How common is anterior placenta
What It Means for Mom and Baby
It’s only natural to be concerned about every aspect of your pregnancy. After all, your top priority is to ensure the health of that sweet little one growing inside you. So if you’ve been told you have an anterior placenta, you’re likely wondering what that means and whether it can pose a threat to baby. Fortunately, you can rest assured that this scientific-sounding term simply means your placenta is positioned in front of baby. In general, it’s nothing to worry about. Still, it’s a good idea to educate yourself about the changes happening in your body. Ready to learn more about how an anterior placenta affects pregnancy and delivery? Here’s what you need to know.
In this article:
What is anterior placenta?
How an anterior placenta affects pregnancy
How an anterior placenta affects delivery
Anterior placenta risks
What Is Anterior Placenta?
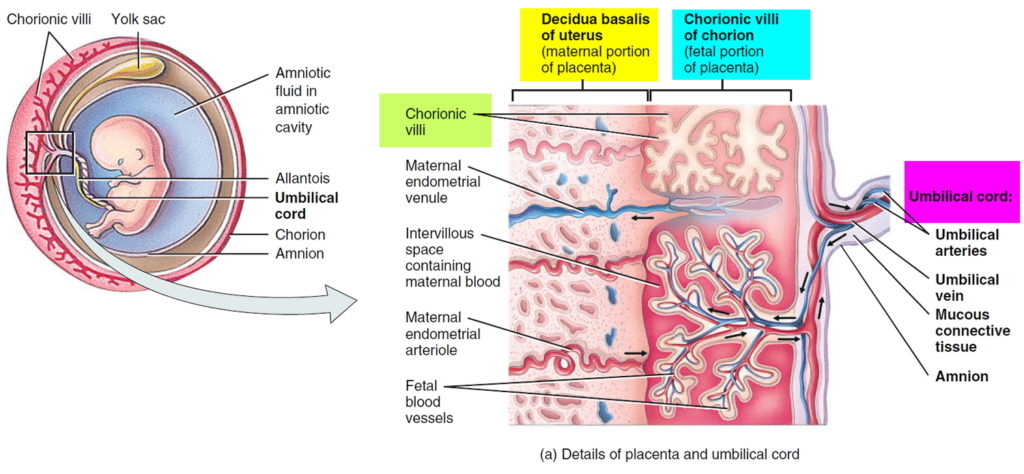
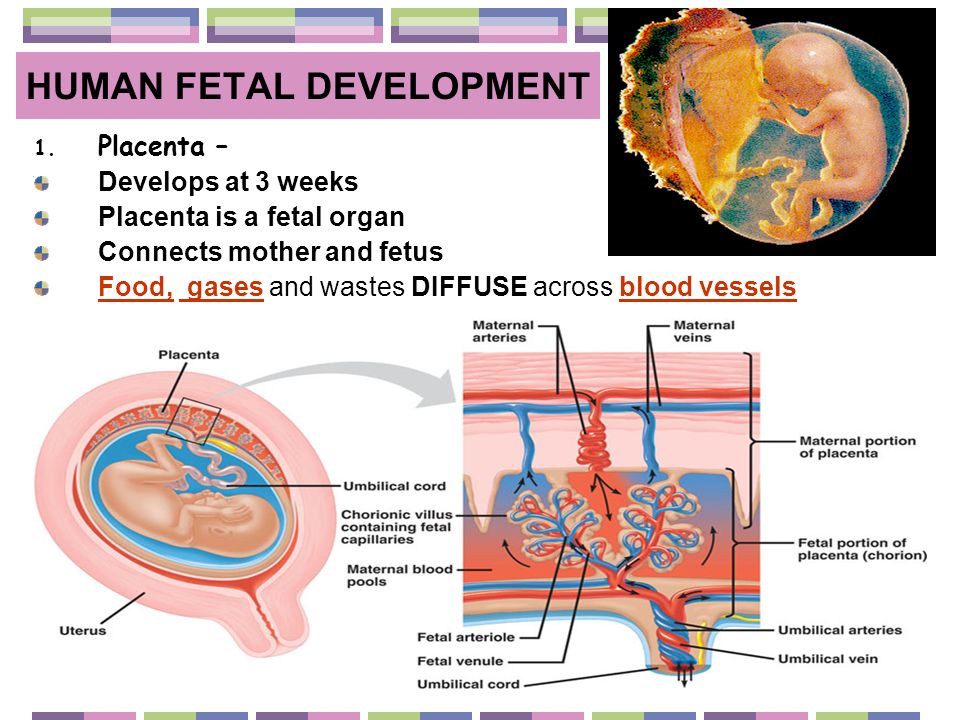
The placenta is an organ that develops in pregnancy. Along with the umbilical cord, it supplies oxygen, nutrients and hormones to baby, and helps remove waste. As baby grows during those first weeks of gestation, so will the placenta. It can develop anywhere along the uterus and may even move positions throughout pregnancy. When the placenta is located on the front side of the uterus, it’s referred to as an “anterior placenta.” This is completely normal, says Eric Strand, MD, an ob-gyn and associate professor at Washington University. “The placenta will typically grow either along the front (anterior) wall, back (posterior) wall, or top (fundal) of the uterus.”
How common is anterior placenta?
All of the previously mentioned placental positions are considered normal and safe. Still, if your placenta has been located in front of baby, you might be wondering: “How common is anterior placenta?” It’s estimated that 33 to 50 percent of pregnancies have an anterior placenta. The placenta can migrate, though, and this position is slightly less typical toward the end of pregnancy.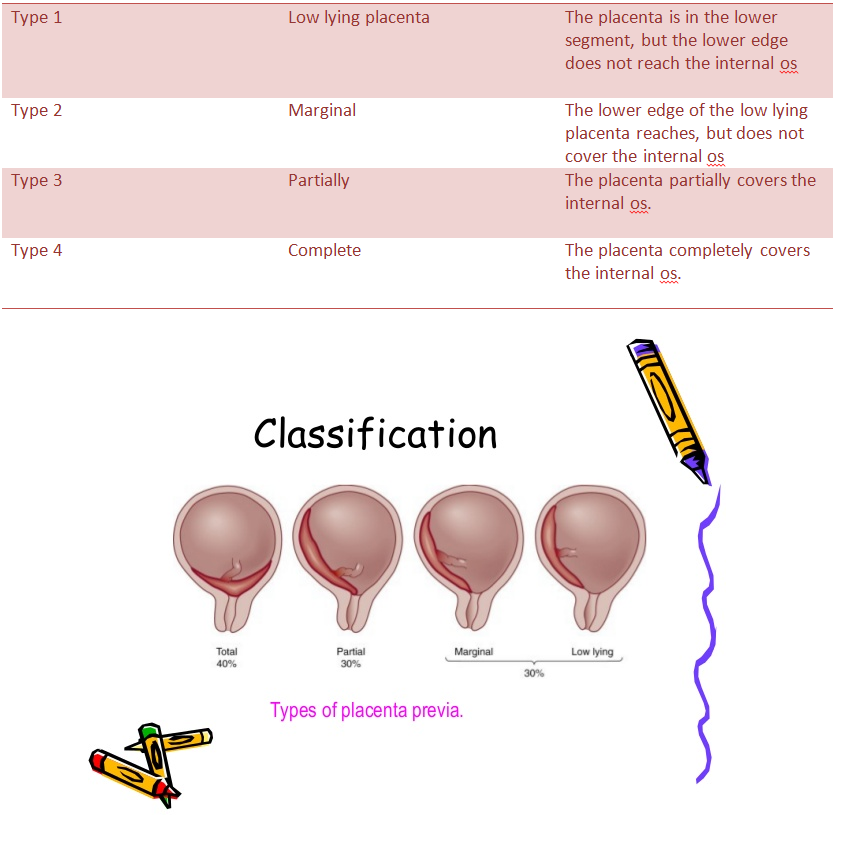
Anterior vs. posterior placenta
If you have an anterior placenta, the organ has developed on the front wall of the uterus closest to your stomach. On the other hand, a posterior placenta means that it’s growing on the wall of the uterus closest to your spine.
You may hear your OB mention a few other keywords in regards to your placental position: “Fundal” means toward the top of your uterus, and “lateral” means on a side. Most doctors will tell you that none of these positions are cause for concern. However, if they mention that you have a low-lying placenta or placenta previa, it may be a red flag (more on this later).
How is anterior placenta diagnosed?
Wondering how you’ll know if you have an anterior placenta? Ultrasound is the best way to diagnose the condition. At your mid-pregnancy ultrasound, your doctor or ultrasound tech will be able to see your placenta’s position, and may tell you that it’s growing in front of baby.
How Does Anterior Placenta Affect Your Pregnancy?
Having an anterior placenta is generally considered harmless, but if you’ve been pregnant before with a different placental position, there are some things that may seem slightly different this time around.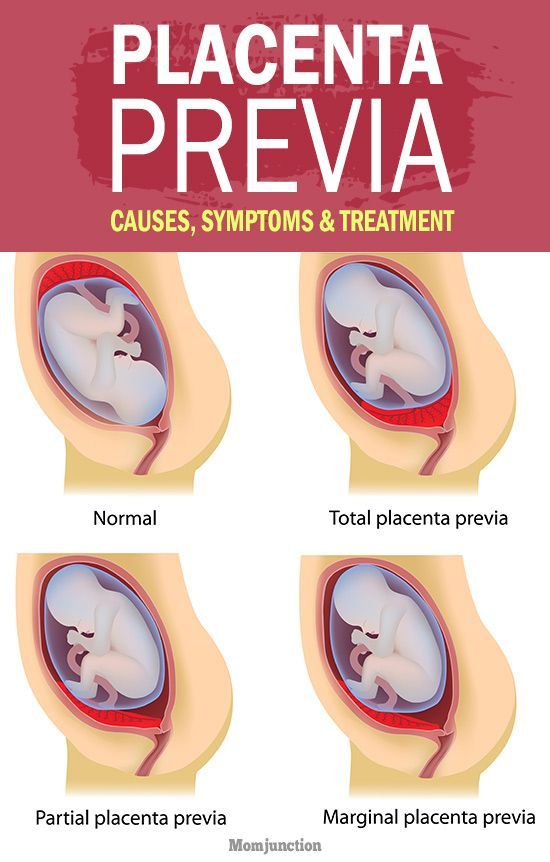
Many women wonder if this uterine position will affect how their baby bump looks—but no, there’s no specific anterior placenta belly shape, says Heather Bartos, MD, an ob-gyn and the medical director of Be. Women’s Health and Wellness in Frisco, Texas. You can’t identify an anterior placenta just by looking at a pregnant belly. (To confirm an anterior placenta, ultrasound is needed.) It’s true there’s an extra layer of cushioning when the placenta is located toward the front of the body, but it doesn’t increase the size of your bump.
So how does an anterior placenta actually impact pregnancy? Below, some things to keep in mind, plus a few minor anterior placenta risks to be aware of.
Feeling fetal movement
There’s nothing more exciting than feeling those first tiny kicks. But if you have an anterior placenta, you may have to wait a bit longer for this important milestone. What does baby movement feel like with anterior placenta? “It can be more difficult for a mother to initially feel the baby move with an anterior placenta,” says Strand.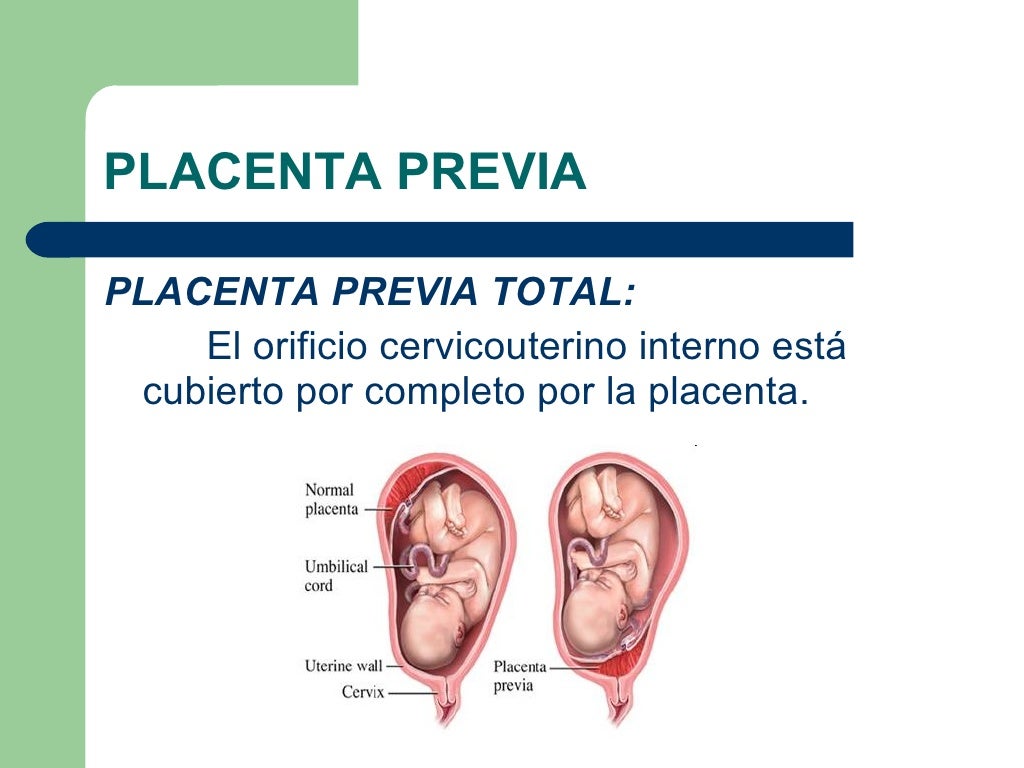 “Essentially, it’s an extra layer of cushioning between the baby and the mother.”
“Essentially, it’s an extra layer of cushioning between the baby and the mother.”
While most moms-to-be may start feeling baby kick between 18 and 20 weeks, you may not notice it until closer to 20 to 22 weeks, especially if you’re not familiar with the way those early flutters feel. Bartos says that an anterior placenta essentially has a muffling effect. She had an anterior placenta in her own pregnancies, and says that the position made it more difficult for her partner to feel kicks or movement from the outside too.
Still, if you’re having trouble detecting movement and feeling concerned, trust your gut and give your doctor a call. There’s no harm in getting checked.
Detecting fetal heartbeat
Typically at every visit from 10 weeks and beyond, your doctor will assess baby’s heart rate via fetal doppler or ultrasound. As the weeks pass, it’ll get easier for your doctor to find the heartbeat. But if you have an anterior placenta, you may hear more of a muffled “whooshing” sound, says Bartos.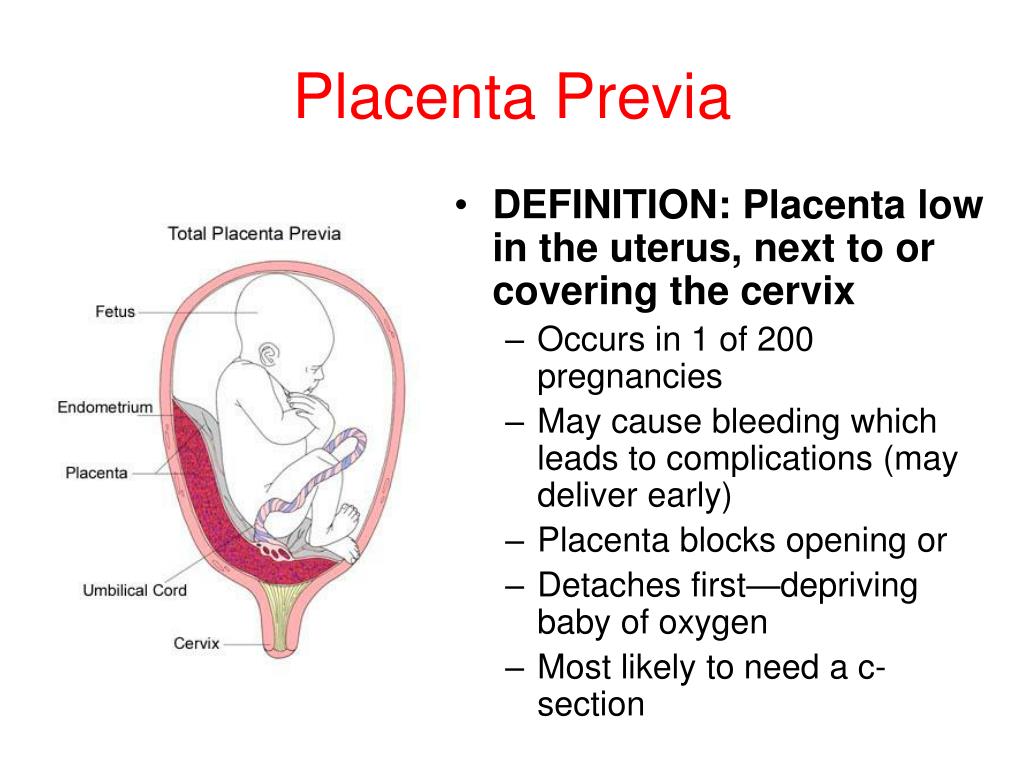
Getting diagnostic tests
Amniocentesis is a procedure that’s performed to detect abnormalities in the fetus. However, it may be a bit more difficult for your doctor to perform this test if your placenta is anterior; that’s because the needle used to draw amniotic fluid out of the gestational sac will need to work around the placenta. Fortunately, with today’s advanced ultrasound equipment, this is considered little more than a slight inconvenience.
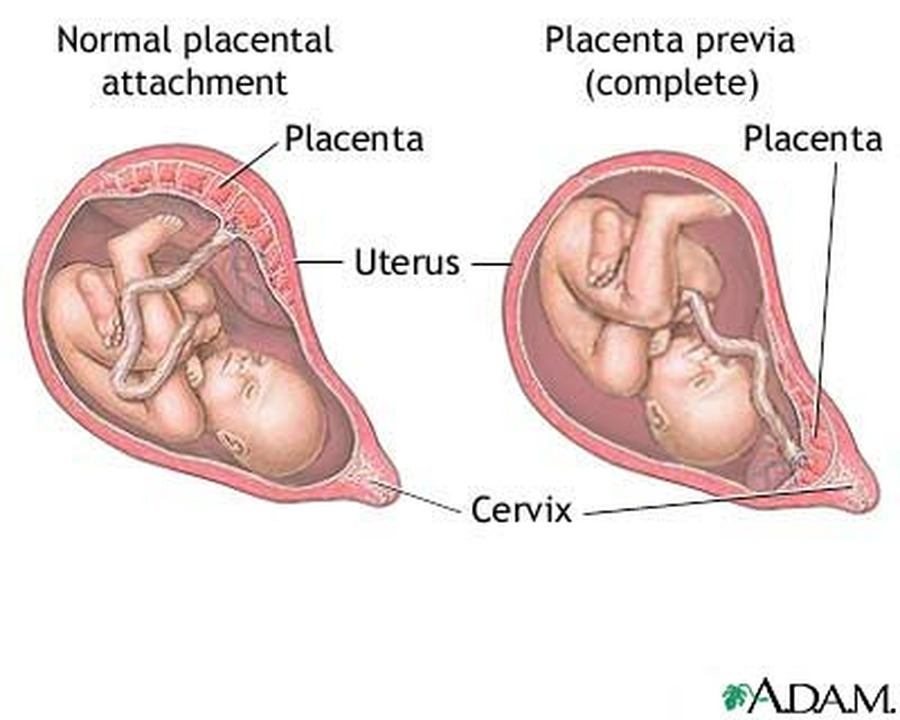
Anterior placenta previa
Your doctor won’t be fazed by the anterior or posterior position of your placenta. However, they may be alerted if your placenta is in a low-lying position. This is known as placenta previa, a relatively rare condition that affects about 1 in 200 pregnancies.
Anterior placenta previa means that the placenta is positioned in front of the uterus but also covering all or part of the cervix. (It’s important to note that placenta previa can occur with a posterior placenta as well; it has nothing to do with the fact that your placenta is anterior.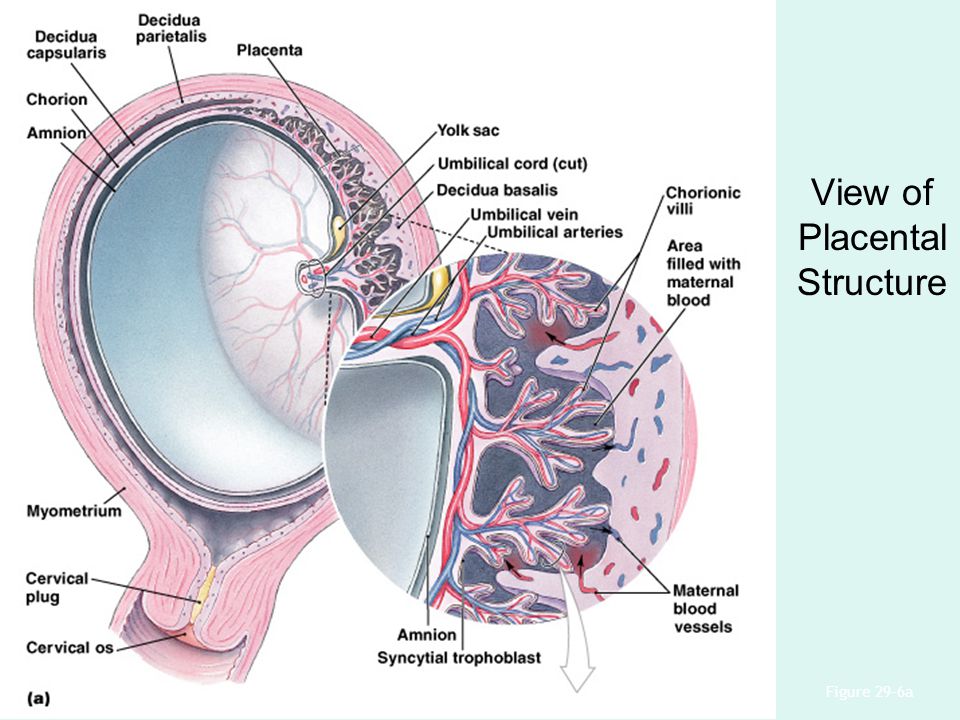 )
)
If you’re told you have anterior placenta previa, your doctor will likely take a “wait and watch” approach, since the condition often corrects itself as pregnancy progresses. “Throughout pregnancy, the placenta typically migrates away from the cervix—so while a low-lying placenta is pretty common at the time of the anatomy scan (5 to 10 percent of the time), it resolves itself about 95 percent of the time,” says Strand.
If it remains staunchly low as the weeks go by and your due date approaches, your doctor will likely discuss the potential need for a scheduled c-section to ensure your health and safety—and that of baby. Vaginal delivery with placenta previa can be dangerous and lead to hemorrhaging.
How Does Anterior Placenta Affect Delivery?
When it finally comes time to meet baby, your anterior placenta most likely won’t affect much on the big day. Strand says, “We do not currently think that an anterior placenta has any negative impact on pregnancy outcomes or route of delivery.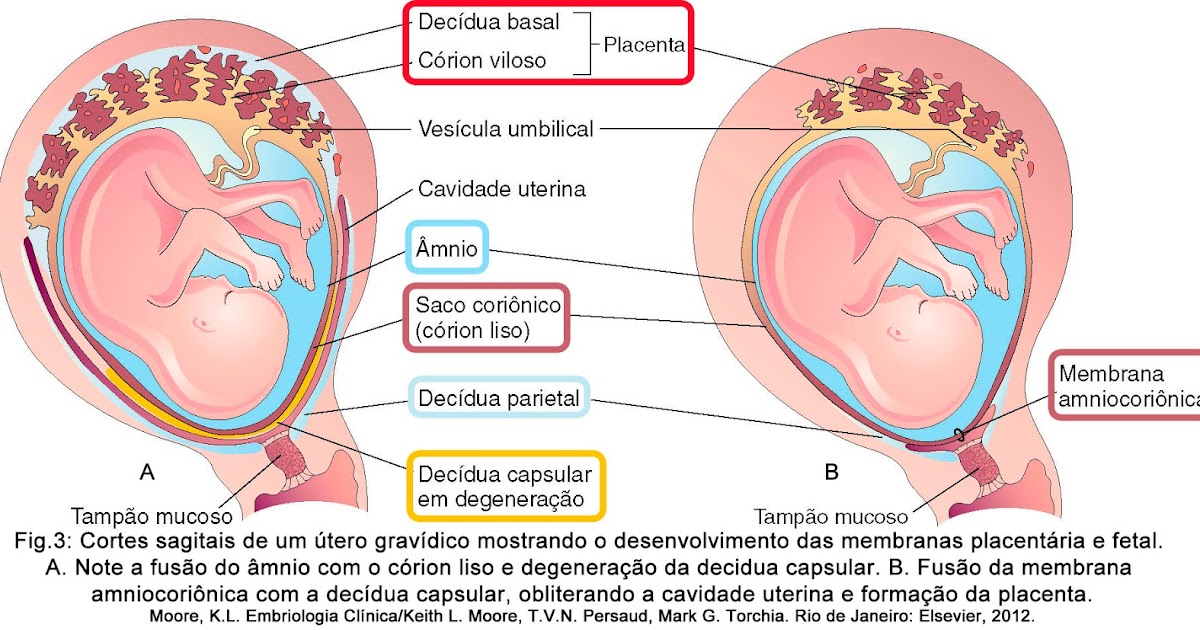 ”
”
Still, one small study indicated that an anterior placenta may increase the need for an induction, c-section or manual placenta removal. It’s worth noting that the researchers couldn’t find any clear reason for this correlation though, so more follow up is needed.
Anterior Placenta Risks
“I think the biggest risk of anterior placenta is that the mom gets used to not feeling the baby move as much, so if there’s an issue with the baby, she may not be able to tell as readily,” Bartos says. Despite this, anterior placenta moms don’t get nonstress tests or further testing, she adds.
As for other potential risks, a 2013 study indicated a slightly higher incidence of certain pregnancy complications, including:
- Pregnancy-induced hypertension
- Gestational diabetes
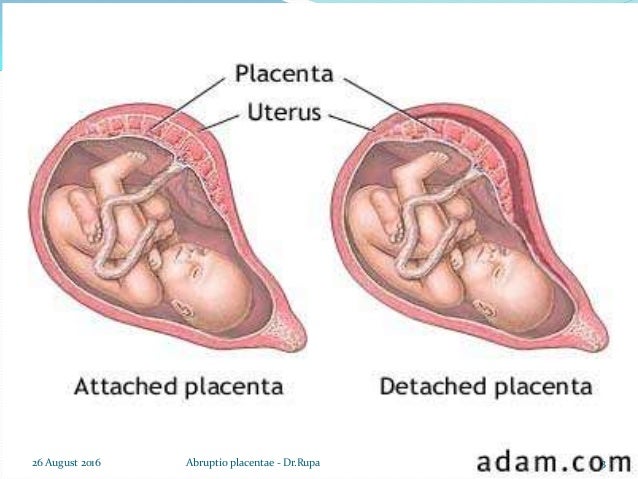
- Placental abruption
- Intrauterine growth restriction
While these supposed anterior placenta risks and complications may sound alarming, it’s important to realize that this research looked at just about 500 cases, and many more moms with anterior placentas have had healthy pregnancies and deliveries.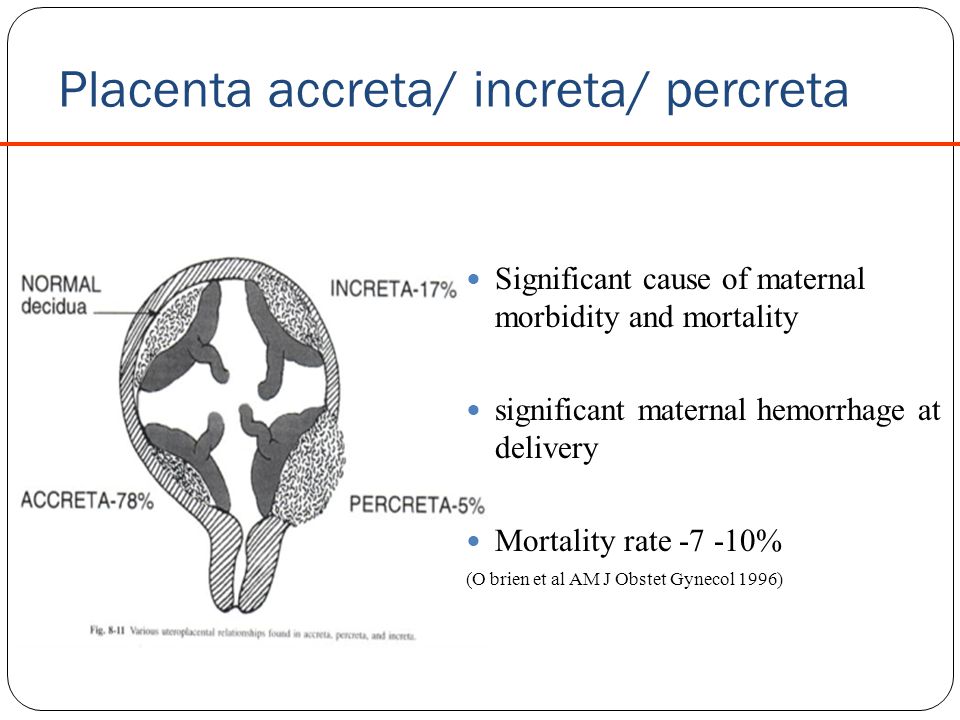 “Nearly one third of all women have an anterior placenta, so if there were major issues or risks, they would be very obvious by now,” Bartos says. The reassuring truth is that having an anterior placenta is considered fairly benign.
“Nearly one third of all women have an anterior placenta, so if there were major issues or risks, they would be very obvious by now,” Bartos says. The reassuring truth is that having an anterior placenta is considered fairly benign.
Now that you understand more about the position of your placenta, you can relax and focus on keeping yourself and baby healthy during your pregnancy. Most doctors would confidently tell you that anterior placenta risks are low. You may just have to wait a bit longer to feel those precious kicks and elbow jabs! Of course, if you have any concerns, talk to your doctor.
About the experts:
Heather Bartos, MD, is an ob-gyn and the medical director of Be. Women’s Health and Wellness in Frisco, Texas. A navy veteran, she spent 12 years serving the women and spouses of the armed forces in Washington, D.C… She earned her medical degree at The University of Texas at Houston.
Eric Strand, MD, is an ob-gyn and associate professor at Washington University. He received his medical degree at Johns Hopkins School of Medicine in Baltimore, Maryland.
He received his medical degree at Johns Hopkins School of Medicine in Baltimore, Maryland.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Placenta Accreta: What It Means for Mom and Baby
How to Ease Leg Cramps During Pregnancy
11 Warning Signs of Pregnancy You Should Never Ignore
Anterior Placenta: Should I Worry?
Anterior Placenta: Should I Worry?- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
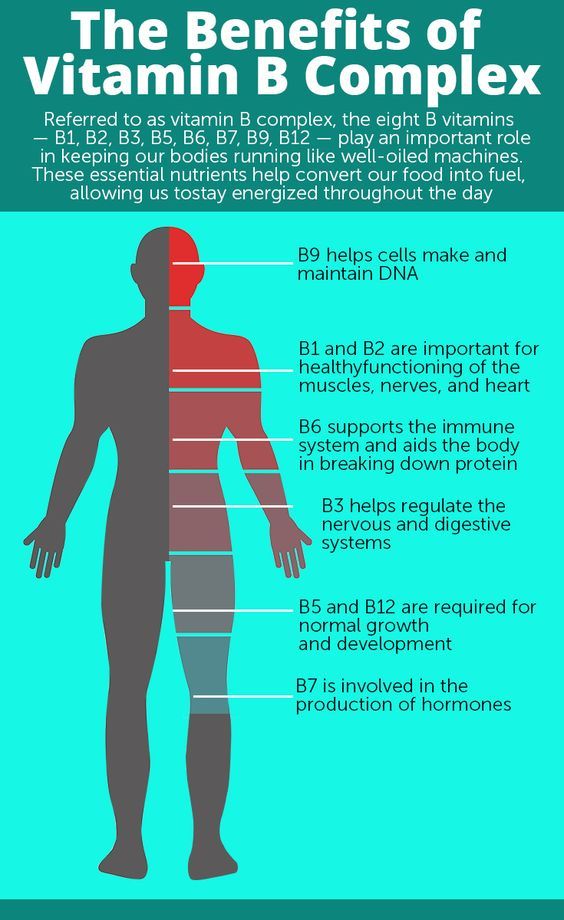
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Valinda Riggins Nwadike, MD, MPH — By Rachel Nall, MSN, CRNA — Updated on Nov 11, 2021
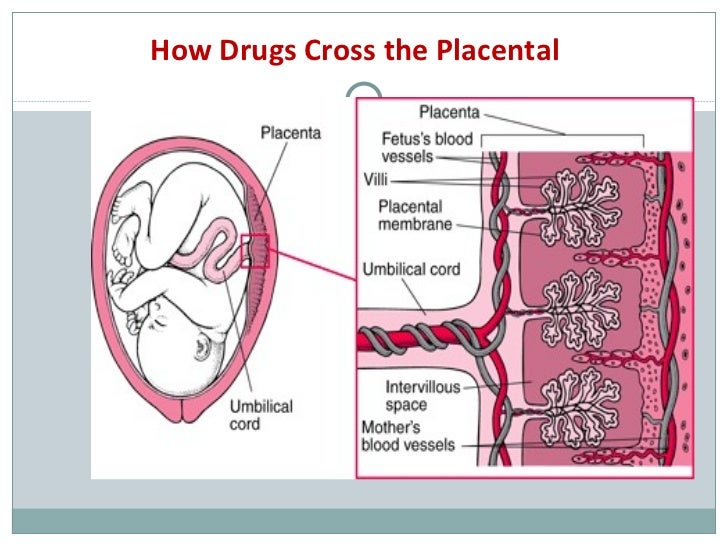
The placenta is a unique organ that’s only present during pregnancy. This disk- or pancake-shaped organ takes nutrients and oxygen from your body and transfers it to your baby. In return, the baby’s side will remove waste products thatgo back into your bloodstream to be eliminated.
This disk- or pancake-shaped organ takes nutrients and oxygen from your body and transfers it to your baby. In return, the baby’s side will remove waste products thatgo back into your bloodstream to be eliminated.
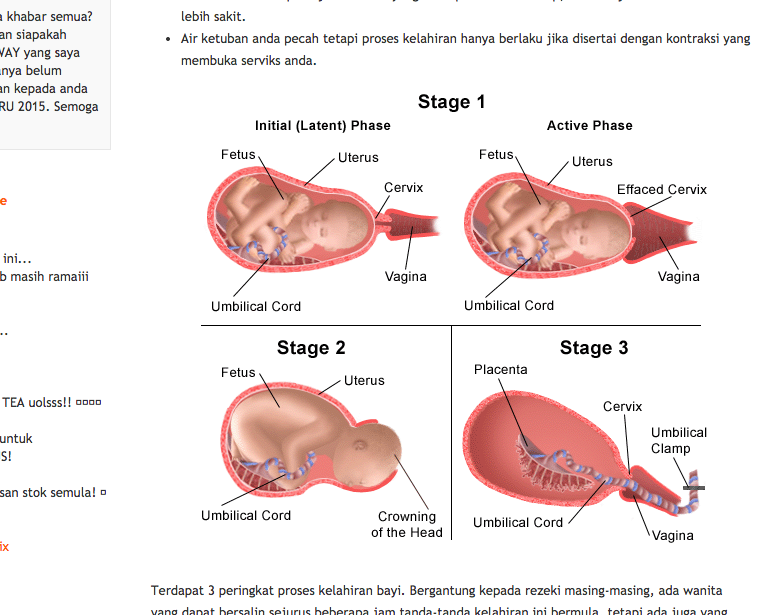
When you deliver your baby, you’ll also deliver the placenta. For the most part, the placenta’s positioning isn’t cause for concern. But there are some positions that are more common than others. The anterior position is a less common place for the placenta to attach.
The placenta can attach virtually anywhere in the uterus to nourish your baby. Usually the placenta positions itself at either the top or side of the uterus.
But it’s always possible that the placenta will attach to the front of the stomach, a position known as an anterior placenta. If the placenta attaches to the back of the uterus, near your spine, this is known as a posterior placenta.
Typically, your doctor will check the position of your placenta during your midpregnancy ultrasound, which should take place between 18 and 21 weeks of pregnancy.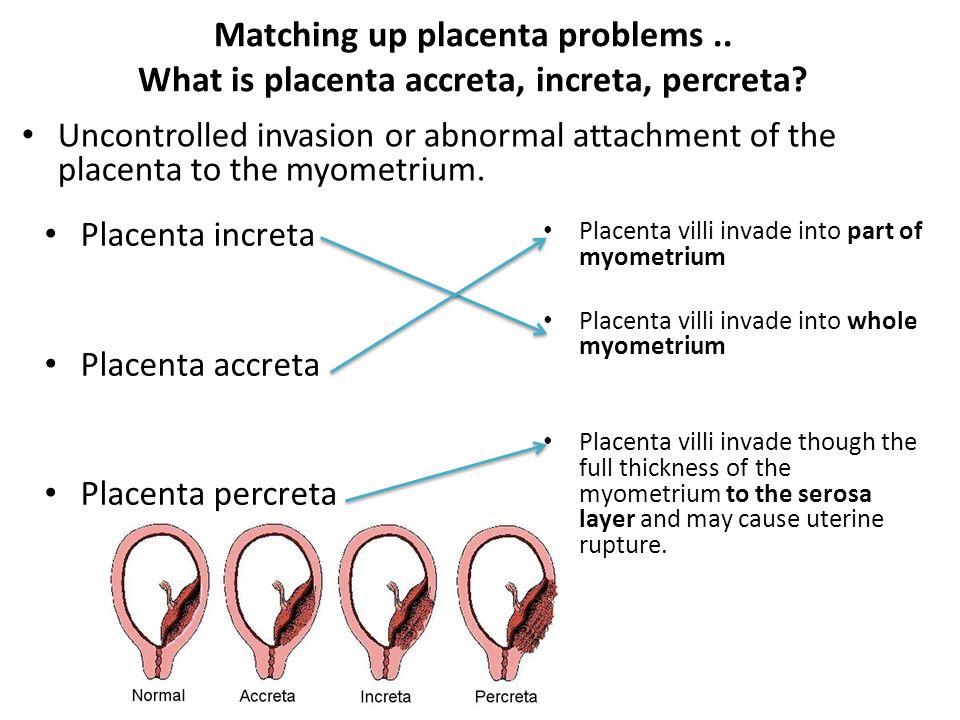
The anterior positioning of the placenta shouldn’t make a difference to your baby. It should continue to nourish your baby regardless of its positioning. But there are a few slight differences you may notice due to the placenta’s front positioning.
The placenta might create an extra space or cushion between your stomach and your baby, for example. You may feel kicks or punches later than in a typical pregnancy, because the placenta can act as a cushion.
Luckily these are minor inconveniences that shouldn’t impact your baby’s health.
An anterior placenta isn’t typically cause for concern. But there is a possibility that the anterior placenta could grow downward instead of upward. This means that your placenta grows toward your cervix.
This could possibly block the baby’s way on delivery day and cause bleeding. This condition is known as placenta previa. If the placenta blocks all or a portion of your cervix during labor, a cesarean delivery, commonly known as a C-section, is required.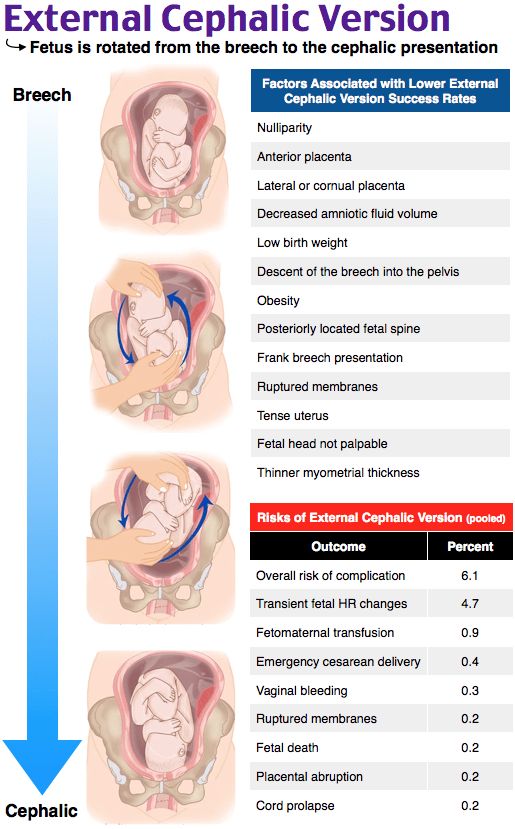
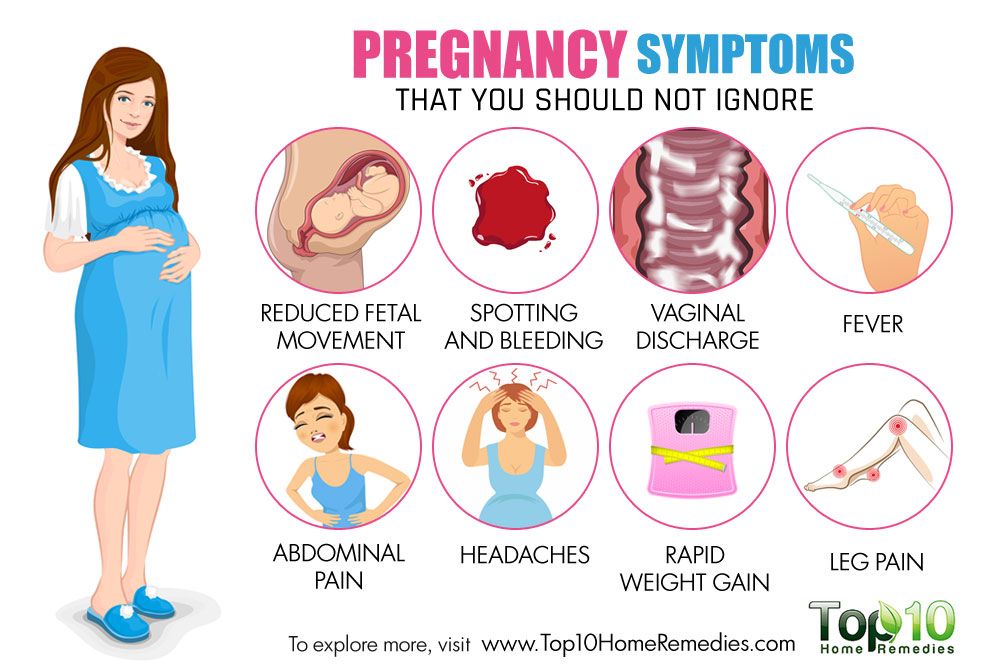
Although an anterior placenta isn’t usually a cause for concern, your doctor may prepare you for signs that could indicate a placenta problem during pregnancy.
Contact your doctor if you experience the following symptoms, which could indicate a placenta problem:
- abdominal pain
- fast uterine contractions
- severe back pains
- vaginal bleeding
If you have experienced a fall or other trauma to your stomach, such as a car accident, call your doctor. These injuries could potentially affect your placenta’s health and may require a doctor’s examination.
Your doctor will continue to monitor the placement of your baby as well as the placenta throughout your pregnancy. Getting regular prenatal care and managing any conditions that may arise throughout your pregnancy can help you deliver a healthy baby.
If you’re concerned about your anterior placenta, talk with your doctor, who can discuss any individual risks given your health history.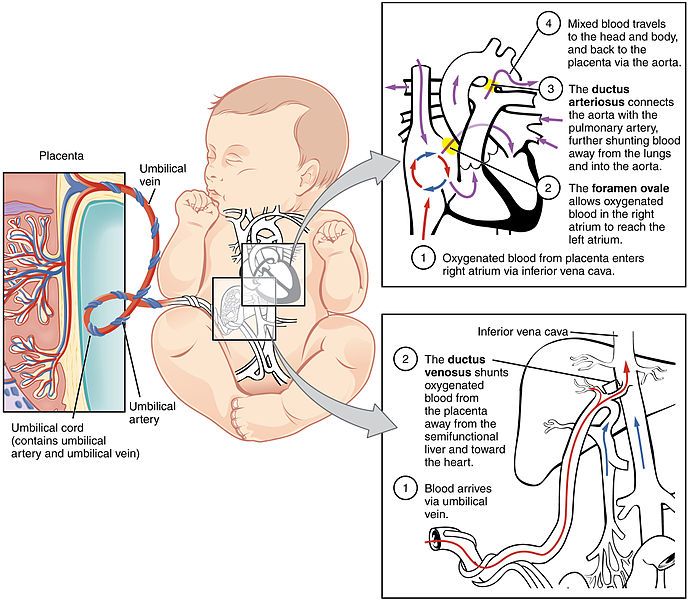 But for most people, an anterior placenta isn’t cause for concern.
But for most people, an anterior placenta isn’t cause for concern.
Last medically reviewed on November 11, 2021
- Parenthood
- Pregnancy
- 2nd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Anderson-Bagga FM, et al. (2021). Placenta previa.
ncbi.nlm.nih.gov/books/NBK539818/ - Placenta problems | Placenta 101. (n.d.).
ontariofetalcentre.ca/placenta-clinic/placenta-101/ - Zia S. (2013). Placental location and pregnancy outcome.
ncbi.nlm.nih.gov/pmc/articles/PMC3935544/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.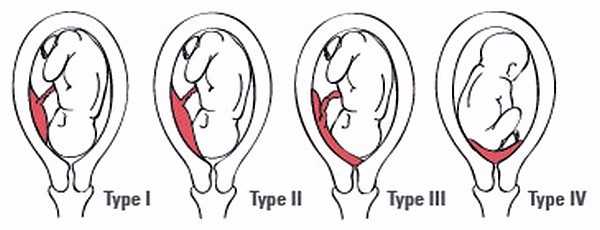
Current Version
Nov 11, 2021
Written By
Rachel Nall, MSN, CRNA
Edited By
John Bassham
Medically Reviewed By
Valinda Riggins Nwadike, MD, MPH
Copy Edited By
Sofia Santamarina
Jan 5, 2018
Written By
Rachel Nall, MSN, CRNA
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Valinda Riggins Nwadike, MD, MPH — By Rachel Nall, MSN, CRNA — Updated on Nov 11, 2021
related stories
Placenta Previa
Placental Insufficiency
Baby Flutters: What Does It Feel Like?
What Is Placental Abruption?
Is Eating Your Placenta Safe?
Read this next
Placenta Previa
Medically reviewed by Fernando Mariz, MD
Placenta previa is when the placenta covers the opening of the cervix during the last months of pregnancy.
 Find out about symptoms and treatment.
Find out about symptoms and treatment.READ MORE
Placental Insufficiency
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Placental insufficiency, also known as placental dysfunction or uteroplacental vascular insufficiency, is an uncommon but serious complication of…
READ MORE
Baby Flutters: What Does It Feel Like?
Medically reviewed by Michael Weber, MD
During pregnancy, those first flutters might not be that noticeable. Here’s what it actually feels like when your baby starts to move.
READ MORE
What Is Placental Abruption?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Placental abruption occurs during a pregnancy when the placenta detaches from the uterine wall too early.
 This can cause bleeding and complications…
This can cause bleeding and complications…READ MORE
Is Eating Your Placenta Safe?
Medically reviewed by Holly Ernst, PA-C
Placentophagia, or the practice of eating your placenta, has gained a lot of publicity as of late. But is eating your placenta safe? Some people think…
READ MORE
Pregnancy-Friendly Recipe: Herby Gruyère Frittata with Asparagus and Sweet Potatoes
Medically reviewed by Kathy W. Warwick, R.D., CDE
So easy and delicious. This frittata is high in protein and rich in essential nutrients your body needs to support a growing baby. Bonus: You can…
READ MORE
The Best Stretch Mark Creams and Belly Oils for Pregnancy in 2023
Stretch marks are easier to prevent than erase. If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.
READ MORE
Why Twins Don’t Have Identical Fingerprints
Medically reviewed by Alana Biggers, M.D., MPH
Identical twins are the same in so many ways, but does that include having the same fingerprints? There's conflicting information out there so we look…
READ MORE
Doula vs. Midwife: What’s the Difference?
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
What is the difference between a doula and a midwife? Do I need to choose? Read on to learn more about the similarities and differences.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
Makarov I.
 O. • Placenta previa
O. • Placenta previa RS80 ultrasound scanner
The benchmark of new standards! Unprecedented clarity, resolution, ultra-fast data processing, and a comprehensive suite of state-of-the-art ultrasound technologies to meet the most demanding diagnostic challenges.
In the normal course of pregnancy, the placenta is usually located in the fundus or body of the uterus, along the back wall, with the transition to the side walls, i.e. in those areas where the walls of the uterus are best supplied with blood. On the anterior wall, the placenta is located somewhat less frequently, since the anterior wall of the uterus undergoes significantly more changes than the posterior one. In addition, the location of the placenta on the back wall protects it from accidental injury. nine0007
Placenta previa is a pathology in which the placenta is located in the lower parts of the uterus along any wall, partially or completely blocking the area of the internal os. The incidence of placenta previa averages from 0.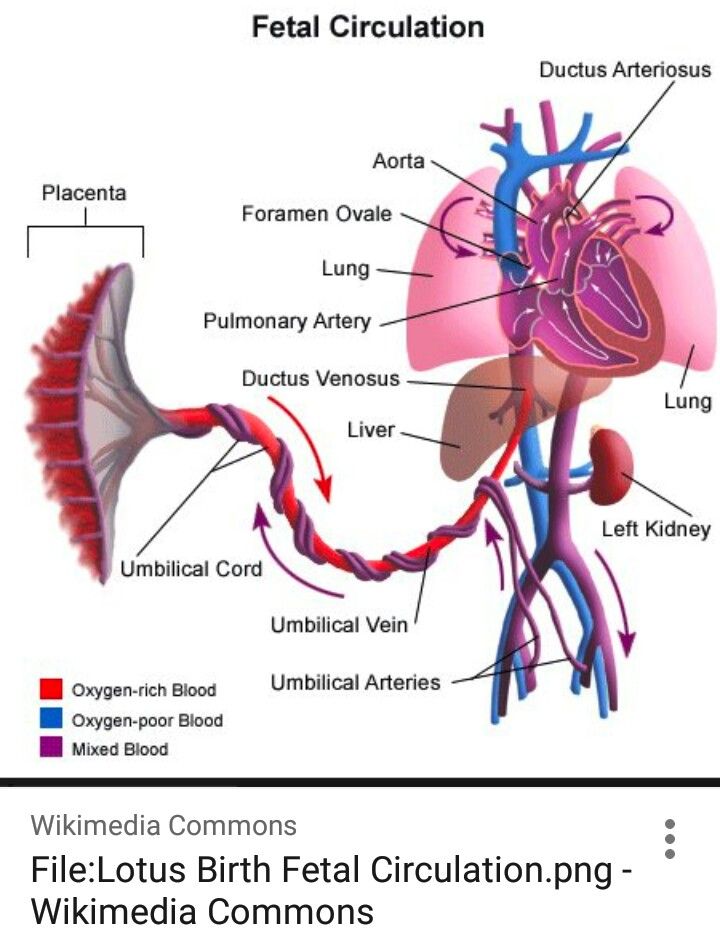 1% to 1% of the total number of births.
1% to 1% of the total number of births.
If the placenta only partially covers the area of the internal pharynx, then this is an incomplete presentation, which occurs with a frequency of 70-80% of the total number of presentations. If the placenta completely covers the area of the internal os, then this is a complete placenta previa. This option occurs with a frequency of 20-30%. nine0007
There is also a low location of the placenta, when its edge is at a lower level than it should be in the norm, but does not cover the area of the internal os.
Causes of low or low placenta
There are several reasons for low or low placenta. The most common causes are pathological changes in the inner layer of the uterus (endometrium) due to inflammation, surgical interventions (curettage, caesarean section, removal of myomatous nodes, etc.), multiple complicated births. In addition, violations of the attachment of the placenta can be caused by uterine fibroids, endometriosis, underdevelopment of the uterus, isthmicocervical insufficiency, inflammation of the cervix, multiple pregnancy.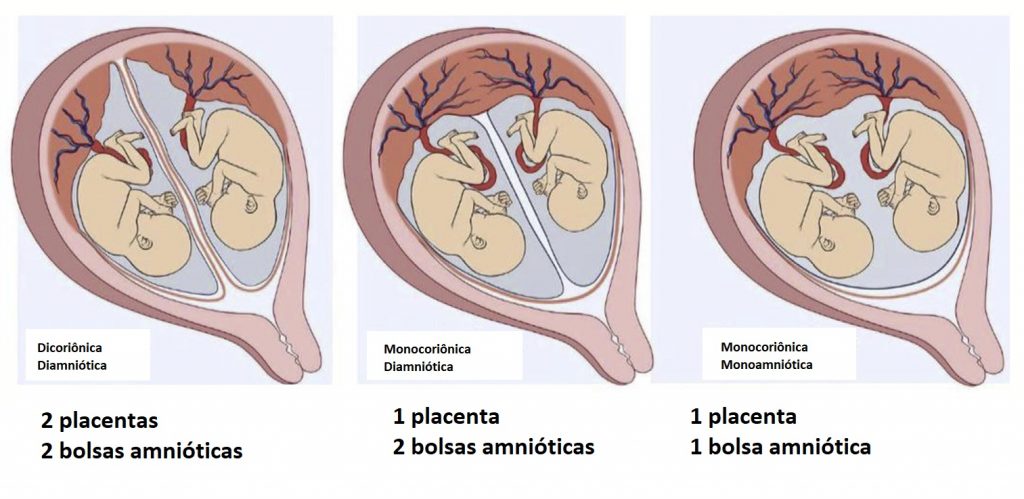 It should be noted that placenta previa is more common in re-pregnant women than in primiparas. Due to these factors, the fetal egg that enters the uterine cavity after fertilization cannot be implanted in the upper sections of the uterus in a timely manner, and this process is carried out only when the fetal egg has already descended into its lower sections. nine0007
It should be noted that placenta previa is more common in re-pregnant women than in primiparas. Due to these factors, the fetal egg that enters the uterine cavity after fertilization cannot be implanted in the upper sections of the uterus in a timely manner, and this process is carried out only when the fetal egg has already descended into its lower sections. nine0007
The most common manifestation in placenta previa is recurrent bleeding from the genital tract. Bleeding can occur during various periods of pregnancy, starting from its earliest terms. However, most often they are observed already in the second half of pregnancy due to the formation of the lower segment of the uterus. In the last weeks of pregnancy, when uterine contractions become more intense, bleeding may increase.
Bleeding is caused by repeated abruption of the placenta, which is unable to stretch following the stretching of the uterine wall as pregnancy progresses or labor starts. In this case, the placenta partially exfoliates, and bleeding occurs from the vessels of the uterus. The fetus does not shed blood. However, he is threatened by oxygen starvation, since the exfoliated part of the placenta is not involved in gas exchange. nine0007
The fetus does not shed blood. However, he is threatened by oxygen starvation, since the exfoliated part of the placenta is not involved in gas exchange. nine0007
Provoking factors for bleeding during pregnancy can be: physical activity, sudden coughing, vaginal examination, sexual intercourse, increased intra-abdominal pressure with constipation, thermal procedures (hot bath, sauna).
With complete placenta previa, bleeding often occurs suddenly, without pain, and can be very heavy. Bleeding may stop, but reappear after some time, or may continue in the form of scanty discharge. In the last weeks of pregnancy, bleeding resumes and / or increases. nine0007
With incomplete placenta previa, bleeding may begin at the very end of pregnancy. However, more often it occurs at the beginning of labor. The amount of bleeding depends on the size of the placenta previa. The more placental tissue is present, the earlier and more bleeding begins.
Recurrent bleeding during pregnancy complicated by placenta previa in most cases leads to the development of anemia.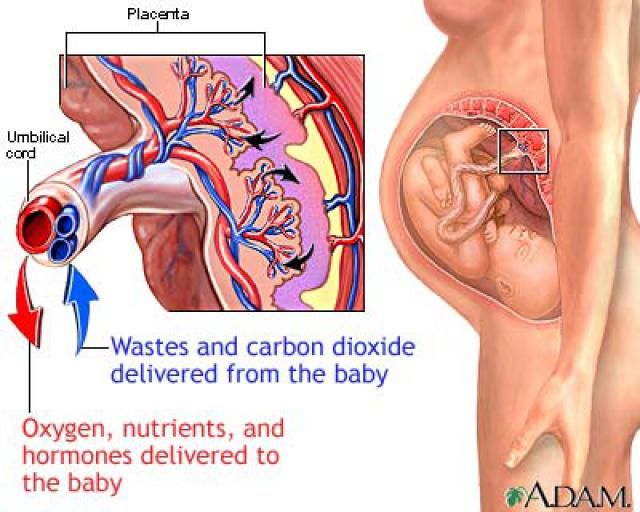
Pregnancy with placenta previa is often complicated by the threat of miscarriage, which is due to the same reasons as the occurrence of an incorrect location of the placenta. Preterm labor most often occurs in patients with complete placenta previa. nine0007
Pregnant women with placenta previa are characterized by low blood pressure, which occurs in 25%-34% of cases.
Preeclampsia (nephropathy, late toxicosis) is also no exception for pregnant women with placenta previa. This complication, which occurs against the background of dysfunction of a number of organs and systems, as well as with symptoms of blood clotting disorders, significantly worsens the nature of recurrent bleeding.
Placenta previa is often accompanied by fetal placental insufficiency, lack of oxygen for the fetus and delayed development. The exfoliated part of the placenta is switched off from the general system of the uteroplacental circulation and does not participate in gas exchange. With placenta previa, an incorrect position of the fetus (oblique, transverse) or breech presentation is often formed, which in turn are accompanied by certain complications.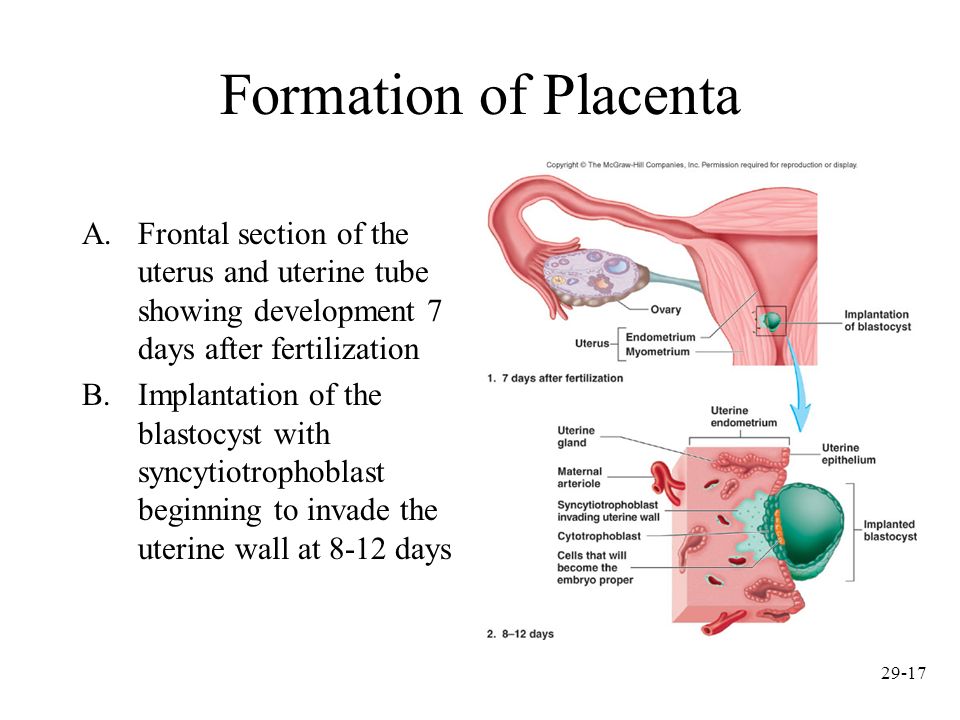 nine0007
nine0007
In obstetric practice, the term "migration of the placenta" is widely rooted, which, in fact, does not reflect the real essence of what is happening. The change in the location of the placenta is carried out due to a change in the structure of the lower segment of the uterus during pregnancy and the direction of growth of the placenta towards a better blood supply to the sections of the uterine wall (towards the bottom of the uterus) compared to its lower sections. A more favorable prognosis in terms of placental migration is noted when it is located on the anterior wall of the uterus. Usually the process of "migration of the placenta occurs within 6-10 weeks and is completed by the middle of 33-34 weeks of pregnancy.
Diagnosis of placenta previa
Placenta previa is not difficult to identify. The presence of placenta previa may be indicated by complaints of a pregnant woman about bleeding. In this case, recurrent bleeding from the second half of pregnancy, as a rule, is associated with complete placenta previa. Bleeding at the end of pregnancy or at the beginning of labor is more often associated with incomplete placenta previa.
Bleeding at the end of pregnancy or at the beginning of labor is more often associated with incomplete placenta previa.
In the presence of bleeding, carefully examine the walls of the vagina and cervix using speculums to exclude trauma or pathology of the cervix, which may also be accompanied by the presence of bloody discharge. nine0007
A vaginal examination of a pregnant woman also easily reveals clear diagnostic signs indicating an incorrect location of the placenta. However, such a study must be performed as carefully as possible, in compliance with all the necessary rules to prevent possible bleeding.
Currently, the most objective and safest method for diagnosing placenta previa is ultrasound, which allows you to establish the fact of placenta previa and the variant of placenta previa (complete, incomplete), determine the size, structure and area of the placenta, assess the degree of detachment, as well as get an accurate picture of the migration of the placenta.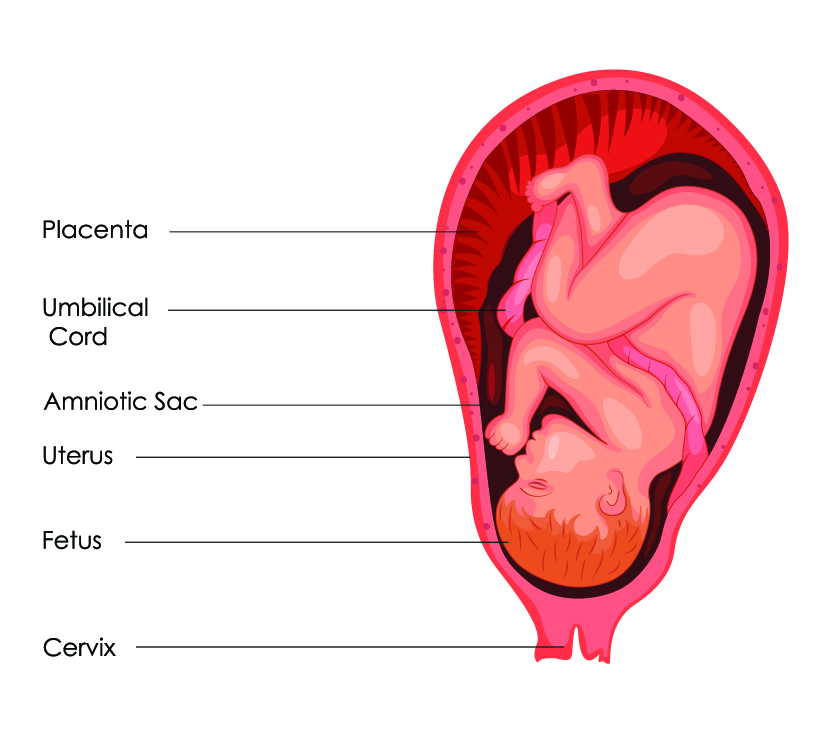 nine0007
nine0007
If the ultrasound revealed a complete placenta previa, then a vaginal examination should not be performed at all. The criterion for the low location of the placenta in the III trimester of pregnancy (28 - 40 weeks) is the distance from the edge of the placenta to the area of the internal os 5 cm or less. Placenta previa is indicated by the presence of placental tissue in the area of the internal os.
The nature of the localization of the placenta in the II and III trimesters of pregnancy (up to 27 weeks) is judged by the ratio of the distance from the edge of the placenta to the area of the internal os, with the diameter value (BDP) of the fetal head. nine0007
If an abnormal location of the placenta is detected, a dynamic study should be carried out to monitor its "migration". For these purposes, it is advisable to perform at least three echographic controls during pregnancy at 16, 24-26 and 34-36 weeks.
Ultrasound should be done when the bladder is moderately full.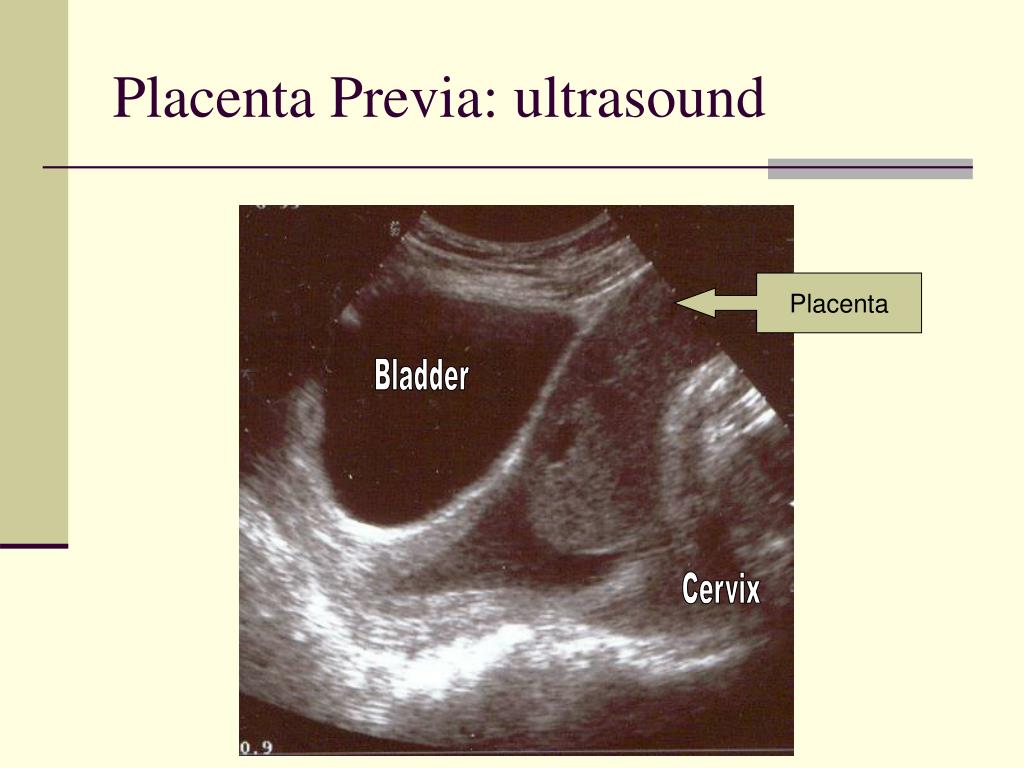 With the help of ultrasound, it is also possible to determine the presence of an accumulation of blood (hematoma) between the placenta and the wall of the uterus during placental abruption (in the event that there was no outflow of blood from the uterine cavity). If the site of placental abruption occupies no more than 1/4 of the area of the placenta, then the prognosis for the fetus is relatively favorable. In the event that the hematoma occupies more than 1/3 of the area of the placenta, then most often this leads to the death of the fetus. nine0007
With the help of ultrasound, it is also possible to determine the presence of an accumulation of blood (hematoma) between the placenta and the wall of the uterus during placental abruption (in the event that there was no outflow of blood from the uterine cavity). If the site of placental abruption occupies no more than 1/4 of the area of the placenta, then the prognosis for the fetus is relatively favorable. In the event that the hematoma occupies more than 1/3 of the area of the placenta, then most often this leads to the death of the fetus. nine0007
Medical support for pregnant women with placenta previa
The nature of management and treatment of pregnant women with placenta previa depends on the severity of bleeding and the amount of blood loss.
In the first half of pregnancy, if there is no blood discharge, then the pregnant woman can be at home under outpatient control in compliance with the regime that excludes the action of provoking factors that can cause bleeding (restriction of physical activity, sexual activity, stressful situations, etc.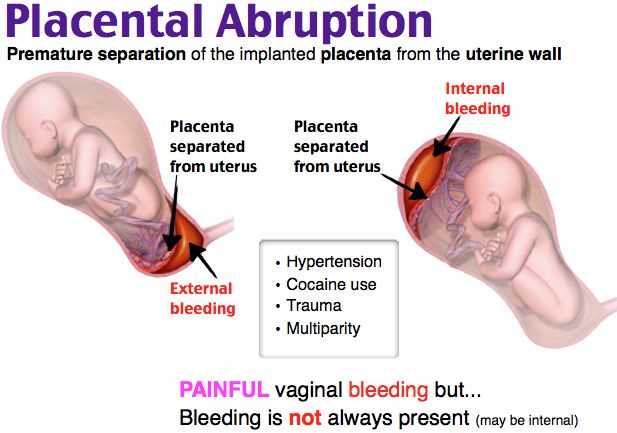 )
)
Observation and treatment for more than 24 weeks of pregnancy is carried out only in an obstetric hospital.
Treatment aimed at continuing the pregnancy up to 37-38 weeks is possible if the bleeding is not heavy, and the general condition of the pregnant woman and the fetus is satisfactory. Even despite the cessation of bloody discharge from the genital tract, pregnant women with placenta previa can under no circumstances be discharged from the hospital before delivery.
Management of pregnant women in an obstetric hospital includes: observance of strict bed rest; the use of drugs that ensure the optimization of the normalization of contractile activity; treatment of anemia and fetal placental insufficiency. nine0007
Emergency caesarean section, regardless of gestational age, is indicated for: recurrent bleeding; a combination of small blood loss with anemia and a decrease in blood pressure; simultaneous profuse blood loss; complete placenta previa and bleeding.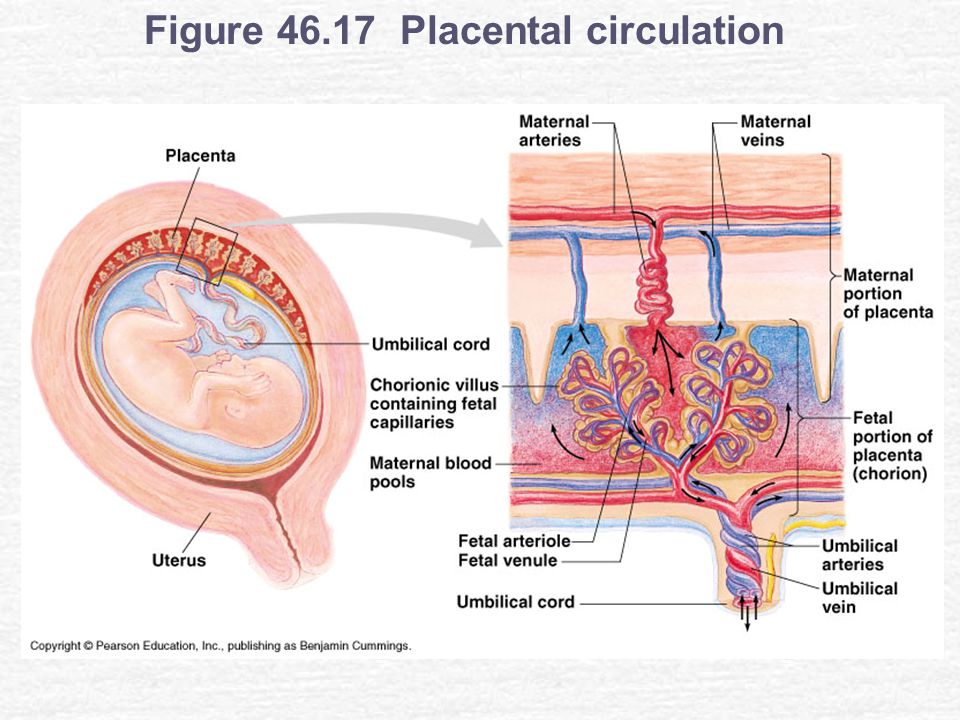
The operation is performed according to vital indications on the part of the mother, regardless of the duration of pregnancy and the condition of the fetus.
In the event that the pregnancy has been carried to 37-38 weeks and placenta previa persists, depending on the situation, the most optimal method of delivery is chosen on an individual basis. nine0007
The absolute indication for elective caesarean section is placenta previa. Childbirth through the natural birth canal in this situation is impossible, since the placenta that covers the internal os does not allow the presenting part of the fetus (fetal head or pelvic end) to be inserted into the pelvic inlet. In addition, in the process of increasing uterine contractions, the placenta will exfoliate more and more, and the bleeding will increase significantly.
In case of incomplete placenta previa and in the presence of concomitant complications (breech presentation, incorrect position of the fetus, scar on the uterus, multiple pregnancy, severe polyhydramnios, narrow pelvis, age of the primiparous over 30 years, etc.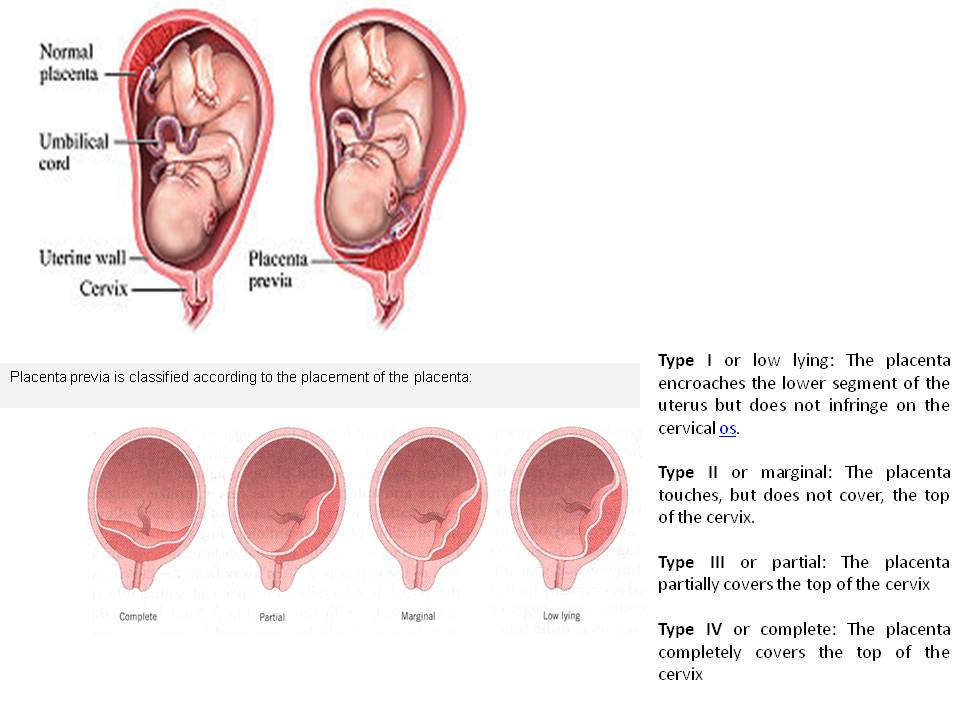 ), a caesarean section should also be performed in a planned manner. nine0007
), a caesarean section should also be performed in a planned manner. nine0007
If the above complications are absent and there is no bleeding, then you can wait until the onset of spontaneous labor activity, followed by early opening of the fetal bladder. In the event that after opening the fetal bladder, bleeding nevertheless began, then it is necessary to resolve the issue of performing a caesarean section.
If, with incomplete placenta previa, bleeding occurs before the onset of labor, then the fetal bladder is opened. The necessity and expediency of this procedure is due to the fact that when the membranes are opened, the fetal head is inserted into the entrance to the pelvis and presses the exfoliated part of the placenta against the wall of the uterus and pelvis, which helps to stop further placental abruption and stop bleeding. If bleeding after opening the fetal bladder continues and / or the cervix is immature, then a caesarean section is performed. In the case of stopping bleeding, it is possible to conduct labor through the natural birth canal (with a favorable obstetric situation).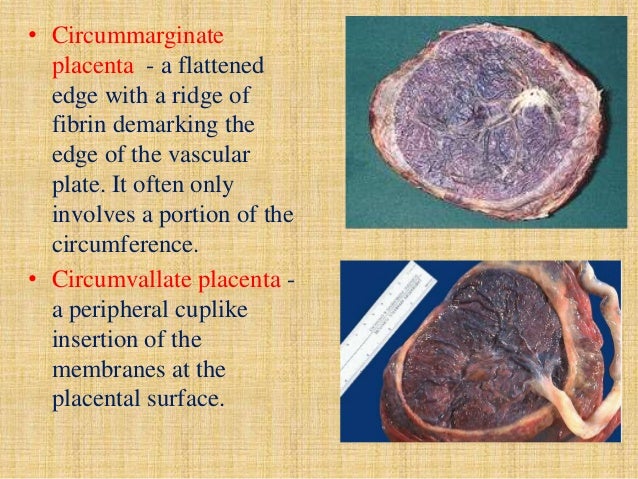 nine0007
nine0007
Bleeding can also begin in the early stages of labor, from the moment of the first contractions. In this case, early opening of the fetal bladder is also shown.
Thus, the management of labor with incomplete placenta previa through the natural birth canal is possible if: the bleeding has stopped after opening the fetal bladder; mature cervix; labor activity is good; there is a cephalic presentation of the fetus.
However, caesarean section is one of the most frequently chosen methods of delivery by obstetricians in placenta previa and is performed with a frequency of 70% -80% in this pathology. nine0007
Other typical complications in childbirth with incomplete placenta previa are weakness of labor and insufficient oxygen supply to the fetus (fetal hypoxia). A prerequisite for conducting labor through the natural birth canal is constant monitoring of the condition of the fetus and the contractile activity of the uterus.
After the birth of a child, bleeding may resume due to a violation of the process of separation of the placenta, since the placental site is located in the lower sections of the uterus, the contractility of which is reduced. nine0007
nine0007
Abundant bleeding often occurs in the early postpartum period due to a decrease in uterine tone and damage to the extensive vasculature of the cervix.
Prevention of placenta previa
Prevention of placenta previa is to reduce the number of abortions, early detection and treatment of various inflammatory diseases of the reproductive system and hormonal disorders.
RS80 ultrasound scanner
Setting new standards! nine0006 Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of state-of-the-art ultrasound technologies to solve the most complex diagnostic problems.
Placenta along the anterior wall of the uterus: norm or pathology?
The placenta is an important organ that forms and develops only during pregnancy. The placenta is a kind of connecting element between mother and baby. Through this important organ, the child receives oxygen and nutrients. The baby receives antibodies, as well as hormones that are responsible for the safety of the pregnancy and the normal development of the unborn child.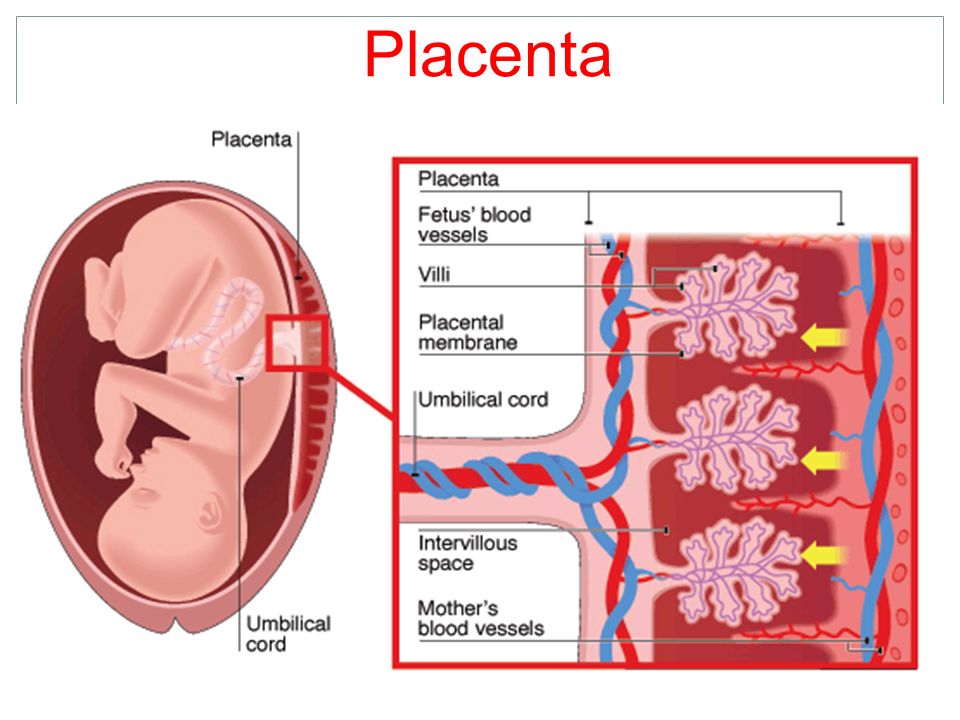 nine0007
nine0007
The formation of the placenta begins a week after fertilization, and after childbirth, within half an hour, it leaves the uterus, having completed all its functions.
Many pregnant women are interested in the question of the correct location of this organ. The placenta is usually located along the anterior or posterior wall, closer to the bottom of the uterus. This arrangement ensures the safety of this body and the performance of its necessary function.
Find out what to do if the placenta is low?
Today, many expectant mothers are worried about what to do if the placenta is low....
The location of the placenta depends on where the fertilized egg will attach after conception. You can find out placentation through ultrasound.
The position of the placenta in the uterus can be as follows:
- placenta along the anterior wall;
- placenta on the back wall;
- placenta in the fundus of the uterus;
- placenta in the area of the lateral wall.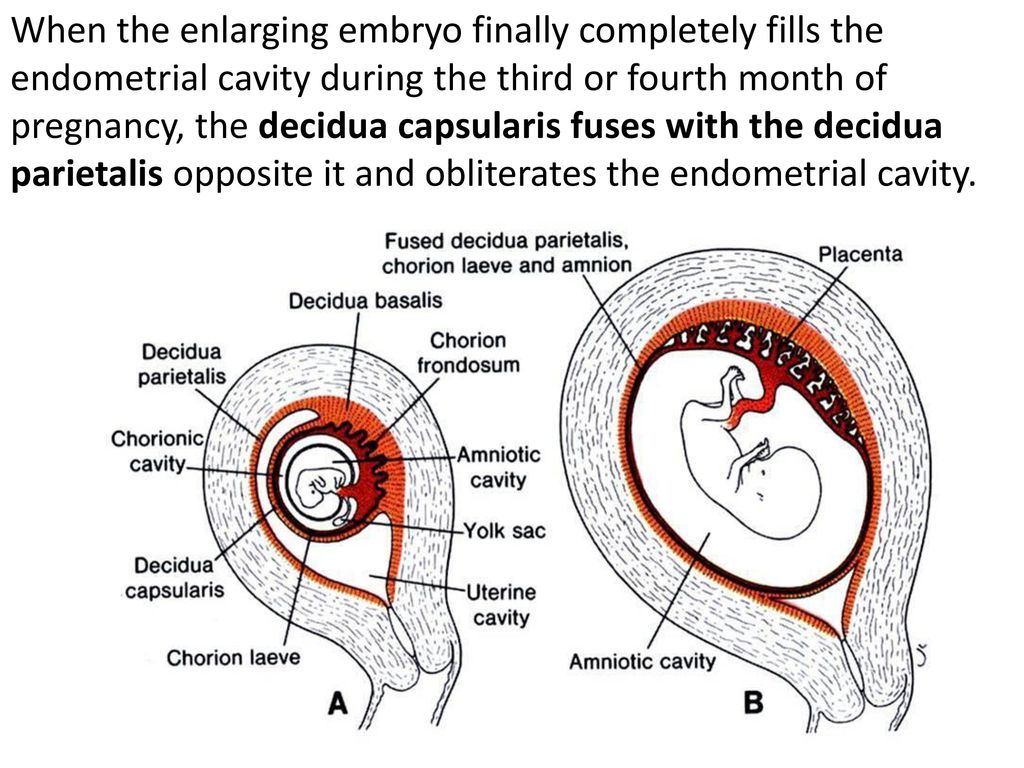 nine0007
nine0007
All of the above are normal and do not pose any threat to either the mother or the fetus.
An anterior placenta can only pose a threat in case of operative delivery (caesarean section). This is associated with an increased risk of possible bleeding. The placenta on the front wall of the uterus can be located exactly in the place where the doctor needs to make an incision to remove the baby.
Marginal placenta previa - a threat to the normal course...
Pregnancy is a happy and anxious time at the same time. Expecting a baby can be overshadowed...
If you are going to have a caesarean section and have an anterior placentation, there is no need to worry in advance. Surgeons will necessarily take all necessary measures in order to reduce the risk, and in case of bleeding, they will be able to quickly stop it.
In some cases, abnormal (incorrect) attachment of the placenta is possible.
Low position of the placenta is a pathology in which the connecting organ between the mother and the fetus is located at a level of six centimeters or less from the internal cervical os. It does not matter where the placenta is located: on the front wall, on the side or on the back. The distance to the cervix plays a role. In most cases, the low location of the placenta does not pose a threat, since with the growth of the abdomen, it moves higher to the bottom of the uterus. nine0007
It does not matter where the placenta is located: on the front wall, on the side or on the back. The distance to the cervix plays a role. In most cases, the low location of the placenta does not pose a threat, since with the growth of the abdomen, it moves higher to the bottom of the uterus. nine0007
Placenta previa is a location in which the internal os is blocked (partially or completely). There are three types of presentation: marginal, lateral and complete.
With marginal presentation, the placenta covers the inner surface of the cervix by no more than one third, with lateral presentation - by two thirds, and with full presentation - completely. It does not matter whether the placenta is located on the front wall of the uterus, on the side or on the back.
Among the complications that are present with such a diagnosis as presentation, the most formidable can be distinguished: fetoplacental insufficiency, which leads to intrauterine growth retardation, the risk of bleeding, especially at 28-32 weeks, when the activity of the uterus increases, the threat of miscarriage .