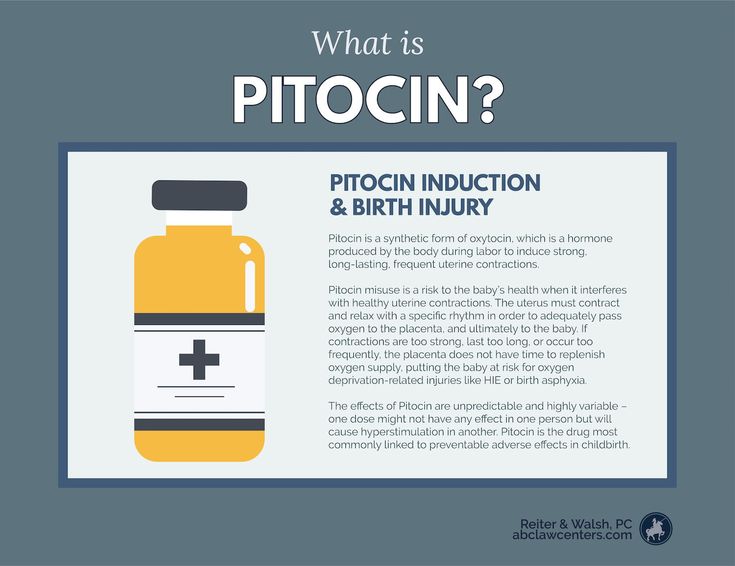
Can I have pain relief during induced labour?
Induced labour is usually more painful than natural labour. Depending on the type of induction you are having, this could range from discomfort with the procedure or more intense and longer lasting contractions as a result of the medication you have been given. Women who have induced labour are more likely to ask for an epidural for relief.
Because inductions are almost always done in hospital, the full range of pain relief should be available to you. There is usually no restriction on the type of pain relief you can have if your labour is induced.
Are there any risks with inducing labour?
There are some increased risks if you have an induced labour. These include that:
- it will not work — in about 1 of 4 cases, women go on to have a caesarean
- your baby will not get enough oxygen and their heart rate is affected
- you or your baby get an infection
- your uterus tears
- you bleed a lot after the birth
What happens if the induction does not work?
Not all induction methods will work for everyone. Your doctor may try another method, or you might need to have a caesarean. Your doctor will discuss all of these options with you.
Your doctor may try another method, or you might need to have a caesarean. Your doctor will discuss all of these options with you.
Learn more here about the development and quality assurance of healthdirect content.
Are You Being Induced? Here's How Long It Takes & What To Expect
Did you just find out that you’re going to be induced?
Do you want to know what it entails and what to expect?
You are in the right place! I have personally induced over 500 women!
In this post, you will learn:
- What an induction of labor is and what to expect,
- How your labor gets induced, and
- How long a typical induction of labor takes.
Are you excited?
Let’s get started.
Disclaimer
***READ FIRST***
Although I am a doctor, I am not your doctor. This information is for informational purposes only and should not substitute the advice from your healthcare professional. All kinds of exercise and dietary changes are potentially dangerous, and those who do not seek counsel from the appropriate health care authority assume the liability of any injury which may occur. Please read my full Disclaimer for more information. Also, this post may contain affiliate links: meaning I may receive a commission if you use them.
Please read my full Disclaimer for more information. Also, this post may contain affiliate links: meaning I may receive a commission if you use them.
Ok, moving on.
What to expect when you’re being induced
When you are being induced there are several things you should expect:
- Expect the entire process to take anywhere from 24-48 hours.
- Depending on the type of induction, expect to have regular painful contractions (every 2-3 minutes).
- Expect to have a vaginal exam every 4-6 hours.
- Expect to have electronic continuous monitoring of your baby’s heart rate.
- Expect to not be able to eat solid foods (you will likely be placed on a clear liquid diet)
- Expect to not be able to walk around after your cervix reaches a certain level of dilation or after your amniotic membranes have been ruptured.
- You may or may not be able to have a support person in the room, especially because of the pandemic.
Okay, now that we have that out of the way, let’s go over all of these in a lot more detail.
How long does it take to give birth after being induced?
An induction of labor can take anywhere from 12 to 24 hours until your baby is born. If you include cervical ripening, the entire process can take 48 hours or more.
Unfortunately, it is impossible to predict how long it will take for you, but we do have standard averages.
It also largely depends on the type of induction you are having.
The different types of induction Methods
There are many different ways we can induce your labor.
The most important factor to determine which induction agent to use is your Bishop Score.
The Bishop Score takes into account:
- How many centimeters dilated you are,
- How effaced your cervix is, (or how thin your cervix is; it’s normally thick)
- The position of your cervix (is it way back posterior, more mid-position, or anterior)
- The consistency of your cervix, (is it firm, medium, or soft), and
- The station.
 (how low is the fetal head relative to your pelvic bone).
(how low is the fetal head relative to your pelvic bone).
Based on these 5 factors, your physician will determine a numerical value from 0 – 13.
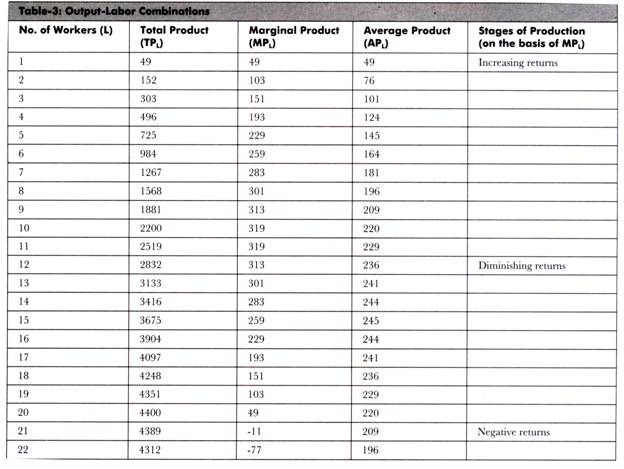
| Score | Dilation | Effacement | Consistency | Position | Station |
|---|---|---|---|---|---|
| 0 | Closed | 0-30% | Firm | Posterior | -3 |
| 1 | 1-2 | 40-50% | Medium | Mid | -2 |
| 2 | 3-4 | 60-70% | Soft | Anterior | -1,0 |
| 3 | 5-6 | 80% | – | – | +1 |
A value greater than 6 indicates a “favorable cervix” meaning you are more likely to have a successful induction.
A value less than 6 indicates a “less favorable bishop score” signifying that your chance of successful vaginal birth is decreased.
If your bishop score is less than 6, we will need to first ripen your cervix. In other words, we try to soften and prepare your cervix for dilation.
In other words, we try to soften and prepare your cervix for dilation.
Let’s talk about how we do that.
Prostaglandin Medications
Prostaglandins are the most commonly used medications for ripening or preparing your cervix for labor induction.
There are two types of prostaglandin medications:
- Misoprostol, also known as Cytotec, and
- Dinoprostone, also known as Cervidil
Cytotec is a prostaglandin E1 analogue that helps to soften the cervix and it often causes uterine contractions.
This medication comes in pill form and could be placed in the vagina or under the tongue.
It could be given every 3-4 hours for a maximum of 6 doses.
I do want to say, this medication is contraindicated if you are attempting a trial of labor after cesarean (TOLAC).
CervidilCervidil is a prostaglandin E2 analogue that is meant to soften the cervix. It may cause dilation and contractions as well.
This medication looks like a small skinny tampon with a long string, and it is placed deep into the vagina to start the ripening process.
The cervidil will be removed:
- if you begin dilating,
- if you begin contracting excessively,
- or if 12 hours have passed (whichever comes first).
Aside from medications, we also have another way to dilate or ripen the cervix.
Mechanical Dilation
Mechanical dilation uses pressure to dilate your cervix, rather than medications.
This can be done using a:
- Cook balloon, or
- Foley catheter balloon
One of these balloons will be inserted into your cervix and the balloon will be filled with sterile water.
You may feel a lot of pressure as the balloon is filling. So if you eventually want an epidural, feel free to get one prior to balloon placement.
The balloon will stay inserted in the cervix until your cervix is about 4 centimeters dilated or after 12 hours (whichever comes first).
A mechanical dilation is a great option for:
- women who are about 0.5-1 centimeter dilated, and/or
- for women who cannot receive additional prostaglandin medication.
It is also a great option if you are considering a trial of labor after cesarean (TOLAC).
Okay, so that’s how to ripen the cervix and get a couple of centimeters of dilation.
Now let’s get to the full-blown induction.
Uterotonic Medications
The most commonly used uterotonic mediation is oxytocin also known as Pitocin.
Oxytocin is a hormone that is normally released by the posterior pituitary gland when the onset of labor occurs and also during breastfeeding.
We give it through the IV to either initiate uterine contractions or augment your labor.
Pitocin mostly works at the uterine receptors to increase the frequency, duration, and amplitude of your contractions.
Once you are on oxytocin, most hospitals will not allow you to eat in case of an emergency (i. e needing an urgent cesarean section).
e needing an urgent cesarean section).
And last but not least we have another intervention up our sleeve…
Amniotomy
Amniotomy is a process in which we “break your water.” This is known as AROM, or artificial rupture of membranes.
This is a bedside procedure that occurs using a small hook to pierce the amniotic sac which causes the amniotic fluid to leak out.
Don’t worry this will not hurt!
After an amniotomy, you will continue to leak- this is completely normal.
Sometimes, an amniotomy alone can get your contractions going. But we often use this in conjunction with pitocin to achieve a regular contraction pattern.
So those are all the ways in which we can induce your labor starting from a closed cervix.
Now let’s talk about timing.
How Long Does An Induction Take (Step By Step)
As I mentioned before, an induction of labor can take upwards of 48 hours in first-time moms and up to 24 hours in women who have given birth before.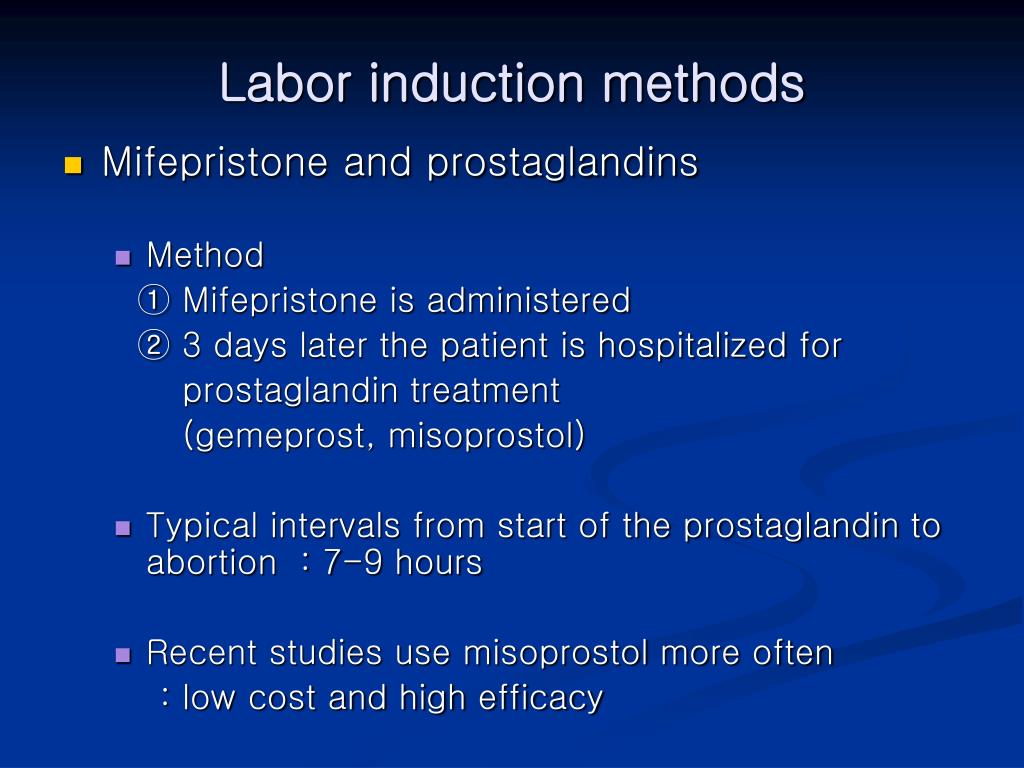
Let’s discuss the three stages of labor and how long each one takes.
Inducing The First Stage of Labor
The first stage of labor corresponds to when you are 0 cm dilated, to 10 cm dilated.
It is broken up into 2 parts, the Latent Phase & The Active Phase
The Latent Phase
The latent phase is the time it takes to get from 0 – 6 centimeters.
- This can take up to 20 hours in primiparous women aka, first-time moms and
- Up to 14 hours in multiparous women aka women who have had a prior delivery.
Yes, I know what you are thinking, it is a long time.
But you have to understand that your cervix and body weren’t yet ready for labor.
You really must be patient during this stage of labor and stay positive.
The Active Phase
Active labor occurs from the time you reach 6 centimeters to the time you are fully dilated or 10 centimeters.
- This stage can last anywhere from 0 – 6 hours on average depending on your parity.
For multiparous women, this stage can be very short!
There have been so many instances where I have seen women go from 6 centimeters to fully dilated in less than an hour.
Studies have shown that after 6 centimeters dilation, labor accelerated faster in multiparous women compared to nulliparous women.
On the other hand, nulliparous women with and without epidural had an active phase of approximately 3.6 and 2.8 hours, respectively.
The Second Stage of Labor
The second stage of labor occurs from full dilatation to delivery of the fetus.
This stage could last anywhere from 1- 4 hours depending on if you are nulliparous or multiparous, the type of pelvis you have, the position of the baby, and whether or not you have an epidural.
Some providers will have you start pushing as soon as you reach full dilatation whereas others will allow you to “labor down.”
Laboring down is a process in which you allow the fetal head to descend further down into the pelvis before you start pushing.
The thought process is that laboring down will help prevent you from pushing for hours, which can tire you out.
Believe it or not, the average time it takes to push a baby out is 90 minutes! It’s not instantaneous like you see in the movies.
To learn more about pushing, how to push effectively, and exercises you could do to prepare you for labor, click here.
The Third Stage of Labor
The third stage of labor occurs from delivery of the fetus to delivery of the placenta.
This should take no longer than 30 minutes.
If after 30 minutes the placenta does not deliver the placenta has to be removed manually.
Your provider will either manually deliver the placenta at the bedside, or take you to the operating room to surgically remove the placenta to reduce your risk of postpartum hemorrhage and infection.
Here is a table of how long a normal induction of labor can take.
| Stage of Labor | Nulliparous Woman | Multiparous Woman |
|---|---|---|
| Cervical Ripening | Up to 12 hours | Usually not needed |
| Latent Phase of Labor (0-5 cm dilated) | Up to 20 hours | Up to 14 hours |
| Active Phase of Labor (6-10 cm dilated) | ~ 6 hours | 0-6 hours |
| The Second Stage (Delivery of the baby) | 1-4 hours | 0-3 hours |
| The Third Stage (Delivery of placenta) | Up to 30 min | Up to 30 min |
The Immediate Postpartum
The fourth stage of labor has been described by some to be the immediate postpartum period.
During this time your provider will:
- assess the tone of your uterus to ensure it has started to contract down.
- assess and repair any lacerations.
- assess your vital signs including blood pressure and heart rate.
- assess the amount of uterine/vaginal bleeding you are experiencing.
This is one of the most important phases of labor as hemorrhage is one of the leading causes of maternal morbidity and mortality in developed and developing nations.
Is induced Labor more painful Than Natural Labor?
Induced labor can be more painful than natural labor.
Pitocin often causes stronger, longer, and more frequent uterine contractions than natural contractions.
Oftentimes, women will get an epidural due to the intensity of the pain.
With that said, I have seen plenty of women get induced without pain medication.
It is possible!
However, I always tell my patients, if you are in pain and you cannot tolerate the pain it is OKAY to have pain relief.
YOU DON’T HAVE TO BE A HERO OR PROVE ANYTHING TO ANYONE.
Getting a break from the pain of the contractions could help you relax and get some rest before needing to push.
Can I Get An Epidural Before The Induction?
You can get an epidural at any point in your induction!
There is no minimum number of centimeters dilated you need to be.
I do want to say however, you must be able to sit still for epidural placement.
So please don’t wait until the pain is so severe that you are unable to sit still.
Also, once you get the epidural, you will be confined to the bed. So no more walking around.
Is being induced harmful to the baby?
The actual induction of labor is not harmful to the baby, however, your baby may not tolerate the frequent contractions.
This is why you will be connected to an electronic fetal heart rate monitor when we start your induction.
The baby communicates with us through its heart rate.
If the baby is in distress, we will know.
Unfortunately, all medications used for induction of labor have side effects and because of that, we need to keep a close eye on your baby’s heart rate tracing.
Do you stay in the hospital after being induced?
Yes, you will be admitted to the hospital for an induction of labor and will stay in the hospital for at least 1-2 days postpartum or 2-4 days post-c-section.
We must monitor you in the early postpartum period to check your bleeding, your blood pressure, and incision if you had a cesarean delivery.
Other Related Questions
Is induction easier if you are already dilated?
Yes, an induction of labor is easier if you are already dilated. The more dilated you are, the more favorable your Bishop Score will be.
If your Bishop Score is 6 or greater, your induction is more likely to be successful than if you have a closed cervix giving you a bishop score of less than 6.
When you are dilated, we do not need to spend time ripening and preparing the cervix for labor as it is already dilated.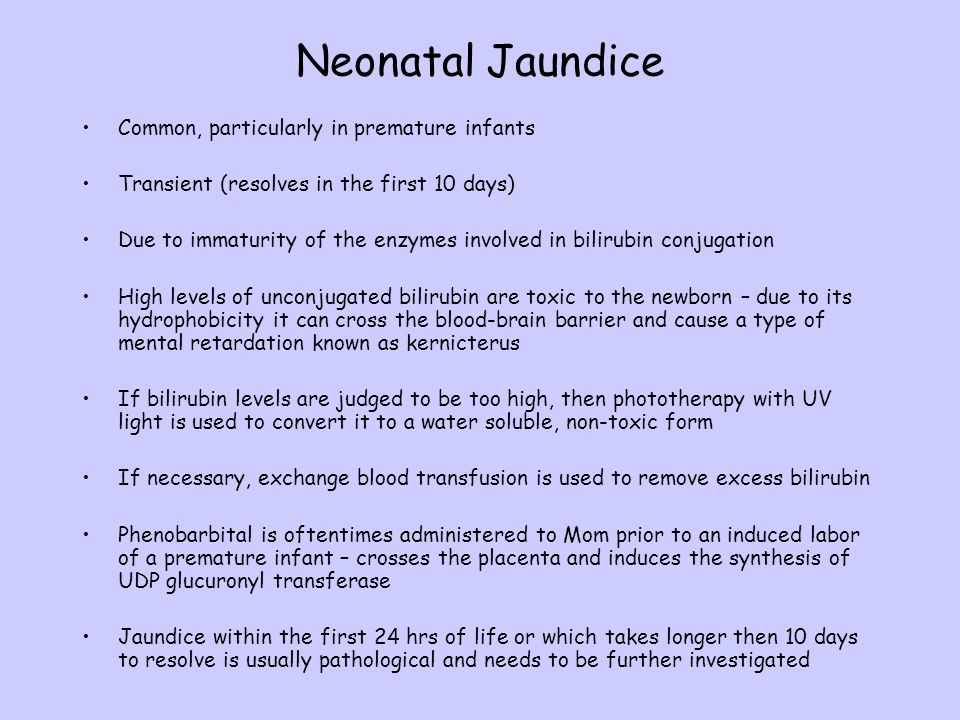
In this case, we can jump straight to the induction agents.
**Also if you have had a vaginal delivery in the past, your induction is more likely to be easier and faster.**
How long does induction take for the second baby?
An induction of labor is usually much quicker for a second baby compared to the first. On average, it can take up to 12-24 hours for second-time moms to give birth after induction.
Why do doctors push inductions?
The most common reason why doctors push inductions is for a medical indication.
Our goal is “healthy mom & healthy baby.”
Inductions are recommended when we determine that it is no longer beneficial for you or your baby to remain inside the uterus.
We want to do everything in our power to ensure the health and wellbeing of both you and your baby.
Are there natural ways to induce labor?
The most effective, natural way to induce your labor is known as membrane sweeping.
Membrane sweeping can be done during a vaginal exam if your cervix is at least 1 cm dilated.
It refers to physically separating the amniotic sac / membrane from the cervix with a finger sweep.
This should only be performed by a doctor or a midwife, and ONLY after you reached full term (39 weeks). That’s because a membrane sweep can lead to uterine contractions and possible rupture of the amniotic membranes.
Aside from membrane sweeping, some providers will encourage women to walk to help induce labor.
Although there haven’t been many scientific studies to prove this, walking is a great way to exercise during the third trimester. I talk about this more in walking to induce labor.
Is inducing labor at 39 weeks safe?
39 weeks is considered full-term. Induction of labor is very safe for you and your baby at this time.
37 – 38 weeks gestation is considered early term and thus we do not electively induce labor at this time.
In fact, there was a famous study done in 2018 called the ARRIVE Trial which compared outcomes in low-risk women at 39 weeks to an elective induction of labor or allowing them to go into spontaneous labor.
This trial showed a decreased rate of cesarean delivery in those women who were electively induced at 39 weeks compared to the women who were expectantly managed.
Is it safe at 38 weeks or less?
The only reason we would induce you prior to 39 weeks is if you have a pregnancy or fetal condition that can have negative consequences by prolonging your pregnancy.
Common examples include:
- Gestational Diabetes
- Gestational Hypertension
- Premature Rupture of Membranes
- Preeclampsia
- Chronic Hypertension
- Cholestasis of Pregnancy
- Growth Restricted Baby
- Twins
- Low Fluid
Do’s and Dont’s Before Being Induced
I do want to mention there are many things that people will tell you to do to induce your labor but have not been proven to be effective.
The following is a list of methods that are not proven or recommended:
- Nipple stimulation
- Castor oil
- Primrose oil
- Spicy food
- Massage
- Acupuncture
Now let’s talk about what you should do.
What Should I Do The Day Before Labor Induction?
The day before your induction of labor should be spent doing something for yourself.
Especially if this is your first baby!
Go out to eat with your partner as you may not be able to eat in labor, take a nice stroll as you may be stuck in bed for hours on end, or watch a movie.
Just do something that is relaxing and not stressful.
You should also make sure your baby bag is packed and you have everything you need for the hospital.
Don’t forget to pack a comfortable pair of slippers, possibly your favorite pillow and/or blanket, and chapstick as your lips get extremely chapped when pushing!
What Are The Disadvantages and Risks of Induced Labor?
I do want to mention that inductions of labor can be associated with some risks and disadvantages.
Those risks include:
- Infection
- Tachysystole (Frequent contractions)
- Failed induction
When you are admitted to the labor floor, typically you will have a cervical exam every 4-6 hours depending on the institution, to assess for change.
If you are being induced for 24-48 hours that can be a lot of examinations!
Although we are using sterile gloves, the vagina has A LOT of bacteria including group b streptococcus (GBS) that is present in some women. Thus, each time we examine you there is a risk of introducing bacteria into the uterus.
The risk of infection is further increased if your amniotic membranes have been ruptured for several hours.
To decrease the risk of infection, most physicians will limit the number of examinations you receive while in labor and/or give you antibiotics if you are found to be GBS positive.
2. TachysystoleTachysystole is defined as having too many uterine contractions, too close together.
The actual definition is the presence of more than 5 uterine contractions in a ten-minute period averaged over 30 minutes.
Tachysystole is considered a risk of induction because it can cause your baby to become distressed.
Think about it- as the uterus contracts the baby, placenta, and umbilical cord are getting squeezed.
During tachysystole, the baby only has about one minute of relaxation to “catch its breath.”
Some babies do fine and can tolerate it, whereas other babies cannot.
If your baby is in distress, we can give medication to relax the uterus to allow your baby more time to recover.
3. Possible need for cesarean sectionOnce we start an induction – the clock has started.
Depending on how many centimeters dilated you are, you have to show signs of progress. If you are not, you will need a c-section.
With that said, the need for a cesarean section can occur even if you don’t have an induction.
Studies show that there is no increased risk of cesarean section during an induction of labor.
Final Words on Labor Induction
So there you have everything you need to know about labor induction.
Do you feel ready?
Now I want to hear from you.
Did you have your labor induced, or are you scheduled for an induction?
What was your experience like or what are you most worried about?
Comment below and let me know!
Related Posts on Pregnancy
- 10 Unique Exercises to Prepare You For Labor
- Does Walking Help to Induce Labor
- What Muscles Are Cut During C Section
References:
- Zhang J, Landy HJ, Ware Branch D, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281-1287. doi:10.1097/AOG.0b013e3181fdef6e
- Finucane EM, Murphy DJ, Biesty LM, et al. Membrane sweeping for induction of labour. Cochrane Database Syst Rev.
 2020;2(2):CD000451. Published 2020 Feb 27. doi:10.1002/14651858.CD000451.pub3
2020;2(2):CD000451. Published 2020 Feb 27. doi:10.1002/14651858.CD000451.pub3 - Grobman WA, Rice MM, Reddy UM, et al. Labor Induction versus Expectant Management in Low-Risk Nulliparous Women. N Engl J Med. 2018;379(6):513-523. doi:10.1056/NEJMoa1800566
- Wood S, Cooper S, Ross S. Does induction of labour increase the risk of caesarean section? A systematic review and meta-analysis of trials in women with intact membranes. BJOG. 2014;121(6):674-685. doi:10.1111/1471-0528.12328
Get Four Free Workouts To Help Strengthen Your Pelvic Floor & Heal Your Mommy Tummy!
YES- I WANT THE PDF!
Brittany N Robles, MD, MPH, CPT
Brittany Robles is a full-time OBGYN, a NASM certified personal trainer, and health & fitness, expert. She holds a Masters of Public Health degree in maternal health with a special interest in exercise and nutrition. She is also the co-author of The White Coat Trainer.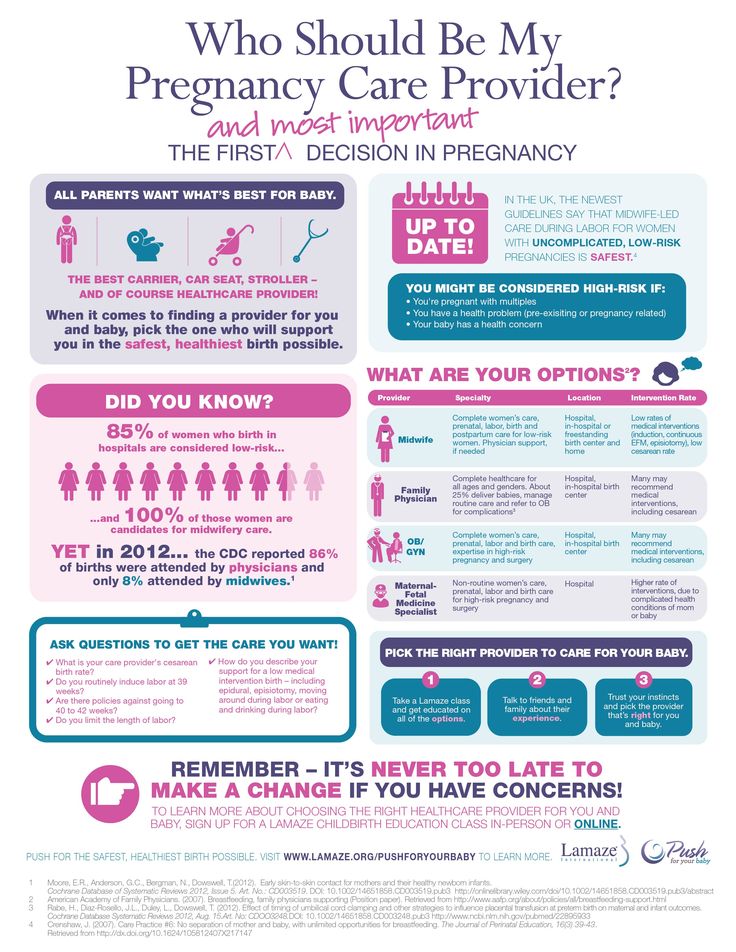 Learn more about her here.
Learn more about her here.
Sharing is Caring – Send This To A Mom In Need!
Induction of labor in women with normal pregnancies of 37 weeks or more
Does a policy of inducing labor at 37 weeks or more of gestation reduce the risks for infants and their mothers compared with a policy of waiting until a later gestational age or until Will there be indications for labor induction?
This review was originally published in 2006 and subsequently updated in 2012 and 2018.
What is the problem?
The average pregnancy lasts 40 weeks from the start of a woman's last menstrual period. Pregnancies lasting more than 42 weeks are described as "post-term" and therefore the woman and her doctor may decide to give birth by induction. Factors associated with postnatal pregnancy and delayed delivery include obesity, first birth, and maternal age over 30 years.
Why is this important?
Protracted (term) pregnancy may increase risks for infants, including greater risk of death (before or shortly after birth). However, induction (stimulation or induction) of labor can also pose risks to mothers and their babies, especially if the woman's cervix is not ready for delivery. Current diagnostic methods cannot predict risks to babies or their mothers per se, and many hospitals have specific policies regarding how long a pregnancy can last.
However, induction (stimulation or induction) of labor can also pose risks to mothers and their babies, especially if the woman's cervix is not ready for delivery. Current diagnostic methods cannot predict risks to babies or their mothers per se, and many hospitals have specific policies regarding how long a pregnancy can last.
What evidence did we find?
We searched for evidence (July 17, 2019) and identified 34 randomized controlled trials in 16 different countries involving more than 21,500 women (mostly at low risk of complications). The trials compared a policy of induction of labor after 41 completed weeks of gestation (>287 days) with a policy of waiting (expectant management).
Labor induction policies were associated with fewer perinatal deaths (22 trials, 18 795 babies). Four perinatal deaths occurred in the induction policy group compared with 25 perinatal deaths in the expectant management group. Fewer stillbirths occurred in the induction group (22 trials, 18,795 infants): two in the induction group and 16 in the expectant management group.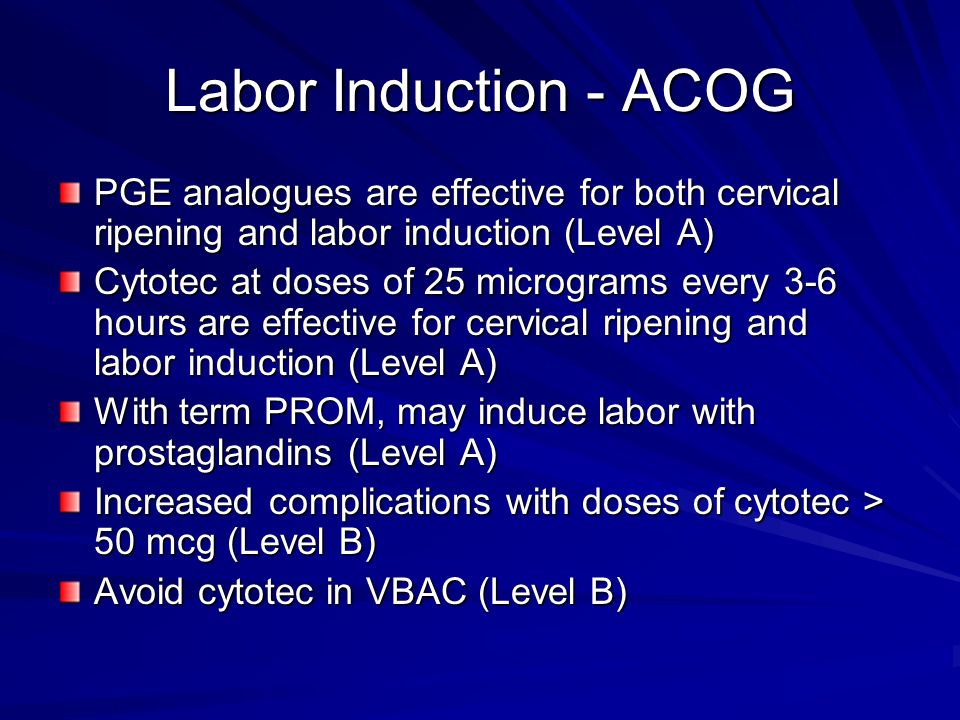
Women in the induction of labor groups in the included studies were probably less likely to deliver by caesarean section than in the expectant management groups (31 studies, 21,030 women), and there was probably little or no difference when compared with assisted vaginal delivery (22 studies, 18,584 women).
Fewer infants were admitted to the neonatal intensive care unit (NICU) in the induction policy group (17 trials, 17,826 infants; high-certainty evidence). A simple test of the baby's health status (Apgar score) at five minutes after birth was likely to be more favorable in the induction groups than expectant management (20 trials, 18,345 infants).
An induction policy may make little or no difference for women who have had a perineal injury, and likely has little or no effect on the number of women with postpartum hemorrhage or breastfeeding at hospital discharge. We are uncertain about the effect of induction or expectant management on length of stay in the maternity hospital due to the very low certainty of the evidence.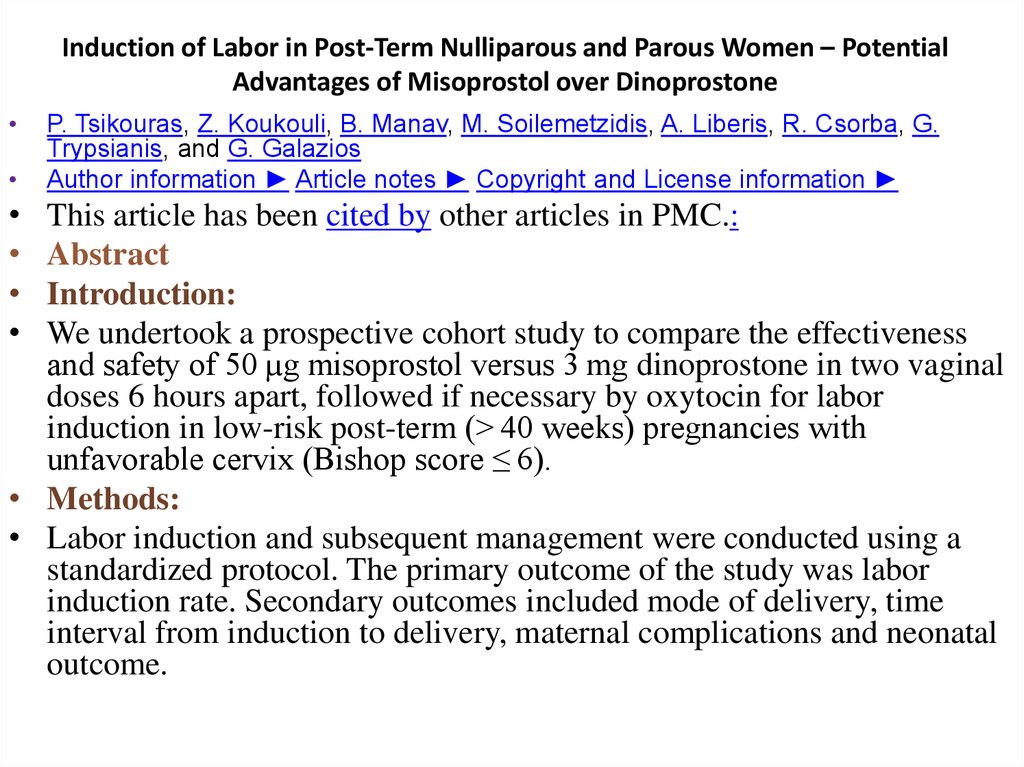
Among newborns, the number of children with trauma or encephalopathy was similar in both groups (moderate and low-certainty evidence, respectively). None of the studies reported the development of neurodevelopmental problems during follow-up of children and postpartum depression in women. Only three trials reported some measure of maternal satisfaction.
What does this mean?
An induction policy compared to expectant management is associated with fewer infant deaths and probably fewer caesarean sections; and probably has little or no effect on assisted vaginal delivery. Determining the best time to offer induction of labor to women at 37 weeks' gestation or more requires further study, as well as further study of women's risk profiles and their values and preferences. Discussing the risks of induction of labor, including benefits and harms, can help women make an informed choice between induction of labor, especially if the pregnancy lasts more than 41 weeks, or expectant management—waiting and/or waiting until labor is induced.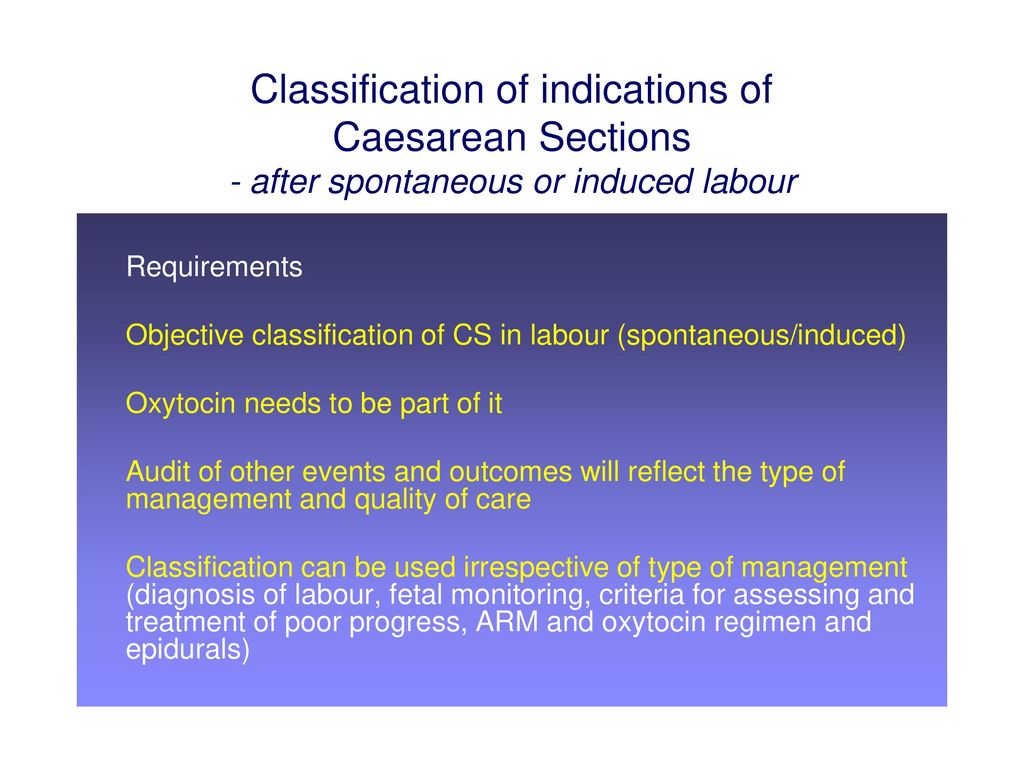 Women's understanding of induction, procedures, their risks and benefits is important to influence their choice and satisfaction.
Women's understanding of induction, procedures, their risks and benefits is important to influence their choice and satisfaction.
Translation notes:
Translation: Alekseeva Lada Igorevna. Editing: Prosyukova Ksenia Olegovna and Ziganshina Lilia Evgenievna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic. For questions related to this translation, please contact us at: [email protected]
Induction of labor or induction of labor
The purpose of this informational material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix in the patient, which is assessed according to the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, position of the presenting part of the fetus in the area pelvis). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body.
 It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
It prepares the body for childbirth, under its action the cervix becomes softer and begins to open. - Balloon Catheter – A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already sufficiently dilated, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions).
 The dose of the drug can be increased as needed to achieve regular uterine contractions.
The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal-related problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.

- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.