Baby sugar water constipation
Constipation – Baby Care Advice
Constipation is a common problem when babies are formula-fed and when they start eating solid food. Straining is typical newborn behavior that is often mistaken as a sign of constipation. Find out how to tell if your baby is constipated, why it might happen, and what you can do about it.
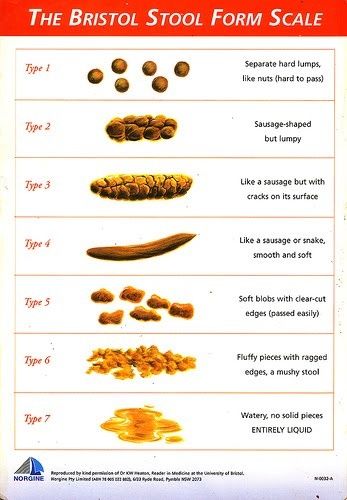
What normal infant stools look likeWhen your baby is breastfedCONSISTENCY: Soft or runny.
COLOR: Yellow, mustard to orange with little white flecks that look like seeds.
FREQUENCY: Can vary from every feed to once every week or so.
CONSISTENCY: Soft paste.
COLOR: Grayish green, yellow, tan or brown, depending on the type of formula.
FREQUENCY: Once (sometimes twice) every 1 or 2 days.
CONSISTENCY: Paste to formed stools. Often contains undigested food.
COLOR: Can very depending on what has been eaten.
FREQUENCY: Can be less frequent - particularly for a breastfed baby.
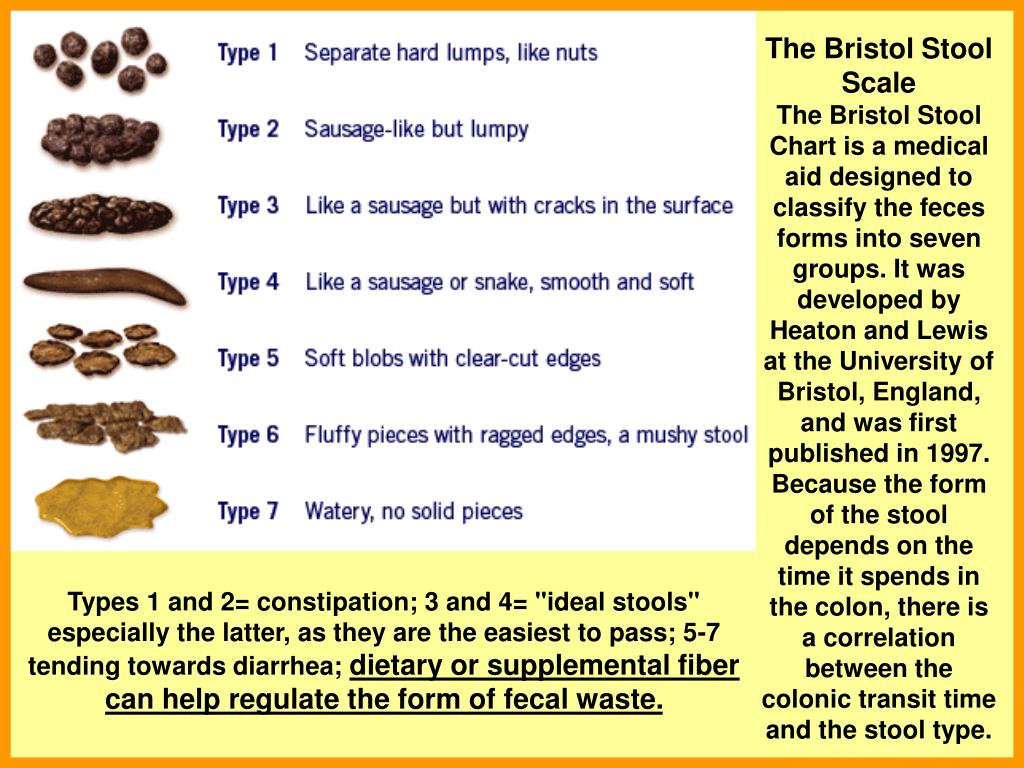
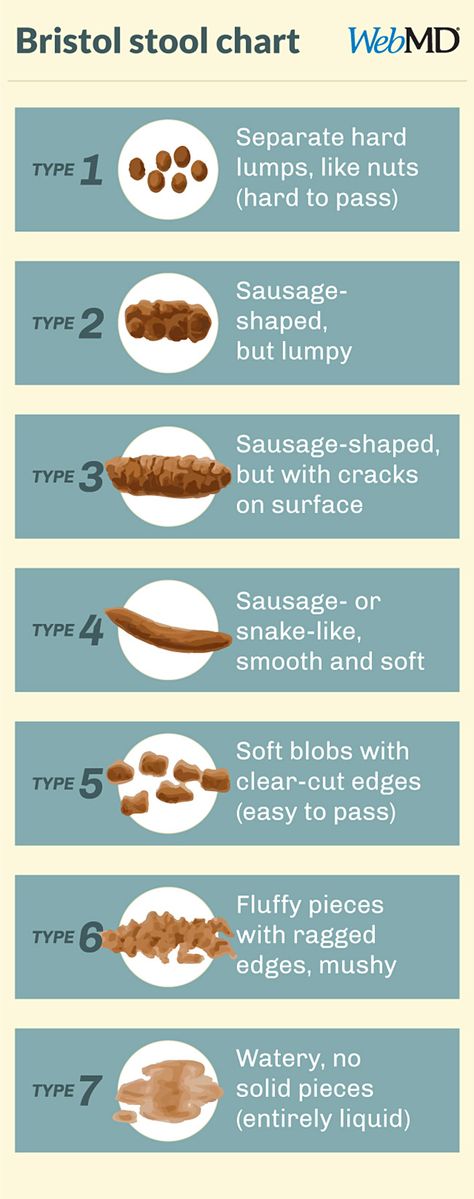
A baby is considered to be constipated if his poop is firm, dry and pebbly!
Crying while having a bowel motion, bleeding from the anus, abdominal pain and reduced appetite can also be signs a baby is constipated.
If your baby's poop is fluid, soft or paste consistency, then he's not constipated.
What causes infant constipation?- Insufficient fluid
- New foods
- Low fiber
- Different types of formula
- Medications
- Is your baby gaining enough weight for his age?
- Does he provide you with 6 or more wet diapers each day?
- Are you making his formula correctly?
- If he has started on solid foods, are you offering him additional water?
If the answer is 'no', he may not be getting enough fluid in the form of breast milk, formula or water and this can lead to constipation.
It is rare for a thriving, fully breastfed baby to become constipated. Your breastfed baby does no need to be offered water before he starts eating solid foods. Water or other fluids should not replace breast milk.
Depending on the climate, your formula fed baby may need extra fluids before he starts on solid foods. If you live in a warm climate, offering your baby water (in addition to formula) is often recommended at an earlier age.
Check how you prepare your baby's formula. Incorrect preparation of formula can result in an insufficient water ratio which can cause constipation. (See Preparing and warming formula for more information).
2. New foodsIt's common for a breastfed baby to experience constipation for the first time when solid foods are introduced into his diet or if he is switched from breast milk to infant formula. His little body is just not used to digesting anything other than breast milk. Introduce new foods slowly to allow time for him to adjust.
Some foods are more constipating than others for both breastfed and formula fed infants. These include cheese, ice-cream, yogurt, white bread, spaghetti, macaroni, white rice, banana, green apples, cooked carrots, corn, turnips and potatoes. Small amounts of these foods will generally not cause a problem, but larger amounts may result in constipation.
3. Low fiberFiber is only found in plant foods such as cereals, fruits and vegetables. Babies over 6 months with high intakes of formula or cow's milk (only recommended after 12 months) often experience constipation. It's not the milk itself that causes this, it's simply that the child fills up on milk which means he will have limited appetite for other foods that provide fiber.
4. Different types of formulaFormula fed babies are more at risk of becoming constipated than are breastfed babies.
Some types of infant formula can be more constipating than others. Casein dominant formula, lactose-free formula, AR (anti regurgitation) and thickened formulas can be more constipating for some babies. Variations can also occur between different brands of the same type of formula.
Variations can also occur between different brands of the same type of formula.
Switching formula (or switching to cow's milk) can lead to changes in stool consistency, resulting in either constipation or loose runny stools. Most often this change is only temporary, until your baby's little tummy gets used to the new formula. (We recommend you rule out other reasons for constipation before switching formula).
5. MedicationsCommon medications given to babies can sometimes cause constipation.
- Pain-killers containing paracetamol, acetaminophen and ibuprophen.
- Antibiotics.
- Antacids containing alumimum.
- Iron supplements
Most babies are not truly constipated unless they experience all of the following...
- Firm, dry pebbly stools.
- No bowel motions for 2-3 days for formula fed babies or 7-10 days for breastfed babies*; and
- Strains and cries while having a bowel motion.
Unless your little one has a problem with all three, he's probably not constipated and you needn't do anything. If your baby is constipated, treatment may be necessary. We suggest you start with 'natural remedies' first.
*It is rare for a fully breastfed baby to become constipated prior to starting solids. 7-10 days without a bowel movement can be very normal where a baby is only offered breast milk. Breast milk is the perfect food for babies and very little is left to waste. Breast milk also has a natural laxative effect that helps protect your baby against constipation.
Natural remedies- Water
- Sugar e.g. brown sugar
- Fruit juice
- Fruit
- Probiotics
Increasing the amount of water your offer your baby is often more effective than adding sugars to his diet. For babies less than 6 months old offer 1 oz of cooled boiled water, once or twice a day. For babies over 6 months offer 2 oz, once or twice a day.
For babies over 6 months offer 2 oz, once or twice a day.
A remedy for constipation that has been around for centuries and still recommended today, is to add some form of sugar to a baby's diet. The sugar works by drawing additional fluid into the baby's bowel to soften the stools. Sugar can come from fruit, in the form of fructose or sorbitol or sucrose from sugar cane.
It's frequently recommended to add some form of sugar (particularly brown sugar) to baby's formula. Rather than do this, we suggest you offer it in a small amount of cooled, boiled water for two reasons...
- The additional water is helpful; and
- Your baby may fuss with feeding once the sugar is stopped.
In the past honey was recommended as a treatment for constipation. However, it is no no longer recommended for children under the age of 12 months because of the associated risk of botulism (a gastro-intestinal illness).
Brown sugar
Add 1/2 teaspoon of brown sugar (the one used for cooking) to 1 oz of cooled boiled water. Offer this to your baby 3 times a day, directly before formula feeds, until his poop is soft and then stop.
Offer this to your baby 3 times a day, directly before formula feeds, until his poop is soft and then stop.
While brown sugar is recommended because it contains molasses, white sugar would do.
CAUTION: Only add sugar or corn syrup to your little one's diet, if you are treating constipation, not both.
3. Fruit JuiceApple, pear or prune or pear can be very effective at relieving constipation. To begin with dilute the juice to 1/4 strength by adding cooled, boiled water. Slowly increase the concentration to 1/2 strength if necessary.
If your baby is aged 3 - 6 months, offer 1 oz of diluted juice (2 oz if he's over 6 months). Offer this twice a day until his poop is soft. Give less rather than more to start with as too much juice can result in abdominal gas, bloating and diarrhea. (See Carbohydrate malabsorption for more information.)
CAUTION:
- Do not treat infant constipation with diluted juice and addition sugars (including Karo) at the same time.
 Choose only one treatment.
Choose only one treatment. - Diluted fruit juice as a treatment for constipation is not recommended for babies less than 3 months old.
- It is not recommended to offer fruit juice on a regular basis to babies less than 3 months.
If your baby has started eating solids, include more fruit and vegetables to his diet, as this may help to reduce the chance of constipation developing in the first place.
Bananas and apple sauce can result in firmer stools. Carrots and squash are constipating for some babies. Prunes, peaches, pears, plums, apricots and peas make stools softer. Colored vegetables tend to help, where as white vegetables can be constipating for some babies.
If your baby is under 9 months avoid citrus fruits such a orange, grapefruit and pineapple, as the acid content in these fruits can be harsh on little tummies, as well as the skin around his mouth and bottom (when it comes out).
5. Probiotics
ProbioticsIn recent decades, there has been much research into the benefits of maintaining a healthy intestinal microflora. Healthy intestinal flora include friendly microorganisms. The main source of friendly microorganisms in a baby's intestinal flora is bifidobacteria. Formula fed babies have only approx 25% of bifidobacteria in their intestines compared to 95% in the intestines of breastfed babies.
Probiotics involve providing live non-pathogenic microorganisms that improve the balance of intestinal microflora. Drinking infant formula with probiotics changes a formula fed baby's intestinal flora to be closer to that of a breastfed baby. Studies have shown probiotic infant formula may soften a baby's stools, decrease nappy rash and provide some protection against gastroenteritis.
Some countries produce infant formulas that include probiotics. (You will find the formula label is clearly marked if it contains probiotics). You can also purchase bifidobacteria from health food stores, which can be added to regular infant formula. Discuss this with your healthcare provider before starting your baby on probiotics.
Discuss this with your healthcare provider before starting your baby on probiotics.
Laxatives are only necessary if 'natural remedies' have failed or where constipation is severe. Although many different types of laxatives can be purchases over-the-counter, most laxatives are not suitable for babies and small children. If you feel your baby needs a laxative to relieve his constipation, we recommend you consult with your baby's doctor about a suitable treatment.
Different laxatives work in different ways;
- Some simply soften the stool.
- Others act as a peristaltic stimulant (in other words they stimulate the natural contractions of the bowel in order to push the stools out).
- Some offer a combination of softener with peristaltic stimulant
- Others offer additional fiber.
Laxative can be given to babies orally, in the form of drops or anally by a suppository or enema.
Parents often become concerned about infant constipation when they observe normal changes in their baby's bowel habits and behavior, which commonly occur around 2 - 6 weeks of age. It's around this age that the frequency of babies' bowel motions often decreases, (this being more obvious in breastfed babies). It is also around this age that many babies are first observed to strain when having a bowel motion or passing gas.
Unfortunately, these changes frequently occur at a time when many babies are becoming increasingly irritable and so parents naturally assume there is a connection. However, in most situations changes in bowel habits have nothing to do with an infant's irritable behavior.
It's not the frequency of bowel motions or straining that determines if your baby is constipated; it's the consistency of his stools.
Why the frequency of stools changeA decrease in the number of times your baby poops doesn't necessarily mean he is constipated.
A decrease in the frequency of bowel motions is often noticeable around 4 weeks of age, particularly when a baby is breastfed. As your baby's digestive system matures his body is better able to digest and absorb the many nutrients in milk (breast or formula) and as a result there in less waste (poop).
It is around this time that a mother's breast milk supply settles to meet her baby's needs, so this also results is less poop. (Nursing mother's often have an abundance of breast milk during the early weeks of breastfeeding.)
A reduction in the number of of bowel motions of a formula fed baby may also be seen around this age. However, it generally less obvious than changes seen in fully breastfed infants.
Other time where a change in the amount and how often a baby poops, may occur as a result of changes in diet. A sudden change in the frequency of bowel motions is commonly seen when...
- A baby is switched from breast milk to formula.
- The type of formula is changed.

- A baby first starts to eat solid foods.
- The amount of solid foods is increased.
- When a baby is first introduced to regular cow's milk.
Straining alone is not a sign of constipation!
Adults strain when they are constipated, so it's natural to assume your baby's straining is due to constipation. However, straining is normal behavior for infants, particularly during the early weeks of life, and is not a sign of constipation unless bowel motions are firm, dry and pebbly.
Young babies often strain due to the effects of the gastro-colic reflex and the defecation reflex. (See infant reflexes for more information). The 'straining' action helps to move stools through your baby's intestines.
Grunting, groaning and going red in the face while having a bowel motion (fluid or paste consistency) or passing gas is commonly seen in infants around 4 - 6 weeks of age. It is at this age your baby is becoming more aware of his body sensations and he is learning to gain some control over his body movements (that will eventually be necessary to voluntarily control his bowel motions in the future).
It is at this age your baby is becoming more aware of his body sensations and he is learning to gain some control over his body movements (that will eventually be necessary to voluntarily control his bowel motions in the future).
As your baby strains he's also learning which muscles do what and how much effort is needed to poop. He may use a little more effort than necessary to begin with, but after a few weeks of practice he will become a 'poop expert' and straining will settle.
Straining may also occurs at times when your baby is learning to pass a larger or slightly thicker consistency stool than he's used to. This often occurs if his diet is changed such as, changing from breast milk to formula or when he starts on solid foods. This is also normal and generally settles in a week or so.
Straining is normal - Crying while having a bowel motion is not!
What to do when your baby strainsIt's not necessary for you do anything when your baby strains while trying to poop.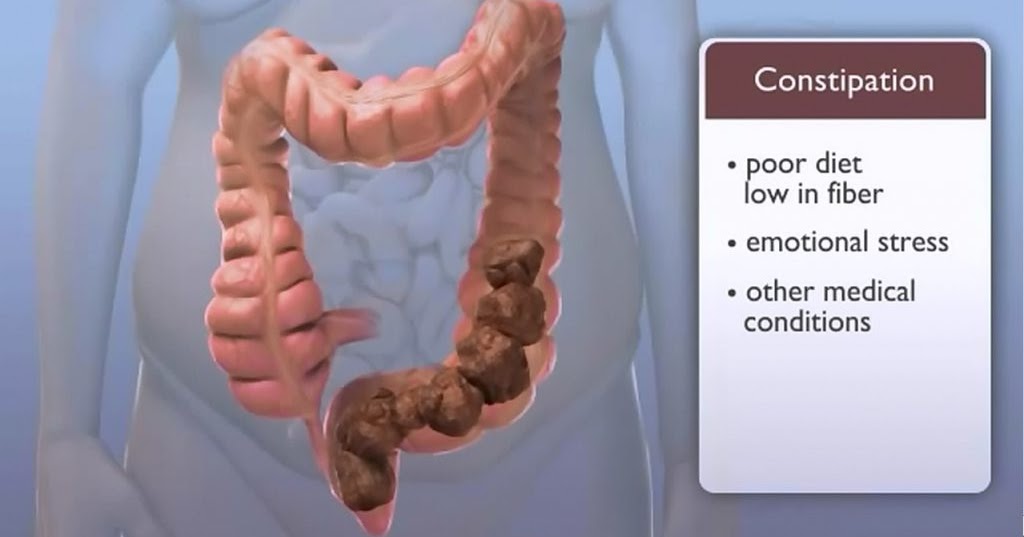 However, if you feel he is straining because of constipation (i.e. firm, dry pebbly poop) you may find lifting his knees to his chest, which is a natural squatting position, by holding his ankles can help him to exert enough pressure to push it out.
However, if you feel he is straining because of constipation (i.e. firm, dry pebbly poop) you may find lifting his knees to his chest, which is a natural squatting position, by holding his ankles can help him to exert enough pressure to push it out.
Alternate this with gently moving his legs backwards and forwards in a 'bicycle' movement. Also try...
- A warm bath.
- A tummy massage.
Your baby's large bowel sits in his abdomen in one large loop. Stools travel in a clockwise direction (clockwise as you face him). To assist him to expel gas that can occur with constipation, it's best to follow the natural path of his large bowel.
Put some oil on your hands and gently but firmly massage his abdomen in a clockwise direction using long stroking actions. Alternate this with lifting his knees and the 'bicycle' movement.
When to see a doctor- If your baby cries while straining.
- If constipation remains a persistent problem.
- If your baby is not gaining weight.
- If the number of wet diapers each day is less than 6.
- If your baby's poop looks unusual or has blood in it.
- If you notice any bleeding from his anus.
- For advice on suitable laxatives.
* Constipation in infants is rarely due to excess iron. Low iron formula should only be given if recommended by your doctor.
Written by Rowena Bennett.
© Copyright www.babycareadvice.com 2020. All rights reserved. Permission from author must be obtained to copy or reproduce any part of this article.
Sugar Water For Babies: Safe Or Unsafe?
Mix sugar in boiled water to make sugar water but follow the proper dosage to avoid health issues.
Research-backed
MomJunction believes in providing reliable, research-backed information to you. As per our strong editorial policy requirements, we base our health articles on references (citations) taken from authority sites, international journals, and research studies. However, if you find any incongruencies, feel free to write to us.
However, if you find any incongruencies, feel free to write to us.
Image: Shutterstock
Sugar water for babies is often used for pain relief. It is prepared by dissolving regular sugar (sucrose or glucose) in water. The solution is commonly used in some cultures as a supplement with breast milk. However, it is not recommended to serve sugar water to babies, especially those younger than six months (1).
Read on to know the use of sugar water for babies and why it is not recommended.
Related: Water For Baby Formula: Which Type Should You Use?
Why Is Sugar Water Used For Babies?
There are several anecdotal and traditional uses of sugar water for babies. Some of the common ones are listed here.
- Aids in pain relief: In medical care, pharmaceutical-grade sugar water (or sweet sucrose water, as often called) is used to provide relief from pain. A research study showed that sterile sugar water could provide moderate pain relief caused by an intravenous procedure, such as the use of vaccine shots during routine immunization in neonates (2) (3).

Several other research studies documented the use of sugar water prior to surgeries or circumcision to provide pain relief to neonates and babies (4).
Quick tip
Give your baby sugar water one to two minutes before the vaccination. Alternatively, you can dip a pacifier in sugar water and give it to the baby before, during, and after the vaccination (10).
Image: iStock
- Support upset stomach: Sugar water or glucose water is often used as a home remedy to provide necessary hydration to babies with an upset stomach. Parents use homemade ORS (oral rehydration solution) made up of warm water, white sugar, and common salt.
Quick tip
Mix six teaspoons of sugar and half a teaspoon salt in one liter of water until completely dissolved to prepare homemade ORS (11).
- Might relieve constipation: Infant constipation is usually common in formula-fed babies and breastfed babies who are transitioning to solids.
 In both cases, sugar water is used as a traditional home remedy to relieve constipation. It is believed that sugar draws additional water into the small intestine and softens the stool. However, there are no clinical studies to support this belief. It is only a home remedy and constipated babies need to be consulted by a pediatrician.
In both cases, sugar water is used as a traditional home remedy to relieve constipation. It is believed that sugar draws additional water into the small intestine and softens the stool. However, there are no clinical studies to support this belief. It is only a home remedy and constipated babies need to be consulted by a pediatrician.
Image: iStock
- Is used for hiccups: In some cultures, sugar water is used to relieve hiccups in babies. However, clinical studies are sparse on this.
- Other purported uses: It was believed that sugar water could cure neonatal jaundice. However, on the contrary, research studies show that sugar water could be harmful in newborn jaundice (5). Doctors do not recommend sugar water to treat neonatal jaundice.
Sugar water is also considered a remedy for colic and gas. However, it is important for you to know that none of these uses are backed by scientific evidence.
How Is Sugar Water Given To Babies?
Image: Shutterstock
The use of sugar water to relieve pain after a medical procedure should be done under medical supervision. A doctor may administer either through a syringe into the baby’s mouth or by placing it on a pacifier (6). Let the pediatrician decide and, if necessary, give sugar water to your baby.
If you want to manage pain at home, then the pediatrician can recommend appropriate medications or pain management techniques. You may also try psychological pain reduction strategies like NNS (non-nutritive sucking), breastfeeding, and skin-to-skin contact.
Related: Can Babies Have Maple Syrup? Safety And Alternatives
Why Is Sugar Water Not Recommended For Babies?
The World Health Organization (WHO) recommends “no use of water” for babies under six months of age (7). For babies older than six months, water can be introduced in small quantities. However, the use of sugar water needs to be avoided due to the following reasons.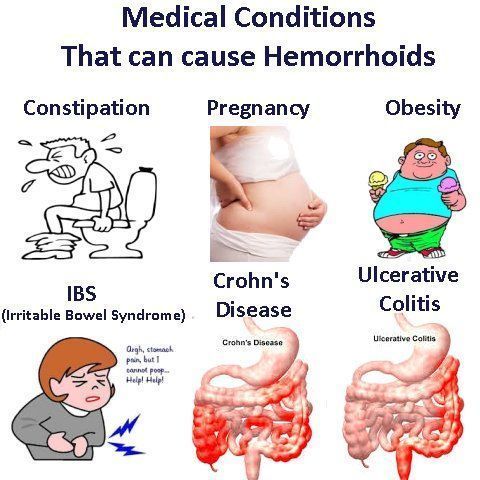
- Could suppress appetite: Sugar water prepared at home can be high in sugar, which can suppress appetite and reduce milk intake in exclusively breastfed infants (8). The same can be expected in formula-fed infants, where the frequency and duration of the feed could come down.
- Can cause electrolyte imbalance: Ingestion of excess sugar water increases the risk of disturbing the electrolyte balance in the body. In severe cases, a baby may even experience water intoxication that can cause seizures.
- Baby might develop a preference for sweet foods: Generally, babies are born with a preference for sweet food. Regular intake of sugar water during their weaning phase may cause them to develop a preference for sweet foods. Besides, sugar water use does not serve any nutritional purpose.
Image: Shutterstock
- Possible exposure to certain health risks: Consumption of excess sugar water can put a baby at an increased risk of excess weight gain, dental cavities, heart disease, diabetes, and fatty liver disease (9).
 This concern is crucial, especially in babies who are on infant formula, which may contain sugar in various forms, like corn syrup.
This concern is crucial, especially in babies who are on infant formula, which may contain sugar in various forms, like corn syrup.
Excess sugar water intake may even cause an upset stomach and spit-up in babies.
If you intend to try sugar water for your baby older than six months, then you should do so after consulting a pediatrician.
Related: Coconut Water For Babies: Safety, Health Benefits, And Side Effects
How Is Sugar Water Prepared For Babies?
Image: Shutterstock
There is no standard recipe to prepare sugar water at home. Try to use as little sugar as possible. Here is one such recipe that you may try under pediatric guidance.
You will need:
- 1 cup plain water (boiled)
- 1tsp sugar
How to:
- Let the boiled water cool until it becomes slightly warm. Take a cup of water and add one teaspoon of sugar to it.
- Mix the sugar in water thoroughly.
 Ensure no granules are left as they could block the nipple of the bottle.
Ensure no granules are left as they could block the nipple of the bottle.
- Taste a drop of the mix. If you feel it is concentrated, then add additional water. However, do not add more than 10-20ml since excess water could dilute the solution.
Note: Avoid giving more than the recommended amount of sugar water to your baby. A concentrated sugar solution can have detrimental effects on an infant’s health, in the long run. Therefore, use it only when required.
1. How much sugar water do I give to my baby?
Your pediatrician is the best person to decide whether you should give your baby sugar water and in what quantities.
2. Does sugar water make babies sleep?
Anecdotally, it is believed that sugar water can distract the baby from pain and may have a calming effect on them. However, there isn’t enough medical research to support the belief. It is suggested to refrain from using sugar water to make the babies fall asleep and try other natural methods.
Using sugar water for babies to relieve pain, constipation, or other signs of discomfort is not advised unless recommended by the pediatrician. Administering too much sugar water at a young age increases the risks of electrolyte imbalance in the body. Also, it makes the baby prone to weight gain and related health issues. If your baby shows signs of colic, consult a healthcare provider or a pediatrician and ask for a safer alternative to sugar water.
Key Pointers
- Sugar water relieves pain, stomach issues, and jaundice in babies.
- However, it is not recommended for babies below six months of age.
- It may cause them to lose their appetite or develop a sweet tooth, eventually posing a risk for dental issues.
- Consult your child’s pediatrician for other remedies and learn the right amount of sugar water to administer to your baby.
References:
MomJunction's articles are written after analyzing the research works of expert authors and institutions. Our references consist of resources established by authorities in their respective fields. You can learn more about the authenticity of the information we present in our editorial policy.
Our references consist of resources established by authorities in their respective fields. You can learn more about the authenticity of the information we present in our editorial policy.
1. Breastfeeding: Getting Started; Stanford Children’s Health
2. Anna Taddio et al.; Effectiveness of sucrose analgesia in newborns undergoing painful medical procedures; National Center For Biotechnology Information
3. Denise Harrison et al.; Efficacy of sweet solutions for analgesia in infants between 1 and 12 months of age: a systematic review; BMJ
4. Analgesic Properties of Oral Sucrose During Routine Immunizations; American Academy of Pediatrics
5. Breastfeeding And Jaundice; American Pregnancy Association
6. Pain and Your Infant: Medical Procedures, Circumcision and Teething; Michigan Medicine
7. Infant and Young Child Feeding; WHO
8. Hasan Boskabadi and Sepideh Bagheri; Comparison between infants receiving traditional supplements (camel thorn, flix weed, and sugar water) and exclusively breast fed infants; National Center For Biotechnology Information
9. Recommended Drinks for Young Children Ages 0-5; Healthy Children; American Academy of Pediatrics
Recommended Drinks for Young Children Ages 0-5; Healthy Children; American Academy of Pediatrics
10. Reduce the Pain of Vaccination in Babies; Caring for Kids
11. Oral Rehydration Solutions: Made at Hom; Rehydration Project
The following two tabs change content below.
- Reviewer
- Author
Swati Patwal is a clinical nutritionist, a Certified Diabetes Educator (CDE) and a toddler mom with over eight years of experience in diverse fields of nutrition. She started her career as a CSR project coordinator for a healthy eating and active lifestyle project catering to school children. Then she worked as a nutrition faculty and clinical nutrition coach in different...
View Profile ›
Dr. Abinaya Mathankumar has around eight years of experience as a pediatrician and a lactation consultant. She did her MBBS from The Tamil Nadu Dr. M.G.R. Medical University in 2012 and completed her postgraduation in 2015.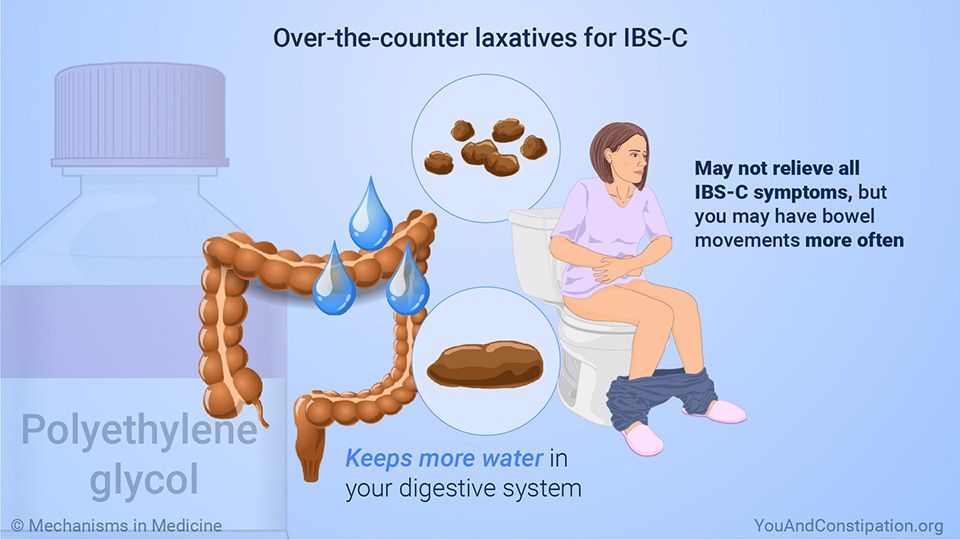 She currently practices at Sakthi Hospital, Thillaipuram, Tamil Nadu, specializing in newborn care and growth and development. She presented her paper on Pediatric Epilepsy...
She currently practices at Sakthi Hospital, Thillaipuram, Tamil Nadu, specializing in newborn care and growth and development. She presented her paper on Pediatric Epilepsy...
View Profile ›
How to deal with constipation in a child?
08/15/17
Manual for parents on a problem that is very common in children with autism
Source: Autism Speaks
to symptoms of chronic constipation includes:
- Very very hard and dense stool.
- Pain and difficulty in emptying the bowels.
- The child has a bowel movement three times a week or less.
Talk to your child's doctor to find out if your child is constipated.
What causes constipation in children with autism?
1. Holding a stool
Some children try to hold a stool and ignore the urge to have a bowel movement. This can happen for various reasons, for example:
- Fear of the toilet.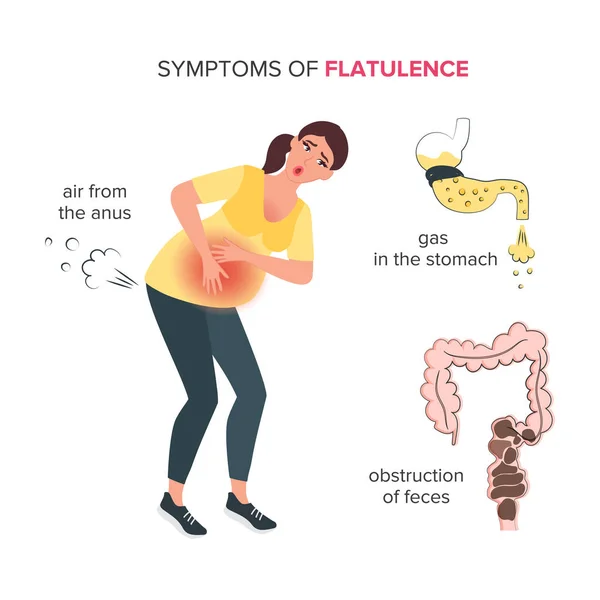
- Reluctance to use the toilet outside the home.
- Unwillingness to interrupt the game.
- Fear of pain during bowel movements.
2. Toilet training
Children may resist and hold stool when toilet training is attempted. This can become a habit that is difficult to break later on.
3. Nutrition problems
- Lack of fiber found in fruits, vegetables and whole grains.
- Dairy products, if the child is allergic to cow's milk or consumes too much dairy products.
- Insufficient intake of water and other beverages, especially when ill.
- Changes in appetite or diet due to illness of the child.
4. Stress and changes in daily routine.
Travel, weather changes, and stress can affect bowel function.
5. Medications
Some medications, such as antacids, antidepressants, and some attention-deficit/hyperactivity disorder medications, can cause stools that are too hard.
6. Associated medical problems.
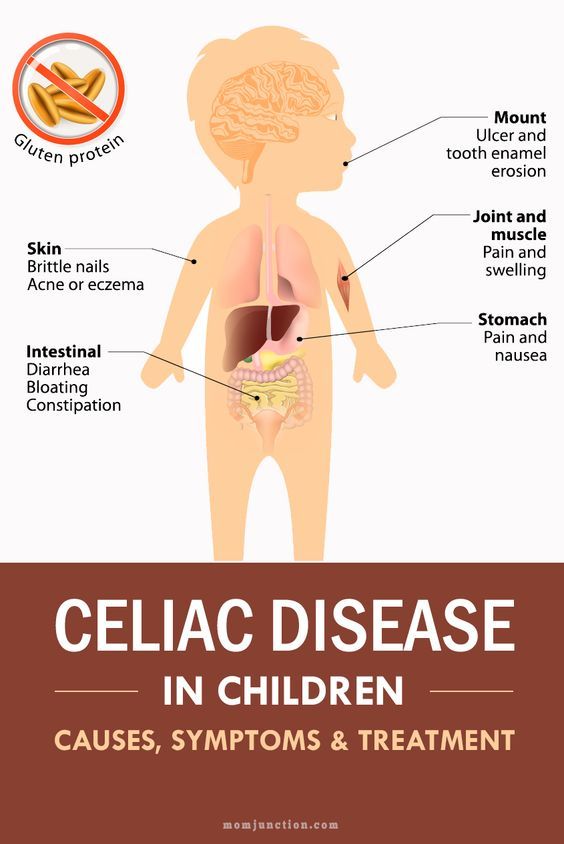
Constipation is common in children who have movement problems, including decreased muscle tone and cerebral palsy. Also, constipation is possible in case of hypersensitivity to gluten or casein.
Acute constipation and encopresis
Acute constipation
Some (but not all) children with chronic constipation may have this problem. Acute constipation can be caused by too much hard stool in the colon. As a result, the child cannot have a bowel movement for several days. Acute constipation is diagnosed by a doctor by palpation of the abdomen or by X-ray. Acute constipation is often accompanied by loss of appetite and lethargy. After a bowel movement, the child feels better and the symptoms decrease.
Encoprese
This problem occurs in some (but not all) constipated children. Encopresis means that during constipation, the child has loose stools. This is a common problem.
Encopresis can develop if a child holds a stool for so long that it becomes difficult for him to have a bowel movement. The stool becomes larger and drier. Due to the retention of large stools, the intestinal muscles get tired and relax. After the muscles relax, loose stools can seep into the underwear.
The child does not feel that this is happening and cannot control loose stools. This usually happens several times a day, causing the underwear to become dirty. Sometimes encopresis is confused with diarrhea, but the child does not actually have diarrhea because most of the stool in the intestines remains solid.
Many children with encopresis experience loss of appetite and decreased interest in daily activities. After a bowel movement, the child feels better and these symptoms decrease.
Treatment of constipation
There are three main approaches to the treatment of constipation.
Talk to your child's doctor about which type of treatment is best for you:
1. Dietary changes
Dietary changes
- Increasing the amount of fiber in your diet will make bowel movements easier.
- Increasing fluid intake , especially water and juice, helps soften stools and reduces the chance of constipation.
2. Behavioral changes
- Regular exercise . Physical activity improves the functioning of the abdominal muscles, which facilitates bowel movements. Regular exercise, including walking, jumping rope, ball games, cycling and swimming, can help with constipation.
- Bowel training in the toilet . It is important that the child knows how to use the toilet at the first urge. The best way to teach this is through planned and extended "sit-downs" where the child is rewarded for simply sitting on the toilet for extended periods of time.
3. Medications
Children often need medication to have regular bowel movements. These can be:
These can be:
- Preparations for daily use.
- Single-dose preparations that "cleanse" the intestines in case of severe difficulty with emptying.
Increasing fiber in the child's diet
A diet high in fiber promotes regular bowel movements and prevents constipation. Fiber is a substance that the body cannot digest. There are two types of fiber - soluble and insoluble. Soluble fiber promotes the entry of water into the intestines. Insoluble fiber facilitates the passage of stool through the intestines. Both types of fiber are needed to prevent constipation.
Fiber is an important part of a healthy diet. A lot of fiber is found in foods such as fruits, vegetables, whole grains, legumes, nuts, and seeds. They also contain a lot of protein, vitamins and minerals. A diet high in these foods is the best way to get enough fiber.
Where to find fiber
When shopping for food, you can check the nutritional information of the product, including the fiber level. Good choices are foods that contain at least 2 grams of fiber per serving.
Good choices are foods that contain at least 2 grams of fiber per serving.
When shopping, look for products that contain whole grains, whole grain flour, and oatmeal. Perhaps there are options for your child's favorite foods with whole grains, that is, higher fiber content. For example, whole-grain cheese crackers, whole-grain wheat flour bread, and high-fiber cereals may be suitable for you.
Recommended Fiber Values
— Ages 1 to 3: 19 grams per day (for boys and girls).
- Ages 4 to 8: 25 grams per day (for boys and girls).
- Ages 9 to 13: 31 grams per day for boys and 26 grams per day for girls.
Examples of high fiber foods
- White beans: 9.5 grams per 1/2 cup.
- Oatmeal: 8.8 grams per 1/2 cup.
- Red beans: 8.2 grams per 1/2 cup.
- Beans: 7.5 grams per 1/2 cup.
- Pear (with skin): 4.3 grams per small pear.
- Raspberries: 4.0 grams per 1/2 cup.
- Baked potatoes (with skin): 3.8 grams per piece.
- Almonds: 3.3 grams per 30 grams.
- Apple (with skin): 3.3 grams per piece.
- Banana: 3.1 grams for one medium-sized piece.
- Orange: 3.1 grams per medium sized piece.
- Peanut butter: 3.0 grams per 2 tablespoons.
- Broccoli: 2.8 grams per 1/2 cup.
- Green peas: 2.5 grams per 1/2 cup.
- Avocado: 2.3 grams per 1/2 cup.
- Corn: 1.6 grams per 1/2 cup.
- Strawberries: 1.5 grams per 1/2 cup.
- Wild rice: 1.5 grams per 1/2 cup.
- Raisins: 1.4 grams per 1/2 cup.
- Popcorn: 1.2 grams per 1 cup.
Increasing fiber and fluid in the child's diet
It is advisable to offer children foods rich in fiber from an early age so that their use becomes a lifelong habit.
If your child is currently constipated, it is important to increase fiber levels very gradually over 2-3 weeks. Too much fiber in the diet can worsen constipation or cause gas, abdominal pain and diarrhea.
Increasing fiber will only be effective if the child also starts drinking more fluids. Make sure your child doesn't just start eating more fiber, but also starts drinking more water and juice.
How to Increase Fiber Without Child Resistance
Children with autism often resist change, especially dietary changes. Parents need to be patient and try different approaches, for example:
- Switch to crackers and whole grain pasta.
- Try whole grain bread and pizza. Many types of whole-grain bread do not differ in appearance from ordinary white bread.
- Offer your child whole grain muesli or popcorn as a snack.
— Offer the child dried fruit as a sweet treat (prunes, dried apricots, raisins).
- Try to make cocktails from frozen fruits or berries based on juice or milk.
- Offer your child carrot, bell pepper, or celery sticks that can be dipped in peanut butter, hummus, or salad dressing.
— Add shredded vegetables or mashed vegetables to your child's favorite foods, such as pasta or pizza.
- Make funny faces or figures out of slices of fruits and vegetables.
- Invite the child to dip fruit slices in nut butter or his favorite kind of yogurt.
- Bake cookies, muffins or pies with whole wheat flour.
Increasing fluid intake
Sufficient water is essential to maintain a healthy body. It is found in both foods and drinks. As you increase the amount of fiber in your diet, you also need to increase your fluid intake.
How much fluid do you need?
- Follow your thirst. The amount of water a child needs varies depending on physical activity and what the child eats. Therefore, it is very important to monitor the signs of thirst in a child.
- When a child drinks enough water, his urine becomes clear, light yellow in color. Dark, tea-colored urine usually means your child needs to drink more.
Fluid types
1. Water: the best source of fluid.
2. 100% juice: good for health, but should be limited.
- 120-180 ml per day for children under 6 years old
- 240-360 ml per day for children over 6 years old
- Some juices (pear, apple, plum) contain sugars that act as a natural laxative and may help with constipation.
3. Milk:
- An important part of a child's nutrition.
— Excessive consumption of milk can lead to constipation.
- Desirable rate for milk: 480-720 ml per day (2-3 cups).
4. Sports drinks and drinks with electrolytes:
- They often have added sugar.
- Not the best choice for children.
- Check with your doctor before giving these drinks to your child.
5. Fruit drinks, soft drinks:
- They usually have added sugar.
- Not the best choice for children.
- It is better to save them for special occasions, such as holidays, you should not give them to the child regularly.
Fluids and constipation
It is very important to increase fluid intake at the same time as increasing fiber. Fluid helps soften stools and make bowel movements easier.
- Some juices (pear, apple, plum) are natural laxatives.
— It is advisable to give the child a lot to drink between meals, this contributes to regular bowel movements.
- Drinks with a lot of sugar, caffeine or "fortified with vitamins" can increase constipation.
Tips for increasing fluid intake
— Encourage your child to drink water between meals, on a full stomach the child may drink too little.
- Offer your child fruits with a high water content, such as grapes, oranges, or watermelon, as snacks and treats.
— Keep a bottle or cup of water handy so your child can always have a drink. Add some citrus juice to your water to make it taste better. Or try adding some other drink to the water.
- Lead by example. Children are more likely to drink water when they see their parents or siblings drinking water.
Children are more likely to drink water when they see their parents or siblings drinking water.
Toilet training
In case of constipation, it is very important to teach the child to use the toilet as soon as he feels the first urge. The easiest way to teach this is with a daily period of time when the child sits on the toilet for a long time. When a child gets used to sitting on the toilet for a long time, it will be easier for him to relax the muscles that hold the stool. With daily toilet seating time, your child will become less likely to hold a stool. When the child stops holding the stool, the intestines return to normal size and become more sensitive.
How to teach your child to sit on the toilet for a long time every day
1. Be patient with yourself and with your child. Learning a new skill, especially this skill, is never easy.
2. Start by teaching your child to sit on the toilet, even if he does not defecate:
- Start with 1-2 minutes. Very slowly increase the time to 10-12 minutes.
Very slowly increase the time to 10-12 minutes.
- Use a visual timer to let your child know how long to sit.
- Offer the child some quiet activity while he sits on the toilet. For example, reading a book, drawing, playing a handheld computer game, listening to music or audio books.
- Try to save the child's favorite pastime for sitting on the toilet and do not offer it at other times.
- Praise your child even for small progress.
- Never force a child to sit on the toilet and never force him to sit on it unless you are working with a behavior specialist to help you do it safely.
3. Choose a time for your child to use the toilet.
- Making toilet use a regular part of a child's daily routine will help develop a normal bowel habit.
— Children with autism often like routine. Making toilet seating a part of the daily routine will reduce the risk of child resistance.
- Try using a visual timetable with pictures, one of the items being toilet time.
— If your child is most likely to have a bowel movement at some time of the day, try to schedule toilet seating for that time.
— Morning is the best time for most people, but it may not be suitable for a child who will be rushed to kindergarten or school in the morning.
- For some children, the best time is after coming home from school or kindergarten.
4. Make sure your child is comfortable.
- Choose the toilet seat or potty that is most comfortable for your child.
— Use a child seat for the toilet if the normal seat is too big for the child.
- Use the footrest if the child's feet do not touch the floor.
How to teach a bowel movement in the toilet
1. Make sure your child sits on the toilet for long periods of time 1-2 times each day.
2. Teach your child that "poop goes down the toilet" by emptying dirty diapers or underwear.
3. Try to time your child to sit on the toilet when you think your child is most likely to have a stool.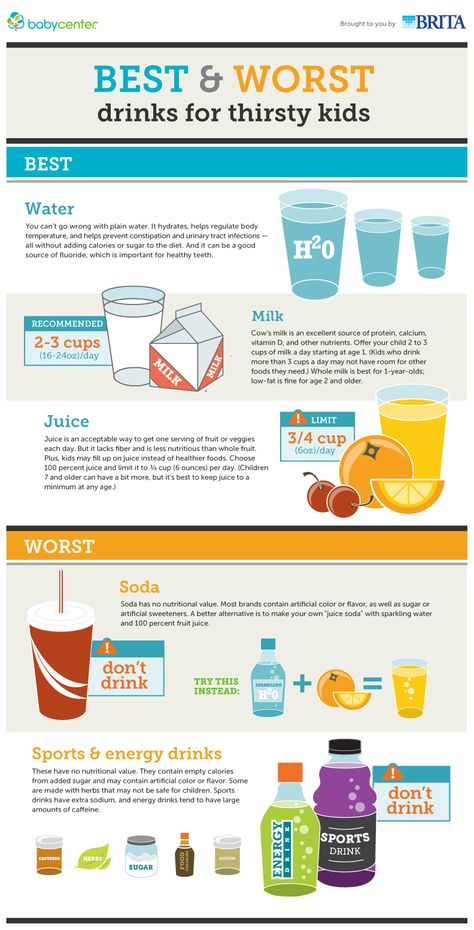
4. Try to stimulate the gastrocolic reflex before sitting on the toilet. This reflex occurs after eating or drinking and allows the bowel muscles to expel stool after eating. To stimulate this reflex, try to get your child to eat or snack, and drink a warm drink before sitting on the toilet.
5. Watch for possible signs in the child's behavior. If you notice that he wants to use the toilet, then take him there. Signs may include:
- Changes in facial expressions.
- Attempts to go to a quiet part of the house.
- Muscular tension.
Positive reinforcement
- Start with rewards for your child just sitting on the toilet.
- When the child begins to empty his bowels on the toilet, start rewarding him for it.
- Small rewards that the child receives immediately after the desired behavior work best.
- Give rewards less frequently over time.
Try not to use food as a reward. Instead, you can reward your child with:
- Sing your favorite song with your child.
- Hugs, tickling, verbal praise.
- Favorite game with a child.
- Stickers that will allow the child to track their progress.
- Time for your favorite pastime.
- Tokens (in the form of stickers, stars or other items) that can then be exchanged for very large rewards, such as a trip to the cinema or to the park.
Many children with autism have special interests. They can be used when planning rewards. For example, if a child is interested in cars, then as a reward, he can look at car magazines. If a child loves trains, then he can receive stickers with trains as a reward.
Positive rewards lead to the desired changes in behavior much faster than any punishment or criticism.
If the child is dirty
- Say something like "I noticed that you are dirty" or "Please change."
- Help the child to do this as needed.
— Do not scold the child or draw attention to what has happened.
If the child does not want to sit on the toilet
- Try to get the child as close to the toilet as possible when he begins to have a bowel movement. If the child does it in diapers while standing, then try to have him do it while standing in the toilet.
If the child does it in diapers while standing, then try to have him do it while standing in the toilet.
- When the child has defecated in the diaper, throw the contents of the diaper down the toilet in front of the child.
- Teach your child to sit on the toilet with their clothes down. Give your child a toy that can keep him busy for a while.
- Over time, move on to having the child sit on the toilet with the lid up but wearing a diaper.
- When the baby is comfortable sitting on the toilet with the lid up, cut a hole in the diaper and enlarge it over time. Try to have the child sit on the toilet in a diaper while having a bowel movement.
Specialist help
Very often it is difficult for a family to change what happens at home. Toilet training can be a very complex behavioral problem. Some families need additional specialist support. Signs that the family needs more help include:
- The child becomes very upset when taken to the toilet.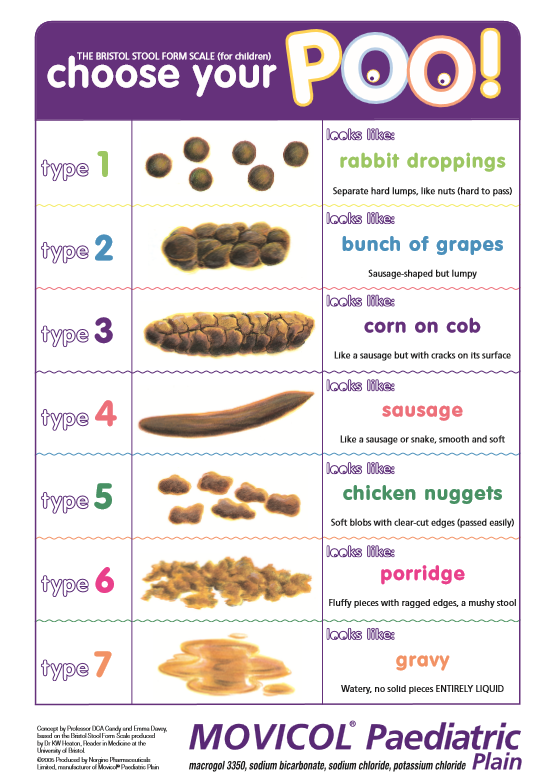
- Child holds stool longer and longer.
— Constipation progresses in the child.
— Everything connected with the toilet causes tantrums or aggression in the child.
Specialists may include child psychologist, behavioral analyst, pediatrician. Sometimes staff at the child care facility that the child attends can help find the right specialist.
Daily preparations
— May be started immediately if the child does not have acute constipation.
- Taken orally.
- Most effective when taken daily.
Purpose of taking the drug:
- Soft stools and bowel movements every day.
- All stool comes out of the bowels.
Dosage of the drug:
- The initial dose of the drug must be prescribed by a doctor. Sometimes the dosage needs to be varied. Talk to your doctor about this, he will help you change the dosage.
When it is necessary to increase the dosage of the drug:
- Small and hard stools.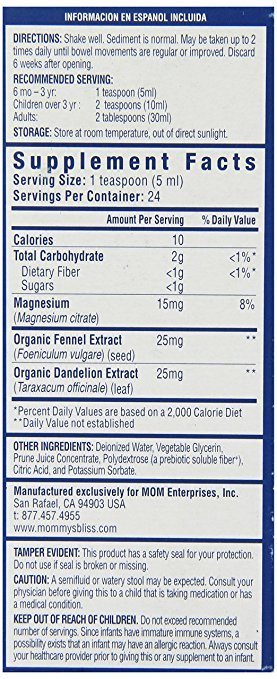
- The child does not have a bowel movement every day.
- The child has difficulty emptying the bowels or is in pain.
When to reduce the dosage of the drug:
- Loose stools.
— The child has abdominal pain or cramps.
Duration of drug treatment
— As a rule, the course of treatment lasts at least 6 months.
— After 6 months of daily bowel movements, the doctor may decide to gradually reduce the dosage of the drug.
- If you stop taking the drug before the intestines return to normal, then constipation will begin again.
— It is important to make sure that the child has soft stools every day.
How do drugs to treat constipation work?
There are three types of laxatives. They act differently.
1. Osmotic laxatives. They carry water into the stool to keep it soft. Safe and often given to children. Usually taken every day. Suitable for long term use.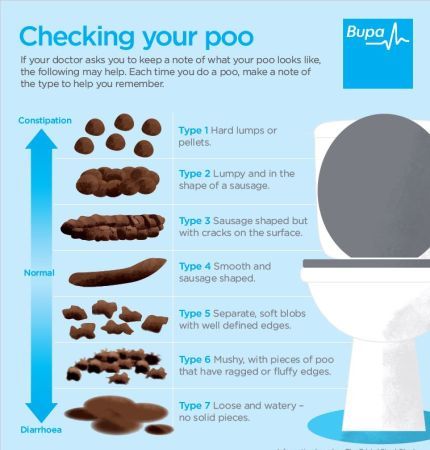
Examples: polyethylene glycol without electrolytes, magnesium hydroxide, magnesium citrate, lactulose, sorbitol.
2. Stimulant laxatives. They promote contractions of the intestinal muscles and promote stool in the intestines. As a rule, they are prescribed for a single dose.
Examples: senna, bisacodyl.
3. Lubricating laxatives. Facilitate the passage of stool through the intestines with an oil base.
Examples: liquid paraffin, glycerin suppositories.
Acute constipation medicines
Acute constipation occurs when large masses of hard stool block the intestines. If the doctor thinks that there is a blockage in the intestines, then as a first treatment option, he may prescribe a drug that will "cleanse" the intestines.
Your doctor will work with you to determine the best type of drug. Sometimes drugs that are taken by mouth are best. Sometimes drugs that are injected into the intestines are better suited. This "clearing" usually takes 2-3 days. It is best to spend it on the weekend or on vacation. The child will need to spend 2-3 days near the toilet and use it often.
Sometimes drugs that are injected into the intestines are better suited. This "clearing" usually takes 2-3 days. It is best to spend it on the weekend or on vacation. The child will need to spend 2-3 days near the toilet and use it often.
These drugs can only be prescribed by a doctor. He will tell you how long and how often to take the drug.
Enema procedure
Most cases of constipation in children are treated with oral medications. In some cases, children need a drug that is injected into the rectum. Talk to your doctor about what treatment is best for your child. Do not give your child an enema without talking to the doctor first. Below is information about giving an enema, if needed.
How to prepare a child for an enema
- Explain the procedure to the child in a way that he can understand, perhaps with illustrations.
- Let the child look at and touch the enema bottle.
- Touch the tip of the enema to his hand so he knows what it's like.
- Help your child practice beforehand how to lie down properly during an enema.
Enema preparation
— Read the instructions for the enema very carefully. Check out the pictures and instructions in the instructions.
- Make sure the enema is at room temperature.
- Prepare everything you need: an enema bottle; towel on which the child will lie; pillows; music, a favorite toy, or other items to help your child stay calm; wet cleansing wipes.
Decide where you will give the enema. Sometimes it's best to put the baby on a blanket or large towel on the bathroom floor next to the toilet.
- Place towels and/or pillows for your child to lie down comfortably.
- Have another person stand at eye level with the child during the procedure - read to him, sing, talk, play music or otherwise distract him and help him lie still.
How to give an enema
1. Wash your hands.
2. Remove the protective cap from the enema tip. The tip should have a lubricant that makes it easier to administer the enema.
The tip should have a lubricant that makes it easier to administer the enema.
3. Help the child lie on his left side with his knees pressed against his chest.
4. Have your helper talk or sing to your child in an effort to soothe and encourage.
5. Hold the enema in one hand. With your other hand, spread your buttocks until you see the anus.
5. Insert the end of the bottle very carefully into the anus. Don't force it in.
6. Position the end of the enema towards the child's back. The contents of the enema should fall on the intestinal wall, and not on the stool.
7. Squeeze the enema until nearly the entire volume has been delivered.
8. If possible, try to have the child lie down for 15-20 minutes. You can hold on to his buttocks to prevent him from pushing out the contents of the enema too soon.
9. If your child wears diapers, put on a diaper.
10. If the child uses the toilet, then put him on the toilet after 15-20 minutes. The liquid should go down the toilet along with the stool.
The liquid should go down the toilet along with the stool.
If at any stage the child becomes very upset, starts crying, screaming, kicking, then it is normal to stop the procedure. Talk to your doctor about other treatments for constipation.
We hope that the information on our website will be useful or interesting for you. You can support people with autism in Russia and contribute to the work of the Foundation by clicking on the "Help" button.
Parenting children with autism, Nutrition and digestion, Comorbidities
Constipation in children under one year old
Usually, parents of babies are worried about the exact opposite problem - too frequent stools. Therefore, not everyone immediately understands what to do if a baby under one year old has constipation.
Gastroenterologist, hepatologist at GMS Clinic Sergey Vyalov gave an interview to the Internet portal parents.ru and spoke about constipation in children under one year old.
Introduction
Constipation, also known as diarrhea, stool retention, discolia, caprostasis, difficulty in emptying the bowel is not a universal condition with unambiguous characteristics. Each person, including a child, has his own indicators of the norm and deviations from it, associated with age, intestinal microflora, diet, state of mind and hormonal background, concomitant diseases. Yet there are a few common points of reference.
What is constipation?
Specialists diagnose constipation if the baby does "big" things:
- regularly and without problems, but passing dry and hard stools;
- with difficulty - the child has to push, the feces do not come out on the first try;
- less than 5 times per day.
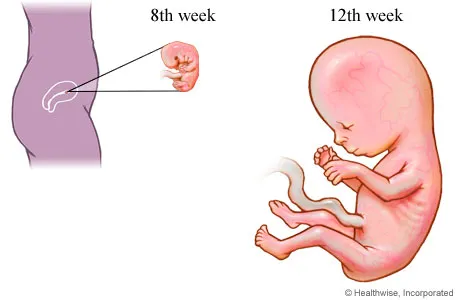
In the first six months of life, constipation is a rather rare occurrence, rather, on the contrary, in the period from 0 to 6 months, 6-10 bowel movements per day are considered the norm. Breastfed babies have more frequent bowel movements, while artificial babies have less.
Breastfed babies have more frequent bowel movements, while artificial babies have less.
Up to 6 months constipation is rare
Usually, parents of babies in the first months of life are alarmed by the condition opposite to constipation - too frequent bowel movements. But in a baby, regardless of whether he eats breast milk or formula, the intestines should work exactly like this - in a mode that is considered diarrhea for older children and adults.
There should be no other option, at least until the introduction of complementary foods at 4-6 months. After all, the baby receives mostly liquid food, the waste products of which have the same consistency and leave the intestines without encountering any obstacles on the way - the baby has not yet learned to control the sphincter that restrains the release of feces.
The baby's intestines have just begun to "get acquainted" with microorganisms that come from mother's milk, from her skin (the baby licks the nipple), from the environment.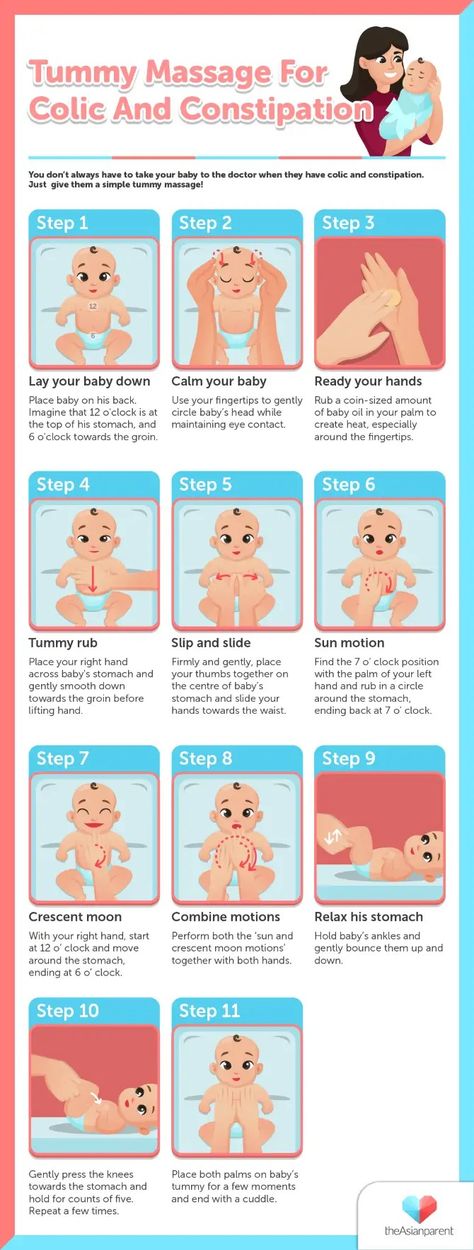 Far from all new "partners" are accepted: there are rejected ones, those who have not taken root, and so on. Checking and rejection are accompanied by loose, unstable stools.
Far from all new "partners" are accepted: there are rejected ones, those who have not taken root, and so on. Checking and rejection are accompanied by loose, unstable stools.
Too frequent bowel cleansing does not need correction and treatment if the child is gaining weight and developing properly. Normal appetite and sleep, gas, absence of fever and other signs of illness indicate that parents have nothing to worry about. If the mother of a baby, tired of changing diapers 10 times in one day, wants to change the situation and asks the doctor to prescribe fixing medicines for the baby, then, unwittingly, she will doom her baby to chronic constipation.
Not according to the rules
And yet, in the first 6 months, constipation in infants is not excluded. It can be called:
- microflora transmitted from mother;
- insufficient fluid volume;
- stress.
Let's say a woman has too many methane-producing bacteria in her stomach and intestines that cause constipation. They grow rather slowly, ferment, releasing carbon dioxide, which contributes to flatulence and bloating. With this deviation, the woman lives, adapted and learned to solve the problem with the intestines in one way or another. Noticing the same thing in a child, she decides that the baby has inherited her features and "saves" him with the same means, making a mistake. Babies should not be given laxatives, especially those containing senna. The baby's body gets used to such drugs too quickly and without them it can no longer cleanse the intestines.
They grow rather slowly, ferment, releasing carbon dioxide, which contributes to flatulence and bloating. With this deviation, the woman lives, adapted and learned to solve the problem with the intestines in one way or another. Noticing the same thing in a child, she decides that the baby has inherited her features and "saves" him with the same means, making a mistake. Babies should not be given laxatives, especially those containing senna. The baby's body gets used to such drugs too quickly and without them it can no longer cleanse the intestines.
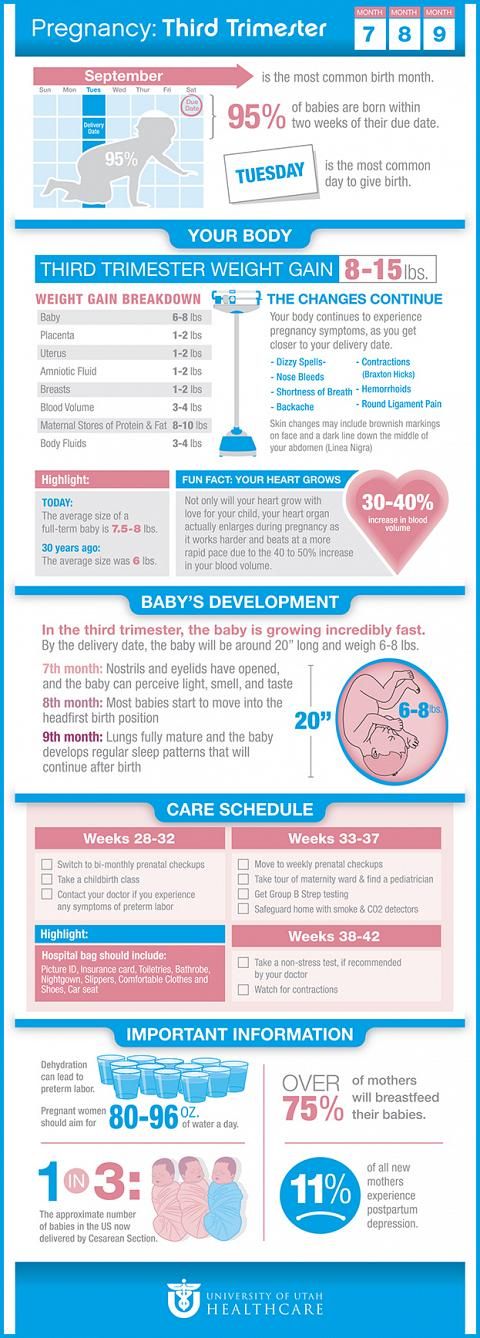
Constipation in a baby up to 6 months is also provoked by a lack of fluid and hormonal fluctuations. At 6 months, the baby should receive a lot of moisture - about 140 ml per kilogram of weight per day. A breastfed child gains this rate from mother's milk and does not need additional sources of liquid (but only if there is no predisposition to constipation). Little artificers are soldered from the moment they switch to a mixture.
If a woman is tense or nervous, then her level of the stress hormone cortisol rises. Through breast milk, saliva or sweat, the substance enters the baby's body and also provokes constipation.
Even if the mother does not breastfeed the baby, the constipating microorganisms sooner or later get to the gastrointestinal system of the crumbs and make negative changes in it.
Constipation after introduction of complementary foods
The kid is growing, improving his skills, and it's time to introduce him to new foods. These circumstances, on the one hand, help to establish peristalsis, and on the other hand, increase the risk of constipation.
By six months, the baby is already trying to control defecation, because he realized that after it there are unpleasant sensations - itching, burning and other discomfort in the areas where the feces get. In order not to experience discomfort, the child tries to restrain the urge. At first, he does not succeed, because the rectum has already learned how to work - reflexively contract and push out waste. And after a couple of months, everything works out, the baby wins and enters the path leading to chronic constipation. To get the baby out of this vicious circle, the mother must minimize the duration of the baby's skin contact with feces and expand the baby's diet by mastering complementary foods.
And after a couple of months, everything works out, the baby wins and enters the path leading to chronic constipation. To get the baby out of this vicious circle, the mother must minimize the duration of the baby's skin contact with feces and expand the baby's diet by mastering complementary foods.
Proteins, fats and carbohydrates that are part of the products are absorbed in the small intestine, and do not reach the large intestine, where feces are formed. What can not be said about fiber. While the baby is drinking breast milk or formula, this component of the dishes is not familiar to him. Even if a nursing woman herself consumes a lot of plant foods, the baby does not get anything. Fiber, as already noted, is not absorbed in the intestines, does not enter the bloodstream, which means that it is not in breast milk. For the first time, a baby gets fiber with complementary foods by trying its first 25 grams of mashed potatoes from zucchini, carrots and other vegetables. Plant fibers literally attract all waste to themselves, as a result, fecal masses are formed, which help the intestines to master the correct peristalsis. There are a lot of muscles in this section of the gastrointestinal tract, in the intestines, they must learn to consistently contract - tighten and relax in order to squeeze waste out.
There are a lot of muscles in this section of the gastrointestinal tract, in the intestines, they must learn to consistently contract - tighten and relax in order to squeeze waste out.
The next new product should be introduced one month after the previous one. The novelty is likely to cause more frequent and loose stools at first. If it does not have a green color and does not foam, there is no need to run to the doctor and ask to prescribe fixatives. Be patient, after a while the innovation will be mastered and will bear fruit. Instead of liquid and shapeless yellow-white feces, you will see brown feces that have formed.
Special constipation
There are other causes of constipation in babies. Unfortunately, they are much more difficult to deal with, since these are developmental pathologies, diseases, and injuries.
Acute constipation. It develops for anatomical reasons, for example, due to obstruction of the large intestine, or during intussusception - the introduction of one part of the intestine into another, which causes blockage of the lumen. Against the background of complete well-being, the baby suddenly becomes restless, cries, refuses to eat. The attack ends as unexpectedly as it began, but after 3-5 minutes it repeats and intensifies: one or two times vomiting appears with an admixture of green bile. If the stool passes, then blood impurities are visible in it. After 5–6 hours, the stool stops, and bloody discharge comes out of the rectum. At the same time, the baby's stomach is soft. The temperature is usually normal. The child may even lose consciousness. With such symptoms, you need to call an ambulance.
Against the background of complete well-being, the baby suddenly becomes restless, cries, refuses to eat. The attack ends as unexpectedly as it began, but after 3-5 minutes it repeats and intensifies: one or two times vomiting appears with an admixture of green bile. If the stool passes, then blood impurities are visible in it. After 5–6 hours, the stool stops, and bloody discharge comes out of the rectum. At the same time, the baby's stomach is soft. The temperature is usually normal. The child may even lose consciousness. With such symptoms, you need to call an ambulance.
Hirschsprung disease. It is based on a violation of the innervation of the large intestine - the central nervous system cannot control this section of the gastrointestinal tract. As a result, processed food accumulates in the intestines. The picture of the disease is quite diverse. If only the short part of the intestine is affected, then constipation forms gradually, and it is possible to do without surgical intervention for quite a long time. When a longer segment is affected, the absence of stool is fraught with a serious condition and immediate surgical intervention is required.
When a longer segment is affected, the absence of stool is fraught with a serious condition and immediate surgical intervention is required.
infectious attack. If in the first months of life the baby suffered an intestinal infection, the nerve cells in the large intestine may die, which will lead to a delay in the act of defecation, accumulation of feces and the development of constipation. With dysentery, the so-called toxic megacolon is possible (a sharp expansion of the colon). The child develops impaired consciousness and repeated vomiting. The abdomen increases sharply due to a greatly enlarged intestine. The complication requires emergency surgical care.
Problems with the CNS. Injuries during childbirth and the syndrome of infantile cerebral palsy also affect the functioning of the gastrointestinal tract, as they are associated with various complications, such as impaired swallowing, regurgitation, and vomiting.
Vasculitis. Vascular inflammation extends to the nerve plexuses and sensitive cells located in the intestinal wall.