How does a child get kawasaki disease
Kawasaki Disease | Symptoms, Diagnosis, Treatment & Long-Term Effects
Kawasaki disease is an illness that makes the blood vessels in the body swell and become inflamed. The exact cause of Kawasaki disease is unknown. Because it causes a high fever and swelling of the lymph nodes, Kawasaki disease is thought to be related to an infection. It may occur in children who have a genetic predisposition to the disease. The disease is not contagious.
The symptoms of Kawasaki disease often go away on their own, and the child recovers. Without medical evaluation and treatment however, serious complications may develop and not be initially recognized.
Kawasaki disease more commonly affects children younger than 5 years old, with the majority of children being less than 2 years old. Kawasaki disease, however, can affect older children as well. The disease occurs more often among boys. It is more commonly seen in the winter and spring months.
Diagnosis
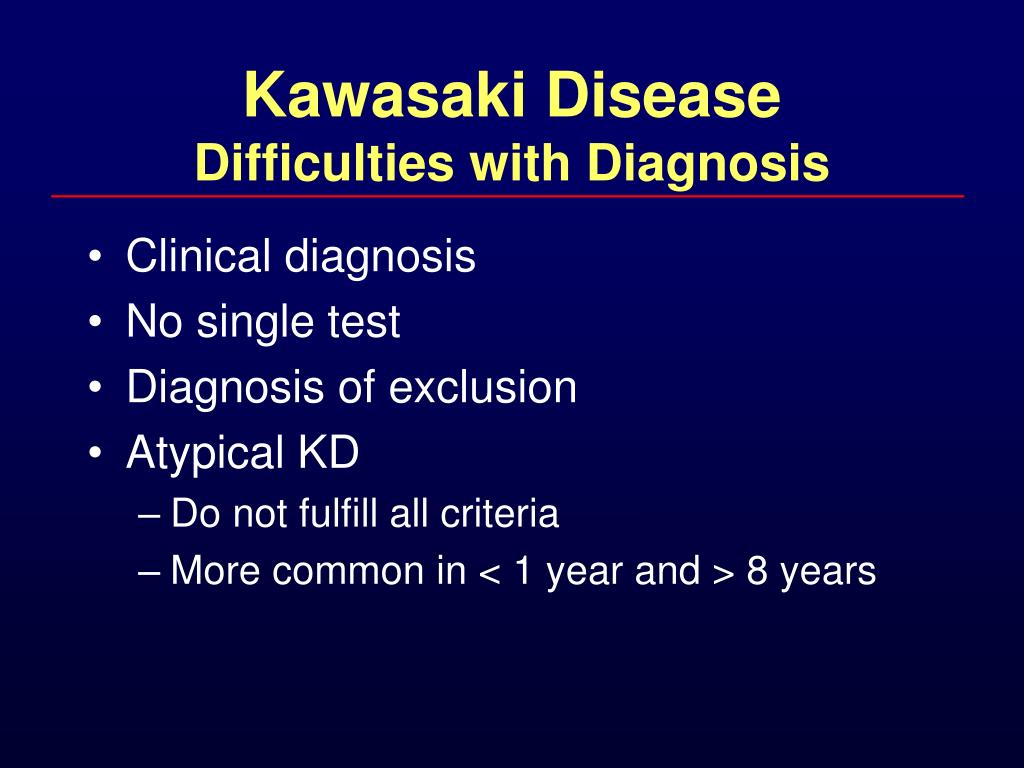
There is no one specific test to diagnose Kawasaki disease. The doctor makes the diagnosis based on your child’s signs and symptoms. Lab tests may help with diagnosis. A prolonged fever (i.e., more than five days and generally higher than 101.3 F) is often the first symptom that alerts a doctor to consider Kawasaki disease. Signs and symptoms that help make the diagnosis include:
- Prolonged high fever (lasting longer than five days and generally higher than 101.3 F)
- A nonspecific red rash that often involves the groin area and may peel
- Red eyes, or conjunctivitis without drainage
- Very red lips and tongue
- Enlarged lymph nodes on one side of the neck
- Swollen & red hands and feet occasionally followed by peeling of skin
- Painful joints
- Irritability in younger patients
- In some children, enlargement of the gall bladder can cause belly pain and vomiting
Other diseases and common viruses may have these same symptoms. To determine if a child has Kawasaki disease, the doctor may order blood tests to look for:
- Recent strep or viral infection
- Body’s immune response
Sometimes a urine sample is also collected.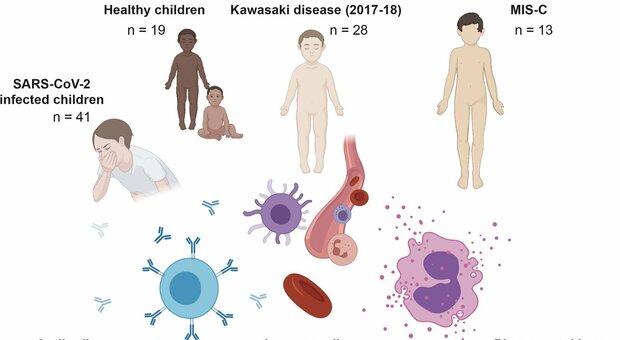
These laboratory tests are helpful; however, the only way to make the diagnosis of Kawasaki disease is by meeting the clinical criteria for most of the signs and symptoms listed above.
If your child meets the criteria for the diagnosis of Kawasaki disease, the cardiology team is consulted. The cardiologist and/or nurse practitioner performs a history and physical exam. Your child will have an electrocardiogram (to assess the electrical system of the heart) and an echocardiogram (ultrasound of the heart). Even if these studies are normal, your child will receive treatment based on clinical symptoms and lab work.
Effect of Kawasaki Disease on the Heart
Kawasaki disease can affect the heart by causing the following complications:
- Coronary artery aneurysms (or ballooning of the arteries)
- Leakage of valves (often mitral valve regurgitation)
- Build-up of fluid around the heart (pericardial effusion)
Kawasaki disease is the leading cause of acquired heart disease in children. In as many as 25 percent of children with Kawasaki disease, the heart becomes affected without proper treatment. Aneurysms of the coronary arteries, the blood vessels that supply oxygen to the heart itself, are the most important complication of Kawasaki disease. With appropriate and timely treatment, the risk of coronary artery involvement decreases to around 5 percent.
In as many as 25 percent of children with Kawasaki disease, the heart becomes affected without proper treatment. Aneurysms of the coronary arteries, the blood vessels that supply oxygen to the heart itself, are the most important complication of Kawasaki disease. With appropriate and timely treatment, the risk of coronary artery involvement decreases to around 5 percent.
In general, if coronary artery changes have not occurred by six to eight weeks after the onset of the illness, the risk of developing these changes is very low.
If a coronary aneurysm develops, the presence of long-term coronary artery changes depends on the size of the aneurysm – the coronary artery changes can resolve, remain unchanged, or progress. Patients with large aneurysms are at risk for developing coronary artery clots or stenosis (narrowing) as the aneurysms heal.
It has been reported that in half of the patients with small coronary aneurysms, the changes resolve during the first year following the illness.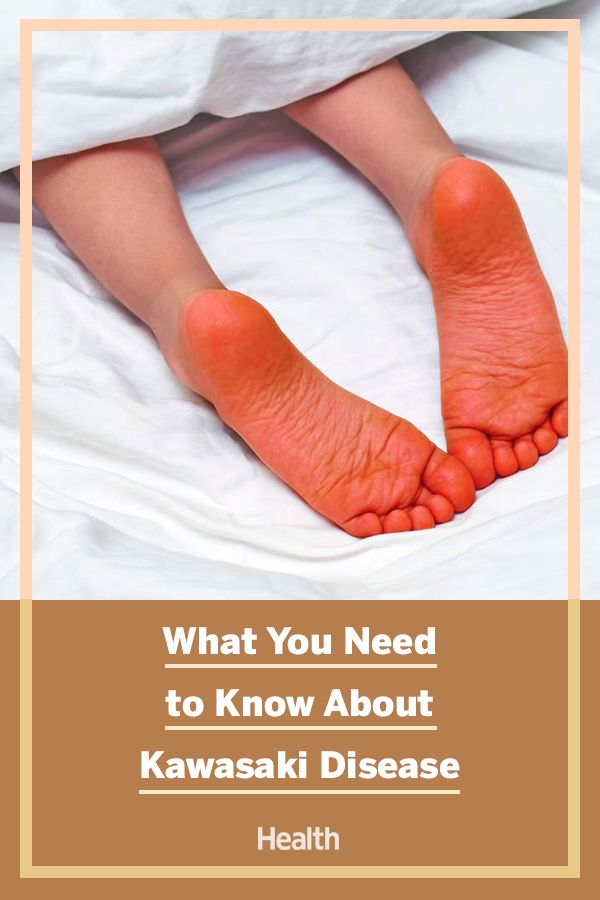 Unfortunately, doctors cannot predict which course a patient will take.
Unfortunately, doctors cannot predict which course a patient will take.
Regardless of coronary artery involvement, your child will need to see a pediatric cardiologist through childhood and often into adulthood. Cincinnati Children’s Heart Institute has a Coronary Artery Clinic that specializes in this patient population.
What if coronary artery changes occur?
Due to the vessel wall irregularity, a coronary artery aneurysm can become a site of blood clot. If a large enough blood clot forms, it can block the blood flow, and the heart tissue becomes deprived of needed oxygen, and in rare cases, could lead to a heart attack.
Depending upon the size and number of the coronary aneurysms, your child may need to be on medicine to prevent blood clotting. If the aneurysms are small and few, the medicine will usually be only aspirin taken once a day. If the aneurysms are large (termed “giant aneurysms”), a blood thinner such as Coumadin (warfarin) is used.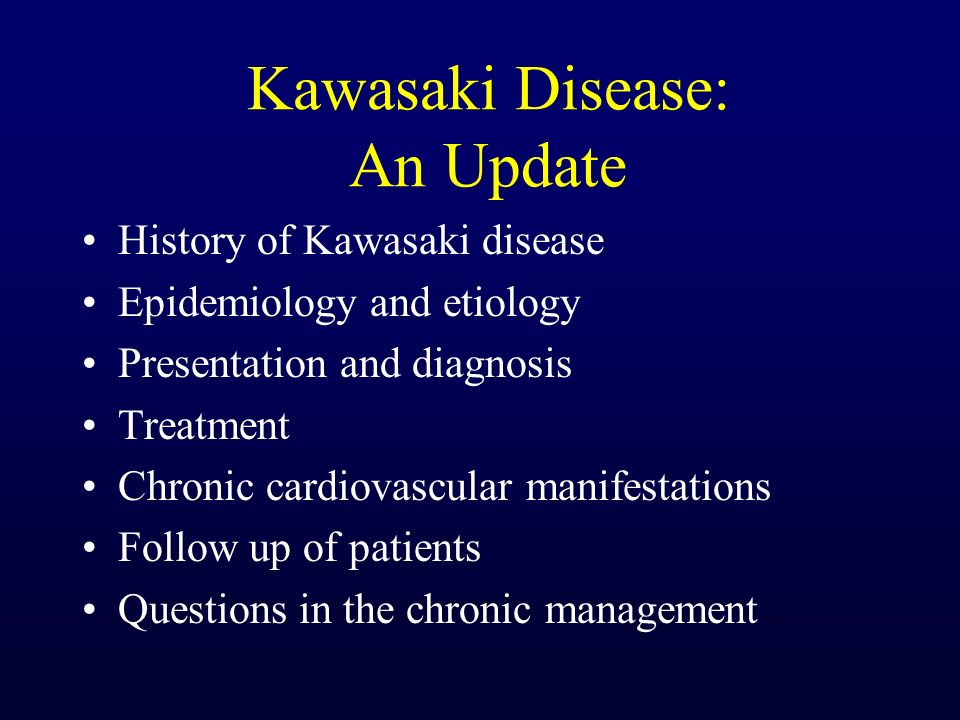
Children with giant coronary aneurysms will need periodic cardiac catheterization to check the size of the vessels. Periodic stress / exercise tests are used to check the heart’s ability to get enough oxygen during exertion.
Children with larger coronary artery aneurysms or abnormal stress / exercise tests may have restrictions from certain physical activities.
Treatment for Kawasaki Disease
Children are usually admitted to the hospital for two – five days.
Treatment includes intravenous gamma globulin (IVIG), which is an infusion through your child’s IV and high-dose aspirin every six hours.
- These medicines help reduce the swelling and inflammation in the blood vessels. IVIG can decrease, but NOT eliminate, the risk of developing coronary aneurysms.
- The infusion is most effective if given within the first 10 days of the illness. The risk of developing coronary changes decreases from 25 percent to less than 5 percent when you give in the first 10 days of illness.
After discharge, your child will continue to take high-dose aspirin until the signs of inflammation and fever have resolved.
- Children continue taking a low-dose aspirin every day for usually six to eight weeks or more.
- Your child will continue to be followed by a cardiologist after Kawasaki disease resolves.
Parents are often concerned about using aspirin in children due to the concern over the link of aspirin use and Reye syndrome. Reye syndrome is an inflammatory process that occurs in the brain and has been connected with patients who have long-term aspirin use and have chicken pox or influenza. Some doctors suggest that if your child is taking aspirin for a long period for any reason, they should have a flu shot to avoid influenza infection.
If your child is on aspirin and they have been exposed to or have chicken pox, you should contact your doctor immediately for advice.
Cardiology Follow-Up
Your child will follow-up with cardiology after discharge. Your child will initially be seen at two weeks and six to eight weeks. We will repeat the echocardiogram and electrocardiogram during these visits to check your child’s coronary arteries. If by six to eight weeks there is no evidence of cardiac involvement, your child's cardiac risks are extremely low.
Your child will initially be seen at two weeks and six to eight weeks. We will repeat the echocardiogram and electrocardiogram during these visits to check your child’s coronary arteries. If by six to eight weeks there is no evidence of cardiac involvement, your child's cardiac risks are extremely low.
If there is no coronary artery involvement by six to eight weeks, your child will then see the cardiology team every year to every few years. Your cardiology team may also ask for more blood work such as cholesterol and triglyceride levels.
Long-Term Outlook
If after one year from the diagnosis of Kawasaki disease there is no heart involvement, your child’s cardiology visits are spaced out to annual visits or even every few years.
Patients that have coronary aneurysms require periodic cardiology evaluations. The frequency of these visits varies depending on the extent of coronary changes. Often these visits are scheduled once every six to 12 months. With the right medical care, these patients also generally have a good prognosis. Since Kawasaki disease affects the coronary arteries, it is prudent for families and patients to practice heart healthy habits which help to prevent adult coronary artery disease and heart attacks.
Since Kawasaki disease affects the coronary arteries, it is prudent for families and patients to practice heart healthy habits which help to prevent adult coronary artery disease and heart attacks.
Reviewed by Amanda Hoerst, MSN, APRN, CNP
Kawasaki Disease in Children | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is Kawasaki disease in children?
Kawasaki disease is a rare illness that most commonly affects children ages 0 to 5, but can sometimes affect children up to the age of 13. It is a type of vasculitis. Vasculitis means inflammation of the blood vessels. It can affect the whole body, including the blood vessels of the heart (coronary arteries). The cause of Kawasaki disease is unknown. Without treatment, affected children are at higher risk of developing problems with the coronary arteries. Other areas of the heart may also be affected. With timely treatment, most children recover with no lasting problems.
Other areas of the heart may also be affected. With timely treatment, most children recover with no lasting problems.
Which children are at risk for Kawasaki disease?
Children of any race or ethnic group can get Kawasaki disease. It's more common in children whose families are from East Asia or Asian ancestry. Most children who get Kawasaki disease are younger than 5 years old. It occurs in boys more often than in girls.
What causes Kawasaki disease in a child?
The cause of Kawasaki disease is not known. Researchers think it may be the result of an infection.
What are the symptoms of Kawasaki disease in a child?
These are common symptoms of Kawasaki disease:
- Fever of 102.0° F to 104.0° F (38.8°C to 40.0°C) that lasts for at least 5 days
- Red rash
- A swollen lymph node, usually in the neck
- Swollen hands and feet
- Red eyes
- Red and dry cracked lips
- Red tongue with white spots (called “strawberry tongue”)
- Irritability
- Fast heart rate
- Diarrhea or vomiting
- Skin peeling
The symptoms of Kawasaki disease can look like other health conditions. Make sure your child sees his or her healthcare provider for a diagnosis.
Make sure your child sees his or her healthcare provider for a diagnosis.
How is Kawasaki disease diagnosed in a child?
Your child's healthcare provider can usually diagnose Kawasaki disease by his or her symptoms and physical exam.
To diagnose Kawasaki, other causes for the symptoms must be ruled out. A fever for 5 days must be present in addition to having 4 out of 5 of the following:
- Red eyes
- Changes in the lining of the mouth
- Skin changes in the hands and feet
- Rash
- Swollen lymph nodes
Other recommended tests include:
-
Lab tests. Blood and urine samples are taken to check for signs of inflammation. These are also used to help rule out other health problems.
-
Electrocardiography (ECG).
 This test records the electrical activity of the heart through small, sticky patches on the child's chest. The patches are connected to a machine with wires. The machine records the electrical activity. This helps check for problems with heart rhythm and heart structure.
This test records the electrical activity of the heart through small, sticky patches on the child's chest. The patches are connected to a machine with wires. The machine records the electrical activity. This helps check for problems with heart rhythm and heart structure.
- Echocardiography (echo). This test uses sound waves to create a picture of the heart. This can show problems with heart structure, valves, and heart function.
- Cardiac catheterization. This test uses a small tube that goes into the blood vessels and takes pictures of the coronary arteries using contrast and X-ray.
How is Kawasaki disease treated in a child?
Treatment will depend on your child’s symptoms, age, and general health.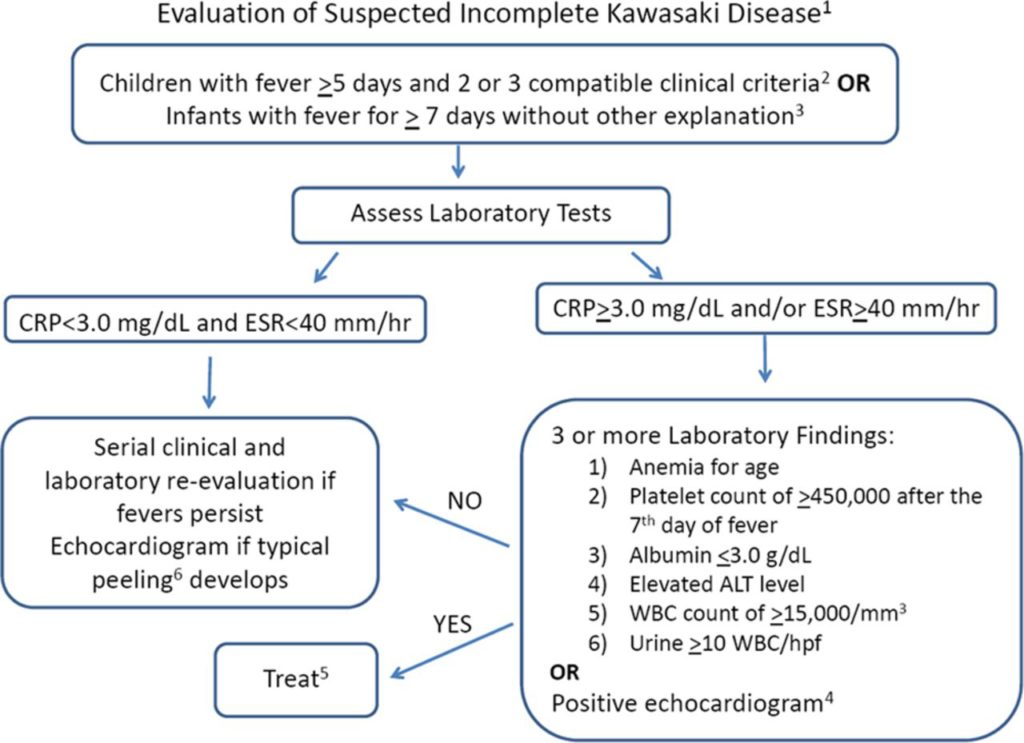 It will also depend on how severe the condition is. Treatment typically starts as soon as the problem is suspected. Your child may need to stay in the hospital for a few days or longer.
It will also depend on how severe the condition is. Treatment typically starts as soon as the problem is suspected. Your child may need to stay in the hospital for a few days or longer.
Your child's healthcare provider may prescribe aspirin or IV (intravenous) gamma globulin (IVIG). Corticosteroids and other medicines may also be prescribed if aspirin and IVIG don't work well. Once your child is home, he or she may need to take low-dose aspirin for 6 to 8 weeks. Don't give your child aspirin without first talking with the child's healthcare provider. If your child develops heart problems, the provider may send you to a pediatric cardiologist. This is a doctor with special training to treat children’s heart problems. Your child may need medicine, procedures, or surgery.
What are possible complications of Kawasaki disease in a child?
Most children with Kawasaki disease get better within a few weeks. But serious complications may occur. Those involving the heart include:
But serious complications may occur. Those involving the heart include:
- Weakening of one of the heart's arteries (coronary artery aneurysm)
- Heart muscle that doesn't work well or heart attack
- Inflammation of the heart muscle (myocarditis), lining of the heart (endocarditis), or covering of the heart (pericarditis)
- Heart valves that don't work well
- Heart failure
Kawasaki disease may also affect other body systems. This includes the nervous, immune, digestive, and urinary systems.
How is Kawasaki disease managed in a child?
If your child has a coronary artery aneurysm, he or she will need echocardiograms, sometimes for several years after the illness. Your child may need more treatment, including blood thinners to prevent clots. It's important to keep follow-up visits with your child's healthcare provider, even if your child is feeling well.
There is a risk for early coronary artery disease after having Kawasaki disease, including early heart attacks. Your child will need to follow a heart-healthy lifestyle for life. This includes eating healthy foods, getting regular exercise, and not smoking. Your child should have regular follow-up with a cardiologist throughout his or her life.
Talk with your child's healthcare provider about what to expect for your child.
When should I call my child's healthcare provider?
Call your child's healthcare provider if your child has the symptoms of Kawasaki disease. If your child is diagnosed with Kawasaki disease, keep all follow-up appointments. Also watch for signs or symptoms of complications, including:
- Tiredness
- Poor feeding or eating
- Trouble breathing
- Swelling
- Chest pain
Key points about Kawasaki disease in children
- Kawasaki disease is a serious condition that affects young children.
 It can damage blood vessels throughout the body.
It can damage blood vessels throughout the body. - Kawasaki disease is diagnosed by having certain symptoms. For example, a fever lasting at least 5 days.
- Your child’s healthcare provider will treat Kawasaki with aspirin, intravenous immune globulin (IVIG), or other medicines.
- A child with Kawasaki disease may have serious complications, especially ones affecting the heart.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child.
 Also know what the side effects are.
Also know what the side effects are. - Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
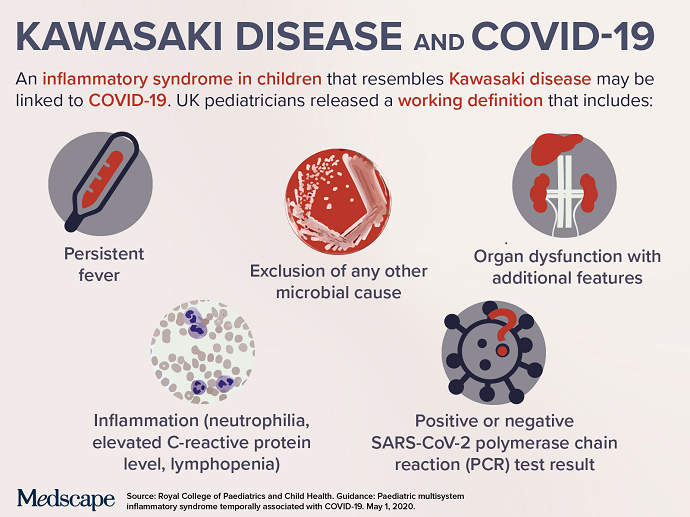
What parents of children who have had COVID-19 need to know
In the Irkutsk region, about 7.3 thousand children were ill with a new coronavirus infection, but after that some of them suffered from Kawasaki-like syndrome. This was announced at a press conference in the Oblastnaya newspaper on February 18, 2021 by the chief pediatric cardiologist of the Irkutsk region, the head of the cardiological center of the Irkutsk Regional Children's Clinical Hospital and the First Russian Center for Research on Kawasaki Disease. T. Kawasaki, Ludmila Bregel, as well as acting. Deputy Chief Physician for Medical Work Vadim Albot and Deputy Chief Physician for Organizational and Methodological Work of the Irkutsk State Regional Children's Clinical Hospital Sergei Belykh.
T. Kawasaki, Ludmila Bregel, as well as acting. Deputy Chief Physician for Medical Work Vadim Albot and Deputy Chief Physician for Organizational and Methodological Work of the Irkutsk State Regional Children's Clinical Hospital Sergei Belykh.
“About 60 children were ill with coronavirus in moderate severity, three in severe form, the rest in mild or asymptomatic,” said Vadim Albot. – There were no deaths of children from COVID-19, except for those cases when the coronavirus infection was associated with severe pathology. However, after the transfer of coronavirus, 18 children fell ill with Kawasaki-like syndrome. This is just over 1%, but the disease is dangerous. There is no correlation between the risk of getting sick with the syndrome and the severity of the disease. There are frequent cases when mild COVID-19caused Kawasaki-like syndrome.
Ludmila Bregel spoke about this in more detail:
- This syndrome has received another name in the world - multisystem inflammatory syndrome associated with COVID-19, similar in its manifestations to the classic Kawasaki disease, discovered by Dr.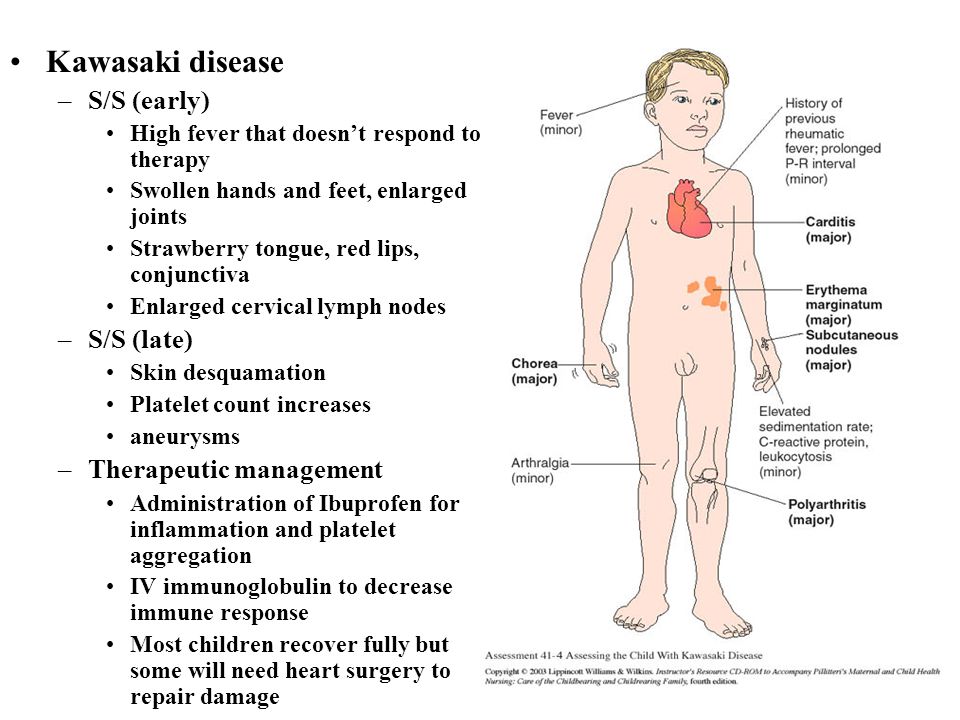 T. Kawasaki in 1967. The causative agent has not yet been identified. The disease belongs to the group of systemic vasculitis. Kawasaki affects children under 2-5 years old, Kawasaki-like syndrome affects mainly schoolchildren. The polysystem nature of the lesion is also more pronounced, in 90% state of shock occurs. The disease does not develop during the main infection with COVID-19, but after a few weeks either after the illness or after contact with the patient. Studies have shown that children with the syndrome do not have a pathogen in the nasopharynx, but all have titers of antibodies of the IgM class indicating the proximity of contact, or class G, which indicate a mature immune response, it occurs by the end of the third week of the disease. The main characteristic of this syndrome is that the child's immune system reacts in a dysfunctional manner with an excessive hyperimmune response. It is the hyperimmune response that contributes to the appearance of formidable symptoms that threaten the life of the child and create conditions for the development of shock with symptoms of cardiac, respiratory, hepatic, renal failure, often cerebral edema, damage to bone marrow hematopoiesis.
T. Kawasaki in 1967. The causative agent has not yet been identified. The disease belongs to the group of systemic vasculitis. Kawasaki affects children under 2-5 years old, Kawasaki-like syndrome affects mainly schoolchildren. The polysystem nature of the lesion is also more pronounced, in 90% state of shock occurs. The disease does not develop during the main infection with COVID-19, but after a few weeks either after the illness or after contact with the patient. Studies have shown that children with the syndrome do not have a pathogen in the nasopharynx, but all have titers of antibodies of the IgM class indicating the proximity of contact, or class G, which indicate a mature immune response, it occurs by the end of the third week of the disease. The main characteristic of this syndrome is that the child's immune system reacts in a dysfunctional manner with an excessive hyperimmune response. It is the hyperimmune response that contributes to the appearance of formidable symptoms that threaten the life of the child and create conditions for the development of shock with symptoms of cardiac, respiratory, hepatic, renal failure, often cerebral edema, damage to bone marrow hematopoiesis. That is, almost all systems are affected, and the state in which children enter is always critical.
That is, almost all systems are affected, and the state in which children enter is always critical.
All 18 patients in the Irkutsk region, fortunately, survived. Most of the children fell ill in late November - early December 2020, in January 2021 and have already left the intensive care unit. Four are recovering at the cardiology department of the IGOCDCH and one is at the Ivano-Matreninsky Children's Hospital. Such a number of children in 2.5 months for Kawasaki-like syndrome is a lot. The first outbreak was registered in March-April 2020 in the Italian city of Bergamo, where 11 patients were admitted in 2-3 weeks. The frequency of the disease exceeded the usual frequency by 30 times. In Moscow - more than 200 cases of the disease. In the Irkutsk region, the excess frequency was 7-8 times.
Early symptoms are also very similar to Kawasaki disease and are characterized by high, drug-resistant fever, rash on the skin and mucous membranes, bright coloration of the lips, conjunctivitis of the eyes, hyperemia of the oral mucosa, redness, peeling and swelling of the palms and soles, swollen lymph nodes.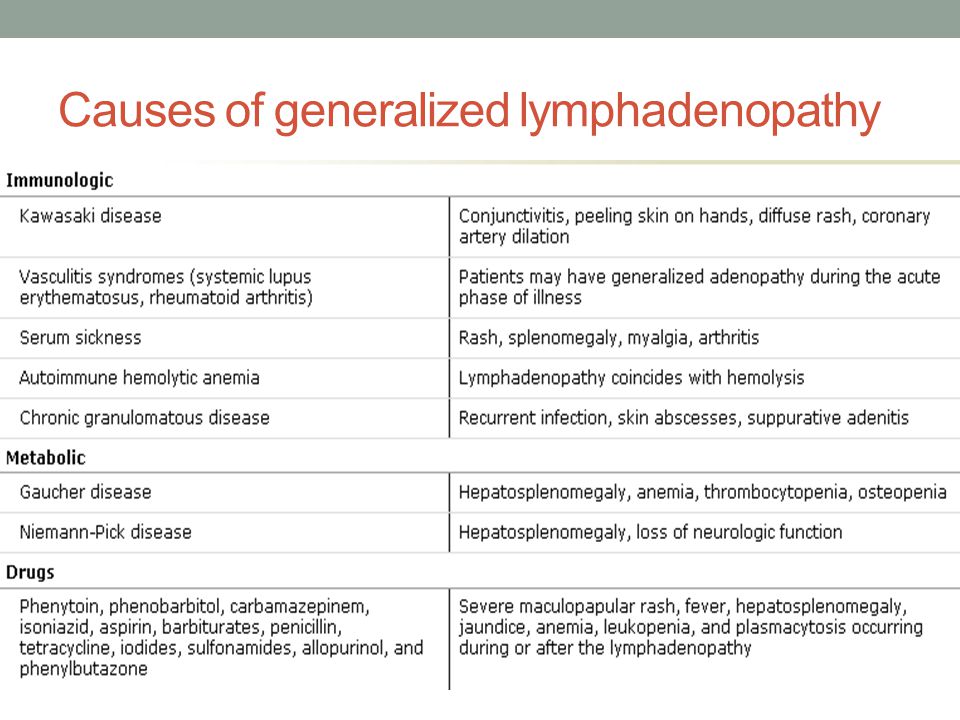 These are external signs, they do not threaten the life of the child. The main process that threatens the heart and other internal organs takes place in the vessels, causing shortness of breath, palpitations, increased blood pressure, changes in the heart and gastrointestinal tract, kidneys, etc. Symptoms of the lesion unfold very quickly, within a few days, and actually develop vasogenic or cardiogenic shock with damage to blood vessels or the heart. Children are admitted immediately to the intensive care unit.
These are external signs, they do not threaten the life of the child. The main process that threatens the heart and other internal organs takes place in the vessels, causing shortness of breath, palpitations, increased blood pressure, changes in the heart and gastrointestinal tract, kidneys, etc. Symptoms of the lesion unfold very quickly, within a few days, and actually develop vasogenic or cardiogenic shock with damage to blood vessels or the heart. Children are admitted immediately to the intensive care unit.
Ludmila Bregel emphasized that the development of this syndrome can be triggered by improper treatment of COVID-19.
- Very often, this infection, like other viral diseases, is treated with antiviral drugs, which are stimulants of the immune system, inducers of interferon synthesis. And since we are talking about a hyperimmune response, these drugs are actually adding fuel to the fire. It is not uncommon for parents to give several similar drugs at the same time. This is deadly.
This is deadly.
Experts noted that municipal hospitals were initially very skeptical about Kawasaki syndrome.
“Now not everyone trusts the concept of multisystem inflammatory syndrome associated with COVID-19, they often confuse it with sepsis,” added Vadim Albot. – We even had a lot of discussions with colleagues in our hospital. When consulting doctors from the districts, we feel some resistance and misunderstanding. It's hard for people to readjust when they're used to being treated for a set of symptoms. The treatment that is useful for one disease may be completely contraindicated for another.
Disputes about a new disease are going on all over the world, while there is no single point of view on this issue, but it is interesting that the treatment is the same everywhere - this is intravenous human immunoglobulin and the treatment regimen for multisystem inflammatory syndrome, if it occurs with damage to the circulatory system. Unlike adults, the lungs of these children are not affected or affected very rarely.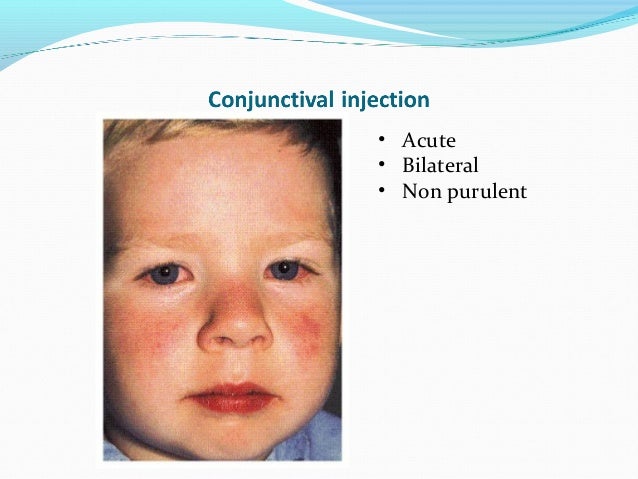 More often it is pulmonary edema caused by heart damage, which looks like pneumonia on MSCT. Treatment of shock with a timely diagnosis can take about a week of stay in intensive care, much more will require the restoration of damage to other organs. The children then spend two to three weeks in the hospital. What consequences this will cause in the future is still unknown.
More often it is pulmonary edema caused by heart damage, which looks like pneumonia on MSCT. Treatment of shock with a timely diagnosis can take about a week of stay in intensive care, much more will require the restoration of damage to other organs. The children then spend two to three weeks in the hospital. What consequences this will cause in the future is still unknown.
- We examine the children after discharge in 3-4-5 weeks, after 2-3 months we plan to re-hospitalize. Perhaps in a few months we will be able to draw conclusions from remote observation,” said Ludmila Bregel.
Sergei Belykh added that the introduction of telemedicine technologies makes it possible to timely diagnose illness in children in remote areas. The doctors of the regional children's hospital advise the pediatricians of the regional hospitals, prompting and helping them to accurately determine the diagnosis, focusing on clear documentation of all the symptoms of the disease in order to confirm or refute the Kawasaki-like syndrome.
Experts urged the medical community and parents to immediately seek help from the specialists of the regional children's clinic at the slightest suspicion of this dangerous disease. This can be done not only by phone, but also in circulation on the official website of IGODKB.
Kawasaki syndrome in children: symptoms and treatment
Coronavirus brings a new misfortune? What is Kawasaki syndrome that affects 9 children0005
Coronavirus brings a new scourge? What is Kawasaki syndrome that affects children
Experienced pediatricians say that a complication in the form of Kawasaki syndrome develops extremely rarely in children. The only antidote for such a disease is not... 08/11/2020, Sputnik Kazakhstan
/html/head/meta[@name='og:title']/@content
/html/head/meta[@name='og:description']/@content 9". In the people, such symptoms are called Kawasaki syndrome.
Sputnik Kazakhstan correspondent asked experienced pediatricians about how dangerous this complication is and how children can be protected.
What is Kawasaki syndrome
Kawasaki Syndrome - a complication of coronavirus The disease got its name because of similar symptoms to the rare Kawasaki disease
Kasawaki syndrome began to be noticed in children two to three weeks after suffering COVID-19.
According to the chief pediatrician of Kazakhstan, chairman of the board of the scientific center of pediatrics and pediatric surgery Riza Boranbayeva, the main difference between Kawasaki disease and Kawasaki syndrome is the age of patients.
The first Russian vaccine against coronavirus is named "Sputnik V"
A rare disease - Kawasaki disease - was first described in the medical literature in 1967 by Japanese pediatrician Tomisaku Kawasaki. For more than 50 years, this disease has occurred exclusively in children from birth to eight years of age. Kawasaki syndrome, which now affects children around the world, is also possible in those growing up to 20 years old.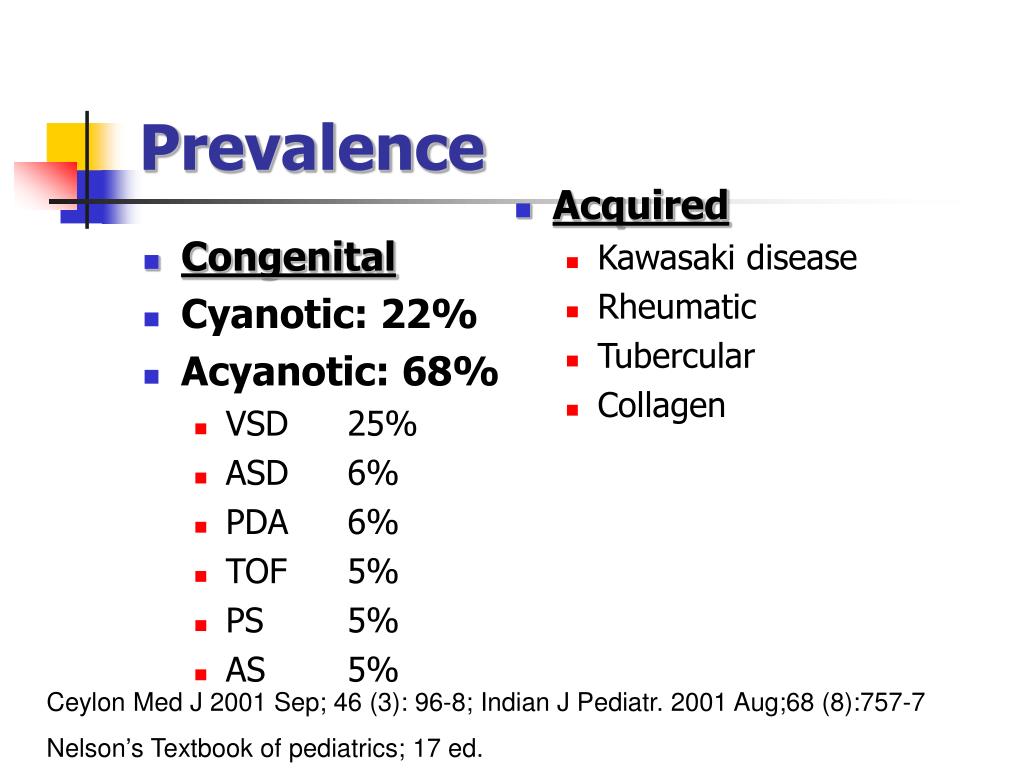
"A maximum of five children are diagnosed with Kawasaki disease every year in Kazakhstan. There are years when only one child could get this rare disease. Kawasaki disease develops when exposed to various viruses. There is also a description that the disease manifests itself in children with a genetic predisposition" - said the chief pediatrician of Kazakhstan.
Kawasaki syndrome was first mentioned in April of this year at the height of the coronavirus pandemic. For the first time, a description of the complication of coronavirus in children, which manifested itself in the form of Kawasaki syndrome, appeared in England and the USA. The appearance of the syndrome is typical for countries where there are a large number of people who have had coronavirus.
"We have studied all international publications. This is a very rare complication. Of course, parents should be alert about the condition of their children. There are now 10 cases of Kawasaki syndrome in Italy, 53 cases in New York and eight cases in London. These are the numbers testify that such a complication after suffering COVID-19 occurs extremely rarely," said Riza Boranbayeva.
These are the numbers testify that such a complication after suffering COVID-19 occurs extremely rarely," said Riza Boranbayeva.
Dangerous Kawasaki syndrome detected in children in Nur-Sultan, Almaty and Petropavlovsk
Family doctor, member of the American Association of Family Physicians (AAFP) Dmitry Kireev also notes that Kawasaki syndrome along with COVID-19 is not fully understood. Doctors do not yet have an answer to the question of why it occurs.
At the same time, the doctor notes that any inflammation can lead to complications in a child. For example, pneumonia can progress to sepsis, chickenpox to encephalitis, and infectious mononucleosis causes the spleen to enlarge and, in rare cases, rupture. But such complications are extremely rare, as is the Kawasaki-like syndrome after the coronavirus.
Kireev said that vascular lesion is a sign of Kawasaki disease itself, but in children with the same name syndrome, there are practically no problems with blood vessels.
Symptoms of Kawasaki syndrome
Kawasaki-like syndrome in children and adolescents develops two to three weeks after the coronavirus. First of all, the child's body temperature rises to 38 or above degrees and lasts for several days. Also, the child may develop cough and shortness of breath, as well as a rash on the legs, arms and body, conjunctivitis. Another characteristic symptom for a rare syndrome is redness of the tongue, swelling of the palms and feet, severe abdominal pain, vomiting and diarrhea.
What to do when such symptoms appear in children and adolescents
Experienced doctors are sure that when any symptoms appear in a child, the first thing a parent should not do is panic and demand that doctors be hospitalized in the infectious diseases department.
"Many people are now in a panic, children are hospitalized with a mild form of coronavirus or asymptomatic. They are sent to infectious disease hospitals, although children most often do not need hospitalization with coronavirus.If the child eats on his own, goes to the toilet, there are no signs of suffocation or rash, then he does not need to be taken to the infectious diseases hospital with a cough and fever," Dmitry Kireev notes.
The only way to keep your child safe from Kawasaki syndrome is to avoid contracting the coronavirus. For this, traditional preventive measures work in the form of frequent airing of the room, frequent washing of hands, wearing masks in public places, the right level of humidity in the house, good nutrition and drink, as well as the minimum number of child contacts during a pandemic. If a child is infected with coronavirus and the illness is mild, the child must be placed in home quarantine, but not taken to the hospital.
Infected with COVID-19, but no symptoms: what to do
Hospitalization, according to Riza Boranbayeva, is required only if the child's condition worsens, a rash appears on the body and signs of suffocation. If these symptoms appear, you should immediately contact your local doctor and call an ambulance.