Membrane sweep during pregnancy
Does It Speed Up Your Labor?
Written by WebMD Editorial Contributors
Reviewed by Dan Brennan, MD on June 15, 2021
In this Article
- Understanding Labor Induction
- How Membrane Sweeping Works
- Pros and Cons of Membrane Sweeping
- Risks of Not Having Labor Induced
When you near the end of your pregnancy, your medical team watches you closely for signs that they may need to induce your labor. If your baby needs to be born sooner than everyone else counted on, membrane sweeping, also called sweep and stretch or membrane stripping, may be the labor-induction method your doctor chooses.
Understanding Labor Induction
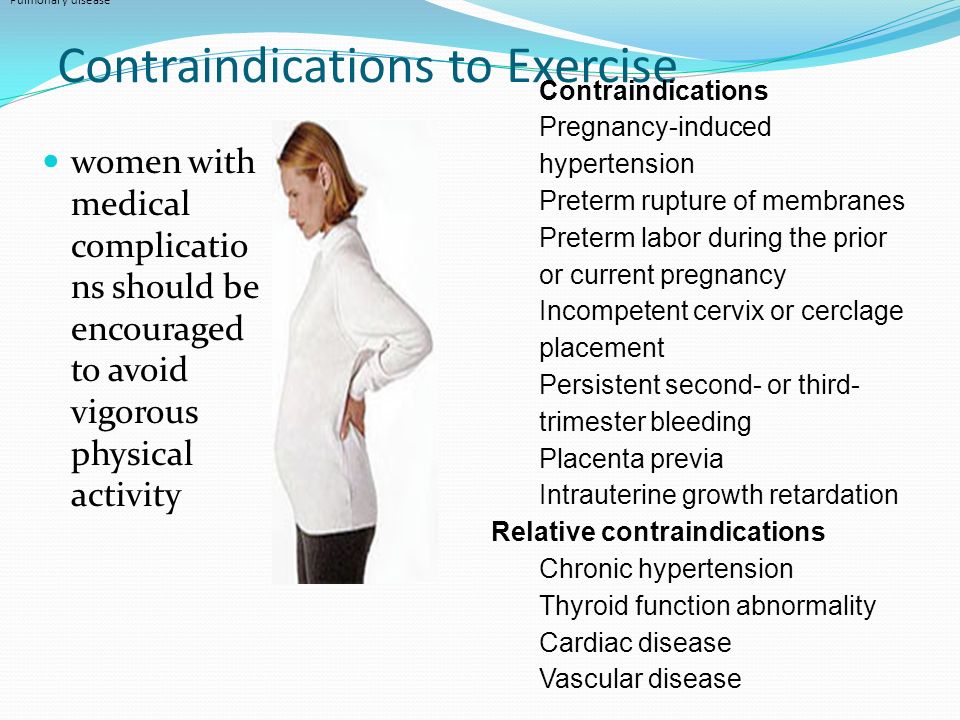
Usually, a woman’s body goes into labor without much prompting, in preparation for a baby’s birth. But if you or your baby is at risk, your doctor may want to induce your labor sooner.
There may be other, practical reasons why a doctor may want to induce. But labor induction techniques should not be used before 39 weeks’ gestation unless there is a medical reason.
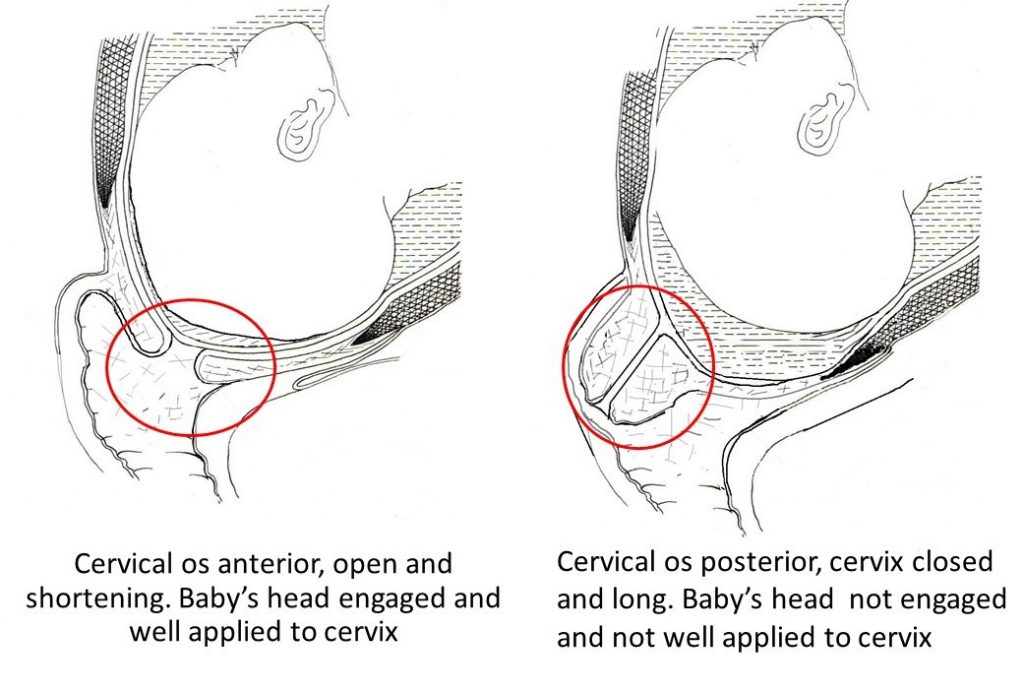
Your cervix prepares for labor by:
- Ripening, which is also called softening
- Opening, also called dilation
- Thinning, also called effacement
These things may start to happen but then stall. Or your water may break, but contractions don’t follow. In these cases, a doctor may choose to induce labor, to stimulate the body’s progress.
Other conditions that call for inducing labor include:
- Status of one or two weeks past the estimated due date
- High blood pressure
- Placenta detached from the uterus
- Infection
- Lung disease
- Diabetes
If your doctor doesn’t try membrane sweeping or another labor induction method, it increases your risk for a cesarean section delivery. While a C-section is sometimes necessary, it is considered higher-risk, so your doctor may want to avoid doing one if possible.
How Membrane Sweeping Works
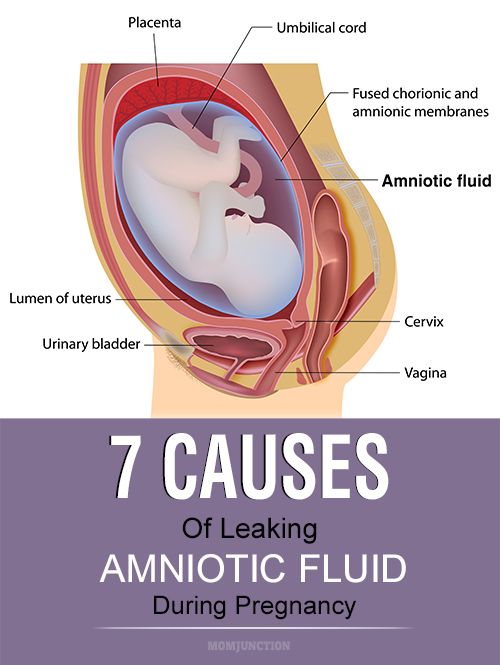
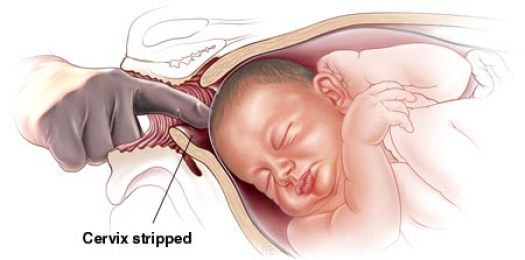
Your doctor inserts a gloved finger into your vagina and up into your cervix to separate your water (amniotic) sac, or bag, from your uterus without breaking the sac. Your doctor uses this technique to urge your body to release prostaglandins, hormones that stimulate labor. As the water sac separates from your uterus, your cervix may soften and contractions may begin.
Your doctor uses this technique to urge your body to release prostaglandins, hormones that stimulate labor. As the water sac separates from your uterus, your cervix may soften and contractions may begin.
Your membranes can only be swept once your cervix opens enough for your doctor to insert a finger. Membrane sweeping to induce labor works for one in eight women. It’s one of the less risky labor-induction techniques.
Pros and Cons of Membrane Sweeping
Pros of membrane sweeping. The idea of forcing your body into labor may be daunting, but this technique has been used for decades.
Compare membrane sweeping to other ways to induce labor:
- Taking medicine that softens your cervix
- Taking medicine that causes your uterus to contract
- Using a balloon catheter to encourage the cervix to open
- Having medicine inserted vaginally to ripen your cervix
When membrane sweeping works and labor begins, there’s no need to help labor along with drugs like oxytocin, by breaking your water, or by using other, more invasive methods.
It’s considered a safe way to speed up your labor without increasing your risk for infection. It can also prevent you from needing to deliver via C-section.
Cons of membrane sweeping. You may start to feel uncomfortable afterward, with irregular contractions and some bleeding. In addition, if membrane sweeping brings on too many contractions, your uterus may be overstimulated.
Too many contractions can put you at risk for:
- Irregular fetal heart rate
- Too much pressure on your umbilical cord
- Uterine tear
- Increased risk of cesarean birth
- Fetal death
Medical problems you may have had before or during your pregnancy can also contribute to these complications. Your doctor will weigh the pros and cons of membrane sweeping before using it to induce your labor.
Risks of Not Having Labor Induced
Your health. If your doctor wants to sweep your membranes or use any other labor-induction technique around the time of your due date, take this into account: If you let your pregnancy go past full-term, you will be at greater risk of a difficult delivery as your baby continues to grow in utero. You’re also at an increased risk for a type of high blood pressure that's associated with pregnancy, after your due date.
You’re also at an increased risk for a type of high blood pressure that's associated with pregnancy, after your due date.
Your baby’s health. Your baby is also at risk as your pregnancy stretches on. With each passing week, the placenta becomes less effective at passing nutrients and blood to your baby. A baby that grows larger than your birth canal will allow for, may be stressed during delivery. A C-section may become unavoidable.
Staying pregnant longer can increase the risk of your baby passing their first meconium stool in utero. If your baby breathes meconium in the birth canal, it greatly increases their risk of developing an infection. A baby born after 42 weeks of gestation also has an increased risk of sudden infant death syndrome (SIDS).
Membrane Sweep | North Bristol NHS Trust
From 40 weeks pregnant, if you are a first time mum and 41 weeks for subsequent pregnancies, at the discretion of your midwife you will be offered a vaginal examination to perform a membrane sweep.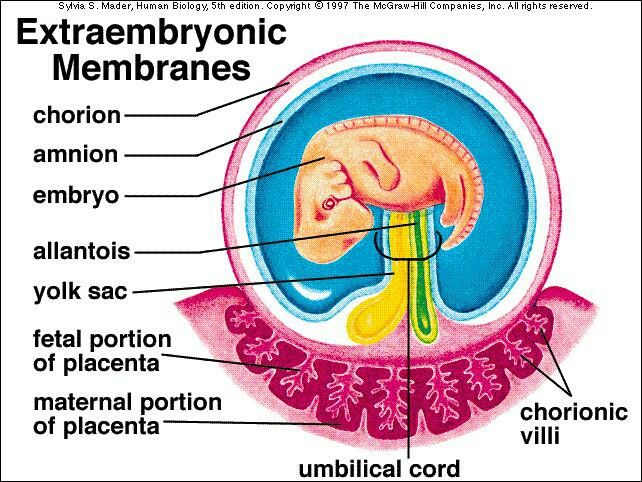
Membrane sweeping involves your midwife or doctor placing a finger just inside your cervix (neck of the womb) and making a circular, sweeping movement to separate the membranes from the cervix. This has been shown to increase the chances of labour starting naturally within the next 48 hours and can reduce the need for other methods of induction of labour. It May be carried out at home, during an antenatal appointment at your surgery or in hospital.
The procedure may cause some slight discomfort, slight bleeding or a ‘show’ and/or tightening of the womb. All of these are normal, and will not cause any harm to you or your baby. It will not increase the chance of your baby getting an infection.
Membrane sweeping is not recommended if your waters have broken.
Whether you have decided to have a membrane sweep or not, you will always be offered a date to have your labour induced (started off). We will ensure you are offered an appointment to attend the hospital between 41 and 42 weeks of pregnancy for a review and to commence your induction of labour.
Can I choose not to have a membrane sweep?
If you decide not to have a membrane sweep, this is not a problem as it is your choice. However, if your pregnancy continues beyond the recommended 12 – 14 days past your due date, you will be invited to attend the Quantock Assessment Unit for further review to ensure that both you and your baby remain well whilst awaiting the onset of natural labour.
At this appointment a midwife will talk to you about how you are feeling, and perform a full antenatal check which will include taking your blood pressure, testing your urine and examining your abdomen to assess the growth and position of your baby.
Your baby’s heartbeat will be monitored for a minimum of 20 minutes and you may be offered an ultrasound scan to assess how much water (amniotic fluid) is surrounding your baby where appropriate. This information will help us when discussing the future care of your pregnancy and possible induction of labour with you.
What happens if my waters break?
Sometimes a woman’s waters break before labour starts. This is known as pre-labour rupture of membranes. If you think your waters have broken it is important you discuss this with a midwife.
This is known as pre-labour rupture of membranes. If you think your waters have broken it is important you discuss this with a midwife.
You may be invited to attend the hospital for an antenatal check to assess both your well-being and that of your baby and to confirm that your waters have broken.
If your waters have broken but you have not gone into labour you will be offered the choice of either:
- A ‘wait and see’ approach to await the onset of natural labour if all remains well. 9 out of 10 women whose waters break before labour starts will go into labour naturally within 24 hours of the waters breaking.
- Induction of labour if there are concerns about either your well-being, or that of your baby.
These options will be discussed with you at the time so that you can make a decision on which you would prefer. One of the functions of the membranes is to provide a sterile environment for your baby. The longer the time interval between your membranes breaking and the birth of your baby, the more likely it is that an infection will develop. Due to this fact, we currently recommend a ‘wait and see’ approach of no more than 24 hours following the breaking of your waters. If labour has not started naturally during this time, induction of labour will be recommended.
Due to this fact, we currently recommend a ‘wait and see’ approach of no more than 24 hours following the breaking of your waters. If labour has not started naturally during this time, induction of labour will be recommended.
It is important that you are happy with the choices you make for your care.
For more information visit www.nhs.uk/conditions/pregnancy-and-baby/pages/induction-labour
Injection of saline into the uterine cavity (amnioinfusion) to reduce complications associated with infection of the membranes of the fetus (vesicle) and amniotic fluid (amniotic fluid) during pregnancy (chorioamnionitis)
What is the problem?
Chorioamnionitis is an infection of the fetal membranes and fluid that surrounds the baby in the womb (womb). This disease is usually treated with antibiotics and delivery. As an additional method of treatment, the introduction of a saline solution into the mother's uterine cavity, either through a needle inserted through the abdominal wall (transabdominally) or through a catheter inserted into the vagina (transcervical), is considered. The theoretical premise is that this method may have a beneficial flushing or diluting effect on organisms that cause infection.
The theoretical premise is that this method may have a beneficial flushing or diluting effect on organisms that cause infection.
Why is this important?
Chorioamnionitis can lead to serious complications such as infection of the baby or mother. Any effective complementary treatment would be helpful.
What evidence did we find?
We searched for evidence available up to 6 July 2016 and found only one randomized controlled trial reporting data from 34 women. Data were available from 17 women who received transcervical amnioinfusion and 17 women without it. All of the women were taking paracetamol and antibiotics, and each had a special catheter placed in their cervix to evaluate their contractions (ie, how often the contractions occur, how long they last, and how strong they are).
The risk of bias in this trial was high due to the small number of participants, reporting inconsistencies, and lack of information about the blinding procedure. outcomes of this review, such as postpartum uterine infection ( low-quality evidence ), child infection (low-quality evidence), caesarean section (low quality evidence), duration of antibiotic treatment length of hospital stay . The body temperature of the mother at delivery , which was not predicted by the outcome for our review, was lower by 0.38°C in women undergoing the amnioinfusion procedure (with a likely decrease range of 0.74 to 0.02). About these outcomes as death or serious illness in children were not reported, nor was the number of children from with a low Apgar score after they were born (a low Apgar score may mean the baby needs medical attention). In addition, most of the other outcomes listed in this review were not reported in the included study.
outcomes of this review, such as postpartum uterine infection ( low-quality evidence ), child infection (low-quality evidence), caesarean section (low quality evidence), duration of antibiotic treatment length of hospital stay . The body temperature of the mother at delivery , which was not predicted by the outcome for our review, was lower by 0.38°C in women undergoing the amnioinfusion procedure (with a likely decrease range of 0.74 to 0.02). About these outcomes as death or serious illness in children were not reported, nor was the number of children from with a low Apgar score after they were born (a low Apgar score may mean the baby needs medical attention). In addition, most of the other outcomes listed in this review were not reported in the included study.
We did not identify any studies that looked at the administration of the solution through the mother's abdominal wall (transabdominally).
What does this mean?
There is insufficient evidence to support the use of amnioinfusion for chorioamnionitis in clinical practice. We believe that the decrease in temperature may have been due in part to the direct cooling effect of the fluid administered, and that further research is needed to determine whether such a cooling effect may be beneficial to the child.
Further randomized controlled trials in this area are needed. Future clinical trials should compare transabdominal or transcervical amnioinfusion with treatment without amnioinfusion in women with infection of the amniotic fluid and membranes (chorioamnionitis) and report on the significant outcomes listed in this review.
Translation notes:
Translation: Anastasia Evgenievna Volozhanina. Editing: Kamalova Aelita Askhatovna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected]
For questions related to this translation, please contact us at: [email protected]; [email protected]
Postpartum hygiene
Congratulations! You have become a mother!
The postpartum period is no less important and responsible stage in the life of a family than pregnancy.
The postpartum period lasts 6-8 weeks (begins after the birth of the placenta and ends when the organs and systems that have changed during pregnancy return to their original state).
In the process of healing the inner surface of the uterus, postpartum discharge appears - lochia, which is a wound secret. Their character during the postpartum period changes: in the first days, lochia has a bloody character; from the 4th day, their color changes to reddish-brown; by the 10th day they become light, liquid, without blood, and after 3 weeks there is practically no discharge. There may be discomfort due to uterine contractions. To relieve discomfort, bend forward and gently massage your belly. If discomfort in the uterine area occurs during feeding, try choosing a different position. It is convenient to feed lying on your side. The stomach may ache for another reason. It hurts the abdominal muscles that were actively involved during childbirth, try to relax or do a light massage.
If discomfort in the uterine area occurs during feeding, try choosing a different position. It is convenient to feed lying on your side. The stomach may ache for another reason. It hurts the abdominal muscles that were actively involved during childbirth, try to relax or do a light massage.
In most non-nursing women, menstruation occurs on the 6-8th week after childbirth, more often it comes without the release of an egg from the ovary. However, ovulation and pregnancy may occur during the first months after childbirth. In lactating women, the time of the onset of the first menstruation after childbirth can be delayed for many months.
The normal postpartum period is characterized by a good general condition of the woman, normal temperature, sufficient lactation. For the prevention of infectious complications, strict adherence to sanitary and epidemiological requirements and personal hygiene rules is important.
POSTPARTUM HYGIENE
The strictest cleanliness is essential.
- The mother should take a shower twice a day (morning and evening), then wash the mammary gland with soap and brush her teeth.
- Particular attention should be paid to the cleanliness of hands. Nails should be cut short, hands should be washed more often with soap and be sure before each feeding of the child (if the hands are dirty, you can infect the child, infect the nipples).
- Among the hygienic measures of particular importance in the postpartum period is the maintenance of cleanliness of the external genitalia and the surrounding skin.
- Should be washed with warm water and soap (liquid with a dispenser, because microbes feel great on lumps) with a fluid stream, washing the genitals should be from front to back (from the pubis to the anus) after each visit to the toilet at least 4-5 times a day (you need to go to the toilet exactly at such a frequency that the filled bladder does not interfere with uterine contraction).
Wash hands cleanly before washing.
- Keep the pads clean, change them every 3-4 hours regardless of fullness. Remove pads from front to back to prevent microorganisms from entering the vagina from the anus. If there are seams on the perineum, they should be washed thoroughly enough - you can simply direct a jet of water at it. After washing, you need to dry the perineum and the seam area by blotting the towel from front to back.
- Do not take a bath for the first 6 weeks after giving birth. This is due to the fact that the entrance to the vagina is not yet closed enough and pathogenic microbes can penetrate into it along with water. It is clear that at this time you can not swim in the pool, river, lake, sea.
- The use of tight underwear is strictly excluded, as it puts significant pressure on the perineum, which disrupts blood circulation, preventing healing.
- If there are stitches on the perineum, a woman should not sit down for 7-14 days (depending on the degree of damage).
 At the same time, you can sit on the toilet already on the first day after childbirth. By the way, about the toilet. Many women are afraid of severe pain and try to skip bowel movements, as a result, the load on the muscles of the perineum increases and the pain intensifies.
At the same time, you can sit on the toilet already on the first day after childbirth. By the way, about the toilet. Many women are afraid of severe pain and try to skip bowel movements, as a result, the load on the muscles of the perineum increases and the pain intensifies.
To avoid constipation after childbirth, do not eat foods that have a fixative effect. If the problem of constipation is not new to you, drink a tablespoon of vegetable oil before each meal. The stool will be soft and will not affect the healing process of the stitches.
- Underwear and bed linen must be cotton. We change underwear daily, bedding - at least once every three to five days.
- Stitches after caesarean section do not require special care. After the stitches and bandage are removed, you can take a shower. Do not scrub the seam area with a washcloth. With painful sensations in the anterior abdominal wall, a postpartum or postoperative bandage, which must be worn for 4 months, will help to cope.
 Young mothers are often interested in: will the seams come apart if you carry a baby in your arms? For the first 2-3 months after surgery, it is recommended to lift no more than your child's weight.
Young mothers are often interested in: will the seams come apart if you carry a baby in your arms? For the first 2-3 months after surgery, it is recommended to lift no more than your child's weight.
It happens that redness, irritation, bloody or purulent discharge occurs at the suture site. This indicates suppuration or divergence of the seams. Then you should immediately consult a doctor in a antenatal clinic.
Sexual life after childbirth can be resumed after 6-8 weeks. By this time, the woman's body is already completely back to normal. Your doctor will advise you on contraceptives.
To fully recover from childbirth, at least two years must pass before the next pregnancy.
BREASTFEEDING
Feeding the baby should not go by the clock, but on demand, incl. in nighttime. At one feeding, put the baby on one breast so that he suckles for a long time and receives later milk, which contains brain and intelligence development factors, growth factors and immunoglobulins. Later, the milk comes in droplets like colostrum, the child sucks it intermittently. Sometimes the mother at this moment thinks that the child is indulging and tearing him off the breast. You don't need to do this. Let him let her go.
Later, the milk comes in droplets like colostrum, the child sucks it intermittently. Sometimes the mother at this moment thinks that the child is indulging and tearing him off the breast. You don't need to do this. Let him let her go.
Breast milk is the best food for a baby!
- After the baby has had enough, the mother should carefully feel the mammary gland. If the breast is soft and there is no soreness and seals anywhere, then pumping is not necessary. If necessary, you can wash the mammary glands with warm water after feeding, starting from the nipple and ending with the armpit, and dry with a clean towel.
Very useful for the breasts after childbirth and air baths, which are best taken after feeding, to give the breast the opportunity to rest, "breathe". The duration of such an air bath may not exceed 15-20 minutes, but the benefits of it are enormous.
- The nipple should be carefully inspected daily, the surface of which should not be cracked, and as a preventive measure, leave a drop of milk on the nipple and let it dry in the open air.
Only breast milk should be used as the main and only product for feeding a newborn. The use of nipples, horns and "pacifiers" is unacceptable, as this leads to a weakening of sucking in newborns and, accordingly, to incomplete emptying of the mammary gland, a decrease in prolactin production.
Are you worried about the question - do I have enough milk?
To resolve this issue, you need to observe the child, if he urinates more than 6 times a day, then he receives a sufficient amount of milk. The reason for the decrease in the amount of milk can be:
- rare feeding break (3 or more hours)
- if you do not feed at night
- short feedings or by the hour
To increase the amount of milk, you need to reorganize the feeding regimen, feed often and for as long as you want child. Try to feed with one breast so that the baby sucks out milk later, you can strain the empty breast for 10 minutes, thereby increasing the flow of milk. It is necessary to improve the mother's nutrition or use herbal teas to increase lactation.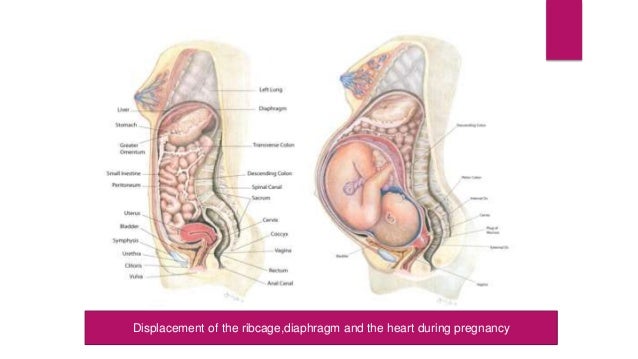
NUTRITION
Nursing mother's diet should be rich in calories (3200 kcal), balanced with the proper amount of proteins, fats, carbohydrates, vitamins and microelements. This diet will be dominated by lactic acid, protein foods, fresh fruits and vegetables. Food should be rich in vitamins and minerals. Spicy, fatty, fried, smoked foods, canned food, sausages, alcohol and potential allergens for the child (chocolate, citrus fruits, coffee) should be excluded from the diet.
The food of the puerperal should be 5-6 times a day. It is necessary to distribute products in the daily menu in such a way that those that are rich in protein and are much more difficult to digest in the gastrointestinal tract (meat, fish, cereals) would be used during the first half of the day, and in the second half it is advisable to give preference to milk. - vegetable food.
Conditions requiring special attention
Unfortunately, the first month after childbirth does not always go smoothly.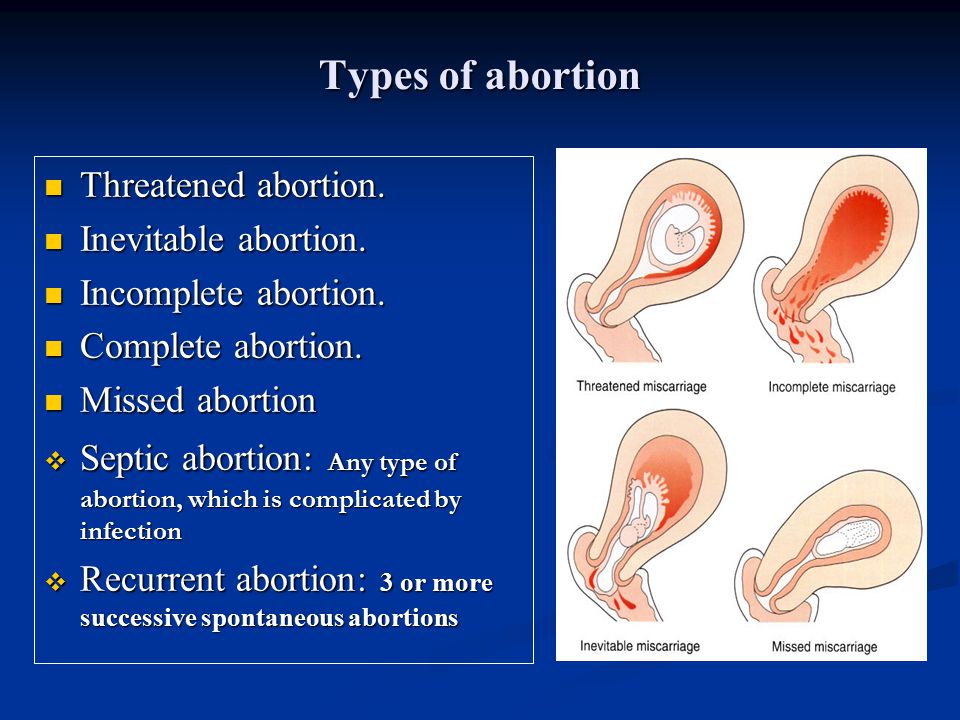 Situations may arise, when medical attention is needed . Monitor your well-being, regularly measure your body temperature, as fever is most often the first sign of complications in the postpartum period.
Situations may arise, when medical attention is needed . Monitor your well-being, regularly measure your body temperature, as fever is most often the first sign of complications in the postpartum period.
All complications of the postpartum period can be divided into several groups:
1. Complications of the uterus.
Subinvolution of the uterus - a decrease in the rate of contraction of the uterus, due to a delay in the uterus of postpartum discharge. The disease often occurs 5-7 days after childbirth, due to the closure of the cervical canal with a blood clot or a piece of membranes, as well as the inflection of the uterus due to relaxation of the ligamentous apparatus.
Infection of the contents of the uterus can lead to inflammation of the uterine mucosa - endometritis. Predisposing factors for the occurrence of endometritis are difficult childbirth, violations of the separation of the placenta during childbirth, infections of the genital tract during pregnancy, impaired immunity, abortion.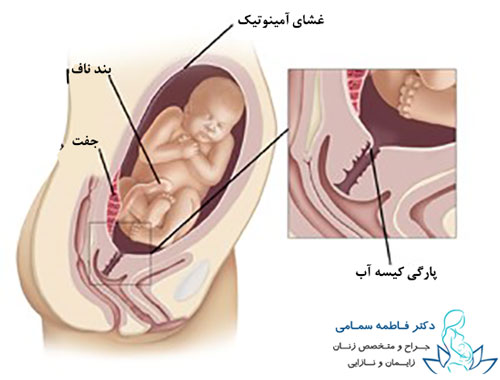 Symptoms of the disease are: fever, unpleasant odor in lochia, aching pain in the lower abdomen. If these symptoms appear, you should consult an obstetrician-gynecologist at the place of residence. To clarify the diagnosis, an ultrasound examination is performed and, if necessary, surgery, during which the contents are removed from the uterine cavity (washing or curettage of the uterus). After surgery, antibiotics must be prescribed.
Symptoms of the disease are: fever, unpleasant odor in lochia, aching pain in the lower abdomen. If these symptoms appear, you should consult an obstetrician-gynecologist at the place of residence. To clarify the diagnosis, an ultrasound examination is performed and, if necessary, surgery, during which the contents are removed from the uterine cavity (washing or curettage of the uterus). After surgery, antibiotics must be prescribed.
2. Breast complications.
Laktostasis - stagnation of milk in the mammary gland. At the same time, the chest swells and becomes painful, foci of seals appear, a short-term rise in body temperature is possible. In itself, lactostasis is not a disease, requiring only gentle pumping of the breast, restriction of fluid intake, and frequent feeding of painful breasts. However, when an infection joins, it turns into lactational mastitis, requiring immediate medical attention , antibiotic therapy, and sometimes surgery. The question of the possibility of breastfeeding with mastitis is decided individually, depending on the stage of the disease.
The question of the possibility of breastfeeding with mastitis is decided individually, depending on the stage of the disease.
Another complication of the breast is the appearance of cracks in the nipples. The main reason for their appearance is improper attachment of the baby to the breast, when the baby captures only the nipple, and not the entire areola. Such a seizure is very painful for the mother - and this is the main danger signal. Breastfeeding doesn't have to be painful. Good advisory and practical help for lactostasis and cracked nipples is provided by breastfeeding consultants. Treatment of cracks consists in treating the nipple with wound healing drugs.
Hypogalactia - insufficient milk production. In order to increase the amount of milk, a mother needs to increase the frequency of feedings, not skip night feedings, offer her baby both breasts in one feeding, drink more, eat well and sleep a lot.
3. Complications from the tissues of the cervix, vagina and skin.
Inflamed wounds of these tissues are called postpartum ulcers. When an infection is attached, these wounds swell, become covered with a purulent coating, and their edges are painful. For the purpose of treatment, they are treated with various antiseptics, sometimes they require surgical treatment.
4. Complications of the venous system.
Hemorrhoids (varicose veins of the rectum) also cause pain. When infringed, they increase, become swollen, tense and painful. Thorough hygiene helps to reduce pain (shower after each visit to the toilet), applying ice to the perineum. Certain medications can be used as prescribed by a doctor.
Thrombophlebitis is a disease of the veins characterized by inflammation of the venous wall and thrombosis of the vein. After childbirth, thrombophlebitis of the pelvic veins most often occurs. Usually this disease occurs in the third week after childbirth. In terms of symptoms, it is very similar to endometritis, but requires a different treatment.