Pain after miscarriage left side
Acute pelvic pain following miscarriage heterotopic pregnancy must be excluded: case report
- Journal List
- BMC Emerg Med
- v.19; 2019
- PMC6814984
BMC Emerg Med. 2019; 19: 59.
Published online 2019 Oct 25. doi: 10.1186/s12873-019-0268-8
,1,2,3 and 4
Author information Article notes Copyright and License information Disclaimer
- Data Availability Statement
Background
Heterotopic pregnancies are increasing in prevalence and this case highlights the importance of excluding the diagnosis in patients with pelvic pain following miscarriage. A known pre-existing intrauterine pregnancy can be falsely reassuring and delay the diagnosis of a potentially life-threatening concurrent ectopic pregnancy.
Case presentation
In this report, we describe a case of spontaneous heterotopic pregnancy in a woman who had initially presented with pelvic pain and vaginal bleeding, and was diagnosed on pelvic ultrasound with a missed miscarriage; a non-viable intrauterine pregnancy. She re-presented 7 days later with worsening pelvic pain and bleeding, and a repeat pelvic ultrasound identified a ruptured tubal ectopic pregnancy in addition to an incomplete miscarriage of the previously identified intrauterine pregnancy. She underwent an emergency laparoscopy where a ruptured tubal ectopic pregnancy was confirmed.
Conclusion
Being a time critical diagnosis with the potential for an adverse outcome, it is important that the emergency physician considers heterotopic pregnancy as a differential diagnosis in patients presenting with pelvic pain following a recent miscarriage. The same principle should apply to pelvic pain in the context of a known viable intrauterine pregnancy or recent termination of pregnancy. A combination of clinical assessment, beta human chorionic gonadotropin levels, point of care ultrasound and formal transvaginal ultrasound must be utilized together in these situations to explicitly exclude heterotopic pregnancy.
The same principle should apply to pelvic pain in the context of a known viable intrauterine pregnancy or recent termination of pregnancy. A combination of clinical assessment, beta human chorionic gonadotropin levels, point of care ultrasound and formal transvaginal ultrasound must be utilized together in these situations to explicitly exclude heterotopic pregnancy.
Keywords: Heterotopic pregnancy, Miscarriage, Acute pelvic pain, Early pregnancy
The etiology of pelvic pain following miscarriage is diverse. A heterotopic pregnancy (HP) should be considered amongst the differential diagnoses, which include endometritis, incomplete miscarriage, ruptured ovarian cyst and non-gynecological causes such as appendicitis or urinary tract infection. HP has traditionally been a rare diagnosis in which an intrauterine and ectopic pregnancy occur concurrently. The prevalence of HP is increasing, primarily due to artificial reproductive technology (ART) and pelvic infections [1]. A missed diagnosis of HP can be life-threatening if the ectopic pregnancy ruptures and causes intra-abdominal bleeding.
A missed diagnosis of HP can be life-threatening if the ectopic pregnancy ruptures and causes intra-abdominal bleeding.
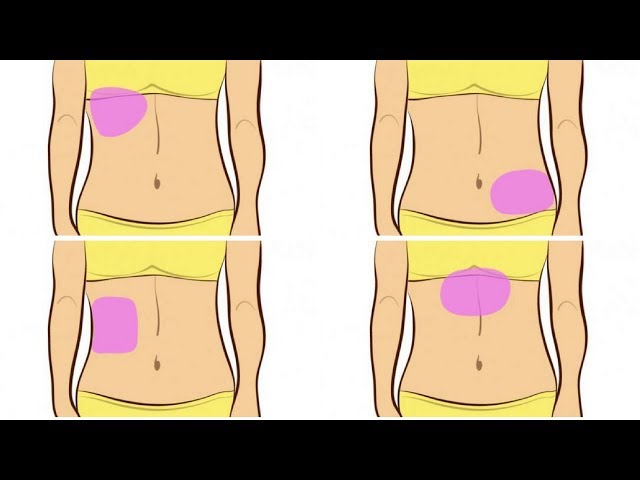
A 33-year-old female, gravidity two and parity one, presented to the Emergency Department with acute-onset sharp pelvic pain, right worse than left, and mild vaginal bleeding. She was found to be pregnant with a beta human chorionic gonadotropin (β-hCG) level of 1442 mIU/ml. The pregnancy was spontaneous and unplanned; she was breastfeeding 6 months after a normal vaginal delivery and using the oral contraceptive pill, levonorgestrel, 30mcg daily. She had no significant past gynecological, medical or surgical history. She underwent a formal departmental transvaginal ultrasound (TV US) verified by a Consultant Radiologist that identified an intrauterine pregnancy (IUP) with crown rump length of 8.5 mm without cardiac activity, consistent with 6 + 5 weeks gestation. This met the widely accepted ultrasound criteria for a missed miscarriage [2]. There was a physiological corpus luteal cyst in the left ovary, and the right ovary was normal.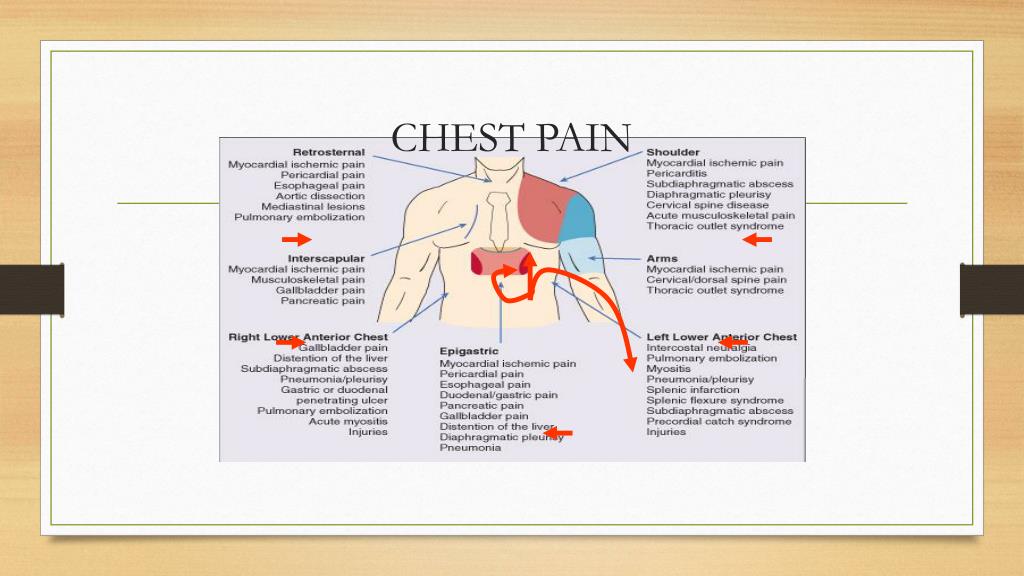 After observation overnight, she was discharged for expectant management of the miscarriage as she was clinically stable and had a falling β-hCG from 1442 mIU/ml to 915 mIU/ml over 24 h. She re-presented to the Emergency Department 7 days later with worsening pelvic pain, mostly right sided, and ongoing mild vaginal bleeding. She was hemodynamically stable and mildly tender to palpate in the left iliac fossa. The β-hCG had risen to 2267 mIU/ml. Her hemoglobin dropped to 12.4 g/dL, previously 15.0 g/dL. The Emergency Physician requested a formal departmental TV US, which revealed a new solid right adnexal mass measuring 64x60x40mm with internal vascularity and adherent to the right ovary (Fig. ). There was a large volume of fluid in the pelvis with low-level echoes. The left-sided corpus luteal cyst was again visualized. An endometrial cavity lesion of 16x9x16mm was thought to be retained products of conception. A diagnosis was made of a HP, with a suspected ruptured tubal ectopic pregnancy and retained products of conception from an incomplete miscarriage of the previously identified non-viable intrauterine pregnancy.
After observation overnight, she was discharged for expectant management of the miscarriage as she was clinically stable and had a falling β-hCG from 1442 mIU/ml to 915 mIU/ml over 24 h. She re-presented to the Emergency Department 7 days later with worsening pelvic pain, mostly right sided, and ongoing mild vaginal bleeding. She was hemodynamically stable and mildly tender to palpate in the left iliac fossa. The β-hCG had risen to 2267 mIU/ml. Her hemoglobin dropped to 12.4 g/dL, previously 15.0 g/dL. The Emergency Physician requested a formal departmental TV US, which revealed a new solid right adnexal mass measuring 64x60x40mm with internal vascularity and adherent to the right ovary (Fig. ). There was a large volume of fluid in the pelvis with low-level echoes. The left-sided corpus luteal cyst was again visualized. An endometrial cavity lesion of 16x9x16mm was thought to be retained products of conception. A diagnosis was made of a HP, with a suspected ruptured tubal ectopic pregnancy and retained products of conception from an incomplete miscarriage of the previously identified non-viable intrauterine pregnancy. A gynecology consult was summoned and the patient was transferred to theatre for surgery.
A gynecology consult was summoned and the patient was transferred to theatre for surgery.
Open in a separate window
TV US from initial presentation (image on left) showing normal right adnexa. The image on right shows an intra-uterine pregnancy with CRL measurement. The absence of a FHR in a CRL measuring above 7 mm was consistent with a missed miscarriage. The gestational sac measured 20 mm. It was eccentrically placed consistent with a true gestational sac. The gestational sac border was also irregular, a feature of a non-viable pregnancy
A diagnostic laparoscopy was performed with dilation and curettage. A 100 ml hemoperitoneum and ruptured right fallopian tube infundibular ectopic pregnancy adherent to the right ovary was identified (Fig. ). A right salpingectomy was performed. Histology confirmed a ruptured tubal ectopic pregnancy and endometrial curettings confirmed retained products of conception. She had an uncomplicated recovery. Her follow-up β-hCG level was negative.
Open in a separate window
TV US (image on left) shows a 64 × 60 × 40 mm solid appearing mass in the right adnexa separate to the right ovary and free pelvic fluid. At laparoscopy, there was a ruptured right fallopian tube infundibular ectopic pregnancy with haemoperitoneum
HP has traditionally been a rare diagnosis where there is a concurrent intrauterine and ectopic pregnancy. It can be potentially life-threatening if the ectopic ruptures and causes intra-abdominal bleeding. The case highlights the importance of explicitly excluding a HP in all patients presenting with pelvic pain after miscarriage. Such vigilance must also apply to patients presenting with a known viable IUP, and also following a termination of pregnancy.
HP’s are estimated to occur in 1 in 30,000 pregnancies in spontaneous conceptions and increases to 1 in 100 pregnancies if associated with ART, tubal ligation, pelvic inflammatory disease or non-infectious causes of tubal damage such as endometriosis [1]. The patient discussed was using a low-dose progesterone-only pill, which when contraception fails and ovulation occurs may be associated with ectopic pregnancy due to impaired fallopian tube motility [3, 4]. The patient otherwise had no known predisposing factors for a HP.
The patient discussed was using a low-dose progesterone-only pill, which when contraception fails and ovulation occurs may be associated with ectopic pregnancy due to impaired fallopian tube motility [3, 4]. The patient otherwise had no known predisposing factors for a HP.
A delay in diagnosis is more likely to require operative intervention such as salpingectomy [5]. A review of delayed or misdiagnosed HP and ectopic pregnancies identified factors contributing to delayed diagnosis could be classified under 3 categories: (1) clinician factors: unawareness of HP as a diagnostic entity due to its rarity in spontaneous pregnancies, false re-assurance from the presence of a confirmed IUP and patients missed to follow-up due to misinterpretation of β-hCG trends; (2) patient factors: non-compliance with follow-up, and (3) complicated presentations having atypical symptoms, such as GI symptoms [6].
The most common presenting symptom of a HP is unilateral pelvic pain, and others include vaginal bleeding and presyncope [3]. Patients may also report persisting pregnancy symptoms after a miscarriage or termination of pregnancy. Up to 13% of patients may present with signs of shock [5]. Clinical signs include vaginal bleeding, abdominal tenderness to palpation, peritoneal irritation, an enlarged uterus greater than 8 week size, cervical motion tenderness and tender adnexal mass on vaginal examination [7]. These non-specific symptoms and signs may be erroneously attributed to a co-existing IUP, and exemplify the difficulty in clinically diagnosing HPs. It is important to obtain a gynaecology opinion for any patients who re-present with undifferentiated pain [7].
Patients may also report persisting pregnancy symptoms after a miscarriage or termination of pregnancy. Up to 13% of patients may present with signs of shock [5]. Clinical signs include vaginal bleeding, abdominal tenderness to palpation, peritoneal irritation, an enlarged uterus greater than 8 week size, cervical motion tenderness and tender adnexal mass on vaginal examination [7]. These non-specific symptoms and signs may be erroneously attributed to a co-existing IUP, and exemplify the difficulty in clinically diagnosing HPs. It is important to obtain a gynaecology opinion for any patients who re-present with undifferentiated pain [7].
β-hCG levels and TV US together play a critical role in excluding a HP. After a miscarriage, a positive β-hCG result may be normal in the resolution of the pregnancy. Whilst β-hCG levels can be assessed 3 weeks after miscarriage to ensure no molar pregnancy, there is no recommendation to routinely assess β-hCG levels in the follow-up of a miscarriage to exclude heterotopic pregnancy [2]. If a β-hCG level is performed, an abnormal rise or fall in the quantitative β-hCG level may be suggestive – not diagnostic – of a HP. β-hCG levels are expected to fall following a miscarriage or termination of pregnancy. Higher initial β-HCG levels are associated with a more rapid decline, however, in general, by 48 h β-HCG levels should fall by 35% and by the seventh day it is expected that β-hCG levels fall between 60 and 84% [8]. The rate of β-hCG decline is slower in ectopic pregnancies. In the case presented, the β-hCG level after the miscarriage had risen leading to suspicion of a HP. Interestingly, one in three ectopic pregnancies have occurred in the presence of appropriately falling or rising β-hCG levels [9], highlighting the importance of not depending on trends in β-hCG levels in isolation to exclude a HP.
If a β-hCG level is performed, an abnormal rise or fall in the quantitative β-hCG level may be suggestive – not diagnostic – of a HP. β-hCG levels are expected to fall following a miscarriage or termination of pregnancy. Higher initial β-HCG levels are associated with a more rapid decline, however, in general, by 48 h β-HCG levels should fall by 35% and by the seventh day it is expected that β-hCG levels fall between 60 and 84% [8]. The rate of β-hCG decline is slower in ectopic pregnancies. In the case presented, the β-hCG level after the miscarriage had risen leading to suspicion of a HP. Interestingly, one in three ectopic pregnancies have occurred in the presence of appropriately falling or rising β-hCG levels [9], highlighting the importance of not depending on trends in β-hCG levels in isolation to exclude a HP.
Formal departmental TV US underpins the exclusion of a HP. However, it is essential to note that Emergency Physician (EPs) performed point-of-care ultrasound (PPOCUS) may play a critical role in risk stratification. PPOCUS has a greater than 99% sensitivity and specificity in excluding ectopic pregnancies, but this is through the visualisation of an IUP on transabdominal imaging, which may provide false reassurance and delay the diagnosis of a concurrent extrauterine pregnancy [10]. PPOCUS may play a more useful role in determining patients needing prompt operative care – in those with ruptured ectopic pregnancy. Rather than focusing on identifying an IUP, visualisation of fluid in the hepatorenal space (Morison’s pouch) by PPOCUS has been found to be strongly predictive of the need for operative intervention with a positive likelihood ratio of 112 [11]. In an appropriately trained EP, PPOCUS takes less than 5 min to complete [11]. A recent meta-analysis found that there are significant time savings with PPOCUS, especially at night where access to formal departmental US is limited [12]. If PPOCUS does not identify free fluid, a formal departmental TV US to assess the adnexa should then be arranged, with the urgency dependant on clinical concern and resources.
PPOCUS has a greater than 99% sensitivity and specificity in excluding ectopic pregnancies, but this is through the visualisation of an IUP on transabdominal imaging, which may provide false reassurance and delay the diagnosis of a concurrent extrauterine pregnancy [10]. PPOCUS may play a more useful role in determining patients needing prompt operative care – in those with ruptured ectopic pregnancy. Rather than focusing on identifying an IUP, visualisation of fluid in the hepatorenal space (Morison’s pouch) by PPOCUS has been found to be strongly predictive of the need for operative intervention with a positive likelihood ratio of 112 [11]. In an appropriately trained EP, PPOCUS takes less than 5 min to complete [11]. A recent meta-analysis found that there are significant time savings with PPOCUS, especially at night where access to formal departmental US is limited [12]. If PPOCUS does not identify free fluid, a formal departmental TV US to assess the adnexa should then be arranged, with the urgency dependant on clinical concern and resources. Identifying of an IUP is re-assuring but a systematic assessment of the adnexa must occur to exclude an ectopic pregnancy, and suspicious adnexal masses should undergo further follow-up for change in appearance or size. In the case discussed, there was only an interval of 7 days between presentations and imaging of the right adnexa which highlights the speed at which ectopic pregnancies may develop and rupture. Tubal ectopic pregnancies make up 95% of ectopic pregnancies [3]. Findings of a tubal ectopic on TV US include an empty uterus with an endometrium less than 8-10 mm, free fluid in the pelvis, pseudo-gestational sac in up to 20% of cases, and a complex adnexal mass of varying appearance (inhomogeneous mass, hyperechoic ring, distinct gestational sac with or without a yolk sac and fetal heart) moving separate to the ovary [13].
Identifying of an IUP is re-assuring but a systematic assessment of the adnexa must occur to exclude an ectopic pregnancy, and suspicious adnexal masses should undergo further follow-up for change in appearance or size. In the case discussed, there was only an interval of 7 days between presentations and imaging of the right adnexa which highlights the speed at which ectopic pregnancies may develop and rupture. Tubal ectopic pregnancies make up 95% of ectopic pregnancies [3]. Findings of a tubal ectopic on TV US include an empty uterus with an endometrium less than 8-10 mm, free fluid in the pelvis, pseudo-gestational sac in up to 20% of cases, and a complex adnexal mass of varying appearance (inhomogeneous mass, hyperechoic ring, distinct gestational sac with or without a yolk sac and fetal heart) moving separate to the ovary [13].
Delayed diagnosis of a HP is pertinent for the Emergency Physician as the consequences to the patient can be dire. This case highlights the importance of maintaining a high index of suspicion for a HP in patients with pelvic pain after miscarriage, with the same principle applied to those with a recent termination of pregnancy or known IUP.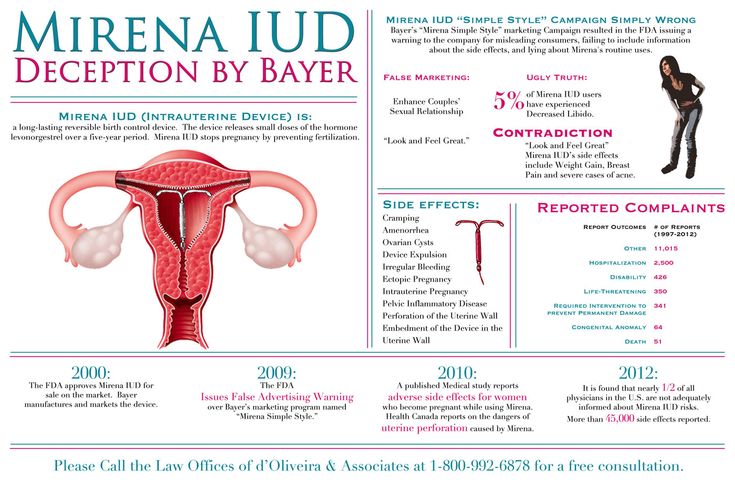 A combination of history, examination, β-hCG levels, PPOCUS and formal TV US should be considered to explicitly exclude HP in these patients.
A combination of history, examination, β-hCG levels, PPOCUS and formal TV US should be considered to explicitly exclude HP in these patients.
The authors have no acknowledgements.
| ART | Artificial reproductive technology |
| EP | Emergency physician |
| HP | Heterotopic pregnancy |
| PPOCUS | Physician performed point-of-care ultrasound |
| TV US | Transvaginal ultrasound |
| β-hCG | beta human chorionic gonadotropin |
UT and KA were involved in study conceptualization, manuscript writing and critical revisions. AB as the senior author supervised the study and revised the manuscript. All authors read and approved the final manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data sharing is not applicable to this article as no datasets were generated during the study.
Not applicable.
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Udit Thakur, Phone: +61 403337406, Email: [email protected].
Kiran Atmuri, Email: moc.liamg@irumtanarik.
Angelika Borozdina, Email: ua.gro.htlaehogidneb@anidzoroBA.
1. Govindarajan M, Rajan R. Heterotopic pregnancy in natural conception. J Hum Reprod Sci. 2008;1(1):37. doi: 10.4103/0974-1208.39595. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management in early pregnancy of ectopic pregnancy and miscarriage. Clin Guidel. 2012;154:77-82.
Clin Guidel. 2012;154:77-82.
3. Barnhart KT. Ectopic pregnancy. N Engl J Med. 2009;361(4):379–387. doi: 10.1056/NEJMcp0810384. [PubMed] [CrossRef] [Google Scholar]
4. Furlong LA. Ectopic pregnancy risk when contraception fails. A review. J Reprod Med. 2002;47(11):881–885. [PubMed] [Google Scholar]
5. Tal J, Haddad S, Gordon N, Timor-Tritsch I. Heterotopic pregnancy after ovulation induction and assisted reproductive technologies: a literature review from 1971 to 1993. Fertil Steril. 1996;66(1):1–12. doi: 10.1016/S0015-0282(16)58378-2. [PubMed] [CrossRef] [Google Scholar]
6. Wang LL, Chen X, Ye DS, Liu YD, He YX, Guo W, Chen SL. Misdiagnosis and delayed diagnosis for ectopic and heterotopic pregnancies after in vitro fertilization and embryo transfer. J Huazhong Univ Sci Technolog Med Sci. 2014;34(1):103–107. doi: 10.1007/s11596-014-1239-7. [PubMed] [CrossRef] [Google Scholar]
7. Dart RG, Kaplan B, Varaklis K. Predictive value of history and physical examination in patients with suspected ectopic pregnancy.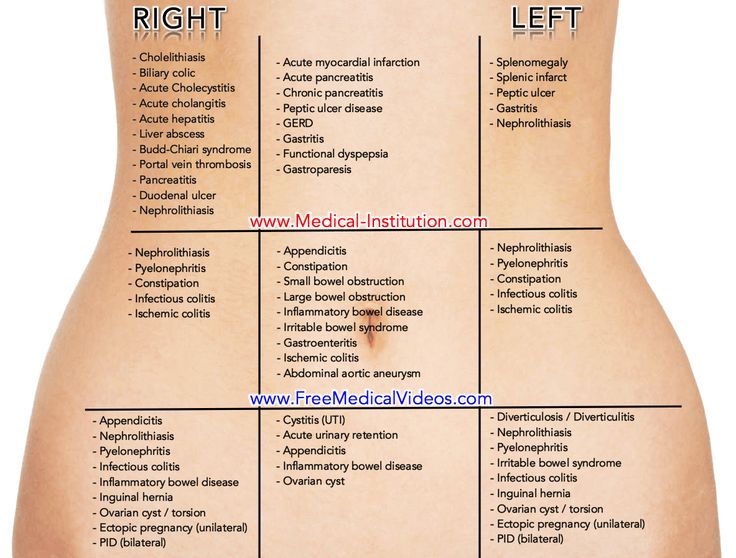 Ann Emerg Med. 1999;33(3):283–290. doi: 10.1016/S0196-0644(99)70364-1. [PubMed] [CrossRef] [Google Scholar]
Ann Emerg Med. 1999;33(3):283–290. doi: 10.1016/S0196-0644(99)70364-1. [PubMed] [CrossRef] [Google Scholar]
8. Barnhart K, Sammel MD, Chung K, Zhou L, Hummel AC, Guo W. Decline of serum human chorionic gonadotropin and spontaneous complete abortion: defining the normal curve. Obstet Gynecol. 2004;104(5, Part 1):975–981. doi: 10.1097/01.AOG.0000142712.80407.fd. [PubMed] [CrossRef] [Google Scholar]
9. Silva C, Sammel MD, Zhou L, Gracia C, Hummel AC, Barnhart K. Human chorionic gonadotropin profile for women with ectopic pregnancy. Obstet Gynecol. 2006;107(3):605–610. doi: 10.1097/01.AOG.0000198635.25135.e7. [PubMed] [CrossRef] [Google Scholar]
10. Stein JC, Wang R, Adler N, Boscardin J, Jacoby VL, Won G, Goldstein R, Kohn MA. Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann Emerg Med. 2010;56(6):674–683. doi: 10.1016/j.annemergmed.2010.06.563. [PubMed] [CrossRef] [Google Scholar]
11. Moore C, Todd WM, O'Brien E, Lin H.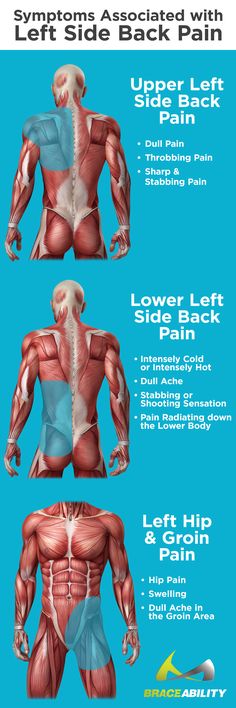 Free fluid in Morison’s pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007;14(8):755–758. doi: 10.1197/j.aem.2007.04.010. [PubMed] [CrossRef] [Google Scholar]
Free fluid in Morison’s pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007;14(8):755–758. doi: 10.1197/j.aem.2007.04.010. [PubMed] [CrossRef] [Google Scholar]
12. Beals T, Naraghi L, Grossestreuer A, Schafer J, Balk D, Hoffmann B. Point of care ultrasound is associated with decreased emergency department length of stay for symptomatic early pregnancy. Am J Emerg Med. 2019;S0735-6757(19):30174–30173. [PubMed] [Google Scholar]
13. Murray H, Baakdah H, Bardell T, Tulandi T. Diagnosis and treatment of ectopic pregnancy. Can Med Assoc J. 2005;173(8):905–912. doi: 10.1503/cmaj.050222. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Articles from BMC Emergency Medicine are provided here courtesy of BioMed Central
Pelvic Pain After Miscarriage - Lake City PT
Suffering a miscarriage is one of the most devastating experiences for a pregnant person. Feelings of distress, hopelessness, and even trauma can be amplified if the pregnancy was wanted and planned. While so incredibly harrowing, sadly miscarriages are also not uncommon.
Feelings of distress, hopelessness, and even trauma can be amplified if the pregnancy was wanted and planned. While so incredibly harrowing, sadly miscarriages are also not uncommon.
Right now, estimates tell us that around 26% of all pregnancies end in a miscarriage. Besides the natural emotional pain and psychological distress, miscarriages can also affect your body in different ways. Pelvic pain, for example, is a commonly reported physical side effect of miscarriages.
Types of Miscarriage
In gynecology, miscarriage is defined as the spontaneous loss of a pregnancy before the 20-week mark. When a baby dies after the 20th week of gestation, the term most commonly used is “stillbirth”.
Unfortunately, there are several different types of miscarriages, all with different signs and symptoms.
Chemical Pregnancy
Chemical pregnancies are one of the earliest types of miscarriage. They tend to happen before a pregnancy has reached its fifth week, which is also why they are not always easily identified as miscarriages but can be mistaken for heavy periods.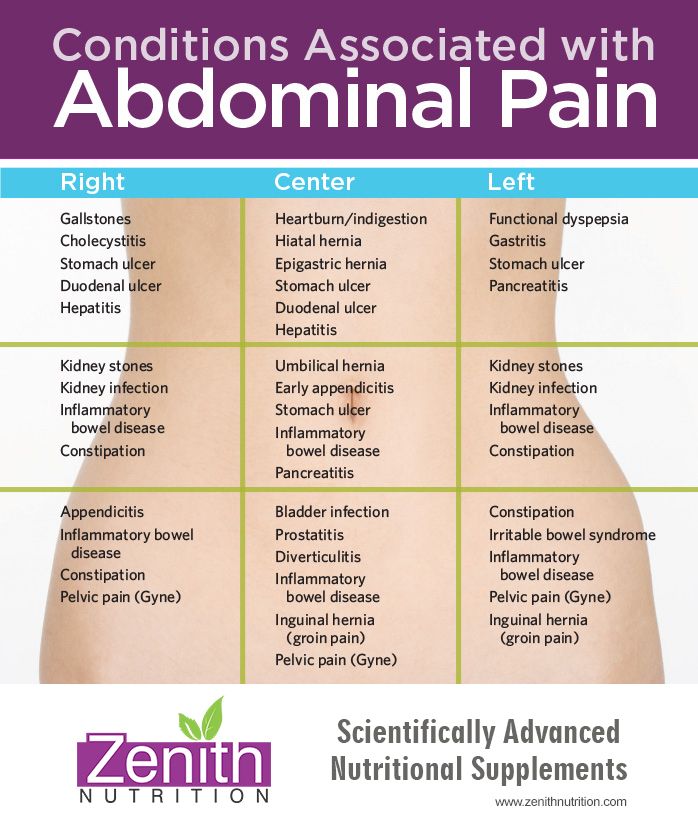
First-Trimester Miscarriage
Most miscarriages happen in the first trimester of pregnancy, which ends at around 12 weeks. During a first-trimester miscarriage, a person can experience heavy bleeding, pelvic pain, back pain, and severe nausea or sickness.
Second-Trimester Miscarriage
While less reported and only affecting a very small percentage of the overall pregnant population, second-trimester miscarriages do happen. They present similar symptoms as first-trimester losses, although these are generally more intense as the pregnancy has progressed over a number of weeks.
Missed Miscarriage
Most miscarriages can be diagnosed when a pregnant woman starts noticing physical symptoms such as severe pain, cramps, and bleeding. However, some women do not report any symptoms at all: this is what happens with a missed miscarriage.
Missed miscarriages tend to occur in the first trimester of pregnancy, although they can also happen at a later gestational age.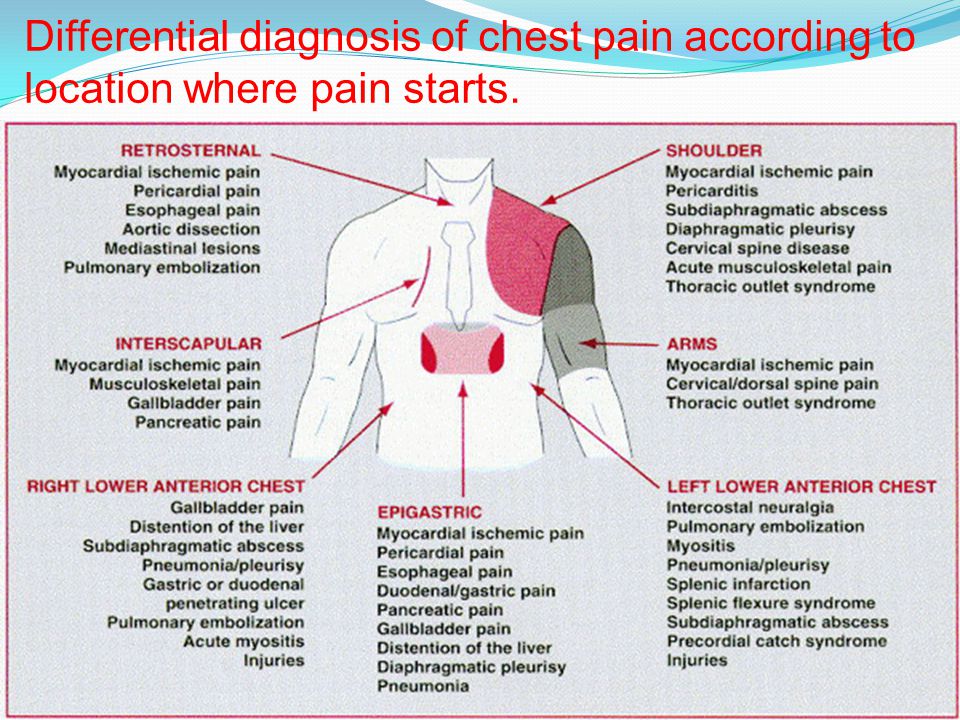
Ectopic Pregnancy
An ectopic pregnancy is a type of miscarriage in which the embryo does not develop inside the womb but somewhere else, such as in one of the Fallopian tubes. Embryos developing outside the womb have no chance of survival, which is why ectopic pregnancies are classified as miscarriages.
Molar Pregnancy
When a mass of non-fetal tissue grows inside the uterus, a molar pregnancy occurs. This mass, medically called a “mole”, is the result of abnormal conception and can be diagnosed during a first-trimester ultrasound.
Blighted Ovum
Also known as “anembryonic pregnancy”, a blighted ovum happens when the fertilized egg implants correctly into the womb but does not grow into an embryo despite its gestational sac continuing to develop.
Can Pelvic Pain Signal Imminent Miscarriage?
While post-miscarriage pelvic pain is normal, it is also important to note that this type of pain while the pregnancy is still ongoing might be a sign of imminent miscarriage. Some of the most common signs that a miscarriage might be about to happen include:
Some of the most common signs that a miscarriage might be about to happen include:
- Vaginal bleeding
- Loss of fluid or tissue from the vagina
- Loss of the main pregnancy symptoms
- Abdominal pain and cramps
- Pelvic pain
As you might expect, the intensity and severity of cramps and pelvic pain increase the longer a pregnancy goes on. While in early pregnancy you can alleviate miscarriage-associated pelvic pain by using over-the-counter medication, taking warm baths, or applying a hot water bottle to the affected area, these remedies do not tend to work so well if you are miscarrying in your second trimester.
Post-Miscarriage Pelvic Pain
After a miscarriage, you may experience pelvic pain that varies in severity and intensity depending on how far along you were in your pregnancy. For example, if you experience a miscarriage in the first trimester, your pain might feel similar to pregnancy cramps, and it might last only for a few days.
However, if your miscarriage happens later in pregnancy, your pelvic pain, cramps, and bleeding will be stronger, and they will take longer to ease and disappear completely. If you start feeling or being sick and running a fever alongside your pelvic pain after a miscarriage, seek medical attention right away, as it might be a sign of infection.
Miscarriage Recovery
The recovery journey after a miscarriage can be long and complex, as it involves lots of different aspects of a woman’s life. It’s essential that you allow yourself the time and space you need to grieve and come to terms with what has happened to you and your baby, without letting anyone else force you to “rush” things or expect you to feel better quickly.
Recovery must happen from an emotional, psychological, and physical point of view. Emotionally, you may find solace in confiding in your partner, family, and friends, as well as connecting with other people who have been through a similar experience. Psychologically, you may be advised to attend some counselling sessions, in order for a trusted professional to help you process your feelings.
Psychologically, you may be advised to attend some counselling sessions, in order for a trusted professional to help you process your feelings.
Your body, too, will need the right type of care following a miscarriage. Once again, it’s paramount to rely on the support of a qualified expert who can accompany you on your journey towards restoring your body to its health.
Choosing Physical Therapy for Pelvic Pain
As we mentioned, pelvic pain is one of the most commonly reported concerns that plague women after a miscarriage. This is because the pelvis is one of the areas that are most affected by the physiological and hormonal changes that the pregnant body goes through – even in very early pregnancy.
In order to re-establish the correct strength, health, and balance in your pelvis region post-miscarriage, you might want to look into physical therapy for pelvic pain. At Lake City PT, we specialize in diagnosing and treating post-miscarriage pelvic pain.
Get in touch with us today and schedule your initial consultation. One of our expert therapists will be happy to see you and offer you all the support you need to create a bespoke treatment for your pelvic pain.
One of our expert therapists will be happy to see you and offer you all the support you need to create a bespoke treatment for your pelvic pain.
Hippocrates Clinic - Pain after miscarriage
Miscarriage occurs as a result of a natural termination of pregnancy during the first 20 weeks. Pregnancy is terminated in 20% of pregnant women, while 50% of these women do not even know about their "interesting" position. A miscarriage can occur before the implantation of the embryo, then the fertilized egg comes out along with the menstrual flow. Often implantation of can fail: the pregnancy is terminated almost immediately after implantation, accompanied by bleeding.
Pain after a miscarriage may be due to remnants of the ovum or endometrium in the uterus.
At the first signs of pain, the doctor prescribes curettage to remove the remaining tissue in the uterine cavity. Pain in this case is localized in the lower abdomen, in the lower back. The pain is sharp, cutting, tingling in the ovaries, fever, profuse blood discharge with clots can be observed.
Pain after miscarriage may be associated with cause of termination of pregnancy : inflammation, infection, chronic disease in the genitals, hormonal imbalance. Pain immediately after a miscarriage is cramping in nature, dizziness, slight nausea may occur. This is due to the intense contraction of the uterus and its contraction to its normal size.
Pain after miscarriage and adnexitis
Pain after miscarriage is often caused by the fact that the remnants of the endometrium and the ovum remained in the uterine cavity. Sometimes even after scraping small pieces of endometrium may remain. Dead tissues often provoke the development of inflammatory and infectious diseases of the genital organs. One of the most common diseases after a miscarriage is adnexitis.
Inflammation of the ovaries and appendages most often manifests itself after curettage, as well as with incomplete removal of dead tissues and the fetus during miscarriage. Pain in this case is of a particularly acute nature: a cutting, stabbing sensation in the region of the ovaries, severe pulling pain in the lower back, profuse bleeding. Adnexitis manifests itself as acute pain and in the absence of bleeding. This is due to strong inflammatory processes in the ovaries. Often in women there is a violation of the menstrual cycle, anovulation, an increase in body temperature, a decrease in mood.
Pain in this case is of a particularly acute nature: a cutting, stabbing sensation in the region of the ovaries, severe pulling pain in the lower back, profuse bleeding. Adnexitis manifests itself as acute pain and in the absence of bleeding. This is due to strong inflammatory processes in the ovaries. Often in women there is a violation of the menstrual cycle, anovulation, an increase in body temperature, a decrease in mood.
Pain after miscarriage and adenomyosis
Pain after miscarriage is often indicative of disorders in the female genital organs. This can be caused by partial release of dead fetal tissues and uterine mucosa from its cavity. Pain after a miscarriage has spasmodic , cramping in nature, there is a sharp pain in the ovaries and lower back.
Remnants of the endometrium, microflora disorders, hormonal failure often lead to abnormal growth of the tissues of the uterine mucosa.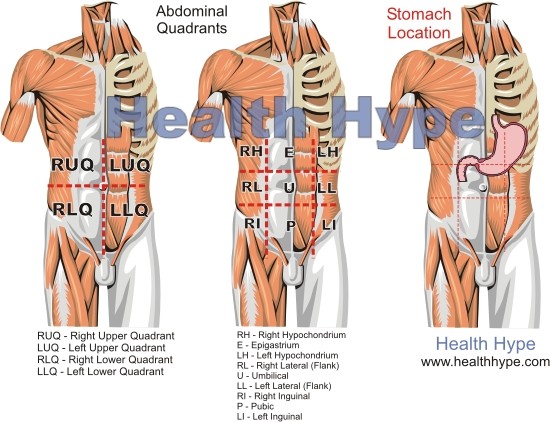 This disease is accompanied by the formation of inflammatory foci in places where the endometrium grows into the muscle tissue of the uterus. These foci provoke extramenstrual bleeding, pain in the lower abdomen throughout the cycle and in the future - by changes in the shape of the uterus and infertility.
This disease is accompanied by the formation of inflammatory foci in places where the endometrium grows into the muscle tissue of the uterus. These foci provoke extramenstrual bleeding, pain in the lower abdomen throughout the cycle and in the future - by changes in the shape of the uterus and infertility.
Pain after a miscarriage and algomenorrhea
Pain after a miscarriage occurs if there is some kind of disorder. If the miscarriage did not occur completely, then the remnants of tissues in the uterine cavity could trigger inflammatory processes and provoke pain in the lower abdomen. Curettage often causes inflammation of the mucous membrane of the uterus, ovarian dysfunction and infection. Hormonal disorders during miscarriage in combination with inflammation can change the nature of menstruation, pain symptoms may be more pronounced. These disorders often lead to algomenorrhea or aggravation of its symptoms.
After a miscarriage, algomenorrhea can become more acute : the lower abdomen may hurt more, the chest may swell and hurt. Headaches often appear, weakness of the body is felt more strongly. Significantly reduced work capacity. Against the background of a miscarriage, the psychological state may worsen throughout the entire cycle: depression, apathy appear, appetite and mood decrease.
Pain after miscarriage and amenorrhea
Miscarriage occurs for a number of reasons, depending on the characteristics of the woman's body. Almost every abortion at a later date (6-20 weeks) is accompanied by pain sensations . Every fourth miscarriage provokes violation of the menstrual cycle . A sharp hormonal decline, the stressful state of the body, inflammatory processes after scraping become the cause of amenorrhea - the absence of menstruation.
Amenorrhea after a miscarriage may manifest itself as pinkish discharge, pulling pains in the lower abdomen, periodic swelling and soreness of the chest. In case of amenorrhea, absence of ovulation is observed . Often amenorrhea can occur as a result of severe stress on the body after a miscarriage and thus the ovaries rest before a new pregnancy.
In case of amenorrhea, absence of ovulation is observed . Often amenorrhea can occur as a result of severe stress on the body after a miscarriage and thus the ovaries rest before a new pregnancy.
Pain after miscarriage and anovulatory cycle
Pain after miscarriage is often associated with hormonal disorders and inflammatory processes in the genitals. Violation of ovarian function after termination of pregnancy provokes a failure of the menstrual cycle, irregular bleeding, anovulation. A common consequence of a miscarriage is an anovulatory cycle. It's related to an insufficient amount of pituitary and hypothalamic hormones to regulate the functioning of the ovaries, the formation of eggs, follicles and the corpus luteum. Ovarian dysfunction leads to the onset of an anovulatory cycle and the absence of the process of egg maturation. It is the violation of ovulation that causes acquired infertility in women who have had a miscarriage.
Pain after miscarriage and leucorrhea
Pain after miscarriage and leucorrhoea associated with abortion and removal of the fetus and amniotic membranes. Incomplete excretion of the fetus and endometrium leads to inflammation and multiplication of bacteria, which can provoke the development of dangerous diseases. If a miscarriage occurred at a gestational age of more than 3 weeks, then doctors in most cases assign scraping. Residual tissues can cause not only inflammation, but also decomposition, decay of fetal tissues. This provokes serious consequences with the possibility of blood poisoning. Leucorrhoea after a miscarriage in the early stages is bloody, profuse, reminiscent of menstruation. In this case, removal of clots and constant acute pain in the lower abdomen is possible. Discharge and pain may last one to three days. The pain after curettage is pulling, dull, encircling the lower abdomen. The leucorrhoea is dark brown, not very copious, and lasts about a week. Profuse bleeding with sharp pain in the lower abdomen may be a sign of profuse curettage and damage to uterine mucosa.
Profuse bleeding with sharp pain in the lower abdomen may be a sign of profuse curettage and damage to uterine mucosa.
Which doctors should I contact?
- Gynecologist
- Gynecologist-endocrinologist
Miscarriage. What to do after a miscarriage?
When a woman finds out about her pregnancy, she changes her rhythm of life, especially if the pregnancy is desired. However, depending on many circumstances, miscarriage , that is, a natural termination of pregnancy, may occur. Statistics say that up to 20 percent of pregnancies end in pathological abortions. Often a woman may not know that she was pregnant, as a miscarriage sometimes occurs at a very early stage and seems to be just a normal delay in menstruation followed by heavy discharge.
If a woman finds out that she is pregnant and wants to become a mother, she should be very attentive to her condition. The threat of miscarriage often occurs in the early stages of pregnancy and therefore it is necessary to know what symptoms and signs precede a sudden miscarriage.
Signs
The main sign of a suspected miscarriage is bleeding from the uterus. They happen not abundant, pale scarlet or gray-brown. The discharge most often gradually increases and is characterized by sudden spasms or pulling pains in the lower abdomen. These symptoms may last for some time.
The pains are often so mild that the woman simply does not pay attention to them. They are able to be interrupted, and the woman simply forgets about them, especially if the discharge also stopped, and before that they were insignificant. Meanwhile, the very first symptoms should alert you and you should urgently go to the gynecologist for examination and consultation. Even if the process has stopped, after a few days you can feel a sharp deterioration in health, and then you can no longer save the life of the unborn child. Be sure to pay attention to what exactly comes out with the discharge, if there are tissue fragments, it means that miscarriage has already occurred. Therefore, one should not hesitate to go to the doctor, the fetus may come out, in whole or in parts, there may be white particles or a round gray bubble. When the body is completely cleansed, the pain will subside, but before that it may continue for some time.
Therefore, one should not hesitate to go to the doctor, the fetus may come out, in whole or in parts, there may be white particles or a round gray bubble. When the body is completely cleansed, the pain will subside, but before that it may continue for some time.
Terms of miscarriages
A miscarriage is classified as early if it occurred before twelve weeks from the onset of pregnancy. Starting from the 22nd week, if a spontaneous miscarriage has occurred, it is considered late. If the termination of pregnancy occurred before thirty-seven weeks, then this is already called premature birth. All subsequent fetal rejections are called term births and are generally considered normal, since during this period, mostly able-to-survive children are born. In modern medicine, children born after 22 weeks are nursed and subsequently do not differ from those born at term with normal weight.
Types of miscarriages
Specialists have identified several types of miscarriages.
- Complete or unavoidable - characterized by pain in the lower back and dilatation of the cervix, hemorrhages from it. The fetal membrane necessarily bursts, and the pregnancy is terminated. The fetus comes out of the uterus, and all discomfort in the form of pain and bleeding stops.
- Miscarriage is different in that the fetus died, but remained in the mother's body. This can be detected by a doctor when examining a woman and when listening to the fetal heartbeat.
- Repeated miscarriage is rare, it occurs only some time after the first and can occur up to three times in a row in the early stages.
Causes of spontaneous abortion
The vast majority of women, having learned about their pregnancy, want to give birth to a healthy baby. And if there is a spontaneous miscarriage , then for a failed mother this is a real tragedy. Many, having experienced an abortion, try to conceive a child faster again, but first you need to know the reasons for what happened in order to save the fetus in the future. According to statistics, the largest number of miscarriages occurs precisely in the early stages.
Many, having experienced an abortion, try to conceive a child faster again, but first you need to know the reasons for what happened in order to save the fetus in the future. According to statistics, the largest number of miscarriages occurs precisely in the early stages.
There are several reasons for this:
- Violations in genetics.
This is the most common cause of miscarriage. This is not due to heredity, it is a consequence of the mutation of parent germ cells, which accidentally ended up in unfavorable conditions. This is also the influence of radiation, poisoning, viruses, that is, temporary situations that affected the quality of germ cells. The body thus gets rid of a weak non-viable fetus. It is impossible and unnecessary to prevent such spontaneous abortion. It is only necessary, having decided to become pregnant, to try to cleanse your body of possible harmful influences.
- Hormonal disorders
The cause of miscarriage at a very early stage also lies in the lack of the hormone progesterone, or in the fact that a woman has an excess of male sex hormones that suppress the production of estrogen and progesterone in her body. In this case, the fetus can be saved medically by administering the necessary medicines to the woman. The work of the adrenal glands, as well as the thyroid gland, affects the production of hormones, so a lot depends on the work of these glands throughout the pregnancy process.
In this case, the fetus can be saved medically by administering the necessary medicines to the woman. The work of the adrenal glands, as well as the thyroid gland, affects the production of hormones, so a lot depends on the work of these glands throughout the pregnancy process.
- Immunological causes .
In this case, the vitality of the fetus is directly affected by the Rh conflict. The embryo will inherit the positive Rh of the man, and if the partner has a negative Rh, then her body simply rejects cells that are foreign to him. A similar situation can be prevented by injecting the expectant mother with a variety of progesterone, a process called immunomodulation.
Sexually transmitted infections such as toxoplasmosis, syphilis, trichomoniasis, chlamydia and others are of great danger. External infection: bacteria and viruses infect the fetal membranes, and the body will inevitably reject the embryo. Therefore, before becoming pregnant, you should be examined to know for sure that there are no infections, and if the result is positive, undergo treatment.
In addition, all inflammatory processes, various diseases of the internal organs, which are accompanied by a persistent high temperature, can also lead to unexpected rejection of the fetus. Rubella is especially dangerous, and viral hepatitis is common. But even a sore throat, mild pneumonia, appendicitis sometimes play a key role and lead to a miscarriage, so the expectant mother must undergo a thorough examination even before the child is conceived, and then beware of all kinds of infections and weakening of the body.
- Medical abortion.
If a woman had an abortion in a hospital and then became pregnant and decided to give birth, there is a risk that she will have a miscarriage. Abortion is a stress factor for the body, ovarian dysfunction is often observed, inflammatory processes in the female genital organs can begin, and all this will lead, at best, to miscarriage and subsequent repeated miscarriages, and at worst, to infertility. Therefore, you need to think very seriously before going for an abortion.
Therefore, you need to think very seriously before going for an abortion.
- Medicines and certain herbs.
It is advisable for a pregnant woman not to take any medication at all, especially during the first three calendar months. Medicines and herbs can cause various defects in the fetus, which in turn will lead to its rejection. Analgesics and uncontrolled hormonal contraceptives are especially dangerous. Parsley and nettle should be eaten with caution - they cause a high tone of the uterus, which in turn can reject the fetus.
- Stress.
It is no coincidence that in ancient times, pregnant women were protected from unrest, they were created comfortable conditions, they tried to give as many positive emotions as possible. Now the direct dependence of the health of the unborn baby on the mental state during pregnancy has already been proven. Any stress, fear and overstrain can cause an unexpected termination of pregnancy. If you have a problem (death of a loved one, divorce, etc.), you need to find sedatives with the help of a doctor, they will help you cope with this period.
If you have a problem (death of a loved one, divorce, etc.), you need to find sedatives with the help of a doctor, they will help you cope with this period.
- Unhealthy lifestyle.
Of course, the intake of alcoholic beverages, an unhealthy lifestyle, smoking, even coffee consumption in large quantities, improper diet - all this can lead to a transient miscarriage. Therefore, the expectant mother should prioritize and change her rhythm of life in advance in order to give birth to a healthy child.
- Sexual intercourse, falling, heavy lifting.
All of these factors can affect the fetus, so you should protect yourself and your baby by avoiding these activities.
What to do after a miscarriage?
Having experienced the tragedy of losing a child, parents often intend to immediately conceive a new baby, but they are afraid that everything will happen again. In this case, you do not need to make independent decisions, but consult a doctor. And first of all, it is necessary to identify the cause that led to the miscarriage. For this, the expectant mother needs to undergo as thorough an examination as possible.
In this case, you do not need to make independent decisions, but consult a doctor. And first of all, it is necessary to identify the cause that led to the miscarriage. For this, the expectant mother needs to undergo as thorough an examination as possible.
If no obvious cause is found, the fetus most likely has a chromosomal abnormality. In this case, you should not worry, since the next conception will occur with a different set of chromosomes, which means that there will be no repeated miscarriage. If the miscarriage was repeated, it is necessary to contact a geneticist and conduct a study of the set of chromosomes of both parents. If it turns out that the cause was an infection, then it is necessary to fully recover. If we are talking about sexual infections, then both parents need to undergo therapy. It is necessary to take tests for hormonal studies, hemostasis systems and determine the immune status.
After a miscarriage, should be treated, if necessary, and pause between conceptions. During pregnancy, you should not take medications to prevent re-spontaneous pathological termination of pregnancy. Therefore, you can become pregnant only after the end of the course of treatment. If the cause was hormonal abnormalities, then the expectant mother should take special drugs to stabilize the background, and at this time she should never become pregnant. During the pause, you need to choose contraceptives with the help of a doctor. You can go to a specialized clinic where you will be prescribed a full course of rehabilitation.
During pregnancy, you should not take medications to prevent re-spontaneous pathological termination of pregnancy. Therefore, you can become pregnant only after the end of the course of treatment. If the cause was hormonal abnormalities, then the expectant mother should take special drugs to stabilize the background, and at this time she should never become pregnant. During the pause, you need to choose contraceptives with the help of a doctor. You can go to a specialized clinic where you will be prescribed a full course of rehabilitation.
The first week after a miscarriage women often experience pain in the lower abdomen, heavy bleeding, so you should refrain from sexual intercourse with a man. If there is severe bleeding, acute pain in the lower abdomen, convulsions, high fever, palpitations, nausea, vomiting, then you should immediately consult a doctor to identify the cause of this condition. It is necessary to plan a subsequent pregnancy not earlier than three months after this situation, but preferably six months later. Until that time, it is worth reconsidering your outlook on life, giving up hard work, eating right and wisely, taking vitamins, exercising, losing weight if you are overweight, stop smoking, drinking alcohol, think over your daily routine.
Until that time, it is worth reconsidering your outlook on life, giving up hard work, eating right and wisely, taking vitamins, exercising, losing weight if you are overweight, stop smoking, drinking alcohol, think over your daily routine.
It is very important during this recovery period to have a positive attitude and confidence that the next attempt will be successful. This is harder to do than to say, because after a miscarriage the woman is in a depressed state and is afraid of a repetition of the situation. You can’t get hung up on your problem, during this period it’s better to do some favorite thing, relax, change the situation, travel, visit the city more often. The modern ecological situation in cities has a bad effect on women's health, so private trips to nature, a trip to the sea, to friends in another city can distract from painful thoughts. An important role in this case is played by the woman's relatives and, above all, the husband, who can surround her with care and attention, creating peace of mind.