How far along can you have a miscarriage
Miscarriage, stillbirth and ectopic pregnancy
Some medical issues can happen during pregnancy that are beyond your control. Sometimes this can lead to the death of the child before it is born.
Miscarriage
If a pregnancy ends before 24 weeks, it is known as a miscarriage. Miscarriages are quite common in the first three months of pregnancy. At least one in six confirmed pregnancies end in miscarriage.
Many miscarriages which occur early in pregnancy (before 14 weeks) are a result if developmental problems with the baby.
There are other potential causes, such as hormonal or blood-clotting problems.
Later miscarriages can be caused by:
- infection
- problems in the placenta
- the cervix being too weak and opening too early in the pregnancy
A miscarriage in the first few weeks of pregnancy may start like a period, with spotting or bleeding accompanied by mild cramps or back pain. The pain and bleeding may get worse and there can be quite severe cramping pains.
If miscarriage happens later in pregnancy, you may go through an early labour. If you bleed or begin to have pains at any stage of your pregnancy, you should contact your GP or midwife.
Some women find out that their baby has died only when they go for a routine scan. If they have not experienced any pain or bleeding, this can be a terrible shock, especially if the scan shows the baby died days or weeks before. This is sometimes called a missed or silent miscarriage.
Treatment for miscarriage
Sometimes it’s preferable to wait and let the miscarriage happen naturally, but there are three ways to actively manage a miscarriage, including:
- medicine – you may be offered tablets or pessaries to start the process of miscarriage
- surgery – if you have been pregnant for less than 14 weeks, your doctor may recommend an operation called an ERPC (evacuation of retained products of conception)
- induced labour – if your baby dies after 14 weeks, you may go into labour and, although many women would prefer not to go through labour, it is safer than an operation to remove the baby
- Find out more about miscarriages
Recurrent pregnancy loss
Your healthcare professional may consider a diagnosis of recurrent miscarriage or recurrent pregnancy loss after the loss of two or more pregnancies. Normally you will be referred to a clinic following the loss of three pregnancies.
Normally you will be referred to a clinic following the loss of three pregnancies.
There are several factors involved in this, including:
- your age
- how far along your pregnancy was
- your past medical history
For more information on recurrent pregnancy loss follow the link below to the Public Health Agency website .
- Recurrent Pregnancy Loss patient information booklet
Stillbirth and neonatal death
In the UK, about 4,000 babies are stillborn every year. Stillbirth is when a pregnancy has lasted for at least 24 weeks and the baby is dead when it is born. About the same number of babies die after birth, often without a clear cause.
Sometimes a baby dies in the uterus (an intra-uterine death or IUD), but labour does not start spontaneously. If this happens, you will be given medicines to induce labour. This is the safest way of delivering the baby. It also gives you and your partner the chance to see and hold the baby at birth, if you want to.
- Find out more about stillbirth
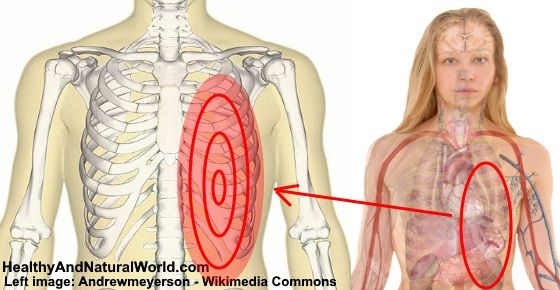
Ectopic pregnancy
An ectopic pregnancy occurs when a pregnancy develops outside of the womb, usually in one of the fallopian tubes. An ectopic embryo will not survive and the pregnancy will miscarry.
The consequences of an ectopic pregnancy can be serious and even life-threatening. It is important to get medical advice immediately if you could be pregnant and experience any of the symptoms of ectopic pregnancy.
- Find out more about ectopic pregnancy
More useful links
- Death and bereavement
- Registering a stillbirth
- Cruse Bereavement Care
- Time off for dependants (compassionate leave)
- Bereavement Network (Health and Social Care Trust website)
Help improve this page - send your feedback
You must have JavaScript enabled to use this form.
What do you want to do?report a problem
leave feedback
ask a question
Report a problemWhich problem did you find on this page? (Tick all that apply)
A link, button or video is not working
There is a spelling mistake
Information is missing, outdated or wrong
I can't find what I'm looking for
Another issue
Messages
Tell us more about the problem you're having with the nidirect website.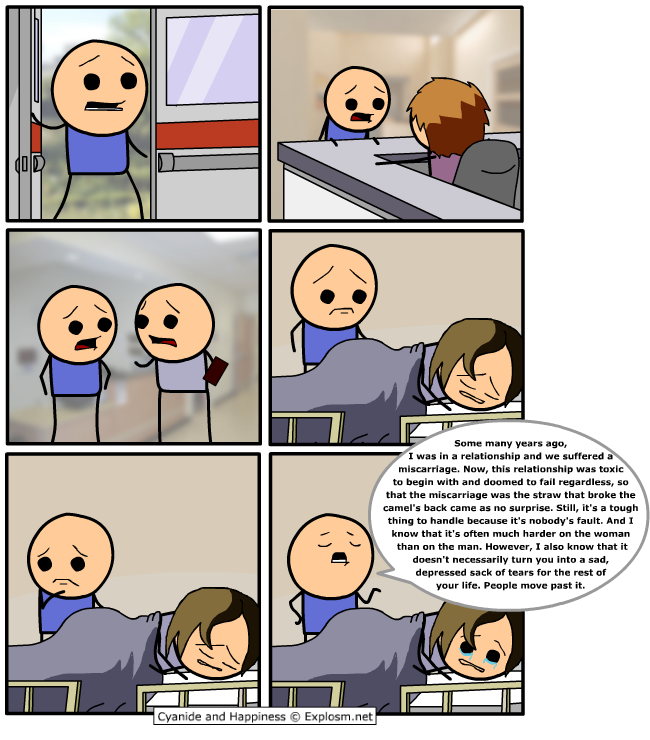
Enter your feedback
What is your question about?Choose a topic for your question: - Select -AnglingBenefitsBirth certificatesBlue BadgeCareersCompensation due to a road problemChild MaintenanceCivil partnership certificatesCoronavirus (COVID-19)COVID vaccination certificateCriminal record checks (AccessNI)Death certificatesEducational Maintenance AllowanceEmployment rightsHigh Street Spend Local SchemeMarriage certificatesMotoringnidirect accountPassportsPenalty Charge NoticesPensionsPRONI - historical recordsRates or property valuationProblems with roads and streetsSmartpassMy question is about something else
What to do next
Miscarriages (for Parents) - Nemours KidsHealth
What Is a Miscarriage?
A miscarriage is the loss of a pregnancy (the loss of an embryo or fetus before it's developed enough to survive). This sometimes happens even before a woman knows she is pregnant. Unfortunately, miscarriages are fairly common.
A miscarriage usually happens in the first 3 months of pregnancy, before 12 weeks' gestation. A very small number of pregnancy losses are called stillbirths, and happen after 20 weeks’ gestation.
What Happens During a Miscarriage?
Often, a woman can have an extra heavy menstrual flow and not realize it’s a miscarriage because she hadn’t known she was pregnant.
Some women who miscarry have cramping, spotting, heavier bleeding, abdominal pain, pelvic pain, weakness, or back pain. Spotting does not always mean a miscarriage. Many pregnant women have spotting early in the pregnancy and go on to have a healthy baby. But just to be safe, if you have spotting or any of these other symptoms anytime during your pregnancy, talk with your doctor.
What Is Stillbirth?
Many experts define a stillbirth as the death of a baby after the 20th week of pregnancy. It can happen before delivery or during labor or delivery. A stillbirth also is sometimes referred to as intrauterine fetal death or antenatal death.
There are some known risk factors for stillbirth, such as smoking, obesity, problems with the placenta, a pregnancy lasting longer than 42 weeks, and some infections. But the cause of many stillbirths isn’t found.
The most common sign of a stillbirth is decreased movement in the baby. If you notice your baby moving less than usual, call your doctor right away. Your doctor can use an ultrasound to look for the heartbeat or, later in pregnancy, give you a fetal non-stress test. This involves lying on your back with electronic monitors on your abdomen. The monitors record the baby's heart rate and movements, and contractions of the uterus.
Why Do Miscarriages Happen?
The most common cause of pregnancy loss is a problem with the chromosomes that would make it impossible for the fetus to develop normally.
Other things that could play a role include:
- low or high hormone levels in the mother, such as thyroid hormone
- uncontrolled diabetes in the mother
- exposure to environmental and workplace hazards, such as radiation or toxic agents
- some infections
- uterine abnormalities
- incompetent cervix, which is when the cervix begins to open (dilate) and thin (efface) before the pregnancy has reached term
- the mother taking some medicines, such as the acne drug Accutane
A miscarriage also can be more likely in pregnant women who:
- smoke, because nicotine and other chemicals in the mother’s bloodstream cause the fetus to get less oxygen
- drink alcohol and or use illegal drugs
What Happens After a Miscarriage?
If a woman miscarries, her doctor will do a pelvic exam and an ultrasound to confirm the miscarriage. If the uterus is clear of any fetal tissue, or it is very early in the pregnancy, many won’t need further treatment.
If the uterus is clear of any fetal tissue, or it is very early in the pregnancy, many won’t need further treatment.
Sometimes, the uterus still contains the fetus or other tissues from the pregnancy. A doctor will need to remove this. The doctor may give medicine to help pass the tissue or may dilate the cervix to do:
- a dilation and curettage (D&C), a scraping of the uterine lining
- a dilation and extraction (D&E), a suction of the uterus to remove fetal or placental tissue
A woman may have bleeding or cramping after these procedures.
If a baby dies later in a woman’s pregnancy, the doctor might induce labor and delivery. After the delivery, the doctor will have the baby and the placenta examined to help find the cause of death if it's still unknown.
Women who have had several miscarriages may want to get checked to see if any anatomic, genetic, or hormonal problems are making miscarriages more likely.
Can Miscarriages Be Prevented?
In most cases, a miscarriage cannot be prevented because it’s caused by a chromosomal abnormality or problem with the development of the fetus. Still, some things — such as smoking and drinking — put a woman at a higher risk for losing a pregnancy.
Still, some things — such as smoking and drinking — put a woman at a higher risk for losing a pregnancy.
Good prenatal care can help moms and their babies stay healthy throughout the pregnancy. If you’re pregnant:
- Eat a healthy diet with plenty of folic acid and calcium.
- Take prenatal vitamins daily.
- Exercise regularly after you've gotten your doctor's OK.
- Keep a healthy weight. Pregnant women who are overweight or too thin may be more likely to have miscarriages.
- Avoid drugs and alcohol.
- Avoid deli meats and unpasteurized soft cheeses such as feta and other foods that could carry listeriosis.
- Limit caffeine intake.
- If you smoke, quit.
- Talk to your doctor about all medicines you take. Unless your doctor tells you otherwise, many prescription and over-the-counter medicines should be avoided during pregnancy.
- Avoid activities that could cause you to get hit in the belly.
- Make sure you’re up to date on all recommended vaccines.
- Know your family medical and genetic history.
- Go to all of your scheduled prenatal visits and discuss any concerns with your doctor.
- Call your doctor right away if you have fever; feel ill; notice the baby moving less; or have bleeding, spotting, or cramping.
Trying Again After a Miscarriage
If you've had a miscarriage, take time to grieve. The loss of a baby during pregnancy is like the loss of any loved one. Give yourself time to heal emotionally and physically. Some health care providers recommend that women wait one menstrual cycle or more before trying to get pregnant again.
Some other things that can help you get through this difficult time:
- Find a support group. Ask your doctor about local support groups for women who are trying again after a loss.
- Find success stories. Other women who have had a successful pregnancy after having a miscarriage can be a great source of encouragement.
 Your doctor might know someone to talk with.
Your doctor might know someone to talk with.
During future pregnancies, it can help to:
- Be proactive. The more you know about the medical aspects of your pregnancy, the better you'll be able to discuss treatment options and outcomes with your doctor.
- Monitor the baby's movements. If you're far enough along to feel kicks and jabs — usually between 18 and 22 weeks — keep a log of the baby's activities each morning and night and report any changes or lack of movement to your doctor. If your baby isn't moving, eat or drink something sugary and lie down on your side. You should feel at least 10 movements in a 2-hour period. If you don't, call your doctor right away.
- Try not to compare. No two pregnancies are exactly alike, so try not to dwell on any similarities between this pregnancy and the one that ended in a loss.
- Stay positive. Envision a good end to help you stay positive.

Reviewed by: Larissa Hirsch, MD
Date reviewed: October 2020
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage.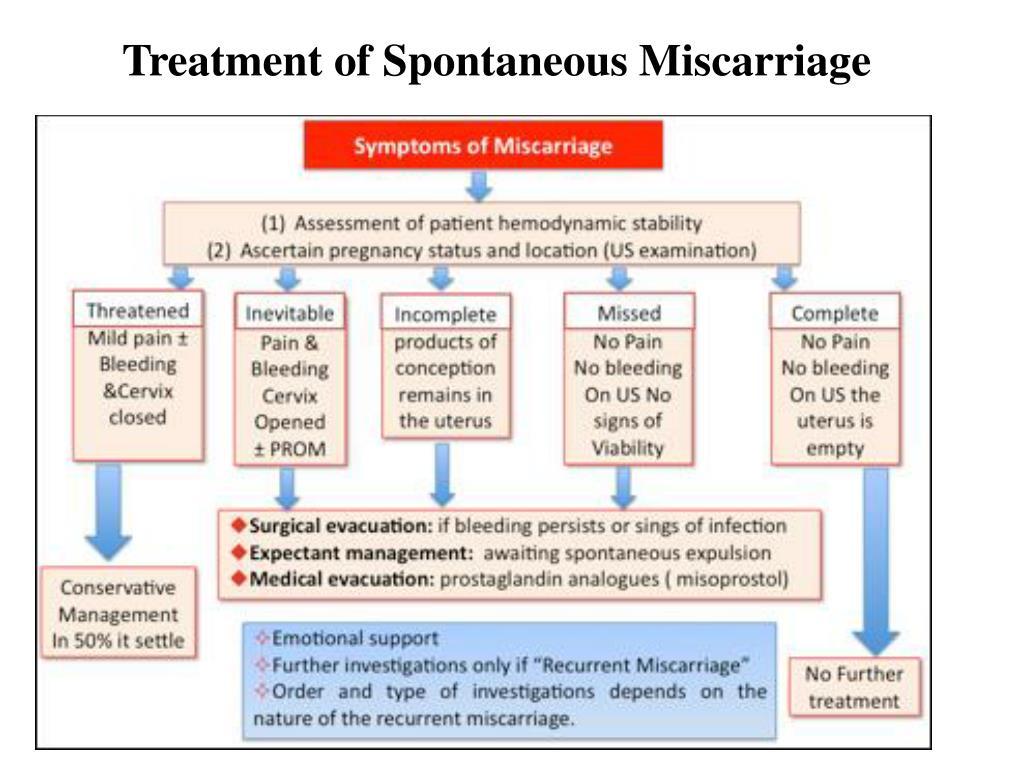 Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be started.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis.
- antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption.
- use of caffeine (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes per day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss?
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repetition of a gynecologist's examination, ultrasound, tests after 7-10 days. If a the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed.
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy.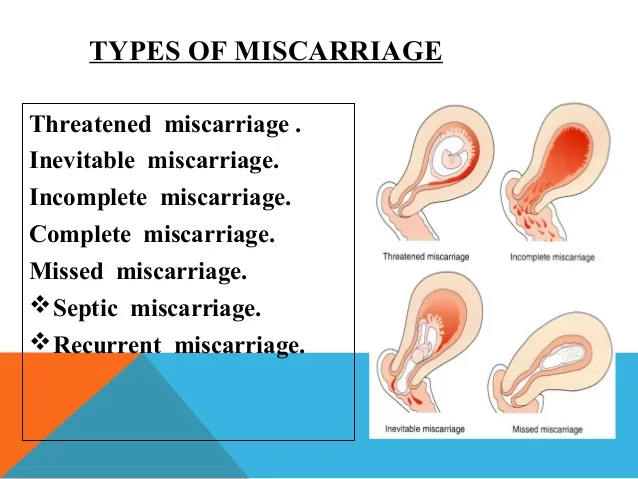 Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities of a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist).