How common are ear infections in babies
Ear Infections in Babies and Toddlers
Featured Expert:
Ear infections in babies and toddlers are extremely common. In fact, according to the National Institutes of Health, five out of six children will experience an ear infection before their third birthday.
"Many parents are concerned that an ear infection will affect their child's hearing irreversibly—or that an ear infection will go undetected and untreated," says David Tunkel, M.D., Johns Hopkins Medicine pediatric otolaryngologist (ENT). "The good news is that most ear infections go away on their own, and those that don't are typically easy to treat."
Childhood Ear Infections Explained
Ear infections happen when there is inflammation— usually from trapped bacteria—in the middle ear, the part of the ear connects to the back of the nose and throat. The most common type of ear infection is otitis media, which results when fluid builds up behind the eardrum and parts of the middle ear become infected and swollen.
If your child has a sore throat, cold, or an upper respiratory infection, bacteria can spread to the middle ear through the eustachian tubes (the channels that connect the middle ear to the throat). In response to the infection, fluid builds up behind the eardrum.
Children are more likely to suffer from ear infections than adults for two reasons:
- Their immune systems are underdeveloped and less equipped to fight off infections.
- Their eustachian tubes are smaller and more horizontal, which makes it more difficult for fluid to drain out of the ear.
"In some cases, fluid remains trapped in the middle ear for a long time, or returns repeatedly, even when there's no infection," Tunkel explains.
Ear Infection Signs and Symptoms
The telltale sign of an ear infection is pain in and around the ear.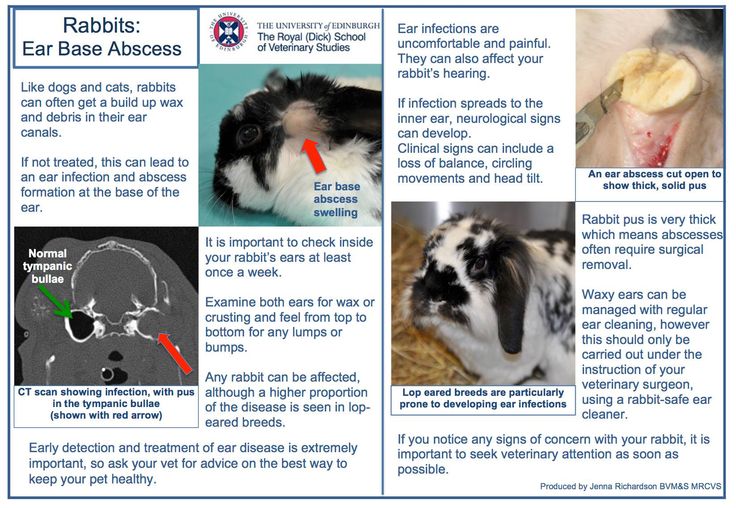 Young children can develop ear infections before they are old enough to talk. That means parents are often left guessing why their child appears to be suffering. When your child can't say "my ear hurts," the following signs suggest an ear infection could be the culprit:
Young children can develop ear infections before they are old enough to talk. That means parents are often left guessing why their child appears to be suffering. When your child can't say "my ear hurts," the following signs suggest an ear infection could be the culprit:
- Tugging or pulling the ear
- Crying and irritability
- Difficulty sleeping
- Fever, especially in younger children
- Fluid draining from the ear
- Loss of balance
- Difficulty hearing or responding to auditory cues
Signs that require immediate attention include high fever, severe pain, or bloody or pus-like discharge from the ears.
Pediatric Otolaryngology
Our pediatric otolaryngologists provide compassionate and comprehensive care for children with common and rare ear, nose, and throat conditions. As part of the Johns Hopkins Children's Center, you have access to all the specialized resources of a children's hospital.
Learn more about Pediatric Otolaryngology
Ear Infection Treatments
Most ear infections go away without treatment. "If your child isn't in severe pain, your doctor may suggest a 'wait-and-see' approach coupled with over-the-counter pain relievers to see if the infection clears on its own," Tunkel says.
The reason: Treating an infection with antibiotics may cause the bacteria causing the infections to become resistant to those antibiotics—and that makes treating future infections more difficult. Equally important, in most cases antibiotics aren't necessary. Otitis media tends to get better without them. While you may be tempted to treat your child's ear infection with homeopathic or natural medicine, Tunkel warns they aren’t well studied.
Your best bet is to work with your child's health care provider to determine the appropriate course of action. In nearly every case, treatment decisions depend on the child’s age, degree of pain and presenting symptoms.
Under 6 months
Babies under six months almost always receive antibiotics. At this age, children are not fully vaccinated. Equally important, there's no research about the safety of skipping antibiotics for babies under 6 months of age — and complications from ear infections can be more severe when they occur in young babies. Bacteria trapped behind the eardrum can spread to other parts of the body and cause serious infections.
6 months to 2 years
For children between the ages of 6 months and 2 years, the American Academy of Pediatrics (AAP) recommends shared decision-making between parents and providers about whether to treat ear infections that are not severe. The best course is often to watch the child for two to three days before prescribing antibiotic treatment. If the child is in pain, or the ear infection is advanced, your child's doctor may suggest immediate antibiotic treatment.
Over 2 years
With children over the age of 2, ear infections that are not severe are likely to clear on their own, without treatment. "In the meantime, you can treat pain with over-the-counter medications, such as ibuprofen or acetaminophen," Tunkel says. If there's no improvement after two to three days, antibiotics may be warranted.
"In the meantime, you can treat pain with over-the-counter medications, such as ibuprofen or acetaminophen," Tunkel says. If there's no improvement after two to three days, antibiotics may be warranted.
Unfortunately, some children suffer from recurrent ear infections, sometimes up to five or six a year. Kids who get repeated infections may benefit from a surgical procedure where doctors insert small tubes in the eardrums to improve air flow and prevent fluid buildup. "Tubes don't prevent all ear infections, but they make managing them significantly easier," Tunkel explains.
Ear Infection Prevention
There are several steps you can take to reduce your child's risk of developing ear infections, including:
- Vaccinate your child: Children who are up-to-date on their vaccines get fewer ear infections than their unvaccinated counterparts. The 13-valent pneumococcal conjugate vaccine (PCV13) protects against 13 types of infection-causing bacteria.
- Consider breastfeeding: Breast milk contains antibodies that may help reduce the risk of ear infections and a host of other ailments. Whether you feed milk or formula, make sure your child sits up during feedings to prevent fluid from flowing into the middle ear.
- Wash your hands frequently: The best way to protect your child against cold and flu is to keep your hands clean. Wash your hands with soap and water and scrub them clean for a full 20 seconds each time you visit the sink.
- Steer clear of sick people: Don't allow your child to spend time with children or adults who are sick.
- Avoid secondhand smoke: Studies show that children who are exposed to secondhand smoke are up to three times more likely to develop ear infections than those who don't have those exposures.
Whether your child has ear infections or not, it's important to ensure they're able to hear well. "No child is too young to have a hearing test," Tunkel says. "We use a variety of techniques to test infant hearing and we can identify a hearing problem even in newborns."
"No child is too young to have a hearing test," Tunkel says. "We use a variety of techniques to test infant hearing and we can identify a hearing problem even in newborns."
Ear Infections in Children, Babies & Toddlers
What is an ear infection?
An ear infection is an inflammation of the middle ear, usually caused by bacteria, that occurs when fluid builds up behind the eardrum. Anyone can get an ear infection, but children get them more often than adults. Five out of six children will have at least one ear infection by their third birthday. In fact, ear infections are the most common reason parents bring their child to a doctor. The scientific name for an ear infection is otitis media (OM).
What are the symptoms of an ear infection?
There are three main types of ear infections. Each has a different combination of symptoms.
- Acute otitis media (AOM) is the most common ear infection. Parts of the middle ear are infected and swollen and fluid is trapped behind the eardrum.
 This causes pain in the ear—commonly called an earache. Your child might also have a fever.
This causes pain in the ear—commonly called an earache. Your child might also have a fever. - Otitis media with effusion (OME) sometimes happens after an ear infection has run its course and fluid stays trapped behind the eardrum. A child with OME may have no symptoms, but a doctor will be able to see the fluid behind the eardrum with a special instrument.
- Chronic otitis media with effusion (COME) happens when fluid remains in the middle ear for a long time or returns over and over again, even though there is no infection. COME makes it harder for children to fight new infections and also can affect their hearing.
How can I tell if my child has an ear infection?
Most ear infections happen to children before they’ve learned how to talk. If your child isn’t old enough to say “My ear hurts,” here are a few things to look for:
- Tugging or pulling at the ear(s)
- Fussiness and crying
- Trouble sleeping
- Fever (especially in infants and younger children)
- Fluid draining from the ear
- Clumsiness or problems with balance
- Trouble hearing or responding to quiet sounds
What causes an ear infection?
An ear infection usually is caused by bacteria and often begins after a child has a sore throat, cold, or other upper respiratory infection. If the upper respiratory infection is bacterial, these same bacteria may spread to the middle ear; if the upper respiratory infection is caused by a virus, such as a cold, bacteria may be drawn to the microbe-friendly environment and move into the middle ear as a secondary infection. Because of the infection, fluid builds up behind the eardrum.
If the upper respiratory infection is bacterial, these same bacteria may spread to the middle ear; if the upper respiratory infection is caused by a virus, such as a cold, bacteria may be drawn to the microbe-friendly environment and move into the middle ear as a secondary infection. Because of the infection, fluid builds up behind the eardrum.
Image
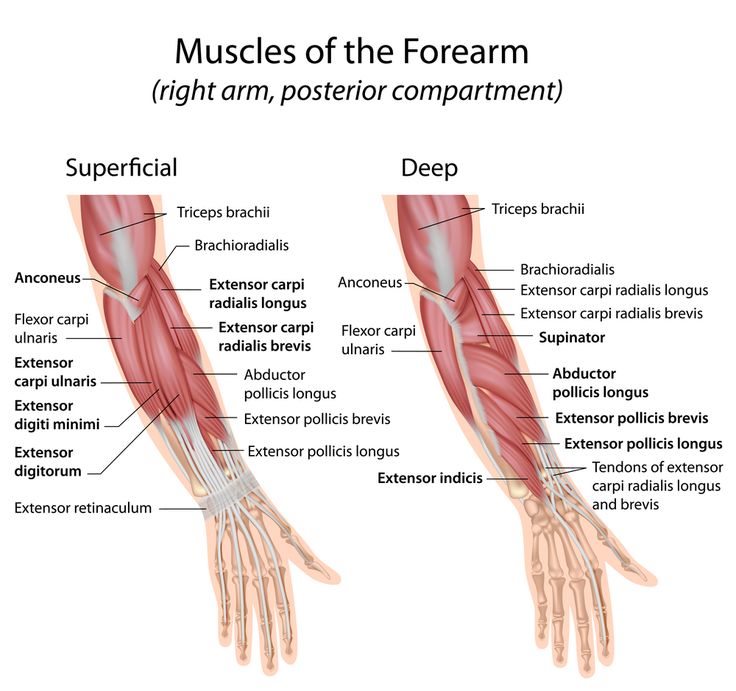
Source: NIH/NIDCDThe ear has three major parts: the outer ear, the middle ear, and the inner ear. The outer ear, also called the pinna, includes everything we see on the outside—the curved flap of the ear leading down to the earlobe—but it also includes the ear canal, which begins at the opening to the ear and extends to the eardrum. The eardrum is a membrane that separates the outer ear from the middle ear.
The middle ear—which is where ear infections occur—is located between the eardrum and the inner ear. Within the middle ear are three tiny bones called the malleus, incus, and stapes that transmit sound vibrations from the eardrum to the inner ear.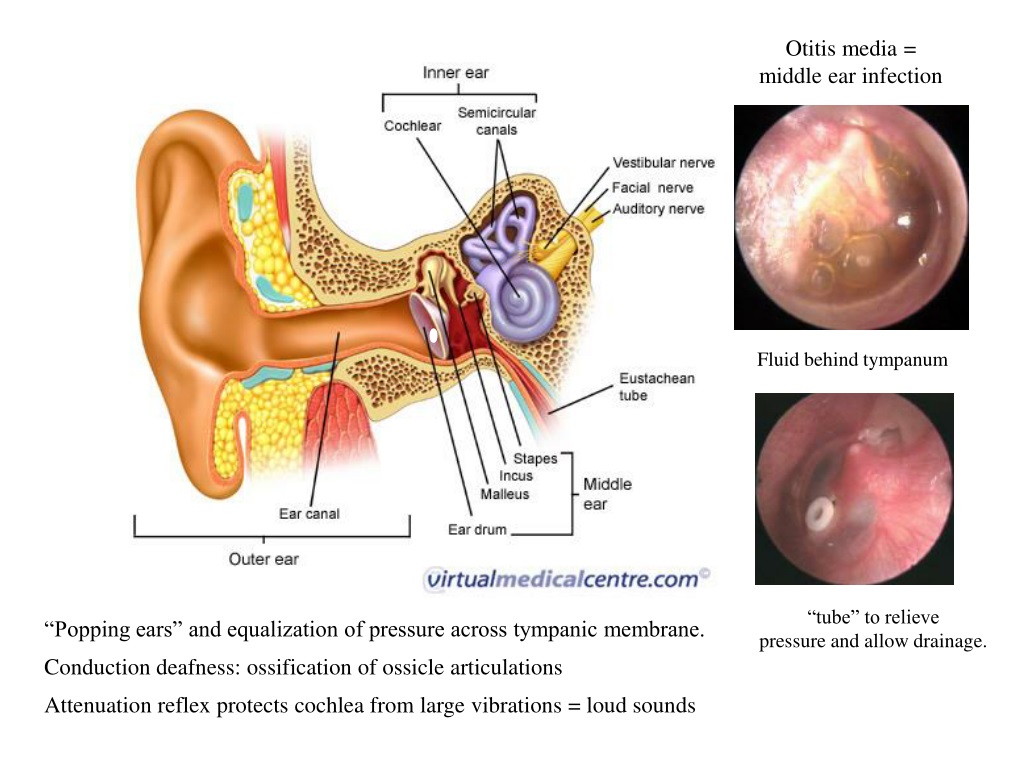 The bones of the middle ear are surrounded by air.
The bones of the middle ear are surrounded by air.
The inner ear contains the labyrinth, which help us keep our balance. The cochlea, a part of the labyrinth, is a snail-shaped organ that converts sound vibrations from the middle ear into electrical signals. The auditory nerve carries these signals from the cochlea to the brain.
Other nearby parts of the ear also can be involved in ear infections. The eustachian tube is a small passageway that connects the upper part of the throat to the middle ear. Its job is to supply fresh air to the middle ear, drain fluid, and keep air pressure at a steady level between the nose and the ear.
Adenoids are small pads of tissue located behind the back of the nose, above the throat, and near the eustachian tubes. Adenoids are mostly made up of immune system cells. They fight off infection by trapping bacteria that enter through the mouth.
Why are children more likely than adults to get ear infections?
There are several reasons why children are more likely than adults to get ear infections.
Eustachian tubes are smaller and more level in children than they are in adults. This makes it difficult for fluid to drain out of the ear, even under normal conditions. If the eustachian tubes are swollen or blocked with mucus due to a cold or other respiratory illness, fluid may not be able to drain.
A child’s immune system isn’t as effective as an adult’s because it’s still developing. This makes it harder for children to fight infections.
As part of the immune system, the adenoids respond to bacteria passing through the nose and mouth. Sometimes bacteria get trapped in the adenoids, causing a chronic infection that can then pass on to the eustachian tubes and the middle ear.
How does a doctor diagnose a middle ear infection?
The first thing a doctor will do is ask you about your child’s health. Has your child had a head cold or sore throat recently? Is he having trouble sleeping? Is she pulling at her ears? If an ear infection seems likely, the simplest way for a doctor to tell is to use a lighted instrument, called an otoscope, to look at the eardrum.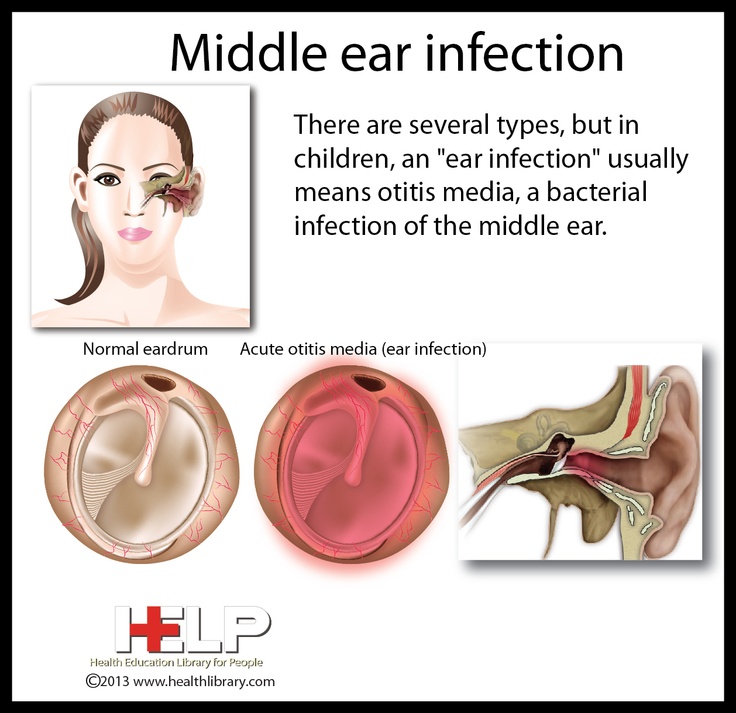 A red, bulging eardrum indicates an infection.
A red, bulging eardrum indicates an infection.
A doctor also may use a pneumatic otoscope, which blows a puff of air into the ear canal, to check for fluid behind the eardrum. A normal eardrum will move back and forth more easily than an eardrum with fluid behind it.
Tympanometry, which uses sound tones and air pressure, is a diagnostic test a doctor might use if the diagnosis still isn’t clear. A tympanometer is a small, soft plug that contains a tiny microphone and speaker as well as a device that varies air pressure in the ear. It measures how flexible the eardrum is at different pressures.
How is an acute middle ear infection treated?
Many doctors will prescribe an antibiotic, such as amoxicillin, to be taken over seven to 10 days. Your doctor also may recommend over-the-counter pain relievers such as acetaminophen or ibuprofen, or eardrops, to help with fever and pain. (Because aspirin is considered a major preventable risk factor for Reye’s syndrome, a child who has a fever or other flu-like symptoms should not be given aspirin unless instructed to by your doctor.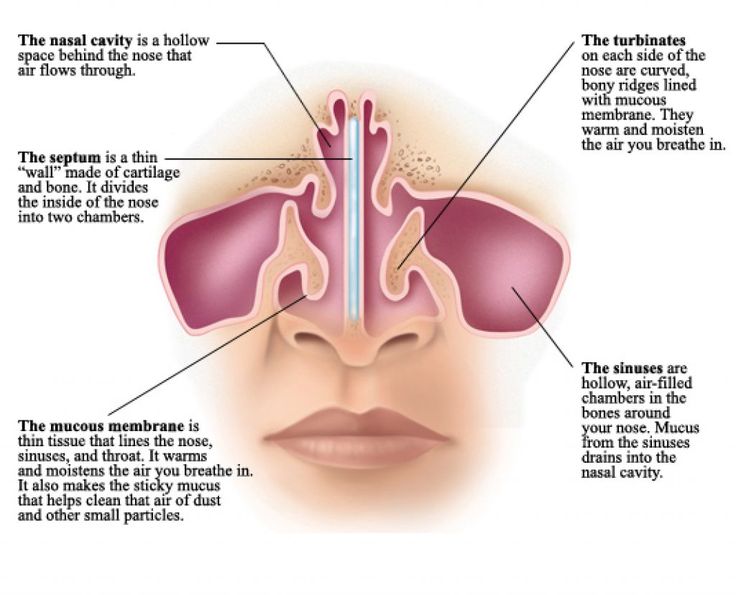 )
)
If your doctor isn’t able to make a definite diagnosis of OM and your child doesn’t have severe ear pain or a fever, your doctor might ask you to wait a day or two to see if the earache goes away. The American Academy of Pediatrics issued guidelines in 2013 that encourage doctors to observe and closely follow these children with ear infections that can’t be definitively diagnosed, especially those between the ages of 6 months to 2 years. If there’s no improvement within 48 to 72 hours from when symptoms began, the guidelines recommend doctors start antibiotic therapy. Sometimes ear pain isn’t caused by infection, and some ear infections may get better without antibiotics. Using antibiotics cautiously and with good reason helps prevent the development of bacteria that become resistant to antibiotics.
If your doctor prescribes an antibiotic, it’s important to make sure your child takes it exactly as prescribed and for the full amount of time. Even though your child may seem better in a few days, the infection still hasn’t completely cleared from the ear.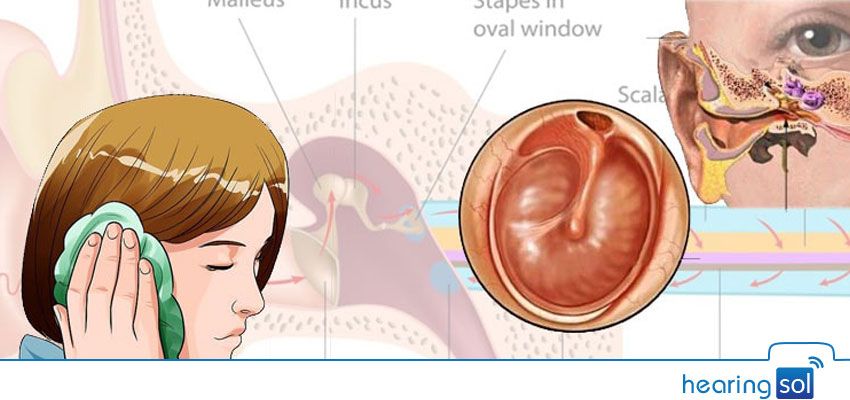 Stopping the medicine too soon could allow the infection to come back. It’s also important to return for your child’s follow-up visit, so that the doctor can check if the infection is gone.
Stopping the medicine too soon could allow the infection to come back. It’s also important to return for your child’s follow-up visit, so that the doctor can check if the infection is gone.
How long will it take my child to get better?
Your child should start feeling better within a few days after visiting the doctor. If it’s been several days and your child still seems sick, call your doctor. Your child might need a different antibiotic. Once the infection clears, fluid may still remain in the middle ear but usually disappears within three to six weeks.
What happens if my child keeps getting ear infections?
To keep a middle ear infection from coming back, it helps to limit some of the factors that might put your child at risk, such as not being around people who smoke and not going to bed with a bottle. In spite of these precautions, some children may continue to have middle ear infections, sometimes as many as five or six a year. Your doctor may want to wait for several months to see if things get better on their own but, if the infections keep coming back and antibiotics aren’t helping, many doctors will recommend a surgical procedure that places a small ventilation tube in the eardrum to improve air flow and prevent fluid backup in the middle ear.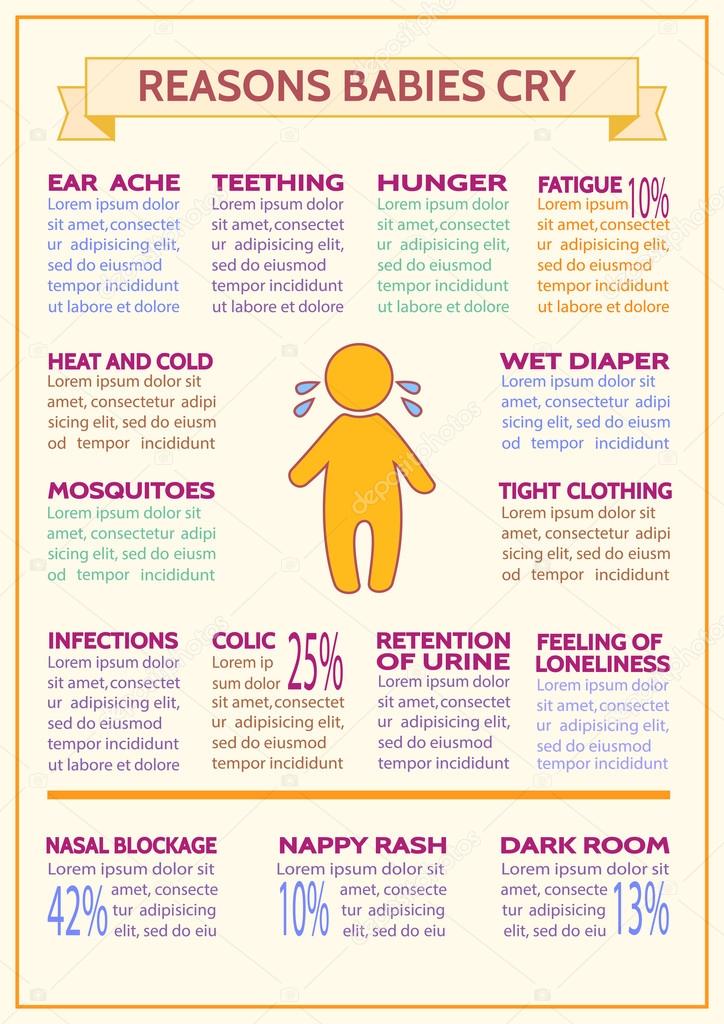 The most commonly used tubes stay in place for six to nine months and require follow-up visits until they fall out.
The most commonly used tubes stay in place for six to nine months and require follow-up visits until they fall out.
If placement of the tubes still doesn’t prevent infections, a doctor may consider removing the adenoids to prevent infection from spreading to the eustachian tubes.
Can ear infections be prevented?
Currently, the best way to prevent ear infections is to reduce the risk factors associated with them. Here are some things you might want to do to lower your child’s risk for ear infections.
- Vaccinate your child against the flu. Make sure your child gets the influenza, or flu, vaccine every year.
- It is recommended that you vaccinate your child with the 13-valent pneumococcal conjugate vaccine (PCV13). The PCV13 protects against more types of infection-causing bacteria than the previous vaccine, the PCV7. If your child already has begun PCV7 vaccination, consult your physician about how to transition to PCV13. The Centers for Disease Control and Prevention (CDC) recommends that children under age 2 be vaccinated, starting at 2 months of age.
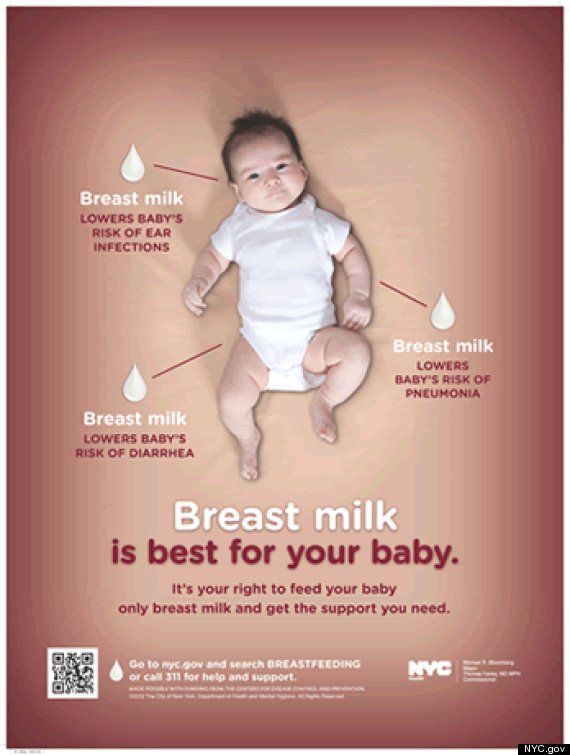 Studies have shown that vaccinated children get far fewer ear infections than children who aren’t vaccinated. The vaccine is strongly recommended for children in daycare.
Studies have shown that vaccinated children get far fewer ear infections than children who aren’t vaccinated. The vaccine is strongly recommended for children in daycare. - Wash hands frequently. Washing hands prevents the spread of germs and can help keep your child from catching a cold or the flu.
- Avoid exposing your baby to cigarette smoke. Studies have shown that babies who are around smokers have more ear infections.
- Never put your baby down for a nap, or for the night, with a bottle.
- Don’t allow sick children to spend time together. As much as possible, limit your child’s exposure to other children when your child or your child’s playmates are sick.
What research is being done on middle ear infections?
Researchers sponsored by the National Institute on Deafness and Other Communication Disorders (NIDCD) are exploring many areas to improve the prevention, diagnosis, and treatment of middle ear infections. For example, finding better ways to predict which children are at higher risk of developing an ear infection could lead to successful prevention tactics.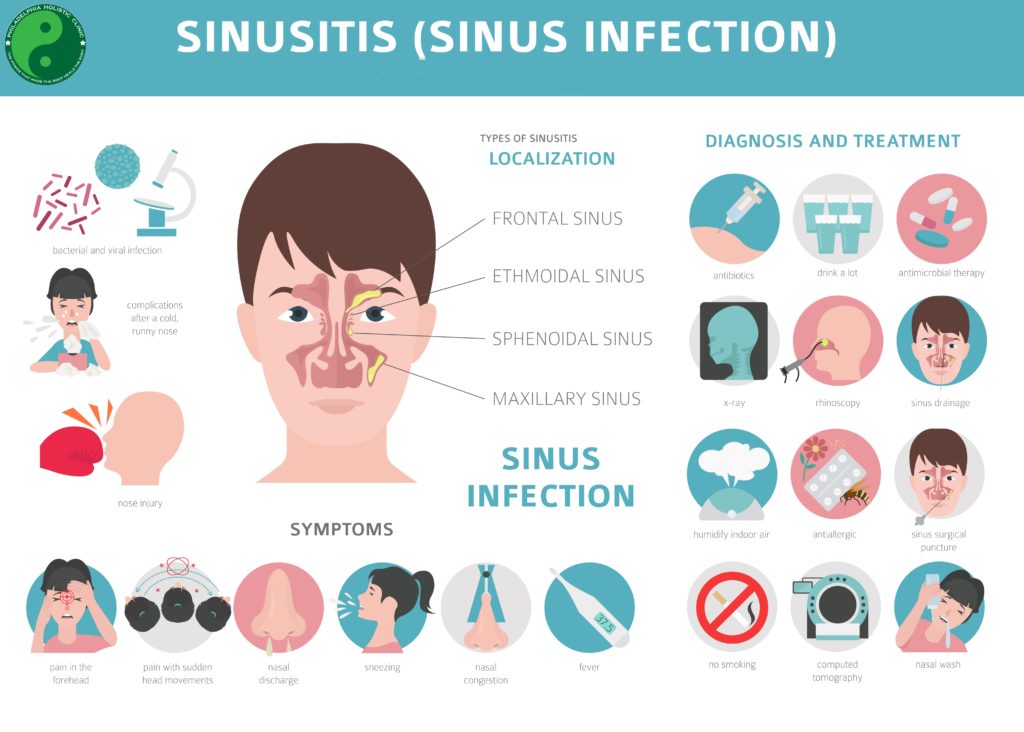
Another area that needs exploration is why some children have more ear infections than others. For example, Native American and Hispanic children have more infections than do children in other ethnic groups. What kinds of preventive measures could be taken to lower the risks?
Doctors also are beginning to learn more about what happens in the ears of children who have recurring ear infections. They have identified colonies of antibiotic-resistant bacteria, called biofilms, that are present in the middle ears of most children with chronic ear infections. Understanding how to attack and kill these biofilms would be one way to successfully treat chronic ear infections and avoid surgery.
Understanding the impact that ear infections have on a child’s speech and language development is another important area of study. Creating more accurate methods to diagnose middle ear infections would help doctors prescribe more targeted treatments. Researchers also are evaluating drugs currently being used to treat ear infections, and developing new, more effective and easier ways to administer medicines.
NIDCD-supported investigators continue to explore vaccines against some of the most common bacteria and viruses that cause middle ear infections, such as nontypeable Haemophilus influenzae (NTHi) and Moraxella catarrhalis. One team is conducting studies on a method for delivering a possible vaccine without a needle.
Where can I find additional information about ear infections?
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, smell, taste, voice, speech, and language.
Use the following keywords to help you search for organizations that can answer questions and provide printed or electronic information on ear infections:
- Otitis media (ear infection)
- Speech-language development
- Early identification of hearing loss in children
NIDCD Information Clearinghouse
1 Communication Avenue
Bethesda, MD 20892-3456
Toll-free voice: (800) 241-1044
Toll-free TTY: (800) 241-1055
Email: nidcdinfo@nidcd. nih.gov
nih.gov
Ear infections in children!
How can you tell if your child has an ear infection?
The easiest way to find out if your child is likely to get an ear infection (or any other illness) is to watch their mood change.
If your baby is fussing or crying more than usual, look for the problem. If he has a fever (weak or strong), you have another big clue. Ear infections are usually accompanied by a cold or sinus infection, so keep that in mind. nine0005
You may also notice the following symptoms:
Your child is pulling, grabbing, or tugging at his ears. This may be a sign that he is in pain. (Babies touch their ears for many other reasons, so if your baby is fine, he probably doesn't have an ear infection.)
Diarrhea or vomiting. The bacteria that cause an ear infection can also affect the gastrointestinal tract.
Decreased appetite. nine0004 Ear infections can cause gastrointestinal disturbances.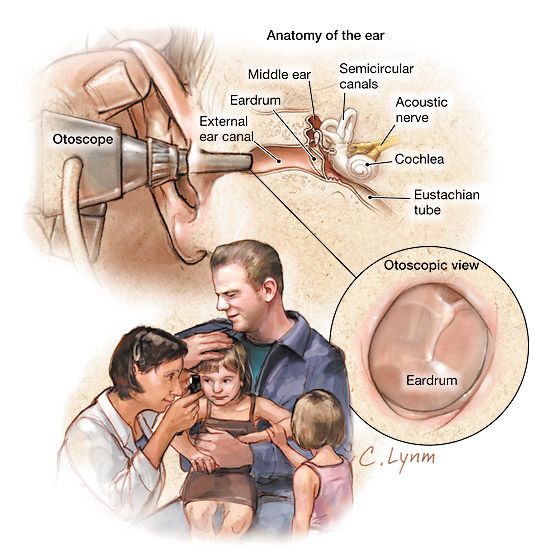 They can also force your child to swallow without chewing food. If your baby has an ear infection, he may refuse the breast or bottle after taking the first few sips.
They can also force your child to swallow without chewing food. If your baby has an ear infection, he may refuse the breast or bottle after taking the first few sips.
Yellow or whitish fluid that flows from the ear. This does not happen to most children, but it is a sure sign of infection. It also signals that a small hole has formed in the eardrum. (Don't worry - it will clear up once the infection clears up.)
Bad smell You may notice a bad smell coming from your child's ear.
Sleep problems . Lying down can make an ear infection more painful.
How common are ear infections in children?
Ear infections are the second most commonly diagnosed illness in children in the United States (after the common cold). A large study found that 23 percent of children had at least one ear infection by their first birthday, and more than half had at least one ear infection by age 3. nine0005
What causes ear infections in children?
An ear infection can be caused by bacteria or viruses.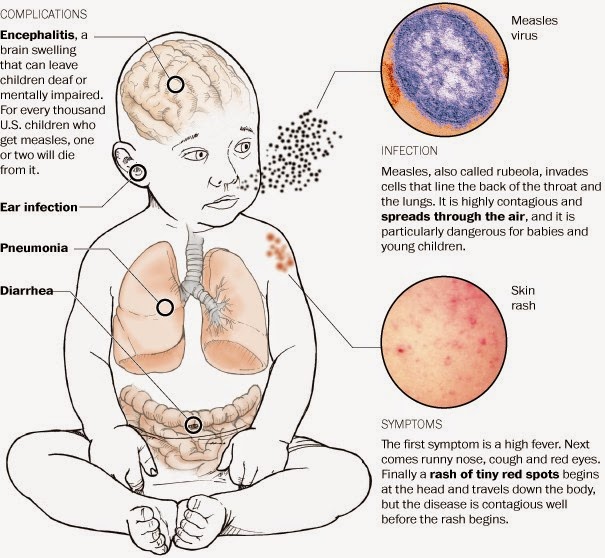 This happens when fluid builds up in the area behind your child's eardrum and then becomes infected.
This happens when fluid builds up in the area behind your child's eardrum and then becomes infected.
Normally, any fluid that enters this area is rapidly drained through the Eustachian tubes, which connect the middle ear to the back of the nose and throat. But if the Eustachian tube is blocked—as is often the case with colds, sinus infections, even allergies—fluid enters the middle ear. nine0005
Microbes like to grow in dark, warm, damp places, so a fluid-filled middle ear is an ideal breeding ground. As the infection gets worse, the inflammation in and behind the eardrum also tends to get worse, making the condition more painful. The child may also develop a fever as their body fights off the infection.
Acute otitis media is the medical term for a painfully inflamed middle ear, accompanied by accumulation of fluid, red tympanic membrane, and sometimes fever. nine0005
The use of a pacifier may increase the risk of middle ear infections in infants and young children.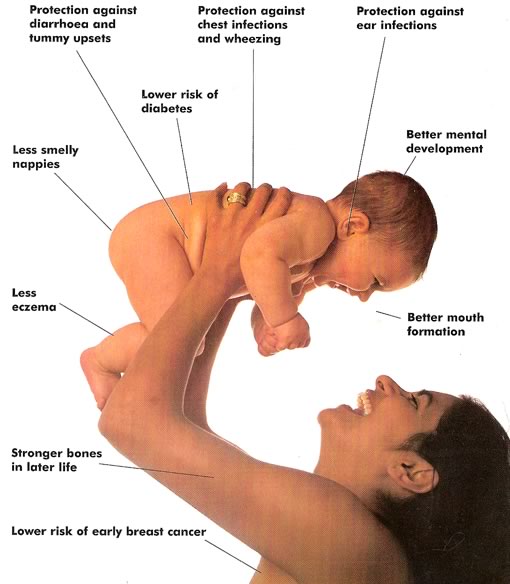 In one study, the incidence of ear infections was 33% lower in children who did not use pacifiers.
In one study, the incidence of ear infections was 33% lower in children who did not use pacifiers.
Babies are more prone to ear infections because they have short (about 1/2 inch) horizontal Eustachian tubes. As children get older, their tubes triple in size and become more vertical, so the fluid "drains" more easily.
When to call the doctor if your child has an ear infection
Call at the first sign of an ear infection. The doctor will examine your child's ear with an instrument called an otoscope. Red tympanic membrane, bulging and possibly draining, probably infected.
The doctor may also check to see if the eardrum moves in response to a device called a pneumatic otoscope, which releases a short stream of air into the ear. If it doesn't move, this is another sign that fluid is building up in the middle ear and may be infected. nine0005
How to treat an ear infection in a child?
Most ear infections go away on their own, but severe cases need to be treated with antibiotics.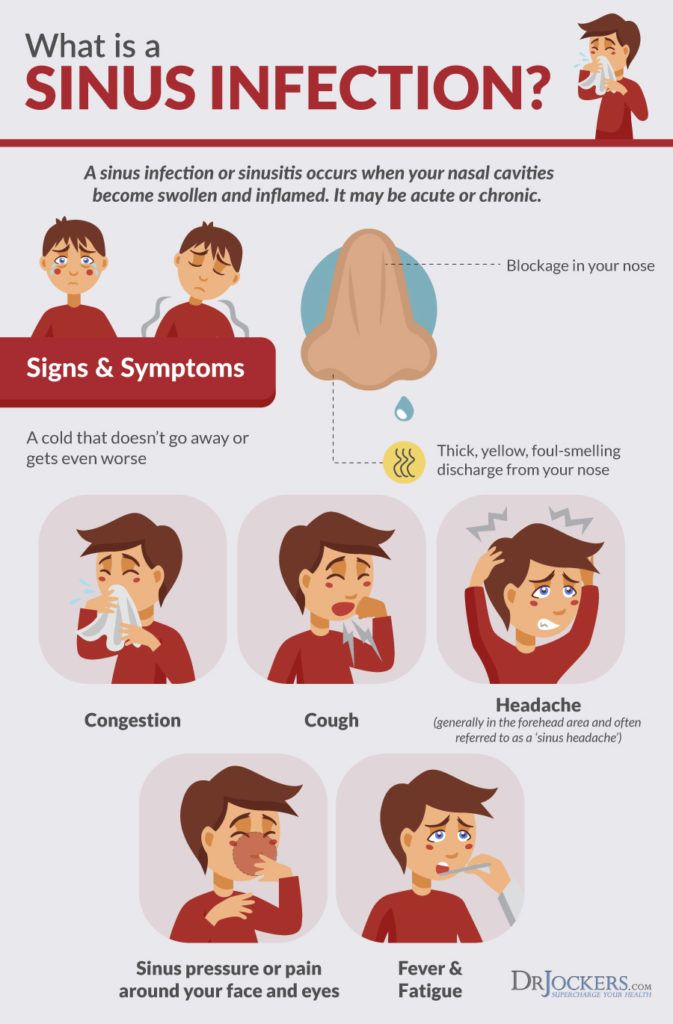 The American Academy of Pediatrics (AAP) encourages parents to discuss with their doctor whether to wait until the end or start taking antibiotics when symptoms are still relatively mild.
The American Academy of Pediatrics (AAP) encourages parents to discuss with their doctor whether to wait until the end or start taking antibiotics when symptoms are still relatively mild.
For years, antibiotics have been the first line of defense against ear infections, but doctors are now prescribing them more judiciously. Too much use of antibiotics is a problem as it can leave children vulnerable to antibiotic-resistant infections. nine0005
If your child is at least 6 months old, your doctor may recommend that you give him acetaminophen or ibuprofen for children to help relieve the pain caused by the infection. (Never give your child aspirin because it makes them more susceptible to Reye's syndrome, a rare but potentially fatal disease.)
Do not hesitate to call the doctor if your child gets worse or has not improved significantly after a few days. If your child does not feel better after 48 to 72 hours, the doctor may prescribe antibiotics and ask you to come back for a follow-up.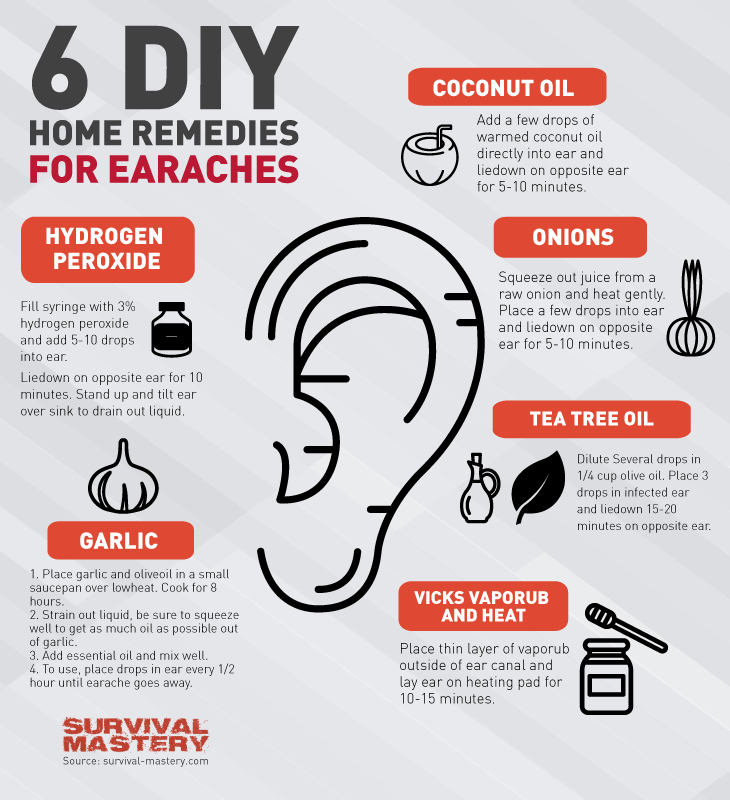 If your child is taking an antibiotic but does not improve after a few days, the doctor may want to change the medication or see your child again. nine0005
If your child is taking an antibiotic but does not improve after a few days, the doctor may want to change the medication or see your child again. nine0005
If your doctor prescribes antibiotics, be sure to give your child the full course. You may need to have another ear exam in a few weeks so the doctor can determine how well the medicine has worked.
How to prevent future ear infections
Ear infections are not contagious, but are often the result of respiratory infections. The best way to reduce the spread of germs is to wash your hands often—always after going to the bathroom, changing diapers, and before eating or preparing food. nine0005
You can also: Keep track of your child's vaccinations. Immunizations help prevent certain diseases that can lead to ear infections. For example, the pneumococcal conjugate vaccine has significantly reduced the number of ear infections in children. Studies show that because pneumococcal conjugate vaccine is included in the immunization schedule, the number of children aged 3 who have had at least one ear infection has been reduced by 20 percent.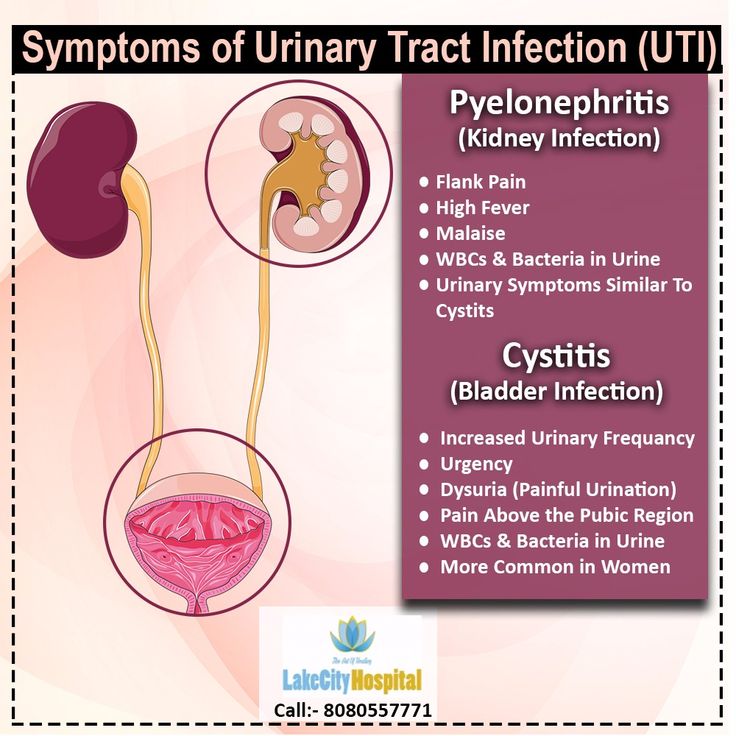 nine0005
nine0005
If your child has recurring ear infections, especially after flu attacks, talk to your doctor about whether your child should get an annual flu shot. (Only babies aged 6 months or older can get the flu shot.)
Breastfeed your baby for at least six months. A study by the US Centers for Disease Control and the Food and Drug Administration, published in the journal Pediatrics, found that babies who were breastfed for the first six months of life were less likely to develop ear infections. The risk of ear infections was actually 70 percent higher in formula fed babies. nine0005
Some doctors, including otolaryngologist Robert Reuben, believe that mothers pass certain immune antibodies to their babies through breast milk. However, these antibodies decrease after six months.
Keep your child away from tobacco smoke. Researchers have concluded that children whose parents smoke are more likely to get ear infections and have hearing problems.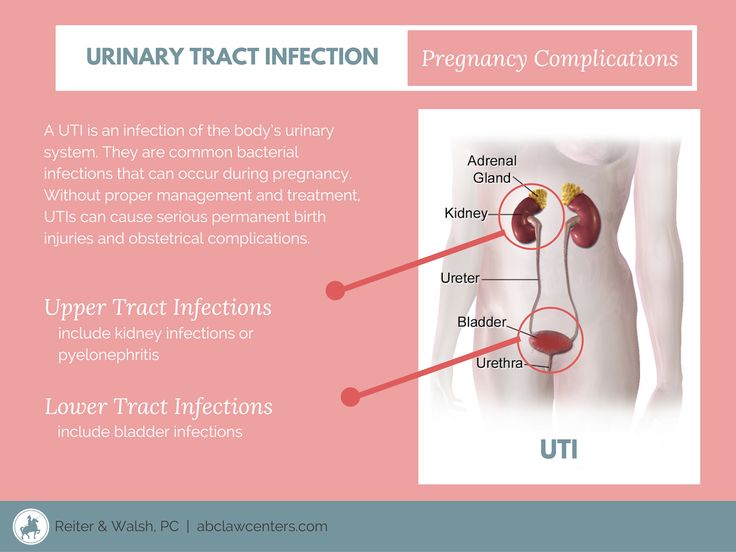
Children living with a smoker have a 37% higher risk of middle ear infections and hearing problems and a 62% higher risk if the mother is a smoker in the family. Children are also 86 percent more likely to have surgery for middle ear problems when their mothers smoke, compared to children who do not have a family history of smokers. nine0005
Even weekends spent in a home with a smoker can significantly harm a child and increase their chances of getting an ear infection. Tobacco smoke appears to suppress the immune system, making it harder for a child to fight infection. Do not allow people to smoke in your home, and keep your child away from smoke.
Can ear tubes help with repeated ear infections in children?
Children who get multiple ear infections—which can be a single ear infection that persists for months despite antibiotic treatment—are candidates for ear tubes. Approximately 670,000 children in the United States undergo this procedure each year.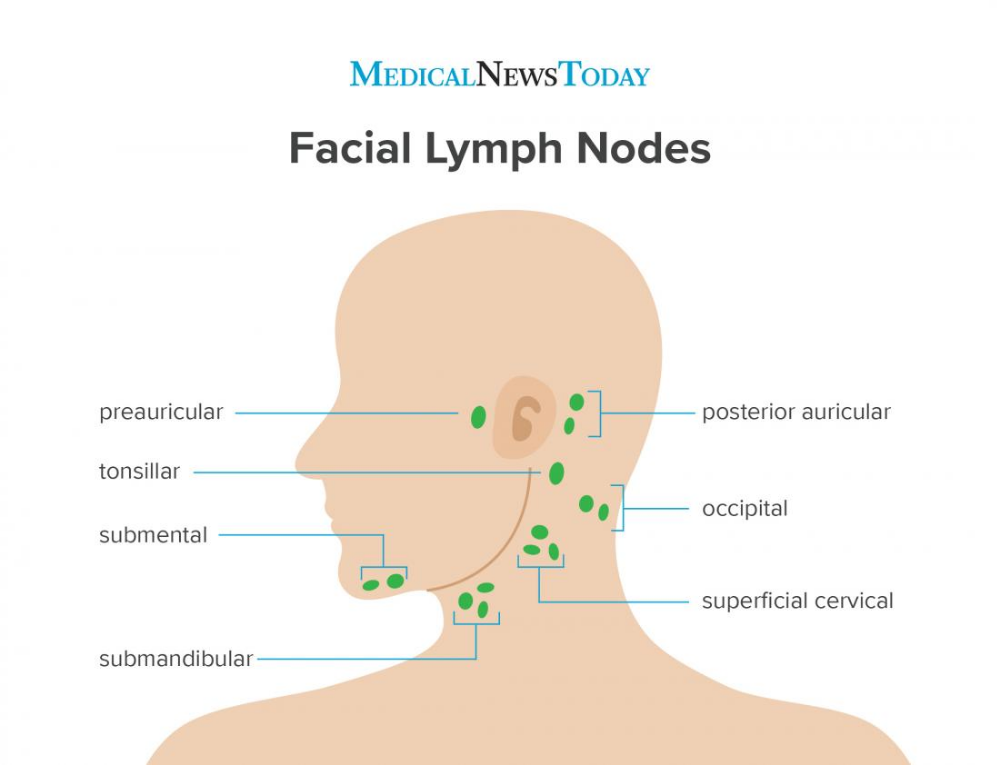 nine0005
nine0005
Ear tubes are inserted under general anesthesia. The otolaryngologist makes a small incision in the child's eardrum and inserts a small tube into the slot. The tube relieves pressure and acts as a vent, allowing air to flow in and out so bacteria cannot grow.
"This is an artificial Eustachian tube that allows the ear to 'breathe' until the real Eustachian tube returns to normal function," Reuben explains.
Your child's doctor may suggest this surgical solution because a child with persistent ear fluid is a prime candidate for repeated ear infections and hearing loss. nine0005
In addition, while studies are inconclusive, some experts suggest that hearing loss due to persistent fluid in the ears may lead to speech delays.
Reuben refers to a study that found that children with persistent hearing problems have some hearing problems later in life, especially when listening to speech in noisy environments such as classrooms.
"Furthermore," he says, "some of these children, especially those with developmental delays and those with certain language delays, are more prone to behavioral problems.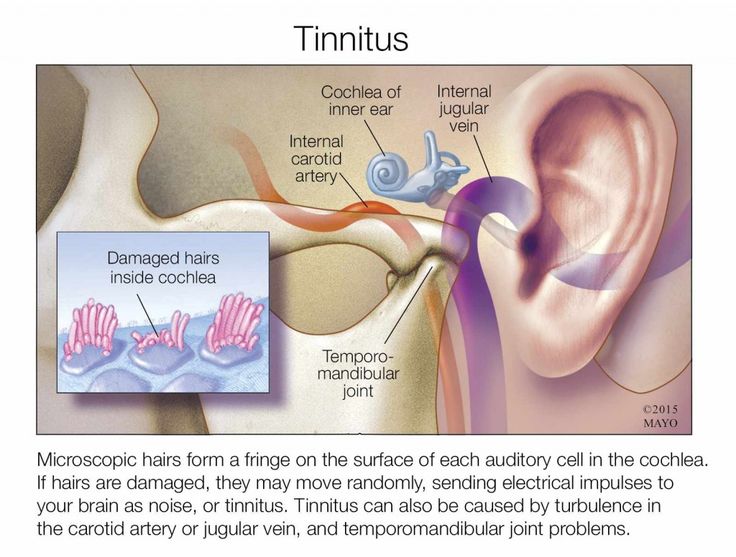 " Reuben says the length of time a child has hearing loss, as well as the degree of the impairment, are important factors. nine0005
" Reuben says the length of time a child has hearing loss, as well as the degree of the impairment, are important factors. nine0005
AAP recommends tubes for children with:
- Hearing loss above a certain level.
- Structural damage to the middle ear.
- Persistent middle ear infections or persistent fluid accumulation.
Talk to your child's doctor and weigh the pros and cons for you and your child.
How serious are ear infections in children?
They can be very serious. A severe or untreated infection can cause your child's eardrum to rupture. Tears don't happen very often and usually heal quickly, but it's important to check with your child's doctor to make sure the infection has cleared up and the eardrum is healing well. nine0005
Repeated ear infections can sometimes lead to hearing loss and scarring. And in very rare cases, untreated ear infections lead to mastoiditis (an infection of the skull behind the ear) or meningitis.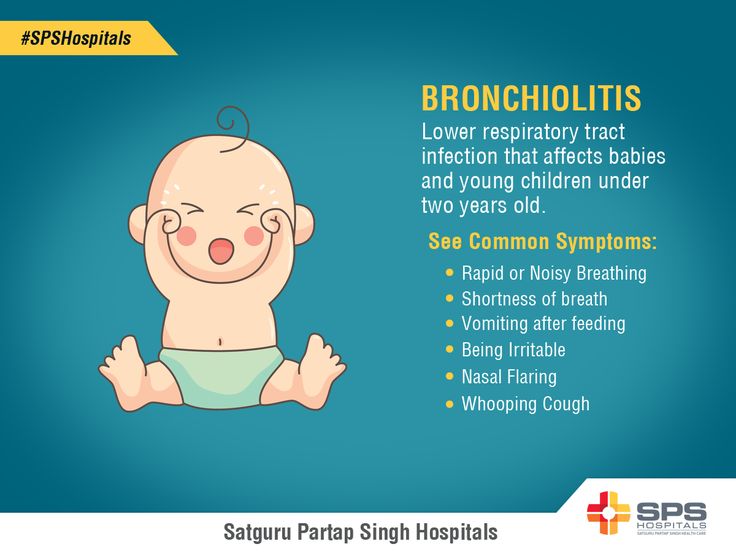
Different types of otitis - one danger!
The city advertising newspaper ARENA published No. 20 with an interview with an otorhinolaryngologist-surgeon of the highest category Novozhilov A.A.
Ear pain is one of the most severe types of pain known to man. And most often the cause of it becomes otitis. How to recognize otitis media in a small child in time? What complications are dangerous for otitis media, what remedies can provide first aid and which, on the contrary, can harm? When are ear drops a waste of time? nine0004
Alexey Aleksandrovich Novozhilov, leading otosurgeon, otorhinolaryngologist at the Alexandria multidisciplinary medical center, will answer questions.
- Hello, Alexey Alexandrovich. The first question concerns babies. How can parents tell if their child has earaches?
- It all depends on the age of the child. The younger the child, the more difficult it is to determine the cause of his anxiety. Children under one year of age have more pronounced general anxiety without local symptoms, sleep disturbance, screaming, loss of appetite. Sometimes the child stretches his hand to his ear, shrugs his shoulder on the affected side, a sudden start of the child may be observed. From 1 to 3 years old, if the child already knows how to talk or at least understands you, then he will be able to report his worries or show the place that worries him: touch, scratch. The ENT doctor will tell you exactly about the condition of your child's ears after the examination. nine0005
Children under one year of age have more pronounced general anxiety without local symptoms, sleep disturbance, screaming, loss of appetite. Sometimes the child stretches his hand to his ear, shrugs his shoulder on the affected side, a sudden start of the child may be observed. From 1 to 3 years old, if the child already knows how to talk or at least understands you, then he will be able to report his worries or show the place that worries him: touch, scratch. The ENT doctor will tell you exactly about the condition of your child's ears after the examination. nine0005
- Otitis externa, otitis media, internal - what's the difference?
- Our auditory analyzer consists of three sections: the outer ear (pinna, external auditory canal (to the tympanic membrane)), middle ear (tympanic cavity with ossicles), inner ear (labyrinth and cochlea). Otitis, depending on the localization, is accompanied by pain in the ear and ear area, fever, deterioration in general condition, and hearing loss.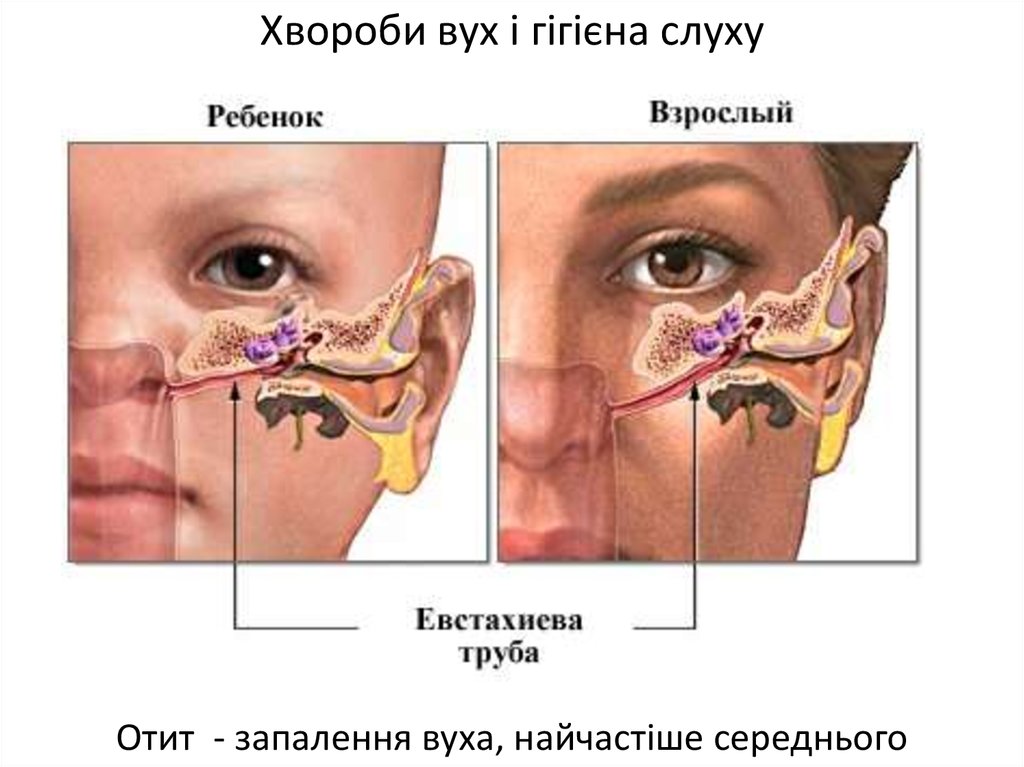 In severe cases, discharge from the ear, dizziness, problems with coordination are possible. Otitis externa is usually associated with improper ear hygiene, water entering the ears from public waterways when an infection is introduced into the ear canal, or injury from a foreign body. It is manifested by pain in the external auditory canal and ear area, a feeling of ear congestion, there may be discharge from the ear, fever. nine0005
In severe cases, discharge from the ear, dizziness, problems with coordination are possible. Otitis externa is usually associated with improper ear hygiene, water entering the ears from public waterways when an infection is introduced into the ear canal, or injury from a foreign body. It is manifested by pain in the external auditory canal and ear area, a feeling of ear congestion, there may be discharge from the ear, fever. nine0005
Up to 30% of ear diseases are due to otitis media. Most often, children under 5 years of age suffer from it due to the anatomical features of the structure of the ear (short and wide Eustachian tube, loose mucous membrane). Otitis media is divided into several subtypes depending on the degree of development of the inflammatory process (catarrhal, exudative, purulent). The patient has a feeling of ear congestion, tinnitus, hearing loss. In severe forms, there is a significant increase in body temperature, severe pain in the ear, headaches, general weakness, discharge from the ear (serous, purulent) is possible. nine0005
nine0005
As for inflammation of the inner ear, it occurs if otitis media is not treated. The infection penetrates the inner ear and provokes the development of labyrinthitis. In addition to pain, fever, patients experience imbalance, nausea, dizziness and vomiting.
- Exudative otitis - what is it and how to treat it?
- Otitis exudative is a non-purulent disease characterized by accumulation of exudate in the tympanic cavity. One of the causes of the disease is a violation of the ventilation function of the auditory tube, which leads to the appearance of negative pressure in the tympanic cavity. For diagnosis, otomicroscopy is performed - a study to determine the condition of the eardrum, audiometry - to determine the type and degree of hearing loss, as well as tympanometry - to determine the level of mobility of the membrane. The initial forms of exudative otitis are amenable to drug treatment. According to indications, physiotherapy, blowing of the auditory tube, antibacterial therapy is prescribed.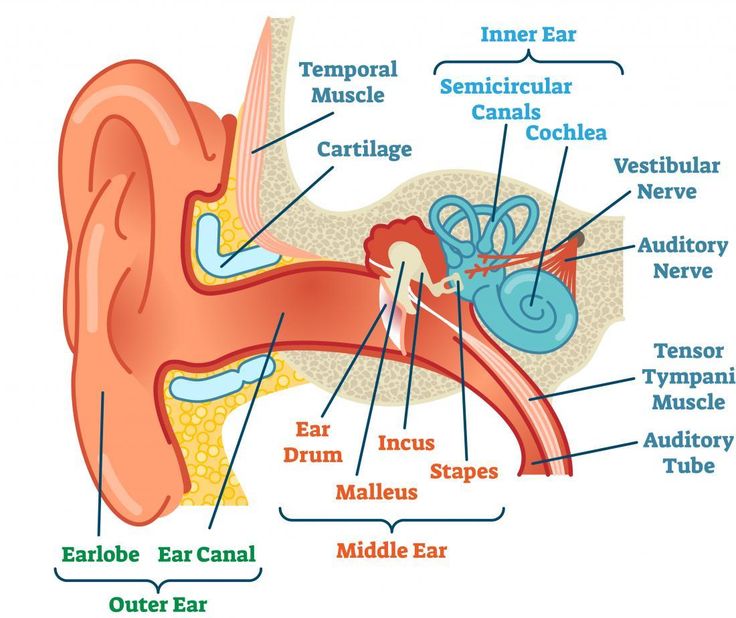 With a protracted course, severe hearing loss and no effect of therapy, surgical treatment is prescribed. Exudative otitis media is a very insidious disease, since, if left untreated, adhesions in the tympanic cavity may occur, persistent hearing loss may develop, and in the most advanced cases, deafness. The consequences of exudative otitis media can be adhesive otitis media. Both diseases often end in hearing loss. nine0005
With a protracted course, severe hearing loss and no effect of therapy, surgical treatment is prescribed. Exudative otitis media is a very insidious disease, since, if left untreated, adhesions in the tympanic cavity may occur, persistent hearing loss may develop, and in the most advanced cases, deafness. The consequences of exudative otitis media can be adhesive otitis media. Both diseases often end in hearing loss. nine0005
- Let's talk about first aid at home. What can not be done with otitis media?
- If you suspect otitis, you should definitely consult a doctor (preferably an ENT doctor). Only a doctor will be able to make a diagnosis and prescribe medication in accordance with the degree of complexity of otitis media. But it happens that the ears start to hurt unexpectedly: in the evening or at night, on a day off, on the road, in the country, when there is no way to quickly come to the reception. And the earache is unbearable. It is enough to take an anesthetic (nurofen, paracetamol) and drip vasoconstrictor drops (nazivin, xylene) into the nose. The compress will temporarily relieve pain, but will not cure. nine0003 You also need to remember that if there is discharge from the ear, then a warming compress is strictly prohibited!
The compress will temporarily relieve pain, but will not cure. nine0003 You also need to remember that if there is discharge from the ear, then a warming compress is strictly prohibited!
Do not clean the ears with a cotton swab or other objects, do not remove foreign objects from the ear on your own. Also, you can not interrupt the treatment until the period indicated by the doctor, despite the fact that the pain has passed. Untreated otitis media can become chronic and lead to partial or complete hearing loss.
- Can chronic otitis media be cured? nine0004
- Chronic otitis is an inflammatory process in the ear, which is associated with persistent perforation (hole) of the membrane. In the presence of a defect in the membrane, the infection freely penetrates into the middle ear. Chronic otitis is manifested by persistent hearing loss and periodic discharge from the ear. Chronic otitis must be treated without fail, with untimely treatment, it can lead to purulent complications - abscess, meningitis, sepsis, etc.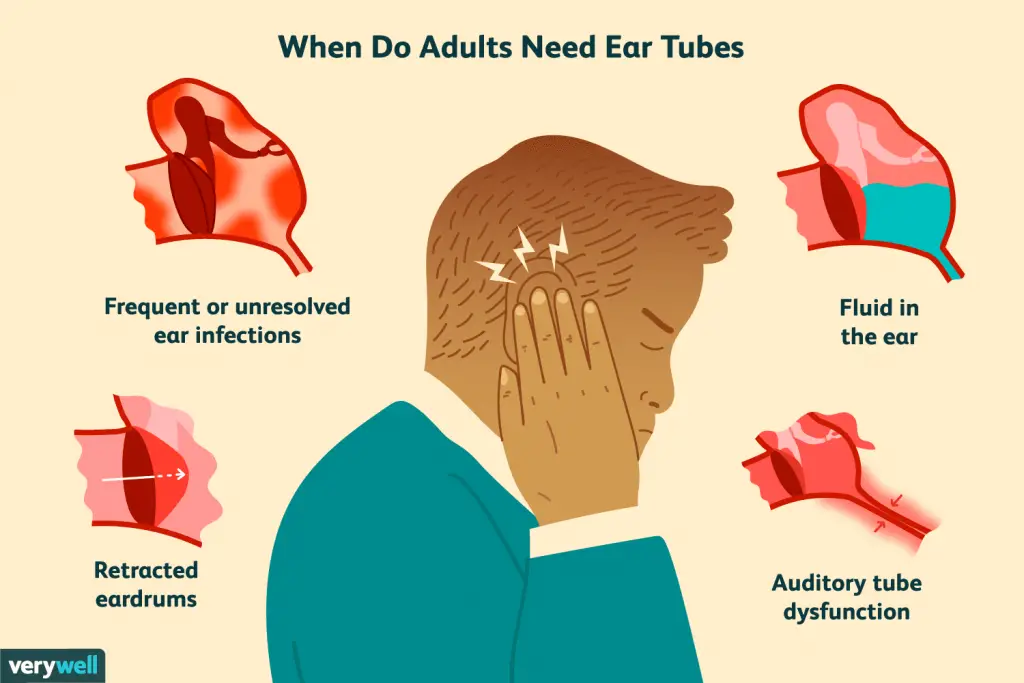 , since the focus of purulent inflammation is located very close to the brain, large vessels and nerves. Chronic otitis media leads to purulent exacerbations, hearing loss and significantly impairs the quality of life - you must constantly avoid getting water in the ear (when washing, bathing), you can not dive, any cold can lead to an exacerbation. If the membrane is damaged, exacerbations will continue. A simple perforation of the membrane causes periodic inflammation of the ear, over time this can damage the auditory nerve, which can no longer be restored. Chronic otitis media can be complicated by cholesteatoma, which destroys the middle and inner ear, can lead to paresis of the facial nerve, dizziness, complete deafness, and purulent intracranial complications. The use of drops is a way to relieve the exacerbation of otitis, to stop the discharge for a while. Sometimes, with hearing loss with the development of adhesions in the middle ear, impaired mobility of the auditory ossicles, patients install hearing aids to improve hearing.
, since the focus of purulent inflammation is located very close to the brain, large vessels and nerves. Chronic otitis media leads to purulent exacerbations, hearing loss and significantly impairs the quality of life - you must constantly avoid getting water in the ear (when washing, bathing), you can not dive, any cold can lead to an exacerbation. If the membrane is damaged, exacerbations will continue. A simple perforation of the membrane causes periodic inflammation of the ear, over time this can damage the auditory nerve, which can no longer be restored. Chronic otitis media can be complicated by cholesteatoma, which destroys the middle and inner ear, can lead to paresis of the facial nerve, dizziness, complete deafness, and purulent intracranial complications. The use of drops is a way to relieve the exacerbation of otitis, to stop the discharge for a while. Sometimes, with hearing loss with the development of adhesions in the middle ear, impaired mobility of the auditory ossicles, patients install hearing aids to improve hearing.