Hip dysplasia pavlik harness
Pavlik Harness Treatment for Children
What is Pavlik harness treatment for children?
The Pavlik harness is a soft splint. It is most commonly used for treating infants with developmental dysplasia of the hip (DDH). It helps keep the infant's hips and knees bent and the thighs spread apart. It can also help promote healing in babies with broken thighbones (femurs).
DDH occurs when the hip joint does not form normally. The hip joint is a ball-and-socket joint. The socket is a cup-shaped structure in the pelvis called the acetabulum. The ball, or head, is the rounded upper end of the femur. In DDH, the cup-shaped cavity of the acetabulum is more shallow than normal. As a result, the head of the femur does not fit into it well. The femoral head may slide partially out of the socket (sublux). In severe DDH, the head of the femur can slide completely out of the socket (dislocate). It may stay dislocated.
Strong fibrous tissues called ligaments normally help hold the femoral head in the acetabulum. In DDH, the ligaments may become stretched and loose.
By holding your baby's legs out and bent, the Pavlik harness helps keep the femoral heads in their sockets. It allows the ligaments to tighten. It encourages normal development of the acetabulum.
Why might my child need a Pavlik harness treatment?
It is normal for the hips of infants to be a bit loose. But this usually resolves on its own. It is particularly common in babies who were born feet or bottom first (breech). If their hips are too loose, they can sublux or dislocate easily. They may need treatment.
If your healthcare provider has concerns about possible DDH, he or she may recommend that your baby go to an orthopedist for evaluation. Sometimes the evaluation can involve an ultrasound of the baby's hips. If your baby has DDH, the orthopedist will probably recommend a device such as a Pavlik harness to encourage your baby's hips to develop normally.
Girls and breech babies have the highest risk for DDH. It also runs in some families. It is more common in first-born babies.
It also runs in some families. It is more common in first-born babies.
Healthcare providers sometimes use a Pavlik harness for femur fractures in infants younger than 6 months. The harness helps hold the baby's leg still so that the bone can heal.
What are the risks of Pavlik harness treatment for a child?
Pavlik harness treatment is usually successful in treating DDH. But sometimes complications can occur. They may include:
- Skin breakdown (dermatitis), especially in the groin, behind the knee, on the shoulder, or on the leg
- Lack of treatment success
- Nerve damage in the leg or shoulder
- Bone breakdown because of decreased blood supply (avascular necrosis)
- Flattening of the back of the femoral head
- Downward dislocation of the hip
- Subluxation of the knee
The most common complication is skin problems. You can reduce the risk for these skin problems by keeping all appointments and having the straps of the harness adjusted by the orthopedist as needed. Only the orthopedist should adjust the straps. You should keep your baby’s skin clean and dry. Don’t use lotions, ointments, or powders under the harness. If nerve problems develop, they typically go away on their own. If the Pavlik harness is not successful, your child may need a rigid brace instead.
You can reduce the risk for these skin problems by keeping all appointments and having the straps of the harness adjusted by the orthopedist as needed. Only the orthopedist should adjust the straps. You should keep your baby’s skin clean and dry. Don’t use lotions, ointments, or powders under the harness. If nerve problems develop, they typically go away on their own. If the Pavlik harness is not successful, your child may need a rigid brace instead.
How do I help my child get ready for Pavlik harness treatment?
You should not need to do much to prepare for your child's Pavlik harness treatment. Your baby may need to wear the harness for several months. During this time, it will be important to keep your baby's skin clean and dry. That will include changing diapers often. Consider stocking up on leak-proof diapers. Also ask what type of clothes to bring when you take your baby in for the first fitting. Your baby will need regular follow-up visits for harness adjustments and monitoring as he or she continues to grow.
What happens during Pavlik harness treatment for a child?
The Pavlik harness is a soft splint with a number of straps that fasten. It consists of a chest strap and leg straps. The chest strap goes across the baby's back and reaches around to close in the front. The leg straps attach to the front of the body strap, loop under each foot, cross over in the back, and attach to the top of the body strap. Each leg strap has two additional straps that wrap around the lower leg. The harness helps support the baby's legs in a bent, outward-rotated position. It prevents the baby from straightening his or her legs. It makes it hard for the baby to bring his or her legs together.
At first you should keep your baby in the harness all the time. You will learn how to put on your baby's clothes without taking off the harness. You will also learn how to change your baby's diaper in the harness. You may need to give your baby sponge baths with the harness on instead of full baths with the harness temporarily off. You will need to make sure to dry your baby well after bathing and after diaper changes.
You will need to make sure to dry your baby well after bathing and after diaper changes.
The harness is adjustable, so it can change as your baby grows. You will need to visit your baby's orthopedist regularly for adjustments. It is very important to have your baby's legs positioned correctly. Only allow the healthcare provider to make the adjustments. Do not try to adjust the harness yourself.
Your baby will also need regular ultrasounds to follow development of the hip joint. If the harness does not seem to be working within about 3 weeks, your baby's orthopedist may recommend using a cast or having surgery instead.
The orthopedist will tell you when you can take your baby out of the harness. After about 6 weeks, you will be able to take your baby out of the harness during the day. The baby will need to continue wearing the harness at night for about 6 more weeks.
What happens after Pavlik harness treatment for a child?
Most children have normal hip development after Pavlik harness treatment.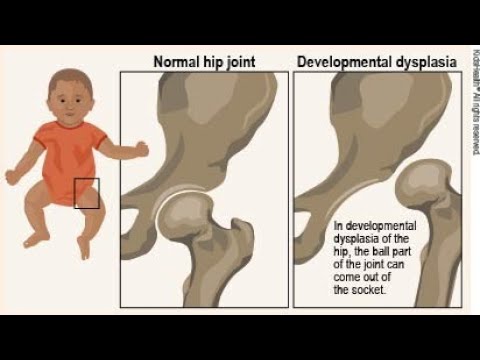 It is important to continue follow-up as recommended by your child's orthopedist. Follow any instructions your child's orthopedist gives you. If your child has problems walking or seems to be in pain, he or she may need more treatment. Your child may need follow-up exams and imaging tests such as ultrasound or X-ray. Talk with your child's orthopedist about other signs to watch for. Ask when you should bring your child in for evaluation.
It is important to continue follow-up as recommended by your child's orthopedist. Follow any instructions your child's orthopedist gives you. If your child has problems walking or seems to be in pain, he or she may need more treatment. Your child may need follow-up exams and imaging tests such as ultrasound or X-ray. Talk with your child's orthopedist about other signs to watch for. Ask when you should bring your child in for evaluation.
Next steps
Before you agree to the test or the procedure for your child make sure you know:
- The name of the test or procedure
- The reason your child is having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- When and where your child is to have the test or procedure
- Who will do the procedure and what that person’s qualifications are
- What would happen if your child did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or your child has problems
- How much will you have to pay for the test or procedure
Kids Health Information : Pavlik Harness for DDH
Developmental dysplasia (or dislocation) of the hip (DDH) is an abnormal development of the hip joint.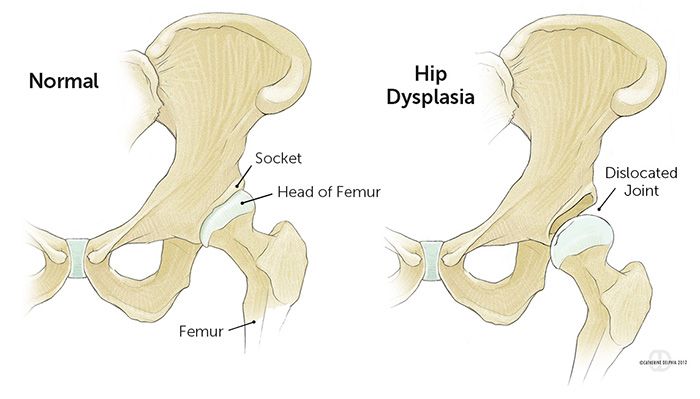 In DDH, the ball at the top of the thigh bone is not stable within the hip socket and the ligaments of the hip joint may also be stretched and loose. See our
Developmental dysplasia of the hip fact sheet for more information.
In DDH, the ball at the top of the thigh bone is not stable within the hip socket and the ligaments of the hip joint may also be stretched and loose. See our
Developmental dysplasia of the hip fact sheet for more information.
Babies with DDH often need to wear a brace. The Pavlik Harness is one type of brace used to treat DDH. It has straps that are fastened around the baby's legs and held up by shoulder and chest straps. This holds the hips and knees up with the legs apart. This is the best position for the hip joint to be in. It allows contact between the thigh and hip bones and helps strengthen the muscles and ligaments while the hip is developing.
Your doctor will let you know if your baby needs to wear the harness 24 hours a day without removing it at all, or if the harness can be removed for bathing.
Care at home
Putting the harness on
Your baby's orthotist will make sure the harness fits your baby correctly, and will show you how to put it on and how to check that it is positioned properly.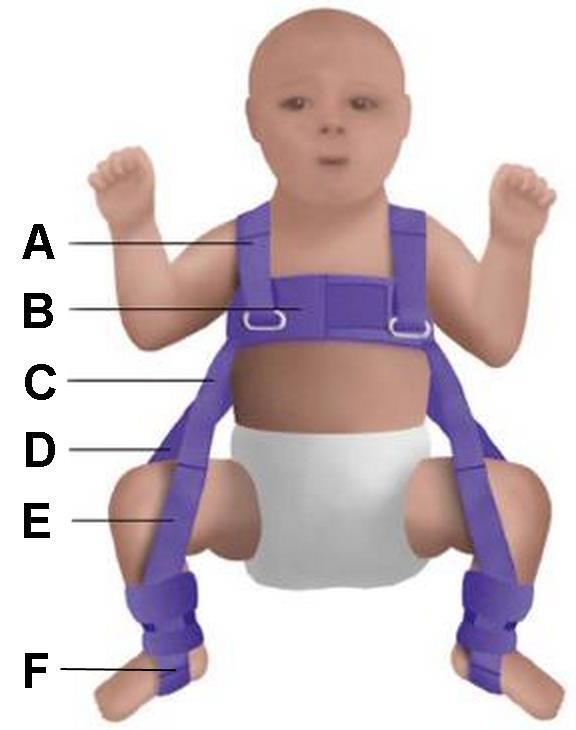
- The chest strap should be firm but you should be able to fit two fingers underneath it. This allows the chest to expand properly when your child is breathing.
- The ankle and lower leg straps should be firm to hold the foot, but not too tight.
Getting used to the harness
It takes some babies a couple of days to get use to the harness. Some babies may cry a little or seem unsettled for the first couple of nights. This should settle down after a few days.
Hygiene and skin care
Monitor your baby's skin daily. Take care to clean your baby's skin and if you notice any skin irritation or redness, contact the orthotist.
- Try to keep the harness dry at all times.
- If your doctor says the harness must be on 24 hours a day, it cannot be removed for bathing. In this case, your baby will need to have sponge baths. The orthotist will show you how to do this.
- If you are allowed to remove the harness for bathing, then only undo the Velcro straps to remove it.
 Do not adjust or undo the metal buckles.
Do not adjust or undo the metal buckles. - When bathing your baby, pay particular attention to the creases behind the knees and hip creases. Dry the skin well with a towel before reapplying the harness.
- Always try to keep your baby's legs apart if bathing them with the harness off.
Nappies and clothing
Your baby can wear normal nappies under the Pavlik Harness. When changing the nappy, do not hold your baby's feet together as this will move the hips from the correct position. Loose-fitting clothes that do not pull the knees together should be worn over the harness.
Feeding
You will be able to continue breastfeeding when using the Pavlik Harness. You might need to try some different positions until you find one that is comfortable for both you and your baby.
Positioning your baby
Your baby will be sleeping on their back with the harness on.
It is important to regularly change your baby's head's position while they are asleep to avoid a flat spot developing on the back of the head. The skull bones are very soft and the pressure of being in one position for too long can affect the shape of their head. See our
Plagiocephaly fact sheet for more information.
The skull bones are very soft and the pressure of being in one position for too long can affect the shape of their head. See our
Plagiocephaly fact sheet for more information.
Supervised tummy time for your baby will decrease the risk of developing a flat spot. It will also promote body stability, limb coordination and head control in your baby. Tummy time is important, even when your baby is wearing a Pavlik Harness.
Cleaning the harness
The Pavlik Harness should be washed only if absolutely necessary.
- Remove the soiled section of the brace (remember how it is attached), wash in cold water with soap and gently clean with a nail brush.
- Blot dry with a towel, or use a hair dryer on low heat.
- Do not tumble dry the harness (it may shrink).
Potential problems
Femoral nerve palsy is a very rare problem that can happen when using a Pavlik Harness. If you notice that your baby stops kicking, contact the orthotist as soon as possible.
Follow-up
Your orthotist will usually arrange regular reviews to monitor the progress of your baby's growth and adjust the orthosis as required. The review with the orthotist will be linked with your doctor's appointment. If your doctor's appointment is changed, you will also need to reschedule your orthotist’s appointment.
Contact your orthotist if you have any questions or concerns regarding your child's treatment with a Pavlik Harness.
Key points to remember
- Monitor your baby's skin daily. Take care to clean your baby's skin and if you notice any skin irritation or redness, contact the orthotist.
- Always try to keep your baby's legs apart, especially when bathing with the harness off.
- Babies may cry a little or seem unsettled for the first couple of nights after the harness is fitted. This should settle down within a couple of days.
- The Pavlik Harness should be washed only if absolutely necessary and do not tumble dry.

- Make sure you vary the position of your sleeping baby to avoid plagiocephaly (misshapen head).
For more information
- Kids Health Info fact sheet: Developmental dysplasia of the hip
- Kids Health Info fact sheet: Plagiocephaly
Common questions our doctors are asked
What should I do if my baby gets a rash under the harness?
It is important to monitor your baby’s skin each day, and contact the orthotist if a rash appears. If mild skin irritation occurs, a barrier ointment (like Vaseline) can be helpful, but discuss this with your child's orthotist.
My baby seems very reluctant to spend time on her tummy. How should I deal with this?
Tummy time is
difficult to achieve when your child is placed in any kind of orthosis (e.g.
harness, spica, plaster), though you can try encouraging tummy time during
orthosis-free time, if allowed. Fortunately, in the long-term, your child's
developmental ability will not suffer by missing out on tummy-time for this
short period in their life.
Developed by The Royal Children's Hospital Orthotics and Prosthetic department. We acknowledge the input of RCH consumers and carers.
Reviewed August 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit www.rchfoundation.org.au.
Hip dysplasia - clinic "Family Doctor".
“Your child has hip dysplasia” - very often this phrase from the mouth of an orthopedic doctor causes a state close to emotional shock in the parents of the baby. But is everything so gloomy and scary, and what kind of pathology is this?
Dysplasia - this term means a violation of the formation of any organ or body system. In this material we will talk about hip dysplasia.
Hip dysplasia is understood as a violation of the formation of the hip joint, which captures all the elements that make up the joint: the bone and cartilage base, the ligamentous-capsular apparatus and the muscle component.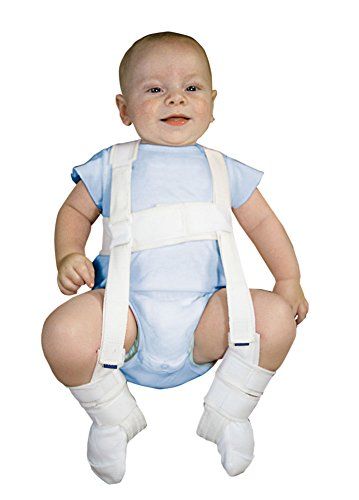 This definition is quite broad and includes the physiological immaturity of the hip joint, preluxation, subluxation and dislocation of the hip.
This definition is quite broad and includes the physiological immaturity of the hip joint, preluxation, subluxation and dislocation of the hip.
Physiological immaturity consists in the incomplete formation of the joint components without violating the congruence (correct matching) of the articular surfaces of the bones and, as a rule, requires minimal treatment or only dynamic observation, and it is this form of hip joint pathology that is mainly assigned the diagnosis of "dysplasia", although this is not entirely correct. terminologically. With pronounced immaturity of the hip joint, treatment is necessary to create favorable conditions for the proper maturation of the joint components.
Predislocation of the hip is already a pathology of the joint associated with the lack of stability of the femoral head in another component of the hip joint - the acetabulum and already requires close attention. In the absence of adequate treatment, hip predislocation can lead to the development of joint deformity (arthrosis), which leads to pain and impaired joint mobility, and can also lead to hip dislocation after the start of walking.
Dislocation of the hip is the most severe form of the pathology of the development of the hip joint, which consists in the almost complete discrepancy between the articular surfaces of the femoral head and the acetabulum. Such a malformation of the joint requires maximum efforts for a thorough diagnosis and active and prompt treatment. Late diagnosis or inadequate treatment leads to gross impairment of the hip joint mobility and, ultimately, leads to disability.
Now we understand why so much attention is paid to hip dysplasia by pediatricians and orthopedists. Why is it the hip joint that is most susceptible to these misfortunes?
The fact is that the hip joint, due to its anatomical and physiological characteristics, is the most loaded joint in our body, and a failure in one of its constituent components leads to dysfunction of the joint and, ultimately, to a deterioration in the quality of life of the patient. That is why the diagnosis of hip dysplasia can so often be heard from the lips of an orthopedist, although one cannot but recognize the fact of some overdiagnosis of this pathology, but given the severity of the consequences in the absence of treatment, this is still justified.
According to statistics, the incidence of hip dysplasia is 4-6 cases per 1000 newborns, in girls it occurs 6-7 times more often. Unilateral lesion predominates over bilateral (more often the left hip joint is affected). There is inheritance from mother to daughter. Quite a lot of factors leading to impaired intrauterine joint formation have been noted, among them are breech presentation of the fetus, narrowness of the uterus, oligohydramnios, toxic and biological (primarily viral diseases of the mother during pregnancy) factors and much more.
When and by what methods can and should hip dysplasia be diagnosed? Can a mother herself suspect the presence of hip dysplasia in a child and, if so, with what methods? The answer to this question depends on the severity of the joint injury. Let's try to answer this question by tying the timing and methods of diagnosis to the age of the baby.
When conducting ultrasound diagnostics during pregnancy, it is possible to diagnose only gross violations - subluxation and dislocation of the hip, that is, those changes in which the articular surface of the femoral head does not correspond to the surface of the acetabulum of the child's pelvis.
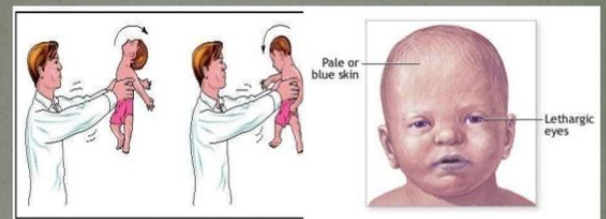
In the first 7-10 days of a child's life, an examination can reveal a “click symptom” or “slipping symptom” - dislocation and reduction of the hip in the joint. These symptoms are revealed in a child as follows: in the supine position, the legs are bent at the knee and hip joints at an angle of 90 degrees. The thumbs are located on the inner surface of the child's thighs, the index and middle fingers on the outer. With careful abduction and traction of the hips, the femoral head is set into the acetabulum with a characteristic click.
After the 2nd - 3rd week of a child's life, limitation of hip abduction comes to the fore in the diagnosis of hip dysplasia. To identify it, the legs of the child bent at the knee and hip joints in the supine position are bred without violence. Normally, it is possible to spread the hips to an angle of 85-90 degrees to the surface. With increased muscle tone and spasm of the muscles adducting the thigh, abduction can be limited to an angle of about 70 degrees, but such a restriction of hip abduction can also be caused by impaired joint formation. Limitation of hip abduction on one side in most cases is a sign of pathology from the hip joint.
Limitation of hip abduction on one side in most cases is a sign of pathology from the hip joint.
In favor of the pathology of the hip joint, symptoms such as shortening of one limb, turn of the foot on the side of the lesion outward from the middle position (external rotation of the foot) also speak.
The most widely known in parents (so to speak, "mommy symptom") - the asymmetry of the subgluteal folds - is not absolute and can be caused by many factors, but its importance in the diagnosis of hip dysplasia should not be underestimated, since this is the most common question that is addressed to orthopedic doctor.
To confirm the diagnosis of hip dysplasia and control the dynamics of treatment, ultrasound diagnostics are currently widely used. The positive aspects of this method of examination include painlessness, non-invasiveness, relative safety and a sharp increase in recent availability. Also, with the help of an ultrasound examination of the joint, minimal changes in the structure of the hip joint can be detected. But, unfortunately, this examination method does not always give accurate results (its reliability is about 85-90%. Nevertheless, to date, ultrasound diagnostics is the main method of screening for the diagnosis of hip dysplasia.
But, unfortunately, this examination method does not always give accurate results (its reliability is about 85-90%. Nevertheless, to date, ultrasound diagnostics is the main method of screening for the diagnosis of hip dysplasia.
In the case when the clinical picture differs from the data of the ultrasound examination or in case of late diagnosis of the pathology of the hip joint, the X-ray method is used. With a correctly performed radiograph, the picture of the structure of the joint and the position of the femoral head in the joint become completely clear. But due to the rather large radiation exposure during radiography, this examination method is used as rarely as possible.
In children older than a year, the main symptom is lameness on the affected side when walking or a "duck" gait with a bilateral process. Diagnosis at this age is belated. The clinical picture in this case almost always requires confirmation by x-ray, since it is necessary to accurately determine the relative position of the joint components.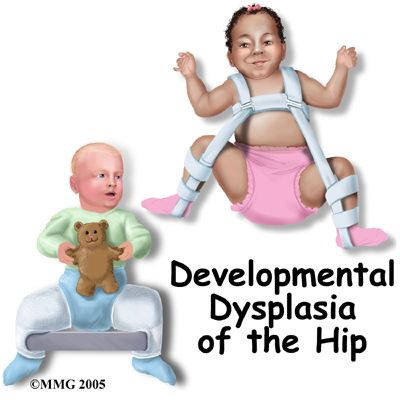
And so, the child was diagnosed with hip dysplasia, what to do next and how to help the baby?
Treatment of hip dysplasia should be started as early as possible. The goal of the treatment is to center the femoral head in the joint and create conditions for the formation of the entire acetabulum. Early, most gentle, but systematic treatment allows you to completely restore the anatomy and function of the underdeveloped hip joint.
The centering of the hip in the joint in the early stages of treatment is achieved by wide swaddling - two diapers are placed between the divorced hips of the child and fixed with a third. In severe degrees of hip dysplasia, special splints are used to center the femoral head (Pavlik's stirrups, Freik's pillow, etc.). When using these tires, parents may have questions and difficulties in caring for their baby, here are some tips to help you and your baby adjust during this period:
1. Only a baby diaper (disposable or gauze) should be under the stirrups or pillow.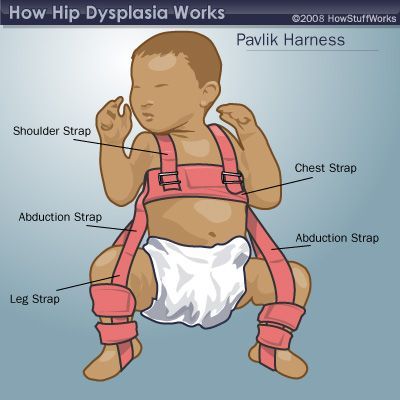 If you prefer to use gauze diapers, wear oilcloth panties that have zippers on the sides.
If you prefer to use gauze diapers, wear oilcloth panties that have zippers on the sides.
2. When changing a diaper, do not lift the child by the legs, but put your hand under the buttocks.
3. The vests can be changed without removing the stirrups: unfasten the shoulder straps from the chest strap and remove the vest over your head.
Over the tires you can wear loose pants, suits, dresses.
4. During the splint period, bathing the child is less frequent, so it is necessary to examine the skin under the straps, under the knees and around the neck 2-3 times a day to make sure there are no signs of inflammation (redness) of the skin. During this period, it is necessary to wipe the baby's skin with a soft cloth soaked in warm water. When carrying out water procedures, you can unfasten one foot part of the stirrup, but do not remove it, and keep the leg in a bent and retracted position.
5. It is also necessary to monitor the hygienic condition of the tire itself, it must always remain dry, avoid getting powders and lotions under the belts, this can cause inflammation on the baby's skin.
6. When feeding, be especially careful to ensure that the baby's hips do not come together.
The wearing of these devices (orthoses) is long-term - from 3 months to a year, and it is extremely important for the parents of a child who has been diagnosed with hip dysplasia to be patient and not be cowardly during the treatment period and meticulously follow the doctor's prescriptions.
After centering the femoral head, they begin massage and therapeutic exercises aimed at creating the correct ratio of the articular surfaces. We can recommend some exercises that are easy to do at home.
1. In the position of the child lying on his back, we bend the child's legs at the knee and hip joints as much as possible, and then fully straighten them.
2. In the previous starting position, we bend the child's legs at the knee and hip joints at a right angle, moderately spread the hips and, giving a moderate load along the axis of the hips, perform rotational movements with the hips.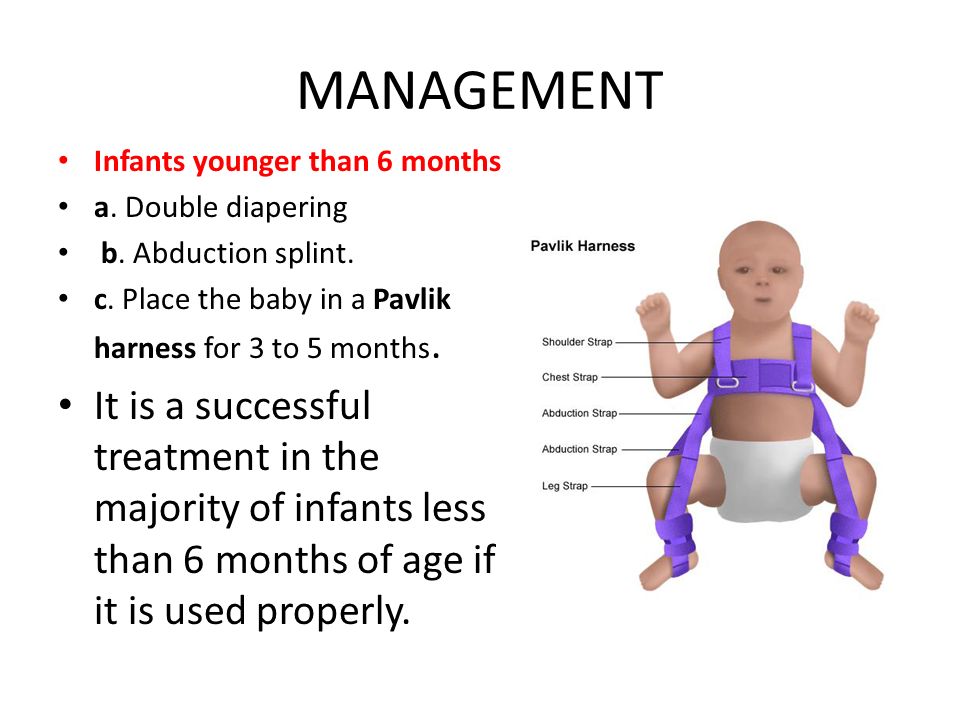
3. In the position of the child lying on his back, we breed the legs of the child bent at the knee and hip joints as much as possible to the surface of the table.
All exercises are performed 8-10 times 3-4 times a day.
Also during this period, physiotherapy (paraffin baths, electrophoresis with calcium and phosphorus preparations) is used to improve the nutrition of the joint components and complex orthopedic massage.
In cases of late diagnosis of hip dysplasia or in the absence of adequate treatment in the early stages, treatment is carried out by long-term staged plastering, as well as surgical treatment, but in these cases there are no standard treatment regimens and patient care tactics are developed individually.
After treatment of hip dysplasia, the child should be kept in the dispensary with an orthopedist for a long time - from 3 to 5 years until the end of growth. If necessary, control radiographs are performed once every 2 years to monitor the correct development of the joint.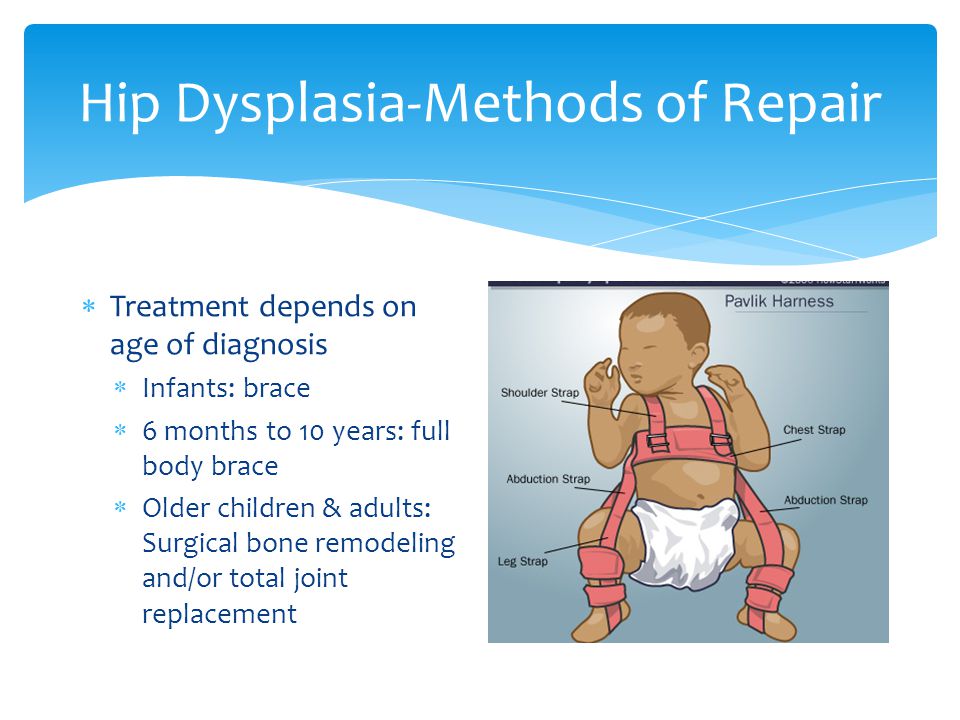 Also, restrictions on the load on the joint are often imposed. For children treated for hip dysplasia, it is desirable to visit specialized orthopedic groups in preschool institutions.
Also, restrictions on the load on the joint are often imposed. For children treated for hip dysplasia, it is desirable to visit specialized orthopedic groups in preschool institutions.
In severe degrees of hip dysplasia, functional disorders are, as a rule, lifelong in nature, even with timely and properly conducted treatment.
So what do the parents of the baby need to do in order to recognize hip dysplasia in time and, if this diagnosis was made to the child, to prevent serious complications?
First of all, it is necessary to show the child to the orthopedist in time. The recommended terms of examination by an orthopedist are 1 month, 3 months, 6 months and 1 year.
If the orthopedist nevertheless made a diagnosis of hip dysplasia, then the effectiveness of treatment by 50 percent depends on the correct and timely fulfillment by the child's parents of the doctor's prescriptions. It is important to remember that the sooner treatment is started, the better the results and the less chance of severe complications.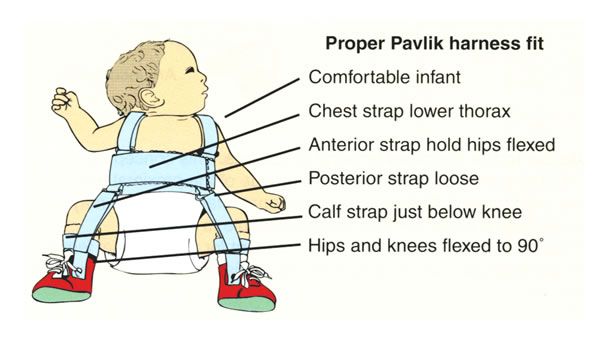 With early diagnosis of hip dysplasia and correct and timely treatment, a positive result is achieved in 96-98% of cases. You should not be AFRAID of this diagnosis, but it is necessary to treat the child, he needs your help and care!
With early diagnosis of hip dysplasia and correct and timely treatment, a positive result is achieved in 96-98% of cases. You should not be AFRAID of this diagnosis, but it is necessary to treat the child, he needs your help and care!
I hope this material helped you understand what kind of incomprehensible and frightening diagnosis it is - hip dysplasia, and it became clear to you how to deal with this pathology.
We recommend that you seek advice from the orthopedists of the Family Doctor clinic by calling the contact center in Moscow +7 (495) 775 75 66, or through the online appointment form.
Dysplasia of hip joints in newborns
Dysplasia of hip joints in newborns. Classification. Conservative and surgical treatment.
Introduction.
The term hip dysplasia (DHD) encompasses a wide range of pathological conditions, ranging from subtle acetabular dysplasia to irreducible dislocation of the hip with proximal displacement.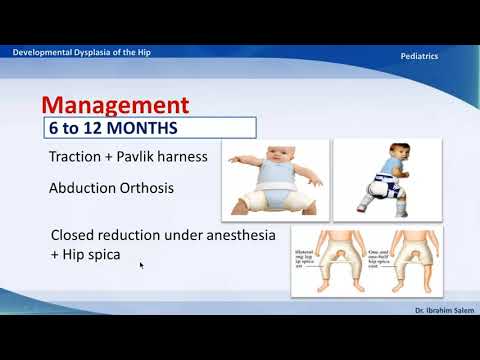 The incidence of hip dysplasia ranges from 1.5 to 2.5 per 1000 newborns. Unlike the term "congenital hip dysplasia", DTS includes congenital malformations and developmental disorders. The radiological definition relies on the preservation of Shenton's line, which remains unchanged in subluxations but is impaired in dysplasia.
The incidence of hip dysplasia ranges from 1.5 to 2.5 per 1000 newborns. Unlike the term "congenital hip dysplasia", DTS includes congenital malformations and developmental disorders. The radiological definition relies on the preservation of Shenton's line, which remains unchanged in subluxations but is impaired in dysplasia.
The term "dysplasia" is generally used for hip dislocation with a positive Ortolani sign, ie when it is possible to rule into the acetabulum. Dysplasia is characterized by ridges in the posterior superior and inferior zones of the acetabulum. According to Ortolani, the neolimbus or ridge is composed of cellular hyaline cartilage. An additional diagnostic test to detect dysplasia is the "Barlow maneuver", when simultaneous flexion at the hip joint and adduction brings the femoral head out of the acetabulum. It has been proven that untreated DTS leads to the development of degenerative joint diseases.
TTP classification
TTP is classified according to the ultrasound pattern. The two main measured sonographic parameters in DTS are alpha and beta angles. The alpha angle depends on the degree of development of the bone roof and is located between the lateral wall of the ilium and the roof of the acetabulum. The angle beta is formed by the upper bony edge of the acetabulum and the middle of the limbus, and characterizes the degree of development of the cartilaginous roof. The cartilaginous prominence, or head-to-socket insertion index, evaluates coverage by the upper edge of the femoral head. According to these indicators, four types and eight subtypes of DTS are distinguished.
The two main measured sonographic parameters in DTS are alpha and beta angles. The alpha angle depends on the degree of development of the bone roof and is located between the lateral wall of the ilium and the roof of the acetabulum. The angle beta is formed by the upper bony edge of the acetabulum and the middle of the limbus, and characterizes the degree of development of the cartilaginous roof. The cartilaginous prominence, or head-to-socket insertion index, evaluates coverage by the upper edge of the femoral head. According to these indicators, four types and eight subtypes of DTS are distinguished.
Screening for DTS may be based on clinical and/or ultrasound findings. Some researchers argue that clinical examination for hip dysplasia, due to the high rate of spontaneous stabilization in the first 4 weeks of life, should be delayed until after the neonatal period. There is an opinion that in the first two weeks it is safer to control DTS by ultrasound.
Conservative treatment
The treatment of DTS has evolved markedly since the forced closed reduction proposed by Lorenz and immobilization with a cast in the position of maximum abduction. Ortolani was the first to identify dislocations in children under 12 months of age, using the clinical maneuver named after him, and developed a variant of abduction fixation.
Ortolani was the first to identify dislocations in children under 12 months of age, using the clinical maneuver named after him, and developed a variant of abduction fixation.
In the 1950s, Arnold Pawlik developed the harness and stirrup system that is still used today. The concept of forced hip reduction with simultaneous flexion and abduction shortens the hip and corrects acetabular dysplasia, minimizing the risk of avascular necrosis of the femoral head. Maintaining the activity of the quadriceps and gluteal muscles helps to reduce dislocation.
The use of Pavlik's stirrups is contraindicated in severe muscular imbalances, as in L2-L4 myelomeningocele, severe rigidity, as in arthrogryposis, or ligamentous weakness, as in Ehlers-Danlos syndrome.
There are modes of using Pavlik stirrups from 3 weeks to 9 months. Studies have shown the effectiveness of calculating the time of using stirrups based on the age at which treatment began: treatment for at least 3 months in children under 3 months of age, in children over 4 months of age. - a period equal to twice the age. Other investigators recommend an average duration of treatment of 3.6 months. at the beginning before the age of one month, 7.0 months. at the age of 1 3 months, 9.3 months. – from 3 to 9 months. The best way to control the results of treatment with a tourniquet Pavlik ultrasound.
- a period equal to twice the age. Other investigators recommend an average duration of treatment of 3.6 months. at the beginning before the age of one month, 7.0 months. at the age of 1 3 months, 9.3 months. – from 3 to 9 months. The best way to control the results of treatment with a tourniquet Pavlik ultrasound.
The effectiveness of the Pavlik tourniquet in DTS 7% -99%.
Failure is most often due to incorrect use. The incidence of femoral head necrosis ranges from 0% to 28%. The use of the Pavlik tourniquet is associated with excessive flexion leading to trauma to the femoral nerve, which leads to a high incidence of aseptic necrosis of the femoral head.
The maximum possible application time of the Pavlik tourniquet is unknown. Some studies have shown that prolonged unsuccessful treatment according to the technique is associated with a high incidence of aseptic necrosis of the femur, deformity of the head, and deficiency of the posterior wall of the acetabulum.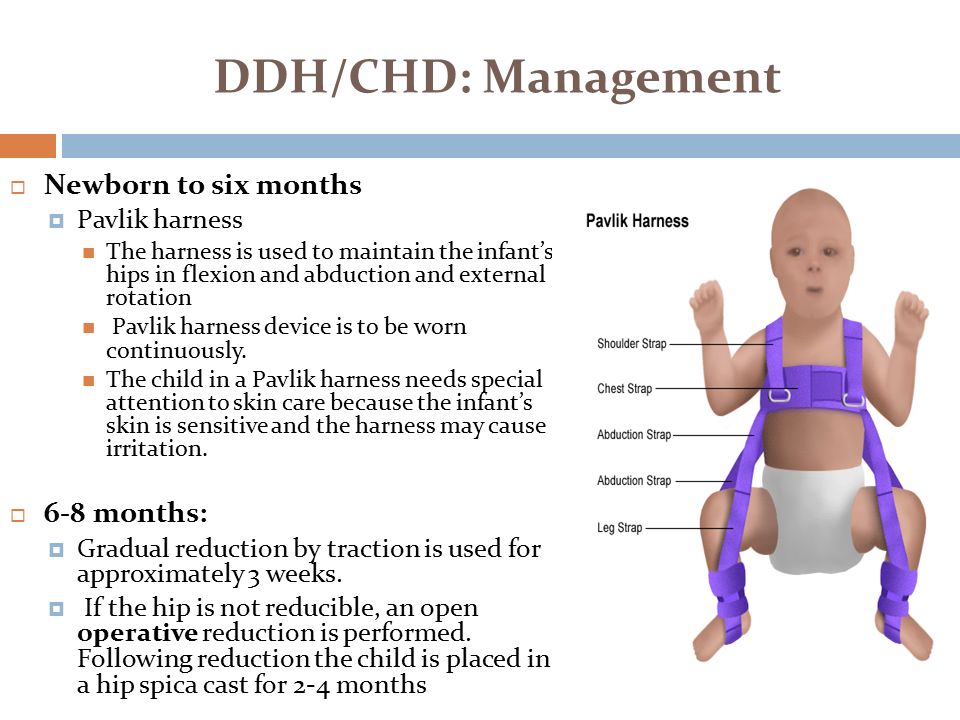 Other investigators have argued that prolonged use of the tourniquet increases the likelihood of a successful outcome, without increasing the incidence of avascular necrosis of the femoral head or residual dysplasia.
Other investigators have argued that prolonged use of the tourniquet increases the likelihood of a successful outcome, without increasing the incidence of avascular necrosis of the femoral head or residual dysplasia.
In support of this, after 12 weeks of application of the Pavlik tourniquet, half of the children with type III DTS responded to therapy. A significant proportion of children had a formal reason for surgery after 4 weeks of ineffective use of the tourniquet.
Investigators reported that with long-term use of the Pavlik tourniquet in children with type III and IV DTH, the incidence of aseptic necrosis of the femur is 16%, which is equivalent to complications with short-term therapy.
Aseptic necrosis of the femur is established according to the Salter criteria.
A L B T E Rnative non-surgical methods of treatment
There are several alternative devices used in children with the dial-up joint of Le-Damani, Frame, Lorensa and Ortolan. However, most studies have shown that the Pavlik tourniquet is more effective and less likely to develop aseptic necrosis of the femur.
However, most studies have shown that the Pavlik tourniquet is more effective and less likely to develop aseptic necrosis of the femur.
The Frejck pillow, for example, is associated with poor outcomes and a high incidence of aseptic necrosis of the femur because it forcefully abducts the thigh.
Some devices based on the Pavlik tourniquet have shown promising results. The Wagner stocking, for example, showed very high efficacy and a low risk of aseptic necrosis of 2.6%.
Surgical treatment
If conservative treatment of DTS is ineffective, surgical methods are used in combination with femoral or pelvic osteotomy.
Femoral osteotomies are performed to correct excessive anterior displacement or valgus deformity of the femoral neck. The choice between the Salter pelvic osteotomy and the Pemberton pericapsular osteotomy is based on the acetobular index, the angle between the Hilgenreiner line and the line drawn to the lateral edge of the acetabulum from the triradial epiphysis.