How long after chlamydia treatment
Chlamydia - Treatment - NHS
Chlamydia can usually be effectively treated with antibiotics. More than 95% of people will be cured if they take their antibiotics correctly.
You may be started on antibiotics once test results have confirmed you have chlamydia. But if it's very likely you have the infection, you might be started on treatment before you get your results.
The two most commonly prescribed antibiotics for chlamydia are:
- doxycycline – taken every day for a week
- azithromycin – one dose of 1g, followed by 500mg once a day for 2 days
Your doctor may give you different antibiotics, such as amoxicillin or erythromycin, if you have an allergy or are pregnant or breastfeeding. A longer course of antibiotics may be used if your doctor is concerned about complications of chlamydia.
Some people experience side effects during treatment, but these are usually mild. The most common side effects include stomach ache, diarrhoea, feeling sick, and thrush in women.
When can I have sex again?
If you had doxycycline, you shouldn't have sex – including vaginal, oral or anal sex, even with a condom – until both you and your partner(s) have completed treatment.
If you had azithromycin, you should wait 7 days after treatment before having sex (including oral sex).
This will help ensure you don't pass on the infection or catch it again straight away.
Will I need to go back to the clinic?
If you take your antibiotics correctly, you may not need to return to the clinic.
However, you will be advised to go back for another chlamydia test if:
- you had sex before you and your partner finished treatment
- you forgot to take your medication or didn't take it properly
- your symptoms don't go away
- you're pregnant
If you're under 25 years of age, you should be offered a repeat test for chlamydia 3 to 6 months after finishing your treatment because you're at a higher risk of catching it again.
Testing and treating sexual partners
If you test positive for chlamydia, it's important that your current sexual partner and any other recent sexual partners you've had are also tested and treated.
A specialist sexual health adviser can help you contact your recent sexual partners, or the clinic can contact them for you if you prefer.
Either you or someone from the clinic can speak to them, or the clinic can send them a note to let them know they may have been exposed to a sexually transmitted infection (STI).
The note will suggest that they go for a check-up. It will not have your name on it, so your confidentiality will be protected.
Page last reviewed: 01 September 2021
Next review due: 01 September 2024
Causes, Symptoms, Treatment & Prevention
Overview
Chlamydia trachomatis bacterium.
What is chlamydia?
Chlamydia is a common sexually transmitted infection (STI) that’s caused by a bacteria called chlamydia trachomatis (C. trachomatis). Once a person's infected, they can spread chlamydia to their partners through intercourse, anal sex or oral sex. Infections can also occur when partners share sex toys that have become contaminated with the bacteria responsible for chlamydia.
Chlamydia infections are treatable and curable. But it’s important to receive treatment as soon as possible. Left untreated, chlamydia can lead to serious complications.
Who does chlamydia affect?
Anyone who’s sexually active can get chlamydia. The bacteria that causes chlamydia gets transmitted through vaginal fluid and semen, which means that people of all genders who have sex can become infected with chlamydia and infect their partners, too. If you’re pregnant and have chlamydia, you can pass it on to your newborn.
How common is chlamydia?
Chlamydia is the most common STI caused by bacteria. Nearly 2 million cases of chlamydia were reported to the CDC in 2019. The number of infections is likely even higher. When compared to previous years, 2019 infection rates increased among people of all genders, all races and ethnicities, and in every region of the U.S. Most cases of chlamydia are asymptomatic, which means there are no signs or symptoms of an infection. Many of these cases likely go unreported.
Nearly 2 million cases of chlamydia were reported to the CDC in 2019. The number of infections is likely even higher. When compared to previous years, 2019 infection rates increased among people of all genders, all races and ethnicities, and in every region of the U.S. Most cases of chlamydia are asymptomatic, which means there are no signs or symptoms of an infection. Many of these cases likely go unreported.
Certain demographic characteristics (like age, gender and race) may make you more likely to get diagnosed with chlamydia. You’re more likely to get diagnosed if you’re:
- A teen or young adult aged 15 to 24. More than half of all diagnosed chlamydia cases in the U.S. occur in this age group.
- A cisgender woman aged 15 to 24. Young women in this age group are targeted for chlamydia screenings, and the rate of infection among those who are tested is high.
- A man who has sex with men (MSM). Chlamydia infections disproportionately affect men who have sex with men.
- Black and non-Hispanic. Chlamydia infections disproportionately affect non-Hispanic Black populations.
Higher rates of transmission among certain groups are less about sexual behavior and more about networks and lack of access to STI prevention resources. For example, chlamydia is more likely to spread from person to person within communities that have higher infection rates. And it’s more likely to spread among groups that don’t have easy access to sex education or barriers to STIs like condoms and dental dams.
Symptoms and Causes
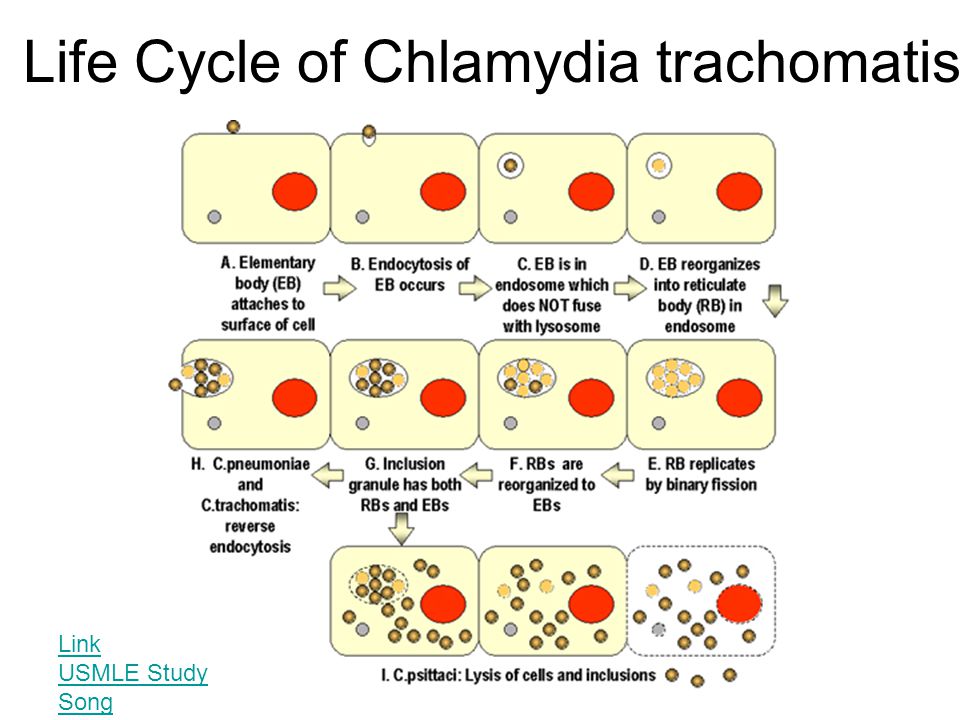
What causes chlamydia?
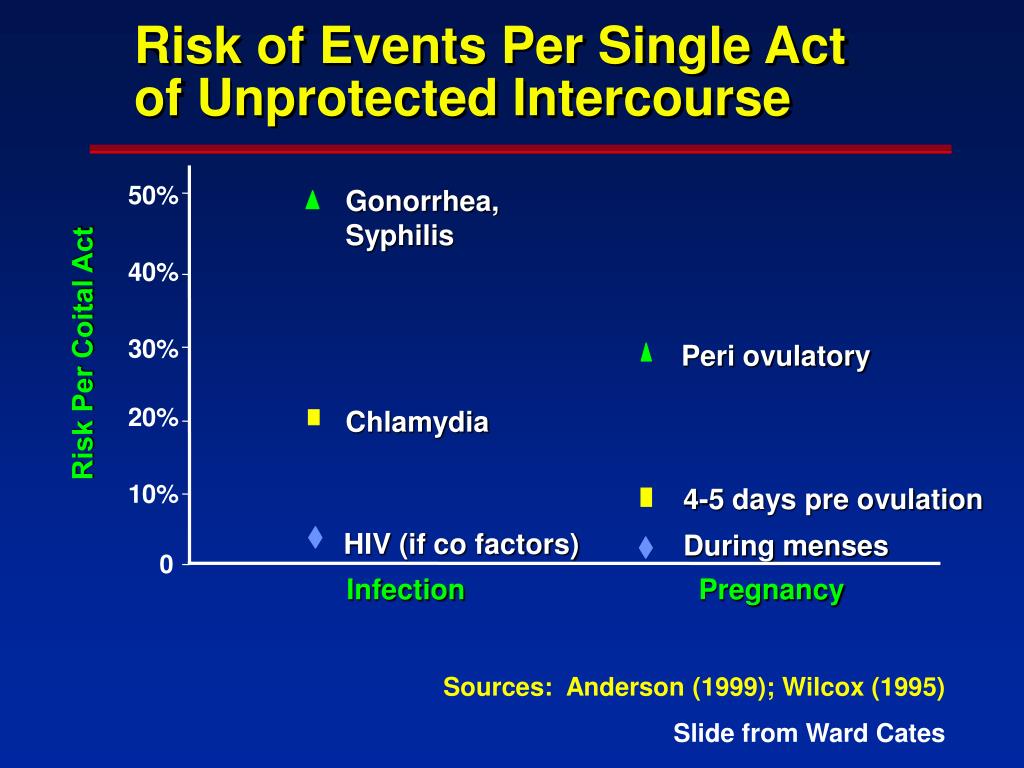
Chlamydia infections spread through sexual contact, when vaginal fluid or semen containing the bacteria that causes chlamydia travels from one person to another. Sexual contact includes all kinds of sex, including sex that doesn’t involve penetration or ejaculation. There are lots of ways that the fluids from one person’s genitals can transmit the bacteria that causes chlamydia.
- Intercourse. Bacteria pass from one person’s penis to their partner’s vagina or vice versa.
- Anal sex. Bacteria passes from one person’s penis to their partner’s anus or vice versa.
- Oral sex. Bacteria passes from one person’s mouth to their partner’s penis, vagina, or anus, or vice versa.
- Sex involving toys. Bacteria pass from a toy with the bacteria to a person’s mouth, penis, vagina or anus.
- Manual stimulation of the genitals or anus. Less commonly, infected vaginal fluid or semen can come in contact with a person’s eye, causing an infection called conjunctivitis. For example, this can happen if you touch the genitals of an infected person and then rub your eyes without washing your hands first.
What doesn’t cause chlamydia?
Not all situations involving an exchange of body fluids or intimacy cause chlamydia. You can’t get chlamydia from:
- Kissing.
- Sharing food or drinks.
- Hugging or holding hands.
- Using a toilet after someone else.
- Inhaling droplets after someone coughs or sneezes.
How long can you have Chlamydia without knowing?
Chlamydia is sometimes called a silent infection because the majority of people who have chlamydia — regardless of gender — never notice symptoms. People who do notice symptoms often don’t recognize the signs that they have chlamydia until a few weeks after they’ve been infected. Because chlamydia cases are often asymptomatic, it’s easy to spread chlamydia to someone else without realizing it. And it’s easy to miss out on receiving the treatment needed to prevent the serious complications that can result from chlamydia.
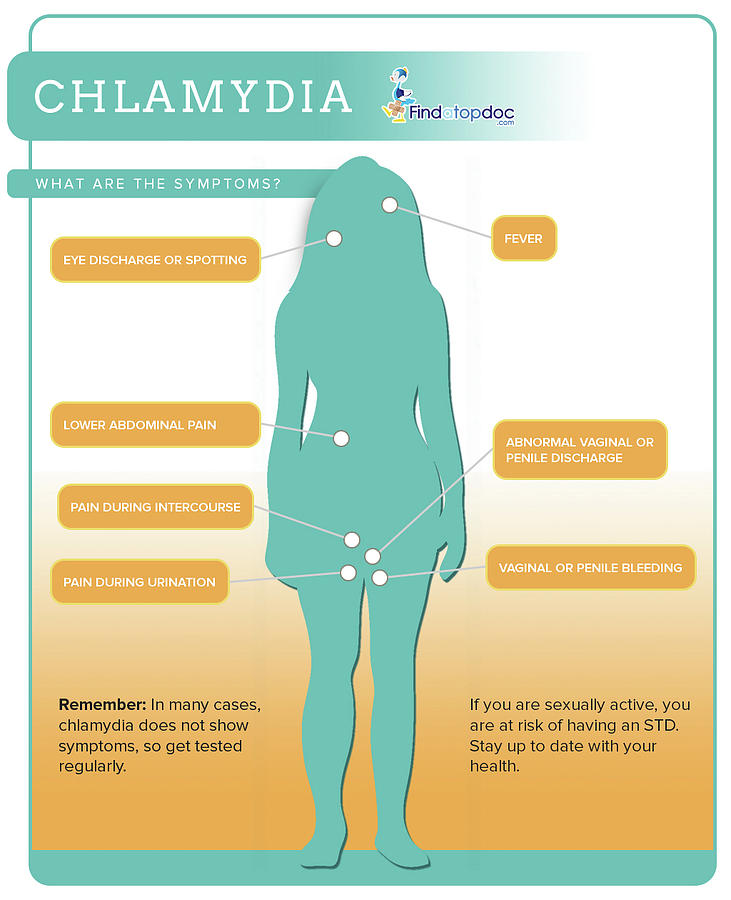
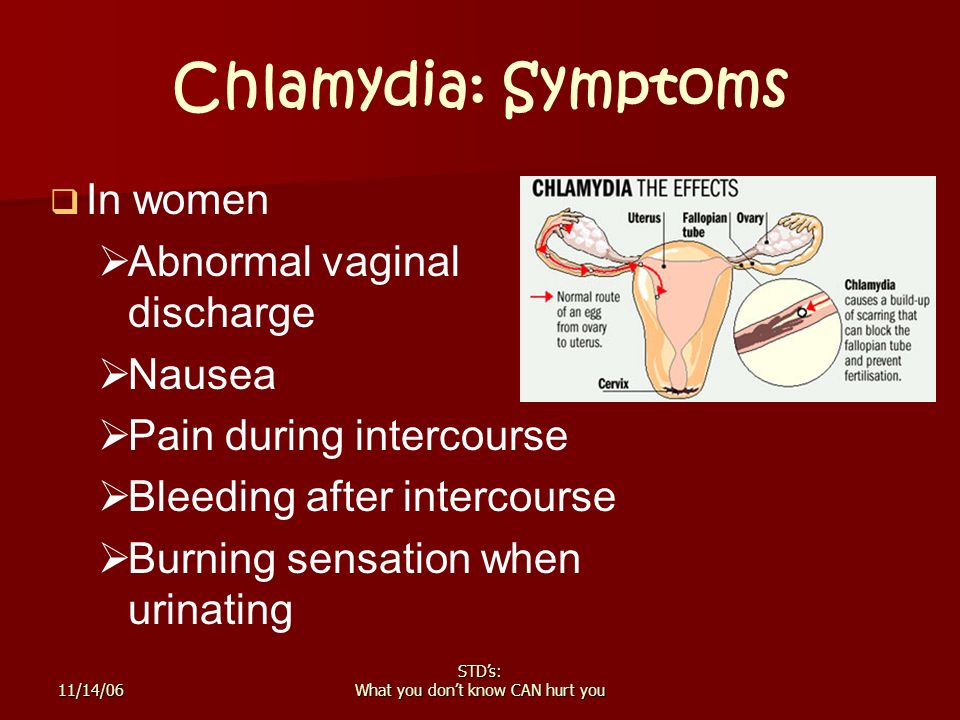
What are the symptoms of Chlamydia?
If you do notice symptoms, you’ll likely experience them differently based on your reproductive anatomy. Many of the symptoms that cisgender women experience can also affect transgender men and nonbinary individuals with vaginas. Many of the symptoms that cisgender men notice can affect transgender women and nonbinary individuals with penises, too.
Many of the symptoms that cisgender men notice can affect transgender women and nonbinary individuals with penises, too.
Signs of chlamydia if you have a vagina
Chlamydia bacteria often cause symptoms that are similar to cervicitis or a urinary tract infection (UTI). You may notice:
- White, yellow or gray discharge from your vagina that may be smelly.
- Pus in your urine (pyuria).
- Increased need to pee.
- Pain or a burning sensation when you pee (dysuria).
- Bleeding in between periods.
- Painful periods.
- Painful intercourse (dyspareunia).
- Itching or burning in and around your vagina.
- Dull pain in the lower part of your abdomen.
Signs of chlamydia if you have a penis
Chlamydia bacteria most often infect your urethra, causing symptoms that are similar to nongonococcal urethritis. You may notice:
- Mucus-like or clear, watery discharge from your penis.
- Pain or a burning sensation when you pee (dysuria).
Signs of chlamydia that all genders may notice
Chlamydia can affect parts of your body other than your reproductive organs, such as your:
- Anus. You may notice pain, discomfort, bleeding or a mucus-like discharge from your bottom.
- Throat. You may have a sore throat, but you usually won’t notice symptoms if the bacteria’s in your throat.
- Eyes. You may notice symptoms of conjunctivitis if C. trachomatis bacteria gets in your eye. Symptoms include redness, pain and discharge.
See your healthcare provider immediately if you notice any of these symptoms.
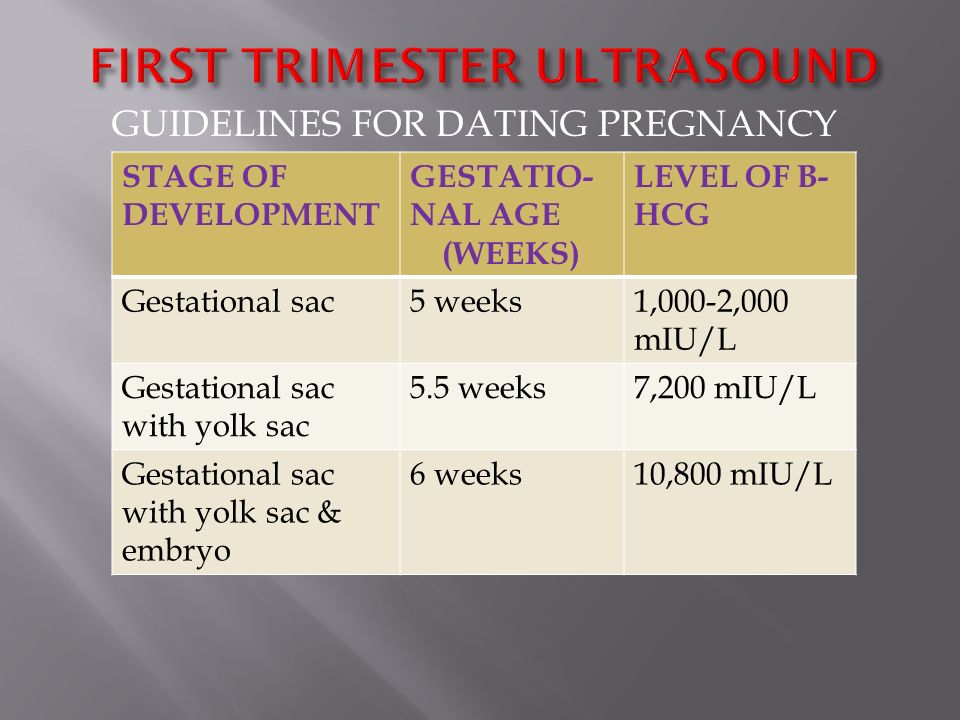
Diagnosis and Tests
How is Chlamydia diagnosed?
The most common test for chlamydia is called a nucleic acid amplification test (NAAT). Your provider takes a sample of fluid by doing a vaginal/cervical swab or collecting a urine sample. Then, they send the sample off to a lab to check for the bacteria that causes chlamydia.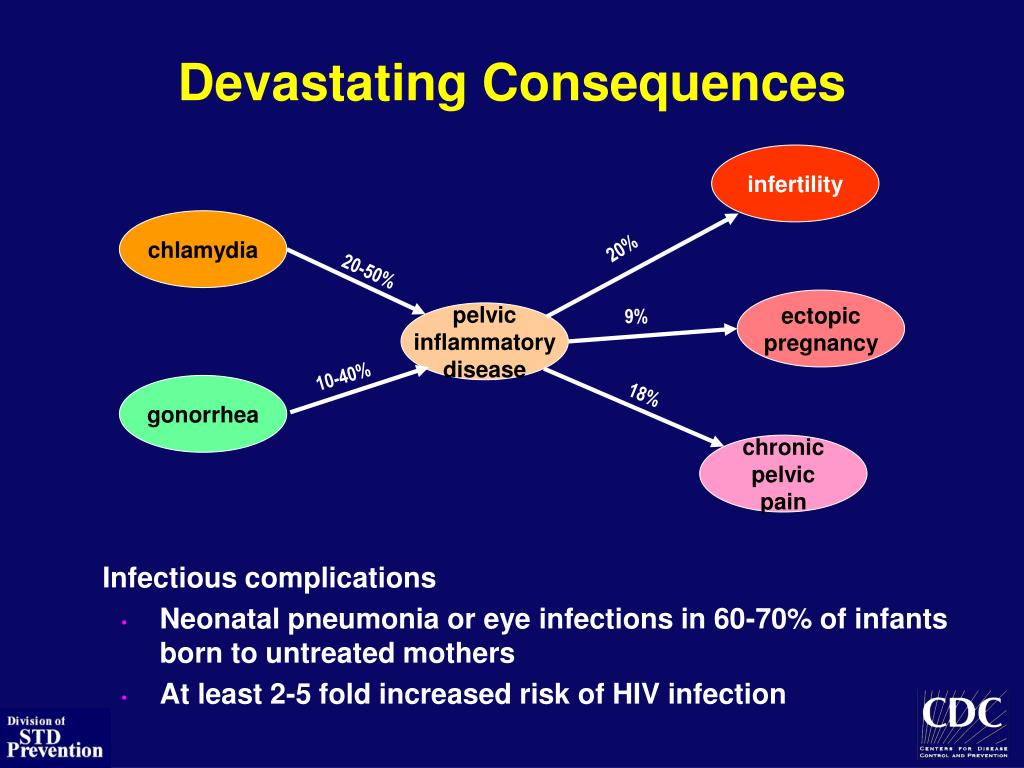 Your provider may do the test in an office, or they may ask you to do an at-home chlamydia test. Follow your provider’s instructions carefully to ensure you get accurate test results.
Your provider may do the test in an office, or they may ask you to do an at-home chlamydia test. Follow your provider’s instructions carefully to ensure you get accurate test results.
Because most chlamydia cases are asymptomatic, it’s important to get screened for chlamydia even if you don’t notice any signs of infection. The CDC recommends that sexually active cisgender women who are high-risk for chlamydia get screened regularly. Women, more so than men, experience the most severe complications from chlamydia. Transgender men and nonbinary individuals with vaginas should be screened regularly, too, as they can experience the same complications of chlamydia.
You’re considered high-risk if you:
- Are under 25.
- Are pregnant.
- Have a new partner.
- Have multiple partners.
- Have had chlamydia infections previously.
Cisgender men, or trans and nonbinary individuals with penises, should be screened for chlamydia if:
- They live in a setting where chlamydia spreads frequently, like correctional facilities, adolescent clinics and sexual health clinics.

- They have sex with other men.
Regardless of your age, reproductive anatomy, or other risk factors — you should discuss your sexual history and sexual activity with your healthcare provider. Your provider is your best resource for offering guidance on how often you should be tested for chlamydia and other STIs.
Management and Treatment
How is chlamydia treated?
Chlamydia can be cleared up with antibiotics in about a week or two. But don’t stop taking your medication just because your symptoms improve. Ask your provider about what follow-up is needed to be sure your infection is gone after you’ve finished taking your medicine.
Part of your treatment should also include avoiding sexual activities that could cause you to get re-infected and ensuring that any sexual partners who may be infected also get treatment. You should:
- Abstain from sex until your infection has cleared up. Starting treatment doesn’t mean that you’re in the clear.
 Take all your medication as your provider directs, and avoid all sexual contact in the meantime.
Take all your medication as your provider directs, and avoid all sexual contact in the meantime. - Contact all sexual partners. Tell any sexual partners from the last 3 months that you’re infected so that they can get tested, too.
- Get tested for other STIs (HIV/AIDS, syphilis, herpes, gonorrhea). It’s common to have multiple STIs, and it’s important to receive treatment that’s tailored to each infection.
Antibiotics can get rid of your infection, but they can’t reverse any harm the bacteria may have caused to your body before treatment. This is why it’s so important to get screened regularly for chlamydia, to see your provider at the first sign of symptoms, and get treatment immediately if you’re infected.
What medications are used to get rid of chlamydia?
The most common antibiotics used to treat chlamydia infections are:
- Azithromycin.
 Usually taken as a single dose.
Usually taken as a single dose. - Doxycycline. Usually taken over 7 days.
Make sure you only take antibiotics prescribed by your provider, and take all medications until they’re gone, even if your symptoms improve.
Can chlamydia be cured?
Yes. Chlamydia can be treated and cured. Some sexually transmitted bacterial infections are starting to become resistant to antibiotics, though, and this makes them harder to treat. With this in mind, the best way to fight chlamydia is to prevent infections from spreading.
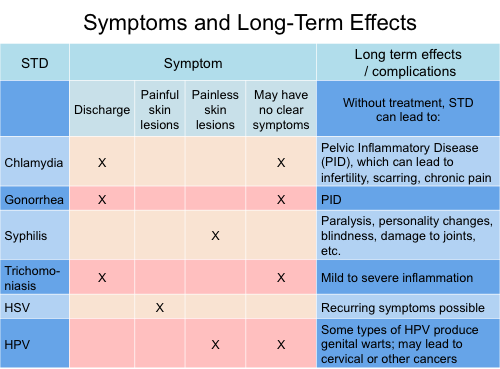
What can happen if chlamydia isn’t treated?
Untreated chlamydia can put your health at risk. Make an appointment with your provider immediately if you notice any symptoms of chlamydia, and get regular STI screenings to avoid complications later.
Complications of chlamydia for people with vaginas
Untreated chlamydia can cause:
- Pelvic inflammatory disease (PID). PID is a serious condition that requires hospitalization.
 It can occur when an untreated STI, like chlamydia, damages your reproductive organs. PID can lead to infertility and chronic pelvic pain. It can also cause an ectopic pregnancy, which is life-threatening for the fetus and potentially deadly for the mother or gestational parent, too.
It can occur when an untreated STI, like chlamydia, damages your reproductive organs. PID can lead to infertility and chronic pelvic pain. It can also cause an ectopic pregnancy, which is life-threatening for the fetus and potentially deadly for the mother or gestational parent, too. - Pregnancy complications. An untreated infection can lead to pre-term delivery. Also, if you’re pregnant and have chlamydia, you can pass the infection on to your newborn. Babies born with chlamydia may have pneumonia or conjunctivitis that could lead to blindness if not treated.
Complications of chlamydia for people with penises
Untreated chlamydia can cause:
- Epididymitis. Infection can spread to the testicles and the tube that carries sperm to your testicles (epididymis), causing symptoms like pain, swelling and tenderness in your testicles.
- Reduced fertility. Chlamydia can harm your sperm, negatively impacting your ability to conceive.
Complications of chlamydia that can affect all genders
Untreated chlamydia can:
- Increase your risk of getting reactive arthritis, which causes your joints to swell and feel painful.
- Increase your chances of contracting HIV.
How soon after treatment will I feel better?
You should start to feel better within a week after you begin taking antibiotics. Be sure to continue taking your antibiotics until they’re gone, even if your symptoms improve.
Prevention
How can I protect myself from chlamydia?
The only way to avoid getting chlamydia is to abstain from having vaginal, anal or oral sex with someone who has a chlamydia infection. And be sure that sex toys that carry the bacteria don’t come in contact with your genitals.
It’s not always possible to know if a current or potential partner has chlamydia, though, especially since many people with chlamydia never notice symptoms. With prevention in mind, it’s a good idea to make safer sex practices a regular part of your sex life:
- Use condoms during intercourse, anal sex and oral sex.
- Use dental dams during oral sex or vagina-to-vagina contact.
- Don’t share sex toys, but if you do, wash them after each use and cover toys used for penetration with a condom.
- Have sex with only one partner, who only has sex with you.
Outlook / Prognosis
How long does chlamydia last?
With treatment, chlamydia should go away within a week or two. It’s important to take all antibiotics to fight the infection. Don’t have sex during treatment, or you could get reinfected.
Does chlamydia go away on its own?
You should never wait for chlamydia to go away on its own. Left untreated, chlamydia can cause serious harm to your health. If you are sexually active, you run the risk of infecting others, putting them at risk of experiencing severe complications as well.
Living With
When should I see my healthcare provider?
When it comes to chlamydia, it’s a good idea to be proactive. Speak with your healthcare provider about your risks of infection.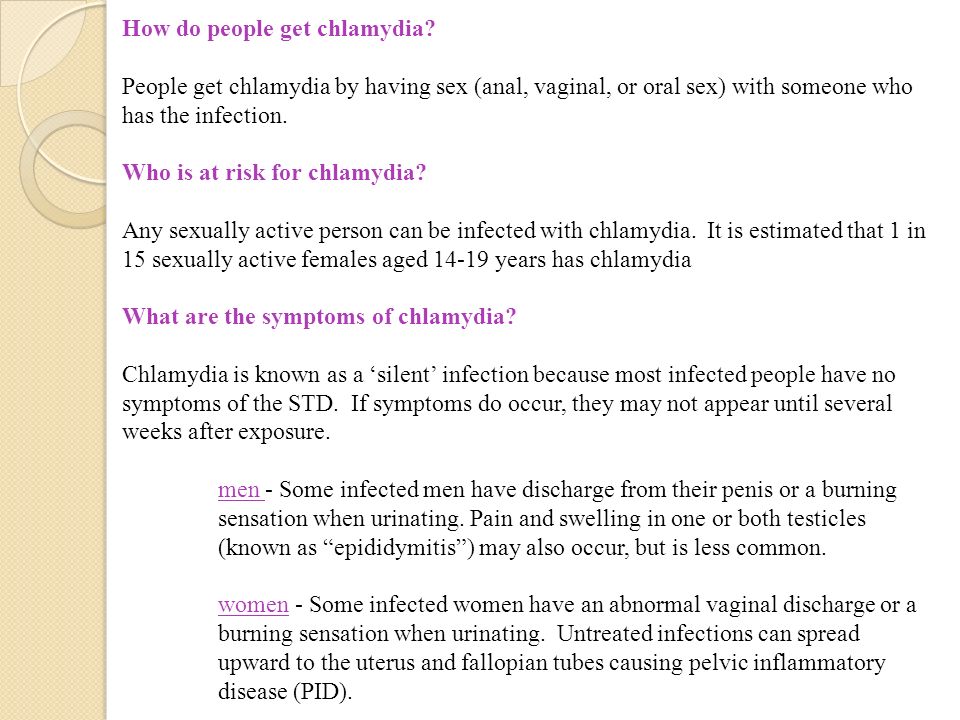 Make a plan to get screened regularly for STIs based on your provider’s recommendations for how often you should be tested. Make an appointment with your healthcare provider if your partner tests positive for chlamydia or if you notice any signs or symptoms that you may be infected.
Make a plan to get screened regularly for STIs based on your provider’s recommendations for how often you should be tested. Make an appointment with your healthcare provider if your partner tests positive for chlamydia or if you notice any signs or symptoms that you may be infected.
Frequently Asked Questions
What are the first symptoms of chlamydia?
Most people who have chlamydia never notice symptoms. But an unusual discharge from your vagina or penis may be a sign that you have a chlamydia infection. Pain, bleeding or a discharge from your bottom can also be a sign of chlamydia.
Does chlamydia have a smell?
Chlamydia doesn’t always have a smell. But one of the symptoms of chlamydia is an unusual vaginal discharge that has an unpleasant odor.
How did I get chlamydia if I didn’t cheat?
You can get chlamydia if your partner had vaginal, oral or anal sex with someone who was infected and then had sex with you. People in relationships may have different ideas about what kinds of sexual contact counts as “cheating,” and this miscommunication can lead to infections.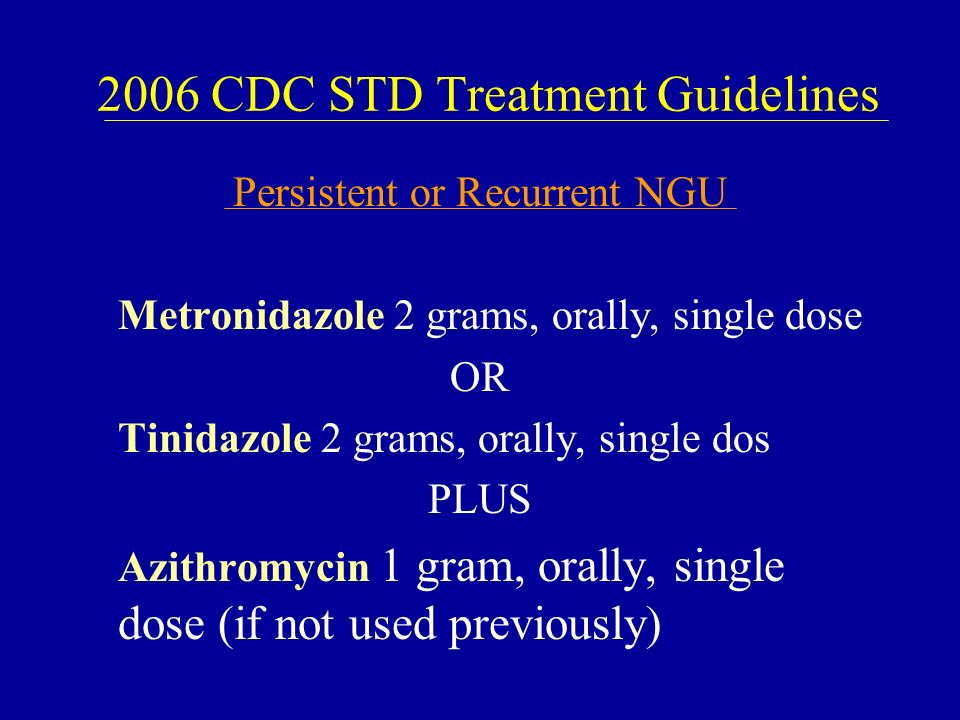 Communicate honestly with your partner about what sex you’re having and what sex they’re having. Practice safer sex to reduce your risk of catching chlamydia, and get regularly screened to be sure.
Communicate honestly with your partner about what sex you’re having and what sex they’re having. Practice safer sex to reduce your risk of catching chlamydia, and get regularly screened to be sure.
A note from Cleveland Clinic
It can be embarrassing to talk about anything sex-related with your healthcare provider, including STI prevention. But your sex life is an important part of your health that your provider needs to know about to care for you. Not getting the treatment you need for chlamydia can pose serious risks to your health. Speak with your provider about getting regularly screened for chlamydia and other STIs to reduce your risks of complications. Practice safer sex to prevent the spread of chlamydia.
Chlamydia - KVD №2
What is chlamydia?
Chlamydia is a common sexually transmitted infection (STI). The disease is caused by the bacterium Chlamydia trachomatis (Chlamydia trachomatis), which affects the female genital area and is the cause of non-gonococcal urethritis in men. Manifestations of chlamydia are usually minor or absent, but serious complications develop. Complications can cause irreparable damage to the body, including infertility - all this proceeds very secretly.
Manifestations of chlamydia are usually minor or absent, but serious complications develop. Complications can cause irreparable damage to the body, including infertility - all this proceeds very secretly.
Chlamydia also causes penile discharge in infected men.
Chlamydia transmission routes
Chlamydia can be transmitted through:
- vaginal or anal contact with an infected partner;
- less common with oral sex;
- use of sex toys with an infected partner;
- infection of a newborn during childbirth from a sick mother.
Absolutely all sexually active people can get chlamydia. The greater the number of sexual partners, the greater the risk of infection. The risk of infection is especially high in girls, because their cervix is not fully formed. About 75% of new cases occur in women under 25 years of age. By the age of 30, approximately 50% of sexually active women have had chlamydia. In sexually active men, the risk of infection is highest between the ages of 20 and 24.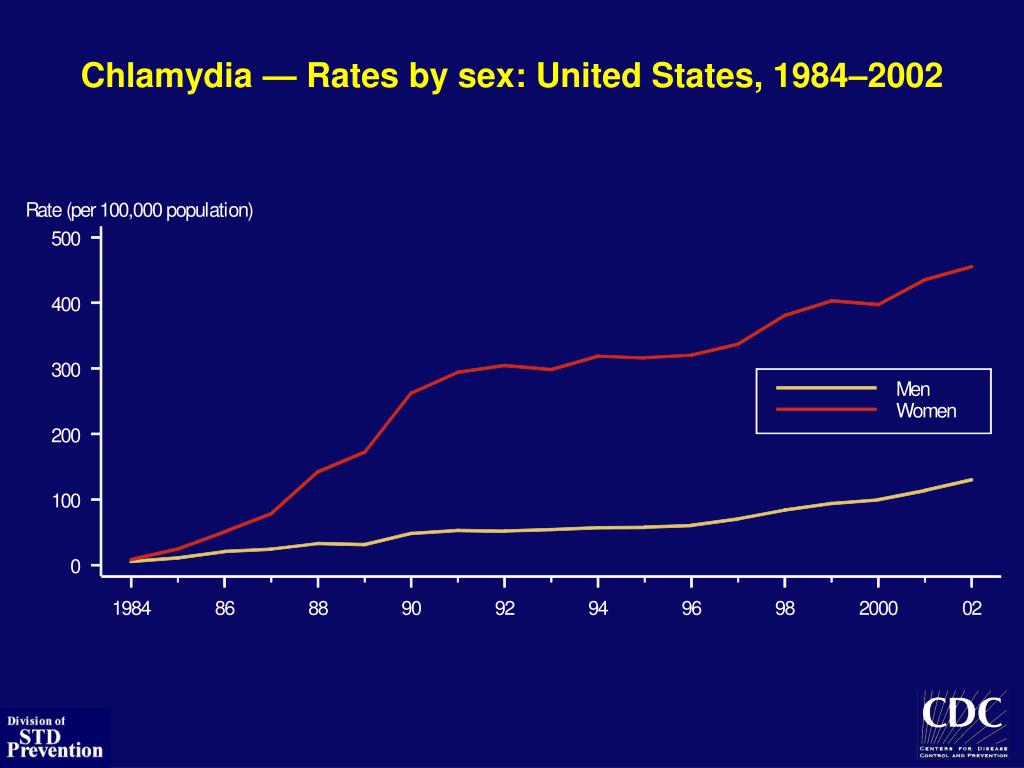
You cannot get chlamydia through kisses, hugs, dishes, baths, towels.
Manifestations of chlamydia
Chlamydia is very secretive. About 75% of infected women and 50% of infected men are asymptomatic. If manifestations of the disease develop, then this occurs approximately 1 to 3 weeks after infection.
In women, chlamydia first affects the cervix and urethra (urinary canal).
Manifestations:
- unusual vaginal discharge;
- pain or discomfort when urinating;
If the infection penetrates to the appendages, manifestations are possible:
- pain in the lower abdomen;
- pain in the lumbar region;
- nausea;
- slight increase in temperature;
- pain during intercourse or bleeding after it;
- bleeding between periods.
Symptoms in men:
- clear or cloudy discharge from the penis;
- pain or discomfort when urinating;
- there may be burning and itching in the area of the outlet of the urethra;
- rarely pain and/or swelling of the testicles.
Men or women who have anal sex with an infected partner can infect the rectum, resulting in inflammation, pain, discharge, or bleeding from the rectum.
Chlamydia can cause sore throat (pharyngitis) in men and women who have oral contact with an infected partner.
What complications can develop if chlamydia is not treated?
If the disease is not treated, serious short-term and persistent complications develop. Like the disease itself, complications often occur insidiously.
In women with untreated chlamydia, infection can spread from the urethra to the fallopian tubes (the tubes that carry the egg from the ovaries to the uterus) - this causes (in 40% of cases) the development of pelvic inflammatory disease (PID). PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID.
Women with chlamydia are more susceptible to HIV infection, the risk increases by almost 5 times.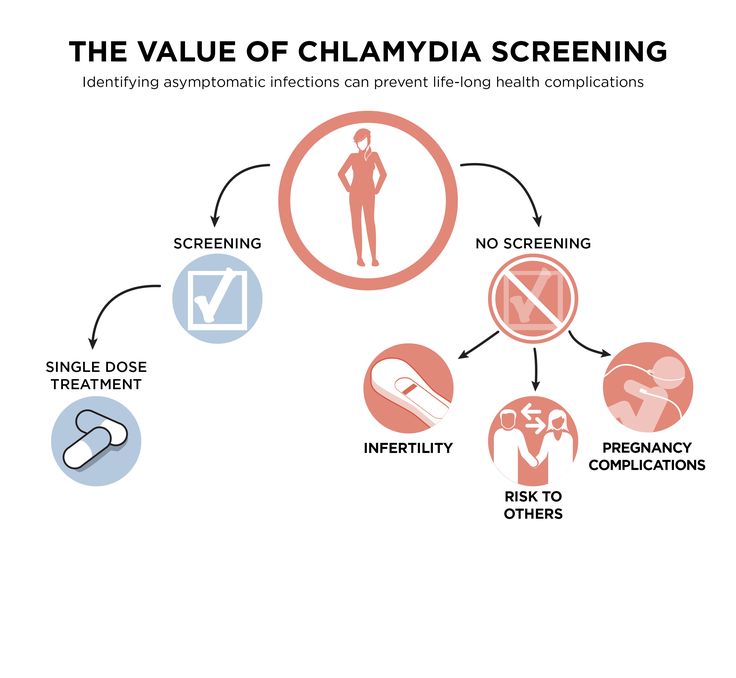
To prevent serious consequences of chlamydia, annual chlamydia screening is required for all sexually active women 25 years of age and younger. An annual examination is necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Complications of chlamydia are rare in men. The infection sometimes extends to the epididymis and causes pain, fever, and, rarely, male infertility (sterility).
Rarely, chlamydial infection can cause inflammation of the joints in combination with skin lesions, inflammation of the eyes and urinary tract - this is the so-called Reiter's syndrome.
The effect of chlamydia on a pregnant woman and her child
Chlamydia in pregnant women increases the risk of miscarriage, premature detachment of the placenta. Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn.
Diagnosis of chlamydia
Diagnosis includes observation of the patient's clinical symptoms, testing for chlamydia smears from the cervix, scraping from the urinary canal, the first morning urine.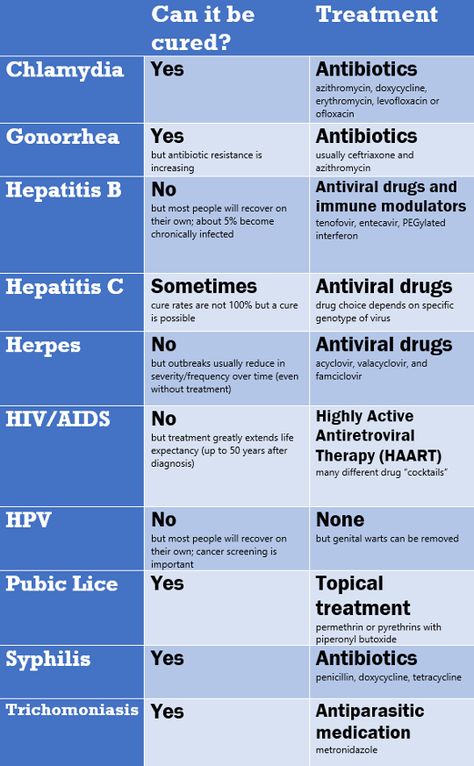 Most often, the study is carried out by PCR (polymerase chain reaction). Swabs and scrapings may cause minor discomfort.
Most often, the study is carried out by PCR (polymerase chain reaction). Swabs and scrapings may cause minor discomfort.
In addition, a blood test by ELISA (enzyme-linked immunosorbent assay) for the presence of immunity to chlamydia is carried out, this auxiliary test often helps to establish an accurate diagnosis.
Treatment of chlamydia
Treatment of chlamydia is with oral antibiotics. To prevent re-infection, all sexual partners must be found, examined and treated. Patients with chlamydia should refrain from unprotected sex during treatment, otherwise it is possible to re-infect the sexual partner. Unfortunately, after successful treatment, re-infection with chlamydia is possible, since a strong immunity to this microorganism does not develop. Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment.
Prevention of chlamydia
The best way to prevent sexually transmitted infections is through long-term sexual contact with one healthy sexual partner.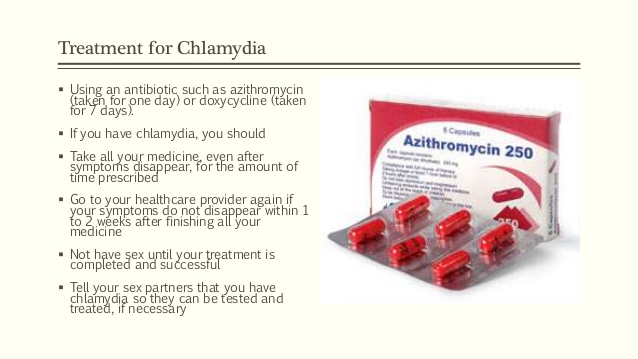 Latex male condoms, when used correctly, drastically reduce the risk of transmission.
Latex male condoms, when used correctly, drastically reduce the risk of transmission.
Annual chlamydia screening required for all sexually active women 25 years of age and younger. An annual examination is also necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Any manifestations, such as pain or discomfort when urinating, unusual rash, discharge are a signal to stop sexual intercourse and immediately examine in a specialized clinic - KVD. If the patient is found to have chlamydia (or any other STI), he must inform his sexual partners so that they also undergo a full examination and appropriate treatment. This will reduce the risk of developing serious complications and prevent the possibility of re-infection.
Patients with chlamydia should refrain from unprotected sex during treatment, otherwise the sexual partner may be re-infected.
Questions about chlamydia: page 2
Is it possible to get chlamydia in the household? What drugs are effective in the treatment of ureaplasmosis and mycoplasmosis? Can chlamydia be treated during pregnancy? Doctors of medical clinics "Art-Med" answer questions about diseases: chlamydia, ureaplasmosis and mycoplasmosis.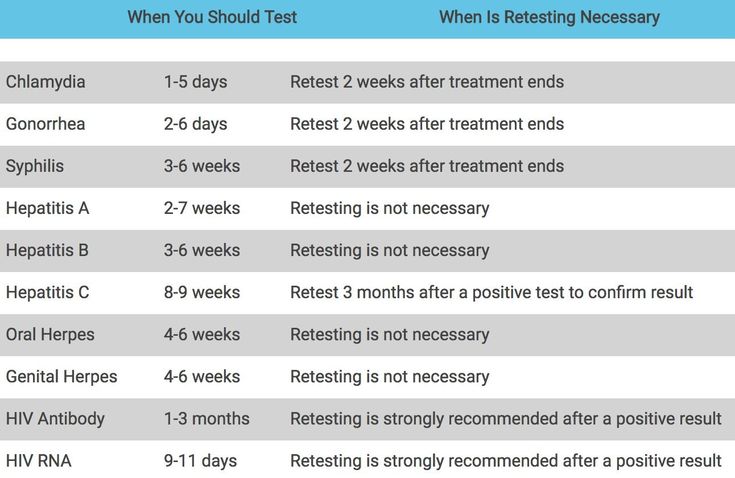
Ask a Question
My husband was prescribed antibiotics ciprofloxacin for 10 days, 2 times a day. Do these antibiotics treat chlamydia?
Chlamydiae are usually sensitive to ciprofloxacin, so this drug can be used in the treatment of chlamydial infections.
Chlamydia was found in my girlfriend's blood. So I have too. I want to work in Russia. To obtain a work permit in Russia, I have to pass tests, I read that they will not give permission if a person has venereal lymphogranuloma (Chlamydia urogenital). Chlamydia and Chlamydia urogenital the same disease? If not, will I be allowed to work with chlamydia?
Lymphogranuloma venereum, although caused by chlamydia, is of a different serotype. Urogenital chlamydia cannot spoil your career in Russia.
My husband and I were tested (smears), he was diagnosed with chlamydia, and I have mycoplasmosis. Why do we have different diagnoses?
Why do we have different diagnoses?
In this situation, incomplete sampling of the material, laboratory error, and peculiarities of the immune status are possible. To clarify the situation, it is worth repeating the study, and it is better by sowing.
My husband and I are undergoing treatment for chlamydia, when should I get tested? Immediately after treatment or later? And when can you make a PA?
You can have sex with a condom after your treatment is over. It is worth taking an analysis no earlier than 3 weeks after the end of antibiotic therapy.
I passed tests for the number of ureaplasmosis, high results came. My husband did not take tests, but both of us were prescribed treatment with Wilprofen and Trichopolum and Klion suppositories. During the treatment, we had sex in a condom. After treatment, a month later, you need to repeat the tests. Do you use condoms now after treatment and before retests, or can you already refuse them?
Use condoms until you get negative results after treatment.
I did a ureaplasma culture and the results of the analysis revealed that I have sensitivity to only one antibiotic. The doctor prescribed ofloxacin tablets (sensitivity to it) and clindamycin suppositories (resistance to them). Should I use these candles, because I'm afraid that they can only get worse?
Not worth it.
The essence of the problem is as follows: recently my wife had a miscarriage, she decided to take tests, and as a result, sowing on mycoplasma and ureaplasma gave growth. Sensitivity to antibiotics is also very individual: Azithromycin -R; Dioxycycline-R; Ofloxacin -I; Tetracycline-R; Josamycin -R; Clindamycin-R; Pristamycin -R; Erythromycin-R. How to treat this disease now? And along the way, can I take antibiotics without passing the test, if so, which ones and in what dosage?
Your spouse's microbes are only moderately sensitive to ofloxacin. Therefore, you can be treated (it is possible without a preliminary additional examination), and you need this drug. Treatment regimens are discussed only at the reception.
Treatment regimens are discussed only at the reception.
I was diagnosed with chlamydia by PCR, prescribed treatment with doxycycline 1 capsule 2 times a day for 14 days, suppositories Genferon 1 million. rectally 1 time per day for 10 days, Neo-Penotran suppositories vaginally 7 days at night, how effective is this treatment? I went to my gynecologist and suggested treatment Azithromycin 1g - 1 time + suppositories Genferon 1 million. vaginal 10 days once a day, which treatment is most effective? Confused by a single dose of an antibiotic, as I read that chlamydia develops in 72 hours and it is necessary to catch all its stages of development. When is the best time to check for chlamydia after treatment? What day of the monthly cycle?
Both regimens have a right to exist. The control analysis should be taken after 3 weeks and 3 months after the end of therapy. It is better to do this immediately after the end of menstruation.
I would like to ask if ureaplasmosis should be treated? Some doctors say that it’s not necessary, that it’s just urogenital dysbacteriosis, others say that it’s necessary, because it can lead to consequences, I was treated and on an ultrasound they told me that something incomprehensible was going on with my bladder, then whether some disease caused by ureaplasmosis or is it from inflammation (cervicitis).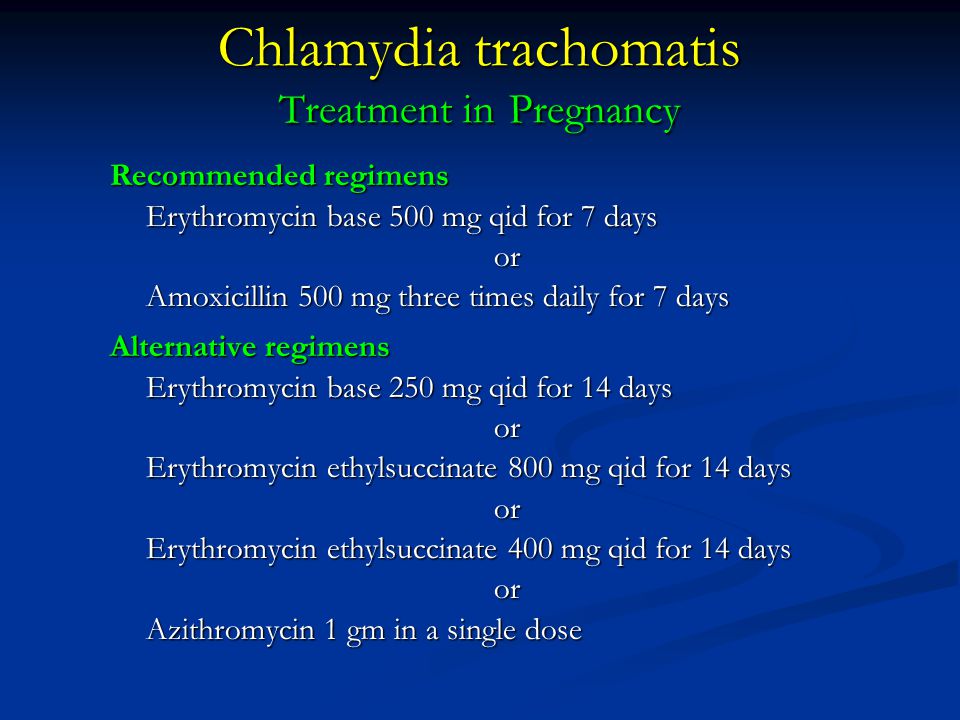 Could it be?
Could it be?
To clarify the need for treatment, it is worth taking a culture for ureaplasma. Read more about this infection in the "Medical Publications" section.
My husband and I were treated for infections a year ago. The analysis was not repeated. I still had doubts that I had not recovered, because some of the symptoms did not go away. A year later, my husband had discharge, is it possible to re-infect in a year? How can this be?
Perhaps one of the partners did not recover and became the cause of family infection. Without knowing the situation, it is also impossible to exclude infection "from outside" or the appearance of a disease that is not directly related to the infection. In any case, a comprehensive examination is necessary.
My sexual partner and I were diagnosed with mycoplasmosis, ureaplasmosis and gardnerella, what could cause them if before our first sexual intercourse they were tested and both of them were positive? After our general treatment, is it possible that the infections can resume their action?
In this situation, it is worth clarifying in what quantity these microorganisms are determined, whether treatment is necessary.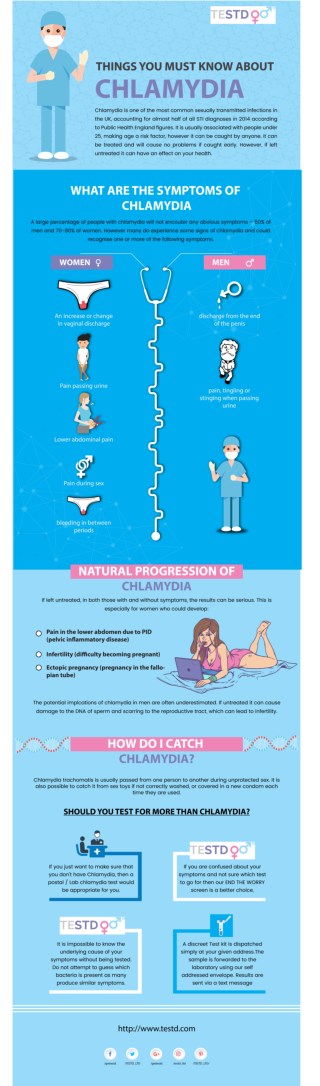 Submit a culture for mycoplasma and ureaplasma, as well as bacterial culture from the vagina. Read more about this in the Medical Publications section.
Submit a culture for mycoplasma and ureaplasma, as well as bacterial culture from the vagina. Read more about this in the Medical Publications section.
2 months after giving birth, she took tests and the smear was normal, after sexual contact with her husband, she took a smear again and bacteria were found, the doctor said that she was suspected of chlamydia, ureaplasmosis, mycoplasmosis. Before pregnancy, I took all the tests and nothing was found. In this regard, I have 2 questions: could I infect the child if I put terginon suppositories 10 days before the birth and in what cases can it be that nothing was found in the smear before pregnancy, and after the birth the infection was found?
To begin with, I recommend that you undergo an examination to confirm or refute the doctor's assumption. And after receiving the results, it will be possible to answer your questions.
PCR diagnostics revealed chlomidia and genital mycoplasmas.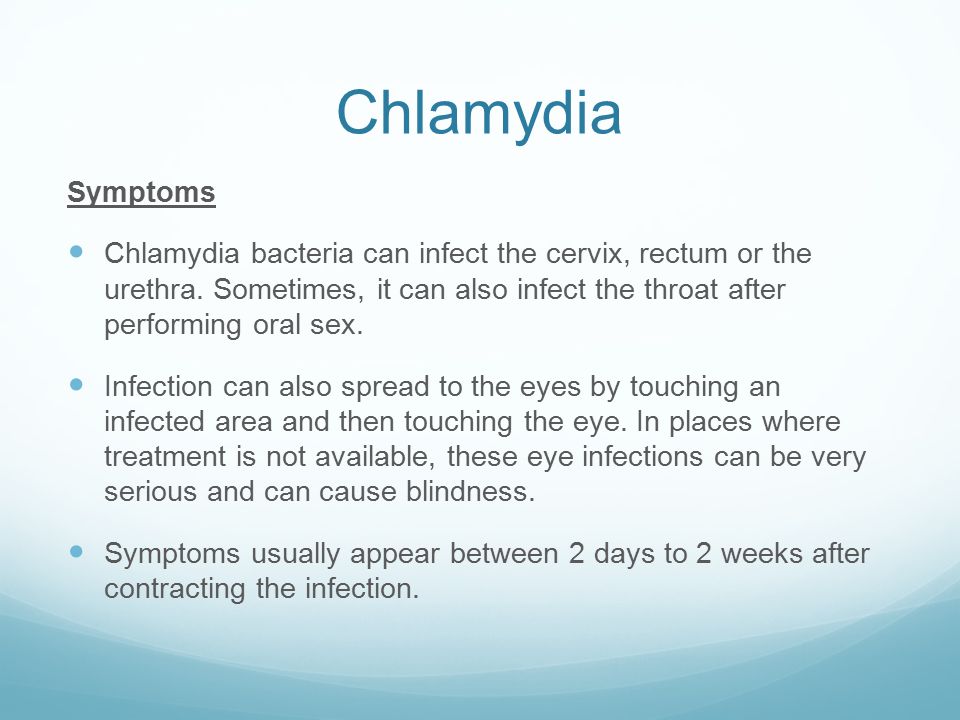 The day before the start of treatment, unprotected intercourse occurred. As a result, pregnancy. Now 3-4 weeks pregnant. What effect could be on the fetus? She took wilprofen, vagid suppositories, viferon, eco-femin, fluconazole, vitamins.
The day before the start of treatment, unprotected intercourse occurred. As a result, pregnancy. Now 3-4 weeks pregnant. What effect could be on the fetus? She took wilprofen, vagid suppositories, viferon, eco-femin, fluconazole, vitamins.
You have an increased risk of fetal death and miscarriage up to 8 weeks. After this period, the risk will be the same as for everyone.
Ureplasmosis was diagnosed. I am pregnant, 31st week. The doctor prescribed medication for a course of 10 days and a control smear in three weeks. Is it possible to have sex after the course (10 days), but before passing the control smear?
Yes, you can, but with a condom.
Chlamydia was diagnosed in my partner, treatment was prescribed, my analysis showed a negative result, but the analysis for the flora and, subsequently, ultrasound revealed prostatitis. The doctor prescribed me vilprafen 500 mg 3 times a day for 14 days, suppositories imunofan for 10 days and Miramixin spray. Then he said that this is a 100% guarantee of a cure and that it is not even necessary to take tests. Is this true and how long after the completion of treatment is it possible to have sexual intercourse with the same partner?
Then he said that this is a 100% guarantee of a cure and that it is not even necessary to take tests. Is this true and how long after the completion of treatment is it possible to have sexual intercourse with the same partner?
It's still worth taking tests. Sex is possible after the end of the course of antibiotic therapy. But unprotected sex is recommended only after receiving negative results after treatment.
My husband was diagnosed with mycoplasmosis, but I am not, although I passed the tests 2 times in two different laboratories. How is this possible? Do I need preventive treatment?
Did the husband take a culture for mycoplasma? If not, then it is worth doing, it is possible that this microbe is detected in a small amount, insufficient for infection.
After a miscarriage last year, I was diagnosed with chlamydia. Treatment with viferon 2, macmiror, trichopolum, rovamycin and nystatin was prescribed.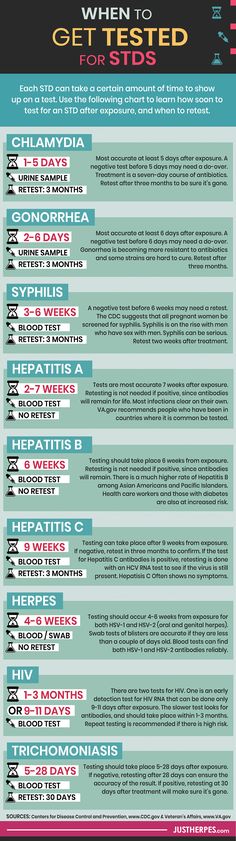 Perhaps for 1 course of treatment will be cured by these drugs? When should treatment be started (before or during menstruation)? How soon after treatment should I take tests again and start planning a pregnancy?
Perhaps for 1 course of treatment will be cured by these drugs? When should treatment be started (before or during menstruation)? How soon after treatment should I take tests again and start planning a pregnancy?
Treatment is best started during menstruation. Control tests should be taken no earlier than 2 weeks after the end of therapy. You should also exclude other causes of miscarriage, after which it will be possible to talk about the timing of its planning. Read more about this in the Medical Publications section.
Six months ago, I was diagnosed with chlamydia, and none of the sampling methods (neither PCR, nor blood) revealed this disease in my husband. I went through a course of treatment, he did not. Did he need to undergo treatment with me?
If he does not have an infection, then there is nothing to treat.
I was diagnosed with ureaplasmosis and candidiasis against its background, antibiotics were prescribed, and then immuno-restorative drugs. When do you start taking the latest? And how long after the course of treatment should I go for retests?
When do you start taking the latest? And how long after the course of treatment should I go for retests?
The treatment regimen should be discussed with the treating doctor. Control tests are taken no earlier than 2 weeks after the end of antibiotic therapy.
Passed tests, they found ureaplasma urealyticum, gardnerella vag, candida spp. They prescribed the treatment of mulimen, sumamed, lamicon and terzhinan. The partner was advised to drink lamicone for 10 days and sumamed, although he has no symptoms. Is it necessary?
Your partner should be examined and then treated appropriately.
My young man has an advanced form of mycoplasmosis and chlamydia, the doctor prescribed treatment, do I need to see a doctor or can I be treated with the same drugs as prescribed for him or pass control tests?
You'd better come to a gynecologist, undergo an examination and choose an adequate treatment, and only then take control tests.
I was diagnosed with ureaplasmosis and chlamydia, before I found out that I had an infection, had unprotected intercourse on the last day of my period, what is the probability that I infected my partner, does the probability of infecting during my period decrease or increase? And correctly, I was prescribed a treatment regimen, 10 days of Viferon suppository at night in the rectum, 20 days of Unidox salute 1-2 times a day and Miko-Max 1 rev on the 7th, 14th, 21st and 28th day of treatment.
The prescribed treatment regimen has the right to exist. Your sexual partner should also be treated. Read more about these infections in the Medical Publications section.
Passed PCR for chlamydia, ureaplasma, mycoplasma. Ureaplasma was found. Do I need to be further examined for CMV or is there an antibiotic that is suitable, if necessary, for treatment in both cases. 5 years ago, before pregnancy, she was checked for the entire TORCH - complex, nothing was found.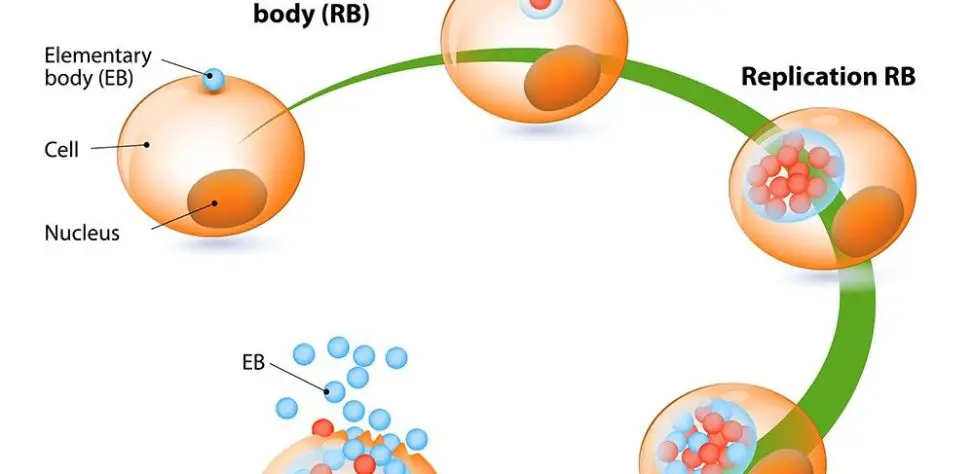 But for some reason, ureaplasma has now appeared in the analysis, although it does not cause me any anxiety.
But for some reason, ureaplasma has now appeared in the analysis, although it does not cause me any anxiety.
In this situation, in order to clarify the need for treatment and select adequate therapy, I recommend taking a culture for ureaplasma. CMV is not sensitive to antibiotics.
ELISA showed mycoplasma lg A, ureaplasma was negative. PCR showed ureaplasma, mycoplasma was negative. What does it mean? This is mistake?
To clarify the situation, I recommend taking a culture for mycoplasma and retake a blood test for the presence of antibodies to it.
Is it possible to cure male infertility after mycoplasmosis?
It depends on the cause of infertility. Mycoplasmosis does not really affect this problem.
I was prescribed the antibiotic rifampicin for the treatment of ureaplasma (before that, I had already taken several courses of treatment with other drugs - to no avail). The annotation for this antibiotic does not indicate that it acts on ureaplasma. Is the appointment of rifampicin justified in this case?
The annotation for this antibiotic does not indicate that it acts on ureaplasma. Is the appointment of rifampicin justified in this case?
In this situation, it would be advisable to do a ureaplasma culture to determine which antibiotics your ureaplasma is sensitive to.
I was diagnosed with ureaplasmosis and after 30 days of treatment I need to do a second analysis. 30 days after the start of treatment or after the end?
After graduation.
My young man was diagnosed with "Ureaplasmosis" and prescribed medication. I also passed the necessary tests, they also found ureaplasma in me. Then I made a tank. analysis, which showed a titer of 10 * 2 CFU. The doctor did not prescribe treatment, he said that with such an indicator, treatment is not required. The rest of the tests are normal, there are no unpleasant sensations in the vagina, there are no discharges either. Can a young person get this disease from me and what should I do to prevent it?
Ureaplasma infection requires a fairly large number of microbes.