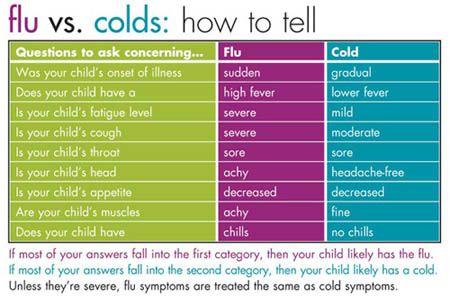
How high fever in child
Fevers (for Parents) - Nemours KidsHealth
All kids get a fever from time to time. Usually, a fever isn’t dangerous or bad for kids. It can even be a good thing because it can help the immune system fight infection.
Still, parents might be unsure about how to handle a fever at home and when to call the doctor. Here are some tips.
What Is a Fever?
In general, a fever means the body’s temperature is 100.4°F (38°C) or higher. Different ways of measuring a temperature — rectal, armpit, ear, forehead, mouth — get a slightly different number, so the number that means a child has a fever is a little different too.
What Causes Fevers?
Fevers in kids are usually caused by an infection. A fever helps the body by stimulating the immune system to fight the infection. Doctors also think the higher temperature makes it harder for the germs to grow.
A few other reasons kids can have a fever:
Overdressing: Infants, especially newborns, may get fevers if they're overdressed, wrapped in a blanket, or in a hot environment because they don't regulate their body temperature as well as older kids. But because fevers in newborns can be a sign of a serious infection, even infants who are overdressed must be checked by a doctor if they have a fever.
Immunizations: Babies and kids sometimes get a mild fever that lasts about a day after getting vaccinated.
A child who is teething might have a slight rise in body temperature, but it's probably not the cause if the temperature is higher than 100°F (37.8°C).
When Is a Fever a Sign of Something Serious?
In most healthy kids who are acting well, a fever isn’t serious.
But a fever can be serious for:
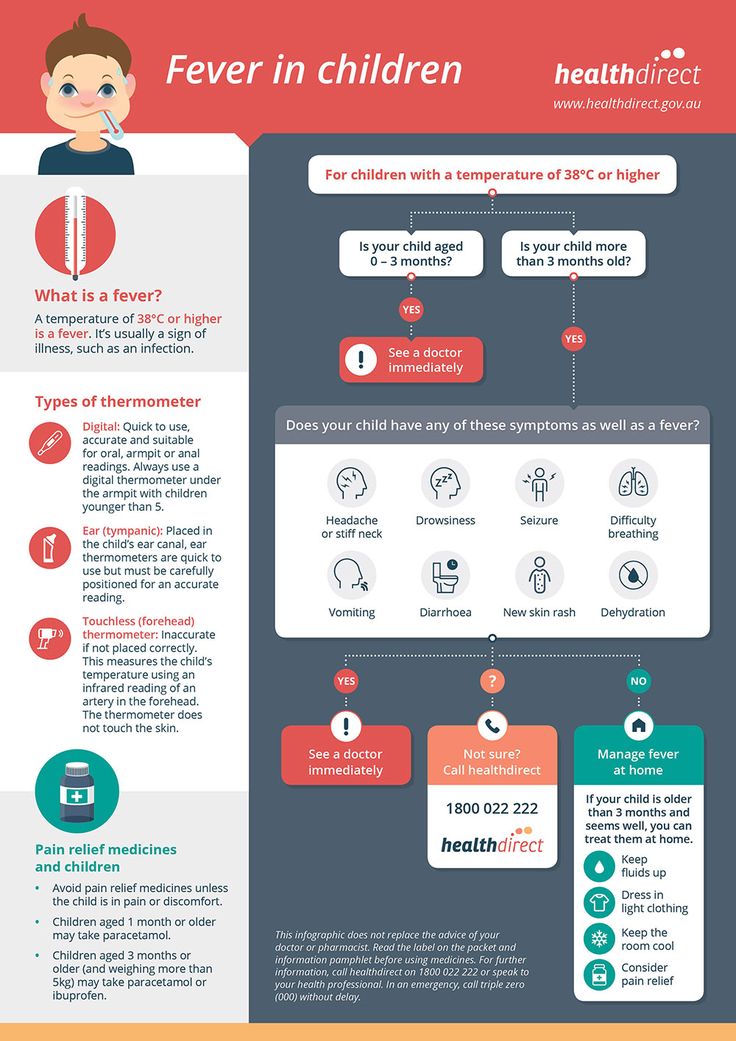
- Infants younger than 3 months: If an infant younger than 3 months has a rectal temperature of 100.4°F (38°C) or higher, call your doctor or go to the emergency department right away.
- Kids with some health conditions: If your child has an ongoing health issue, make sure you know if the doctor should be called for fever.
A fever is probably not serious if your child is 3 months or older and:
- is still interested in playing
- is drinking well
- is alert and smiling
- has a normal skin color
- looks well when their temperature comes down
Don't worry too much about a child with a fever who doesn't want to eat. This is common with infections that cause fever. For kids who still drink and urinate (pee) normally, not eating as much as usual is OK.
This is common with infections that cause fever. For kids who still drink and urinate (pee) normally, not eating as much as usual is OK.
What Are the Signs of a Fever?
Kids with a fever might:
- feel warm
- act differently (they might be fussy or cranky, or quieter than usual)
- breathe a little faster or have a faster heart rate than normal
- have a headache
- have chills or sweating
- have red or flushed skin
For any of these signs, take your child’s temperature to know if they really have a fever.
If your child feels warm or is acting unwell, use a digital thermometer to confirm a fever. Different ways of taking the temperature are more accurate than others at measuring the true body temperature.
The best way to take a temperature:
- for kids 3 years old and younger: a rectal temperature
- for kids 4 or older who can cooperate: an oral temperature (by mouth)
- for any age: under the armpit (axillary) and temporal artery (forehead) are easiest but less accurate.
 Tympanic (in the ear) is OK for kids 6 months and older.
Tympanic (in the ear) is OK for kids 6 months and older.
It's a fever when a child's temperature is at or above one of these levels:
- rectal (in the bottom), tympanic (in the ear), or temporal artery (across the forehead): 100.4°F (38°C)
- oral (in the mouth): 100°F (37.8°C)
- axillary (under the arm): 99°F (37.2°C)
How Can I Help My Child Feel Better?
No treatment is needed if a child is still playing and drinking normally and doesn’t have pain.
Treating a fever with medicine isn't needed if a child is still playing and drinking normally and doesn’t have pain. Give medicine only when a fever causes a child discomfort or keeps them from drinking.
While kids have a fever, keep an eye on them, help them to rest, and keep offering fluids to drink. They need to drink a little extra to make up for the fluids they lose from sweating.
Home Care Measures
Medicines
If your child is uncomfortable from a fever or not drinking fluids well, you can give one of these medicines:
- acetaminophen (such as Tylenol or a store brand)
or - ibuprofen (such as Advil, Motrin, or a store brand).
 Do not give to children under 6 months old.
Do not give to children under 6 months old.
Follow the package directions for how much to give and how often. If you don't know the recommended dose or your child is younger than 2 years old, call the doctor to find out what to use and how much to give.
- If your child has any medical problems, check with the doctor to see which medicine to use.
- Unless instructed to by a doctor, never give aspirin to a child. Such use is linked to Reye syndrome, a rare but serious illness.
Do not give any medicine for fever to infants younger than 3 months old unless instructed to by a doctor.
Staying ComfortableIf your child has a fever:
- Have them wear lightweight clothing and stay covered with a light sheet or blanket. Heavy clothes and blankets can keep the body from cooling, which can make your child uncomfortable.
- Keep the room at a comfortable temperature — not too hot or too cold.

- Make sure they get plenty of rest. Staying in bed all day isn't necessary, but a sick child should take it easy.
- They should stay home from school or childcare until their temperature has been normal for 24 hours.
Lukewarm sponge baths to lower a fever generally are not recommended. In fact, sponge baths can make kids uncomfortable from shivering. Never use rubbing alcohol (it can cause poisoning when absorbed through the skin) or ice packs/cold baths (they can cause chills that can raise body temperature).
Food and DrinksOffer plenty of fluids to avoid dehydration because fevers make kids lose fluids faster than usual. Oral rehydration solutions (like Pedialyle, Enfalyte, or store brands) are a good choice. You also can give water, soup, ice pops, and flavored gelatin. Avoid drinks with caffeine, including colas and tea, which can make dehydration worse by making kids pee more often.
Let kids eat what they want (in reasonable amounts), but don't force it if they don't feel like eating much.
When Should I Call the Doctor?
The temperature that should trigger a call to the doctor depends on a child's age, the illness, and whether they have other symptoms. You might ask if your doctor has specific guidelines on when to call about a fever.
In general, call the doctor if your child is:
- younger than 3 months old with a rectal temperature of 100.4°F (38°C) or higher
- 3 months or older with a temperature higher than 102.2°F (39°C)
- any age but has a health problem like cancer or sickle cell disease and has a fever
Also call if a child 3 months or older has a fever and:
- refuses fluids or seems too ill to drink enough
- has lasting diarrhea or repeated vomiting
- has any signs of dehydration (peeing less than usual, not having tears when crying, less alert and less active than usual)
- has a specific complaint (like a sore throat or earache)
- still has a fever after 2–3 days
- has a rash
- has pain while peeing
Get emergency care if your child shows any of these signs:
- crying that won't stop
- extreme irritability or fussiness
- sluggishness and trouble waking up
- a rash or purple spots that look like bruises on the skin (that were not there before your child got sick)
- blue lips, tongue, or nails
- in an infant, the soft spot on the head seems to be bulging out or sunken in
- stiff neck
- severe headache
- limpness or refusal to move
- trouble breathing that doesn't get better when the nose is cleared
- leaning forward and drooling
- seizure
- moderate to severe belly pain
What Else Should I Know?
All kids get fevers, and in most cases they're back to normal within a few days.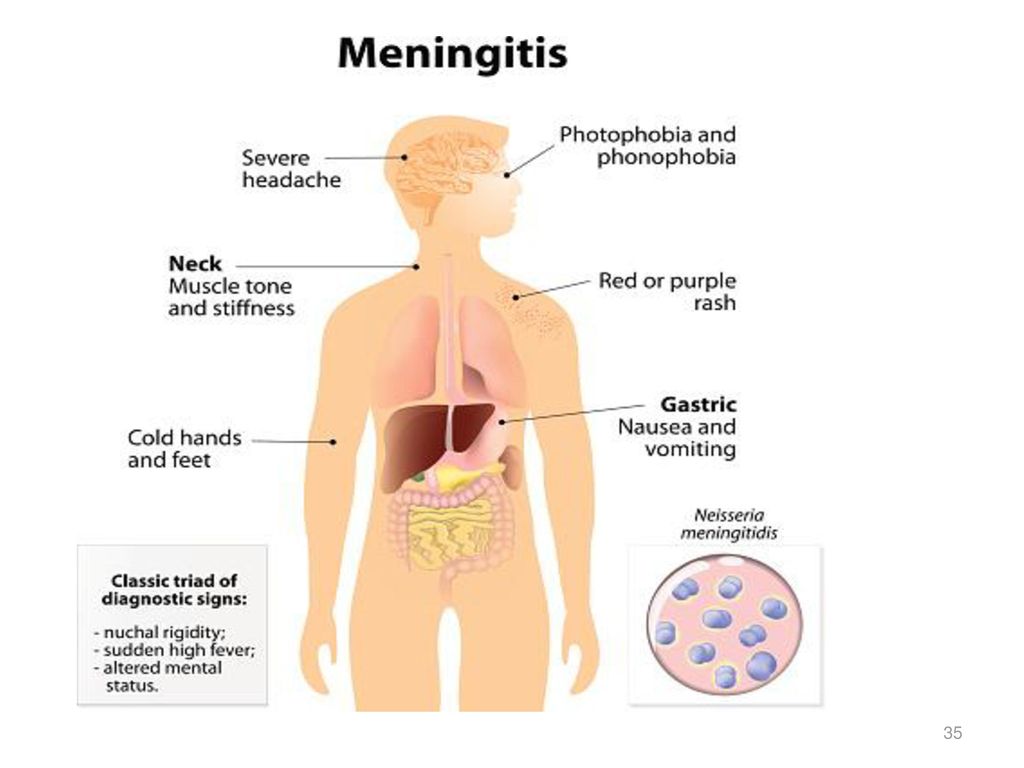 For older babies and kids, the way they act can be more important than the reading on your thermometer. Everyone gets a little cranky when they have a fever. This is normal and should be expected.
For older babies and kids, the way they act can be more important than the reading on your thermometer. Everyone gets a little cranky when they have a fever. This is normal and should be expected.
But if you're ever in doubt about what to do or what a fever might mean, or if your child is acting ill in a way that concerns you even with no fever, always call your doctor for advice.
Reviewed by: Melanie L. Pitone, MD
Date reviewed: November 2022
Fever - Myths Versus Facts
Many parents have false beliefs (myths) about fever. They think fever will hurt their child. They worry and lose sleep when their child has a fever. This is called fever phobia. In fact, fevers are harmless and often helpful. Let these facts help you better understand fever.
MYTH. My child feels warm, so she has a fever.
FACT. Children can feel warm for a many reasons. Examples are playing hard, crying, getting out of a warm bed or hot weather. They are "giving off heat." Their skin temperature should return to normal in about 20 minutes. About 80% of children who act sick and feel warm do have a fever. If you want to be sure, take the temperature. These are the cutoffs for fever using different types of thermometers:
They are "giving off heat." Their skin temperature should return to normal in about 20 minutes. About 80% of children who act sick and feel warm do have a fever. If you want to be sure, take the temperature. These are the cutoffs for fever using different types of thermometers:
- Rectal (bottom), ear or forehead temperature: 100.4° F (38.0° C) or higher
- Oral (mouth) temperature: 100° F (37.8° C) or higher
- Under the arm (Armpit) temperature: 99° F (37.2° C) or higher
MYTH. All fevers are bad for children.
FACT. Fevers turn on the body's immune system. They help the body fight infection. Normal fevers between 100° and 104° F (37.8° - 40° C) are good for sick children.
MYTH. Fevers above 104° F (40° C) are dangerous. They can cause brain damage.
FACT. Fevers with infections don't cause brain damage. Only temperatures above 108° F (42° C) can cause brain damage. It's very rare for the body temperature to climb this high. It only happens if the air temperature is very high. An example is a child left in a closed car during hot weather.
It's very rare for the body temperature to climb this high. It only happens if the air temperature is very high. An example is a child left in a closed car during hot weather.
MYTH. Anyone can have a seizure triggered by fever.
FACT. Only 4% of children can have a seizure with fever.
MYTH. Seizures with fever are harmful.
FACT. These seizures are scary to watch, but they stop within 5 minutes. They don't cause any permanent harm. They don't increase the risk for speech delays, learning problems, or seizures without fever.
MYTH. All fevers need to be treated with fever medicine.
FACT. Fevers only need to be treated if they cause discomfort (makes your child feel bad). Most fevers don't cause discomfort until they go above 102° or 103° F (39° or 39.5° C).
MYTH. Without treatment, fevers will keep going higher.
FACT. Wrong, because the brain knows when the body is too hot. Most fevers from infection don't go above 103° or 104° F (39.5°- 40° C). They rarely go to 105° or 106° F (40.6° or 41.1° C). While these are "high" fevers, they also are harmless ones.
MYTH. With treatment, fevers should come down to normal.
FACT. With treatment, most fevers come down 2° or 3° F (1° or 1.5° C).
MYTH. If you can't "break the fever", the cause is serious.
FACT. Fevers that don't come down to normal can be caused by viruses or bacteria. The response to fever medicines tells us nothing about the cause of the infection.
MYTH. Once the fever comes down with medicines, it should stay down.
FACT. It's normal for fevers with most viral infections to last for 2 or 3 days. When the fever medicine wears off, the fever will come back. It may need to be treated again. The fever will go away and not return once the body overpowers the virus. Most often, this is day 3 or 4.
It may need to be treated again. The fever will go away and not return once the body overpowers the virus. Most often, this is day 3 or 4.
MYTH. If the fever is high, the cause is serious.
FACT. If the fever is high, the cause may or may not be serious. If your child looks very sick, the cause is more likely to be serious.
MYTH. The exact number of the temperature is very important.
FACT. How your child looks and acts is what's important. The exact temperature number is not.
MYTH. Oral temperatures between 98.7° and 100° F (37.1° to 37.8° C) are low-grade fevers.
FACT. These temperatures are normal. The body's normal temperature changes throughout the day. It peaks in the late afternoon and evening. A true low-grade fever is 100° F to 102° F (37.8° - 39° C) .
SUMMARY. Keep in mind that fever is fighting off your child's infection. Fever is one of the good guys.
Fever is one of the good guys.
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Last Reviewed: 12/21/2022
Last Revised: 01/13/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Normal values of body temperature in children, measurement of the child's body temperature
It is believed that a healthy child should have a body temperature of 36.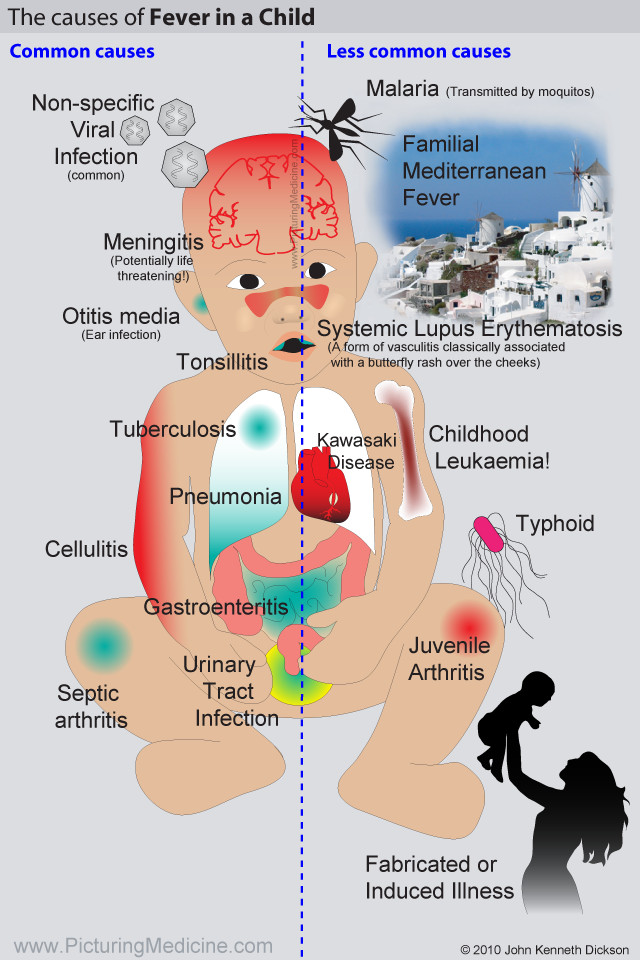 6 °C. And its increase over 37 degrees is regarded as a sign of illness. But it is not so.
6 °C. And its increase over 37 degrees is regarded as a sign of illness. But it is not so.
Body temperature depends on age and measurement area. It can increase after physical exertion, emotional arousal and feeding.
Devices and time for measuring body temperature nine0005
To determine the temperature, the following types of thermometers are used:
-
digital;
-
mercury;
-
infrared.
The optimal time for thermometry is 7-9 am and 17-19 pm. As prescribed by the doctor, the determination of the temperature during the day in children can be performed 3-4 times. nine0005
What temperature is considered normal for a child?
Immediately after the birth of a newborn, the temperature of his body decreases by 1-2 ° C, then within 24 hours it rises to 36-37 ° C. In the first 3 months of a baby's life, its indicators are unstable and depend on external factors: indoor air temperature, sleep, food intake. Normally, these fluctuations do not exceed 0.6 °C per day. For children of the first year of life, a temperature of 37.7 is the norm. nine0005
Normally, these fluctuations do not exceed 0.6 °C per day. For children of the first year of life, a temperature of 37.7 is the norm. nine0005
The average body temperature for a child is 37°C. Usually in the morning - 36.3 ° C, and in the evening it can rise to 37.6 ° C.
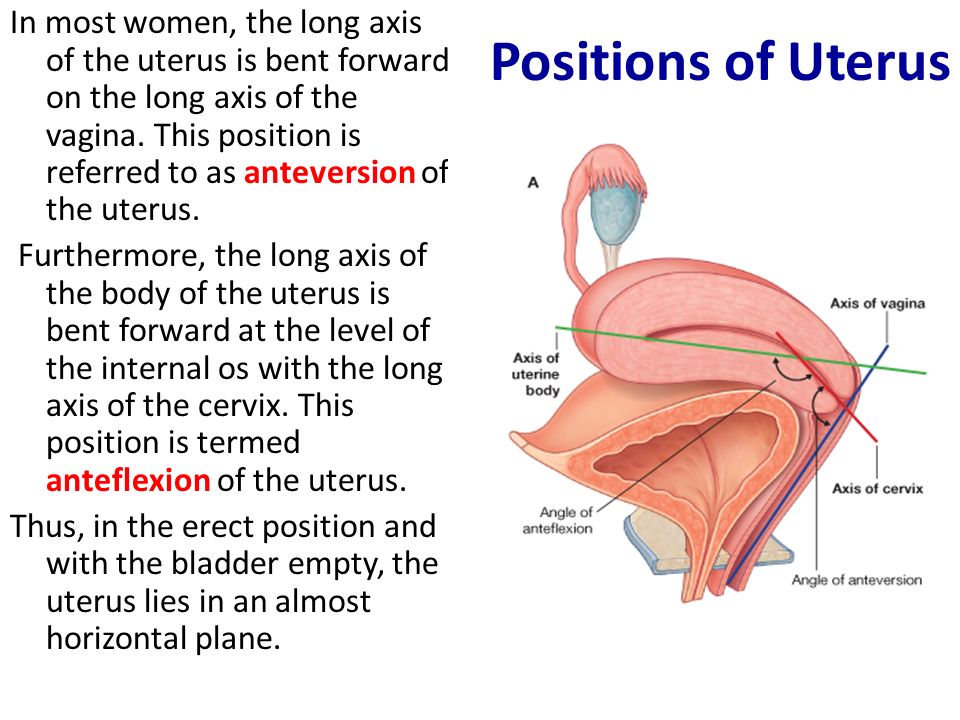
In what areas can the temperature of children be taken?
Underarm
The temperature measurement time under the arm is 5-10 minutes and depends on the type of device.
In the rectum
It is used in children under 5 years of age and in debilitated patients. For this method, it is desirable to use medical electronic thermometers with a soft tip. It will take 1-1.5 minutes to determine the rectal temperature. nine0005
Oral
The procedure is performed both under the tongue and behind the cheek. Contraindications to the use of this method are: children under 4-5 years of age, increased excitability and impaired nasal breathing.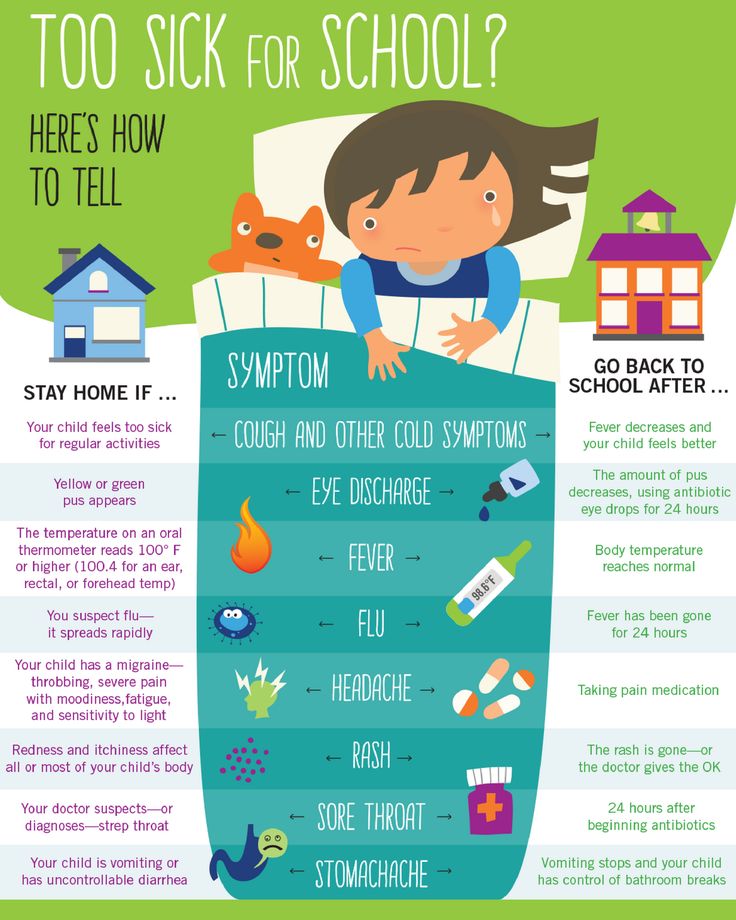 The duration of temperature measurement by the oral method is from 10 seconds to 3 minutes.
The duration of temperature measurement by the oral method is from 10 seconds to 3 minutes.
In the ear
The temperature in the ear is measured with an infrared sensor. The tip of the thermometer is inserted into the ear canal and the result appears on the display. nine0005
On forehead
Forehead temperature can be measured with a contact and non-contact thermometer. It will take 3 to 5 seconds to get the result. If the baby is sleeping or excited, then it is more convenient to use a non-contact method for measuring temperature.
Crotch
Mainly used in infants. The measurement time in the inguinal fold is 5 minutes. The method is inconvenient because the baby is not easy to keep in one position during this time. nine0005
Ranges of normal temperature in children depending on age and area of measurement are presented in the following table:
| 0-2 years | 3-10 years | 11-18 years old | |
|---|---|---|---|
| In the armpit | 34. 7 - 37.2 7 - 37.2 | 35.8 - 36.6 | nine0095 35.1 - 36.8|
| On the forehead | 36.7 - 37.5 | 36.7 - 37.5 | 36.5 - 37.4 |
| in the ear | 36.3 - 37.7 | 36.3 - 37.7 | 36.7 - 37.8 |
If a child has a fever, what should I do? nine0001
home
Articles
Health
Kurilova Alina Petrovna Pediatrician
14.05.2019
Before you start taking antipyretics, you need to answer a few questions:
-
what is the age of the child?
-
How does a child tolerate an increase in a particular temperature? nine0005
-
Have there been any family or child history of febrile seizures?
-
Are there any other symptoms of the disease besides fever?
An increase in temperature or fever is a protective and adaptive reaction of the body in response to the effects of pathogenic stimuli, which results in a restructuring of thermoregulation processes, leading to an increase in body temperature, which stimulates the body's natural resistance. nine0005
nine0005
An increase in temperature affects the child's body both positively and negatively.
The positive effect of is that when the temperature rises in the child's body, the immune system is activated, phagocytosis increases, the production of antibodies increases and the level of interferon increases, which helps to stop the reproduction of pathogenic microorganisms and overcome the infection.
Negative influence high temperature per child is manifested in the occurrence of convulsions (febrile), an increased load on the baby's cardiopulmonary system (heart rate and respiratory rate become more frequent). Therefore, fever is dangerous for children with malformations of the heart and bronchopulmonary system, heart rhythm disturbance. Also, when the temperature rises, the work of the brain, liver, stomach, kidneys and other internal organs suffers, which is dangerous for children with chronic pathologies of internal organs, symptoms of dehydration, developmental disorders and diseases of the nervous system. nine0005
nine0005
Fever varies:
-
with the flow:
-
acute (fever up to 2 weeks),
-
subacute (up to 6 weeks),
-
chronic (over 6 weeks).
-
-
by the degree of increase of the indicator: nine0005
-
subfebrile (increase to +38.0 degrees)
-
febrile (from +38.0 to +39.0 degrees),
-
pyretic (from + 39.0 to + 41.0 degrees),
-
hyperpyretic (over +41.0 degrees).
-
-
according to the type of temperature curve: nine0005
-
constant (temperature fluctuations during the day are not higher than 1 degree).
-
laxative (daily fluctuations up to 2 degrees),
-
atypical (fluctuations are chaotic, different and irregular),
-
debilitating (a combination of laxative and atypical fever with fluctuations during the day more than 2-3 degrees), nine0005
-
intermittent (a combination of short periods of temperature increase and decrease to normal numbers),
-
return (alternation of periods of temperature increase with periods of temperature normalization from 2 to 7 days).
-
On the recommendation of the WHO (World Health Organization), antipyretics are prescribed for children according to age:
-
from the moment of birth to 2 months at a temperature of +38.0 degrees,
-
children from 3 months to 24 months at a temperature of +38.5 degrees,
-
children from 1 to 5 years old at a temperature of +39.0 degrees,
-
children over 5 years old with indicators of + 39.5- + 40.0 degrees. nine0005
On the other hand, the approach to each child should be individual.
If a child
- restless or feeling weak,
- cannot tolerate muscle pain, headache,
- have nausea,
- no appetite,
then you must first apply physical methods to improve the well-being of the child :
-
put to bed - so the body will save strength to fight the infection, calm the child;
-
drink fractionally with water or sweetened warm herbal tea with chamomile, linden, cranberry juice;
-
provide access to fresh air;
-
to feed in the presence of appetite in small portions of warm food (for example, soup, liquid porridge on the water, a light breakfast).
 nine0005
nine0005
Also, according to the clinical variant of the course of fever, apply additional cooling measures.
With "red" or "pink" fever
- the child's body feels hot to the touch,
- skin red or pink, moist,
- the child himself does not complain about his well-being, he is active, his appetite does not disappear.
In this case, child needs
- undress,
- wipe with a towel soaked in water at room temperature,
- apply a cool compress to the forehead,
- drink water at room temperature
- and be sure to call a doctor.
With "white or pale" fever
- the child's limbs and body are cold to the touch,
- lips and nail beds become bluish,
- pale and dry skin,
- there is a violation of well-being: the child is lethargic, delirium is possible.
In this case child needs
- warm by rubbing the limbs with hands or using warm water (no other means!),
- put on socks,
- cover with a blanket
- and drink warm tea or water.
The use of antipyretics for such symptoms is ineffective - you need to urgently call a doctor! nine0255
An exception is children at risk, who have their temperature reduced above 37.1 degrees. These are children,
- with diseases of the nervous system,
- convulsions due to fever,
- suffering from chronic diseases of the circulatory system, respiratory organs or with hereditary metabolic diseases and other risks (overheating, symptoms of dehydration, etc.).
Febrile convulsions are diagnosed more often in children under 6 years of age with temperatures above +38 degrees, as well as in children with pathology of the nervous system at any temperature. For such children, it is recommended to lower the temperature to febrile levels (not higher than +38.0) or to those values recommended by a neuropathologist. nine0005
Usually, against the background of an increase in temperature, the child's heart rate and respiratory rate increase: the respiratory rate increases by 4 respiratory movements for every degree above +37. 0 degrees, and the pulse rate - by 20 beats per minute for every degree. However, against the background of diseases of the cardiovascular system and respiratory organs, such as malformations or cardiac arrhythmias, inadequate increases or slowdowns in heart rate and respiration are possible. Such children, on the recommendation of a cardiologist and pulmonologist, are prescribed antipyretic drugs to febrile numbers (ie, not higher than +38.0 degrees). nine0005
0 degrees, and the pulse rate - by 20 beats per minute for every degree. However, against the background of diseases of the cardiovascular system and respiratory organs, such as malformations or cardiac arrhythmias, inadequate increases or slowdowns in heart rate and respiration are possible. Such children, on the recommendation of a cardiologist and pulmonologist, are prescribed antipyretic drugs to febrile numbers (ie, not higher than +38.0 degrees). nine0005
Children with hereditary metabolic diseases (diseases of the thyroid gland, kidneys, liver, disorders in the immune system, and others) and children with imperfect compensatory mechanisms of thermoregulation during fever (these are some children from birth to 2 months) are also prescribed antipyretic drugs on the recommendation of related specialists means to febrile digits.
Overheating - increase in body temperature due to additional exposure to heat
- prolonged sun exposure,
- use of excess clothing,
- excessive wrapping of children).
The danger of overheating is associated with the risk of heat stroke. It manifests itself
- not only in elevated temperature,
- but also in impaired consciousness, convulsions,
- disorders of the heart and breathing.
First aid is to call the ambulance "112". nine0386
Until the doctor arrives
- undress the child,
- move to a cool place or shade,
- supply fresh air or fan (but not cool air!),
- apply a cold compress to the forehead,
- Wipe the body with cool water or cover with a sheet soaked in cool water.
Antipyretic therapy for children should be prescribed strictly individually, taking into account clinical and anamnestic data. nine0005
It is important to know that taking antipyretic drugs does not shorten the duration of the febrile period. At the end of the drug, the temperature rises again.
Antipyretics have a lot of side effects:
- allergic reactions,
- bleeding,
- stomach injuries (vomiting, regurgitation),
- Reye's syndrome (against the background of rash, vomiting, psychomotor agitation occurs).
 nine0018
nine0018
In addition, the decrease in body temperature should not be critical, it is not necessary to achieve normal performance. It is enough to lower the temperature by 1.0 or 1.5 degrees, which will improve the child's well-being and avoid collapse.
The collapse develops with a critical (rapid and sharp) decrease in temperature for a short time (from 40-41 degrees to 37-36.0 degrees) by 2.5 - 3.0 degrees or more.
The result is
- acute cardiovascular insufficiency, accompanied by vasospasm and circulatory disorders.
Child feels
- cold or chilly,
- severe weakness,
- headache,
- thirsty,
- he has pale skin up to a bluish tint,
- sticky sweat,
- cold extremities,
- insomnia,
- shortness of breath up to shallow breathing,
- palpitations,
- lowering blood pressure,
- convulsions,
- loss of consciousness.