Vaginal muscle pain
Vaginal pain: Causes, symptoms, and treatment
Vaginal pain can be a temporary symptom of infection or injury. However, in some cases, it can be a chronic symptom with no known cause.
Persistent vaginal pain with no clear cause is called vulvodynia. It is a common gynecological condition that affects up to 16% of females in the United States.
Fear or embarrassment may keep a person from seeking professional treatment for vaginal pain. Anecdotal evidence suggests that some doctors can be quick to dismiss this symptom.
However, the right healthcare provider will work diligently to diagnose and treat the problem.
Read on to learn about the symptoms and causes of vaginal pain, as well as the treatment options.
A wide range of conditions can cause vaginal pain, but the following are the most common:
Infection
Yeast infections are among the most common causes of vaginal pain. About 75% of females develop a vaginal yeast infection at some point during their life.
A yeast infection can cause itching, burning, and, sometimes, a cottage cheese-like discharge from the vagina.
These infections do not usually spread through sexual intercourse, and most experts do not recommend treating sexual partners.
Bacterial vaginosis (BV) is also a common infection, particularly among people who are sexually active.
Although BV does not always cause symptoms, some people may experience the following symptoms in the vagina:
- pain
- itching
- burning
- a fishy odor
- discomfort during sex
Many people mistake the symptoms of BV for those of a yeast infection. However, the two have different causes and require different treatments.
Some other infections, especially chlamydia and gonorrhea — both of which are sexually transmitted infections (STIs) — can also cause pain and unusual discharge.
Physical trauma
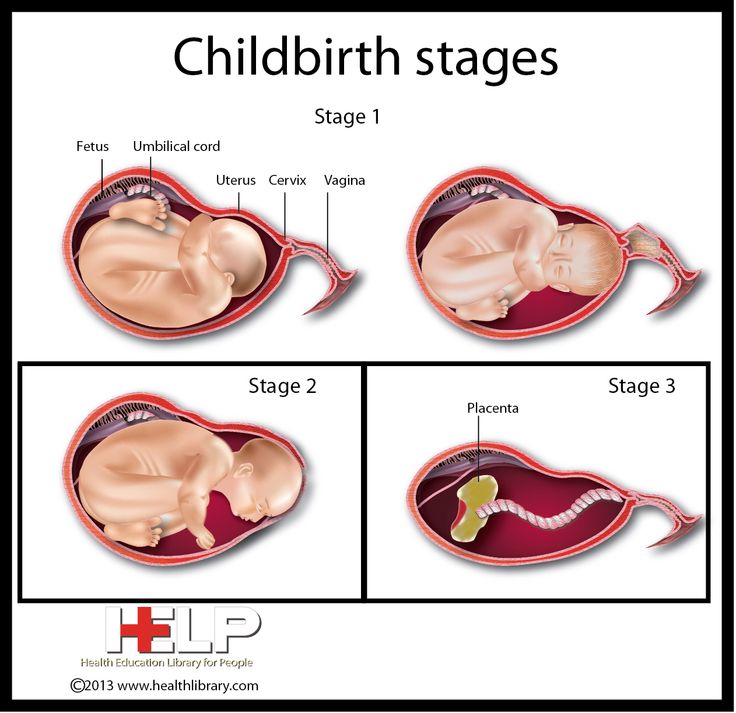
Physical injury to the vagina or vulva can cause vaginal pain. Relatively minor injuries, such as cuts from shaving, may sometimes be responsible, but one of the most common causes of injury and pain is childbirth.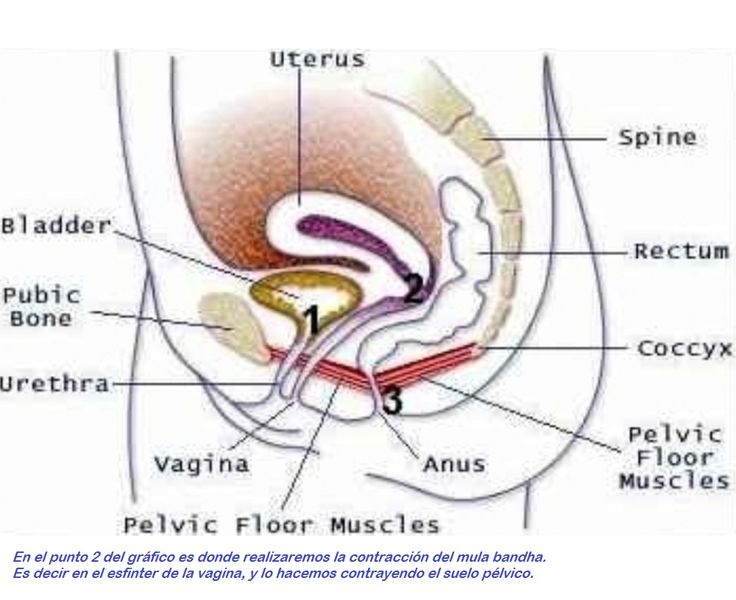
Giving birth causes vaginal tearing in most people during their first vaginal delivery. The tear usually extends into the perineum, which is the area between the vagina and anus. Doctors refer to this as a perineal tear. It is also possible for the clitoris or labia to tear during childbirth.
A doctor or midwife may need to stitch up serious tears. The stitches that they use will dissolve over time and do not require removal.
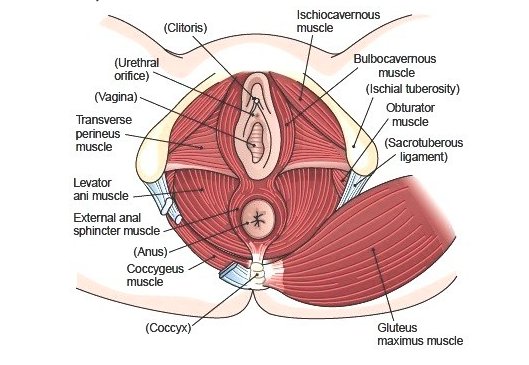
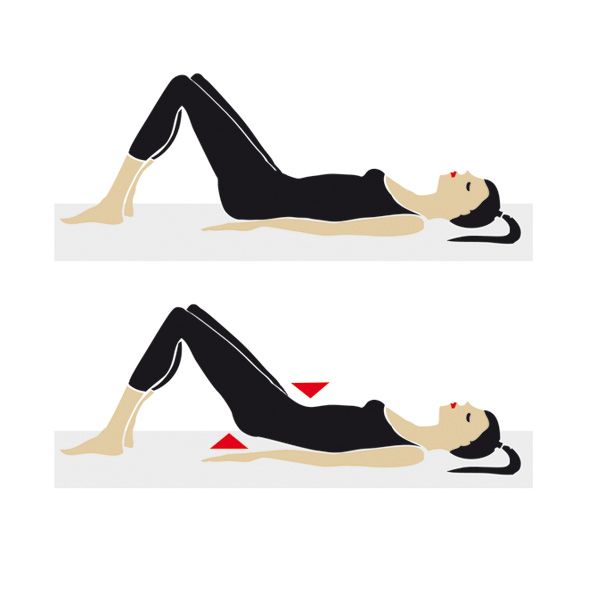
Pelvic floor dysfunction or injury
Damage to the muscles of the pelvic floor can cause pain in the vagina, stomach, and back, as well as affecting muscles in other areas.
Some factors that can increase the risk of pelvic floor problems include:
- age
- pregnancy
- injury from childbirth
- episiotomy, which is a surgical incision to enlarge the vaginal opening into the perineum during labor
Some people with pelvic floor dysfunction also experience incontinence, especially when sneezing or jumping. A person may also experience fecal incontinence, pain when passing stool, or both symptoms.
A person may also experience fecal incontinence, pain when passing stool, or both symptoms.
Vulvodynia
Vulvodynia is a type of chronic pain in the vulva, vagina, or both. The pain varies from person to person, but many report a burning pain that is fairly continuous, though sexual intercourse can trigger or worsen it.
Doctors do not fully understand vulvodynia and why it occurs. The diagnostic process can be lengthy because it involves excluding other causes of vaginal pain.
Anyone who suspects that they have vulvodynia should see a doctor, as various treatments are available.
Bartholin’s cyst
The Bartholin’s glands sit on either side of the entrance to the vagina and help lubricate it.
A blockage in one of these glands can give rise to a cyst, which may feel like a hard lump or look like a pimple. The cyst can cause pain, usually on one side of the vagina.
Bartholin’s cysts may get larger over several days before disappearing or rupturing. Sometimes, they become infected, causing intense pain.
Sometimes, they become infected, causing intense pain.
Vaginal pain can have many different characteristics. Describing the pain in detail can help a healthcare provider correctly diagnose the problem.
Below are the most common types of vaginal pain:
Burning
Vaginal yeast infections, BV, and other types of infection often cause a burning sensation, especially during or after intercourse.
Vulvodynia also often causes burning pain, though this typically occurs alongside other symptoms.
Itching
Itchiness is a classic sign of an infection, such as a yeast infection, BV, or an STI.
Less frequently, a pelvic floor injury causes nerve dysfunction that feels like itchiness or another unusual sensation.
Some people experience vaginal itchiness specifically during intercourse. Some possible causes of this include:
- vulvodynia
- the rupture of a Bartholin’s cyst
- healing following a physical injury
Tension or muscle spasms
Tightness, soreness, and muscle spasms in the vagina may indicate pelvic floor dysfunction. Some people also experience pain with different characteristics or in other areas — for example, they may have lower back pain or hip discomfort.
Some people also experience pain with different characteristics or in other areas — for example, they may have lower back pain or hip discomfort.
Vulvodynia can cause the vaginal muscles to tense before or during intercourse. Some people report that their muscles tense so forcefully that they are unable to have intercourse.
Tenderness or sensitivity
If the skin around the vagina and vulva feels painful, tender, or sensitive, this may be a symptom of a Bartholin’s cyst.
The area may also be discolored, and there may be a hard lump or visible swelling. If an infection develops, the pain may become intense.
Trauma to the vagina or vulva can also cause tenderness and sensitivity. Many people report soreness after giving birth, especially following a perineal tear.
Pain during intercourse
Intercourse can make any type of vaginal pain worse because friction causes irritation.
However, if a person only experiences vaginal pain during intercourse, vulvodynia may be the cause.
If a fishy odor follows painful intercourse, this could indicate BV.
A doctor can usually diagnose a vaginal yeast infection based on a person’s symptoms alone, though they may need to test a sample of discharge. This test will help the doctor rule out bacterial infections and STIs, such as gonorrhea and chlamydia.
The diagnostic process may also involve the doctor:
- performing a physical examination of the area to check for recent injuries
- carrying out an internal vaginal exam to check for muscle abnormalities, swelling, and irritation
- taking a comprehensive medical history, during which they are likely to ask about risk factors for specific vaginal health issues
People with vulvodynia do not typically have detectable symptoms of a physical disorder. Therefore, the doctor will need to rule out other causes of vaginal pain to arrive at this diagnosis.
The cause of the pain will determine the treatment options.
Antibiotics can treat gonorrhea, BV, chlamydia, and some other bacterial infections. Physical injuries, such as deep or infected wounds, may also require antibiotics.
Physical injuries, such as deep or infected wounds, may also require antibiotics.
As yeast is a fungus rather than a bacterium, antibiotics will not treat a yeast infection, and they may make it worse. Instead, the doctor may recommend an over-the-counter treatment or prescribe oral antifungal medication.
Bartholin’s cysts typically go away on their own, although warm compresses can speed this process. If a cyst grows very large, a doctor may surgically drain it. If a cyst becomes infected, it may require antibiotics.
Physical therapy may help with pelvic floor injuries, and the physical therapist can work with the person to develop a plan for strengthening the pelvic floor at home. Physical therapy may also help with vulvodynia.
Vulvodynia is notoriously difficult to treat. The right treatment varies from person to person, but it often includes a combination of:
- oral and topical pain medications
- nerve stimulation
- drugs called nerve blocks
- pelvic floor exercises
- sex therapy
- avoiding known triggers, where possible
Home remedies cannot treat bacterial vaginal infections, and trying these methods may give an infection time to get worse.
Anyone who suspects that they have a bacterial infection should see a doctor for a diagnosis and treatment.
However, certain home remedies may help with symptoms of other conditions. People may find that applying warm compresses to a Bartholin’s cyst several times a day reduces the time it takes to resolve.
Those with a vaginal tear can often ease the pain using a sitz bath, ice packs, numbing sprays, or a combination of these remedies.
Strategies for preventing some forms of vaginal pain include:
- wearing a condom during sex
- undergoing regular STI testing and asking all partners about their STI status
- changing out of clothes as soon as possible if they become wet or sweaty, as moisture provides an ideal environment for yeast
- asking a doctor or midwife about methods of preventing tears during childbirth, if pregnant
Vaginal pain may be temporary or chronic, and it can range from mild irritation to severe, debilitating pain.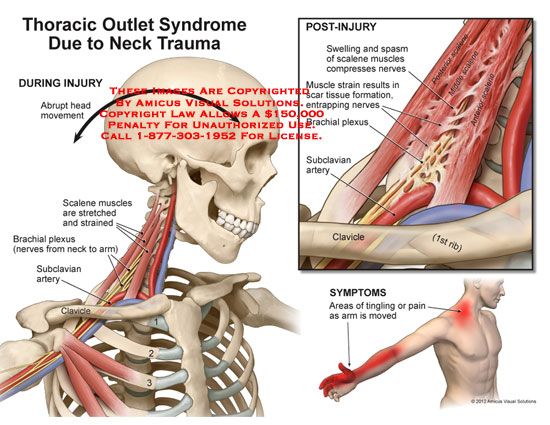 The feeling may result from infection, injury, or no identifiable cause.
The feeling may result from infection, injury, or no identifiable cause.
Anyone with vaginal pain should see a doctor or another healthcare provider for a diagnosis. Most often, vaginal pain goes away once a person finds the right treatment.
The cause of chronic vaginal pain can be difficult to diagnose. Typically, a healthcare provider will only diagnose vulvodynia after ruling out other possible causes of the pain. Although experts know little about the causes of vulvodynia, many treatments are available.
Some people have reported that healthcare providers can be unsympathetic about vaginal pain and unhelpful. If this is the case, it is important to ask for a second opinion from someone who specializes in this type of pain.
Vaginal pain: Causes, symptoms, and treatment
Vaginal pain can be a temporary symptom of infection or injury. However, in some cases, it can be a chronic symptom with no known cause.
Persistent vaginal pain with no clear cause is called vulvodynia. It is a common gynecological condition that affects up to 16% of females in the United States.
It is a common gynecological condition that affects up to 16% of females in the United States.
Fear or embarrassment may keep a person from seeking professional treatment for vaginal pain. Anecdotal evidence suggests that some doctors can be quick to dismiss this symptom.
However, the right healthcare provider will work diligently to diagnose and treat the problem.
Read on to learn about the symptoms and causes of vaginal pain, as well as the treatment options.
A wide range of conditions can cause vaginal pain, but the following are the most common:
Infection
Yeast infections are among the most common causes of vaginal pain. About 75% of females develop a vaginal yeast infection at some point during their life.
A yeast infection can cause itching, burning, and, sometimes, a cottage cheese-like discharge from the vagina.
These infections do not usually spread through sexual intercourse, and most experts do not recommend treating sexual partners.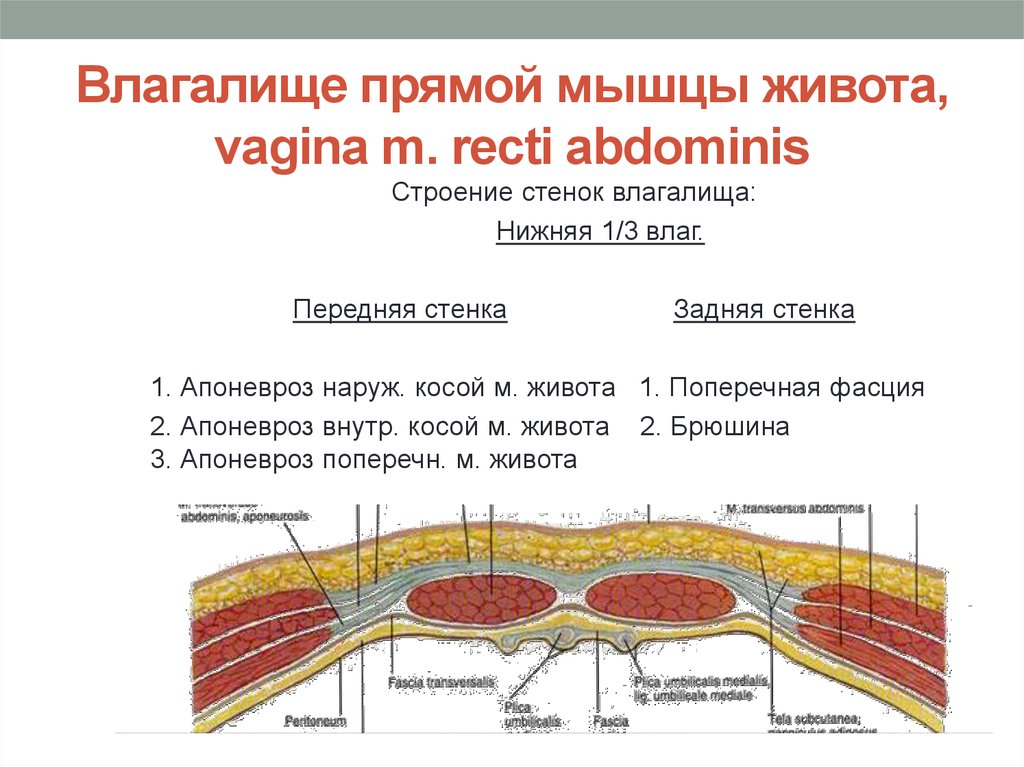
Bacterial vaginosis (BV) is also a common infection, particularly among people who are sexually active.
Although BV does not always cause symptoms, some people may experience the following symptoms in the vagina:
- pain
- itching
- burning
- a fishy odor
- discomfort during sex
Many people mistake the symptoms of BV for those of a yeast infection. However, the two have different causes and require different treatments.
Some other infections, especially chlamydia and gonorrhea — both of which are sexually transmitted infections (STIs) — can also cause pain and unusual discharge.
Physical trauma
Physical injury to the vagina or vulva can cause vaginal pain. Relatively minor injuries, such as cuts from shaving, may sometimes be responsible, but one of the most common causes of injury and pain is childbirth.
Giving birth causes vaginal tearing in most people during their first vaginal delivery. The tear usually extends into the perineum, which is the area between the vagina and anus. Doctors refer to this as a perineal tear. It is also possible for the clitoris or labia to tear during childbirth.
Doctors refer to this as a perineal tear. It is also possible for the clitoris or labia to tear during childbirth.
A doctor or midwife may need to stitch up serious tears. The stitches that they use will dissolve over time and do not require removal.
Pelvic floor dysfunction or injury
Damage to the muscles of the pelvic floor can cause pain in the vagina, stomach, and back, as well as affecting muscles in other areas.
Some factors that can increase the risk of pelvic floor problems include:
- age
- pregnancy
- injury from childbirth
- episiotomy, which is a surgical incision to enlarge the vaginal opening into the perineum during labor
Some people with pelvic floor dysfunction also experience incontinence, especially when sneezing or jumping. A person may also experience fecal incontinence, pain when passing stool, or both symptoms.
Vulvodynia
Vulvodynia is a type of chronic pain in the vulva, vagina, or both.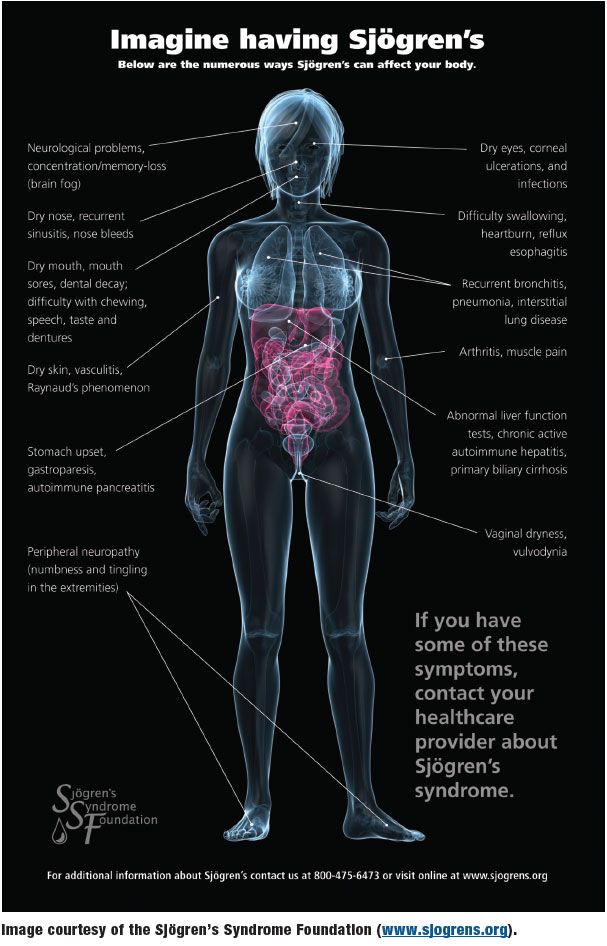 The pain varies from person to person, but many report a burning pain that is fairly continuous, though sexual intercourse can trigger or worsen it.
The pain varies from person to person, but many report a burning pain that is fairly continuous, though sexual intercourse can trigger or worsen it.
Doctors do not fully understand vulvodynia and why it occurs. The diagnostic process can be lengthy because it involves excluding other causes of vaginal pain.
Anyone who suspects that they have vulvodynia should see a doctor, as various treatments are available.
Bartholin’s cyst
The Bartholin’s glands sit on either side of the entrance to the vagina and help lubricate it.
A blockage in one of these glands can give rise to a cyst, which may feel like a hard lump or look like a pimple. The cyst can cause pain, usually on one side of the vagina.
Bartholin’s cysts may get larger over several days before disappearing or rupturing. Sometimes, they become infected, causing intense pain.
Vaginal pain can have many different characteristics. Describing the pain in detail can help a healthcare provider correctly diagnose the problem.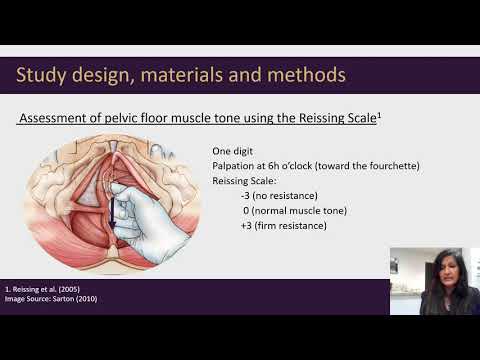
Below are the most common types of vaginal pain:
Burning
Vaginal yeast infections, BV, and other types of infection often cause a burning sensation, especially during or after intercourse.
Vulvodynia also often causes burning pain, though this typically occurs alongside other symptoms.
Itching
Itchiness is a classic sign of an infection, such as a yeast infection, BV, or an STI.
Less frequently, a pelvic floor injury causes nerve dysfunction that feels like itchiness or another unusual sensation.
Some people experience vaginal itchiness specifically during intercourse. Some possible causes of this include:
- vulvodynia
- the rupture of a Bartholin’s cyst
- healing following a physical injury
Tension or muscle spasms
Tightness, soreness, and muscle spasms in the vagina may indicate pelvic floor dysfunction. Some people also experience pain with different characteristics or in other areas — for example, they may have lower back pain or hip discomfort.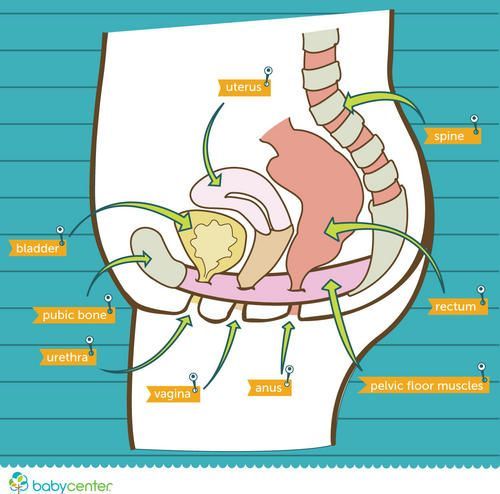
Vulvodynia can cause the vaginal muscles to tense before or during intercourse. Some people report that their muscles tense so forcefully that they are unable to have intercourse.
Tenderness or sensitivity
If the skin around the vagina and vulva feels painful, tender, or sensitive, this may be a symptom of a Bartholin’s cyst.
The area may also be discolored, and there may be a hard lump or visible swelling. If an infection develops, the pain may become intense.
Trauma to the vagina or vulva can also cause tenderness and sensitivity. Many people report soreness after giving birth, especially following a perineal tear.
Pain during intercourse
Intercourse can make any type of vaginal pain worse because friction causes irritation.
However, if a person only experiences vaginal pain during intercourse, vulvodynia may be the cause.
If a fishy odor follows painful intercourse, this could indicate BV.
A doctor can usually diagnose a vaginal yeast infection based on a person’s symptoms alone, though they may need to test a sample of discharge. This test will help the doctor rule out bacterial infections and STIs, such as gonorrhea and chlamydia.
This test will help the doctor rule out bacterial infections and STIs, such as gonorrhea and chlamydia.
The diagnostic process may also involve the doctor:
- performing a physical examination of the area to check for recent injuries
- carrying out an internal vaginal exam to check for muscle abnormalities, swelling, and irritation
- taking a comprehensive medical history, during which they are likely to ask about risk factors for specific vaginal health issues
People with vulvodynia do not typically have detectable symptoms of a physical disorder. Therefore, the doctor will need to rule out other causes of vaginal pain to arrive at this diagnosis.
The cause of the pain will determine the treatment options.
Antibiotics can treat gonorrhea, BV, chlamydia, and some other bacterial infections. Physical injuries, such as deep or infected wounds, may also require antibiotics.
As yeast is a fungus rather than a bacterium, antibiotics will not treat a yeast infection, and they may make it worse.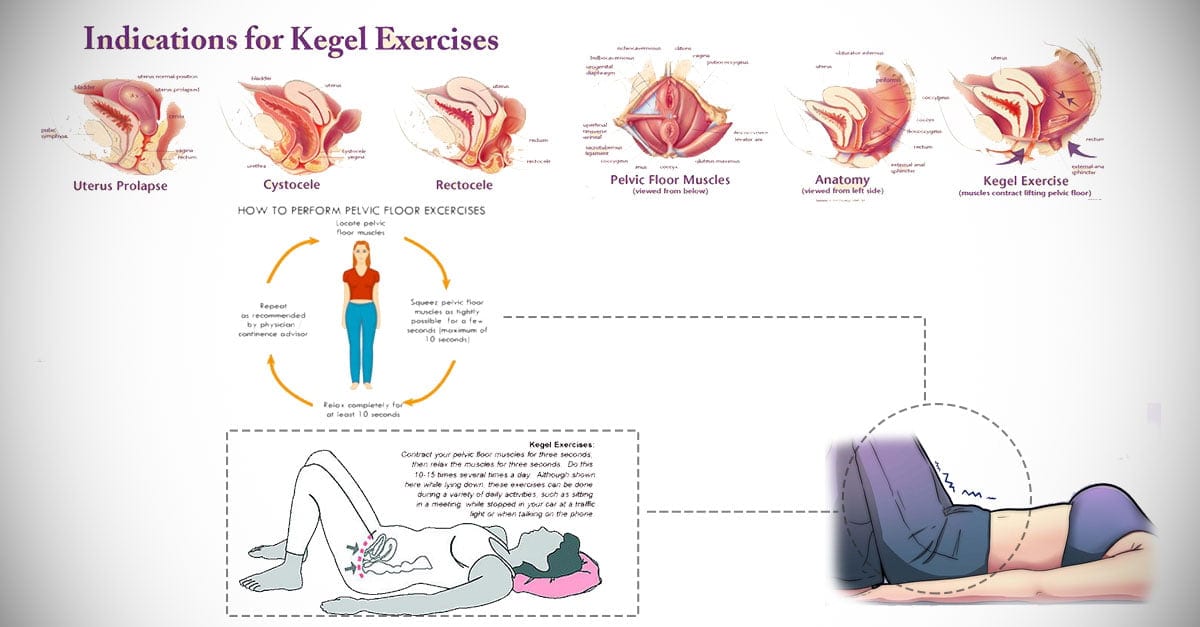 Instead, the doctor may recommend an over-the-counter treatment or prescribe oral antifungal medication.
Instead, the doctor may recommend an over-the-counter treatment or prescribe oral antifungal medication.
Bartholin’s cysts typically go away on their own, although warm compresses can speed this process. If a cyst grows very large, a doctor may surgically drain it. If a cyst becomes infected, it may require antibiotics.
Physical therapy may help with pelvic floor injuries, and the physical therapist can work with the person to develop a plan for strengthening the pelvic floor at home. Physical therapy may also help with vulvodynia.
Vulvodynia is notoriously difficult to treat. The right treatment varies from person to person, but it often includes a combination of:
- oral and topical pain medications
- nerve stimulation
- drugs called nerve blocks
- pelvic floor exercises
- sex therapy
- avoiding known triggers, where possible
Home remedies cannot treat bacterial vaginal infections, and trying these methods may give an infection time to get worse.
Anyone who suspects that they have a bacterial infection should see a doctor for a diagnosis and treatment.
However, certain home remedies may help with symptoms of other conditions. People may find that applying warm compresses to a Bartholin’s cyst several times a day reduces the time it takes to resolve.
Those with a vaginal tear can often ease the pain using a sitz bath, ice packs, numbing sprays, or a combination of these remedies.
Strategies for preventing some forms of vaginal pain include:
- wearing a condom during sex
- undergoing regular STI testing and asking all partners about their STI status
- changing out of clothes as soon as possible if they become wet or sweaty, as moisture provides an ideal environment for yeast
- asking a doctor or midwife about methods of preventing tears during childbirth, if pregnant
Vaginal pain may be temporary or chronic, and it can range from mild irritation to severe, debilitating pain. The feeling may result from infection, injury, or no identifiable cause.
The feeling may result from infection, injury, or no identifiable cause.
Anyone with vaginal pain should see a doctor or another healthcare provider for a diagnosis. Most often, vaginal pain goes away once a person finds the right treatment.
The cause of chronic vaginal pain can be difficult to diagnose. Typically, a healthcare provider will only diagnose vulvodynia after ruling out other possible causes of the pain. Although experts know little about the causes of vulvodynia, many treatments are available.
Some people have reported that healthcare providers can be unsympathetic about vaginal pain and unhelpful. If this is the case, it is important to ask for a second opinion from someone who specializes in this type of pain.
Pain during sexual intercourse - the causes of occurrence, in what diseases it occurs, diagnosis and methods of treatment
I confirm More
- INVITRO
- Library
- Symptoms
- Pain during intercourse
Vaginismus
nine0002 CandidiasisPapillomatosis
Cystitis
Endometriosis
Prostatitis
10693 03 June nine0003
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests.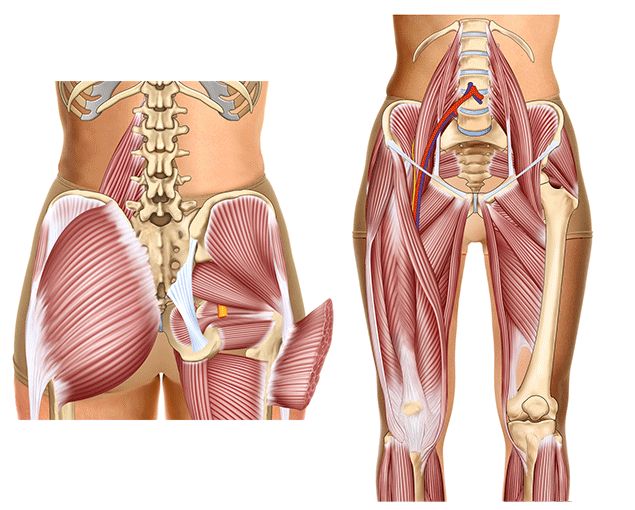 For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes. nine0003
Pain during intercourse: causes, diseases in which it develops, methods of diagnosis and treatment.
Definition
Pain and discomfort during intercourse (dyspareunia) refers to extremely unpleasant and painful sensations that occur in the genitals during coition. The reaction to this pain is so pronounced that it makes a person refuse sexual intercourse. Fear of pain causes muscle spasm, which does not allow you to enjoy intimacy, is accompanied by impaired blood circulation in the pelvic organs and dystrophic changes in tissues. nine0003
The vicious circle of psychogenic and organic changes largely determines the ineffectiveness of treatment when using only drug therapy.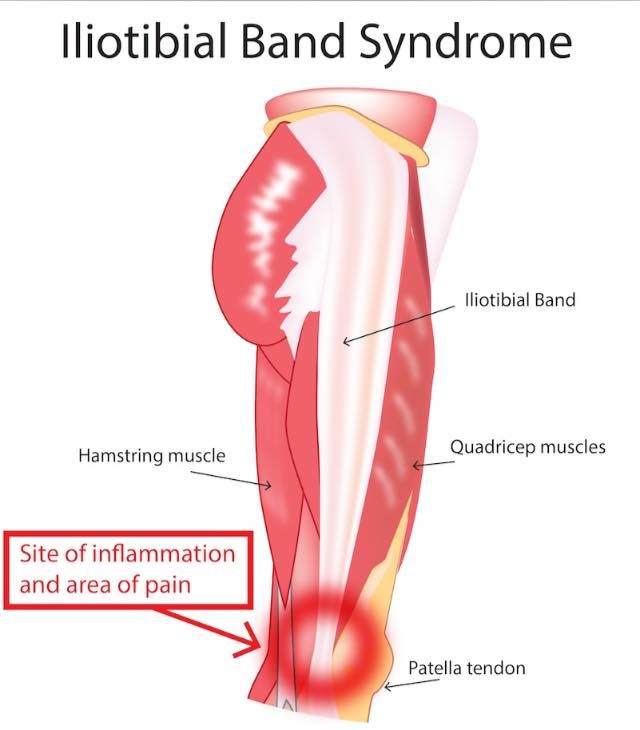
Types of pain during intercourse
Pain during intercourse can vary in intensity and character. Depending on the nature of the disease, moderate diffuse (diffuse) pain or a feeling of heaviness in the lower abdomen, a feeling of spasm, burning, itching may prevail. Rarely, widespread severe pain in the uterus or lower abdomen can be observed. nine0003
Pain is differentiated by localization (at the entrance to the vagina or deep pain in the uterus), time of occurrence (at the beginning of coition, during the active phase or after intercourse), situational (only with a certain partner or only in a certain position).
Regardless of the localization and nature of the pain, it is always accompanied by negative emotions, forcing fear and hostility towards sexual intercourse.
Possible causes of pain during intercourse
The international classification of diseases distinguishes two causes of pain syndrome - organic (associated with diseases of the genitourinary tract) and psychosomatic (the primary link is associated with a psychological disorder).
Organic dyspareunia in women
In women, the pain may be caused by vaginismus, or spasmodic contraction of the muscles in the vagina when the penis enters. The cause of vaginismus most often lies in a negative attitude towards sex, caused by previous stress, pain or rape. nine0003
Less commonly, dyspareunia occurs after trauma to the genital organs, childbirth, or pelvic surgery. According to statistics, more than a quarter of women experience pain after a caesarean section, as well as many nursing mothers.
Pain followed by contraction of the vaginal muscles can be caused by insufficient amount of lubricant (lubricant) in the absence of arousal at the beginning of sexual intercourse, as well as due to atrophy of the vaginal mucosa due to a decrease in estrogen (female sex hormone) levels in women during menopause. nine0003
A decrease in estrogen levels and dryness of the vaginal mucosa can be the result of chemotherapy and radiological therapy.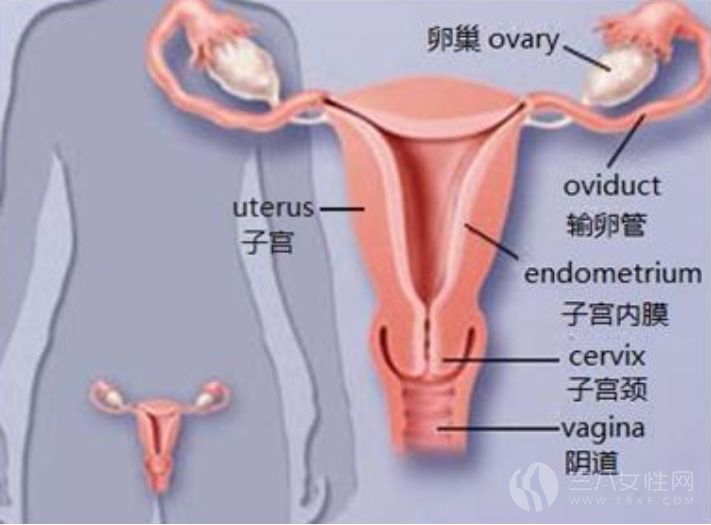
Inflammation of the mucous membrane of the vulva is associated with atrophic tissue changes due to impaired carbohydrate metabolism and estrogen deficiency. Diabetic vulvitis is characterized by the standard signs of inflammation - redness, swelling and pain during sexual intercourse.
Vulvodynia (vulvar vestibulitis) is also a common cause of dyspareunia, where pain occurs when the penis enters the vagina. This condition is explained by a multiple increase in the transmission of impulses from the receptors of the vagina to the brain. With such sensitivity, even a slight irritation is perceived by a woman as a strong and unbearable pain. Sometimes such pain can be provoked by vulvovaginal candidiasis and papillomatosis. nine0003
Painful intercourse is observed when there are pathological processes in the urethra and bladder. So, interstitial cystitis (painful bladder syndrome) in almost half of the cases is accompanied by dyspareunia, which makes women see a doctor.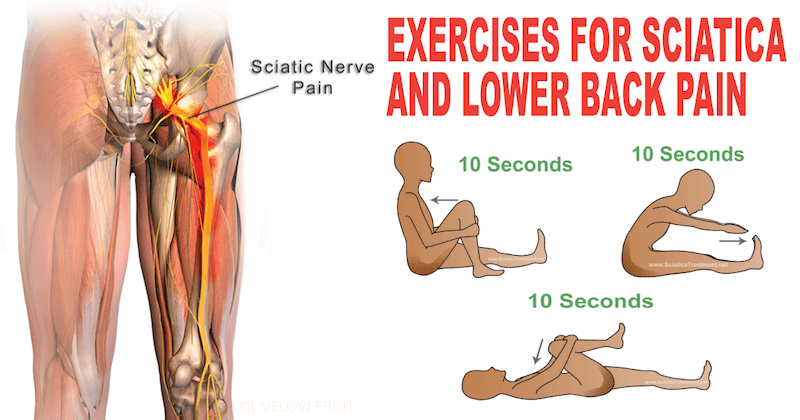 Pain in this case occurs not only during intercourse, but also when the bladder is full, and its peak occurs at the time of the urge to urinate.
Pain in this case occurs not only during intercourse, but also when the bladder is full, and its peak occurs at the time of the urge to urinate.
Pelvic pain, one of the manifestations of which is dyspareunia, is characterized by constant or cyclic painful, pulling sensations in the sacrum, lower back or lower abdomen. This condition may be due to both a gynecological disease and may not have an obvious organic basis. Most often, dyspareunia in the composition of pelvic pain occurs in patients with endometriosis, while they also complain of pelvic pain, dysmenorrhea (severe cyclic pain in the lower abdomen) and heavy menstruation. nine0003
Pelvic pain and dyspareunia sometimes occur with the pathological position of the uterus (uterus bend, retroversion of the uterus), weakening the tone of the pelvic floor.
Congestive and inflammatory changes in the pelvic organs lead to adhesive processes, which aggravates the pain syndrome.
Organic dyspareunia in men
In men, the most common causes of pain during intercourse are inflammatory diseases of the prostate and urethra.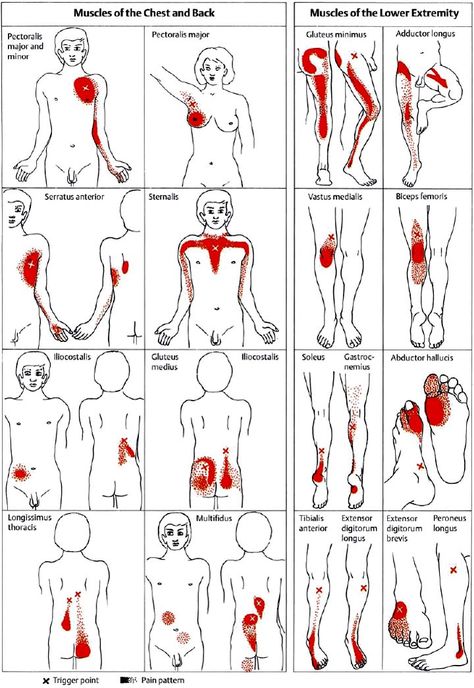 nine0003
nine0003
The pain usually occurs at the time of ejaculation. If the pain syndrome accompanies the moment of erection, it can be caused by inflammation or loss of elasticity of the foreskin.
Dyspareunia is often a symptom of urinary tract infections such as urogenital chlamydia. At the same time, there may be discharge from the urethra, painful urination, and symptoms of epididymitis (inflammatory disease of the epididymis) or prostatitis (inflammatory disease of the prostate gland). nine0003
Fibrous plaques in the albuginea and cavernous tissue of the penis in Peyronie's disease cause deformation of the penis during erection, which is accompanied by painful sensations during intercourse.
Psychosomatic dyspareunia
In addition to the organic nature, dyspareunia also has psychogenic causes: improper sexual education, psycho-emotional trauma, delayed psychosexual development, unfavorable beginning of sexual life. Often, patients have a history of gynecological and urological diseases that are characterized by a long course. Psychosomatic dyspareunia can also be accompanied by pathology of the genital organs, but their severity is low and most often represented by only minor changes. nine0003
Psychosomatic dyspareunia can also be accompanied by pathology of the genital organs, but their severity is low and most often represented by only minor changes. nine0003
Which doctors to contact for pain during intercourse
Dyspareunia combines a complex of problems, the solution of which can be provided by the joint work of doctors.
Typically, a woman who experiences pain during intercourse goes to a gynecologist, however, treatment without taking into account psychosomatic disorders may be ineffective, therefore it is recommended to include a sex therapist in therapy.
A man who experiences pain during intercourse should contact urologist. nine0003
Diagnosis and examination of pain during sexual intercourse
Diagnosis of the disease that caused dyspareunia is difficult and usually includes several stages.
First of all, a thorough medical history is needed, which allows you to identify not only the nature and location of pain, but also the time of its onset (from the very beginning of sexual activity, after childbirth or surgery, with the onset of menopause, etc. ). It is very important to assess psychosocial factors - stress during the first sexual intercourse, cases of unwanted sex, violence, dissatisfaction with family life, lack of libido. nine0003
). It is very important to assess psychosocial factors - stress during the first sexual intercourse, cases of unwanted sex, violence, dissatisfaction with family life, lack of libido. nine0003
After taking a history of women, an examination of the external genitalia is performed, which allows visualization of areas of redness, signs of candidiasis or vaginosis. The doctor also conducts a digital or bimanual (two-handed) examination, in particular, this is necessary to detect vaginismus and vulvodynia. If discharge is present, a Pap smear, wet-slide microscopy, and culture are required.
Culture of genital secretions for microflora, determination of sensitivity to antimicrobials and bacteriophages
Bacteriological examination of biomaterial for the purpose of isolating and identifying opportunistic pathogens - pathogens of nonspecific infectious...
Up to 6 business days
Available with home visit
RUB 1,565
Add to cart
If endometriosis is suspected, your doctor may order a colposcopy, ultrasound, magnetic resonance imaging, or computed tomography. nine0003
nine0003
Colposcopy
Examination to assess the condition of the mucous membrane of the vagina and cervix and diagnose pathological changes, including neoplasms in the early stages...
1,890 rubles Sign up
US examination of pelvic organs (uterus, adnexa)
Ultrasound scanning of the organs of the female reproductive system to assess the shape and size, as well as exclude pathology. nine0003
RUB 2,390 Sign up
MRI of the pelvis and external genitalia
RUB 8,740 Sign up
The diagnosis of "interstitial cystitis" is made sequentially after the exclusion of pathology from the bladder. Clinical and biochemical blood tests are required, as well as a blood test for antibodies to the herpes simplex virus, cytomegalovirus. nine0003
Clinical and biochemical blood tests are required, as well as a blood test for antibodies to the herpes simplex virus, cytomegalovirus. nine0003
Clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes)
Synonyms: Complete blood count, UAC. Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram. Brief description of the study Clinical blood test: general...
Up to 1 business day
Available with house call
RUB 810
Add to cart
Creatinine (in the blood) (Creatinine)
Synonyms: Blood test for creatinine; Serum creatinine; Serum creatinine, GFR estimate.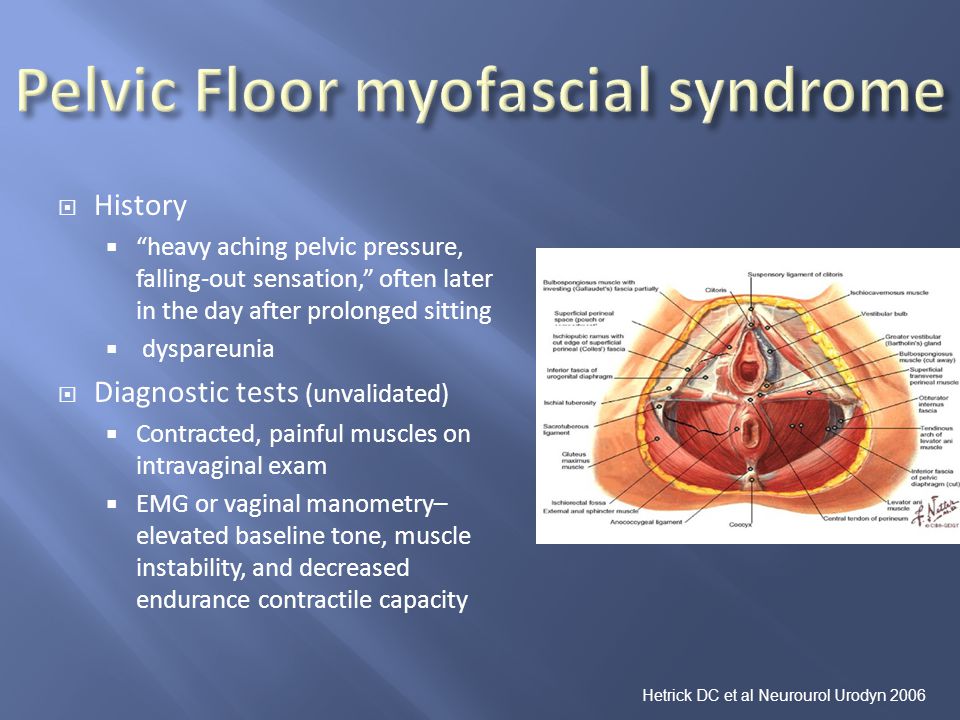 Creat; Cre; Blood Creatinine; Serum Creatinine; Serum Creat. Brief description of the definition ...
Creat; Cre; Blood Creatinine; Serum Creatinine; Serum Creat. Brief description of the definition ...
Up to 1 business day
Available with house call
370 RUB
Add to cart
Avidity of IgG antibodies to herpes simplex virus types 1 and 2
Herpes simplex virus (HSV) infection is part of a group of reproductively significant infections referred to as the TORCH complex Up to 5 working days
Available with home visit
830 RUB
Add to cart
Avidity of IgG antibodies to cytomegalovirus (anti-Cytomegalovirus avidity, anti-CMV-IgG avidity)
Cytomegalovirus infection is included in the group of reproductively significant infections, referred to as the TORCH complex (the name is formed by initial letters in Latin . ..
..
Up to 2 working days
Available with home visit
RUB 1,410
Add to cart
In addition, microscopic and bacteriological examination of urine, smears from the urethra and cervical canal, ultrasound examination of the kidney and bladder, as well as excretory urography, CT of the urinary tract and cystoscopy of the walls of the bladder are carried out. nine0003
General urinalysis (Urine analysis with sediment microscopy)
Method of determination Determination of physical and chemical parameters is carried out on an automatic analyzer using the "dry chemistry" method. Hardware microscope...
Up to 1 business day
Available with home visit
410 RUB nine0003
Add to cart
Urine Culture, Routine, quantitative.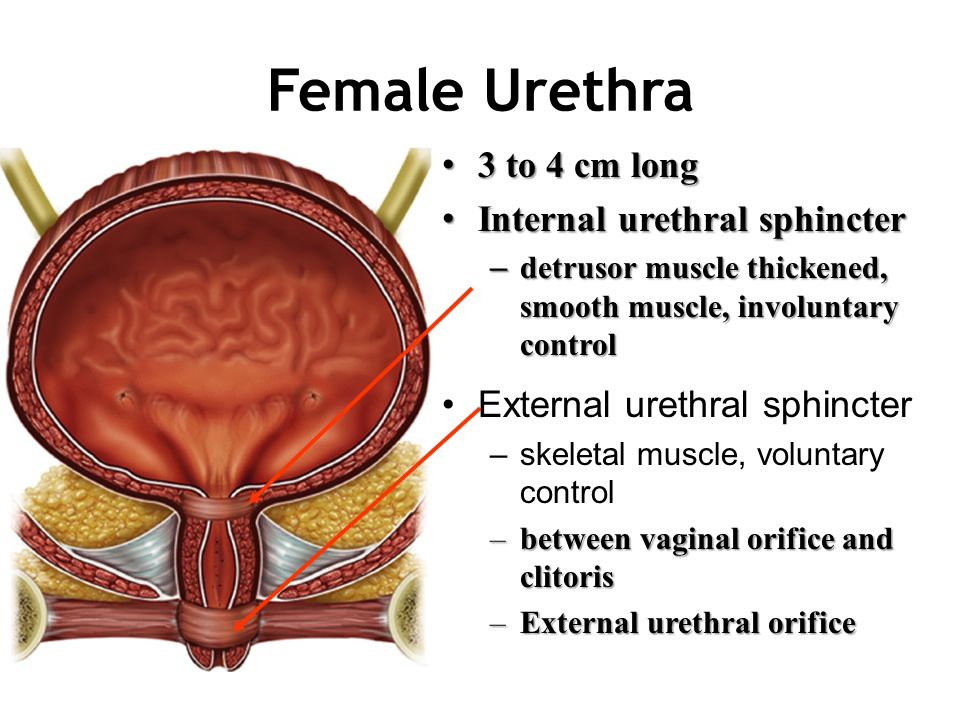 Aerobic Bacteria Identification. Antibiotic Susceptibility, enlarged testing
Aerobic Bacteria Identification. Antibiotic Susceptibility, enlarged testing
Synonyms: Urine Culture, Routine, quantitative. Aerobic Bacteria Identification. Antibiotic Susceptibility Enlarged Testing. Brief description of the study "Urine culture for microflora and determination of sensitive ...
Up to 6 business days
Available with home visit
2 300 RUB
Add to cart
Gram Stain. Bacterioscopic examination of different smears
Synonyms: Gram-stained smear analysis. Microscopic (bacterioscopic) examination of Gram-stained smear. Brief description of the study Microscopic examination of a smear, stained ...
Up to 2 working days
Available with home visit
RUB 685
Add to cart
Comprehensive ultrasound examination of the urinary system (kidneys, ureters, bladder)
Comprehensive ultrasound scan of the urinary system, which allows to detect pathology at an early stage of development.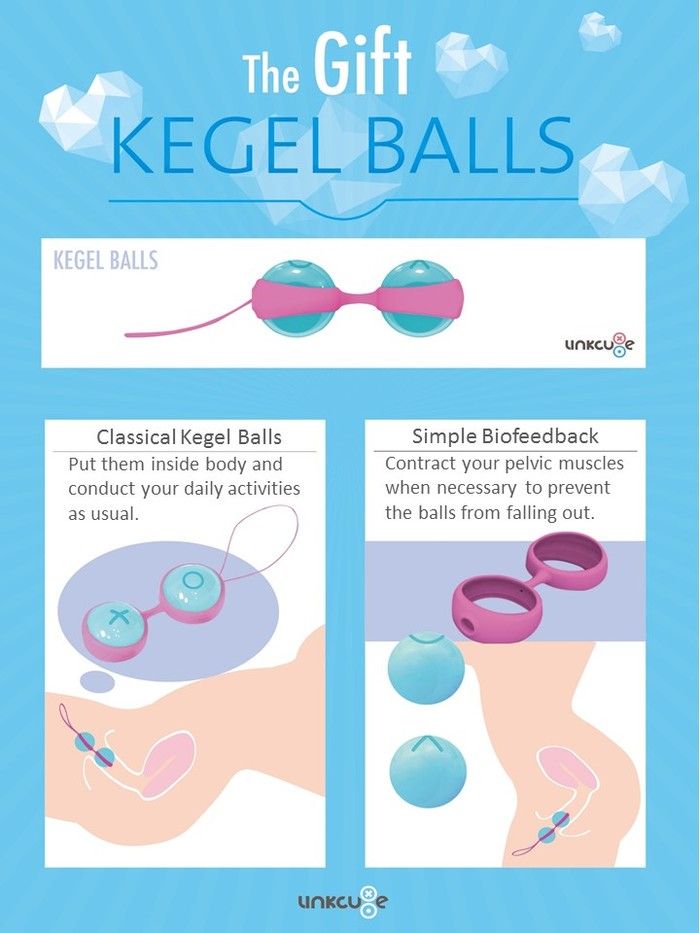 nine0003
nine0003
RUB 2,490 Sign up
Ultrasound of the bladder, determination of the volume of residual urine
Examination of the bladder to assess its structure and functional features.
RUB 2,040 Sign up
CT urinary tract
Method for assessing the state of the urinary system using computed tomography.
RUB 5,140 Sign up
For men with complaints of pain during intercourse, the doctor prescribes a study to determine the DNA of Chlamydia trachomatis in prostate secretion, ejaculate by polymerase chain reaction (PCR) with real-time detection in order to exclude urogenital chlamydia. nine0003
nine0003
Chlamydia, DNA determination (Chlamydia trachomatis, DNA) in prostate secretion, ejaculate
Determination of Chlamydia trachomatis DNA in prostate secretion, ejaculate by polymerase chain reaction (PCR) with real-time detection. Chlamydia (...
Up to 1 business day
Available with home visit
455 RUB nine0003
Add to cart
Diagnosis of prostatitis is carried out by examining the middle portion of urine in order to detect an increased content of leukocytes and pathogenic microorganisms. In addition, the level of prostate-specific antigen in the blood serum increases in a patient with prostatitis.
General urinalysis (Urine analysis with sediment microscopy)
Method of determination Determination of physical and chemical parameters is carried out on an automatic analyzer using the "dry chemistry" method.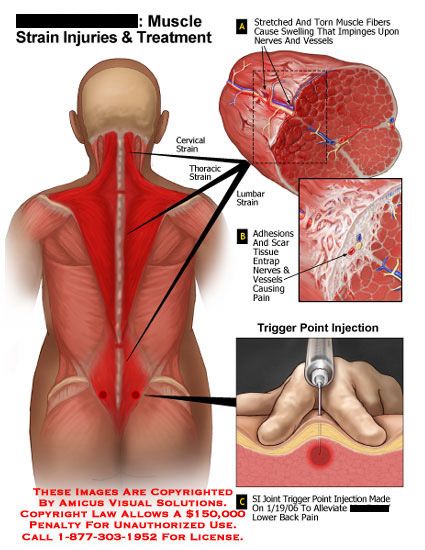 Hardware microscope...
Hardware microscope...
Up to 1 business day
Available with home visit
410 RUB
Add to cart
PSA total (Prostate-specific antigen total, PSA total)
Total PSA is a protein specific to prostate tissue used as a tumor marker. Physiological excretory product of the prostate ...
Up to 1 business day
Available with home visit
790 RUB
Add to cart
Treatment of conditions characterized by pain during intercourse
Organic dyspareunia requires treatment of the underlying gynecological or urological disease. If it is carried out correctly and in a timely manner, then the pain during intercourse disappears as it heals. However, organic pathologies often exist in parallel with psychological disorders - in these cases, as in psychosomatic dyspareunia, the psychotherapeutic help of a sex therapist is needed. nine0003
If it is carried out correctly and in a timely manner, then the pain during intercourse disappears as it heals. However, organic pathologies often exist in parallel with psychological disorders - in these cases, as in psychosomatic dyspareunia, the psychotherapeutic help of a sex therapist is needed. nine0003
An indication for sexological correction is the fear of sexual intercourse even after the elimination of the main organic cause of pain, decreased libido, and lack of orgasm.
What to do about pain during intercourse
Patients with dyspareunia are advised by doctors not to accumulate "pain" experience, which ultimately leads to irreversible organic and psychological changes.
Sources:
- Yarotskaya E.L. Pelvic pain in gynecology: modern approaches to the examination, treatment and rehabilitation of patients // Obstetrics and gynecology: Clinical recommendations. - No. 2, 2016. - 2. - P. 82–94.

- Clinical guidelines "Cystitis in women". Developed by: Russian Society of Urology. – 2021.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes. nine0003
Recommendations
-
Urine in urine
8128 January 16
-
Hypercalcemia
7917 11 January
-
Oliguria
7859 January 10
Show more
Menopause
Cervical cancer
nine0002 PregnancyPremenstrual syndrome (PMS)
Dysmenorrhea
Adnexitis
Endometritis
nine0002 SalpingitisEndometriosis
Ovarian cyst
Uterine fibroma
Heaviness in the lower abdomen
The abdomen is a concentration of vital organs that are located close to each other, which makes it difficult to determine the source of discomfort. Diagnosis of pathologies associated with pain and a feeling of heaviness in the lower abdomen is difficult. nine0003
Diagnosis of pathologies associated with pain and a feeling of heaviness in the lower abdomen is difficult. nine0003
More
Dysmenorrhea
Endometriosis
Myoma
PCOS
nine0002 TumorPainful menstruation
Painful menstruation (dysmenorrhea) is experienced by almost half of girls and women. For many of them, pain and discomfort lead to disability within 1-3 days. Clinicians do not attribute this condition to an independent disease, but associate it with a menstrual cycle disorder, which is manifested by cramping or pulling pains in the lower abdomen and in the lumbar region during menstrual bleeding.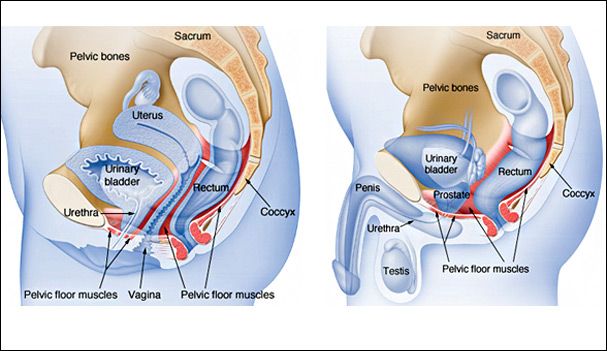 nine0003
nine0003
More
Hemorrhoids
Cystitis
Urethritis
Prostatitis
nine0002 OrchitisEpididymitis
Condyloma
Polyp
Varicose veins
Blood in semen
Blood in semen: causes, diseases, diagnosis and treatment.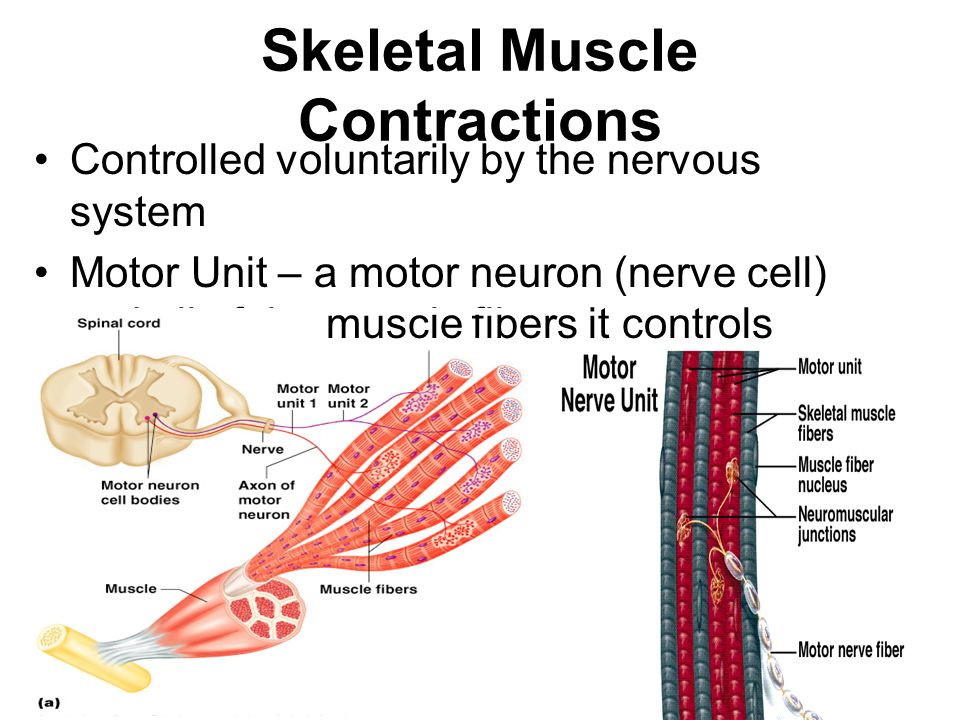 nine0003
nine0003
More
Pneumonia
Cough
Gastritis
Gastroduodenitis
nine0002 PyelonephritisCystitis
Prostatitis
Otitis
Conjunctivitis
Klebsiella
Klebsiella: causes of appearance, in which diseases it occurs, diagnosis and methods of treatment.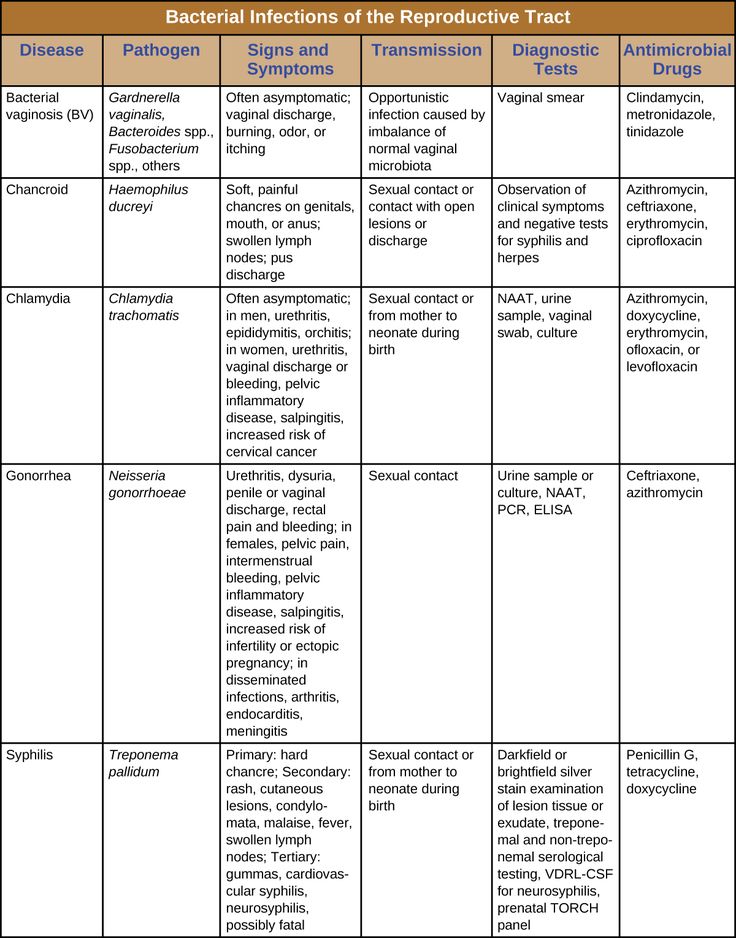 nine0003
nine0003
More
Fungus
Cystitis
Thrush
Colpitis
Flakes in urine
Flakes in the urine: the causes of occurrence, in what diseases they occur, diagnosis and methods of treatment.
More
Nothing found
Try changing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing your request or select medical office from list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Please try editing your query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Subscribe to our newsletters
nine0062Enter e-mail
I consent to processing of personal data
Subscribe
What can cause pain in the vagina? Featured Articles
Vaginal pain is a concern for many women, it occurs for various reasons and in some cases goes away on its own.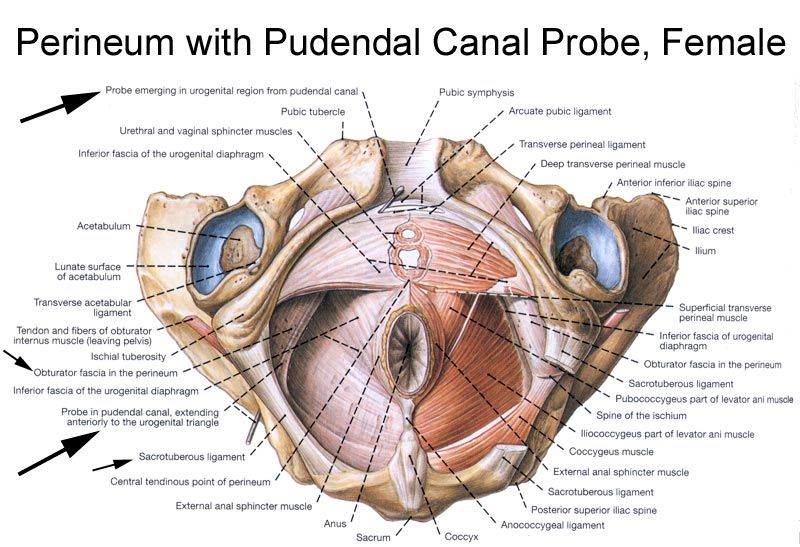 However, pain may indicate serious diseases that require treatment, so alarming symptoms should not be left unattended.
However, pain may indicate serious diseases that require treatment, so alarming symptoms should not be left unattended.
As a rule, the diagnosis of the cause of pain in the vagina is not difficult for an experienced doctor, but there is such a thing as vulvodynia: the presence of pain in the labia and vagina, the cause of which cannot be established. It is believed that if, after a complete examination, the cause of such pain is not found, its origin is associated with a neurogenic factor, as well as immune and genetic factors. nine0003
Pain is a protective reaction of the body in response to any stimuli.
Pain in the vagina can be as follows:
- associated or not associated with physical activity, sexual intercourse.
- intensity: varies from weak to strong.
- character: pulling, stabbing, cutting, blunt, sharp.
- duration: acute, chronic.
- persistence: constant, intermittent, recurrent. nine0006
- accompanying symptoms: vaginal discharge, itching, burning.

What are the possible causes of pain in the vagina?
- inflammatory diseases of the genital organs, in particular those caused by genital infections. Colpitis (inflammation of the vaginal mucosa) is manifested by pain in the vagina, burning and itching during and after intercourse, yellowish discharge with an unpleasant odor. Colpitis can be caused by both specific (gonococci, Trichomonas, chlamydia) and non-specific flora (streptococci, staphylococci, E. coli). Colpitis can turn into cervicitis (inflammation of the cervical mucosa), metritis and endometritis (inflammation of the uterus), adnexitis (inflammation of the uterine appendages). nine0006
- vaginal candidiasis (thrush). It is provoked by such conditions as reduced immunity, taking antibiotics, wearing tight and narrow underwear, poor hygiene, endocrine diseases (diabetes mellitus), malnutrition (eating fatty, spicy, smoked foods).
- inflammation of the Bartholin's gland. Bartholin's glands are located in the vestibule of the vagina, produce mucus to moisturize the vulva and the entrance to the vagina.
 Inflammation of the glands is more often unilateral, characterized by stabbing pains during movement, during intercourse. nine0006
Inflammation of the glands is more often unilateral, characterized by stabbing pains during movement, during intercourse. nine0006 - endometriosis. This condition causes soreness in the vagina, especially during sexual intercourse. After contact, bleeding from the vagina and pulling pain in the lower abdomen are possible.
- Vulvar kraurosis: in older women, this condition is often characterized by thinning of the skin of the external genital organs. Due to a lack of hormones, the skin becomes easily vulnerable, injured even when it comes into contact with underwear, and itches.
- injuries, foreign bodies in the vagina. nine0006
- dryness of the mucous membrane during menopause. Due to impaired functioning of the ovaries and lack of estrogen, dryness of the vaginal mucosa occurs, which causes pain that is aggravated during intercourse.
- medical manipulations (therapeutic and diagnostic). Pain syndrome often occurs after hysteroscopy, the installation of an intrauterine device.
- various anomalies in the development of the vagina. nine0011 benign neoplasms (fibromas, fibromyomas) of the vagina often cause pain during examination and during sexual intercourse, malignant neoplasms are manifested by pain, but more often in the later stages.
- acute surgical pathology: ovarian apoplexy. This is a hemorrhage in the ovary due to rupture of the cyst or vessels of the follicle. Apoplexy is accompanied by hemorrhage into the abdominal cavity. This condition is provoked by injuries, douching of the vagina, aggressive sex. The general condition of the woman is deteriorating, she is worried about weakness, severe abdominal pain, nausea and vomiting are possible. Apoplexy requires urgent surgical treatment. nine0006
- prolapse of the body of the uterus (complete, incomplete), prolapse of the walls of the vagina. They are more common in women over 45 years of age. Simultaneously with pulling pains, urinary and fecal incontinence is noted.