Labor is induced by
Labor Induction | ACOG
Amniotic Fluid: Fluid in the sac that holds the fetus.
Amniotic Sac: Fluid-filled sac in a woman's uterus. The fetus develops in this sac.
Amniotomy: Artificial rupture (bursting) of the amniotic sac.
Anesthesia: Relief of pain by loss of sensation.
Breech Presentation: A position in which the feet or buttocks of the fetus appear first during birth.
Cervix: The lower, narrow end of the uterus at the top of the vagina.
Cesarean Birth: Birth of a fetus from the uterus through an incision (cut) made in the woman's abdomen.
Chorioamnionitis: A condition during pregnancy that can cause unexplained fever with uterine tenderness, a high white blood cell count, rapid heart rate in the fetus, rapid heart rate in the woman, and/or foul-smelling vaginal discharge.
Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Eclampsia: Seizures occurring in pregnancy or after pregnancy that are linked to high blood pressure.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Fibroids: Growths that form in the muscle of the uterus. Fibroids usually are noncancerous.
Genital Herpes: A sexually transmitted infection (STI) caused by a virus. Herpes causes painful, highly infectious sores on or around the vulva and penis.
Gestational Diabetes: Diabetes that starts during pregnancy.
Hemorrhage: Heavy bleeding.
Hormone: A substance made in the body that controls the function of cells or organs.
Hypertension: High blood pressure.
Intravenous (IV) Line: A tube inserted into a vein and used to deliver medication or fluids.
Kidneys: Organs that filter the blood to remove waste that becomes urine.
Laminaria: Slender rods made of natural or synthetic material that expand when they absorb water. Laminaria are inserted into the opening of the cervix to widen it.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women's health.
Oxytocin: A hormone made in the body that can cause contractions of the uterus and release of milk from the breast.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Placenta Previa: A condition in which the placenta covers the opening of the uterus.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain over the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Prelabor Rupture of Membranes (PROM): Rupture of the amniotic membranes that happens before labor begins. Also called premature rupture of membranes.
Prostaglandins: Chemicals that are made by the body that have many effects, including causing the muscles of the uterus to contract, usually causing cramps.
Umbilical Cord: A cord-like structure containing blood vessels. It connects the fetus to the placenta.
Uterus: A muscular organ in the female pelvis. During pregnancy, this organ holds and nourishes the fetus. Also called the womb.
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).
- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.
- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery.
 Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
Induction of labor or induction of labor
The purpose of this informational material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix of the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body.
 It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
It prepares the body for childbirth, under its action the cervix becomes softer and begins to open. - Balloon Catheter - A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already dilated sufficiently, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions).
 The dose of the drug can be increased as needed to achieve regular uterine contractions.
The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.
- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.
Induction of labor, compared with spontaneous labor, increases the risk of prolonged labor, the need for instrumentation
(use of vacuum or forceps), postpartum hemorrhage, uterine rupture, the onset of too frequent uterine contractions and the associated deterioration of the fetus, prolapse umbilical cord, as well as premature detachment of the placenta.
If induction of labor is not successful
The time frame for induction of labor varies from patient to patient, on average labor begins within 24-72 hours. Sometimes more than one method is required.
The methods used do not always work equally quickly and in the same way on different patients. If the cervix does not dilate as a result of induction of labor, your doctor will tell you about your next options (which may include inducing labor later, using a different method, or delivering by caesarean section).
ITK833
This informational material was approved by the Women's Clinic on 01/01/2022.
Harbingers of childbirth - How to understand that it is time to go to the hospital?
January 10, 2017
Alekseeva Inna
Obstetrician-gynecologist, Doctor of the highest category
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www.instagram.com/roddompravda/
Tips and opinions from leading child professionals: https://www.instagram.com/emc.child/
Every pregnant woman with excitement and joy awaits the upcoming birth. The closer the cherished date, the more attentively the expectant mother listens to the changes taking place in her body and in the behavior of the baby. Of course, the expectant mother wants to know by what signs it is possible to understand that childbirth is just around the corner.
It is customary to call the harbingers of childbirth external, really tangible changes in the body, which are direct preparation for the onset of labor. The tissues of the birth canal - the cervix, vagina, vulva, perineum - become quite elastic, extensible, but at the same time - very strong and resistant to tearing. The cervix is located in the center of the vaginal vault, shortens by almost half its normal length and softens significantly. The cervical canal - the lumen of the cervix connecting the uterine cavity with the vagina - opens slightly, as a result, the diameter of the cervical canal is approximately 2-2.5 cm. Of course, such a significant "perestroika" takes more than one day.
Female sex hormones are responsible for preparing for childbirth. During the nine months of pregnancy, progesterone "reigns" in the body of the expectant mother. It ensures the normal tone of the uterus (relaxed state of the muscles), the production of cervical mucus - a mucous plug in the cervix that protects the fetus from infection. The amount of progesterone during pregnancy largely determines the normal development and growth of the fetus, the necessary concentration of nutrients and oxygen in the mother's blood, as well as their timely and uninterrupted delivery to the baby.
The amount of progesterone during pregnancy largely determines the normal development and growth of the fetus, the necessary concentration of nutrients and oxygen in the mother's blood, as well as their timely and uninterrupted delivery to the baby.
Shortly before childbirth, the production of progesterone decreases markedly, it is replaced by estrogens - female sex hormones. The increase in estrogen in the blood is caused by the need to prepare the body for the upcoming birth. It is these hormones that are responsible for the elasticity and patency of the birth canal. The rate of cervical dilatation in the first stage of labor depends on them. In the second period, when the cervix is fully opened and the fetus passes through the birth canal, it is also very important how elastic and extensible the walls of the vagina are - this will largely determine the duration of the straining period. Finally, the onset of labor itself depends on the level of estrogen: contractions occur as a result of a nerve impulse that is caused by a certain level (“peak”) of estrogen accumulation.
These changes are normal and do not require an unscheduled visit to the doctor or hospitalization. Harbingers of childbirth are manifestations of a planned restructuring in the body of a future mother, the “finishing touches” of preparation for the upcoming joyful event.
The absence of clearly perceptible changes on the eve of the expected date of birth is also not a pathology. Not all expectant mothers note those changes in well-being that are commonly called harbingers. However, this does not mean that there is no preparation. In some cases, the “final preparations” go unnoticed by the pregnant woman. Therefore, do not worry or urgently contact a specialist.
The appearance of any of the "harbingers" indicates the likelihood of the development of regular labor activity over the next two hours - two weeks. None of the sensations described gives a 100% guarantee that a woman will become a mother within the next 24 hours. Hormonal changes before childbirth begin approximately two weeks before the expected birth. Theoretically, during these two weeks, at any time, a pregnant woman can notice certain changes in her state of health. Consequently, the absence of labor activity an hour, a day, or even a week after the first noted changes is not a pathology and does not require special medical advice.
Theoretically, during these two weeks, at any time, a pregnant woman can notice certain changes in her state of health. Consequently, the absence of labor activity an hour, a day, or even a week after the first noted changes is not a pathology and does not require special medical advice.
- Scarlet discharge from the genital tract in any amount.
- Severe abdominal pain.
- Increased blood pressure (above 130/80 mmHg).
- An increase in body temperature to 37.5 ° C and above.
- Increased heart rate (more than 100 beats per minute).
- Severe headache, vomiting, blurred vision.
- Significant increase in edema.
- Absence, sharp decrease, sharp increase in fetal movements.
- Suspected amniotic fluid leakage.
Weight loss . Shortly before the expected date of delivery, the expectant mother may notice some “weight loss”. Weight loss during this period is associated with the removal of excess fluid from the body, that is, a general decrease in edema. The more pronounced the fluid retention during pregnancy, the more mass the pregnant woman will “lose” on the eve of childbirth. During pregnancy, water is retained in the body of all expectant mothers to a greater or lesser extent. The reason is progesterone - a hormone whose main function is to support the processes of pregnancy. Before childbirth, progesterone is replaced by estrogen. It is estrogen that removes excess fluid from the body. The first results are visible on the hands, feet and legs. Depending on the severity of edema, weight loss before childbirth varies from 0.5 to 2.5 kg.
Weight loss during this period is associated with the removal of excess fluid from the body, that is, a general decrease in edema. The more pronounced the fluid retention during pregnancy, the more mass the pregnant woman will “lose” on the eve of childbirth. During pregnancy, water is retained in the body of all expectant mothers to a greater or lesser extent. The reason is progesterone - a hormone whose main function is to support the processes of pregnancy. Before childbirth, progesterone is replaced by estrogen. It is estrogen that removes excess fluid from the body. The first results are visible on the hands, feet and legs. Depending on the severity of edema, weight loss before childbirth varies from 0.5 to 2.5 kg.
Change of stool. Increased frequency and change in the consistency of physiological functions on the eve of childbirth is also associated with an increase in estrogen levels and the removal of fluid from the body of the expectant mother. Similar changes in the body of a non-pregnant woman are observed during menstruation. The chair can become more frequent up to 2-3 times a day, at the same time there may be some liquefaction of the feces. More frequent urge to defecate, a sharp change in the color and smell of feces, combined with nausea and vomiting, is a reason for consulting a doctor - food poisoning can be masked under such "harbingers".
Similar changes in the body of a non-pregnant woman are observed during menstruation. The chair can become more frequent up to 2-3 times a day, at the same time there may be some liquefaction of the feces. More frequent urge to defecate, a sharp change in the color and smell of feces, combined with nausea and vomiting, is a reason for consulting a doctor - food poisoning can be masked under such "harbingers".
Fundal prolapse. Shortly before delivery, the baby presses the presenting part (most often the head) against the lower segment of the uterus and pulls it down, pressing against the entrance to the small pelvis. The fetus "groups", taking the most advantageous position for itself at the time of the onset of contractions. As a result of such "preparations" from the side of the fetus, the uterus "sags", and its upper part - the bottom - ceases to exert pressure on the internal organs. After lowering the bottom of the uterus, the pregnant woman has no shortness of breath (it becomes easier to breathe, there is a feeling of a full breath). If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part. Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent.
If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part. Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent.
Isolation of the mucous plug. During pregnancy, the glands of the mucous membrane of the cervical canal (the lumen of the cervix) secrete a special secret. It is a thick, sticky, jelly-like mass that forms a kind of cork. The mucous plug completely fills the cervical canal, preventing the penetration of bacterial flora from the vagina into the uterine cavity. Thus, cervical mucus, or the mucous plug of the cervix, protects the fetus from ascending infection. Before childbirth, when the cervix begins to soften under the influence of estrogen, the cervical canal opens slightly and the cervical mucus contained in it can be released. In this case, the expectant mother may find small clots of yellowish-brownish mucus, transparent, jelly-like, odorless. The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases.
Thus, cervical mucus, or the mucous plug of the cervix, protects the fetus from ascending infection. Before childbirth, when the cervix begins to soften under the influence of estrogen, the cervical canal opens slightly and the cervical mucus contained in it can be released. In this case, the expectant mother may find small clots of yellowish-brownish mucus, transparent, jelly-like, odorless. The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases.
Training contractions. Training or false contractions are called such contractions that appear shortly before childbirth and are not actually labor activity, since they do not lead to the opening of the cervix. A contraction is essentially a single contraction of the uterine wall; this contraction usually lasts a few seconds. At the time of the contraction, the expectant mother feels a gradually increasing and then gradually decreasing tension in the abdomen. If at this moment you put your hand on your stomach, you can notice that the stomach becomes very hard, but after the contraction it completely relaxes and becomes soft again. In addition to involuntary tension of the uterus, other changes in the well-being of the expectant mother during false contractions are usually not noted. It is not difficult to distinguish training fights from real ones. In most cases, false contractions are weak, painless, irregular or alternating at a significant interval (30 minutes or more).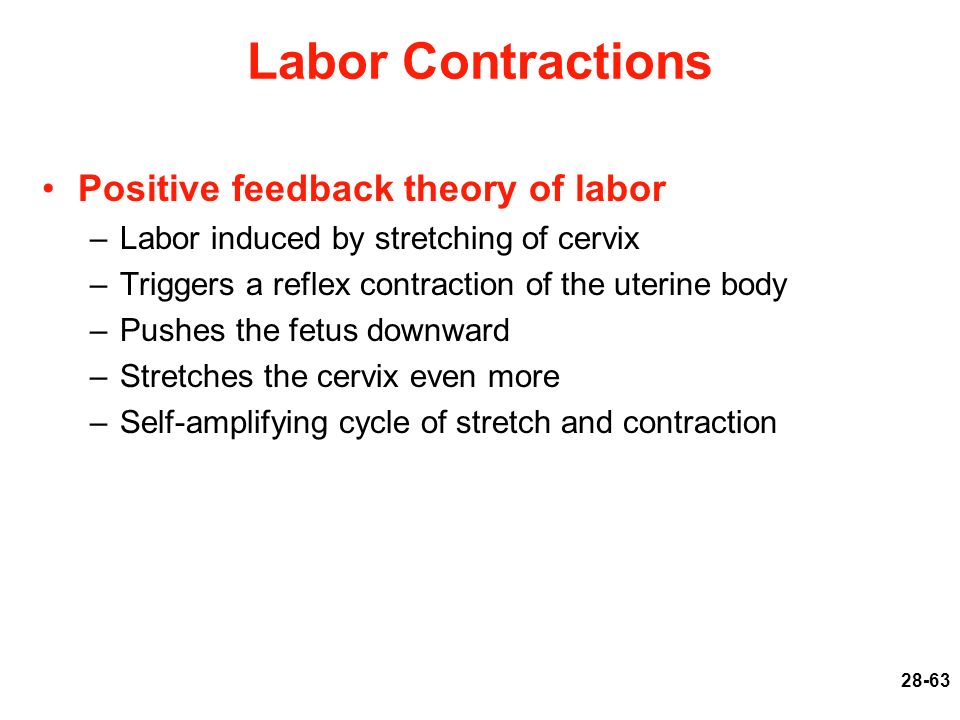 Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization. False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days.
Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization. False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days.
Discomfort. In the last weeks before giving birth, many pregnant women report discomfort in the lower abdomen and in the area of the sacrum (the area slightly below the waist). Such changes in
the well-being of the expectant mother is caused by sprain of the pelvic ligaments and increased blood flow to the pelvic organs. Usually these minor sensations, described as a feeling of "light languor" in the lower abdomen, are comparable to similar phenomena in the period before or during menstruation.