How does a child get sickle cell
Sickle Cell Disease (for Parents)
What Is Sickle Cell Disease?
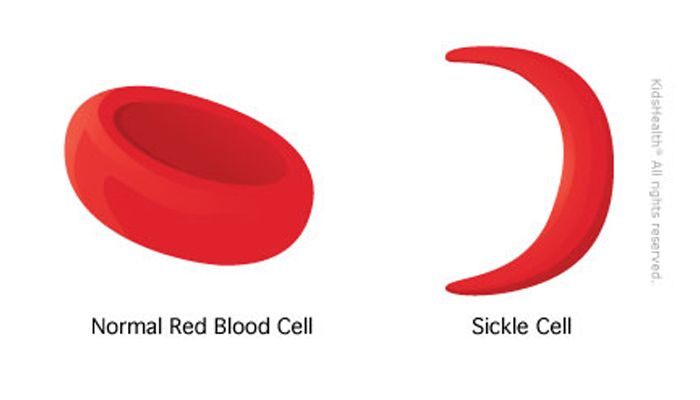
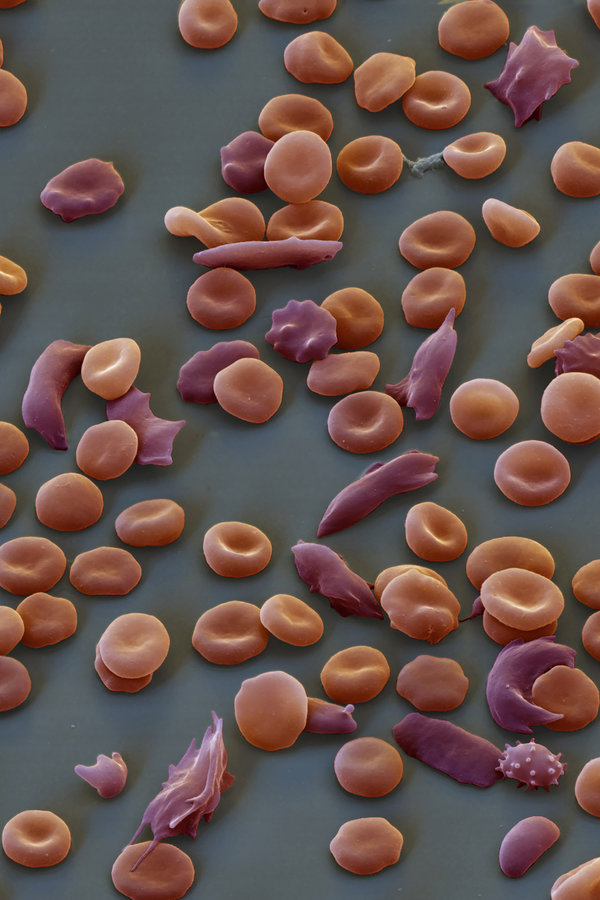
Sickle cell disease is a group of conditions in which red blood cells are not shaped as they should be. Red blood cells normally look like round discs. But in sickle cell disease, they're shaped like sickles, or crescent moons, instead.
The sickle shaped cells cause problems because:
- They are stiff and sticky and block small blood vessels when they get stuck together. This stops blood from moving as it should, which can lead to pain and organ damage.
- They break down faster than normal red blood cells. That leads to too few red blood cells, a condition called anemia.
The two most common symptoms of sickle cell disease are pain and anemia.
The pain caused by sickle cell disease is called a pain crisis or vaso-occlusive crisis. In a pain crisis:
- Pain may happen in any part of the body.
- Cold, stress, illness, or dehydration can bring on pain but often there is not an obvious trigger.
- The pain may last a few hours, a few days, or sometimes longer.
Sometimes pain can be managed at home. But someone with severe pain might need treatment in a hospital.
Signs of anemia include:
- paleness, often seen in the skin, lips, or nailbeds
- tiredness
- dizziness
- being short of breath
- feeling lightheaded
- being irritable
- trouble paying attention
- a fast heartbeat
People with sickle cell anemia may have jaundice (skin and whites of the eyes look yellow). This happens because the sickle-shaped red blood cells break down faster than normal cells.
What Problems Can Happen?
People with sickle cell disease can have problems that need care by a doctor right away, such as:
- Acute chest syndrome: This is caused by inflammation, infection, an blocked small blood vessels of the lung. Signs include chest pain, coughing, trouble breathing, and fever.
- Aplastic crisis: This is when the body temporarily does not make enough red blood cells, which can cause severe anemia. Signs include paleness, extreme tiredness, and a fast heartbeat.
- Hand-foot syndrome: This painful swelling of the fingers and toes (also called dactylitis) is the first sign of sickle cell anemia in some infants.
- Infection: Kids with sickle cell disease are at risk for some bacterial infections. It's important to watch for fevers of 101°F (38°C) or higher, which can be signs of an infection. Get medical care right away if a fever happens.
- Priapism: Males with sickle cell disease can have painful, long-lasting erections. If it's not treated quickly, damage can cause problems with getting erections later in life.
- Splenic sequestration crises: The spleen traps the abnormal red blood cells and gets very large. This can lead to a serious, quick drop in the number of red blood cells in the bloodstream.
 Signs include paleness, weakness or extreme tiredness, an enlarged spleen, and belly pain.
Signs include paleness, weakness or extreme tiredness, an enlarged spleen, and belly pain. - Stroke: Sickle-shaped cells can block small blood vessels in the brain, causing a stroke. Signs include headache, seizures, weakness in the arms and legs, speech problems, a facial droop, or loss of consciousness.
People with sickle cell disease are also at risk for problems such as leg ulcers, bone or joint damage, gallstones, kidney damage, and eye damage. Kids can have delayed growth and delayed puberty.
The frequency and severity of symptoms and problems varies a lot between different people with sickle cell disease.
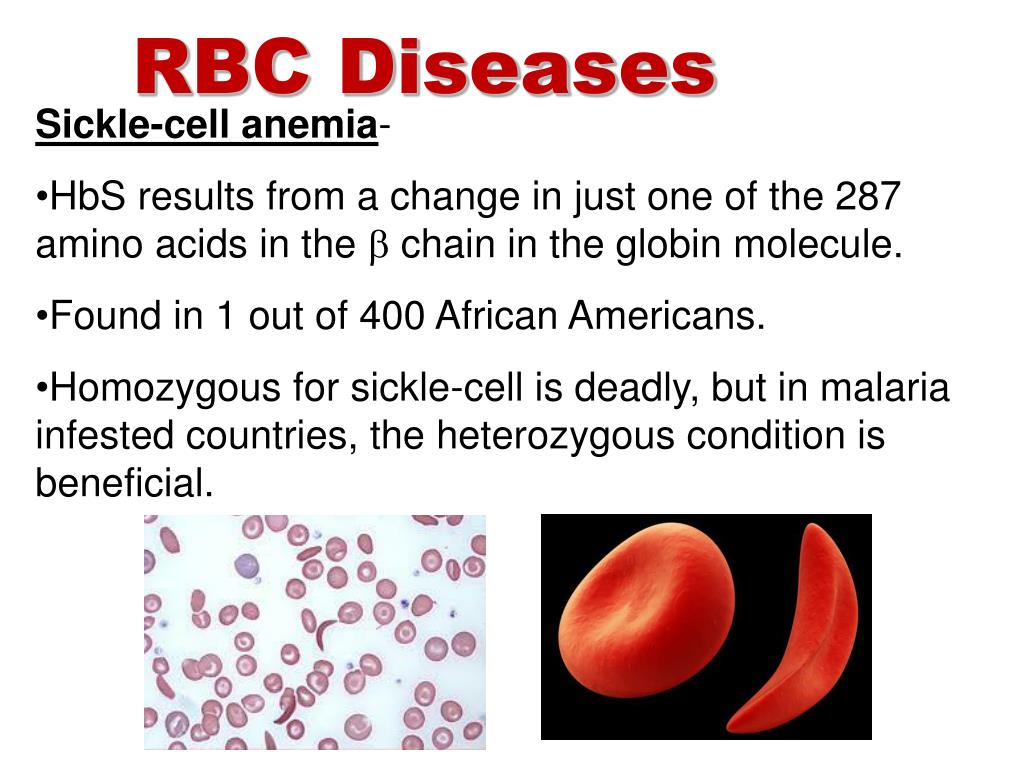
What Causes Sickle Cell Disease?
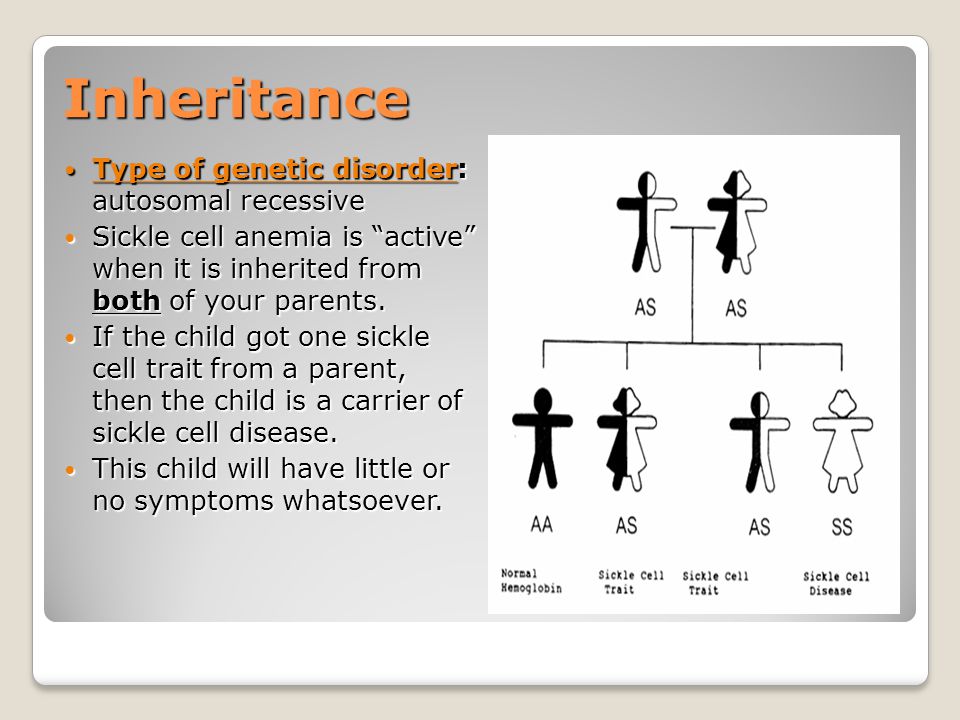
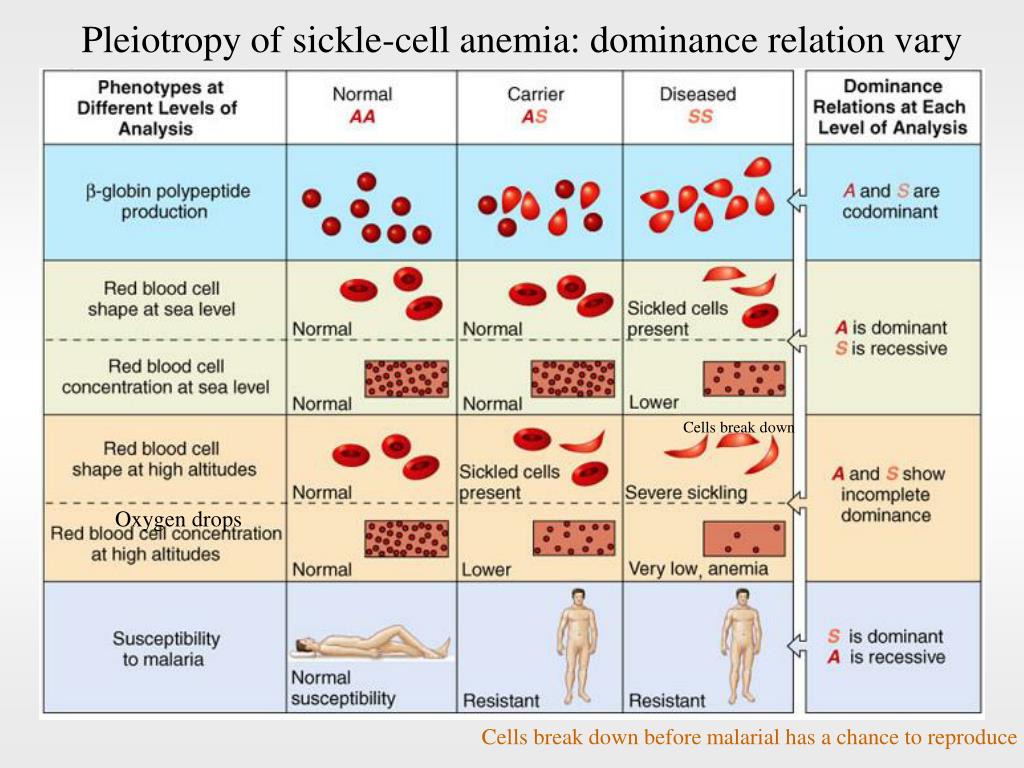
Sickle cell disease is a group of conditions passed down in families through their genes. The type of sickle cell disease a person has depends on the hemoglobin genes each parent passes down to them. Hemoglobin is the protein inside red blood cells that carries oxygen. Someone with sickle cell disease has at least one sickle cell gene.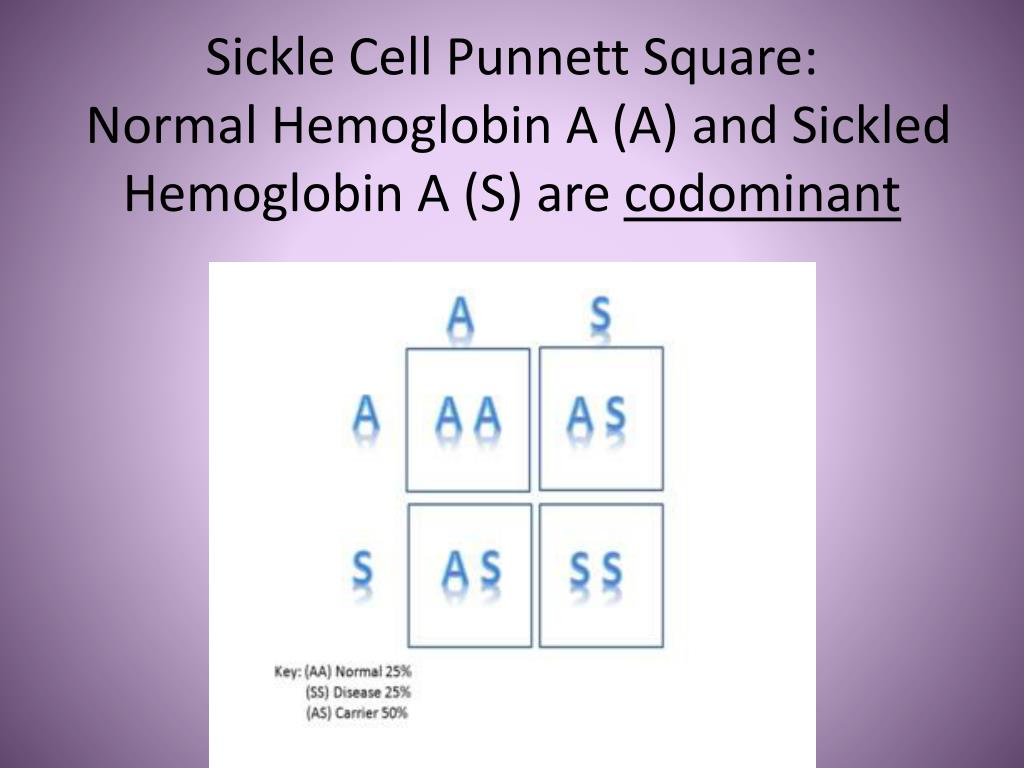 The other hemoglobin gene can be either another sickle cell gene or a gene for a different type of abnormal hemoglobin. The genes cause the body to make hemoglobin that causes the red blood cells to become sickle shaped.
The other hemoglobin gene can be either another sickle cell gene or a gene for a different type of abnormal hemoglobin. The genes cause the body to make hemoglobin that causes the red blood cells to become sickle shaped.
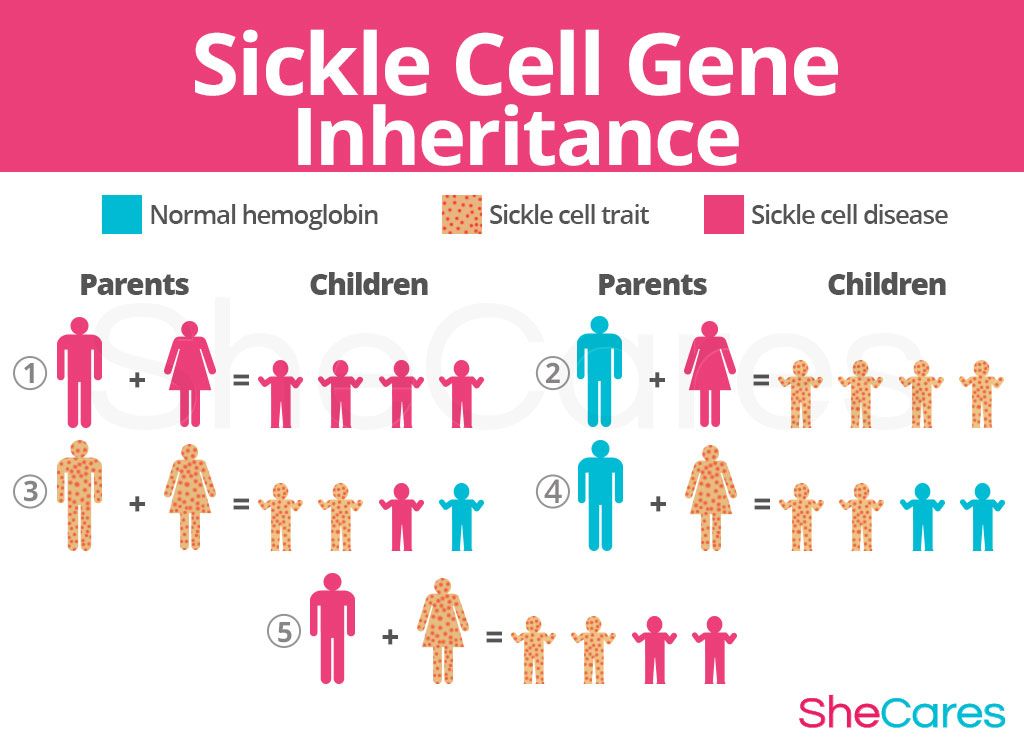
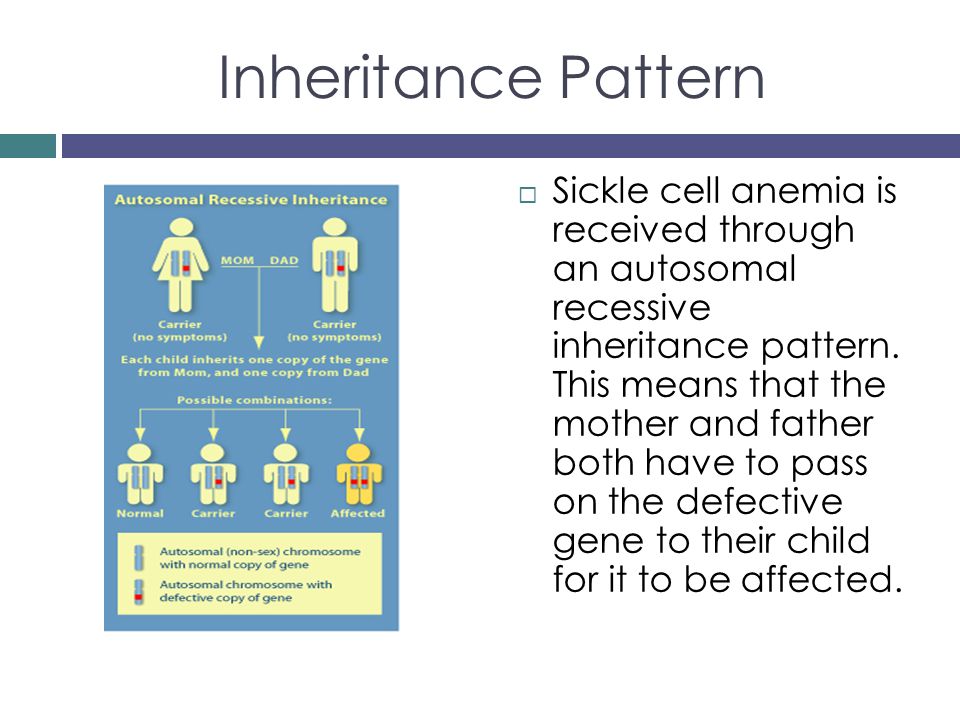
Here’s how sickle cell genes can run in families:
- A child who gets two sickle cell genes, one from each parent, will have sickle cell disease.
- A child who gets a sickle cell gene from one parent and a normal hemoglobin gene from the other parent has sickle cell trait. Most people with sickle cell trait don't have symptoms, but they can pass the sickle cell gene to their children.
- Someone who gets a sickle cell gene from one parent and another kind of abnormal gene from the other parent may have a different form of sickle cell disease, such as hemoglobin SC disease or sickle beta thalassemia.
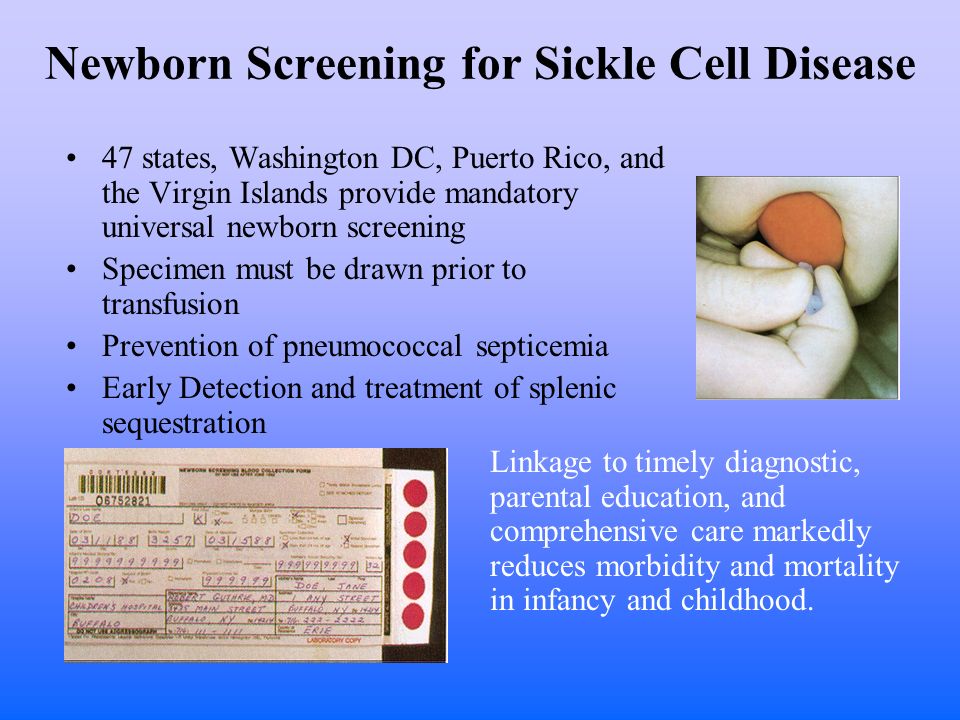
How Is Sickle Cell Disease Diagnosed?
Sickle cell disease and sickle cell trait usually are found at birth with a blood test during routine newborn screening tests.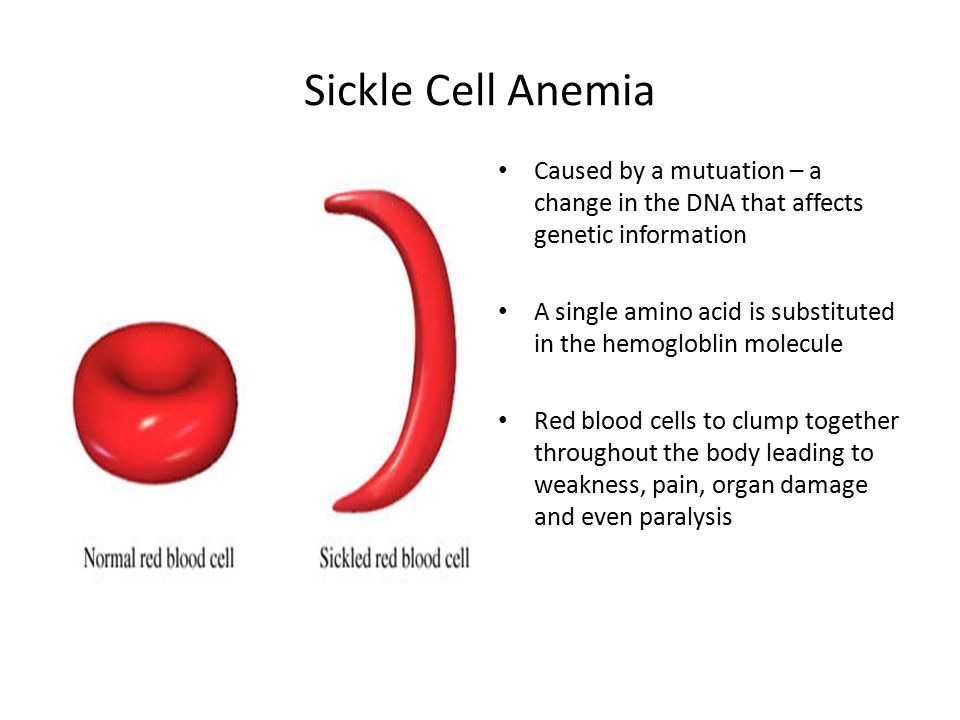 A second blood test (called a hemoglobin electrophoresis) will confirm the diagnosis.
A second blood test (called a hemoglobin electrophoresis) will confirm the diagnosis.
Sickle cell disease also might be diagnosed before a baby is born with a test on the amniotic fluid or with a sample of tissue from the placenta.
How Is Sickle Cell Disease Treated?
Sickle cell disease is a lifelong condition. Treatment helps people with sickle cell disease avoid problems and stay active. A treatment plan includes:
- Immunizations and daily doses of penicillin to help prevent infection. Kids with sickle cell disease should get all recommended vaccinations, including the pneumococcal, flu, coronavirus (COVID-19), and meningococcal vaccines.
- Folic acid supplements, which can help kids make new red blood cells.
- Medicines to help manage pain when it does happen.
A doctor may recommend other treatments for a child with sickle cell disease, such as:
- hydroxyurea, a daily medicine that makes the cells less sticky. This helps decrease the frequency and intensity of painful episodes and many other problems.
 It is strongly recommended for many children with sickle cell disease.
It is strongly recommended for many children with sickle cell disease. - blood transfusions for severe anemia or to treat or prevent some problems
- voxelator (Oxbryta), a daily medicine to reduce sickling and increase the number of red blood cells by helping them hold on more tightly to oxygen
- crizanlizumab (Adakveo), a medicine given by IV infusion that can help make red blood cells more slippery and can reduce pain crises
- L-glutamine, a daily medicine taken by mouth to reduce pain
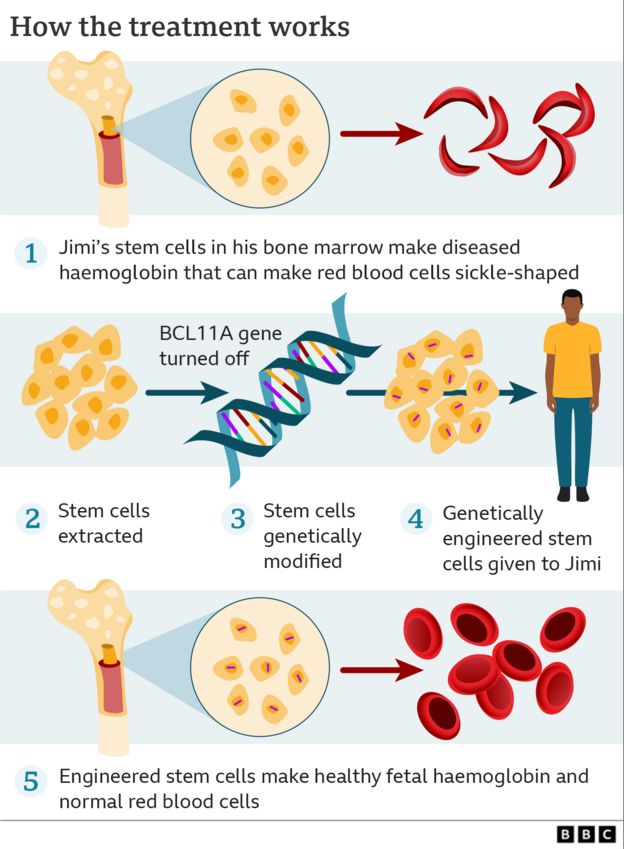
Stem cell transplant (also called bone marrow transplant) is the only proven cure for sickle cell disease. Transplants are complex and risky but often very successful. They're currently an option only for some patients.
Scientists and doctors are using clinical trials to develop new medicines to treat and prevent problems. They're also studying gene therapy as a potential cure for sickle cell anemia by changing or replacing the abnormal gene that causes it.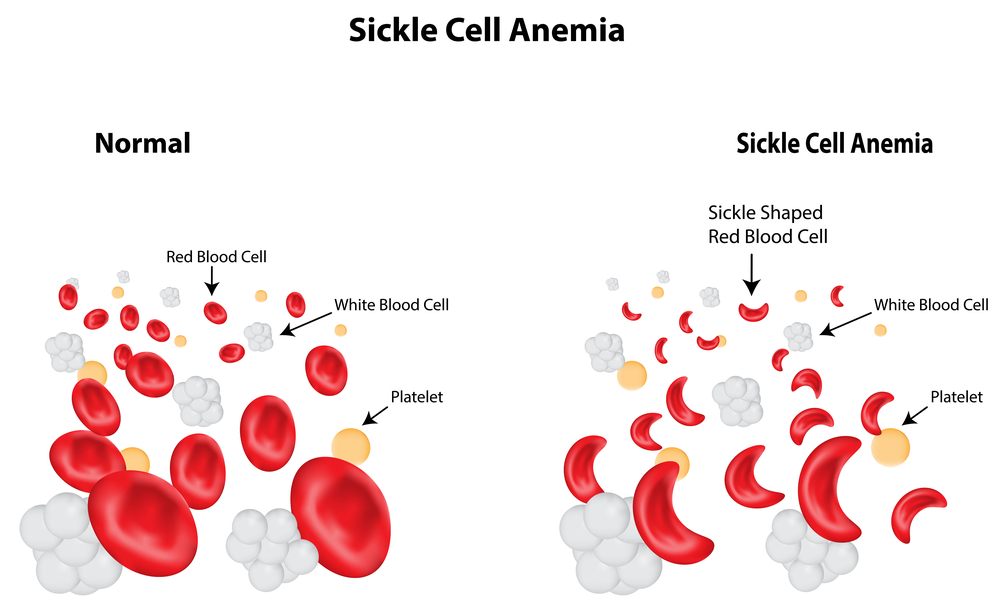
When Should I Call the Doctor?
Get emergency medical care right away if your child has any of these problems:
- fever of 101°F (38°C) or higher
- pain that isn't getting better with medicine
- chest pain
- severe headaches or dizziness
- severe stomach pain or swelling
- shortness of breath or trouble breathing
- extreme tiredness
- skin that's yellow or very pale
- a penile erection that is not going away or is painful
- sudden change in vision
- seizures
- weakness or trouble moving part of the body
- slurred speech
- loss of consciousness (passing out)
- numbness or tingling
How Can Parents Help?
When your child has sickle cell disease there is a lot you can do to help:
Learn all you can about sickle cell disease. Tell all caregivers about the condition, how to care for your child, and signs of trouble to watch for.
Take your child to all visits with their doctors and specialists. Keep track of any symptoms and share your concerns.
Help your child avoid pain crisis triggers:
- Encourage your child to drink lots of liquids and get enough rest.
- In cold weather, your child should dress warmly and not stay out too long.
- In hot weather, your child should limit time outdoors and drink lots of fluids.
- Help your child learn ways to manage stress.
- Talk to the doctor about which activities are OK for your child and which to avoid.
- Make sure your child takes all prescribed medicines.
Make healthy choices. As a family, eat healthy foods and stay active. As your child gets older, make sure they know not to smoke, drink alcohol, or use drugs because these can cause pain and other problems.
You also can find more information and support online at:
- The CDC
- Sickle Cell Disease Association of America
Sickle Cell Disease: Information for Parents
Every year, roughly 2,000 babies are born with sickle cell disease, the most common inherited blood disorder in the United States.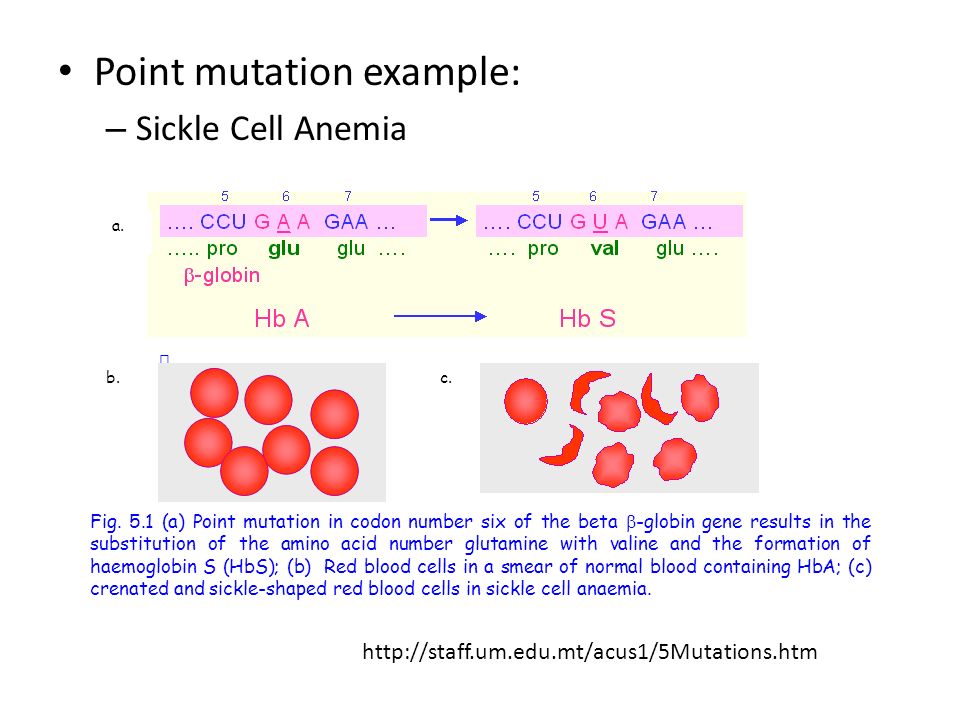 Children with sickle cell disease experience episodes of severe pain and ongoing medical challenges. Early and ongoing medical care can minimize complications and help children with the disorder lead full and active lives.
Children with sickle cell disease experience episodes of severe pain and ongoing medical challenges. Early and ongoing medical care can minimize complications and help children with the disorder lead full and active lives.
In children with sickle cell disease, a protein called hemoglobin inside the red blood cells forms chains that clump together and cause the red blood cell to be shaped like a crescent moon or the letter C―called a sickle cell.
Compared to normal red blood cells that are disk-shaped and flexible, sickled cells are stiff, sticky and fragile. They break apart and leave the blood stream sooner than normal red blood cells. This results in blocking of normal blood flow, preventing blood, and the oxygen it carries, to get to everywhere in the body.
Image Source: U.S. National Library of Medicine
How do infants and children get sickle cell disease?
Babies are born with sickle cell disease.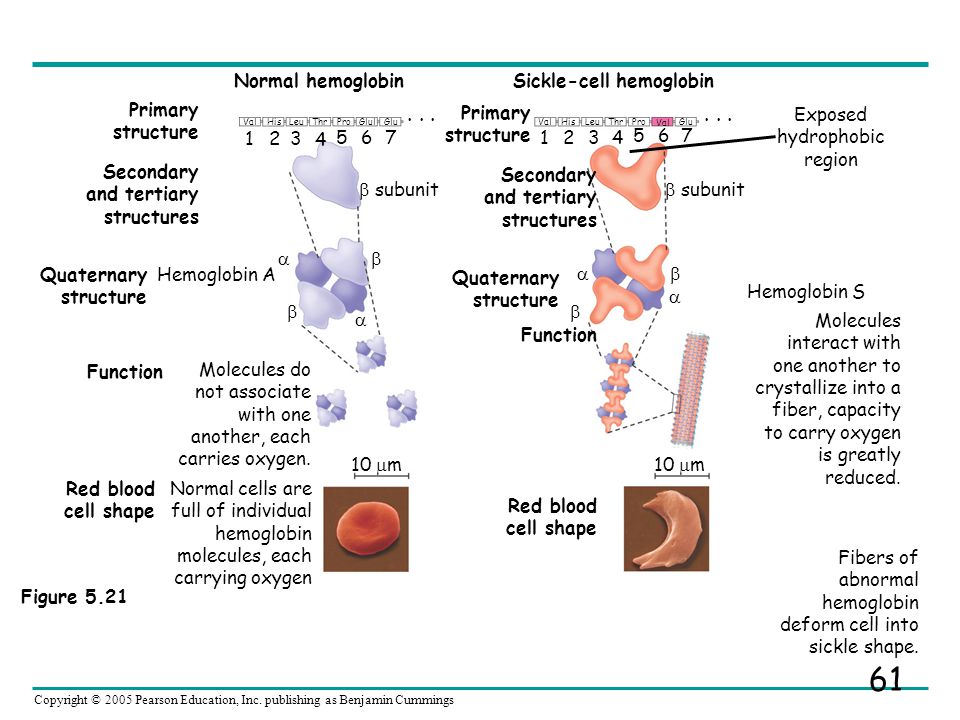 Sickle cell disease is a genetic condition, so children get it in the same way they inherit the
color of their eyes, skin, and hair through the combination of genes they inherit from their parents.
Sickle cell disease is a genetic condition, so children get it in the same way they inherit the
color of their eyes, skin, and hair through the combination of genes they inherit from their parents.
How is sickle cell disease inherited?
Everyone inherits one hemoglobin gene from their mother and one hemoglobin gene from their father. Inheriting one mutated or abnormal gene, but having a normal gene from the other parent, is called having a trait. Inheriting two abnormal hemoglobin traits or genes determines whether a child has sickle cell disease.
The normal hemoglobin gene is labeled A. The most common mutated hemoglobin genes or hemoglobin traits are called S or C. The mutated (changed) hemoglobin gene associated with sickle cell disease is S. Common types of mutated (changed or abnormal) hemoglobin genes that combine with S to cause sickle cell disease are S, C and Beta thalassemia.
People who have inherited one of the following gene combinations DO NOT have sickle cell disease:
A + A (AA): no sickle cell disease
A + S (AS): carrier of the hemoglobin "S" gene, known as sickle cell trait
A + C (AC): carrier of the hemoglobin "C" gene
People who have inherited one of the following gene combinations DOhave sickle cell disease:
S + S (SS): Sickle cell anemia or Hemoglobin SS
S + C (SC): Sickle hemoglobin C disease or Hemoglobin SC
S + beta thalassemia trait (S-beta thalassemia): a form of sickle cell disease
Image source: Centers for Disease Control and Prevention
How do I know if my baby has sickle cell trait or disease?
Every state in the US performs a
newborn screening test for sickle cell disease.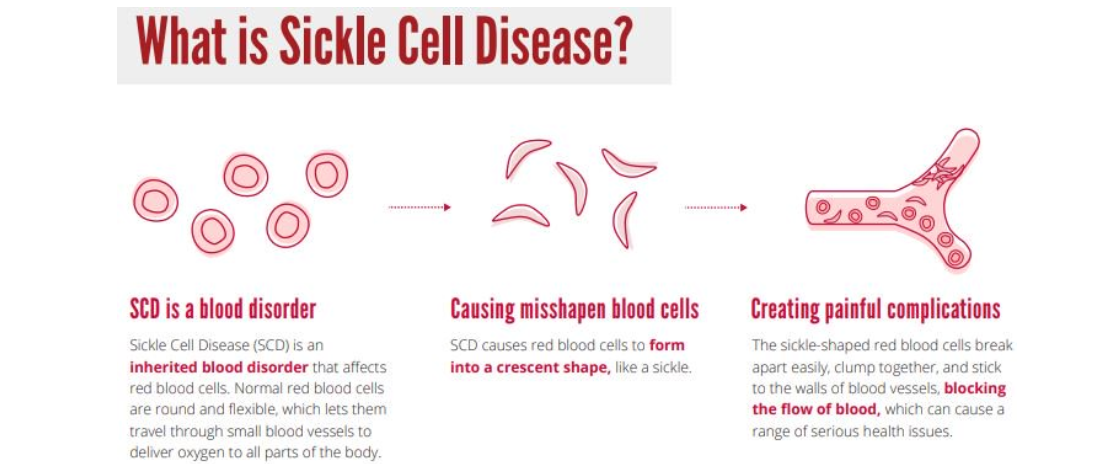 If this test is concerning for sickle cell disease, the baby is referred to a pediatric hematologist. If the test indicates sickle cell trait, the parents are counselled by the general pediatrician and the child generally does not need to see a hematology specialist.
If this test is concerning for sickle cell disease, the baby is referred to a pediatric hematologist. If the test indicates sickle cell trait, the parents are counselled by the general pediatrician and the child generally does not need to see a hematology specialist.
Early diagnosis, before infants show any symptoms allows infants with sickle cell disease to get early treatment and may decrease their risk of infections or other serious complications.
Why is sickle cell disease more common in children of African heritage?
A carrier of a single hemoglobin S gene is said to have sickle cell trait or hemoglobin S trait. About 1 in 12 people of African ancestry carry S trait. Sickle cell trait is also common in people with ancestors from the Caribbean, Middle East, India, South America, Central America and Mediterranean countries such as Turkey, Greece and Italy. Sickle cell trait is found today in descendants of these populations no matter where they live.
People with hemoglobin S trait alone do NOT have sickle cell disease.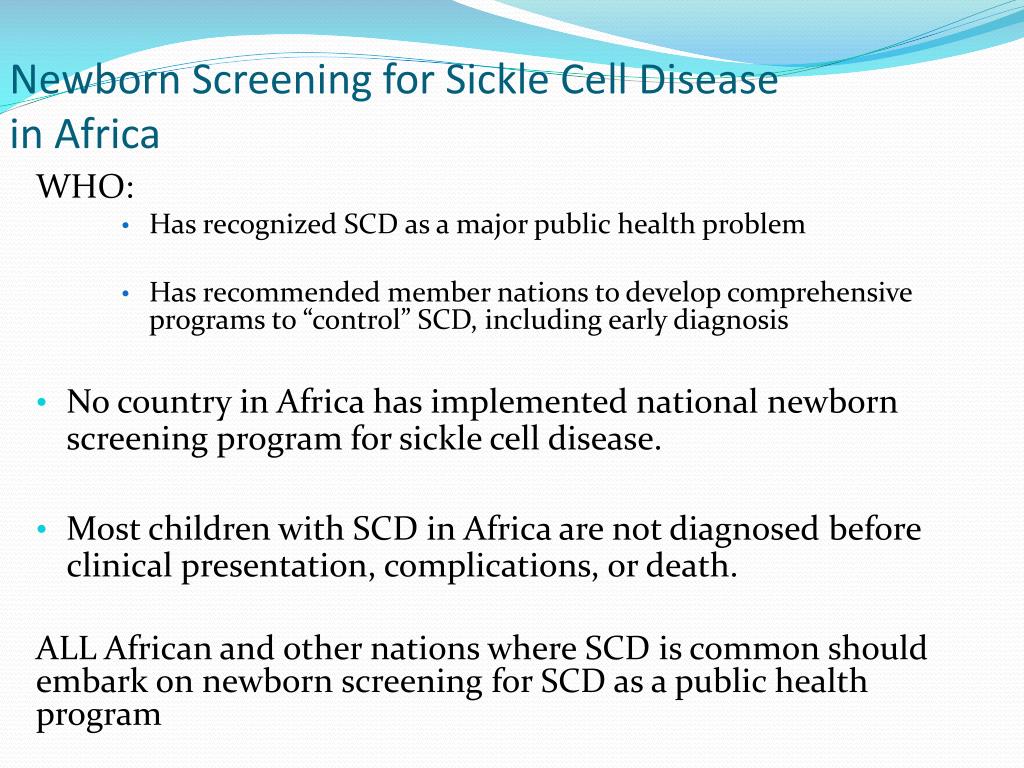 However, if their reproductive partner also has the hemoglobin S trait, then together they have a 1 in 4 chance (25%) of having a child with sickle cell disease. This is why
even bi-racial and/or multi-racial children can have sickle cell disease; About
1 in 365 people of African ancestry have sickle cell disease.
However, if their reproductive partner also has the hemoglobin S trait, then together they have a 1 in 4 chance (25%) of having a child with sickle cell disease. This is why
even bi-racial and/or multi-racial children can have sickle cell disease; About
1 in 365 people of African ancestry have sickle cell disease.
Why is sickle cell disease sometimes called sickle cell anemia?
Sickle cell disease is an umbrella term for the many specific types of sickle cell disorders. Anemia―meaning a lower-than-normal number of red blood cells―happens with all forms of sickle cell disease. While normal red blood cells can live for 120 days, sickled cells last only 7 to 20 days; the body can't replace them fast enough resulting in anemia.
Children who have inherited two abnormal genes have sickle cell disease; which specific genes have been inherited determines what the disorder is called. Sickle cell anemia refers to the two most severe forms of sickle cell disease, hemoglobin SS and sickle beta zero thalassemia.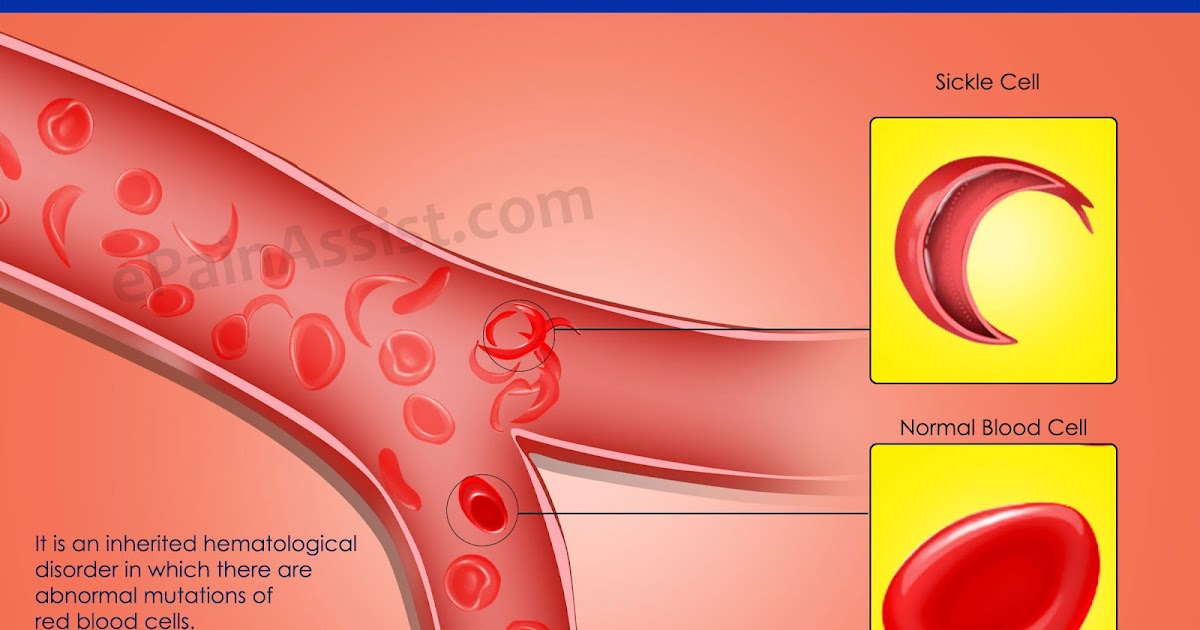
Main Types of Sickle Cell Disorders | |
Hemoglobin SS | The most severe form, affecting 65% of children with sickle cell disease. Most or all of the hemoglobin is abnormal, causing chronic anemia. |
Hemoglobin SC disease | Roughly 25% of children with sickle cell disease have this mild to moderate form of the disease. Symptoms generally develop later in childhood, but may be as severe as in SS. |
Sickle beta plus thalassemia | Affects around 8% of children with sickle cell disease. This is generally considered a mild form of sickle cell disease, but severity can vary greatly. |
Sickle beta zero thalassemia | A severe but less common form, accounting for 2% of sickle cell disease. It is similar to hemoglobin SS. |
Why are infants and children with sickle cell disease at higher risk of infection?
Sickle cell disease may cause damage to the spleen, kidneys, lungs and brain. Once damaged by sickled cells the spleen may not be able to filter bacteria from the blood as well as it normal.
As a result, infants and children with sickle cell disease have a compromised immune system, which means they are more likely to have certain infections which may be fatal.
Antibiotics to prevent secondary infections in infants & children with sickle cell disease:
National guidelines recommend newborns diagnosed with severe sickle cell disease (SS and S beta zero thalassemia) receive antibiotics twice a day until they are 5 years old.
Research shows that children with sickle cell anemia given twice daily penicillin (an antibiotic) had 84% less risk of
Streptococcus pneumoniae bacterial infection, which can cause serious conditions like
pneumonia and
meningitis.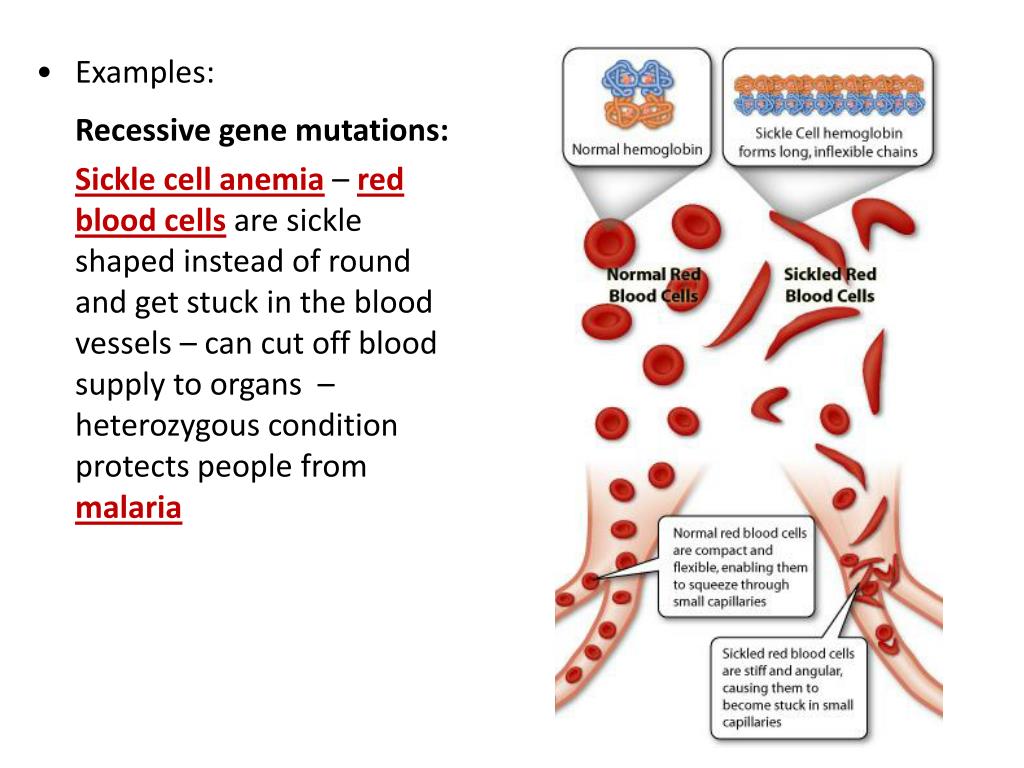
What is outlook for children with sickle cell disease?
Sickle cell disease is a chronic disease, but the outlook is improving. Early diagnosis and starting antibiotics shortly after birth for those with severe forms of sickle cell have greatly improved life expectancy. Today other treatments are available to minimize complications which can improve quality of life and life expectancy.
Is there a cure for sickle cell disease?
Stem cell (bone marrow) transplants is the only cure for sickle cell disease. This treatment requires a donor with suitable bone marrow. Similar to other treatments stem cell transplant has benefits and risks which should be discussed before proceeding. Other promising treatments being explored include gene therapy. A collaborative research effort led by the U.S. National Heart, Lung, and Blood Institute was created in 2018 to speed up the search for cures.
Who are the doctors that care for children with sickle cell disease?
In addition to regular visits with their pediatrician, children with sickle cell disease should see a
pediatric hematologist at least periodically. These doctors specialize in the care of children with sickle cell disease.
These doctors specialize in the care of children with sickle cell disease.
More information:
- Sickle Cell Trait: Parent FAQs
-
Can Biracial Children Get Sickle Cell Disease?
- I Didn't Know This Could Happen (AAP Voices)
- Sickle Cell Disease (Centers for Disease Control and Prevention)
- Evidence-Based Management of Sickle Cell Disease, Expert Panel Report
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Sickle cell anemia - Site zdorovieinfo.ru - the largest medical Internet portal in Russia
Sickle cell anemia is an inherited form of anemia, a disease in which there are not enough healthy red blood cells to carry enough oxygen throughout the body.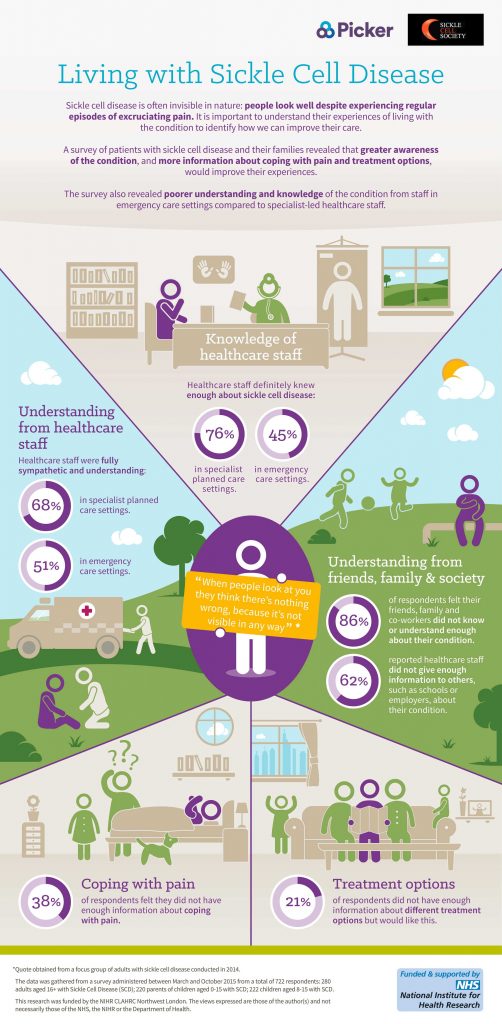
As a rule, red blood cells are flexible and round, easily moving through the blood vessels. In sickle cell anemia, red blood cells become hard and sticky and shaped like crescents or moons.
| Symptoms |
| Clinical manifestations and symptoms of sickle cell anemia vary among patients, but generally include:
|
| When to see a doctor |
| Sickle cell anemia is usually diagnosed in infancy. With the following symptoms, you should immediately consult a doctor (they may indicate the presence of this dangerous disease):
|
| Causes |
| Sickle cell anemia is caused by a mutation in a gene that causes the body to produce a red, iron-rich compound (hemoglobin). Hemoglobin allows red blood cells to carry oxygen from the lungs to all parts of the body. In sickle cell anemia, abnormal hemoglobin causes red blood cells to become hard, sticky, and deformed. The gene for sickle cell anemia is passed down from generation to generation in a pattern of inheritance called autosomal recessive. This means that for a child to get sick, both mother and father must pass on the defective form of the gene. In the presence of one normal hemoglobin gene and one defective form, both normal and deformed hemoglobin are produced in the body. These people do not have symptoms of the disease, but they are carriers of the disease and can pass it on to their children. |
| Complications |
| Sickle cell anemia can lead to many complications, including: Stroke. A stroke can develop if sickle cells block blood flow to an area of the brain. Signs of a stroke include seizures, weakness or numbness in the arms and legs, sudden speech problems, and loss of consciousness. Acute chest syndrome. This life-threatening complication causes chest pain, fever and difficulty breathing. Acute chest syndrome can be caused by an infection in the lungs or sickle cell cells blocking the blood vessels in the lungs. It may require emergency medical attention with antibiotics and other treatments. Pulmonary hypertension. People with sickle cell anemia may develop high blood pressure in the lungs (pulmonary hypertension). Damage to internal organs. Sickle cells, which block blood flow through the blood vessels, immediately deprive the affected organ of blood and oxygen. Sickle cell anemia also has chronically low levels of oxygen in the blood. Chronic deficiency of oxygen-rich blood can damage the nerves and organs in the body, including the kidneys, liver, and spleen. Organ damage can be fatal. Blindness. Sickle cells can block the tiny blood vessels that supply blood to the eyes. Over time, this can damage the retina and lead to blindness. Leg ulcers. Sickle cell anemia can lead to open sores called ulcers. Gallbladder stones. The destruction of red blood cells leads to the formation of a substance called bilirubin. High levels of bilirubin in the body can lead to the formation of gallstones. Priapism. Men with sickle cell anemia may have long, painful erections, a condition called priapism. As in other parts of the body, sickle cells can block the blood vessels in the penis, which can damage the penis and lead to impotence. |
| Diagnostics |
| The presence of the S-defective form of hemoglobin, which underlies sickle cell anemia, reveals a blood test. In adults, a blood sample is taken from a vein in the arm. In young children and infants, a blood sample is usually taken from a finger or heel. If the screening test is negative, the sickle cell anemia gene is absent. If the screening test is positive, additional tests will be done to determine the presence of one or two sickle cell anemia genes. When a disease is detected, a blood test is performed to check the level of red blood cells |
| Treatment |
| Bone marrow transplantation, also known as stem cell transplantation, is the only possible treatment for sickle cell anemia. Blood transfusion helps to increase the number of normal red blood cells. In children with sickle cell disease at high risk of stroke, regular blood transfusions may reduce the risk. Blood transfusions may also be used to treat other complications of sickle cell anemia or to prevent complications. In other cases, therapy for sickle cell anemia is usually aimed at preventing crises, relieving symptoms, and preventing complications. Treatment options may include medicines to reduce pain and prevent complications, and blood transfusions. Infants and children 2 years of age and younger with sickle cell anemia should see a doctor regularly. Older patients can visit the doctor once a year. Medicines A number of drugs are used to treat sickle cell anemia. Including these are antibiotics . Children with sickle cell anemia can start taking penicillin, which helps prevent infections. |
| Lifestyle and home remedies |
| Some simple lifestyle changes can help prevent the complications of sickle cell anemia:
|
Registered with the Federal Service for Supervision of Communications, Information Technology and Mass Media on October 21, 2010 Registration certificate El No. ФС77–42371. © 2022 Copyright ZdorovieInfo
symptoms, treatment, severity, causes, classification and diagnosis of anemia
Daniil Davydov
medical journalist
Author profile
According to WHO, 24.8% of the total population of the Earth has anemia, this is 1 .6 billion people.
Most anemic patients are children and young women. Nevertheless, it is important for everyone to know what anemia is and where it comes from, because every person has a risk of getting some types of anemia, regardless of gender and age.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is anemia
Anemia is a decrease in the mass of red blood cells, that is, erythrocytes, in the human body. Red blood cells deliver oxygen from the lungs to organs and tissues and take carbon dioxide from them. This is due to hemoglobin, an iron-rich protein that gives blood its red color.
Anemia - International Medical Guide Medscape
Complex structure of heme allows iron to take up oxygen Complex structure of heme allows iron to take up oxygen When the mass of red blood cells decreases, the cells that make up our body begin to suffocate a little. At first, a person may not even feel it.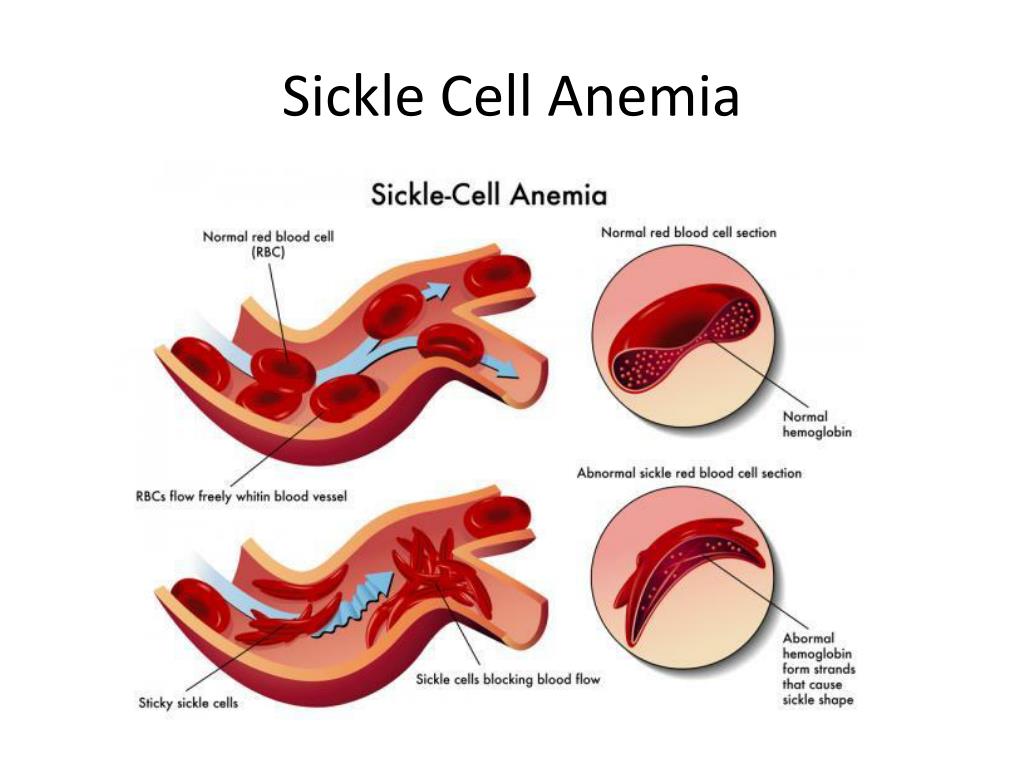 But if the cause of anemia is not eliminated, over time it can lead to health problems.
But if the cause of anemia is not eliminated, over time it can lead to health problems.
Why Anemia is Dangerous - Bulletin of the American Academy of Family Physicians
It all starts with unexplained fatigue, decreased performance, and muscle weakness. But over time, oxygen deficiency can lead to heart failure and even death. Children with anemia develop more slowly than their peers, and pregnant women have a higher risk of giving birth to a child with low body weight and preterm birth more often.
Anemia is not a disease, but a manifestation of the underlying disease. To cure anemia, you first need to establish its true cause. And there can be many reasons.
Assessing Anemia - MSD Physician's Guide
Causes of Anemia
Red blood cells only live for about four months. Then new cells take the place of dead cells, so that in the body of healthy people the number of red blood cells always remains approximately at the same level.
Classification of Anemia by Origin - A Guide for Physicians MSD
Most often, the balance between the birth and death of red blood cells is disturbed for three reasons.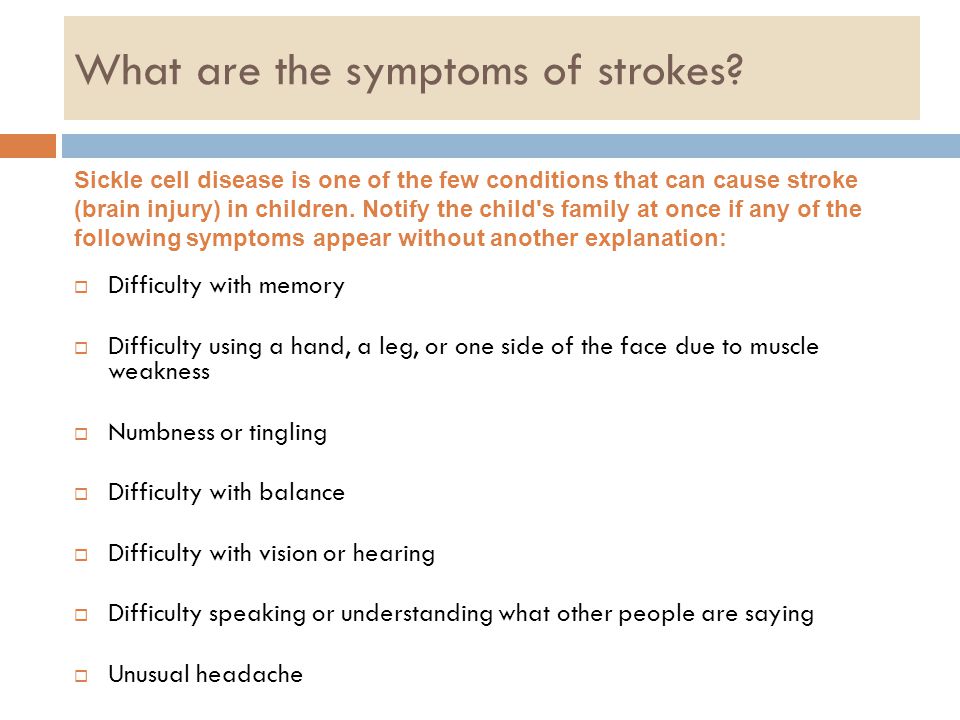
Loss of blood. Doctors call anemia that has developed due to blood loss post-hemorrhagic. They are divided into two forms - acute and chronic.
Anemia Due to Severe Bleeding - A Guide for Physicians MSD
Acute anemia occurs when a person loses a large amount of blood over several hours. This happens, for example, with injuries. Together with blood, erythrocytes are also lost, and new ones do not have time to be produced.
Iron Stored in the Liver and Muscles - US National Institutes of Health Bulletin
Chronic anemia occurs when a person loses blood over several days, weeks, or even months, gradually and imperceptibly. This happens with internal bleeding - for example, with a stomach ulcer or excessively heavy menstruation.
Under normal conditions, the body replenishes iron from dead red blood cells and from food. With chronic blood loss, he cannot take iron from the lost red blood cells, and only 3 mg of iron is absorbed from food per day. Considering that with the daily loss of just one teaspoon of blood, a person loses as much as 2.5 mg of iron, this is clearly not enough.
Considering that with the daily loss of just one teaspoon of blood, a person loses as much as 2.5 mg of iron, this is clearly not enough.
Diagnosis and treatment of iron deficiency anemia in the 21st century - Journal of Therapeutic Advances in Gastroenterology
Can bleeding cause iron deficiency anemia? — an international guide for doctors Medscape
In order to produce new red blood cells to replace those lost, the body has to use the "untouchable reserves" of iron, which are stored in the liver, spleen, bone marrow and muscles. If internal bleeding is not corrected and supplies are not replenished, iron deficiency anemia may develop.
Accelerated destruction of red blood cells. Anemia, in which enough red blood cells are produced in the body, but they do not live long, are called hemolytic. They may be associated with hereditary blood diseases. For example, with thalassemia, in which the production of hemoglobin is disrupted, or with sickle cell anemia, in which short-lived red blood cells that look like a month are formed.
Hemolytic Anemias Bulletin of the National Heart Lung and Blood Institute USA
Thalassemia - Mayo Clinic Booklet
Sickle Cell Anemia - Bulletin of the National Heart, Lung, and Blood Institute USA
How to Distinguish Acquired Hemolytic Anemia from Congenital - Medscape International Physician's Handbook
The disease can be provoked by a bacterial, viral or parasitic infection, taking certain medications, an autoimmune reaction in which red blood cells are destroyed by one's own immune system, or a blood transfusion of the wrong type.
Insufficient production of red blood cells. Anemias in which the body is not able to produce as many red blood cells as needed for a normal supply of oxygen are called hypoproliferative. They are divided into three forms.
Anemia due to inadequate production of red blood cells - a guide for physicians MSD
Microcytic anemia occurs due to problems with absorption of iron from the gastrointestinal tract - such as in patients with celiac disease or inflammation of the gastric mucosa - gastritis or ulcers.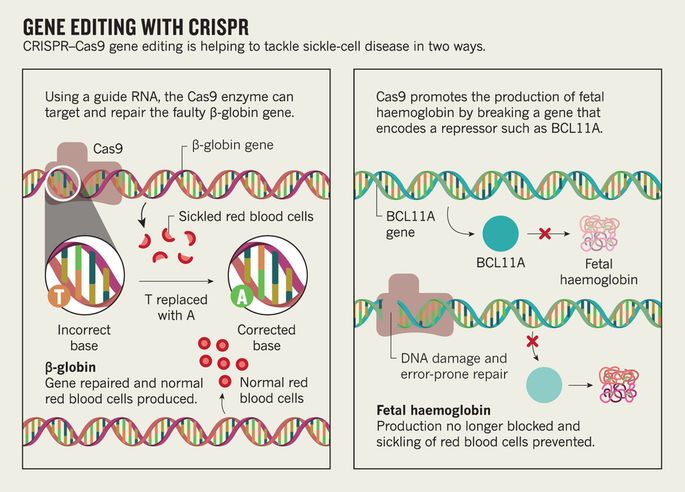
Anemia Caused by Low Iron in Adults - An International Manual for Physicians Uptodate
Well-nourished adult men are adequately supplied with iron from food. But iron deficiency is more common in some groups of people. These include:
- Vegetarians who do not eat iron-rich meat.
- Some women who lose too much iron with menstruation.
- Pregnant women who "share" their iron with the fetus.
- Young children who use iron to grow.
Aplastic anemia can be caused by viruses, radiation, drugs, and even pregnancy—a guide for physicians MSD
When there is not enough iron, little hemoglobin is synthesized. And since there is nothing to fill the red blood cells with, they turn out to be small. Although the cause is not blood loss, iron deficiency anemia can also develop as a result.
In normocytic anemia, red blood cells are of normal size, but very few. This happens either due to genetic disorders, or due to diseases of the bone marrow, in which, as a result, fewer red blood cells are produced than necessary, such as aplastic anemia.
In macrocytic anemia, red blood cells are large, but they are poor in hemoglobin, and they are formed too few to provide normal gas exchange. Most often, macrocytic anemia develops due to a lack of vitamin B9 or vitamin B12.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
Macrocytic anemia can also be caused by liver disease or as a side effect of certain medications, such as zidovudine or methotrexate .
Why You Need Vitamin B12 - US National Institutes of Health Bulletin
Deficiency of Certain B Vitamins - The Most Common Cause of Macrocytic Anemia - A Guide for Physicians MSD
Classification of Anemias
Classifications of anemias are many, but most commonly fall into four retypes.
Iron deficiency anemias are the most common, accounting for approximately 80% of all anemias. They are associated either with bleeding, for example, after surgery or as a result of an injury, or with an unbalanced diet that lacks foods that could be sources of iron, for example, with a strict vegan diet.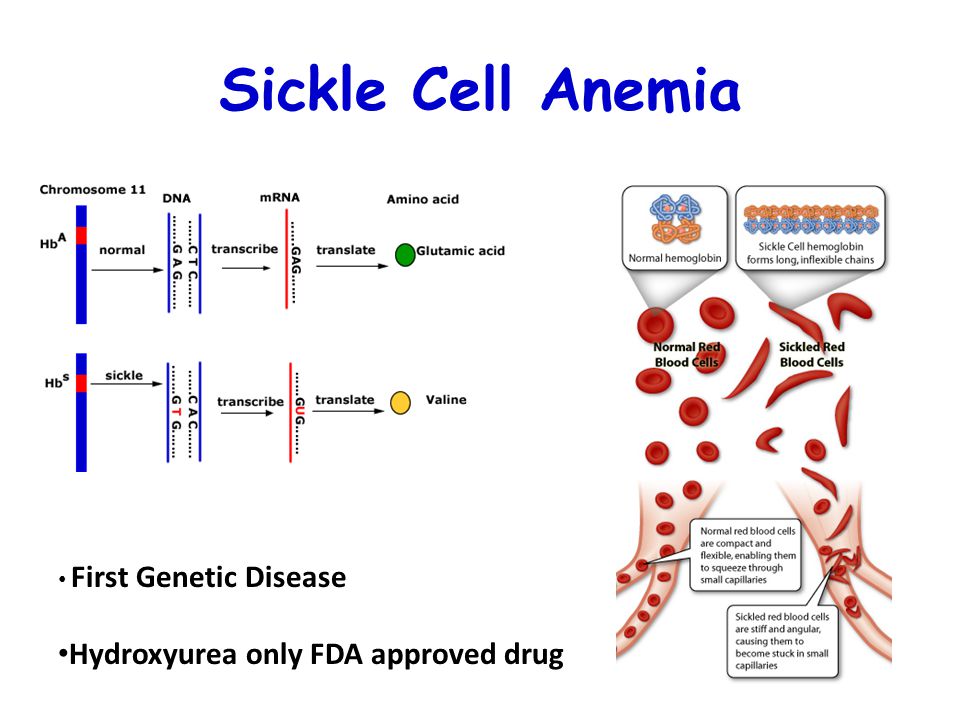
Anemia associated with chronic diseases. According to some data, 30-50% of all older people suffer from anemia that arose due to diseases with which people live for many years. The causes of anemia are oncological and autoimmune diseases, chronic kidney disease.
/guide/minerals/
Dietary minerals: where to get them and how to take them
Anemia associated with a lack of vitamins B9 and B12, affects 0.1% of all inhabitants of Northern Europe. Vitamin B9 deficiency, or folic acid, is most common in pregnant women with poor nutrition, in people with inflammatory bowel diseases and in alcoholism: in these conditions, the absorption of folic acid is impaired.
Vitamin B12 deficiency can develop in vegans because vitamin B12 is found only in foods of animal origin, in hereditary diseases, in people with inflammatory bowel disease, in which the absorption of this substance is impaired, and in patients with diseases of the stomach, in which production is impaired substances necessary for the absorption of vitamin B12.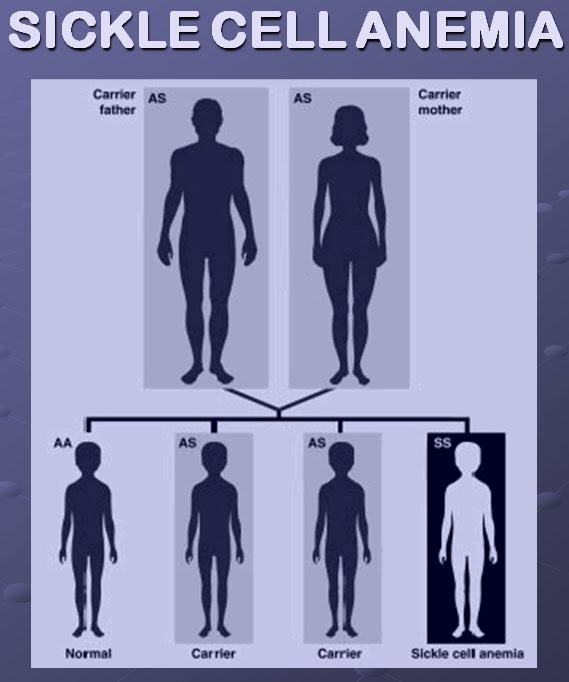
Anemia associated with genetic disorders is rare. Next, we will talk about the types of anemia that are most common.
Anemia can develop for various reasons - here are the main onesSymptoms of anemia
Manifestations of anemia, especially in the early stages, are very similar to the symptoms of ordinary fatigue or professional burnout. Many people do not feel any discomfort at all, or they have non-specific symptoms that may indicate many different diseases, and not one specific one.
Therefore, it is difficult to suspect a disease based only on symptoms.
Symptoms of Anemia - Mayo Clinic Bulletin
Signs of Anemia:
- Easy fatigue.
- Pale or yellowish skin.
- Regular dizziness and headaches.
- Pain in the chest.
- Arrhythmias, i.e. irregular heartbeat.
- Shortness of breath.
- Muscle weakness.
- Cold hands and feet.
Which doctor treats anemia
As a rule, people with symptoms similar to anemia go to a general practitioner.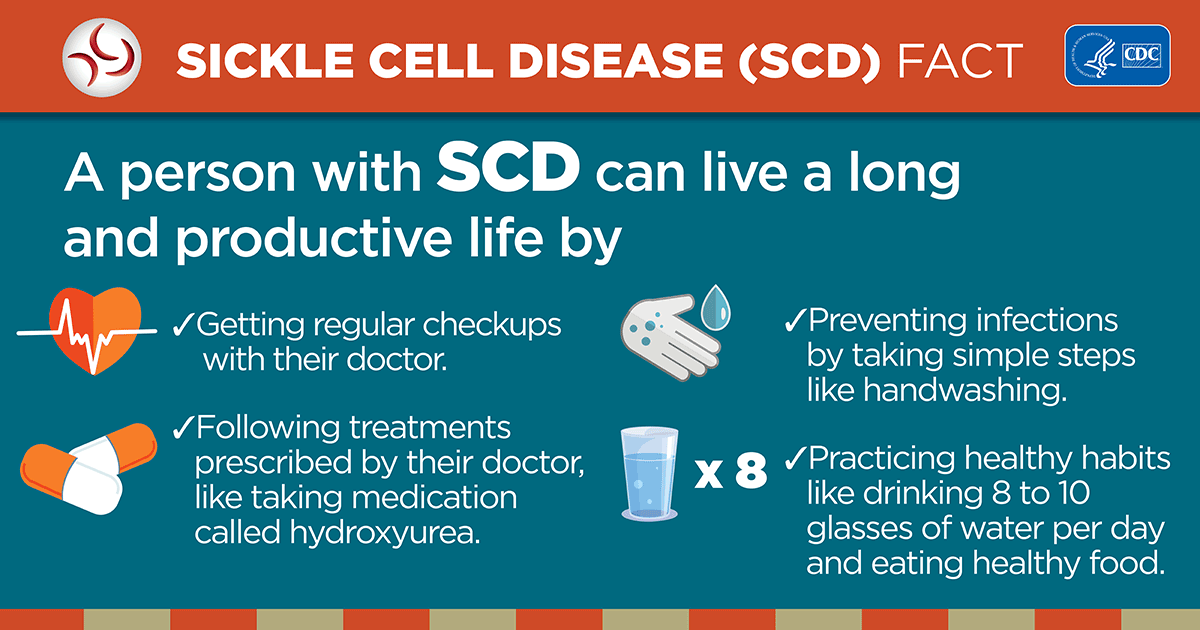 If the doctor suspects that the patient has anemia, he can refer him to a specialist - a hematologist. The cost of an appointment with a general practitioner in Moscow is an average of 2500 RUR, with a hematologist an average of 4000 RUR.0004
If the doctor suspects that the patient has anemia, he can refer him to a specialist - a hematologist. The cost of an appointment with a general practitioner in Moscow is an average of 2500 RUR, with a hematologist an average of 4000 RUR.0004
The majority of my patients are children who were diagnosed with anemia during a routine medical examination at the age of one year, or adults who independently decided to take tests and found changes in them. Sometimes other doctors refer difficult patients to me who have difficulty treating them. But there are much fewer of them.
Diagnosis of anemia
Diagnosis of anemia consists of two stages.
Diagnostic Approach to Anemia in Adults - International Manual for Physicians Uptodate
Hemoglobin concentration for diagnosing anemia and assessing its severity - WHO guidelinesPDF, 335KB
Step 1. Verify that the patient is indeed anemic and not some other disease.
To do this, the doctor will conduct an external examination of the patient: pay attention to the color of the skin, assess the size of the lymph nodes and spleen, ask about bone pain, chronic diseases and the medications that he takes.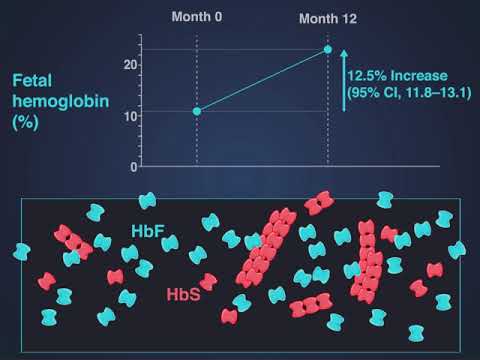
Then the doctor will prescribe a general blood test with a mandatory smear microscopy - this allows you to evaluate the shape and size of red blood cells, as well as the erythrocyte sedimentation rate (ESR).
A complete blood count includes determining the concentration of hemoglobin, hematocrit - the volume of red blood cells, which is expressed as a percentage, and other indicators that describe the state of red blood cells.
/analiz/
You have the right to free tests according to compulsory medical insurance
However, at the first stage of the examination, the doctor pays attention primarily to the level of hemoglobin - this is the main criterion for making a diagnosis of anemia.
Hemoglobin level in g/l in different groups of people as a diagnostic criterion for anemia according to WHO
| Group | Norm | Primary anemia | Moderate anemia | Severe anemia |
|---|---|---|---|---|
| Children 6 months to 5 years | 110 and up | 100-109 | 70-99 | Below 70 |
| Children 5-11 years old | 115 and up | 110-114 | 80-109 | Below 80 |
| Children 12-14 years old | 120 and up | 110-119 | 80-109 | Below 80 |
| Women aged 15 and over | 120 and up | 110-119 | 80-109 | Below 80 |
| Pregnant women | 110 and up | 100-109 | 70-99 | Below 70 |
| Men aged 15 and over | 130 and up | 110-129 | 80-109 | Below 80 |
Children from 6 months to 5 years old
Norm
110 and higher
The initial form of anemia
100-109
Moderate form of anemia
70–9000
9000Children 5-11 years old
Normal
115 and above
Initial form of anemia
110–114
Moderate form of anemia
80-109
Severe anemia
Below 80
Children 12-14 years old
120 and above
The initial form of anemia
110- 110- 119
Moderate form of anemia
80-109
Heavy form of anemia
Below 80
women from 15 years old and older than
Norm
120 and above
The initial form of anemia
110-119
Moderate form of anemia
80-109
Severe anemia
Below 80
Pregnant women
110 and above
The initial form of anemia
100-109
Moderate form of anemia
70–99
Severe anemia
Below 70
men from 15 years old and older than
Norm
130 and above
The initial form of anemia
110–129
Moderate form of anemia
80-109
Severe anemia
Below 80
The cost of a total blood and ESR microscopy, together with blood taking, is in the range of 1100 r.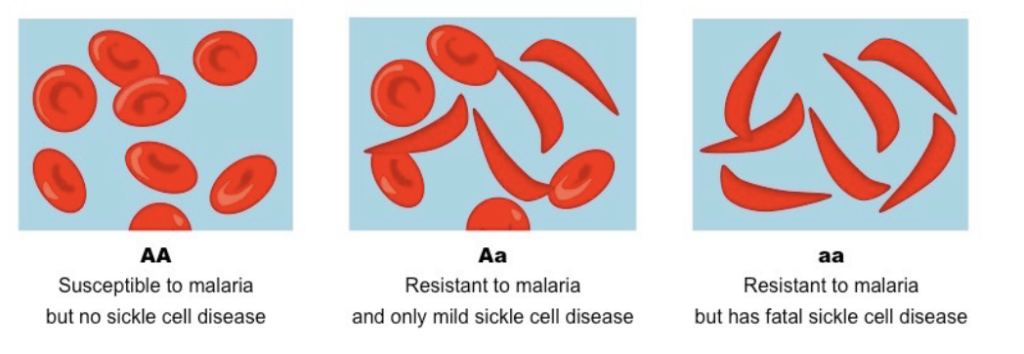
Step 2. Understand the causes of anemia - the method of treatment will depend on this.
At this stage, the doctor will review the results of the complete blood count and smear. These data make it possible to understand what type of anemia the patient has: microcytic, normocytic, or macrocytic.
To clarify the diagnosis, the doctor may order additional tests. If iron deficiency anemia is suspected, hematologists usually prescribe blood tests: for the level of iron, the total iron-binding capacity of serum, for the level of ferritin - as part of this protein, iron is stored in tissues, and for the level of transferrin - as part of this protein, iron is stored in the liver.
- Analysis for iron level together with blood sampling - within 500 R.
- Analysis for total iron-binding capacity together with blood sampling - within 550 R.
- Test for transferrin together with blood sampling - within RUR 850.
- Test for ferritin with blood sampling - within RUR 900.
 or X-ray examination:
or X-ray examination: - Fecal occult blood test, self-collection of biomaterial - within 400 R.
- Endoscopy depending on the zone - from 330 R.
- X-ray of the abdominal cavity - from 568 R.
If B12 deficiency or folate deficiency anemia is suspected, doctors prescribe tests for these vitamins: P.
If the doctor decides that it is a chronic disease, he can order tests for markers of inflammation: for example, ESR and C-reactive protein or a biochemical analysis of blood or urine. Almost all of these tests can be taken under the CHI policy or in a private laboratory for money.
- C-reactive protein analysis together with blood sampling - within 750 R.
- Basic biochemical analysis together with blood sampling - within 2300 R.
- Urinalysis, self-collection of biomaterial - within 350 R.
/esr/
What does a blood test show for ESR
Is it necessary to go to the doctor if a person has low hemoglobin for many years, but feels well
Rimma Tsvetnova
hematologist at the DocMed Evidence-Based Medicine Clinic
A decrease in hemoglobin manifests itself insidiously: if a person has lost a lot of blood at once and his hemoglobin has dropped sharply, then this will significantly affect his well-being and he will need the help of a doctor. But with a gradual decrease in hemoglobin, the body manages to get used to the new working conditions, adapts, and then the person feels good. And sometimes he claims that reduced hemoglobin is his "norm".
But with a gradual decrease in hemoglobin, the body manages to get used to the new working conditions, adapts, and then the person feels good. And sometimes he claims that reduced hemoglobin is his "norm".
If hemoglobin drops below 110 g/l in adults and children older than 6 months, it is worth contacting a general practitioner or pediatrician. Often, taking an anamnesis and examining a doctor sharply narrows the circle of causes, and the plan for further diagnostic and therapeutic measures becomes clear already at the first visit. In other cases, the doctor prescribes a number of laboratory and instrumental studies designed to clarify the situation.
In no case should you take additional tests yourself, even if the laboratory has carefully combined them into a comprehensive service called "anemia diagnosis". Most likely, the received information will be redundant or insufficient.
How to treat anemia
Treatment will depend on the cause that caused this condition.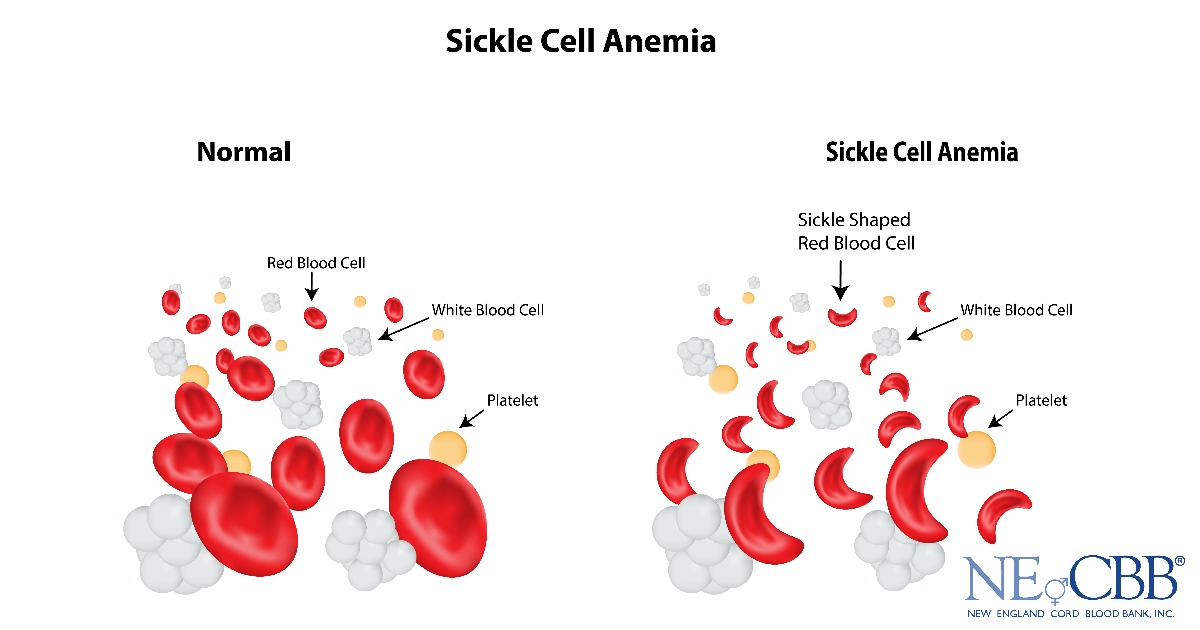
Iron deficiency anemia and anemia of chronic diseases. The approach to treatment depends on the form and severity of iron deficiency anemia. For example, people with an initial form of anemia—most often young women, pregnant women, and children—can benefit from iron supplements in tablets, syrups, or drops. The doctor should choose the medicine and prescribe the dosage. Diet does not cure anemia: even from food rich in iron, too little of it is absorbed to restore reserves.
Management of Iron Deficiency Anemia in Adults - International Physician Textbook Uptodate
Management of Anemia Associated with Chronic Diseases - International Physician Textbook Uptodate
Federal Clinical Guidelines for the Diagnosis and Treatment of Iron Deficiency Anemia, 2015PDF, 685 KB in the population
and internal bleeding, chronic diseases, inflammatory diseases of the stomach and intestines, iron losses are usually more severe. In addition to treating the underlying disease, such patients are usually prescribed intravenous iron preparations.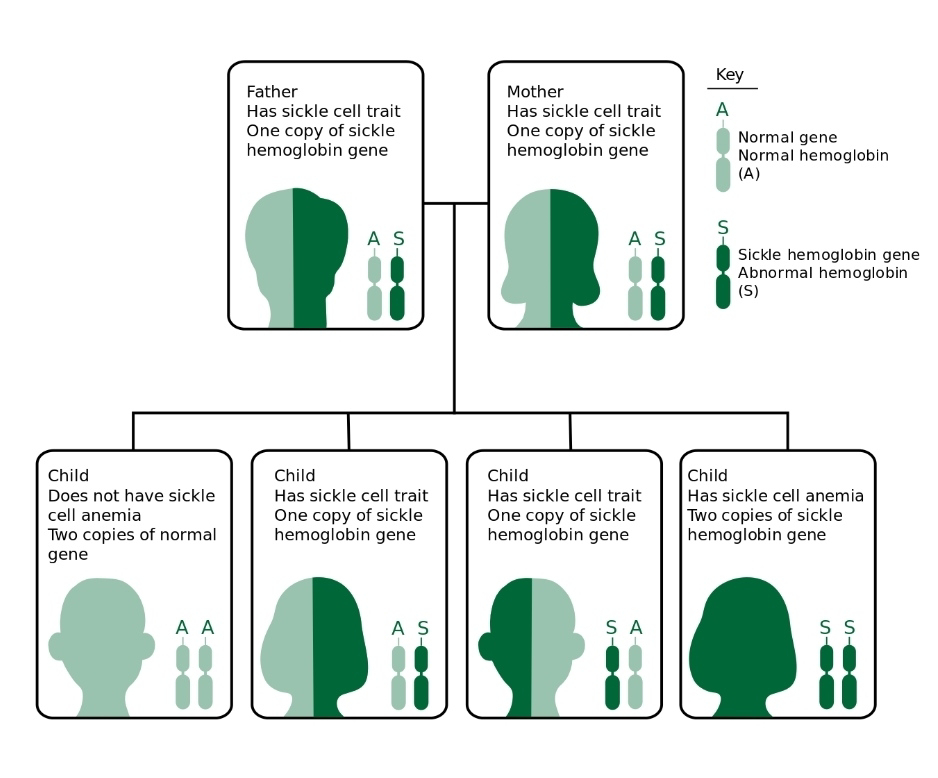 This allows you to replenish stocks faster. And iron introduced into the blood can be absorbed even by patients with inflammatory diseases of the gastrointestinal tract.
This allows you to replenish stocks faster. And iron introduced into the blood can be absorbed even by patients with inflammatory diseases of the gastrointestinal tract.
If the drug and dose were chosen correctly, the symptoms of anemia disappear on average after 7-10 days, and the hemoglobin level returns to normal after 6-8 weeks. Treatment for mild anemia usually lasts 3 months, moderate anemia 4.5 months, and severe anemia 6 months.
The cost of an iron preparation depends on the manufacturer, the number of doses in the package and the dosage form. As a rule, injectables are more expensive than tablets, and tablets are more expensive than drops.
Anemia associated with vitamin B12 deficiency. The approach to treatment depends on the severity of the anemia. In the initial stages, if the deficiency is associated with a lack of vitamins in food, taking vitamins in tablets may be sufficient.
If a person can make dietary adjustments, supplements or medications can be discontinued as soon as the CBC and vitamin B12 blood tests show that the vitamin B12 level has returned to normal.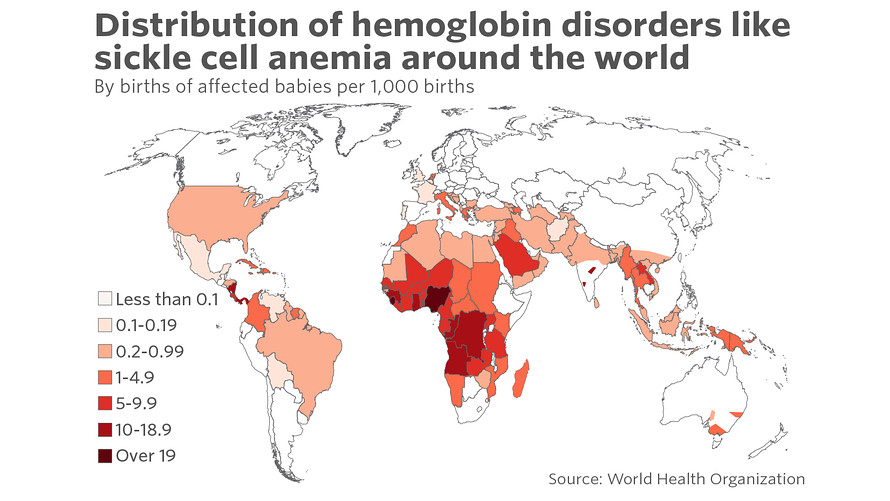
However, vegans need to supplement with the recommended daily dose of vitamin B12 for as long as they are on this type of diet.
Macrocytic Anemia - International Manual for Physicians Uptodate
Federal Clinical Guidelines for the Diagnosis and Treatment of Anemia Due to Vitamin B12 Deficiency, 2014PDF, 618KB
Treatment of Vitamin B12 and Folic Acid Deficiency - Manual for Physicians Uptodate
4
anemia, or if a person is unable to absorb vitamin tablets due to inflammatory bowel disease, they usually require drugs for subcutaneous or intramuscular injection. The doctor must select them.Treatment with vitamin B12 injections lasts an average of 4 weeks, and maintenance therapy lasts 8 months. If the cause of the anemia cannot be corrected, the patient will have to undergo a course of treatment of 10-15 injections annually.
Anemia associated with vitamin B9 deficiency. For most patients with folic acid deficiency, taking medications or supplements in tablets is sufficient: vitamin B9 is well absorbed from tablets, even in people with bowel disease.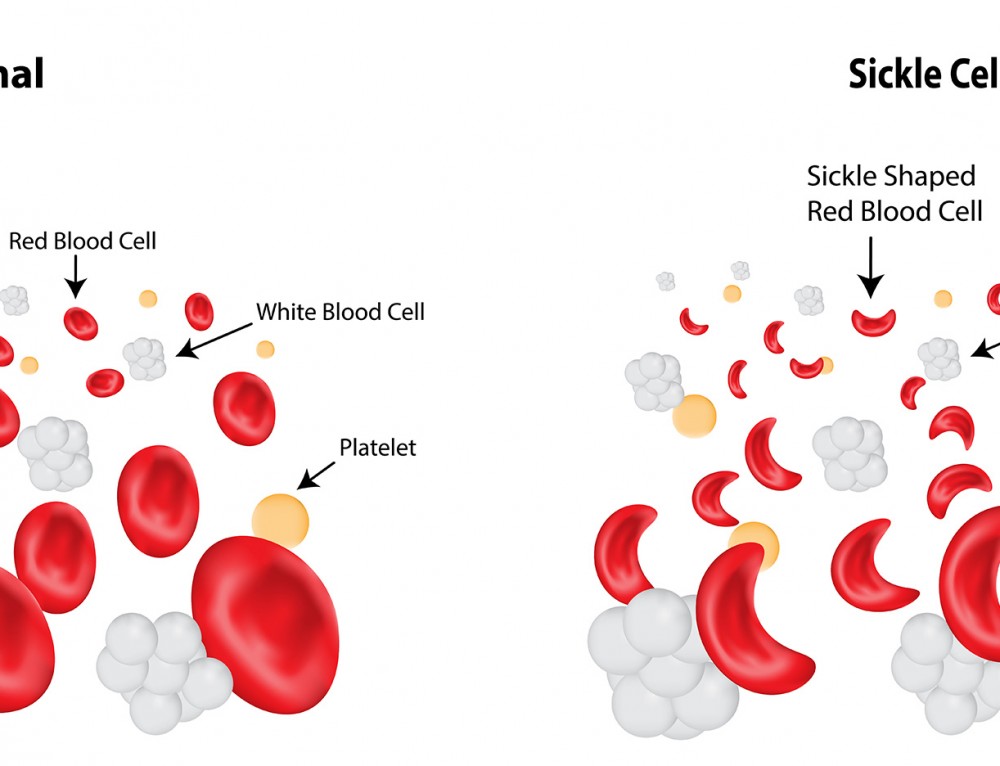 The doctor should select the drug and dosage. Treatment on average takes from one to four months.
The doctor should select the drug and dosage. Treatment on average takes from one to four months.
What drugs should be used to treat B12-deficiency and folic acid deficiency anemia
Rimma Tsvetnova
hematologist at the DocMed Evidence-Based Medicine Clinic
Vitamin B12 deficiency and folic acid deficiency can lead to anemia. These two types of anemia are very similar, but with vitamin B12 deficiency, neurological symptoms can also develop.
In our country, a classic and affordable remedy for the treatment of B12 deficiency anemia is cyanocobalamin - cheap ampoules in an ugly cardboard box. Many patients are confused by the type and price of the drug, they are trying to find something "better", and their search leads to methylcobalamin oral sprays - this is one of the two active forms of vitamin B12. Methylcobalamin eliminates only a part of the symptoms of B12 deficiency, therefore it cannot be recommended for treatment.
Folic acid, which is prescribed for women who are planning and already pregnant, is the same drug that is used to treat folate deficiency anemia.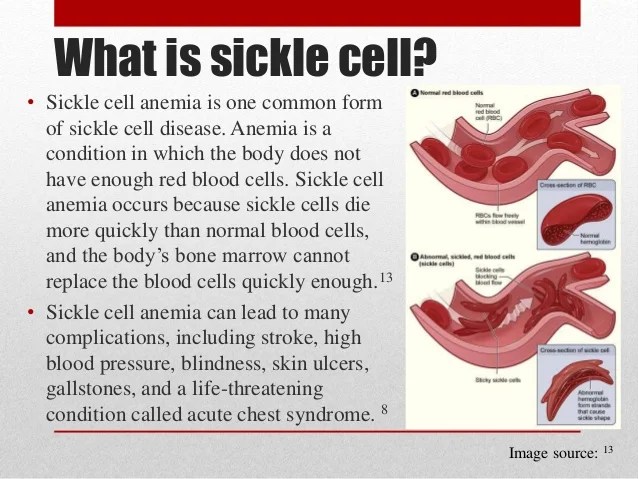 Depending on the weight, age and reason for taking the drug, only the dose changes.
Depending on the weight, age and reason for taking the drug, only the dose changes.
You can spend from 10,458 R for the treatment of iron deficiency anemia
| Purpose | Price |
|---|---|
| Hematologist appointment | Average 4000 R |
| Complete blood count, iron level, total iron binding capacity, transferrin and ferritin | From 3700 R |
| General practitioner appointment | Average 2500 R |
| Iron preparation | 250-1400 R |
Hematologist appointment
Average 4000 R
Complete blood count, iron level, total iron-binding capacity, transferrin and ferritin
from 3700 r
Take of the therapist
on average 2500 r
drug iron
250-1400 r
on the treatment of anemia associated with internal bleeding, you can spend from 10 900 r
| Purpose of | Price |
|---|---|
| Hematologist's appointment | Average 4000 R |
| Complete blood count, iron level, total iron-binding capacity, transferrin and ferritin | From 3700 R |
| General practitioner appointment | Average 2500 R |
| Fecal occult blood test | From 400 R |
| Endoscopy or abdominal x-ray | 300-500 P |
| Surgery | Depends on scope of intervention |
Hematologist appointment
Average 4000 R
Complete blood count, iron level, total iron-binding capacity, transferrin and ferritin
from 3700 r
Therapist reception
on average 2500 r
Calais analysis for hidden blood
of 400 r
Endoscopy or x -ray of the abdominal cavity
300-500 RSurgery
depends on the volume of intervention
Treatment of anemia associated with chronic diseases can be spent from 13,540 R
| Purpose | Price |
|---|---|
| Hematologist's appointment | Average 4000 R |
| Complete blood count, iron level, total iron binding capacity, transferrin and ferritin | From 3700 R |
| CRP, blood chemistry, urinalysis | From 3340 R |
| General practitioner appointment | Average 2500 R |
| Treatment of underlying disease | Depending on disease |
Hematologist appointment
Average 4000 R
Complete blood count, iron level, total iron-binding capacity, transferrin and ferritin
From 3340 R
Appointment with a therapist
On average 2500 R
Treatment of the underlying disease
Depending on the disease
Treatment of B12 deficiency anemia can be spent from R 11 2360332
| Purpose | Price |
|---|---|
| Hematologist's appointment | Average 4000 R |
| Complete blood count, iron level, total iron binding capacity, transferrin and ferritin | From 3700 R |
| General practitioner appointment | Average 2500 R |
| Vitamin B12 test | From 1000 R |
| Cyanocobalamin injection | 36 R |
Reception of a hematologist
On average 4000 r
A total blood level, total iron -binding capacity, transferrin and ferritin
dated 3700 r
Take of therapist
on average 2500 r
Analysis for vitamin B1222
From 1000 R
Cyanocobalamin in injections
36 R
Treatment of folic acid deficiency anemia can be spent from 11 336 R
| Purpose | Price |
|---|---|
| Hematologist's appointment | Average 4000 R |
| Complete blood count, iron level, total iron binding capacity, transferrin and ferritin | From 3700 R |
| General practitioner appointment | Average 2500 R |
| Vitamin B9 test | From 1100 R |
| Folic acid for pregnant women | 36 R |
Reception of a hematologist
On average 4000 r
A total blood level, total iron -binding capacity, transferrin and ferritin
dated 3700 r
Take of therapist
on average 2500 r
Analysis for vitamin B9
From 1100 R
Folic acid for pregnant women
36 R
Complications and severity of anemia
It would be wrong to talk about complications of anemia. Anemia itself is a complication associated, for example, with iron deficiency. There are no complications of complications - it is more correct to assess the severity of anemia, but only a doctor can establish it, everything is complicated there.
Anemia itself is a complication associated, for example, with iron deficiency. There are no complications of complications - it is more correct to assess the severity of anemia, but only a doctor can establish it, everything is complicated there.
Prevention of anemia
Only malnutrition-related anemia can be prevented. This is primarily anemia associated with a lack of iron and B vitamins.
The best way to prevent this, which is suitable for all healthy people, is a varied diet that includes products of plant and animal origin. People at risk who may lack vitamins and iron from food may need vitamin supplements.
For example, women preparing for pregnancy and early pregnancy are advised to take 400 micrograms of folic acid daily as a dietary supplement. For vegans, it makes sense to talk to your doctor about taking a vitamin B12 supplement. Some girls who have recently started their period may benefit from an iron supplement, but the need to take it should also be discussed with a doctor.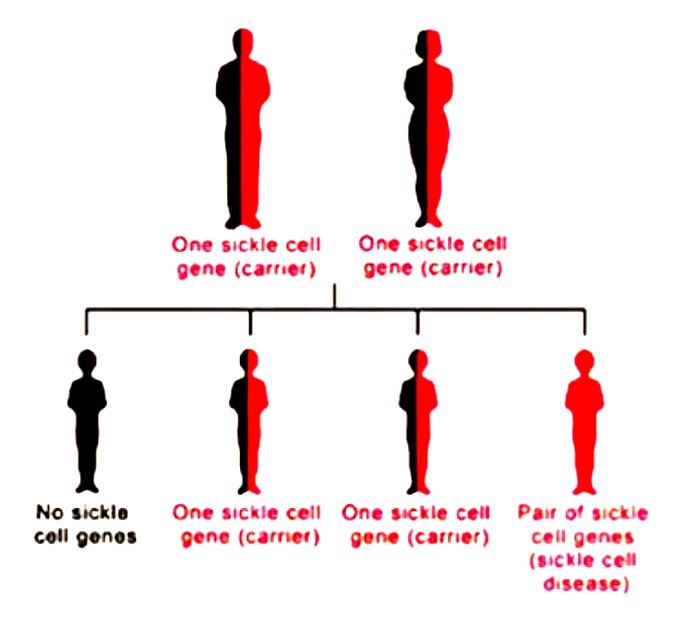
Contraindications for anemia
Only a doctor can formulate contraindications. They depend on what concomitant diseases are present in a person, so it will not be possible to generalize contraindications. In the most common case, with anemia, you have to live as you live, but with medicines.
Is it possible to get vaccinated against coronavirus with anemia
Anemia is not a contraindication for vaccination against coronavirus disease.
The list of contraindications to vaccination is very small. People under the age of 18, pregnant and lactating women, as well as people with infectious and chronic diseases in the acute phase cannot be vaccinated. At the same time, people with symptoms of a cold and intestinal infection can be vaccinated as soon as the temperature subsides.
True contraindications to vaccination are only in people with a very severe allergic reaction, or anaphylaxis:
- for any medication;
- for vaccine components - one of them, polysorbate 80, is in the Russian drug Sputnik V.
 At the same time, there is a cross-allergy to polyethylene glycol and polysorbate: if a patient is allergic to one substance, there may be an allergy to another. Before vaccinating people with an allergy to polyethylene glycol, it makes sense to consult with an allergist. Most likely, it is possible to be vaccinated, but only on the condition that the doctor observes the condition of the vaccinated person for at least half an hour;
At the same time, there is a cross-allergy to polyethylene glycol and polysorbate: if a patient is allergic to one substance, there may be an allergy to another. Before vaccinating people with an allergy to polyethylene glycol, it makes sense to consult with an allergist. Most likely, it is possible to be vaccinated, but only on the condition that the doctor observes the condition of the vaccinated person for at least half an hour; - if the cause of a severe allergic reaction that happened in the past could not be determined.
Remember
- Anemia is a decrease in the mass of red blood cells, or erythrocytes, in the human body. There can be many causes for anemia, but the most common are iron deficiency, vitamin B12 or vitamin B9 deficiency, occult bleeding, or chronic illness.
- Anemia often has no symptoms at all. It can be suspected if a person has hemoglobin below 110 g / l, pale or yellowish skin, cold hands and feet, he quickly gets tired, he often feels dizzy or has a headache, there are arrhythmias and shortness of breath.

 Pain can also occur in the bones. The pain varies in intensity and can last from a few hours to several weeks.
Pain can also occur in the bones. The pain varies in intensity and can last from a few hours to several weeks. 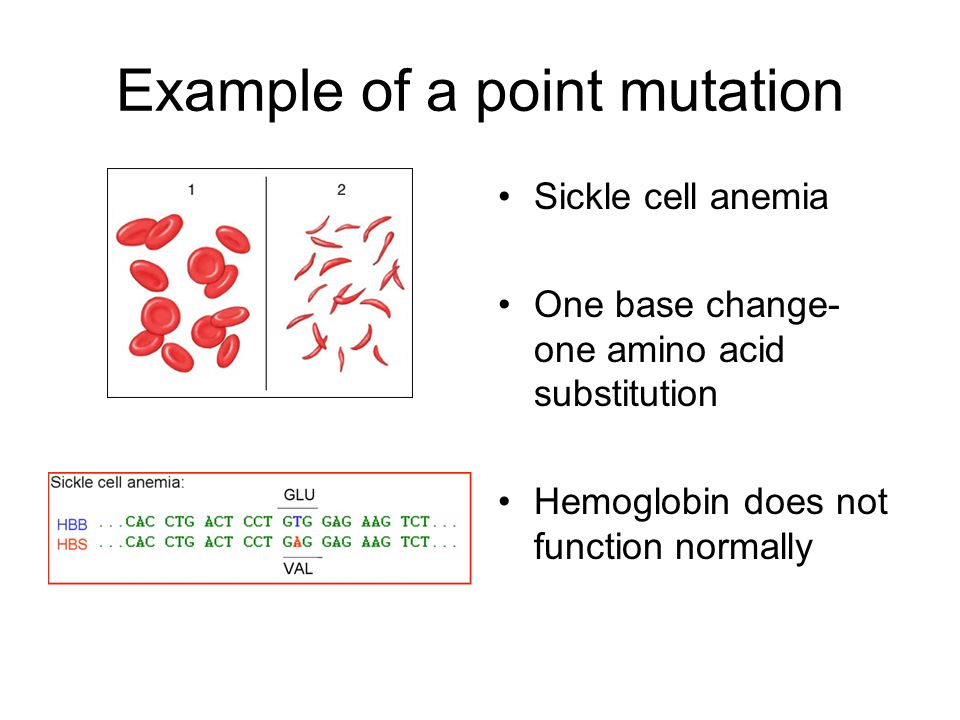
 This complication usually affects adults, not children. Shortness of breath and fatigue are common symptoms of this disease, which can be fatal.
This complication usually affects adults, not children. Shortness of breath and fatigue are common symptoms of this disease, which can be fatal. 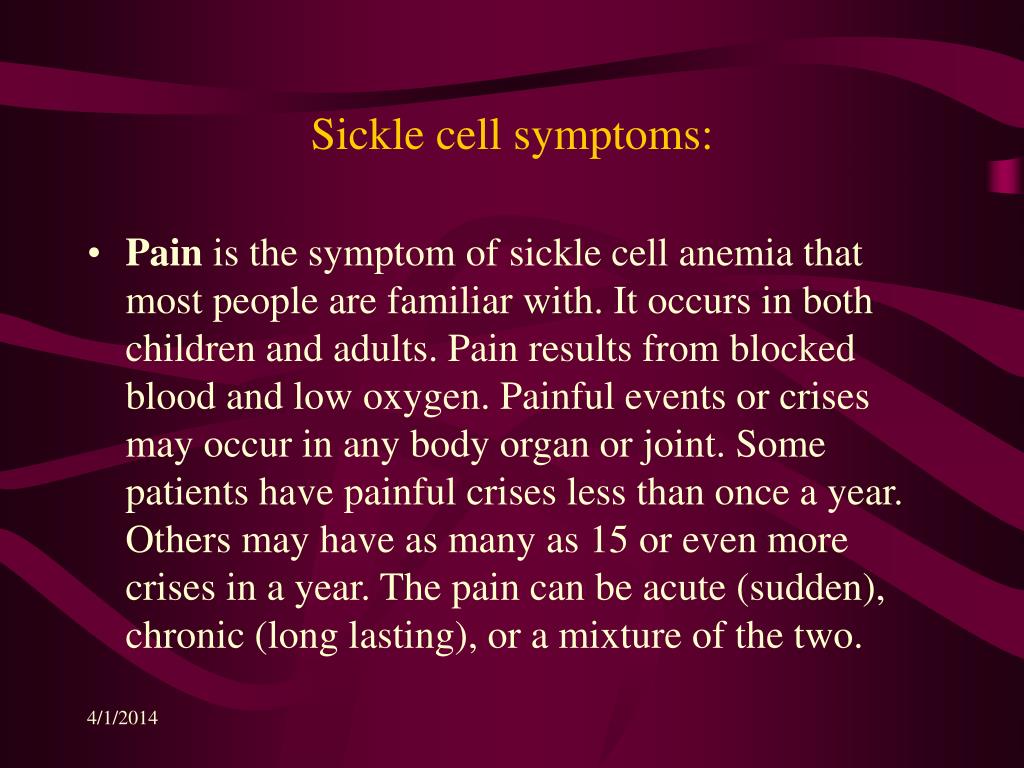
 The procedure is usually reserved for people under the age of 16, as the risks increase further.
The procedure is usually reserved for people under the age of 16, as the risks increase further. 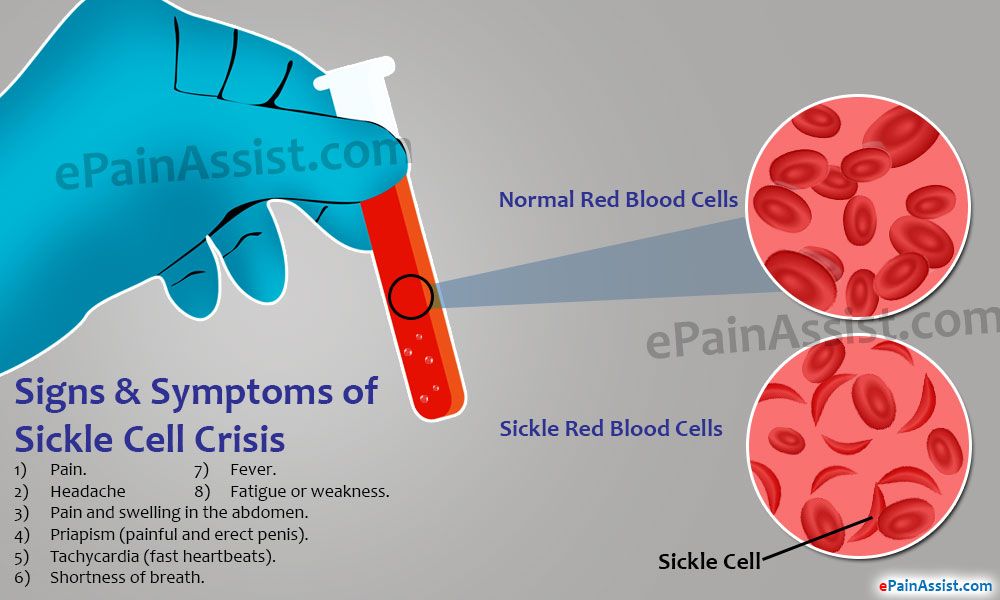 Some adult patients require lifelong antibiotics. Pain medications are used to relieve pain during crises. Hydroxyurea, when taken daily, reduces the frequency of painful crises and may reduce the need for blood transfusions and hospitalizations. To prevent various diseases, both children and adults are recommended to be vaccinated
Some adult patients require lifelong antibiotics. Pain medications are used to relieve pain during crises. Hydroxyurea, when taken daily, reduces the frequency of painful crises and may reduce the need for blood transfusions and hospitalizations. To prevent various diseases, both children and adults are recommended to be vaccinated 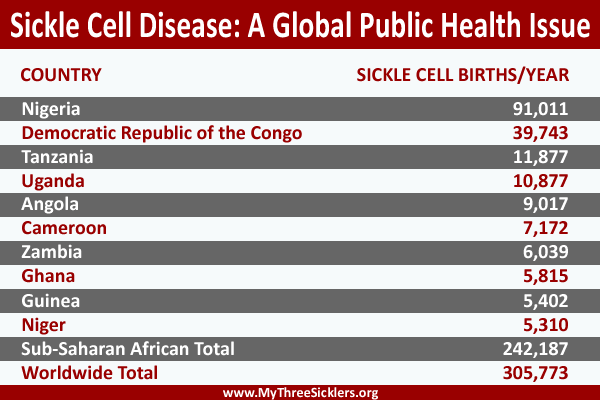 Talk to your doctor about which exercise is right for you.
Talk to your doctor about which exercise is right for you.