How do i know if my baby is allergic to formula
The Signs of Formula Intolerance and What to Do About It
When breastfeeding your baby is not an option for you, mothers can often rely on formula to keep their babies adequately fed, hydrated, developing, and growing both naturally and nutritionally.
Yet, for an estimated 2 to 15 percent of babies, formula intolerance can make feeding time difficult – at least until the causes are identified and treated.
Not to be confused with an allergy (i.e., a milk protein allergy, which is rare in infants), formula intolerance means that your baby has a sensitivity to an ingredient in the formula you’re feeding her. This can lead to irritation within your baby’s digestive system. The condition isn’t life-threatening, but it can cause dehydration and slow weight gain and growth.
As raising a newborn can be a confusing and stressful time for parents, our team at Rainbow Pediatrics wishes to clear any confusion you might have regarding formula intolerance. This includes knowing the signs that your baby may be experiencing the condition, when she or he is likely not experiencing intolerance to formula, and when it’s crucial to bring your baby in for a thorough checkup.
What are the Signs of Formula Intolerance?
It’s been estimated that up to half of all formula-fed babies have their formulas switched up by parents within the first few months of birth. The reason? Parents often mistake common infant responses to feedings with formula intolerance in an attempt to proactively protect their babies.
Parents should be aware that as babies’ digestive systems develop, gassiness, crying, spitting up, and general fussiness are perfectly normal following feedings. These issues typically resolve within the first few months of life, yet continually changing and experimenting with your baby’s formula type can exacerbate the problem.
So, how are you supposed to know if your baby’s dealing with bona fide formula intolerance? Signs to watch for include:
- Diarrhea
- Vomiting
- Blood or mucus in your baby’s stool
- The baby often pulls her legs up toward her belly because of pain
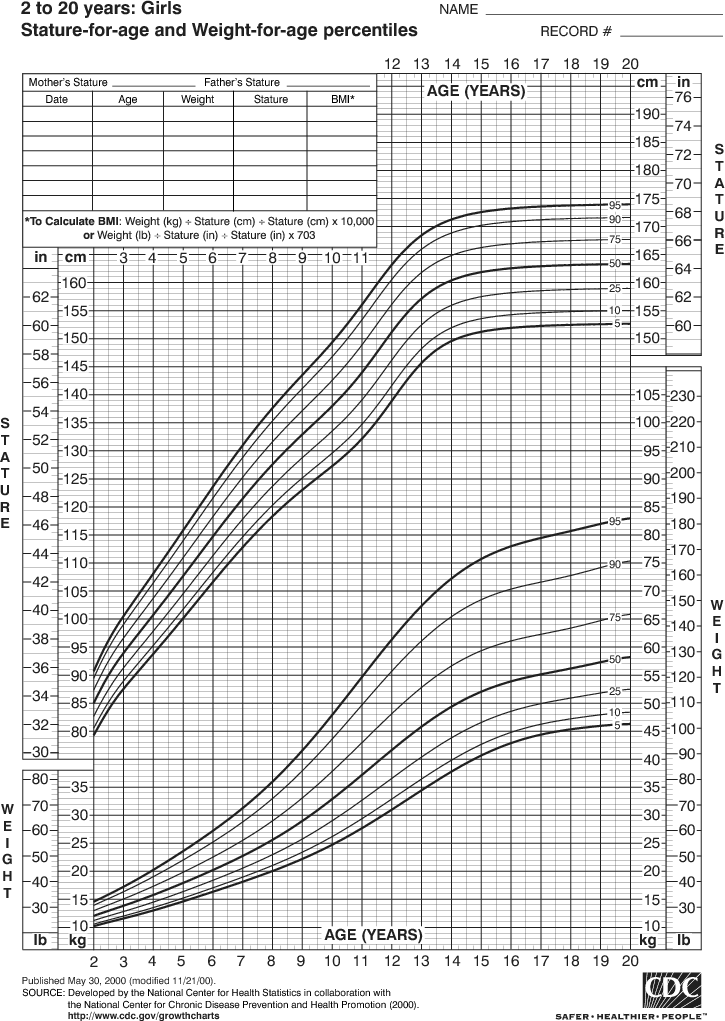
- Difficulty with weight gain or noticeable weight loss
- Constant crying and signs of discomfort
If you find your baby is regularly experiencing one or more of these issues, we recommend you bring him or her to Rainbow Pediatrics for an examination.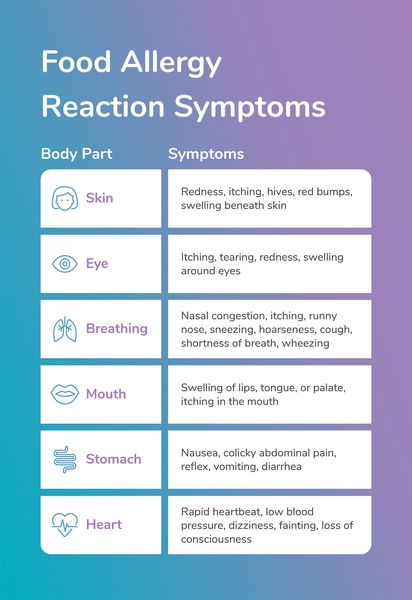 Be prepared to answer questions about the formula(s) you’ve been using and the specific symptoms your baby’s been having.
Be prepared to answer questions about the formula(s) you’ve been using and the specific symptoms your baby’s been having.
During the checkup, we may also take a stool sample to test for a variety of possible health problems, and we may perform tests to see if he or she is experiencing an allergic reaction from the formula.
What if My Baby Has Formula Intolerance?
If we ultimately determine that your baby is suffering from formula intolerance, often, simply changing the baby’s formula will resolve the issue.
If your baby, for instance, is reacting negatively to the iron-fortified formulas made from cow’s milk, which the American Academy of Pediatrics recommends, switching to a formula that uses soy or rice proteins may be beneficial. Formulas made with proteins that have already been broken down (called hydrolyzed formula) are also available and much easier on developing digestive systems.
Along with the formula issue, however, your baby may also require treatment for a health problem caused by the intolerance, such as dehydration or a loss of weight. So, it’s essential that even if you feel 100 percent certain your baby is dealing with formula intolerance, you still consult your pediatrician regarding dietary changes and treatment options.
So, it’s essential that even if you feel 100 percent certain your baby is dealing with formula intolerance, you still consult your pediatrician regarding dietary changes and treatment options.
If you feel your baby may be suffering from formula intolerance, please contact our Rainbow Pediatrics team today to schedule a checkup in one of our Fayetteville-area clinics. Call us at (910) 486-5437.
Signs of a baby formula allergy
If your baby frequently vomits or has diarrhea after drinking formula, they may be allergic to the cow's milk protein found in most formulas.
Formula allergies are typically caused by a milk allergy. A milk allergy is an atypical immune response in which the body reacts to the protein in milk as though it's a foreign invader that needs to be fought off.
Milk allergy is the most common food allergy in children. In fact, 2 to 3 percent of kids under age 3 show symptoms of an allergy. Just because your baby has signs of a milk allergy, though, doesn't necessarily mean they're allergic to milk – it could be an intolerance or sensitivity, which often causes the same gastrointestinal issues.
If you think your baby might be allergic to the formula you're giving them, bring it up with your pediatrician. They can help pinpoint what's causing your baby's discomfort.
A milk allergy or intolerance can be hard to manage, but the good news is most babies outgrow it by about 18 months to 2 years old.
Signs of an allergic reaction to formula
It's not surprising that some of the most common signs of an allergic reaction to formula are gastrointestinal, including:
- Vomiting
- Diarrhea
- Blood or mucus in the stool
- Unusually hard or excessively loose, watery, and foul-smelling poop
- Abdominal pain
Frequent spit up and excessive gassiness may also be signs of a milk allergy.
Not all signs of a formula allergy are gastrointestinal, though. Other signs of an allergy include:
- Itchy, watery, or swollen eyes
- Chronic nasal stuffiness
- Runny nose
- Cough
Your child may also develop itchy raised bumps on the skin known as hives.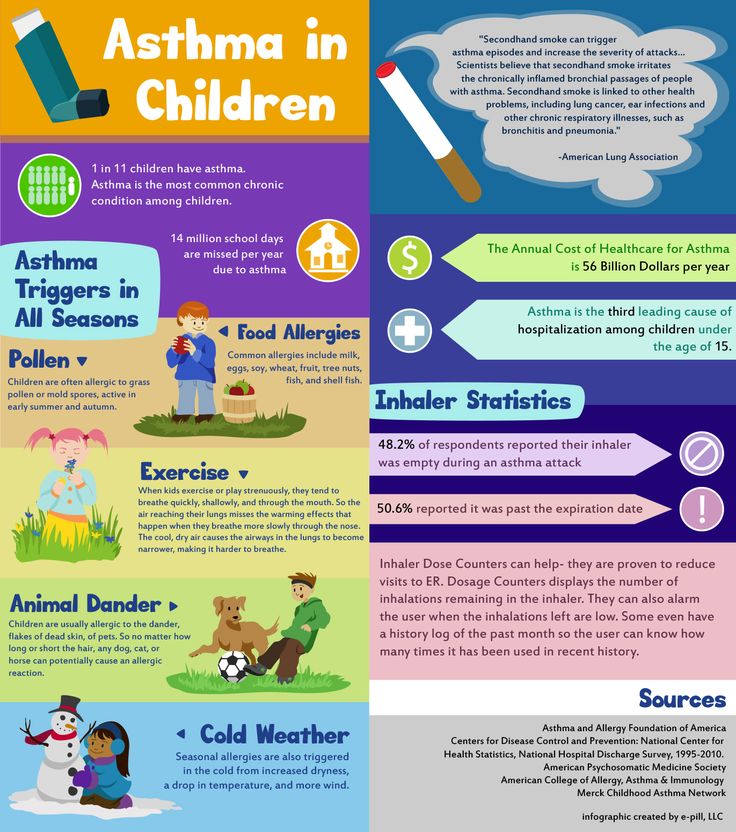 This is a type of skin rash that often occurs as a result of an allergic reaction. Hives can appear anywhere on the body and may look like tiny spots, blotches or large bumps.
This is a type of skin rash that often occurs as a result of an allergic reaction. Hives can appear anywhere on the body and may look like tiny spots, blotches or large bumps.
Another common rash that may appear with a formula allergy is known as eczema (atopic dermatitis) and can cause red, itchy or dry skin. Eczema tends to show up on the cheeks and scalp in babies but can appear anywhere on the body.
If you notice that your baby is continually fussy or crying and has obvious signs of discomfort shortly after you've started feeding, talk to your baby's doctor. Babies with milk allergies can show symptoms anywhere from days to weeks after first drinking cow's milk-based formula.
In some cases, a severe food allergy may cause a life-threatening reaction called anaphylaxis. If your baby has any of the following symptoms, call 911 or go to an emergency room immediately:
- Turning blue
- Wheezing
- Trouble breathing
- Facial swelling (including the lips or tongue)
It can be difficult to tell the difference between a milk allergy and lactose intolerance, since both conditions can cause uncomfortable gastrointestinal symptoms. If you have any concerns at all, talk to your baby's pediatrician. They can help figure out whether your baby has a milk allergy, lactose intolerance, or some other issue.
If you have any concerns at all, talk to your baby's pediatrician. They can help figure out whether your baby has a milk allergy, lactose intolerance, or some other issue.
Lactose intolerance is primarily a digestive issue in which the body doesn't produce enough of the enzyme lactase to properly digest the lactose in milk. Lactose intolerance can cause diarrhea, bloating, and gas in infants, but it's usually not dangerous. It's more common in adults than in children: If your child does have this condition, they likely won't start showing signs until they're at least 3 years old.
What to do if your baby has a formula allergy
First, check with your child's doctor to make sure that something else isn't causing the reaction. Once they rule out other possibilities, they may recommend a hypoallergenic (hydrolyzed) formula or an amino acid-based formula that's processed to avoid allergic reactions.
Your doctor most likely won't recommend a soy formula – soy is also a highly allergenic food, so if your baby is allergic to milk, they may also be allergic to soy. In fact, about 8 to 14 percent of babies with a cow's milk allergy will also have a reaction to soy. Ask your baby's doctor before switching to a soy formula.
In fact, about 8 to 14 percent of babies with a cow's milk allergy will also have a reaction to soy. Ask your baby's doctor before switching to a soy formula.
Your baby's doctor may also recommend keeping epinephrine auto-injectors on hand for your baby in case they accidentally have a milk product and have a severe reaction to it.
advertisement | page continues below
how it manifests itself, what it looks like, what to do, how long it takes for a newborn to be allergic to formula
We deal with the signs of intolerance to baby food and answer the question of what to do if the baby has an allergy to infant formula.
Nutrition for babies in the first year of life if breastfeeding is not possible should be prescribed by a pediatrician. He will definitely ask about the presence of allergies in parents and close relatives, ask about how the pregnancy went, did the mother take antibiotics, does the mother have bad habits. These are all risk factors for food allergies in babies.
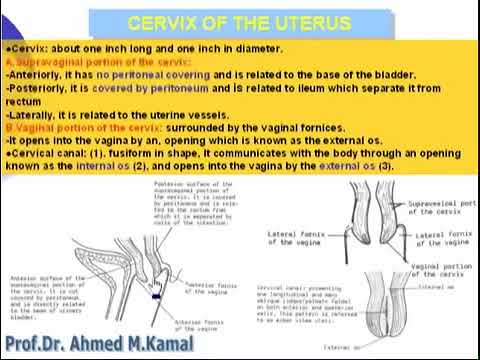
How infants are allergic to formula
The reaction to an allergen manifests itself through different body systems. Here are the symptoms of a food allergy:
- On the skin : redness that starts on the face and spreads throughout the body, small blisters, peeling
- From the digestive system : regurgitation fountain, loose stools, especially green, constipation, bloating, colic
- From the side of the respiratory system : shortness of breath, cough, wheezing
How long does it take to become allergic to the mixture
How quickly the disease will make itself felt depends on the characteristics of the child's health. In some babies, the first signs of allergies occur immediately after feeding. In others, the allergen will manifest itself only after a few days, when it accumulates in the body. In any case, you should immediately contact a specialist who will diagnose and prescribe adequate treatment.
Allergy to hypoallergenic formula
Hydrolyzed mixtures are called hypoallergenic - those where the milk protein is split into amino acids and peptides, which are easily absorbed by the body and in most cases do not cause an undesirable reaction. They are prescribed in cases of severe allergies. They are bitter, and babies are reluctant to eat them.
However, an undesirable reaction can also occur on a hypoallergenic mixture. That is why only a pediatrician should recommend the mixture and select treatment in case of an allergy.
Why are babies allergic to formula?
The reasons are different. A doctor and tests will help to deal with them.
The most common of the reasons:
- temporary or congenital lactase deficiency. The tests prescribed by the pediatrician will help to establish this reason. And treatment can be a temporary or permanent transition to a lactose-free mixture, such as soy. How to recognize lactase deficiency, read the article of our pediatrician.
- allergy to animal protein - casein. After passing the analysis, the doctor will recommend replacing the mixture with soy or hydrolyzed. Read more about lactase deficiency and cow protein allergy in our article.
- incorrect transition to artificial feeding or a new mixture. Learn how to change the mixture so as not to harm the baby's body.
- rotavirus infection. This is a temporary, but rather acute condition, during which the child needs special nutrition. Learn more about nutrition during rotavirus.
- excess food. This is the most common cause of allergic dermatitis in artificial babies who cannot regulate the amount of formula they eat. Why this happens, find out from our material.
- formula is not suitable for your baby. Children prone to allergies may react to the composition of improved mixtures enriched with vitamins and trace elements. How to understand what exactly caused the allergy? It is necessary to pass tests and follow the advice of a pediatrician to switch to a suitable mixture.
What to do
Regardless of whether treatment is required, a reduction in the volume of the mixture eaten or a transition to a new diet, the appointment should be made by a doctor.
Therefore, the first thing to do is to contact a pediatrician who will establish the cause, possibly offer to take tests and prescribe treatment.
Soy mixtures for allergies
Soy infant formula is prescribed for allergies to animal protein - casein. And in the absence of allergies to soy. Therefore, if the doctor has prescribed an analysis for an allergy to animal protein, ask if it is worth immediately taking an analysis for a reaction to soy protein.
Soy nutrition is an absolutely complete replacement for dairy nutrition until the transition to adult food.
Pay attention to soy mixtures Materna, made in Israel. They do not contain GMOs, salt and sugar and are suitable for newborns.
Fermented milk mixtures for allergies
Fermented milk mixtures belong to the category of medicinal. They are enriched with live bacteria that help digest food and absorb nutrients.
They are enriched with live bacteria that help digest food and absorb nutrients.
Only a pediatrician can recommend the use of a fermented milk mixture. As a rule, the baby is not completely transferred to such a diet, but several feedings a day are replaced by them. Do this for a limited period of time while bowel function is restored.
How long does an allergy last
With adequately selected treatment, you will notice an improvement in 5-7 days. Symptoms may persist for up to a month. The prognosis for your particular case can only be given by a pediatrician who knows the history of the baby.
Trust the treatment of your kids only to professionals and let your kids be healthy!
Get a free consultation
Allergy in a child: what should parents know?
Is your city Moscow?
- Pharmacies
- Catalog
- Discounts and promotions
- Loyalty program
- Jobs
- Help
- Rent
- Contacts
- COVID-19
September 6, 2019
With increased sensitivity of the immune system, the protective reaction of the body can be "turned on" even when in contact with environmental factors that are not dangerous for other people: plant pollen, animal hair, dust, food components, cosmetics, etc.
It is important to note that if at least one of the parents suffers from an allergy, there is a possibility that a predisposition to the disease can be passed on to the child. How to detect allergies in the early stages, what measures to take and how to avoid complications?
Symptoms of allergic reactions
- Skin rash or irritation. Manifested in the form of redness, itching, spots, peeling. Rashes from food or contact allergies often resemble insect bites or nettle stings.
- Complicated breathing. Runny nose, cough, sneezing - the most common allergic reaction to dust, pollen, animal hair. Allergens cause irritation of the nasal mucosa or bronchi.
- Conjunctivitis. Redness, itching, tearing of the eyes often occur upon contact with household chemicals, cosmetics, pollen, dust, wool.
- Difficulty in digestion.
 Abdominal pain, diarrhea, vomiting - a reaction to food allergens.
Abdominal pain, diarrhea, vomiting - a reaction to food allergens. - Anaphylactic shock. The most dangerous manifestation of an allergy. Shock can be caused by insect bites, drugs, and some foods (such as nuts). An allergic person has a sharp reddening of the skin, breathing becomes difficult and the heartbeat quickens. Possible loss of consciousness and convulsions. An ambulance must be called immediately!
Symptoms similar to allergies can hide various diseases, so professional diagnosis is indispensable. The presence of an allergy is confirmed by skin tests or a blood test. Do not delay your visit to the doctor in order to prescribe a course of treatment as soon as possible and avoid complications.
Preventive measures
To reduce the risk of allergic reactions, the child's diet and living environment should be closely monitored.
- If a nursing mother has any allergy symptoms, it is important to visit a doctor regularly and follow a diet.
 It is recommended to exclude from the diet food products that are a potential allergen, for example: milk, honey, chocolate, nuts, seafood, citrus fruits, cereals, as well as foods with flavors and flavor enhancers.
It is recommended to exclude from the diet food products that are a potential allergen, for example: milk, honey, chocolate, nuts, seafood, citrus fruits, cereals, as well as foods with flavors and flavor enhancers. - If breastfeeding is not possible, the choice of infant formula should be entrusted to a specialist.
- If the child has already been diagnosed with an allergy, limit contact with the allergen and eliminate potentially dangerous foods from the diet.
- Wet mop regularly, vacuum your furniture and prevent mold growth.
- Do not save on hygiene products for children and household chemicals. Choose products labeled "hypoallergenic".
- Get rid of unnecessary "accumulators" of dust: carpets, soft toys, heavy curtains.
- Replace synthetic bed linen with natural cotton. Pillows, mattress and blanket should be hypoallergenic.
- Keep the room at least 50% humidity.
- Do not smoke in front of a child!
- In case of seasonal allergy to pollen or tree lint, it is recommended to ventilate the room only after rain.