How long do afterbirth pains last
Relief of pain caused by uterine cramping or involution after giving birth
In this update, we include 28 studies (involving 2749 women). The evidence identified in this review comes from middle- to high-income countries. Generally the trials were at low risk of selection bias, performance bias and attrition bias, but some trials were at high risk of bias due to selective reporting and lack of blinding. Our GRADE certainty of evidence assessments ranged from moderate to very low certainty, with downgrading decisions based on study limitations, imprecision, and (for one comparison) indirectness.
Most studies reported our primary outcome of adequate pain relief as reported by the women. No studies reported data relating to neonatal adverse events, duration of hospital stay, or breastfeeding rates. Almost half of the included studies (11/28) excluded breastfeeding women from participating, making the evidence less generalisable to a broader group of women.
Non-steroidal anti-inflammatory drugs (NSAIDs) compared to placebo
NSAIDs are probably better than placebo for adequate pain relief as reported by the women (risk ratio (RR) 1. 66, 95% confidence interval (CI) 1.45 to 1.91; 11 studies, 946 women; moderate-certainty evidence). NSAIDs may reduce the need for additional pain relief compared to placebo (RR 0.15, 95% CI 0.07 to 0.33; 4 studies, 375 women; low-certainty evidence). There may be a similar risk of maternal adverse events (RR 1.05, 95% CI 0.78 to 1.41; 9 studies, 598 women; low-certainty evidence).
NSAIDs compared to opioids
NSAIDs are probably better than opioids for adequate pain relief as reported by the women (RR 1.33, 95% CI 1.13 to 1.57; 5 studies, 560 women; moderate-certainty evidence) and may reduce the risk of maternal adverse events (RR 0.62, 95% CI 0.43 to 0.89; 3 studies, 255 women; low-certainty evidence). NSAIDs may be better than opioids for the need for additional pain relief, but the wide CIs include the possibility that the two classes of drugs are similarly effective or that opioids are better (RR 0.37, 95% CI 0.12 to 1.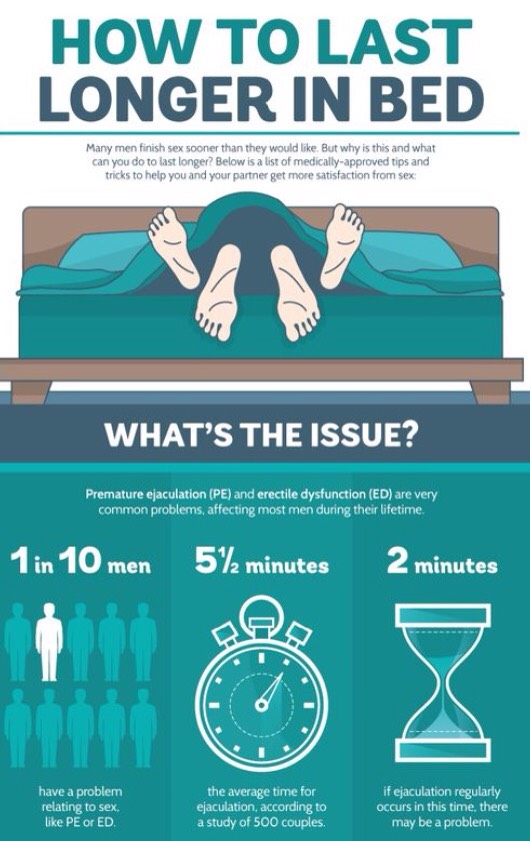 12; 2 studies, 232 women; low-certainty evidence).
12; 2 studies, 232 women; low-certainty evidence).
Opioids compared to placebo
Opioids may be better than placebo for adequate pain relief as reported by the women (RR 1.26, 95% CI 0.99 to 1.61; 5 studies, 299 women; low-certainty evidence). Opioids may reduce the need for additional pain relief compared to placebo (RR 0.48, 95% CI 0.28 to 0.82; 3 studies, 273 women; low-certainty evidence). Opioids may increase the risk of maternal adverse events compared with placebo, although the certainty of evidence is low (RR 1.59, 95% CI 0.99 to 2.55; 3 studies, 188 women; low-certainty evidence).
Paracetamol compared to placebo
Very low-certainty evidence means we are uncertain if paracetamol is better than placebo for adequate pain relief as reported by the women, the need for additional pain relief, or risk of maternal adverse events (2 studies, 123 women).
Paracetamol compared to NSAIDs
Very low-certainty evidence means we are uncertain if there are any differences between paracetamol and NSAIDs for adequate pain relief as reported by the women, or the risk of maternal adverse events. No data were reported about the need for additional pain relief comparing paracetamol and NSAIDs (2 studies, 112 women).
No data were reported about the need for additional pain relief comparing paracetamol and NSAIDs (2 studies, 112 women).
NSAIDs compared to herbal analgesia
We are uncertain if there are any differences between NSAIDs and herbal analgesia for adequate pain relief as reported by the women, the need for additional pain relief, or risk of maternal adverse events, because the certainty of evidence is very low (4 studies, 394 women).
Transcutaneous nerve stimulation (TENS) compared to no TENS
Very low-certainty evidence means we are uncertain if TENS is better than no TENS for adequate pain relief as reported by the women. No other data were reported comparing TENS with no TENS (1 study, 32 women).
Postpartum cramping: Why cramping after birth happens
Postpartum cramping happens as your uterus returns to its pre-pregnancy size after you deliver. The cramps are usually most intense on days two and three after delivery, but they should disappear within a week or two. You will find your cramps more intense while breastfeeding, as nursing can often stimulate uterine contractions. Over-the-counter pain relievers, along with gentle massage and deep breathing exercises can help ease the discomfort. If you have severe pain and symptoms like fever or smelly discharge, you'll want to call your doctor.
You will find your cramps more intense while breastfeeding, as nursing can often stimulate uterine contractions. Over-the-counter pain relievers, along with gentle massage and deep breathing exercises can help ease the discomfort. If you have severe pain and symptoms like fever or smelly discharge, you'll want to call your doctor.
What is postpartum cramping?
Postpartum cramping is pain in your lower belly as it returns to its pre-pregnancy size after your baby’s birth. Another name for these cramps is afterbirth pains.
Some cramping after birth is normal and it's usually mild for first-time moms (if you feel them at all). But the cramps often get worse with each future delivery, and may be most uncomfortable after the second and third babies.
Why do I have postpartum cramping?
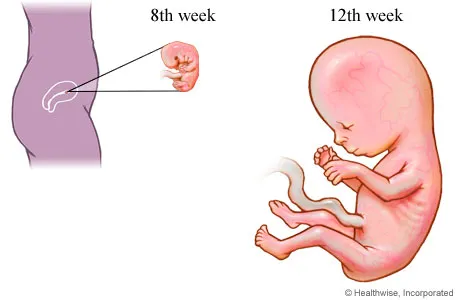
Postpartum cramping happens as your uterus contracts to return to its pre-pregnancy size and shape. (This process is called "involution.") Right after you deliver, your uterus weighs about 2 ½ pounds. By one week postpartum, it's already half that size. And by about six weeks post-birth, it should be down to 2 ounces.
By one week postpartum, it's already half that size. And by about six weeks post-birth, it should be down to 2 ounces.
Cramping after birth serves another important purpose. It narrows blood vessels in your uterus to prevent you from losing too much blood after delivery.
Expect the cramping to be most intense for the first day or two after you give birth. It should taper off by around the third day, though it can take several weeks for your uterus to return to its pre-pregnancy size.
Breastfeeding can bring on postpartum cramping or make it more intense. That's because your baby's sucking triggers the release of the hormone oxytocin. This is the maternal hormone which causes contractions, and it has the same affects it did during delivery, postpartum. This is actually a good thing: The cramps help your uterus shrink back to normal size more quickly, reducing your risk of postpartum anemia from blood loss.
Doctors and midwives routinely give new moms oxytocin immediately after delivery to reduce postpartum bleeding, and this may also intensify cramping.
When should I be concerned about postpartum cramping?
Some cramping after birth is normal and manageable at home, but more severe pain and other symptoms are worth calling your doctor about.
Intense pain in your lower belly could be a uterine infection called endometritis. Pain that extends to your lower back or side might be a urinary tract infection. It's also not normal to have persistent pain or redness around your c-section incision or vaginal laceration.
Advertisement | page continues below
Call your doctor if the cramping hasn't started to ease up after a few days, or if the pain becomes unbearable. These could be signs of an infection or other problem that requires medical attention.
Also report symptoms like these:
- Fever
- Pain or burning when you pee
- Foul-smelling discharge
Is there anything I can do to relieve postpartum cramping?
Cramping is normal, but it's not something you have to tolerate. Because postpartum pain can distract you from the more important tasks of caring for and bonding with your baby, it's worth addressing.
Because postpartum pain can distract you from the more important tasks of caring for and bonding with your baby, it's worth addressing.
An over-the-counter pain reliever like ibuprofen (Advil, Motrin) can help with the pain. Let your doctor know if it doesn't give you relief – they may recommend another medication.
Here are a few other tips you can try to minimize your discomfort:
- Practice deep breathing or other relaxation techniques to distract you from the pain.
- Try to pee often, even if you don't feel the urge to go. A full bladder prevents the uterus from fully contracting and intensifies cramping. Immediately postpartum, your sensation of bladder fullness may be disrupted, so taking regular trips to the bathroom no matter what, will help ease cramping.
- Breastfeed every 2-3 hours during the day and every 3-4 hours at night. This will not only help your milk supply, but will also help minimize your blood loss by encouraging contractions and helping the uterus return to its pre-pregnancy size.
- Lie face down with a pillow or warm heating pad under your lower belly.
- Gently massage your lower belly.
Recovery after childbirth
In most cases, the recovery of normal health is not rapid. The first sensation of incredible relief has passed, and now you notice that the stomach is still large, and even a little sore. To take its former size, the uterus must still be contracted for a long time and diligently. Its weight decreases from 1 kg to 50 g within 6-8 weeks.
Since the contraction of the uterus occurs due to the work of the muscles, this is accompanied by pain sensations of varying intensity, reminiscent of light contractions. You may notice an increase in pain while breastfeeding your baby. The thing is that stimulation of the nipple causes an increase in the level of oxytocin in the blood, which contributes to uterine contractions.
For better uterine contraction, it is recommended to lie on your stomach after childbirth. If you feel good, try to move more and do gymnastics.
If you feel good, try to move more and do gymnastics.
Another disturbing circumstance is pain in the perineum, which appears even if there were no tears and the doctor did not make an incision. This is due to the fact that the tissues have undergone a strong stretch during childbirth. Usually the pain is not very intense and disappears in 2-3 days. But if there were tears or a perineal incision, then it can hurt longer - 7-10 days. You should carefully monitor the seams, carry out hygiene after each visit to the toilet. In addition, it is necessary to treat the sutures daily with antiseptic solutions, you can not sit for 2 weeks.
Haemorrhoids often appear after childbirth. Careful hygiene and daily evening showers help reduce pain. Do not forget about the diet, include in your diet foods rich in fiber and with a slight laxative effect: seaweed, beets, baked apples, cauliflower, germinated cereals. Medications are usually not used because the inflammation usually goes away with time. If everything does not go away by itself and the woman continues to suffer from hemorrhoids, you need to consult a doctor and apply the medicines prescribed by him or take a course of physiotherapy procedures.
If everything does not go away by itself and the woman continues to suffer from hemorrhoids, you need to consult a doctor and apply the medicines prescribed by him or take a course of physiotherapy procedures.
Constipation that occurred during pregnancy may also remind of itself in the postpartum period. They are, in particular, caused by the fear of damaging the seams in the perineum. However, such fear is unfounded. In addition, during a bowel movement, you can hold the area where the stitches are applied with a napkin, which will reduce the stretching of the tissues, and the bowel movement will be less painful. The chair usually does not happen immediately after childbirth, but after 2-3 days. To prevent constipation, eat prunes and dried apricots, drink mineral water. And only if there was no bowel movement on the 3rd day, you can use a laxative candle.
After childbirth, especially strong discharge from the uterus is observed on the first day, then it decreases. After 3 days, the discharge becomes muco-bloody. By the 5-6th week after birth, the discharge from the uterus stops altogether. During this period, hygiene must be carefully observed, because an infection that has entered the uterus can lead to endometritis (an inflammatory process of the uterine mucosa).
By the 5-6th week after birth, the discharge from the uterus stops altogether. During this period, hygiene must be carefully observed, because an infection that has entered the uterus can lead to endometritis (an inflammatory process of the uterine mucosa).
For 9 months, all the organs of the female body worked to ensure the child's proper development and good health. Now he was born and became quite "independent". However, the functions of a woman-mother did not end there. The main one - to provide the baby with food - is taken over by the mammary glands. In the body of a woman, hormonal changes continue, due to which significant changes occur in the mammary glands, and they begin to produce milk. In the first 2-3 days, colostrum is released, and already on the 3-4th day - transitional milk, which gradually turns into mature breast milk. Feeding your baby stimulates milk production. Therefore, in case of insufficient lactation, more frequent breastfeeding is recommended.
However, women often face the opposite problem - an excess amount of milk and difficulty in its outflow. This, in turn, leads to its stagnation and engorgement of the mammary glands - they harden, increase in volume, and painful sensations appear in the chest area. It may even increase body temperature. How to prevent such occurrences?
This, in turn, leads to its stagnation and engorgement of the mammary glands - they harden, increase in volume, and painful sensations appear in the chest area. It may even increase body temperature. How to prevent such occurrences?
First of all, try to breastfeed your baby regularly, and in the first 3-4 days after birth, limit fluid intake to 800 ml per day. Then the mammary glands will gradually become soft again. In addition, it is important to know that in the first days after childbirth, the skin of the nipples is very delicate and may crack. This makes them vulnerable to infection, the entry of which into the cracks is fraught with the development of mastopathy. Therefore, you need to take good care of the nipples and wear a comfortable bra, which will help the proper development of lactation.
To prevent cracks in the nipples, it is necessary to apply the baby to each breast in turn in the first 2-3 days after childbirth. First, give the baby one for 5-7 minutes, then another for 5-7 minutes. To prevent cracks, there is a special cream that needs to be used between feedings, and before them, carefully wash off its remnants.
To prevent cracks, there is a special cream that needs to be used between feedings, and before them, carefully wash off its remnants.
That's all the troubles that are easily forgotten and seem not so significant against the background of new worries. Now your attention will be constantly occupied by the baby. However, it is very important not to forget about yourself, maintain your health and restore your former beauty. Not everyone succeeds, which contributes to the development of postpartum depression.
Lochiometer
After childbirth, under the influence of cellular enzymes secreted by the granulation shaft, blood clots and fragments of the decidua remaining on the walls of the uterus are liquefied. In addition, leukocytes, erythrocytes, plasma and lymph penetrate into the uterine cavity through the wound surface. All these elements form lochia - a postpartum wound secret, which normally actively flows from the uterine cavity through the cervical canal into the vagina.
The first 2-3 days after birth, lochia have a bloody character, then, from the 4th-5th day, they acquire a dark red and brownish hue, and after a week they become yellowish-white due to the high content of leukocytes. From the 10th day, the discharge becomes light, watery, serous-mucous consistency. Gradually, the number of lochia decreases, and by the end of the 3rd week, the discharge practically stops and soon disappears completely.
With a delay in the outflow of postpartum secretions, they speak of a lochiometer - stagnation of lochia in the uterine cavity. The danger of developing lochiometers lies in the high probability of infection of the contents of the uterus, since lymph, serum, blood, and tissue remnants serve as the best nutrient medium for the reproduction of microbial flora. Most often, against the background of lochiometers, endometritis develops.
Causes of the development of lochiometers
The development of lochiometers is due to mechanical obstacles to the outflow of secretions in the cervical canal or insufficient uterine contractility.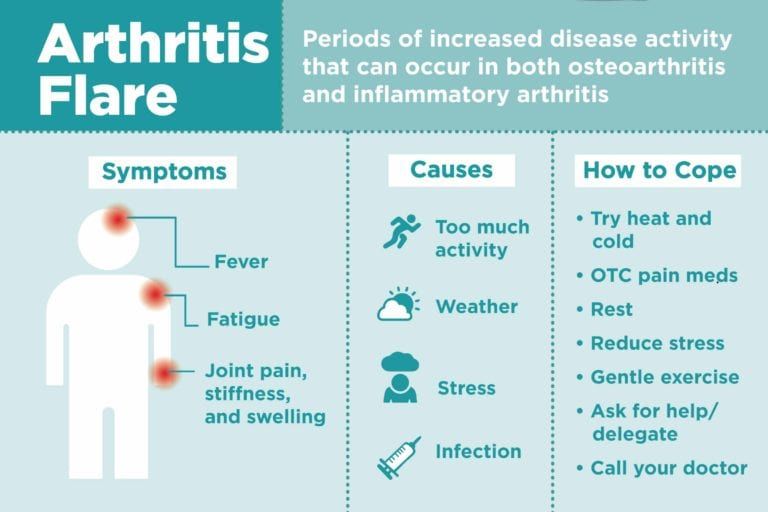
Mechanical obstruction may be due to kinking (hyperanteflexia) of the uterus or obstruction of the cervical canal by blood clots, remnants of the decidua, and flaking uterine tissue.
Insufficient contractile activity of the uterus in the postpartum period usually develops as a result of overstretching of the uterus (with a large fetus, polyhydramnios or multiple pregnancy), weak or discoordinated labor, spasm of the internal os, caesarean section.
The development of lochiometers is facilitated by prolonged bed rest and low activity after childbirth.
Symptoms of lochiometer
Lochiometer develops 5-7 days after birth, characterized by a marked decrease or cessation of postpartum discharge from the uterus. At the same time, there is an increase in the size of the uterus compared to the norm for the current postpartum day, its soreness on palpation. The general health and objective condition of a woman with a lochiometer does not suffer, body temperature is normal, tachycardia is absent.
When delaying timely therapeutic tactics in relation to lochiometers, fever appears (body temperature 38-40 ° C), chills, cramping pains, turbid discharge with an unpleasant odor, tachycardia. After 1-2 days, the temperature drops critically with the simultaneous appearance of liquid purulent lochial discharge.
Diagnosis lochiometers
Lochiometers are diagnosed by characteristic clinical signs. With the help of a gynecological examination, an unevenly enlarged and painful uterus is determined, which has a densely elastic consistency, often - the closure of the internal pharynx, the bend of the uterus.
Clarifying lochiometer diagnostics includes ultrasound. during which the expansion of the uterine cavity is revealed, the presence of hyperechoic blood clots and liquid blood in it.
Treatment of lochiometers
Treatment of lochiometers consists in ensuring the free outflow of lochia, taking into account the cause that caused this condition.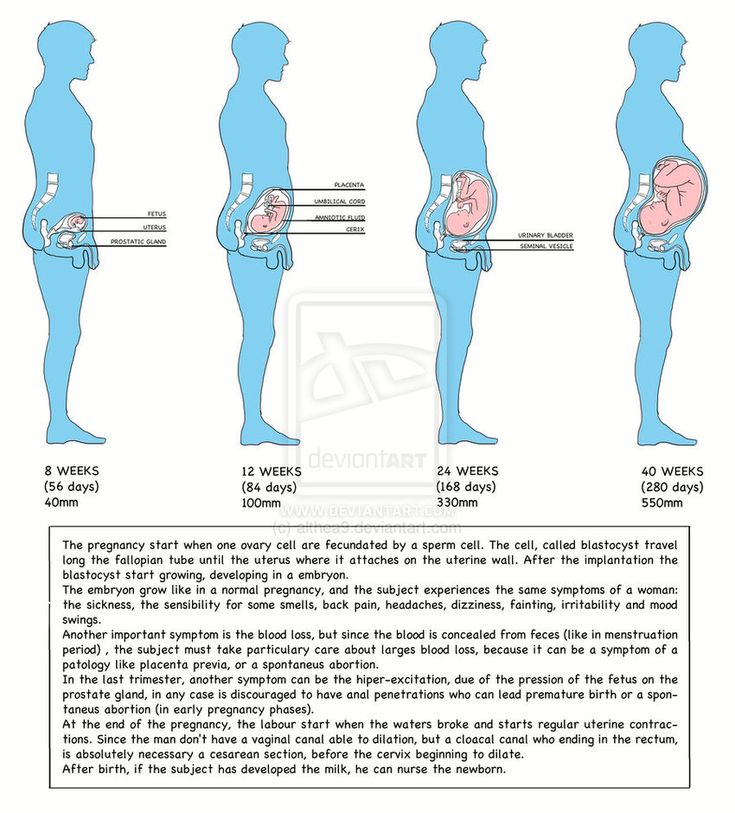
When lochiometers are detected, the gynecologist prescribes injections of antispasmodics (papaverine, no-shpy) to relieve spasm of the uterine os. In the treatment of lochiometers, uterotonic (contracting the uterus) agents are used - oxytocin, methylergometrine. For a free outflow of secretions, the puerperal is recommended to lie on her stomach 2-3 times a day for 1-2 hours.
In case of hyperanteflexion of the uterus, the bend is eliminated during the bimanual examination; exercise therapy is prescribed. In the case of a lochiometer due to blockage of the cervical canal by clots, when viewed on a chair, digital dilatation of the cervical canal and careful removal of clots are performed.
Situations when the lochiometer is not allowed within 2-3 days are considered by clinical gynecology as an indication for instrumental removal of the contents of the uterus with a curette or vacuum apparatus under hysteroscopy control. For the prevention and treatment of postpartum infections against the background of lochiometers, antibiotics are prescribed, taking into account the results of a bacteriological smear.
Complications of lochiometers
If, after the elimination of lochiometers, uterine tenderness, its poor contraction, hyperthermia persist, one should think about the development of postpartum metroendometritis.
If the infection progresses, the condition of the puerperal may worsen due to the development of purulent-resorptive fever, manifested by intoxication, abdominal pain, purulent discharge with a putrid odor. Against this background, the transition of lochiometers to pyometra is noted.
Prevention and prognosis with lochiometer
To prevent the development of lochiometers, competent management of pregnancy and preparation of the woman for childbirth are required, as well as careful monitoring of the puerperal during the postpartum period: regular monitoring of uterine contractions (daily palpation determination of its sensitivity, consistency, fundus height), volume and nature of discharge .
In the postpartum period, a woman needs to monitor the timeliness of emptying the bladder and intestines, breastfeed the newborn on demand, perform postpartum exercises, and lie on her stomach.
After discharge from the maternity hospital, a young mother should also monitor her well-being and discharge from the genital tract. In the event of an increase in temperature, a delay in lochia, a change in their nature or smell, an immediate appeal to a gynecologist is necessary.
The prognosis for timely detection and elimination of lochiometers is favorable.
Anti-inflammatory drugs to relieve pain in the perineum after childbirth
This translation is out of date. Please click here for the latest English version of this review.
What is the problem (question)?
After giving birth, many women experience pain in the perineum, the area between the anus and the vagina. This Cochrane review addresses the question of whether this pain can be relieved with a single dose of a non-steroidal anti-inflammatory drug (NSAID) such as aspirin or ibuprofen.
Why is this important?
Some women experience particularly severe pain in the perineum after childbirth if the perineum ruptures during childbirth or an incision is required (a procedure known as an episiotomy). Even women who give birth without a perineal tear or surgery often experience some discomfort in the perineal area, which can affect a woman's activity as well as her ability to care for a baby. This review is part of a series of reviews looking at the effectiveness of various pain relief medications for perineal pain immediately after childbirth. This review looked at NSAIDs such as aspirin and ibuprofen.
Even women who give birth without a perineal tear or surgery often experience some discomfort in the perineal area, which can affect a woman's activity as well as her ability to care for a baby. This review is part of a series of reviews looking at the effectiveness of various pain relief medications for perineal pain immediately after childbirth. This review looked at NSAIDs such as aspirin and ibuprofen.
What evidence did we find?
We found 28 studies involving 4181 women that studied 13 different NSAIDs (aspirin, ibuprofen, etc.). We included studies up to 31 March 2016. The studies we found only included women who had suffered perineal injuries and were not breastfeeding. Studies were conducted between 1967 and 2013 and were small and of low quality.
Studies have shown that a single dose of NSAIDs provides greater pain relief when assessed 4 hours (low-quality evidence) or 6 hours (very low-quality evidence) after administration, compared with placebo (a pill that mimics a drug) or no treatment in lactating women who have suffered trauma to the perineum during childbirth. Women who received single doses of NSAIDs also needed less additional pain relief 4 hours (low-quality evidence) or 6 hours (low-quality evidence) after their initial dose compared with women who took placebo or received no treatment. Not all studies assessed the adverse effects of the intervention, but some reported adverse effects in mothers such as drowsiness, headache, weakness, nausea, and stomach discomfort. However, there was no clear difference in the incidence of adverse effects 6 hours after drug administration between the groups (very low-quality evidence). One small study reported no adverse effects in mothers 4 hours after drug administration (low-quality evidence). None of the studies assessed possible adverse effects in children.
Women who received single doses of NSAIDs also needed less additional pain relief 4 hours (low-quality evidence) or 6 hours (low-quality evidence) after their initial dose compared with women who took placebo or received no treatment. Not all studies assessed the adverse effects of the intervention, but some reported adverse effects in mothers such as drowsiness, headache, weakness, nausea, and stomach discomfort. However, there was no clear difference in the incidence of adverse effects 6 hours after drug administration between the groups (very low-quality evidence). One small study reported no adverse effects in mothers 4 hours after drug administration (low-quality evidence). None of the studies assessed possible adverse effects in children.
NSAIDs also appeared to be better than paracetamol in relieving pain when assessed 4 hours (but not 6 hours) after drug administration, although such a comparison was made only in three small studies. Women who received a single dose of NSAIDs also needed less additional pain relief 6 hours (but not 4 hours) after taking the medication, compared with women who received paracetamol. There were no adverse effects in mothers 4 hours after taking the drug (according to one small study). Three small studies reported adverse effects in mothers assessed 6 hours after drug administration, but there were no clear differences between the groups. No adverse effects were reported in children in any of the included studies. Breastfeeding women were also excluded from all studies.
There were no adverse effects in mothers 4 hours after taking the drug (according to one small study). Three small studies reported adverse effects in mothers assessed 6 hours after drug administration, but there were no clear differences between the groups. No adverse effects were reported in children in any of the included studies. Breastfeeding women were also excluded from all studies.
Comparisons of different NSAIDs and different doses of the same NSAID did not show any clear difference in their efficacy for the main outcomes assessed in this review. However, there were few data available for some NSAIDs.
None of the included studies reported any of the secondary outcomes considered in this review, including: increased length of stay or readmissions for perineal pain; breastfeeding, perineal pain 6 weeks postpartum, women's opinion, postpartum depression, and disability due to perineal pain.
What does this mean?
In non-breastfeeding women, a single dose of NSAIDs may relieve perineal pain when assessed 4 and 6 hours after drug administration.