How does birth work
Labor | Johns Hopkins Medicine
What You Need to Know
- Labor is a series of continuous, progressive contractions of the uterus that help the cervix dilate (open) and efface (thin). This allows the fetus to move through the birth canal.
- Labor usually starts two weeks before or after the estimated date of delivery. However, the exact trigger for the onset of labor is unknown.
- While the signs of labor may vary, the most common are contractions, rupture of the amniotic sac (“breaking your water”) and bloody show.
- Labor is typically divided into three stages: dilation and effacement of the cervix, pushing and the delivery of the placenta.
- Pain management options during labor include nonmedicated measures, analgesics and anesthesia.
Definition of Labor
Labor is a series of continuous, progressive contractions of the uterus that help the cervix dilate and efface (thin out). This lets the fetus move through the birth canal. Labor usually starts two weeks before or after the estimated date of delivery. However, the exact trigger for the onset of labor is unknown.
Signs of Labor
While each woman experiences labor differently, some common signs of labor may include:
-
Bloody show. A small amount of mucus, slightly mixed with blood, may be expelled from the vagina.
-
Contractions. Uterine muscle spasms that occur at intervals of less than 10 minutes may signify that labor has started. These may become more frequent and severe as labor progresses.
-
Rupture of the amniotic sac (bag of water). If you experience amniotic fluid gushing or leaking from your vagina, go to the hospital immediately and contact your health care provider. Most women go into labor within hours of the amniotic sac breaking. If labor does not begin soon after rupturing your amniotic sac, you will be given medications to induce your labor.
 This step is often taken to prevent infection and other delivery complications.
This step is often taken to prevent infection and other delivery complications.
If you are unsure about the start of your labor, call your health care provider.
Different Stages of Labor
Typically, labor is divided into three stages:
-
First stage. During the onset of labor, your cervix will complete dilation. Early in this stage, you may not recognize that you are in labor if your contractions are mild and irregular. Early labor is divided into two phases:
-
The latent phase is marked by strong contractions that usually occur at five- to 20-minute intervals. During this phase, your cervix will dilate approximately 3 to 4 centimeters and efface. This is usually the longest and least intense phase of labor. You may be admitted to the hospital during this phase. Your doctor will perform pelvic exams to determine the dilation of the cervix.
-
The active phase is signaled by the dilation of the cervix from 4 to 10 centimeters.
 Your contractions will likely increase in length, severity and frequency, occurring at three- to four-minute intervals. In most cases, the active phase is shorter than the latent phase.
Your contractions will likely increase in length, severity and frequency, occurring at three- to four-minute intervals. In most cases, the active phase is shorter than the latent phase.
-
-
Second stage. Often referred to as the pushing stage of labor, this stage starts when your cervix is completely opened and ends with the delivery of your baby. During the second stage, you become actively involved by pushing the baby through the birth canal. Crowning occurs when your baby’s head is visible at the opening of the vagina. The second stage is usually shorter than the first stage, and may take between 30 minutes and three hours for your first pregnancy.
-
Third stage. After your baby is delivered, you will enter the third and final stage of labor. This stage involves the passage of the placenta (the organ that nourished your baby inside of the uterus) out of the uterus and through the vagina.
 The delivery of the placenta may take up to 30 minutes.
The delivery of the placenta may take up to 30 minutes.
Since each labor experience is different, the amount of time required for each stage will vary. If labor induction is not required, most women will deliver their baby within 10 hours of being admitted to the hospital. Labor is generally shorter for subsequent pregnancies.
Johns Hopkins Hospital Designated as Baby-Friendly
The Baby-Friendly Hospital Initiative, a global program launched by the World Health Organization and the United Nations Children’s Fund, has designated The Johns Hopkins Hospital as Baby-Friendly. This designation is given to hospitals and birthing centers that offer an optimal level of care for infant feeding and mother-baby bonding.
Learn more
Induction of Labor
In some cases, labor has to be induced or stimulated to begin.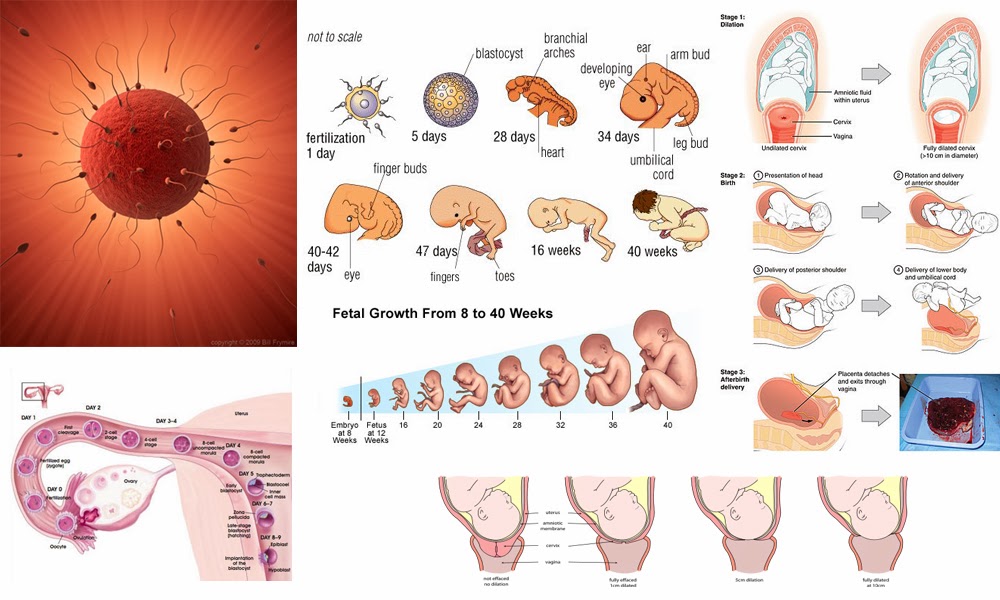 The reasons for induction vary. Labor induction is not initiated before 39 weeks of pregnancy unless there is a problem. The most common reasons for induction include the following:
The reasons for induction vary. Labor induction is not initiated before 39 weeks of pregnancy unless there is a problem. The most common reasons for induction include the following:
-
The mother or fetus is at risk due to complications.
-
The pregnancy has continued too far past the due date.
-
The mother has pre-eclampsia, eclampsia or chronic high blood pressure.
-
The fetus has been diagnosed with poor growth.
Labor may be induced by:
-
Inserting vaginal suppositories that contain prostaglandin to stimulate contractions.
-
Giving an intravenous (IV) infusion of oxytocin (a hormone produced by the pituitary gland that stimulates contractions) or a similar drug.
-
Artificially rupturing the amniotic sac.
Hospital Care During Labor
When you first arrive at the hospital in labor, the nursing staff may perform a physical exam of your abdomen to determine the size and position of the fetus.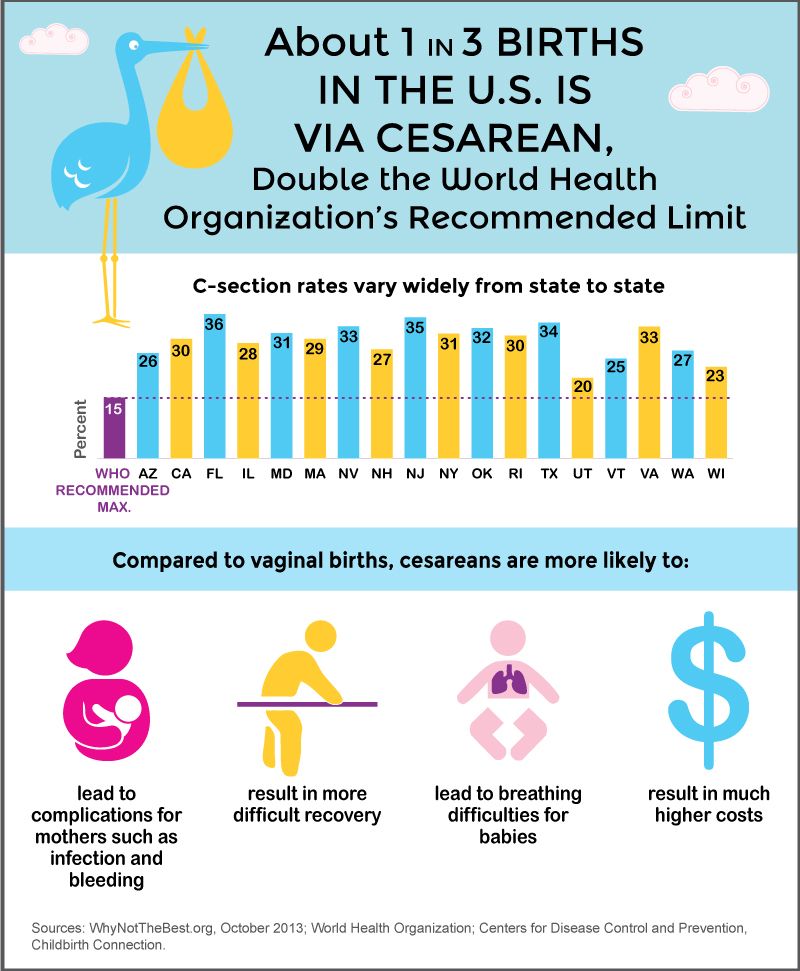 The nurses may also examine your cervix for dilation and effacement.
The nurses may also examine your cervix for dilation and effacement.
To monitor your health, the nursing staff may check the following:
In addition, your baby’s health is carefully monitored during labor. A monitor may be placed over your abdomen to keep track of the fetal heart rate.
You may receive IV fluids during labor. The IV line, a thin, plastic tube inserted into a vein (usually in your forearm), can also be used to give medicine. IV fluids are usually given once active labor has begun and when you have epidural anesthesia.
Pain Management Options During Labor
You have many options to relieve pain during labor and delivery. In general, you and your health care provider should choose the safest, most effective method of pain relief available. This decision will be determined by your:
The following are the most common natural and medication-based methods for managing the pain associated with labor and delivery:
Nonmedicated Pain Management
As part of natural childbirth, these pain management strategies provide comfort and relieve stress without the use of medication. Many women have successfully learned natural techniques to help them feel more comfortable and in control during labor and birth. These techniques include:
Many women have successfully learned natural techniques to help them feel more comfortable and in control during labor and birth. These techniques include:
-
Relaxation. This technique can improve your ability to detect and release tension. During progressive relaxation, you can learn to relax various muscle groups in series.
-
Touch. This may include massage or light stroking to relieve tension. A jetted bath or a shower during labor may also help relieve pain or tension. Ask your health care provider before taking a tub bath during labor.
-
Hot or cold therapy. A warm towel or a cold pack may help relax tense or painful areas.
-
Imagery. Using the mind to form mental pictures may help create and promote relaxed feelings.
-
Meditation or focused thinking. Meditation helps your mind focus on an object or task, such as breathing, instead of discomfort.
-
Breathing. These techniques use different patterns and types of breathing to help direct your mind away from discomfort.
-
Positioning and movement. Many women find that changing positions and moving around during labor helps to relieve discomfort and may even accelerate the process. Rocking in a rocking chair, sitting in the Tailor sit position, sitting on a special birthing ball, walking or swaying may also help relieve discomfort. Your health care provider can help you find comfortable positions that are safe for you and your baby.
Medicated Pain Management
Analgesics. Pain relief medications, such as meperidine, may be used during labor in small amounts with very few complications. However, if given in large amounts or in repeated doses, analgesics can slow the activity of the breathing center in the brain of the mother and child.
Anesthesia. This type of medicine is designed to cause a loss of sensation in various areas of the body. Anesthesia medications include:
-
Local block. Anesthesia injected in the perineal area (the area between the vagina and rectum) numbs the area for repair of a tear or episiotomy after delivery.
-
Pudendal block. Used for vaginal deliveries, this type of local anesthesia is injected into the vaginal area affected by the pudendal nerve. Since it causes complete numbness in the vaginal area without affecting the contractions of the uterus, you can remain active in pushing the baby through the birth canal.
-
Epidural anesthesia (epidural block). This type of anesthesia involves infusing numbing medications through a thin catheter that has been inserted into the space that surrounds the spinal cord in the lower back, causing a loss of sensation in the lower body.
 Infusions of medications may be increased or stopped as needed. This type of anesthesia is used during labor and for vaginal and cesarean deliveries.
Infusions of medications may be increased or stopped as needed. This type of anesthesia is used during labor and for vaginal and cesarean deliveries.The most common complication of epidural anesthesia is low blood pressure in the mother. Because of this, most women need to have an intravenous infusion of fluids before epidural anesthesia is given. Another risk of epidural anesthesia is a postpartum headache. It may develop if the epidural needle enters the spinal canal rather than staying in the space surrounding the canal. Your anesthesiologist will discuss the risks, benefits and alternatives to this method of pain management.
-
Epidural analgesia. This is sometimes called a walking epidural because the medication infused through the epidural is an analgesic. While it does help relieve pain, it does not numb your body or prohibit movement. Combinations of medications may be used in this type of epidural to provide both analgesic and anesthetic effects.
 This type of epidural may be used to relieve pain during labor and vaginal deliveries.
This type of epidural may be used to relieve pain during labor and vaginal deliveries.Similar to epidural anesthesia, the most common complication of epidural analgesia is low blood pressure in the mother. Another risk of epidural analgesia is a postpartum headache caused by the epidural needle entering the spinal canal.
-
Spinal anesthesia. This type of anesthesia involves injecting a single dose of the anesthetic agent directly into your spinal fluid. Spinal anesthesia acts very quickly and causes complete loss of sensation and loss of movement in your lower body. This type of anesthesia is often used for cesarean deliveries.
-
Spinal analgesia. This involves injecting an analgesic medication into the spinal fluid to provide pain relief without numbing. Spinal analgesia may be used in combination with epidural anesthesia or analgesia to provide pain relief during labor or after delivery.

-
General anesthesia. Often used in emergency cesarean deliveries, this type of pain relief involves administering an anesthetic agent that causes you to go to sleep.
What happens to your body during childbirth
Childbirth is challenging and complications occur, but women's bodies are designed to give birth. The shape of the pelvis, hormones, powerful muscles and more all work together to help you bring your baby into the world - before, during and after childbirth.
How your body prepares for labour
Here are some of the ways your body will prepare both you and your baby for the birth ahead.
Braxton Hicks contractions
In the weeks or days before you start having proper contractions, you may experience Braxton Hicks contractions. This is your uterus tightening then relaxing. These contractions don't usually hurt and are thought to help your uterus and cervix get ready for labour.
Braxton Hicks contractions may become more regular as you get closer to the time of birth, but unlike labour contractions, they don't change the shape of the cervix and are sometimes referred to as 'false labour'. Your midwife can tell you if you're experiencing Braxton Hicks contractions or if you are in labour by doing a vaginal examination to look at your cervix.
Changes to the cervix
As labour gets closer, your cervix softens and becomes thinner, getting ready for the dilation (widening) that will allow the baby to enter the vagina. You may also see a 'show', which is a pinkish plug of mucus, stained with blood.
Engagement
Your baby may move further down your pelvis as the head engages, or sits in place over your cervix, ready for the birth. Some women feel they have more room to breathe after the baby has moved down. This is called 'lightening'.
Rupture of the membranes, or 'waters breaking'
Some women find the sac of amniotic fluid containing the baby breaks before labour, contractions start and the fluid runs (or gushes) out of the vagina.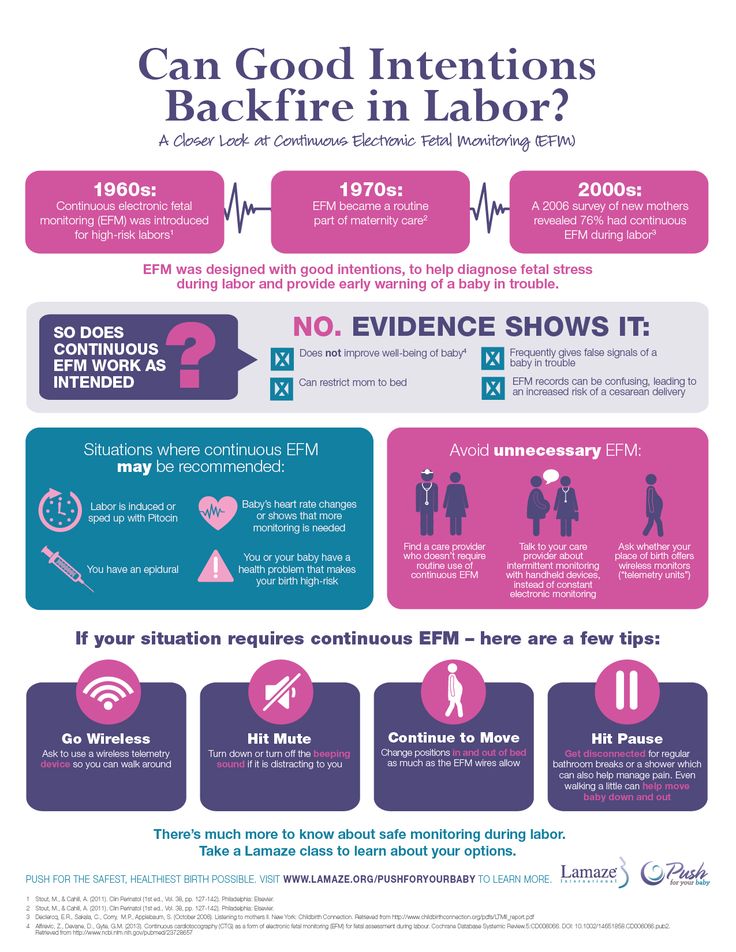 This is referred to as rupture of the membranes, or 'waters breaking'.
This is referred to as rupture of the membranes, or 'waters breaking'.
Let your maternity team know when your waters have broken and take notice of the colour of the fluid. It is usually light yellow. If it is green or red, tell your maternity team since this could mean the baby is having problems.
If your waters have broken but you have not started having regular contractions within 24 hours, you may need your labour to be induced because there is a risk of infection. Your midwife or doctor will talk to you about this.
How will you know when labour has started?
Movies often show women suddenly being struck by painful contractions and rushing to hospital. In real life, many women are not sure if they have actually started their labour.
You may feel restless, have back pain or period-like pain, or stomach disturbances such as diarrhoea.
Labour officially begins with contractions, which start working to open up the cervix. You should phone your midwife when your contractions start, although you probably won't be encouraged to come to the hospital or birthing centre until your contractions are closer together.
How the pelvis is designed for childbirth
Your pelvis is located between your hip bones. Women typically have wider, flatter pelvises than men, as well as a wider pelvic cavity (hole) to allow a baby to pass through.
The organs sitting in a woman's pelvis include the uterus, cervix and vagina, which are held together by a group of muscles. During childbirth, the muscles at the top of your uterus press down on the baby's bottom. Your baby's head then presses on your cervix which, along with the release of the hormone oxytocin (see 'How hormones help you give birth', below), brings on contractions. Your cervix should dilate so your baby can pass through it.
Your pelvis has bones and ligaments that move or stretch as the baby travels into the vagina. Your baby also has spaces between the skull bones called 'sutures', and the gaps where the sutures meet on the skull are called fontanelles. This allows for the baby's head to mould as the skull bones meet or overlap, allowing it to fit more easily as it travels through your pelvis.
This allows for the baby's head to mould as the skull bones meet or overlap, allowing it to fit more easily as it travels through your pelvis.
How hormones help you give birth
Your body produces hormones that trigger changes in your body before, during and after childbirth. Here's how they work to help you deliver your baby.
- Prostaglandin Before childbirth, a higher level of prostaglandin will help open the cervix and make your body more receptive to another important hormone, oxytocin.
- Oxytocin This hormone causes contractions during labour, as well as the contractions that deliver the placenta after the baby is born. These post-birth contractions, including more that can occur during breastfeeding, help your uterus shrink back to its normal size. Oxytocin and prolactin are the two main hormones that produce and let down breast milk for your baby. Skin-to-skin contact between a mother and baby helps to release more of these hormones.
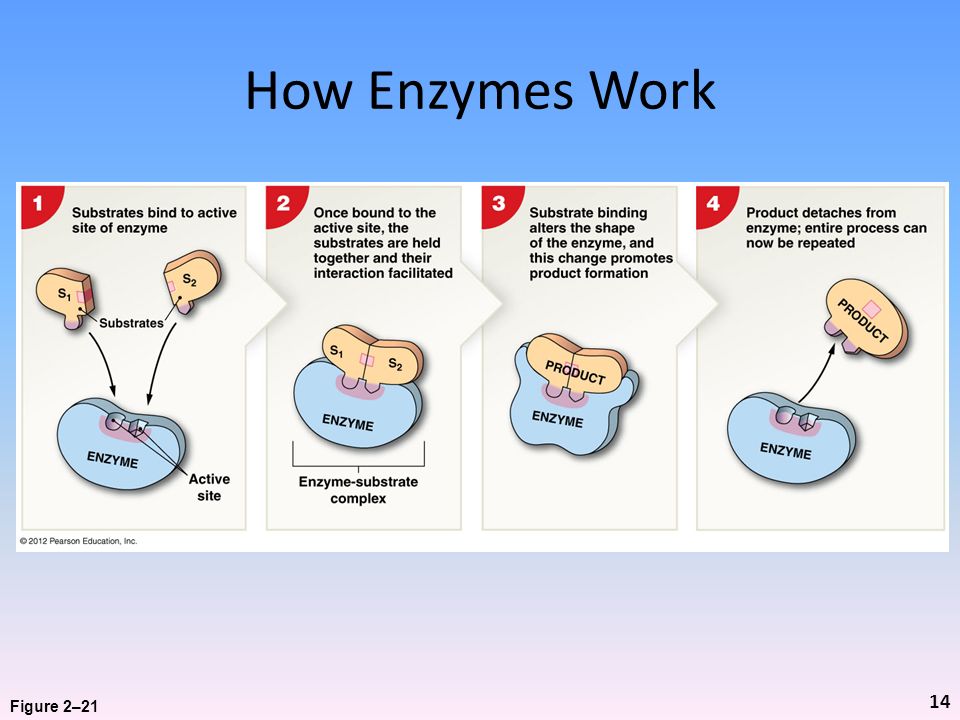
- Relaxin The hormone relaxin helps soften and stretch the cervix for birth, while helping your waters break and stretching the ligaments in your pelvis to allow the baby to come through.
- Beta-endorphins During childbirth, this type of endorphin helps with pain relief and can cause you to feel joyful or euphoric.
- 'Baby blues' After birth, your hormone balance can change again, and this is believed to cause the ‘baby blues’ in some women. You may feel teary, anxious and irritable and your mood can go up and down.
When childbirth doesn’t go to plan
Sometimes, complications can occur before or during childbirth that mean things don’t go as expected.
Sometimes, labour needs to be induced or started. There are a few ways to induce labour, including the mother being offered synthetic prostaglandin. This is inserted into the vagina to soften the cervix and start contractions.
If contractions slow down or stop during labour, the mother may be offered synthetic oxytocin from a drip to increase the contractions. In both these cases contractions can come on strongly and more pain relief may be needed. Your maternity team should explain the benefits and risks of this with you before you agree to it.
The baby could be in a posterior or breech position, not ideally placed above the cervix before the birth. Your maternity team may need to use forceps or a vacuum to help turn the baby or help the baby travel out of the vagina. Sometimes a caesarean is needed.
In rare cases, a mother may experience cephalopelvic disproportion (CPD), which is when the baby’s head is too big to fit through the pelvis. A diagnosis of CPD is usually made when labour hasn’t progressed and synthetic oxytocin has not helped. A caesarean is usually the next step.
More information
If you have any questions about childbirth or pregnancy, you can call Pregnancy, Birth and Baby on 1800 882 436, 7 days a week, to speak to a maternal health nurse.
Learn more here about the development and quality assurance of healthdirect content.
How to behave in childbirth? Learning to give birth quickly and with problems
Childbirth is a natural process, laid down by nature. The whole sequence of events that take place during this period is predetermined, but by your actions you can either speed up the birth of a baby, or complicate his birth.
Childbirth is the final and most important stage of pregnancy. How you behave and how accurately and skillfully you follow the instructions of the obstetrician depends on how you will feel and how quickly your baby will be born. What does a newborn need to know? Let's try to answer the most important questions.
1. When is it time to go to the maternity hospital?
Childbirth is a natural result of hormonal changes that occur in your body during the final stages of pregnancy. The sagging belly and heaviness in its lower part and the lumbar region speak of the imminent denouement of the story. Periodically, weak contractions occur, the stomach tenses and pulls down, but these sensations quickly pass, the uterus relaxes again and becomes soft. Such contractions are harbingers of childbirth, but they are far from real labor activity.
Periodically, weak contractions occur, the stomach tenses and pulls down, but these sensations quickly pass, the uterus relaxes again and becomes soft. Such contractions are harbingers of childbirth, but they are far from real labor activity.
The signal to call an ambulance should be sufficiently strong contractions that are repeated at regular intervals, the appearance of mucous secretions from the genital tract, slightly stained with blood, or the outflow of amniotic fluid.
2. First stage of childbirth: we breathe for two!
From the moment the contractions become regular, the first stage of labor begins, during which the strength, frequency and duration of uterine spasms increases and the cervix opens.
During spastic contraction of the uterine muscle fibers, the blood vessels that carry arterial blood to the placenta and fetus are compressed. The fetus begins to experience a lack of oxygen, and this involuntarily makes you breathe deeper. The reflex increase in the rate of contractions of your heart will ensure the delivery of oxygen to the child. Nature has provided that these processes take place regardless of your consciousness, but you should not completely rely on it.
The reflex increase in the rate of contractions of your heart will ensure the delivery of oxygen to the child. Nature has provided that these processes take place regardless of your consciousness, but you should not completely rely on it.
In the first stage of labor, during each contraction, you need to breathe calmly and deeply, trying not to hold your breath while inhaling. At the same time, the air should fill the upper sections of the lungs, as if raising the chest. You need to inhale through the nose, slowly and smoothly, exhale through the mouth, just as evenly.
3. Auto-training in the prenatal ward
To speed up the opening of the cervix, you need to walk more, but sitting is not recommended, while blood flow in the limbs is disturbed and venous blood stagnation occurs in the pelvis. From time to time it is useful to lie on your side, stroking your lower abdomen with both hands in the direction from the center to the sides, focusing on breathing and saying to yourself: "I am calm, I am in control of the situation, each contraction brings me closer to the birth of a baby. "
"
4. To relieve pain
Acupressure of the lower back can help relieve pain. Find the outer corners of the sacral rhombus on your lower back and massage these points with clenched fists.
Monitor the frequency and duration of contractions and if they weaken or sharply increase, immediately inform your doctor. In case of severe pain, you can ask for an anesthetic, but you should remember that you should not take the medicine too often, this is fraught with narcotic depression of the newborn and a decrease in his adaptive abilities.
If dilatation of the cervix causes reflex vomiting, rinse the mouth with water and then drink a few sips to replace the lost fluid. Do not drink a lot, this can provoke a recurrence of vomiting.
5. The maternity ward is not a place for tantrums
They say that difficult childbirth is a person's retribution for walking upright. Childbirth is actually a painful process, but the presence of reason allows us, representatives of the genus Homo sapiens, to control our emotions. Screaming, crying, tantrums and swearing have no place in the maternity ward. This creates a tense environment, interferes with the normal course of childbirth, complicates diagnostic and therapeutic measures, and ultimately affects their outcome.
Screaming, crying, tantrums and swearing have no place in the maternity ward. This creates a tense environment, interferes with the normal course of childbirth, complicates diagnostic and therapeutic measures, and ultimately affects their outcome.
6. Second stage of labor - pushing and expulsion of the fetus
After the baby's head slips through the dilated cervix and finds itself on the bottom of the pelvis, the pushing period of labor begins. At this time, there is a desire to push, as it usually happens during a bowel movement, but at the same time many times stronger. At first, the attempts are controllable, they can be "breathed", but by the beginning of the third stage of labor, the expulsion of the fetus, they become unbearable.
With the beginning of the straining period, you will be transferred to the delivery room. Having settled down on the delivery table, rest your feet on the special steps, firmly grasp the handrails and wait for the midwife's command.
While pushing, inhale deeply, close your mouth, clench your lips tightly, pull the handrails of the delivery table towards you and direct all the exhalation energy down, squeezing the fetus out of you. When the top of the baby appears from the genital slit, the midwife will ask you to ease your efforts. With gentle movements of her hands, she will first release the baby’s forehead, then his face and chin, after which she will ask you to push again. At the moment of the next attempt, the baby's shoulders and torso will be born. After the newborn is born, you can breathe freely and rest a little, but the birth is not over.
7. Third stage of labor and final
Third stage of labor - afterbirth. At this time, weak contractions are observed, due to which the fetal membranes gradually exfoliate from the walls of the uterus.
About 10 minutes after your baby is born, your midwife will ask you to push again to deliver your afterbirth. The doctor will carefully examine it and make sure that all parts of the membranes have come out. After that, with the help of mirrors, he will examine the cervix and make sure that it is intact. If necessary, all tears will be closed with absorbable sutures.
The doctor will carefully examine it and make sure that all parts of the membranes have come out. After that, with the help of mirrors, he will examine the cervix and make sure that it is intact. If necessary, all tears will be closed with absorbable sutures.
You will have to spend another couple of hours in the delivery room with an ice-filled bladder on your stomach. To quickly contract the uterus, you will be given injections of special drugs. When the threat of postpartum hemorrhage has passed, you will be transferred to the postpartum ward to the baby.
Childbirth completed. Ahead of the postpartum period, during which your body will recover after pregnancy.
More details on Medkrug.RU: http://www.medkrug.ru/article/show/kak_pravilno_vesti_sebja_v_rodah_uchimsja_rozhat_bystro_i_problem
Source: http://www.medkrug.ru/
So, if you have contractions or amniotic fluid has poured out, go urgently to the hospital.

In the admission department of the maternity hospital, you will be met by the midwife on duty, who will complete the necessary documents, measure blood pressure, body temperature, pelvic dimensions, and listen to the fetal heartbeat.
Sanitization: shaving of pubic hair and cleansing enema is carried out only at your request.
In the admission department, a doctor will examine you, perform an ultrasound scan, and then you will be taken to the maternity ward.
If you were admitted to the maternity hospital not fully examined or you have any infectious disease (ARVI, influenza, kidney disease, lung disease, etc.), i.e. there is a possibility of pregnancy complications and a threat to the fetus and mother, you will be hospitalized in a specialized obstetric observational department, where highly qualified specialists successfully treat and safely deliver high-risk women, minimizing the adverse effects of infection on the mother and fetus.
The obstetric observation department is a mini-maternity hospital in a maternity hospital, equipped with all the necessary equipment for high-quality and most favorable delivery and management of the postpartum period.
Observational obstetric department is isolated from other departments and premises of the maternity hospital.
Conducting and receiving childbirth in the maternity hospital around the clock is carried out by a team of highly qualified specialists with many years of experience, consisting of 8 doctors: 4 obstetrician-gynecologists, 2 anesthesiologists, a neonatologist, a neonatologist-resuscitator. In the maternity block, midwives are constantly on duty, who are personally responsible for the woman in labor.
Childbirth is taken on a special bed in the position of a woman on her back with her legs bent and spread apart or in a vertical position (in the absence of contraindications - varicose veins of the lower extremities, external genital organs, elephantiasis) - which provide for the free behavior of a woman in childbirth, the possibility of taking soul, holding the second stage of labor in a “vertical position”, which allows the baby to be born independently, atraumatically, more physiologically.
After birth, the baby is placed on the mother's stomach and applied to the breast. Mom has the opportunity to take the child in her arms in the first minutes of life. The umbilical cord is crossed after the cessation of pulsation.
In the delivery room, in order to prevent gonoblenorrhea, a solution of albucid is instilled into the conjunctival sac of the newborn (eyes) and the genital slit (for girls).
After childbirth, washing the newborn under a tap with water, as it was before, is not performed. Removal of the original lubricant is not performed.
In order to prevent infectious and inflammatory skin diseases in newborns during the first three days of life, skin folds are treated once a day with a 0.5% solution of chlorhexidine.
Within two hours after the birth, the mother and child are in their birth box, then they are transferred to the postpartum ward.
It is important for a woman in childbirth to conduct the so-called "partner birth", when a husband or close relative is present throughout the birth, creating psycho-emotional comfort and a sense of "home environment".