How far apart contractions before going to hospital
Labor: When to Go to the Hospital
Your body starts preparing for labor in advance — as much as a month before you actually give birth. It can be tough to know when it’s happening for sure. We’ll help you spot the difference between a dress rehearsal and the real deal.
Learn to recognize the signs of labor
When to come to the hospital
Timing is different for every pregnancy. At your third trimester prenatal appointments, we’ll talk about how to know when it’s time, what to do, and where to go, but ideally you’ll come to the hospital when you’re in active labor.
It’s common to think the first signs of contractions are your cue to come to the hospital, but that’s usually not the case. Early labor can last for days. All we can do at this stage is wait for signs that your body is ready to deliver, so a lot of people come in too soon and wind up going home again. Getting from point A to point B isn’t fun during any stage of labor, so call us before you come so we can help you avoid multiple trips. Counting your contractions can help you figure out when it’s really time to go.
Real labor vs. false labor
You might have Braxton Hicks contractions — also called false labor — as your due date approaches. They’re basically warm-ups for childbirth, when your uterus expands and contracts, but you’re not in labor.
What’s the difference?
People call these types of contractions false labor because they can trick you into thinking it’s time when it’s really not. Spot the difference with these signs of Braxton Hicks contractions:
- There’s no pattern.
- They don’t last longer than an hour.
- If you move around, they go away.
- They aren’t painful.
If you’re still not sure, just call your care team. That’s what we’re here for.
Induced labor
Sometimes there are signs that it’s time to deliver your baby before labor starts on its own. If that happens, your care team might step in and get things going by inducing labor.
Learn why and how we induce labor
Counting labor contractions
A contraction is a tightening of the uterus that feels like cramping or pressure. You should feel it over your entire uterus and possibly into your back. As labor progresses, your contractions become more frequent and regular, so timing them is a good way to figure out when it’s time to head to the hospital.
Timing is everything. Here’s how it works:
- Start timing your contractions once you feel a few in a row.
- Time the length of each contraction. If the tightness lasts for 30 seconds or longer, they’re labor contractions.
- Count the time between contractions from the start of one to the start of the next.
If this is your first baby, come to the hospital when your contractions:
- Come every 3 to 5 minutes over an hour-long period
- Last at least 45 to 60 seconds
If you’ve given birth before, come to the hospital when your contractions:
- Come every 5 to 7 minutes
- Last at least 45 to 60 seconds
Speeding up the process
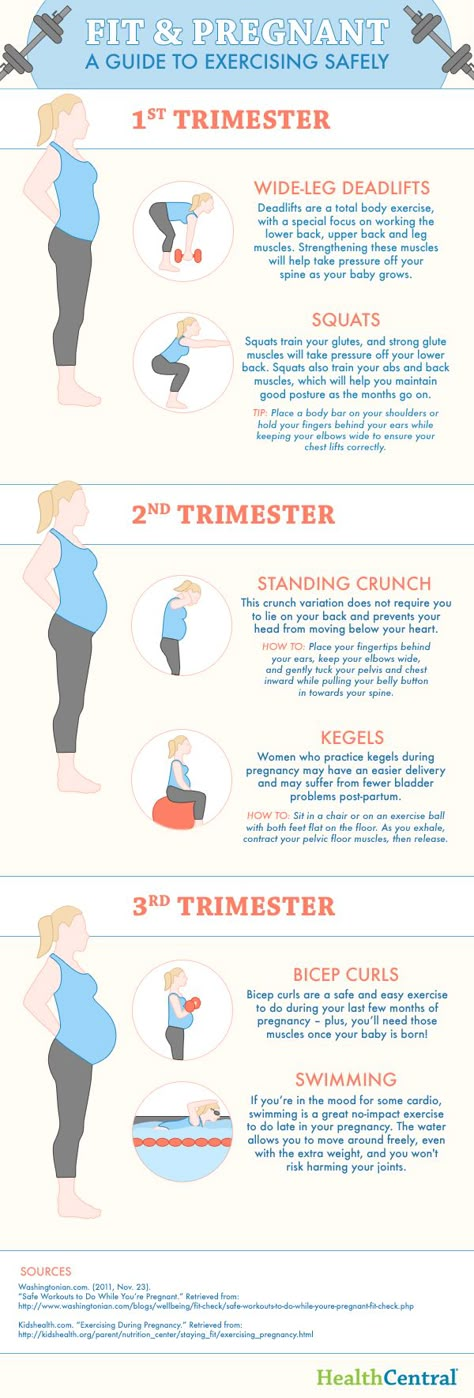
If your contractions are still far apart and you want things to go faster, try walking around. It can help your baby move into your pelvis. The pressure that gravity puts on your cervix can also help things move along. You can also try these labor and birth positions to ease discomfort and possibly speed things up a bit.
It can help your baby move into your pelvis. The pressure that gravity puts on your cervix can also help things move along. You can also try these labor and birth positions to ease discomfort and possibly speed things up a bit.
Planning ahead
The first thing to do is call us to let the care team know you’re on your way. Save the number of Kaiser Permanente's dedicated Labor Line to your phone now so you have it when you need it.
After you call your care team, get going! Grab your hospital bag, head to the hospital, and get ready to meet your new baby.
How to Know When to Go to the Hospital for Labor
Let’s hope you have a timer handy because if you’re reading this, you may need to time your contractions, grab your bag, and head to the hospital.
A simple rule for when to go to the hospital for labor is the 5-1-1 rule. You may be in active labor if your contractions happen at least every 5 minutes, last for 1 minute each, and have been happening consistently for at least 1 hour.
That said, it’s sometimes tricky to recognize true labor. As the calendar hovers close to your due date, you notice every little twinge. Is that gas, the baby kicking, or a sign you’re about to meet your little one?
Or maybe you’re experiencing signs of labor a bit earlier than expected. How can you tell whether it’s go-time, or if your body is just preparing for what’s to come? Here’s a rundown on what to expect and when you should head to the hospital for labor.
For most women, labor starts much differently than in the movies. On screen, labor comes on as a big surprise when the character’s water breaks. But it’s important to note that — in real life — only about 10 percent of women experience their water breaking.
Usually, the signs of labor are much more subtle and gradual. Your process will be different from a friend’s and even from your other pregnancies.
Labor normally has two parts: early labor and active labor.
Early labor
Early labor (also known as the latent phase of labor) is usually still some time away from the actual birth. It helps your baby get into place for birth. During early labor you’ll start feeling contractions that aren’t too strong. The contractions might feel regular or come and go.
It helps your baby get into place for birth. During early labor you’ll start feeling contractions that aren’t too strong. The contractions might feel regular or come and go.
This lets your cervix (the opening to the womb) open and soften. According to the American College of Obstetricians and Gynecologists (ACOG), early labor is the period of time when your cervix dilates up to 6 centimeters.
During this phase, you might also feel your little one move around and kick more than they usually do, or feel additional pressure of the baby “dropping” into place. This is because they’re trying to move down head first (hopefully) into the birth canal.
As your birth canal opens the mucus plug to your cervix may pop out. This is a completely normal part of birth. You might have a clear, pink, or even red glob or discharge in your underwear, or notice it when you wipe after using the toilet.
At this point in early labor you might feel achy and a little uncomfortable, but it’s too soon to go the hospital.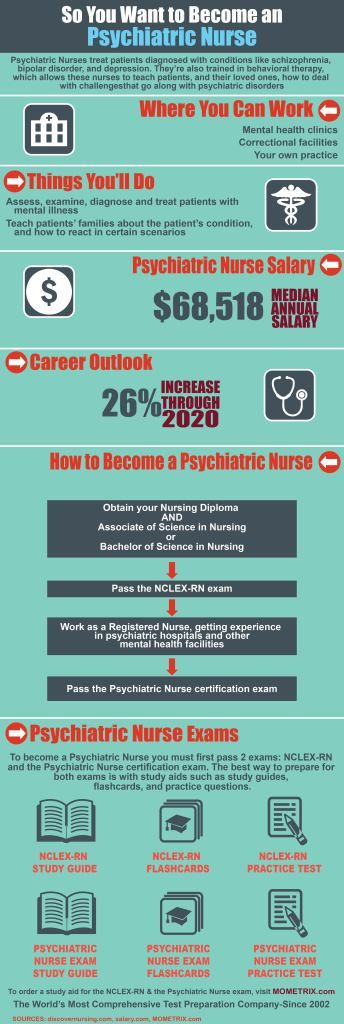 Recent research has shown early labor is much longer and slower than previously believed.
Recent research has shown early labor is much longer and slower than previously believed.
Early labor can last from hours to days. One 2010 study found that labor can take 9 hours to progress just from 4 to 6 centimeters, though it can vary widely from person to person.
Sometimes, early labor will start and then stop for a little while. Along with making sure you partner has your hospital bag ready to go, here’s what you can try to do once you start early labor:
- Try to relax (easier said than done, of course!).
- Walk around the house or yard.
- Lie down in a comfortable position.
- Have your partner gently massage your back.
- Try breathing techniques.
- Meditate.
- Take a warm shower.
- Use a cold compress.
- Do anything that keeps you calm.
If you think you’re in early labor, try to relax and allow your body to progress naturally, at home. Researchers of at least one large study believe that women who allow early labor to progress naturally without intervention may have less risk of cesarean delivery.
Active labor
Per ACOG, the clinical definition of the start of active labor is when your cervix has reached 6 centimeters in dilation. But, you won’t know how dilated you are until you’re checked by a doctor or midwife.
You’ll be able to tell you’re entering active labor when your contractions are stronger, more regular, and happening closer together. It’s a good idea to time them. Write down when your contractions happen and how long they last.
You’ll know you’re in active labor if you have symptoms like:
- painful contractions
- contractions that about 3 to 4 minutes apart
- each contraction lasting about 60 seconds
- water breaking
- lower back pain or pressure
- nausea
- leg cramps
During active labor your cervix (birth canal) opens or dilates from 6 centimeters to 10 centimeters. Your contractions might happen even faster if your water breaks.
You should definitely be on your way to the hospital or birthing center when you’re in active labor — especially if you’ve been pregnant or given birth before.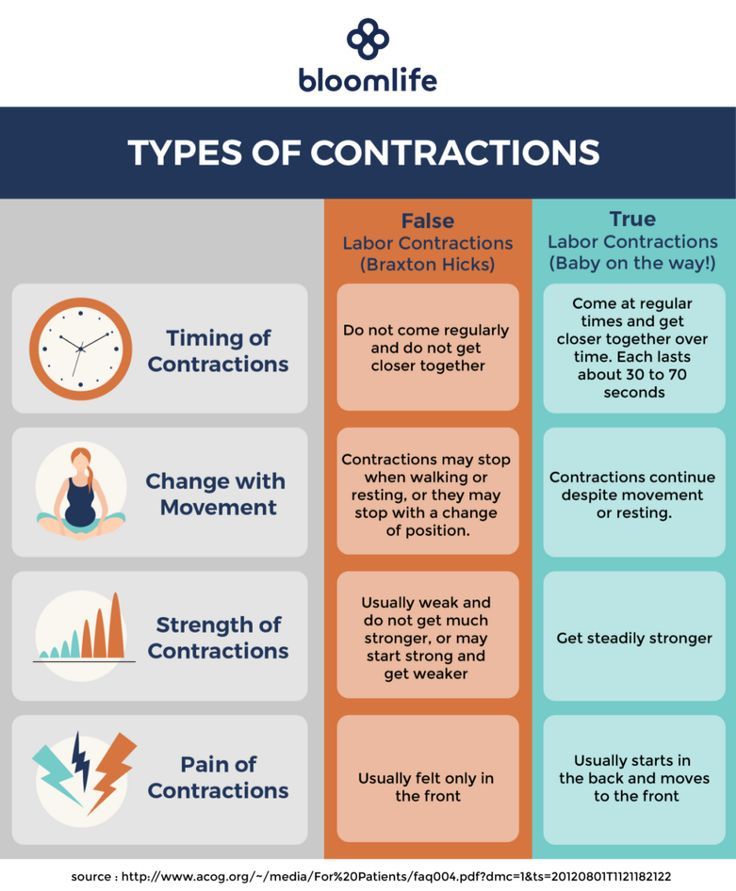 A large 2019 study of more than 35,000 births showed that labor progresses doubly quick when you’ve already gone through it.
A large 2019 study of more than 35,000 births showed that labor progresses doubly quick when you’ve already gone through it.
Sometimes you may think you’re starting labor, but it’s just a false alarm. You might feel contractions, but your cervix is not dilating or effacing.
False labor (also known as prodromal labor) can be pretty convincing and it’s fairly common. A 2017 medical study found that more than 40 percent of pregnant women had false labor when they thought they were in labor.
False labor typically happens pretty close to your due date, at 37 weeks of later. This makes it even more confusing. You may have contractions for up to several hours that happen at regular intervals. False labor contractions are also called Braxton-Hicks contractions.
The difference between false labor and true labor is that false labor contractions won’t make your cervix open up. You can’t measure down there, but you might be able to tell if you are in false or true labor by checking your symptoms:
| Symptom | False Labor | True Labor |
| Contractions | Feel better after walking | Don’t feel better after walking |
| Contraction strength | Stay the same | Get stronger over time |
| Contractions interval | Stay the same | Get closer together over time |
| Contraction location | Generally only at the front | Begin at the back and move to the front |
| Vaginal discharge | No blood | May have some blood |
Shannon Stallock, a midwife in Oregon, recommends letting your OB-GYN or midwife know if you’ve started early labor. You might move along into active labor faster than you expect. A rule of thumb is that labor usually lasts for a shorter period if you’ve had a baby before.
You might move along into active labor faster than you expect. A rule of thumb is that labor usually lasts for a shorter period if you’ve had a baby before.
If you are having a planned C-section you may not go into labor at all. This might be the case if you’ve delivered a baby via C-section before or if you have some complications that make a C-section birth a safer choice.
Call your doctor and go to the hospital if you go into early or active labor before your planned C-section date. Going into labor does not mean that you’ll have to deliver your baby vaginally, but it may mean that you’ll need to have an emergency C-section. Getting to the hospital quickly means more time to get ready for the procedure.
Go to the hospital if you’re not sure whether you’re in false labor or true labor. It’s healthier for you and your baby to err on the side of caution.
The worst that can happen is that you might be in false labor and have to come home and wait. But, that’s safer than if you’re in true labor and delay going to the hospital.
It might feel like an emergency, but skip the emergency room and make a beeline for labor and delivery when you get to the hospital. A very useful tip, especially if this is your first baby, is for you and your partner to do a practice drive to the hospital so you know exactly where to go.
Once you’re at the hospital, your doctor or nurse can tell whether you’re in real labor with a physical checkup. You might also have an ultrasound. The ultrasound scan shows the length and angle of the cervix. A shorter cervix and a bigger angle between the uterus (womb) and cervix mean you’re in true labor.
If you are delivering at home or at a birthing center, you still need to practice a dry run to make sure you are prepared and have everything you need.
For example, if you’re planning on a water delivery, get into the inflatable pool well before your due date and make sure you like it! Always plan ahead for emergencies. Have your doctor on speed dial and a car ready to take you to the hospital if needed.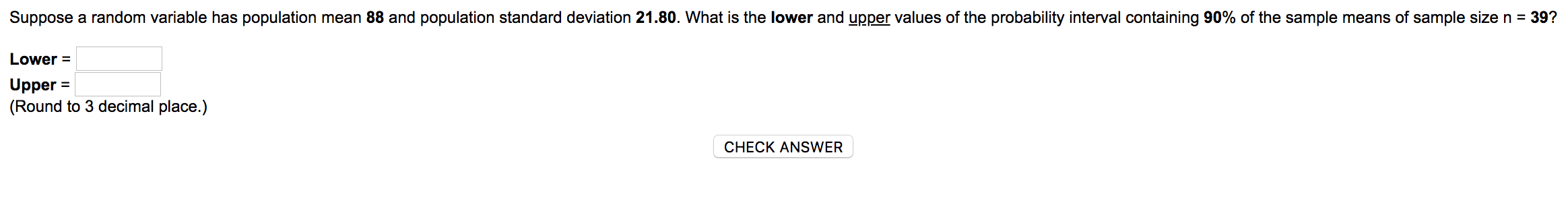
Go to the hospital immediately if:
- Your water breaks.
- You have blood in your vaginal discharge.
- You feel the urge to bear down and push.
If your contractions are 5 minutes apart, lasting for 1 minute, for 1 hour or longer, it’s time to head to the hospital. (Another way to remember a general rule: If they’re getting “longer, stronger, closer together,” baby’s on their way!)
If you’re feeling contractions, but they’re not strong and lengthy yet, you might be experiencing the early phase of labor. Resting and letting your body progress at home may help you deliver vaginally in the long run.
False labor is fairly common. Call your doctor if you are unsure. It’s best to be extra careful to protect your health and the safety of your new little one.
Regardless of what stage of labor you’re in, take a deep breath and smile, because you’re about to meet the newest love of your life.
Reception Department
Home \ Services \ Obstetrics \ Reception Department
The Reception Department carries out a consultative examination of patients and, if necessary, their hospitalization in the maternity or prenatal department.
Hospital admissions are planned or emergency. Emergency hospitalization is carried out out of turn and at any time of the day - these are childbirth, bleeding, outpouring of water, high blood pressure, etc.
Planned hospitalization and appointment for planned hospitalization is carried out on weekdays from 9.00- to 17.00.
For planned hospitalization, there must be a referral from the LC with the order number
A referral for hospitalization with the order number is valid for 10 calendar days.
The referral is given not for childbirth or cesarean, but for hospitalization. How you give birth will be decided only in the maternity hospital.
FOR HOSPITALIZATION IN THE ANTERNATIVE DEPARTMENT YOU NEED:
- Passport (+ its photocopy) page with photo, registration and marriage page
- Compulsory medical insurance policy (+ its photocopy)
- SNILS (+ its photocopy)
- Temporary registration (+ its photocopy) For residents outside of St. Petersburg and Leningrad Region
Petersburg and Leningrad Region
- Photocopy of an insert in an exchange card (with information on reconciliation with a tube dispensary and data on a fluroexamination of the environment of a pregnant woman)
- For citizens other countries and republics, according to the law of the Russian Federation, a notarized passport and two photocopies of it + 2 photocopies of the internal passport of each sheet (1 copy is required for the migration service and 1 copy for paying for hospitalization and paperwork for mother and child)
- A photocopy of an official ID for employees of the Ministry of Emergency Situations and the Ministry of Internal Affairs (and others certified) and a payment agreement from their organization with its photocopy.
- Photocopy of sick leave (preferably)
- Birth certificate
- Referral from the antenatal clinic
- Exchange card
- Bathrobe, shirt, socks, slippers
- Personal hygiene items
- Mug, spoon, plate
- Lining for examination
- All things must be packed in plastic bags, no bags or backpacks can be brought into the airport.
- Before hospitalization, it is necessary to take a shower and shave
FOR HOSPITALIZATION IN THE MATERNITY DEPARTMENT YOU NEED:
- Passport (+ its photocopy) page with photo, registration and marriage
- Compulsory medical insurance policy (+ its photocopy) 90SIL (+ its photocopy)
- Temporary registration (+ its photocopy) For residents outside of St. Petersburg and Leningrad Region
- Photocopy of the insert in the exchange card (with information on reconciliation with the tube dispensary and data on the fluroexamination of the environment of the pregnant woman)
- For citizens of other countries and republics, according to the law of the Russian Federation, a notarized passport and two photocopies of it + 2 photocopies of the internal passport of each sheet (1 copy is required for the migration service and 1 copy for paying for hospitalization and processing documentation for mother and child)
- Xerox service certificate for employees of the Ministry of Emergency Situations and the Ministry of Internal Affairs (and others certified) and a payment agreement from your organization with its photocopy.
- Photocopy of sick leave (preferably)
- Birth certificate
- Exchange card
- Bathrobe, shirt, socks, slippers
- Toilet paper and towel
- Phone with charger
- Bottle of non-carbonated water
- 5 pcs of disposable absorbent diapers
- 4 diapers for a newborn
- Pack of disposable panties
- Compression stockings at the request or appointment of an obstetrician or hematologist
- Packing of postpartum pads
- All things must be packed in plastic bags, no bags or backpacks can be brought into the RD
- A warm cotton hat and noses for the baby
- Before hospitalization, it is necessary to take a shower and shave
Harbingers of childbirth - How to understand that it is time to go to the hospital?
January 10, 2017
Alekseeva Inna
Obstetrician-gynecologist, Doctor of the highest category
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www.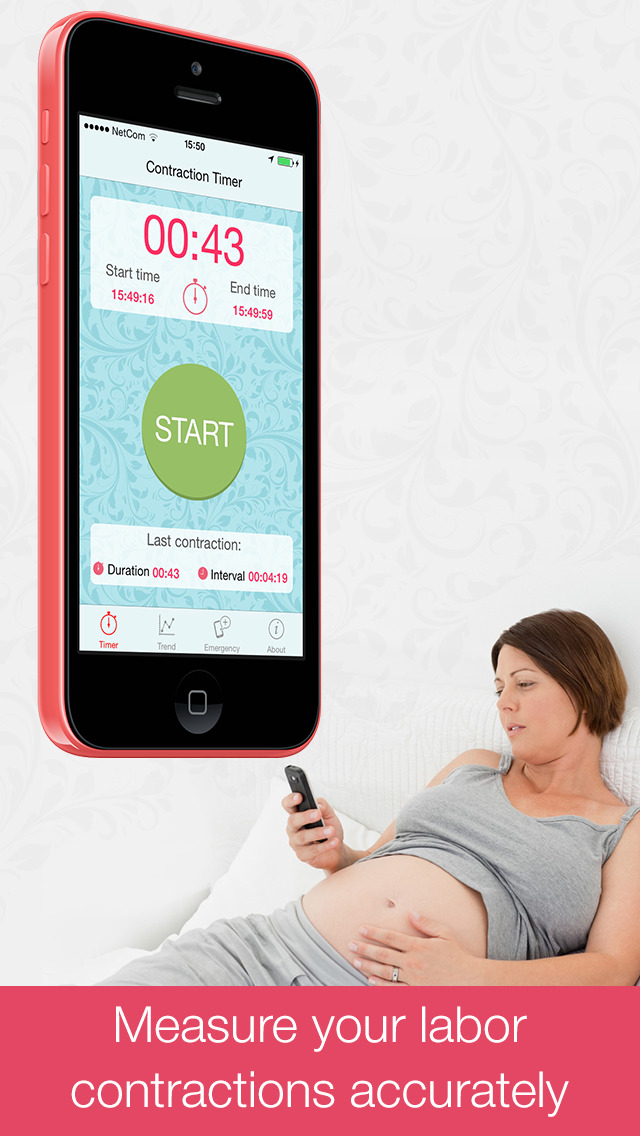 instagram.com/roddompravda/
instagram.com/roddompravda/
Tips and opinions from leading child professionals: https://www.instagram.com/emc.child/
Every pregnant woman with excitement and joy awaits the upcoming birth. The closer the cherished date, the more attentively the expectant mother listens to the changes taking place in her body and in the behavior of the baby. Of course, the expectant mother wants to know by what signs it is possible to understand that childbirth is just around the corner.
It is customary to call the harbingers of childbirth external, really tangible changes in the body, which are direct preparation for the onset of labor. The tissues of the birth canal - the cervix, vagina, vulva, perineum - become quite elastic, extensible, but at the same time - very strong and resistant to tearing. The cervix is located in the center of the vaginal vault, shortens by almost half its normal length and softens significantly. The cervical canal - the lumen of the cervix connecting the uterine cavity with the vagina - opens slightly, as a result, the diameter of the cervical canal is approximately 2-2. 5 cm. Of course, such a significant "perestroika" takes more than one day.
5 cm. Of course, such a significant "perestroika" takes more than one day.
Female sex hormones are responsible for preparing for childbirth. During the nine months of pregnancy, progesterone "reigns" in the body of the expectant mother. It ensures the normal tone of the uterus (relaxed state of the muscles), the production of cervical mucus - a mucous plug in the cervix that protects the fetus from infection. The amount of progesterone during pregnancy largely determines the normal development and growth of the fetus, the necessary concentration of nutrients and oxygen in the mother's blood, as well as their timely and uninterrupted delivery to the baby.
Shortly before childbirth, the production of progesterone decreases markedly, it is replaced by estrogens - female sex hormones. The increase in estrogen in the blood is caused by the need to prepare the body for the upcoming birth. It is these hormones that are responsible for the elasticity and patency of the birth canal. The rate of cervical dilatation in the first stage of labor depends on them. In the second period, when the cervix is fully opened and the fetus passes through the birth canal, it is also very important how elastic and extensible the walls of the vagina are - this will largely determine the duration of the straining period. Finally, the onset of labor itself depends on the level of estrogen: contractions occur as a result of a nerve impulse that is caused by a certain level (“peak”) of estrogen accumulation.
The rate of cervical dilatation in the first stage of labor depends on them. In the second period, when the cervix is fully opened and the fetus passes through the birth canal, it is also very important how elastic and extensible the walls of the vagina are - this will largely determine the duration of the straining period. Finally, the onset of labor itself depends on the level of estrogen: contractions occur as a result of a nerve impulse that is caused by a certain level (“peak”) of estrogen accumulation.
These changes are normal and do not require an unscheduled visit to the doctor or hospitalization. Harbingers of childbirth are manifestations of a planned restructuring in the body of a future mother, the “finishing touches” of preparation for the upcoming joyful event.
The absence of clearly perceptible changes on the eve of the expected date of birth is also not a pathology. Not all expectant mothers note those changes in well-being that are commonly called harbingers. However, this does not mean that there is no preparation. In some cases, the “final preparations” go unnoticed by the pregnant woman. Therefore, do not worry or urgently contact a specialist.
However, this does not mean that there is no preparation. In some cases, the “final preparations” go unnoticed by the pregnant woman. Therefore, do not worry or urgently contact a specialist.
The appearance of any of the "harbingers" indicates the likelihood of the development of regular labor activity over the next two hours - two weeks. None of the sensations described gives a 100% guarantee that a woman will become a mother within the next 24 hours. Hormonal changes before childbirth begin approximately two weeks before the expected birth. Theoretically, during these two weeks, at any time, a pregnant woman can notice certain changes in her state of health. Consequently, the absence of labor activity an hour, a day, or even a week after the first noted changes is not a pathology and does not require special medical advice.
- Scarlet discharge from the genital tract in any amount.
- Severe abdominal pain.
- Increased blood pressure (above 130/80 mmHg).

- An increase in body temperature to 37.5 ° C and above.
- Increased heart rate (more than 100 beats per minute).
- Severe headache, vomiting, blurred vision.
- Significant increase in edema.
- Absence, sharp decrease, sharp increase in fetal movements.
- Suspicion of amniotic fluid leakage.
Weight loss . Shortly before the expected date of delivery, the expectant mother may notice some “weight loss”. Weight loss during this period is associated with the removal of excess fluid from the body, that is, a general decrease in edema. The more pronounced the fluid retention during pregnancy, the more mass the pregnant woman will “lose” on the eve of childbirth. During pregnancy, water is retained in the body of all expectant mothers to a greater or lesser extent. The reason is progesterone - a hormone whose main function is to support the processes of pregnancy. Before childbirth, progesterone is replaced by estrogen. It is estrogen that removes excess fluid from the body. The first results are visible on the hands, feet and legs. Depending on the severity of edema, weight loss before childbirth varies from 0.5 to 2.5 kg.
Before childbirth, progesterone is replaced by estrogen. It is estrogen that removes excess fluid from the body. The first results are visible on the hands, feet and legs. Depending on the severity of edema, weight loss before childbirth varies from 0.5 to 2.5 kg.
Change of stool. Increased frequency and change in the consistency of physiological functions on the eve of childbirth is also associated with an increase in estrogen levels and the removal of fluid from the body of the expectant mother. Similar changes in the body of a non-pregnant woman are observed during menstruation. The chair can become more frequent up to 2-3 times a day, at the same time there may be some liquefaction of the feces. More frequent urge to defecate, a sharp change in the color and smell of feces, combined with nausea and vomiting, is a reason for consulting a doctor - food poisoning can be masked under such "harbingers".
Fundal prolapse. Shortly before delivery, the baby presses the presenting part (most often the head) against the lower segment of the uterus and pulls it down, pressing against the entrance to the small pelvis. The fetus "groups", taking the most advantageous position for itself at the time of the onset of contractions. As a result of such "preparations" from the side of the fetus, the uterus "sags", and its upper part - the bottom - ceases to exert pressure on the internal organs. After lowering the bottom of the uterus, the pregnant woman has no shortness of breath (it becomes easier to breathe, there is a feeling of a full breath). If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part.
Shortly before delivery, the baby presses the presenting part (most often the head) against the lower segment of the uterus and pulls it down, pressing against the entrance to the small pelvis. The fetus "groups", taking the most advantageous position for itself at the time of the onset of contractions. As a result of such "preparations" from the side of the fetus, the uterus "sags", and its upper part - the bottom - ceases to exert pressure on the internal organs. After lowering the bottom of the uterus, the pregnant woman has no shortness of breath (it becomes easier to breathe, there is a feeling of a full breath). If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part. Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent.
Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent.
Isolation of the mucous plug. During pregnancy, the glands of the mucous membrane of the cervical canal (the lumen of the cervix) secrete a special secret. It is a thick, sticky, jelly-like mass that forms a kind of cork. The mucous plug completely fills the cervical canal, preventing the penetration of bacterial flora from the vagina into the uterine cavity. Thus, cervical mucus, or the mucous plug of the cervix, protects the fetus from ascending infection. Before childbirth, when the cervix begins to soften under the influence of estrogen, the cervical canal opens slightly and the cervical mucus contained in it can be released. In this case, the expectant mother may find small clots of yellowish-brownish mucus, transparent, jelly-like, odorless. The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases.
The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases.
Training contractions. Training or false contractions are called such contractions that appear shortly before childbirth and are not actually labor activity, since they do not lead to the opening of the cervix. A contraction is essentially a single contraction of the uterine wall; this contraction usually lasts a few seconds. At the time of the contraction, the expectant mother feels a gradually increasing and then gradually decreasing tension in the abdomen. If at this moment you put your hand on your stomach, you can notice that the stomach becomes very hard, but after the contraction it completely relaxes and becomes soft again. In addition to involuntary tension of the uterus, other changes in the well-being of the expectant mother during false contractions are usually not noted. It is not difficult to distinguish training fights from real ones. In most cases, false contractions are weak, painless, irregular or alternating at a significant interval (30 minutes or more). Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization.
At the time of the contraction, the expectant mother feels a gradually increasing and then gradually decreasing tension in the abdomen. If at this moment you put your hand on your stomach, you can notice that the stomach becomes very hard, but after the contraction it completely relaxes and becomes soft again. In addition to involuntary tension of the uterus, other changes in the well-being of the expectant mother during false contractions are usually not noted. It is not difficult to distinguish training fights from real ones. In most cases, false contractions are weak, painless, irregular or alternating at a significant interval (30 minutes or more). Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization. False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days.
False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days.
Discomfort. In the last weeks before giving birth, many pregnant women report discomfort in the lower abdomen and in the area of the sacrum (the area slightly below the waist). Such changes in
the well-being of the expectant mother is caused by sprain of the pelvic ligaments and increased blood flow to the pelvic organs. Usually these minor sensations, described as a feeling of "light languor" in the lower abdomen, are comparable to similar phenomena in the period before or during menstruation. Discomfort, like training contractions, more often disturbs the expectant mother in the morning and evening hours. The level of discomfort is minimal, it should not worry the expectant mother and does not require medical intervention.
All harbingers of childbirth can appear during the last two weeks before childbirth, their presence, as well as their absence, is the norm and does not require a visit to a doctor.