Is it normal not to have braxton hicks
Is It Normal To Not Have Braxton Hicks
Pregnancy is one of the most exciting journeys that women take. There are different stages that you will have to go through before getting to the delivery date. False labor tends to be a part of this journey, known as Braxton Hicks contractions. So is it normal to not have Braxton hicks? Yes, it is perfectly normal for you not to have false labor pains. Ideally, the contractions occur as a way for the body to prepare itself for the actual thing. However, it is essential to note that this does not mean that labor has started.
Braxton hicks are sometimes referred to as practice contractions, and some women may not notice them. The uterus muscles will flex and relax in readiness for the actual labor and delivery. There is also a group of women who do not know what the Braxton Hick contractions feel like. Every pregnant woman may have a unique journey, which is why some may wonder, is it normal not to have Braxton hicks? In some cases, the contractions are painless. However, for women who have had other deliveries in the past, the contraction may be quite intense.
Our regular advice to to-be moms is that they should not ignore any unusual thing that happens to them during the pregnancy; always talk to your doctor about such concerns.
At What Point Should I Expect Braxton Hicks?Is it normal to not have Braxton hicks? This has become a standard question, especially among first-time moms. Braxton hicks are unique to every mom, and the experiences will vary. Some women do not even know what the contractions feel like. Some women will end up experiencing contractions during actual labor and childbirth. This is normal, and there is nothing to worry about.
Experts refer to Braxton hicks as a warm-up or practice contractions, and it is perfectly normal not to have them. In most cases, they will start in the final trimester of the pregnancy. Some moms may start feeling the contractions as early as 20 weeks, while others may not experience them at all. For mothers who have had prior deliveries, Braxton hicks tend to start earlier.
For mothers who have had prior deliveries, Braxton hicks tend to start earlier.
In trying to answer, “is it normal to not have Braxton hicks?” is important to know how they feel. Generally, this feels like abdomen muscles are being tightened. The majority of women compare this to moderate menstrual cramps. Whereas these contractions may be uncomfortable, they will not cause you to dilate or get into actual labor. Getting or not getting Braxton hicks is absolutely normal, and the experiences vary from woman to woman.
Every Pregnancy Is Different!Many first-time moms ask, is it normal to not have Braxton hicks? As we have established, it is normal not to get the dress rehearsal for the actual delivery. In any case, the practice contractions are usually triggered, so they may not show up in every pregnancy.
Back to News - EliteBaby BlogUse left/right arrows to navigate the slideshow or swipe left/right if using a mobile device
No Braxton Hicks Contractions At 39 Weeks
Braxton Hick contractions are known as practice contractions or false labor. Whether it is your first pregnancy or a subsequent one, these contractions can happen when you least expect them. On the other hand, it is also possible to not experience them. If you have no Braxton Hicks contractions at 39 weeks, there is no cause for alarm. Experts say that these types of contractions are meant to prepare the body for labor and delivery. At whatever stage of your pregnancy, you are in, when they happen, you may find yourself rushing to the hospital. In some cases, they will happen in a very mild manner that you may not even notice them.
Whether it is your first pregnancy or a subsequent one, these contractions can happen when you least expect them. On the other hand, it is also possible to not experience them. If you have no Braxton Hicks contractions at 39 weeks, there is no cause for alarm. Experts say that these types of contractions are meant to prepare the body for labor and delivery. At whatever stage of your pregnancy, you are in, when they happen, you may find yourself rushing to the hospital. In some cases, they will happen in a very mild manner that you may not even notice them.
Having no Braxton Hicks contractions at 39 weeks is fine as this does not affect you or your baby in any way. There are different myths that are propagated but the truth of the matter is that you will have no problems during labor and childbirth even if the Braxton Hicks do not happen. For most first-time mothers, it is possible to have false contractions and not even be aware. In other cases, there are some women who experience intense Braxton Hicks and this can be quite scary. Usually, most women compare these to the tightening of abdomen muscles and can be a little bit uncomfortable.
Usually, most women compare these to the tightening of abdomen muscles and can be a little bit uncomfortable.
Whatever the case, you do not have any reason to worry whether the warm-up contractions happen or not. They may happen towards the tail end of your pregnancy or not at all. There is no specific trend or pattern that they follow but mostly they will occur as you draw closer to the delivery date.
Do All Pregnant Women Experience Braxton Hicks?Most women will experience Braxton Hicks contractions. However, this will vary from woman to woman. In most cases, they will happen in the 3rd trimester but can also start as early as 22 weeks into the pregnancy. There are some women who will not feel this type of contraction until the actual one happens. As such, it is normal to get no Braxton Hicks contractions at 39 weeks. These contractions are quite mild in most cases and could even be painless.
In the final stages of the pregnancy, they may become stronger and some women confuse them with the actual labor.
If you have any concerns about the health of your unborn baby, it is imperative to talk to your doctor. The main difference between these contractions with the actual labor is the fact that the cervix will dilate in true labor. Having your doctor examine you is important so as to check if the cervix is opening up. In such a case, this means that you are getting into actual labor.
Final ThoughtsBraxton Hicks are different in every woman and can be confusing. However, even if there are no Braxton Hicks contractions at 39 weeks, you should not panic. Just go along with your pregnancy and wait for the main event to deliver your baby. Always speak to an expert in the event of unusual experiences.
Back to News - EliteBaby BlogUse left/right arrows to navigate the slideshow or swipe left/right if using a mobile device
Braxton Hicks contractions for how long - 25 recommendations on Babyblog.ru
For fifteen years now we have been living not just in the new century, but in the new millennium.![]() For twenty years we have been using computers and the Internet everywhere. It would seem that with the progress of technology, people have enormous opportunities for the exchange of progressive information, knowledge and best practices. But the real picture is almost the opposite: false, untruthful information, often presented under the “sauce” of intimidation and deceit, is spread and accepted by people faster and easier than truthful and useful information.
For twenty years we have been using computers and the Internet everywhere. It would seem that with the progress of technology, people have enormous opportunities for the exchange of progressive information, knowledge and best practices. But the real picture is almost the opposite: false, untruthful information, often presented under the “sauce” of intimidation and deceit, is spread and accepted by people faster and easier than truthful and useful information.
The worst thing that is now observed in medicine is the filing of many conditions, including quite normal ones, and some diagnoses as something terrible and dangerous, threatening a person’s life, requiring aggressive and extensive treatment immediately. Obstetrics is no exception. On the contrary, in recent years this branch of medicine has grown in a number of countries into a kind of machine of deliberate harm to a pregnant woman and her unborn child.
The concept of "commercial diagnosis", introduced by me ten years ago, is no longer denied by many people and is even used by them in everyday life, conversations and discussions of the situation in the healthcare system.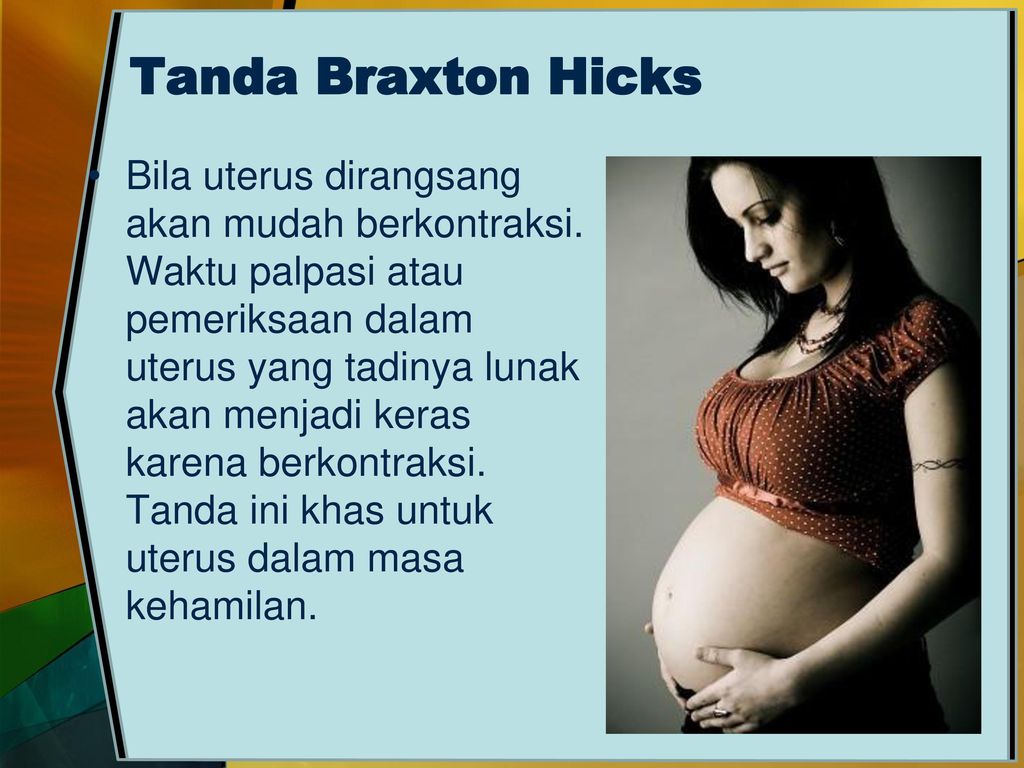 Both doctors and people of other specialties began to talk and write about obstetric aggression. Nevertheless, the number of fictitious diagnoses that do not exist in most countries of the world is striking not only by their backwardness, but also by the lack of a logical analysis of the situation, signs, and examination results when they are made (more precisely, invented).
Both doctors and people of other specialties began to talk and write about obstetric aggression. Nevertheless, the number of fictitious diagnoses that do not exist in most countries of the world is striking not only by their backwardness, but also by the lack of a logical analysis of the situation, signs, and examination results when they are made (more precisely, invented).
INCOMPATIBILITY OF THE SPOUSES
Usually such a diagnosis sounds when:
- unsuccessful planning of pregnancy and infertility;
- loss of pregnancy, even the first or one;
- spontaneous habitual miscarriages;
- in exceptionally "striking cases" in the presence of one child or several healthy children.
If we talk about some kind of “spousal incompatibility”, then we can only talk about psychological incompatibility or sexual temperaments, but there is no other “incompatibility”.
Allergic reaction to semen is extremely rare in humans, but the diagnosis would be allergy, not incompatibility.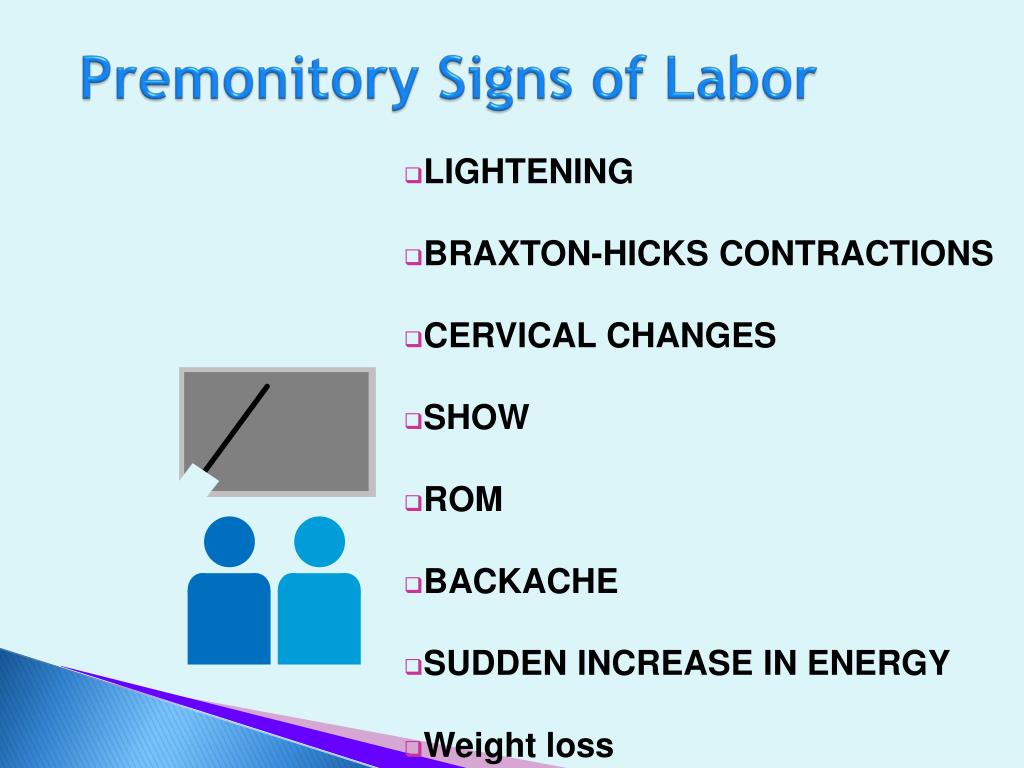
If a married couple cannot conceive, it may be infertility, which requires proper diagnosis. There are different types of infertility or infertility factors, which means that there will be a different approach to the examination of a married couple and treatment.
Very fashionable commercial HLA (human leukocyte antigen) testing in the world of progressive medicine is used in organ and tissue transplantation, to diagnose a number of autoimmune diseases, confirm paternity and monitor the effectiveness of the treatment of a number of diseases, but has nothing to do with conceiving children, carrying a pregnancy , and even more so with the "incompatibility of the spouses." "Genetic incompatibility of partners" is another invention for imposing an expensive examination and treatment.
If one of the partners has affected genes, that is, there are changes in the form of mutations, then such changes may be associated with problems in conceiving and bearing offspring, but this is not incompatibility.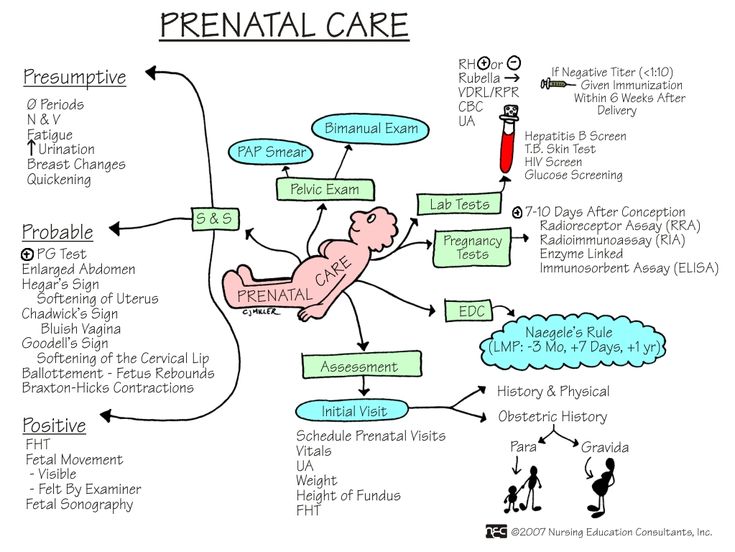 This may be a specific diagnosis (disease, syndrome) on the part of one or both partners. And the recommendations of some doctors to carry out IVF in such cases using the same sexual material, or to find a sexual partner outside of marital relations in order to conceive a child, do not always sound professional.
This may be a specific diagnosis (disease, syndrome) on the part of one or both partners. And the recommendations of some doctors to carry out IVF in such cases using the same sexual material, or to find a sexual partner outside of marital relations in order to conceive a child, do not always sound professional.
TOXICOSIS
The concept of "toxicosis" appeared in Soviet obstetrics in the early 1990s, when everyone in the world of progressive medicine had already completely abandoned this concept. Toxicosis means “a state of poisoning” (toxins are poison), and the logical conclusion is that this is pregnancy poisoning, that is, the embryo / fetus poisons the body, and therefore the life of the expectant mother. But doesn’t a mother poison her unborn child with poor-quality food, water, medication, smoking, and even drinking alcohol?
In the West, they quickly realized the absurdity of such a “diagnosis” and tried to switch to the concept of “preeclampsia”, that is, a condition associated with gestation (pregnancy). However, this definition was also abandoned very quickly, because the more science and medicine developed, the faster the exchange of advanced information and experience, the faster doctors began to understand that many “strange” phenomena during pregnancy are not diseases, but variants of the norm. and vice versa - all complications of pregnancy have specific specific names, which should appear as diagnoses.
However, this definition was also abandoned very quickly, because the more science and medicine developed, the faster the exchange of advanced information and experience, the faster doctors began to understand that many “strange” phenomena during pregnancy are not diseases, but variants of the norm. and vice versa - all complications of pregnancy have specific specific names, which should appear as diagnoses.
In post-Soviet medicine, a completely normal phenomenon - nausea and vomiting at the beginning of pregnancy - is still called early toxicosis (in the rest of the world these are just unpleasant symptoms of this condition), and edema, which for the vast majority of women are normal, hypertension in pregnant women, preeclampsia, eclampsia and about ten other complications of pregnancy, which are independent diagnoses, and not a comprehensive mythical toxicosis.
Remember: there is no such diagnosis - toxicosis!
UTERINE TONE / HYPERTONE
For the first time, normal uterine contractions from the beginning of pregnancy to the end of childbirth were described by the English physician John Braxton Hicks in 1872. Mistakenly, such contractions are called "training bouts", which is not true. In the publication of this doctor, it was about normal uterine contractions throughout pregnancy, and not before childbirth.
Mistakenly, such contractions are called "training bouts", which is not true. In the publication of this doctor, it was about normal uterine contractions throughout pregnancy, and not before childbirth.
The uterus is a muscular organ, therefore, just like any muscle, it has its own mode of contractions, which depends on many factors and can be observed both outside of pregnancy and during pregnancy.
The diagnosis of "tonus" or "hypertonicity" was invented by post-Soviet ultrasound doctors and the rest of the world does not exist in obstetrics, therefore it does not require treatment, and even more so inpatient, with the use of a large number of drugs that have also not been used in modern obstetrics for a long time ("Papaverine" , "No-shpa", "Viburkol", vitamin E, magnesia, etc.)
THREAT OF LOSS OF PREGNANCY
I have already raised the topic of "threat of abortion" more than once, especially since it is consonant with the topic of "preservation of pregnancy". In reality, the threat to a pregnant woman comes more from the medical staff than really from someone else or something (nature), because it is people who intimidate, put pressure on the psyche with negative scenarios, escalate the situation, harm with unsafe treatment.
In reality, the threat to a pregnant woman comes more from the medical staff than really from someone else or something (nature), because it is people who intimidate, put pressure on the psyche with negative scenarios, escalate the situation, harm with unsafe treatment.
The only diagnosis in obstetrics that has a word root consonant with “threat” is “threatened abortion”. This diagnosis is made according to strict criteria, and not because of “tone / hypertonicity of the uterus”, it does not require treatment, because there is no cure.
All other types of threats are fictitious diagnoses. In obstetrics, it is customary to talk about risk factors and determine the group or degree of risk for the development of one or another pregnancy complication (low risk, high risk). Against the background of the presence of various risk factors, pregnancy can proceed quite normally and end safely.
RH AND GROUP CONFLICT
In modern obstetrics there is no such concept or diagnosis as "Rh conflict" or "group conflict".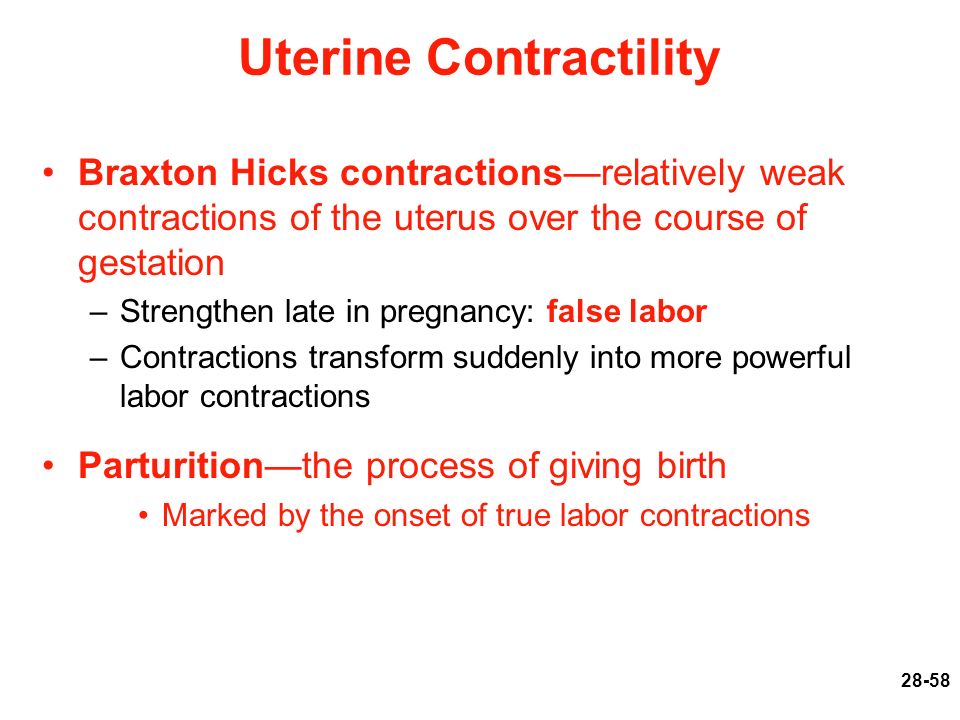 Worst of all, such a “diagnosis” intimidates a married couple to such an extent that she refuses to conceive children: since it is absolutely impossible to get pregnant, then we are not trying. The presence of different blood types, as well as different Rh factors, is a normal phenomenon in human life and is not considered any conflict.
Worst of all, such a “diagnosis” intimidates a married couple to such an extent that she refuses to conceive children: since it is absolutely impossible to get pregnant, then we are not trying. The presence of different blood types, as well as different Rh factors, is a normal phenomenon in human life and is not considered any conflict.
In modern obstetrics, there are more than 50 blood markers (antigens) for which antibodies (immunoglobulins) can be produced, and this condition is called alloimmunization, or sensitization.
During pregnancy, antibodies can be produced in the mother's body against fetal antigens, cross the placenta and destroy the fetal red blood cells, leading to anemia and fetal hemolytic disease. If hemolytic disease of the fetus occurs, then it will end either with the death of the fetus, or the birth of a child with hemolytic disease of the newborn. Unfortunately, many doctors do not understand the types of jaundice, do not know the current norm of bilirubin levels, so the diagnosis of "hemolytic disease of the newborn" in most cases turns out to be false, which means that aggressive treatment of such children is absolutely inappropriate.
If we talk about really rare "blood conflicts", then they arise not between a man and a woman, but between a mother and a fetus. Therefore, the enthusiasm of some doctors for the search for antibodies in the blood of a man is so surprising. Also depressing is the fact of searching for antibodies in the mother's blood after childbirth in order to make a diagnosis of "hemolytic disease of the newborn." And the use of such a dangerous procedure as plasmapheresis, supposedly to “cleanse the blood” of antibodies, is shocking. This procedure has passed into the category of commercial ones, because it is expensive and brings considerable income to those who carry it out.
For the prevention of Rh sensitization in the mother, vaccination with immunoglobulins (D-antibodies) has long been used, which is carried out in the absence of a woman's own antibodies during pregnancy, after childbirth, abortion, and a number of procedures. This prophylaxis does not protect the current pregnancy, but it does prevent hemolytic disease of the fetus and newborn in subsequent pregnancies. However, it is ineffective in preventing sensitization for all other blood markers.
However, it is ineffective in preventing sensitization for all other blood markers.
HEREDITARY (GENETIC) THROMBOPHILIA
In post-Soviet obstetrics, over the past decade, there have been an extremely large number of positions of geneticists who do not understand prenatal genetic screenings and genetics in general, and hematologists (they are fashionably called hemostesiologists, hemastesologists), who do not understand blood and know absolutely nothing about normal changes in the composition of the blood, especially the blood coagulation system in pregnant women.
During pregnancy, blood viscosity increases despite an increase in blood (plasma) volume and a decrease in the concentration of many substances. Therefore, from the very first weeks, pregnancy is accompanied by a hypercoagulable state. It can persist for several weeks, not only after childbirth, but also after abortions and missed pregnancies. This is not a pathological condition, but normal physiological changes.
D-dimer, according to the level of which heparin is prescribed to all pregnant women in a row, is a derivative of fibrinogen. Both of these indicators increase from the first weeks of pregnancy, which is absolutely normal.
Commercially profitable genetic testing leads to the diagnosis of thrombophilia being overused, although several dozen diseases are known to be associated with disorders of the blood clotting process. There are several types of hereditary thrombophilia that have a clear name, and not just "genetic thrombophilia". There are also acquired thrombophilias, which often turn out to be not a separate diagnosis, but a laboratory and clinical symptom of other diseases.
The presence of genes and their combinations does not mean that a person has thrombophilia (and many other diseases). This may indicate a hereditary predisposition, but without clinical and laboratory confirmation, and even more so outside the state of pregnancy, such diagnoses are not made and blood thinning drugs are not prescribed.
Bed rest in hospitals, where pregnant women are kept for weeks and even months, is recognized as the most dangerous factor in the formation of blood clots. It is also surprising that before pregnancy, many women had no idea about their "genetic disease", they took hormonal contraceptives that are incompatible with thrombophilia, and then after giving birth they continue to take them, forgetting about the terrible diagnosis. However, doctors quickly forget about him too.
OLD PLACENTA
The diagnosis of "old placenta", which often sounds in conjunction with the diagnosis of "uteroplacental insufficiency", was born by the same ultrasound specialists.
The placenta is a dynamic organ that undergoes regular changes as pregnancy progresses. Therefore, we can safely say that not only the placenta is aging, but also the fetus itself. The woman also gets older by 9 months!
Placenta insufficiency can be spoken of only when it does not fulfill its function. Just as there is heart or liver failure, placental failure can also exist.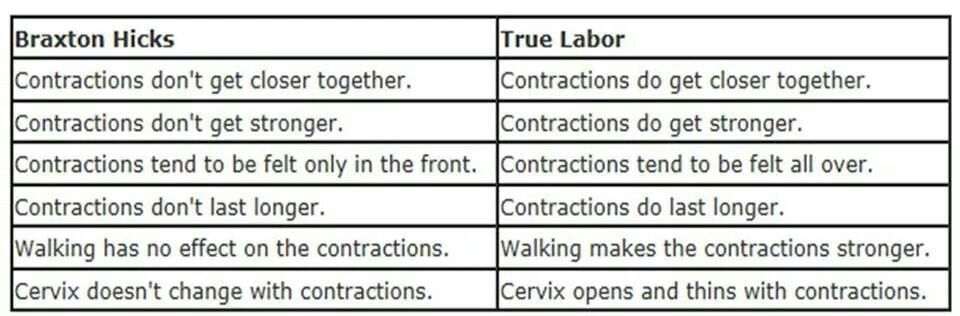 But its presence can only be determined by the state of the fetus. If the fetus develops normally and does not lag behind in growth (for this, growth charts must be kept and the exact gestational age must be known), then what kind of placental insufficiency can we talk about?
But its presence can only be determined by the state of the fetus. If the fetus develops normally and does not lag behind in growth (for this, growth charts must be kept and the exact gestational age must be known), then what kind of placental insufficiency can we talk about?
But what is depressing in all these stories with placentas is that a woman is offered different schemes for "rejuvenation" of the placenta, which necessarily include two fuflomycins - "Kurantil" and "Actovegin". Remember: the placenta cannot be rejuvenated!
In addition, the diagnosis "placentitis" suddenly became fashionable, which was indeed used in veterinary medicine for a very long time, but never in obstetrics! Turning pregnant women into female animals?
oligohydramnios/polyhydramnios tendencies
When I hear or read about the diagnosis of oligohydramnios/polyhydramnios tendency, I want to respond with a great sense of humor: “You know, we all have a lot of tendencies. For example, there is a real tendency with age to get senile dementia. You can buy a lottery ticket - there will be a tendency to enrich. We sit in a car, drive along a highway - we tend to get into a traffic accident and even die. That's right, life tends to end. This means that pregnancy tends to end in term birth and the birth of a healthy baby.
You can buy a lottery ticket - there will be a tendency to enrich. We sit in a car, drive along a highway - we tend to get into a traffic accident and even die. That's right, life tends to end. This means that pregnancy tends to end in term birth and the birth of a healthy baby.
The extremely common diagnosis of "trends" is often the product of ultrasound specialists who somehow do not use the logical thinking of obstetrician-gynecologists to ask a simple question: what kind of nonsense is this?
The state of amniotic fluid is only in the form of a norm, polyhydramnios and oligohydramnios, but there are no trends. These conditions are determined by measuring one pocket (column) of amniotic fluid in centimeters, but most often by the sum of four (namely four, not two or three) pockets, that is, by determining the amniotic index of amniotic fluid (AIF). After 20 weeks, the normal AIH ranges from 8 to 24 cm, of course, adjusted for the condition of the fetus and other ultrasound findings.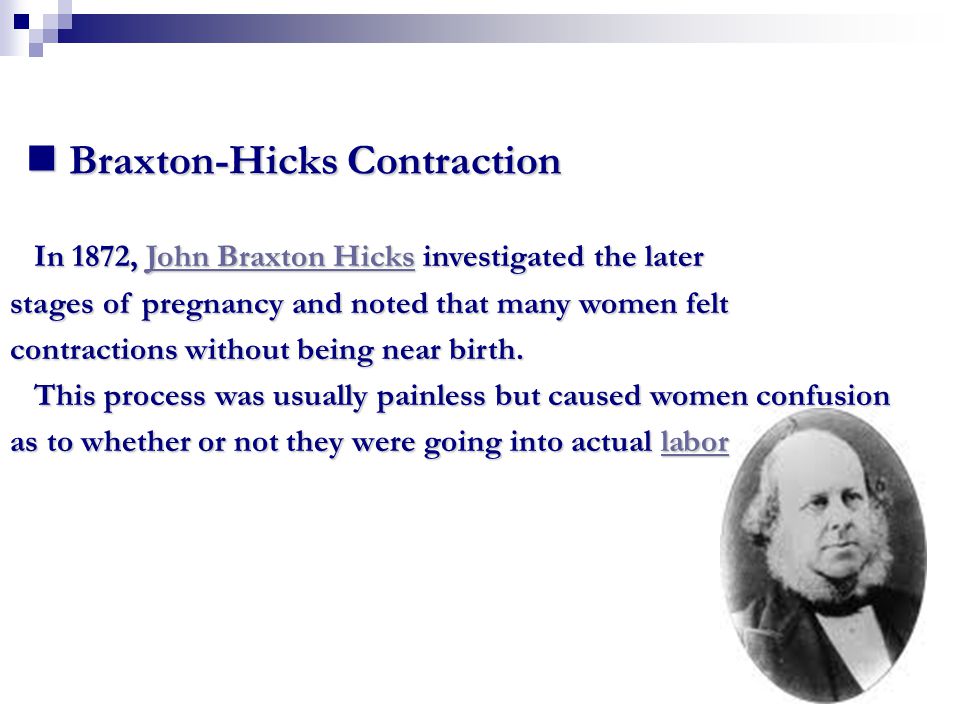
Oligohydramnios and polyhydramnios are practically not treated, therefore, volumetric regimens of antibiotics and fuflomycins, the same "Kurantil", "Actovegin", "Khofitol", "Viferon", "Tivorin" and other similar drugs, and with the obligatory presence of a pregnant woman in a hospital , is a manifestation of medical illiteracy.
fetal asphyxia
Most often, the diagnosis of fetal asphyxia appears in the conclusions of pathologists after pregnancy loss, as well as in stillbirth. Surprisingly, it is specialists who do not see the difference between hypoxia and asphyxia, who are just obliged to find out the cause of abortion and fetal death.
The baby is not breathing inside the uterus. His lungs don't work. Everything he receives from his mother in the form of nutrients and oxygen comes through the umbilical cord. The concept of hypoxia implies a violation of blood flow in the vessels of the fetus (impaired hemodynamics) due to the presence of usually two parallel conditions - anemia (anemia) and acidosis (increased acidity) due to oxygen starvation of tissues.
Asphyxia is understood as suffocation, which is associated with a decrease and even cessation of oxygen supply through the respiratory system. At the same time, the oxygen content in the blood drops sharply, which leads to brain death and death. Since the fetus is not breathing, it cannot have asphyxia.
Asphyxia of a newborn is said when a foreign body (amniotic fluid, mucus, meconium, blood, etc.) enters the child's respiratory tract after birth with the first or subsequent breaths. Therefore, the diagnosis of "fetal asphyxia" simply does not exist, and if it is present in the conclusions of the pathoanatomical examination (autopsy), this indicates the unprofessionalism of the doctor.
Braxton-Hicks contractions. How to distinguish between false and real contractions?
Braxton-Hicks contractions or false labor contractions are irregular contractions and relaxation of the muscles of the uterus as a way of preparing for true labor. They are thought to start around 6 weeks of gestation but are not usually felt until the 2nd or 3rd trimester.
False contractions are a normal part of pregnancy. They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves.
They are also irregular in duration and intensity, occur infrequently, are unpredictable and not rhythmic, and are more uncomfortable than painful.
Braxton Hicks contractions tend to increase in frequency and intensity towards the end of pregnancy. Women often mistake Braxton Hicks contractions for real labor. However, unlike real contractions, they do not dilate the cervix and result in the birth of a baby.
Braxton Hicks contractions occur when the muscle fibers of the uterus contract and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are circumstances that can cause them:
- when the woman is very active,
- when the bladder is full,
- after sexual activity,
- when a woman is dehydrated.
Common among all these circumstances is the potential stress on the fetus and the need for increased blood flow to the placenta to provide oxygen to the fetus.
- Change position or activity level: if you were very active, lie down; if you have been sitting for a long time, go for a walk.
- Relax: take a warm bath, massage, read a book, listen to music or take a nap.
If you have Braxton Hicks contractions or if they continue and become more frequent and intense, you should see your doctor.
When assessing for Braxton Hicks contractions, there are a few key questions to ask yourself. We have prepared a table for you with questions, the answers to which will help you understand what kind of contractions you have:
| Braxton Higgs contractions | Real labor pains | |
|---|---|---|
| How often do contractions occur? | Irregular and do not increase over time.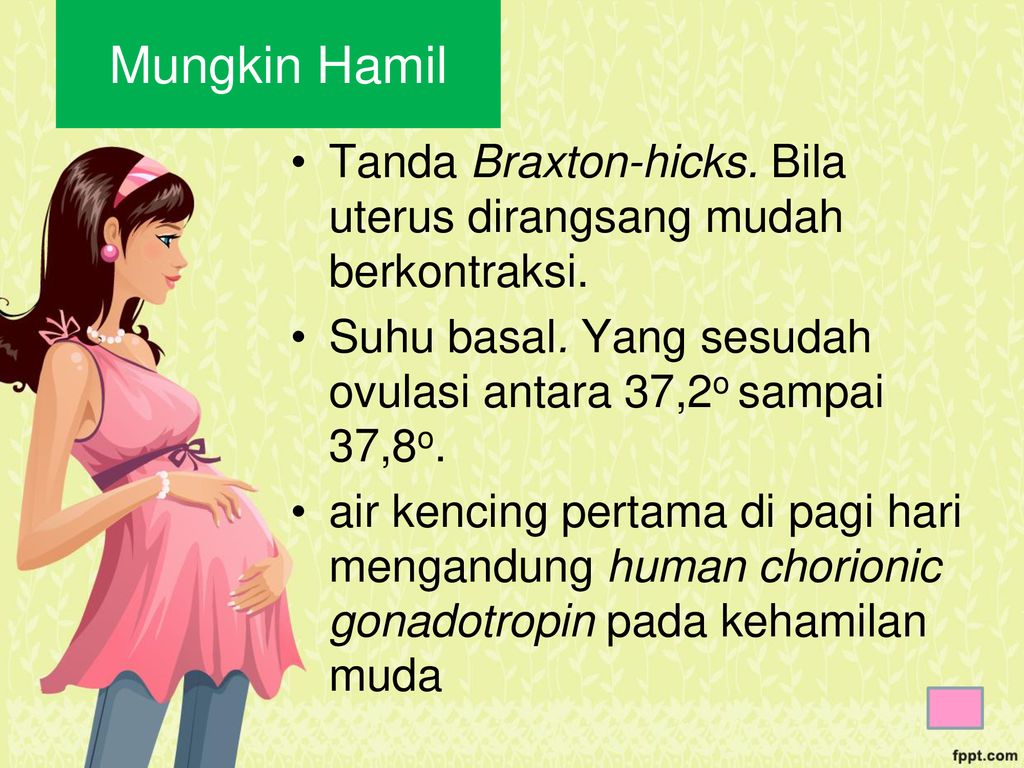 |