Nt measurement 12 weeks
12 Week Scan | SO + GI Scan
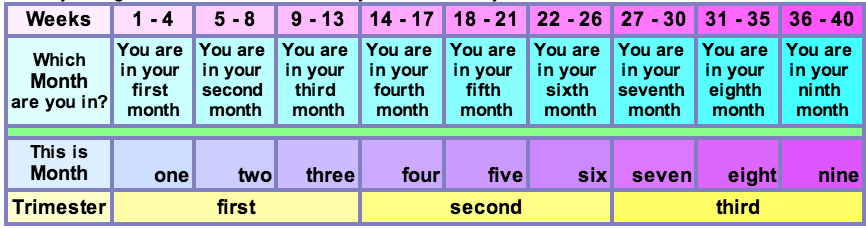
At 12 Weeks: Nuchal Translucency ScanThe nuchal translucency (NT) scan, or “12-week scan,” is an ultrasound performed in the first trimester between 11.5 weeks and 13 weeks, six days. This scan is combined with a blood test that looks at two specific hormones of pregnancy: the free-Beta hCG and PAPP-A (pregnancy associated plasma protein A). This combined test is an extremely accurate non-invasive screening test available to help identify a fetus at risk for Down syndrome as well as other chromosomal abnormalities and some major structural abnormalities. The sensitivity of this only recently eclipsed by NIPT. An ultrasound screening test is non-invasive and does not have any side effects or complications.
However, it will not give a yes/no answer to whether a problem such as Down syndrome is present. The only way to diagnose Down syndrome or other chromosomal abnormalities is by having a diagnostic test — either a CVS or an amniocentesis — and testing the fetal cells. These tests are invasive and require a needle to be passed into the maternal abdomen and uterus and therefore carry a small risk of miscarriage.
Many patients do not wish to have the diagnostic test because of the small risk of miscarriage and prefer to have the ultrasound screening test, the NT scan, to help them decide if they wish to proceed to testing the fetus. Unfortunately, while NT combined with the first trimester biochemical blood test is a very accurate screening test available for chromosomal abnormalities, it will not detect all fetuses affected with Down syndrome or other chromosomal abnormalities.
Chromosomal abnormalities occur when there is a change in the number or structure of the chromosomes. Normally we have 46 chromosomes, 23 pairs numbered 1-22 and a pair of sex chromosomes.
Boys have XY and girls have XX. The most common chromosomal abnormality seen at birth is Down syndrome. In Down syndrome, an extra copy of chromosome 21 is present, giving a total of 47 chromosomes.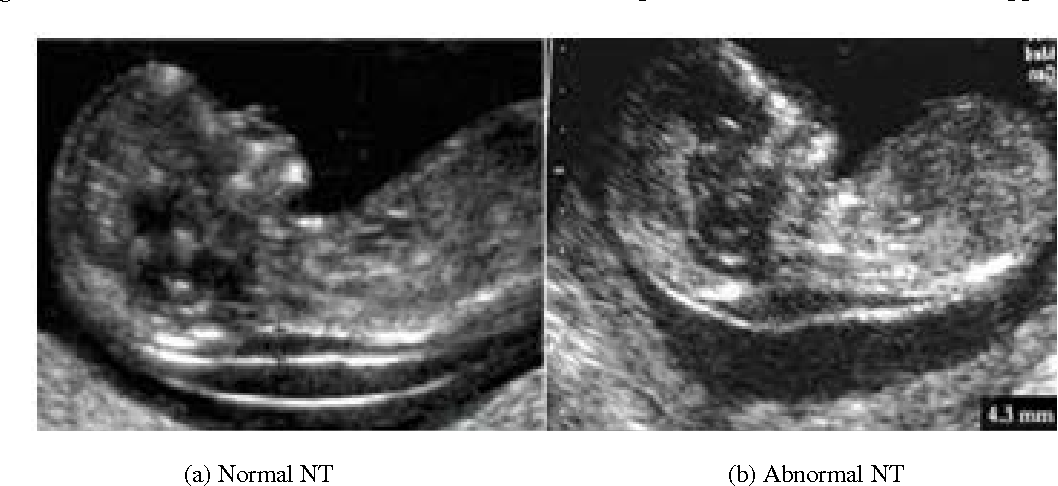
Accredited practices:
To be certain your NT scan is performed correctly, it is important that you have your scan performed at an accredited practice. A NT computer package was developed by the London Fetal Medicine Foundation in the 1990s and was based on more than 100.000 pregnancies.
Strict auditing of the NT ultrasound work performed by every accredited practice in the world is undertaken several times a year. This ensures that the NT scan test is being performed correctly. Recently, the Royal Australian College of Obstetricians and Gynaecologists has taken over regular auditing of Australian practices.
Advantages of the 12 week NT scanThere are several advantages to undergoing a 12-week NT scan, including:
- Estimate individual risk for Down syndrome and other chromosomal abnormality
- Screen for spina bifida
- More accurately date the pregnancy
- Diagnose multiple fetuses
- Diagnose early pregnancy failure
- Allow early detection of some major abnormalities
At the end of the first trimester, there is usually a small amount of fluid beneath the skin of the fetus at the back of the head and neck. This fluid is called the nuchal translucency (NT), and can be easily and accurately measured to within a tenth of a millimetre.
This fluid is called the nuchal translucency (NT), and can be easily and accurately measured to within a tenth of a millimetre.
When there is extra fluid and the NT measurement is thicker than normal, there is an association with chromosomal anomalies such as Down syndrome and some structural abnormalities in the fetus. Not all babies with an increased NT measurement have Down syndrome or any structural abnormality.
The extra fluid at the back of the head and neck usually disappears by 18 weeks. The fluid in itself is not an abnormality and does not harm the baby but may simply be the sign of a potential problem. The baby is measured from head to bottom to determine the crown-rump length and the nuchal translucency is measured. These measurements are entered into the computer program with the patient’s date of birth and the first trimester biochemistry blood test. The computer then calculates the patient’s age-related risk for Down syndrome and the new individual risk for this pregnancy.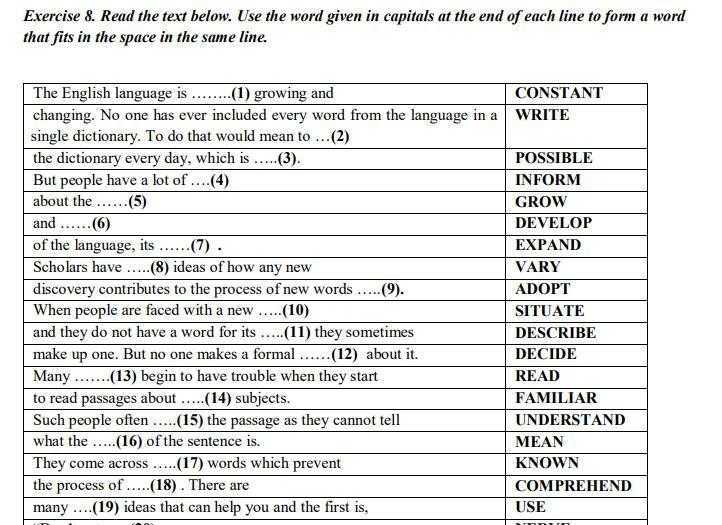 The findings are then discussed with the patient. The combined NT result will provide the patient with a risk assessment. This will either be a high risk (risk is greater than 1 in 300) or a low risk (risk less than 1 in 300). As this is a screening test and not a diagnostic test, even with a low calculated risk, Down syndrome is not completely excluded and can still occur occasionally.
The findings are then discussed with the patient. The combined NT result will provide the patient with a risk assessment. This will either be a high risk (risk is greater than 1 in 300) or a low risk (risk less than 1 in 300). As this is a screening test and not a diagnostic test, even with a low calculated risk, Down syndrome is not completely excluded and can still occur occasionally.
Free- BhCG (Beta human chorionic gonadotrophin) and PAPP-A (Pregnancy associated plasma protein-A) levels can be assessed from a blood test. This is best done at 10 weeks, some two weeks prior to the NT scan but it can also be done just before or on the same day as the NT scan. The PAPP-A level tends to be lower and the BhCG level tends to be higher in pregnancies affected by Down syndrome.
Accuracy of Nuchal TranslucencyWhen the ultrasound is combined with the first trimester blood test (BhCG and PAPPA) and nasal bone, the detection rate increases to 95%. None of these screening tests can give 100% detection. If a pregnant woman wants to completely exclude a chromosome abnormality, then she should consider having prenatal testing with either a CVS or an amniocentesis. Genetic counselling is also recommended. The results of the examination will be available to you shortly after the examination. One of our genetic counsellors or doctors will be available to discuss the result and the options for further testing.
None of these screening tests can give 100% detection. If a pregnant woman wants to completely exclude a chromosome abnormality, then she should consider having prenatal testing with either a CVS or an amniocentesis. Genetic counselling is also recommended. The results of the examination will be available to you shortly after the examination. One of our genetic counsellors or doctors will be available to discuss the result and the options for further testing.
Chromosomally and Anatomically Normal Fetuses With Increased First Trimester Nuchal Translucency Conceived by ICSI
Iran J Radiol. 2015 Apr; 12(2): e7157.
Published online 2015 Apr 21. doi: 10.5812/iranjradiol.7157
1,* and 1
Author information Article notes Copyright and License information Disclaimer
Nuchal translucency (NT) measurements in the first trimester screening between 11 and 14 weeks’ gestation are regarded as a clear marker for aneuploidies. The presence of a thickened NT, even if the karyotype is normal, can be associated with structural abnormalities. Having an abnormal screening of NT, parents and physicians could face dilemma over abortion particularly in a case of IVF/ICSI fetuses. Measurement of the NT thickness combined with biochemical markers has a false-positive rate of 5%. Hereby we present six cases of chromosomally normal fetuses with an increased NT thickness in the first trimester, a normal karyotype and normal follow-up scans, who had a good prognosis for a normal early childhood. This report may help increase the confidence of couples who are reluctant to terminate the pregnancy.
The presence of a thickened NT, even if the karyotype is normal, can be associated with structural abnormalities. Having an abnormal screening of NT, parents and physicians could face dilemma over abortion particularly in a case of IVF/ICSI fetuses. Measurement of the NT thickness combined with biochemical markers has a false-positive rate of 5%. Hereby we present six cases of chromosomally normal fetuses with an increased NT thickness in the first trimester, a normal karyotype and normal follow-up scans, who had a good prognosis for a normal early childhood. This report may help increase the confidence of couples who are reluctant to terminate the pregnancy.
Keywords: Congenital Abnormalities, Prenatal Diagnosis, Nuchal Translucency Measurement
Fetal nuchal translucency (NT) refers to the sonographic appearance of subcutaneous edema in the fetal neck measured according to the fetal medicine foundation (FMF) guidelines. NT is defined as the maximal thickness of the sonolucent zone (fluid accumulation) between the inner aspect of the fetal skin and the outer aspect of the soft tissue overlying the cervical spine or the occipital bone (). To avoid false negative or positive results, the fetus should be in a neutral position, with the head in line with the spine. During the scan, more than one measurement must be taken and the maximum one that meets the criteria should be considered.
To avoid false negative or positive results, the fetus should be in a neutral position, with the head in line with the spine. During the scan, more than one measurement must be taken and the maximum one that meets the criteria should be considered.
Open in a separate window
According to the FMF guidelines, NT is measured as the maximal thickness of the sonolucent zone (fluid accumulation) between the inner aspect of the fetal skin and the outer aspect of the soft tissue overlying the cervical spine or the occipital bone.
For this report, the outcome of 703 pregnancies presenting at Royan Institute after intra cytoplasmic sperm injection (ICSI) between the years 2008 and 2009 were reviewed. First trimester measurements of NT were performed during the routine first trimester screening for 856 fetuses. A total of 12 fetuses with an increased NT (NT ≥ 3) were considered for further investigation. In the follow-up ultrasounds, six out of 12 fetuses showed no anomalies and the result of amniocentesis (karyotype), fetal echocardiography and triple test or double test (the biochemical markers of pregnancy-associated plasma protein-A and free β-human chorionic gonadotropin) were also normal. Six healthy neonates were followed during their first and second year by routine pediatrician visits and the mental, physical or motor developmental delay was not observed in any of the cases and their functions were normal.
Six healthy neonates were followed during their first and second year by routine pediatrician visits and the mental, physical or motor developmental delay was not observed in any of the cases and their functions were normal.
All sonographic measurements were carried out by an expert radiologist with 10 years of experience and FMF certification in the measurement of NT. Images were saved and re-checked by another expert radiologist. Increased NT can be associated with a high incidence rate of chromosomal and non-chromosomal abnormalities. However, in nine studies that have addressed the issue of pediatric long-term follow-up of chromosomally and anatomically normal fetuses with increased NT, this measurement was suggested to be an indefinite indicator for the evaluation of fetal anomalies (1-9).
2.1. Case 1
A 28-year-old woman with a twin pregnancy, which was conceived by ICSI, was referred for routine screening test in the first trimester. The result of semen analysis showed a low motility (35%) with a high abnormal morphology (87%). In the routine first trimester screening at 12 weeks and 2 days of gestation, the NT measurements of the first fetus was 3.4 mm (normal range for this age is 1.2-3.1 mm). Although she refused to undergo the triple test and we had no result for amniocentesis (karyotype) and fetus echocardiography, follow-up ultrasounds revealed normal results. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 3400 grams. Neonates were followed during the first 2 years of their life and none of them had developmental delay.
In the routine first trimester screening at 12 weeks and 2 days of gestation, the NT measurements of the first fetus was 3.4 mm (normal range for this age is 1.2-3.1 mm). Although she refused to undergo the triple test and we had no result for amniocentesis (karyotype) and fetus echocardiography, follow-up ultrasounds revealed normal results. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 3400 grams. Neonates were followed during the first 2 years of their life and none of them had developmental delay.
2.2. Case2
A 35-year-old woman, who was conceived by ICSI, was referred for the routine screening test during her pregnancy. Her obstetric and medical history revealed primary infertility for a period of 7 years, mild endometriosis and polycystic ovaries. The result of semen analysis indicated low motility (35%) and high abnormal morphology (88%). During the routine first trimester screening at 13 weeks of gestation, NT was measured at 3 mm.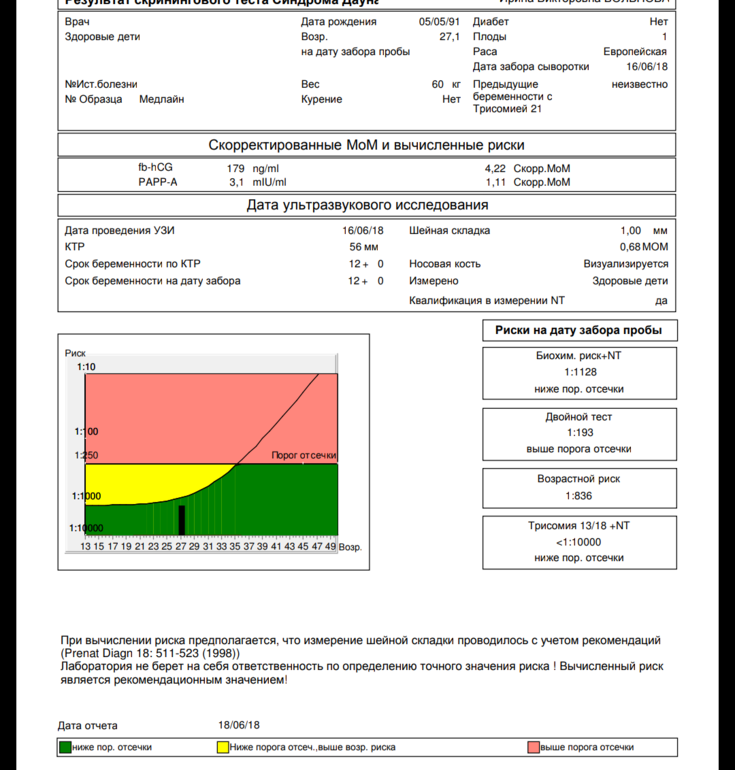 The normal range of NT for this age is 1.6-2.4 mm. Nuchal skin fold (NF) measurements and prenatal follow-up ultrasound findings were normal. A Triple test was performed, and it showed a positive result and a high risk of trisomy 21. The patient was referred for amniocentesis or chorionic villus sampling. The amniocentesis findings were normal and a healthy baby girl (weight = 3600 grams) was born after a full-term pregnancy. She was followed during the first and second year of life and no developmental delay was detected.
The normal range of NT for this age is 1.6-2.4 mm. Nuchal skin fold (NF) measurements and prenatal follow-up ultrasound findings were normal. A Triple test was performed, and it showed a positive result and a high risk of trisomy 21. The patient was referred for amniocentesis or chorionic villus sampling. The amniocentesis findings were normal and a healthy baby girl (weight = 3600 grams) was born after a full-term pregnancy. She was followed during the first and second year of life and no developmental delay was detected.
2.3. Case 3
A 33-year-old pregnant woman conceived by ICSI was referred for a routine screening test. Her obstetric and medical histories were unremarkable. The result of semen analysis indicated low motility (30%) and high abnormal morphology (81%). The result of the routine first trimester screening at 11 weeks and 5 days gestation showed a significant increased NT (NT = 5). The normal range of NT for this age is 1-2.8 mm. Later examination revealed that collection of fluid was not confined to the neck but was enveloped throughout the fetus. The result of follow-up such as prenatal ultrasound findings, result of an amniocentesis (karyotype) and echocardiography were reported normal. She gave birth to a healthy baby boy (weight = 3500 grams) at 37 weeks of pregnancy by elective cesarean section at term. Follow-up after birth till 2 years has revealed no developmental delay.
The result of follow-up such as prenatal ultrasound findings, result of an amniocentesis (karyotype) and echocardiography were reported normal. She gave birth to a healthy baby boy (weight = 3500 grams) at 37 weeks of pregnancy by elective cesarean section at term. Follow-up after birth till 2 years has revealed no developmental delay.
2.4. Case 4
A 26-year-old woman who was conceived by ICSI was referred for a routine screening test during her pregnancy. Her obstetric and medical history showed 8 years of primary infertility and polycystic ovaries. The result of semen analysis showed a low sperm concentration with a low total sperm count, low motility (30%) and high abnormal morphology (86%). First trimester measurement of NT at 12 weeks of gestation was 3.2 mm during the routine first trimester screening. The normal range of NT for this age is 1.1-3 mm. Although she refused to undergo amniocentesis (karyotype) and fetal echocardiography, triple test and follow-up prenatal ultrasound findings were normal. She gave birth at term to a healthy baby boy at 38 weeks (weight = 3500 grams). The 2-year follow-up after birth revealed no developmental delay.
She gave birth at term to a healthy baby boy at 38 weeks (weight = 3500 grams). The 2-year follow-up after birth revealed no developmental delay.
2.5. Case 5
Following the routine screening test during pregnancy, a 31-year-old woman (conceived by ICSI) was referred to this institute. Her obstetric and medical history apart from 7 years primary infertility was unremarkable. The result of semen analysis revealed a low motility (35%) and a high abnormal morphology (92%). The result of routine first trimester screening at 12 weeks and 5 days of gestation showed an increased NT (3.3 mm) and generalized edema. The normal range of NT for this age is 1.5-3 mm. Although she refused to do the triple test and fetal echocardiography, follow-up prenatal ultrasound findings and amniocentesis (karyotype) were normal. She gave birth to a healthy term baby girl (weight = 3400 grams). Follow-up after birth revealed no developmental delay.
2.6. Case 6
A 30-year-old patient (conceived by ICSI) first presented to our institute at 12 weeks and 1 day of gestation and a twin pregnancy was detected. The second fetus was diagnosed with an increased NT (NT = 3.5 mm). The normal range of NT for this age is 1.2-3 mm. The couples’ history was significant for abnormal semen analysis. The result of semen analysis showed a sperm motility of 35% and an abnormal morphology of 80%. In this case, follow-up prenatal ultrasound findings and triple test were normal. Amniocentesis (karyotype) and echocardiography were cancelled because the patient refused to do so. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 2900 grams. The neonates were followed for the first and second year of their life and none of them had developmental delay.
The second fetus was diagnosed with an increased NT (NT = 3.5 mm). The normal range of NT for this age is 1.2-3 mm. The couples’ history was significant for abnormal semen analysis. The result of semen analysis showed a sperm motility of 35% and an abnormal morphology of 80%. In this case, follow-up prenatal ultrasound findings and triple test were normal. Amniocentesis (karyotype) and echocardiography were cancelled because the patient refused to do so. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 2900 grams. The neonates were followed for the first and second year of their life and none of them had developmental delay.
Although measurement of the NT thickness combined with biochemical markers has a false-positive rate of 5% (10), it is regarded as a basic screening test with high sensitivity for identifying fetuses at risk for aneuploidy (1, 11, 12). However, NT is increased in 4.4% of euploid fetuses who are at risk for fetal anomalies and an adverse pregnancy outcome (12).
For this report first trimester ultrasound screening was performed for 703 women with a total number of 856 fetuses who were conceived by ICSI. First trimester measurement of NT was performed for 856 fetuses and 12 out of 856 fetuses with increased NT (NT ≥ 3) were taken for further investigation. In this report, six out of 12 cases who were chromosomally and anatomically normal fetuses with increased first trimester NT were described in detail. All these six fetuses had favorable prognosis despite the increased NT. We had no chromosomal report of the remained six fetuses because of reduction due to multiple pregnancies (4/12) and intrauterine fetal death (IUFD 2/12).
The chance of delivering a healthy baby decreases with NT thickness from approximately 70% for an NT of 3.5-4.4 mm to about 15% for an NT of 6.5 mm or more (13). Based on previous studies, fetuses with increased NT (less than 4 mm), normal karyotype and normal findings in the 20-week scan, showed a markedly increased favorable outcome (14). After a normal detailed genetic sonography and fetal echocardiography, the incidence of adverse outcome and developmental delay were not significantly different from the normal population (9). According to studies performed by Souka et al. fetuses with increased NT thickness have a high risk of adverse or poor pregnancy outcome (1, 13). In this study, we only had one case of increased NT and intrauterine fetal death (IUFD) and one case of premature rupture of the membranes (PROM).
After a normal detailed genetic sonography and fetal echocardiography, the incidence of adverse outcome and developmental delay were not significantly different from the normal population (9). According to studies performed by Souka et al. fetuses with increased NT thickness have a high risk of adverse or poor pregnancy outcome (1, 13). In this study, we only had one case of increased NT and intrauterine fetal death (IUFD) and one case of premature rupture of the membranes (PROM).
This report is limited in number and should be further completed. In this series, semen analysis of all six cases were abnormal with a low motility of 30-35% and a high abnormal morphology of 80-92%. Although specific semen preparation technique in the case of impaired semen parameters in ART cycles is advisable, couples diagnosed with male-factor infertility should receive genetic counseling about the increased risk of congenital abnormalities before IVF-ICSI (15). This report provided six cases of increased NT with normal outcomes. It may help increase the confidence of couples who are reluctant to terminate the pregnancy. However, caution is necessary in cases of increased NT and parents should be offered a detailed fetal evaluation (genetic sonography) at the end of the first trimester and also at 18-22 weeks of gestation. Triple test, amniocentesis, fetal echocardiography and follow-up after birth are necessary.
It may help increase the confidence of couples who are reluctant to terminate the pregnancy. However, caution is necessary in cases of increased NT and parents should be offered a detailed fetal evaluation (genetic sonography) at the end of the first trimester and also at 18-22 weeks of gestation. Triple test, amniocentesis, fetal echocardiography and follow-up after birth are necessary.
1. Souka AP, Krampl E, Bakalis S, Heath V, Nicolaides KH. Outcome of pregnancy in chromosomally normal fetuses with increased nuchal translucency in the first trimester. Ultrasound Obstet Gynecol. 2001;18(1):9–17. doi: 10.1046/j.1469-0705.2001.00454.x. [PubMed] [CrossRef] [Google Scholar]
2. Van Vugt JM, Tinnemans BW, Van Zalen-Sprock RM. Outcome and early childhood follow-up of chromosomally normal fetuses with increased nuchal translucency at 10-14 weeks' gestation. Ultrasound Obstet Gynecol. 1998;11(6):407–9. doi: 10.1046/j.1469-0705.1998.11060407.x. [PubMed] [CrossRef] [Google Scholar]
3. Brady AF, Pandya PP, Yuksel B, Greenough A, Patton MA, Nicolaides KH. Outcome of chromosomally normal livebirths with increased fetal nuchal translucency at 10-14 weeks' gestation. J Med Genet. 1998;35(3):222–4. [PMC free article] [PubMed] [Google Scholar]
Brady AF, Pandya PP, Yuksel B, Greenough A, Patton MA, Nicolaides KH. Outcome of chromosomally normal livebirths with increased fetal nuchal translucency at 10-14 weeks' gestation. J Med Genet. 1998;35(3):222–4. [PMC free article] [PubMed] [Google Scholar]
4. Adekunle O, Gopee A, el-Sayed M, Thilaganathan B. Increased first trimester nuchal translucency: pregnancy and infant outcomes after routine screening for Down's syndrome in an unselected antenatal population. Br J Radiol. 1999;72(857):457–60. doi: 10.1259/bjr.72.857.10505009. [PubMed] [CrossRef] [Google Scholar]
5. Maymon R, Jauniaux E, Cohen O, Dreazen E, Weinraub Z, Herman A. Pregnancy outcome and infant follow-up of fetuses with abnormally increased first trimester nuchal translucency. Hum Reprod. 2000;15(9):2023–7. [PubMed] [Google Scholar]
6. Hiippala A, Eronen M, Taipale P, Salonen R, Hiilesmaa V. Fetal nuchal translucency and normal chromosomes: a long-term follow-up study. Ultrasound Obstet Gynecol. 2001;18(1):18–22. doi: 10.1046/j.1469-0705.2001.00481.x. [PubMed] [CrossRef] [Google Scholar]
doi: 10.1046/j.1469-0705.2001.00481.x. [PubMed] [CrossRef] [Google Scholar]
7. Senat MV, De Keersmaecker B, Audibert F, Montcharmont G, Frydman R, Ville Y. Pregnancy outcome in fetuses with increased nuchal translucency and normal karyotype. Prenat Diagn. 2002;22(5):345–9. doi: 10.1002/pd.321. [PubMed] [CrossRef] [Google Scholar]
8. Cheng CC, Bahado-Singh RO, Chen SC, Tsai MS. Pregnancy outcomes with increased nuchal translucency after routine Down syndrome screening. Int J Gynaecol Obstet. 2004;84(1):5–9. [PubMed] [Google Scholar]
9. Senat MV, Bussieres L, Couderc S, Roume J, Rozenberg P, Bouyer J, et al. Long-term outcome of children born after a first-trimester measurement of nuchal translucency at the 99th percentile or greater with normal karyotype: a prospective study. Am J Obstet Gynecol. 2007;196(1):53 e1–6. doi: 10.1016/j.ajog.2006.08.026. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Nicolaides KH, Spencer K, Avgidou K, Faiola S, Falcon O. Multicenter study of first-trimester screening for trisomy 21 in 75 821 pregnancies: results and estimation of the potential impact of individual risk-orientated two-stage first-trimester screening. Ultrasound Obstet Gynecol. 2005;25(3):221–6. doi: 10.1002/uog.1860. [PubMed] [CrossRef] [Google Scholar]
Multicenter study of first-trimester screening for trisomy 21 in 75 821 pregnancies: results and estimation of the potential impact of individual risk-orientated two-stage first-trimester screening. Ultrasound Obstet Gynecol. 2005;25(3):221–6. doi: 10.1002/uog.1860. [PubMed] [CrossRef] [Google Scholar]
11. Pandya PP, Kondylios A, Hilbert L, Snijders RJ, Nicolaides KH. Chromosomal defects and outcome in 1015 fetuses with increased nuchal translucency. Ultrasound Obstet Gynecol. 1995;5(1):15–9. doi: 10.1046/j.1469-0705.1995.05010015.x. [PubMed] [CrossRef] [Google Scholar]
12. Snijders RJ, Noble P, Sebire N, Souka A, Nicolaides KH. UK multicentre project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10-14 weeks of gestation. Fetal Medicine Foundation First Trimester Screening Group. Lancet. 1998;352(9125):343–6. [PubMed] [Google Scholar]
13. Souka AP, Von Kaisenberg CS, Hyett JA, Sonek JD, Nicolaides KH. Increased nuchal translucency with normal karyotype.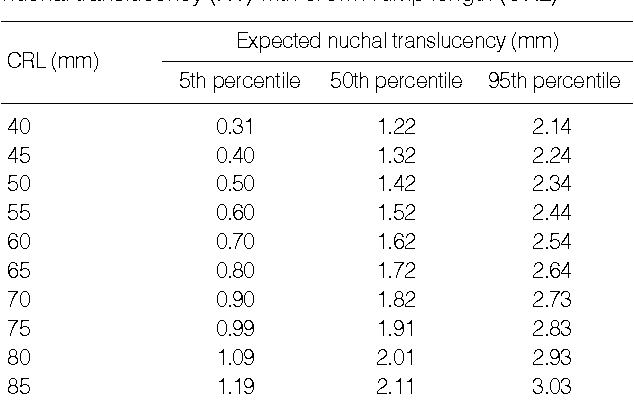 Am J Obstet Gynecol. 2005;192(4):1005–21. doi: 10.1016/j.ajog.2004.12.093. [PubMed] [CrossRef] [Google Scholar]
Am J Obstet Gynecol. 2005;192(4):1005–21. doi: 10.1016/j.ajog.2004.12.093. [PubMed] [CrossRef] [Google Scholar]
14. Bilardo CM, Muller MA, Pajkrt E, Clur SA, van Zalen MM, Bijlsma EK. Increased nuchal translucency thickness and normal karyotype: time for parental reassurance. Ultrasound Obstet Gynecol. 2007;30(1):11–8. doi: 10.1002/uog.4044. [PubMed] [CrossRef] [Google Scholar]
15. Allen VM, Wilson RD, Cheung A, Genetics Committee of the Society of O, Gynaecologists of C, Reproductive Endocrinology Infertility Committee of the Society of O, et al. Pregnancy outcomes after assisted reproductive technology. J Obstet Gynaecol Can. 2006;28(3):220–50. [PubMed] [Google Scholar]
Interpretation of the results of 1 pregnancy screening
Combined prenatal screening is carried out at 11-14 weeks of gestation with an embryo size of at least 45 mm and not more than 84 mm. This is a comprehensive examination of the fetus to assess the parameters of its development. Its main task is the early detection of fetal malformations, the prevention of childhood disability, and the reduction of infant and child mortality.
The first screening consists of an instrumental part - an ultrasound scan and a laboratory one - a blood test to determine the concentration of chorionic gonadotropin (βhCG) and pregnancy-associated protein A (PAPP-A). The cumulative results of these indicators allow you to plan the tactics of pregnancy management.
Why is the examination carried out at 11-14 weeks
The first trimester is the period of formation of all organs and structures of the body. By the end of the first trimester, the embryonic period ends and the fetal period of fetal development begins. It is in the period from 11 weeks 1 day to 13 weeks 6 days of pregnancy that echographic markers of chromosomal abnormalities are best visualized.
Who needs to be examined
According to the results of the study, it is possible to judge the risk of giving birth to children with chromosomal diseases and congenital malformations, therefore it is recommended to carefully consider the issue and examine all pregnant women. Indications for mandatory prenatal screening of the first trimester are:
Indications for mandatory prenatal screening of the first trimester are:
- Women with a history of spontaneous abortions, ectopic and missed pregnancies, premature birth, stillbirth, birth of a child with developmental anomalies.
- Hereditary diseases in the family of the mother or father of the child
- First trimester illness treated with antibiotics or drugs contraindicated during pregnancy.
- Marriage between relatives.
- The woman is over 35 years of age.
- Presence of occupational hazards
How to prepare
Preparation for the first screening is expressed in a sparing diet. Nutritional errors can affect the general condition of a woman and reduce the accuracy of the results. One week before the examination:
- Salty, spicy, fatty, fried foods should be excluded from the diet.
- Do not eat allergenic foods.
- Avoid carbonated drinks.
One day before screening:
- Do not eat chocolate, seafood, fatty meat, flour, limit sweets.
- If the study is scheduled for the morning, eat a light dinner no later than 20:00 hours.
It is advisable to observe moderate physical activity, if there are no contraindications for this. Walking and proper rest are also important.
Survey
A blood test and ultrasound are performed on the same day to avoid errors due to time differences.
- Ultrasound screening is performed first, as its results allow you to determine the exact gestational age, which affects the normative values of hormone levels. The study is carried out both transabdominally and transvaginally. The procedure is painless, safe for women and children, has no contraindications.
- Blood is donated from a vein on an empty stomach or 4 hours after a meal. The material is taken on the day of the ultrasound. The study determines the concentration of hormones and compares with standard indicators.
Only by deciphering the results of ultrasound and hormone analysis, a conclusion is made about possible risks.
What ultrasound shows
At screening during pregnancy, fetometry of the fetus is performed - determination of the size of body parts and all anatomical structures are evaluated.
The results obtained are compared with a statistical table, which indicates the percentile of falling into the sample of standard values. With indicators less than 5 and more than 95 additional examinations are scheduled.
During an ultrasound examination in the 1st trimester, the following parameters are evaluated: the bones of the cranial vault and the brain, the spine, the anterior abdominal wall, the limbs of the fetus, the structures of the face, the organs of the chest and abdominal cavity, as well as the main echographic markers of chromosomal abnormalities.
Collar space thickness (NTP)
The area between the inner surface of the skin of the fetus and the outer surface of the soft tissues covering the cervical spine. TVP is considered the most important marker of chromosomal abnormalities.
This space begins to decrease after 13 weeks, so it can only be assessed at the first screening.
| Gestational age | Collar thickness in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 0.8 | 1.6 | 2.4 | |
| 12 weeks | 0.7 | 1.6 | 2.5 | |
| 13 weeks | 0. 7 7 | 1.7 | 2.7 | |
The discrepancy between the results and the normative values indicates an increased risk of developing chromosomal pathologies. Depending on the formed set of chromosomes, it can be Down syndrome, Patau, Edwards, Shereshevsky-Turner. To clarify the diagnosis in this case, a biopsy of the chorion or placenta, an analysis of cord blood, and amniotic fluid may be prescribed. Only after additional research can an accurate diagnosis be made.
Coccyx-parietal size (KTR)
Shows the distance between the coccygeal and parietal bones. According to this parameter, the exact gestational age is determined on ultrasound, and the ratio of the mass of the fetus to its CTE is also established.
A slight deviation from the norm indicates the features of the physique and is not a cause for concern.
| Gestational age | Coccyx-parietal size in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 34 | 42 | fifty | |
| 12 weeks | 42 | 51 | 59 | |
| 13 weeks | 51 | 63 | 75 | |
If screening during pregnancy showed results that exceed the norm, this indicates that the fetus is quite large. The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
Skull bones and brain
Already from the 11th week, ultrasound examination can detect defects in the bones of the skull, which indicates severe fetal malformations that are incompatible with life. The evaluation of the brain is based on the study of the so-called "butterfly" - the choroid plexus of the lateral ventricles. A clear visualization and its symmetry indicates the normal development of the brain.
| Gestational age | BPR, LZR in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 13. 19 19 | 17.21 | 21.23 | |
| 12 weeks | 19.22 | 21.24 | 24.26 | |
| 13 weeks | 20.26 | 24.29 | 28.32 | |
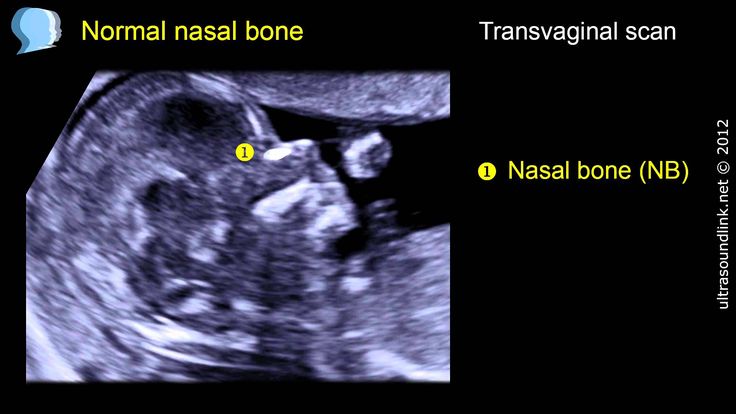
Nasal bone
By the end of the trimester, it should be formed, clearly visualized.
| Gestational age | Nasal bone in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | visualized, not measured | visualized, not measured | visualized, not measured | |
| 12 weeks | 2 | 3. 1 1 | 4.2 | |
| 13 weeks | 2 | 3.1 | 4.2 | |
The pathology of the nasal bone is its absence, hypoplasia (very small size) and a change in its echogenicity.
The diameter of the chest, the circumference of the head and abdomen, the length of the femur also make it possible to judge the proportionality of development.
Heart condition
When examining the heart, its location is assessed, the presence of four chambers of the heart is established - two atria and two ventricles, and their symmetry is assessed. The heart rate is measured.
| Gestational age | Heart rate in beats per minute | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 153 | 165 | 177 | |
| 12 weeks | 150 | 162 | 174 | |
| 13 weeks | 147 | 159 | 171 | |
The venous duct (VP) is a direct communication between the umbilical vein and the central venous system.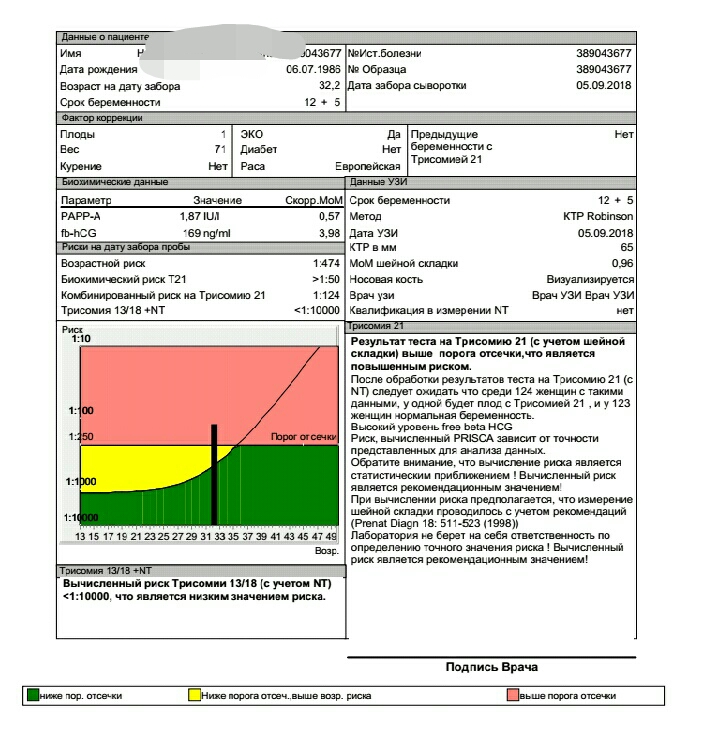 In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
What a blood test shows
Ultrasound results are compared with maternal plasma pregnancy-associated protein A (PAPP-A) and human chorionic gonadotropin (hCG). The values are given in the table:
| Gestational age | hCG in ng/ml | PAPP-A in mU/l |
| 11 weeks | 17.4 - 130.4 | 0.46 - 3.73 |
| 12 weeks | 13.4 - 128.5 | 0.79 - 4.76 |
| 13 weeks | 14.2 - 114.7 | 1. 03 - 6.01 03 - 6.01 |
Differences from the reference values \u200b\u200bmay indicate pathologies of the mother or fetus.
| Deviation | hCG | PAPP-A |
| Above normal |
|
|
| Below normal |
|
|
Survey interpretation
The first study is evaluated only by the totality of all indicators. A single parameter cannot be the basis for an accurate conclusion. The protocol records ultrasound data, hormone analysis, the risks of probable diseases and the complex median coefficient MoM. It indicates the cumulative deviation of the obtained results from the average values. The coefficient must be in the range from 0.5 to 2.5. It is calculated by specialized programs.
What can affect the result
- Incorrect preparation, peculiarities of the woman's condition.
- Obsolete equipment with poor measurement accuracy and insufficient resolution.
- Qualification of the doctor of the ultrasound room, errors in decoding.
- Correctness of MoM calculation algorithms.
Modern diagnostic equipment makes it possible to evaluate more than 15 fetal parameters, build its volumetric reconstruction for examining organs in the early stages of development, and calculate possible risks with high accuracy.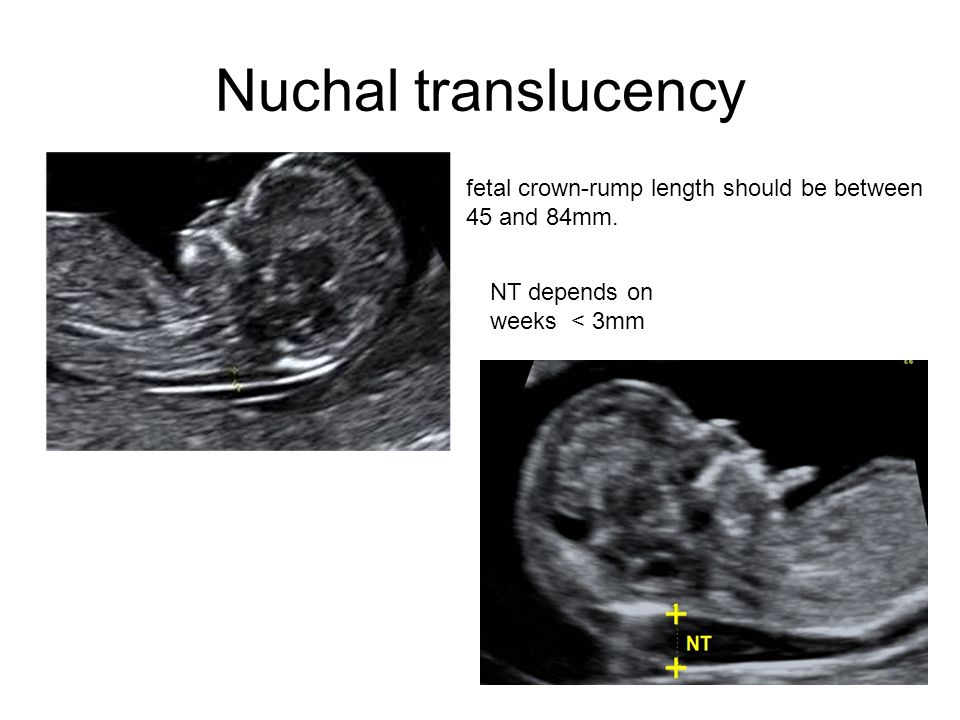 Contact well-equipped clinics and trust specialists with proven qualifications.
Contact well-equipped clinics and trust specialists with proven qualifications.
How to read the first trimester screening
Question: “Hello. Pregnancy 12 weeks. The first ultrasound screening: KTR - 54 mm, TVP (collar space thickness) - 1 mm. The length of the nasal bone is 2.4 mm. Venous circulation is not changed. ( This refers to the blood flow in the venous duct and the fact that there is no reverse blood flow - Guzov II.) "Blood for hCG - 3.59" . (That is, if you look at the MoM, then this is 3.5 times higher than the average median value - Guzov I.I.)
"PAPP-A 0.75 (i.e. slightly reduced). Combined risk for Down's syndrome (i.e. trisomy 21) - 1:244 . Is this very serious? What other examination is needed? Does taking medications Lutein, Metipred affect the result?
Igor Ivanovich Guzov, obstetrician-gynecologist, PhD, founder of the Center for Immunology and Reproduction, answers your questions.
I'll start from the end right away. Taking medication can sometimes affect the result. But Lutein is a drug prescribed, most likely, by an ophthalmologist. Probably, due to the fact that there are some problems with the retina, there may be some trophic changes there. And Metipred was probably prescribed by an obstetrician-gynecologist. Here you need to understand why such therapy is prescribed? It should not affect the analysis results so much directly.
Conclusion: combined screening 1 to 244. You did not write how old you are. Pregnancy 12 weeks.
I just want to show how we analyze and what we prescribe in such cases.
So, this coccygeal-parietal size (KTP) is 54 mm. When calculating risks, it is the main one for determining the gestational age with an accuracy of one day. Because ovulation can come a little earlier, a little later. But there is a fairly stable indicator, which in the period of 11-12 weeks is subject to the smallest spread of fluctuations. Because general biological processes mainly work here, and individual characteristics, differences in fetal growth begin to appear over long periods. And then the coccyx-parietal size is the main indicator for calculating risks, according to which the gestational age is calculated.
But there is a fairly stable indicator, which in the period of 11-12 weeks is subject to the smallest spread of fluctuations. Because general biological processes mainly work here, and individual characteristics, differences in fetal growth begin to appear over long periods. And then the coccyx-parietal size is the main indicator for calculating risks, according to which the gestational age is calculated.
If there is a coccygeal-parietal size, then the risks are calculated in this way: the gestational age is taken (average for a given size), and based on this period, which is calculated according to the KTR, the gestational age is considered.
Can there be any errors here?
Sometimes they can, because the coccyx-parietal size is the size of the baby from the top of the head to the tailbone. Accordingly, it may depend on the degree of flexion of the spine. The child can shrink a little - and then he can shrink a little. It can bend a little - and then it will be a little more.
But in general, it is a fairly reliable indicator by which the gestational age is calculated. When calculating the risks, and this is already a program, the gestational age is considered according to the coccygeal-parietal size. Further, already in relation to this gestational age, all other indicators are calculated.
These figures are 3.59; 0.75 are values expressed in MoM. This is an English abbreviation for multiple of median, which translates as "a multiple of the median".
What do you mean?
Let's say we calculated the gestational age. Let's say it was 11 weeks 3 days, or 11 weeks 4 days, or 12 weeks at the time of the analysis. We get this by the coccyx-parietal size. Within the program, there are figures calculated for each laboratory that characterize the average median value of the indicator for this particular day, calculated by the coccygeal-parietal size.
Next, we compare the biochemical figure that was obtained for the average figure for a given day of pregnancy, and make an adjustment for a number of indicators.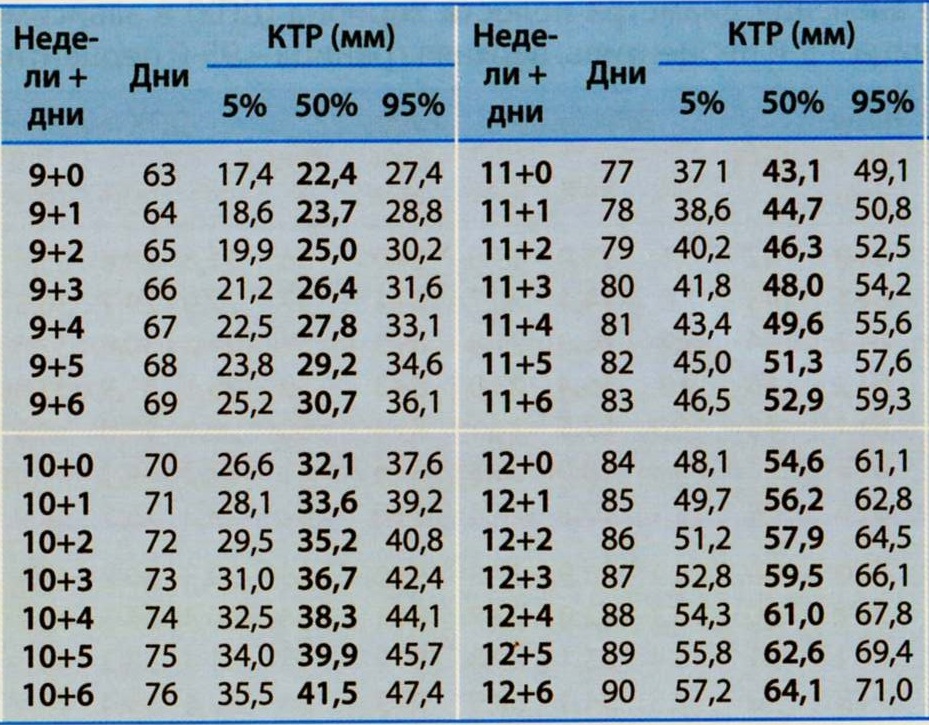 This is, first of all, the weight of a pregnant woman. Race has a certain meaning. The presence of certain factors matters, for example, whether the pregnancy occurred as a result of IVF. There are correction factors depending on whether there is diabetes mellitus and so on.
This is, first of all, the weight of a pregnant woman. Race has a certain meaning. The presence of certain factors matters, for example, whether the pregnancy occurred as a result of IVF. There are correction factors depending on whether there is diabetes mellitus and so on.
There are a number of indicators that the operator enters into the system, places in the appropriate "windows" of the program. As a result, we get MoM. For the program, the thickness values of the collar space are also calculated in MoM. Usually this is not indicated: there is a thickness of the collar space of 1 mm - this thickness of the collar space is translated into MoM, and then MoM goes for mathematical calculation by the program.
The length of the nasal bone is 2.4 mm. This can also be translated into MoMs, but some programs simply take into account "yes" or "not", "+" or "-", whether the nasal bone is or not. It may not be here.
When we analyze all these things, we begin to analyze what the ultrasound shows. Ultrasound examination in your case is good.
Ultrasound examination in your case is good.
The thickness of the collar spaces and is also sometimes called the "neck crease". The collar space is the area of the back of the neck at a given time in a prenatal baby. It shouldn't be too thick. If there is a thickening of this collar space, then this indicates that the area of \u200b\u200bthe back surface of the child's neck may be edematous. This may increase the risks that are calculated by screening associated with Down syndrome. In your case, this is a good value.
Nasal bone in many cases where there is a risk of an increased risk of Down syndrome, it may be either reduced or absent. In this case, the nasal bone is present.
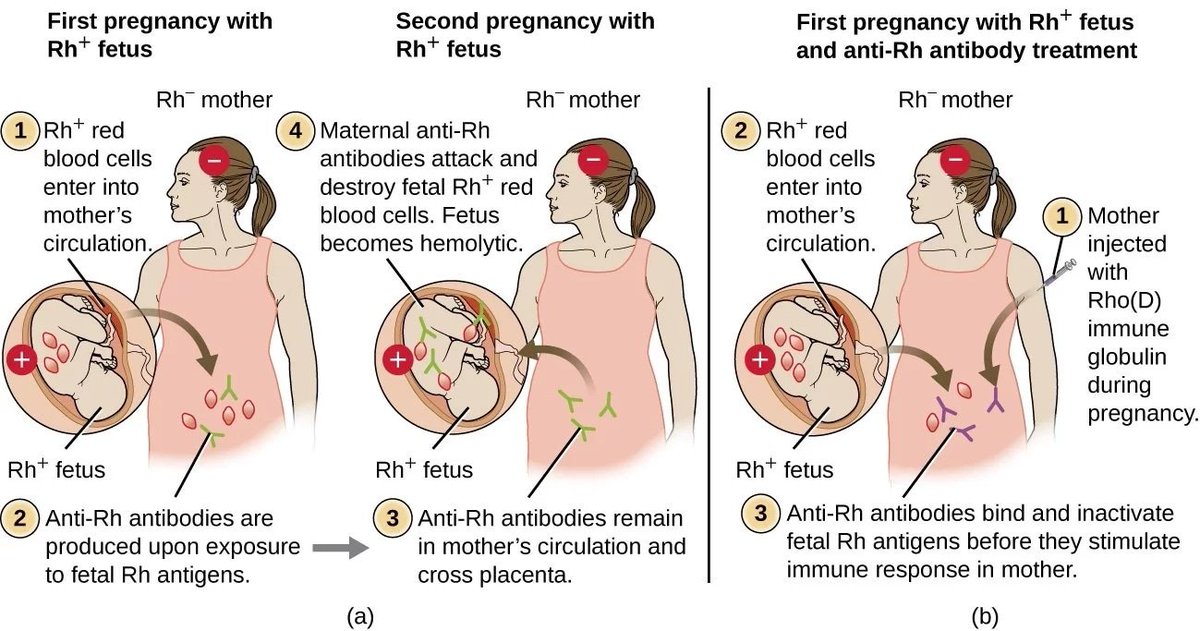
Venous blood flow . You write: "Venous circulation is not changed." This refers to the venous duct. This is such a vessel that exists in the intrauterine fetus, which (if a little primitive) drives blood from the placenta, from the umbilical cord towards the fetal heart.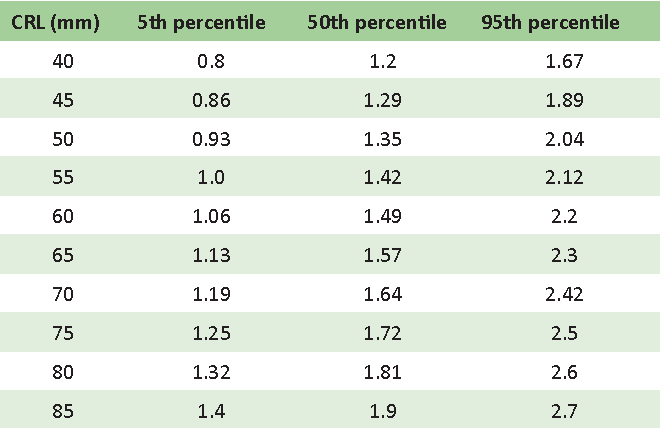
This blood flow must be in one direction, that is, from the umbilical cord towards the fetal heart. Because the child, through this venous duct, actually receives arterial blood, which is further distributed throughout the body. The fetal heart at this stage is very, very small, so if there is a reverse flow, then this reverse flow means that the blood has come to the heart and gone back. This may indicate that there are problems with the emerging valvular apparatus of the heart of the fetus. That is, there is an increased risk of anomalies in the structure of the cardiovascular system, in particular violations of the valvular apparatus.
The child is still very, very small, its size is only 54 mm, it is a small “boy the size of a finger”. We cannot see if he has some kind of valvular disorder or not, but the presence of reversed blood flow, indicating that the blood came to the heart and went back - may indicate the presence of disorders in the formation of the valvular apparatus of the heart in the fetus.
Why does reversed blood flow and nuchal thickening affect the risk of Down syndrome?
This is due to the fact that this trisomy of the 21st pair (Down's syndrome) is often accompanied by a number of anomalies in the child's body, and in a very large percentage of cases there are violations of the formation of the heart and cardiovascular system in the child, that is heart defects can be. And just heart defects can disrupt the blood flow in the body of the fetus, and this will be accompanied by an expansion of the thickness of the collar space and the presence of reverse blood flow.
In the future, always, if we see a reverse flow, we control after 15 weeks of pregnancy on a good ultrasound machine the valvular apparatus. Then we can clearly see whether there are any defects or not. This is what we look at in first trimester screening.
This assessment of the general anatomy of the fetus shows that your baby is well formed, and there are no ultrasound signs that something is going wrong.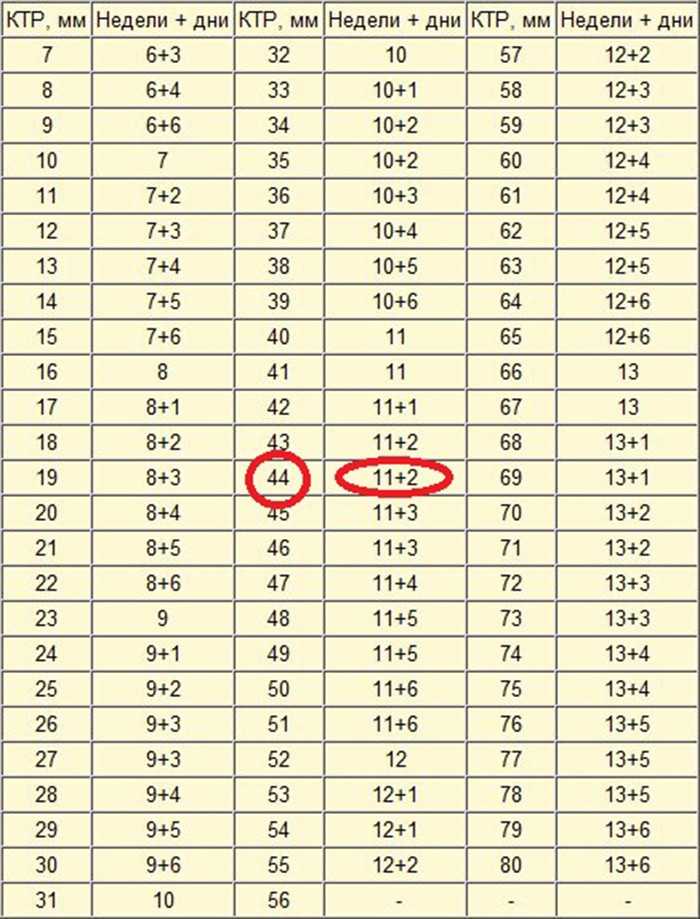
What is missing in ultrasound? And what, according to modern standards, should be included in the ultrasound examination of the first trimester ?
It is imperative to check the blood flow of the uterine arteries, because in this screening we look not only for disorders associated with chromosomal abnormalities. We also look at the risks associated with impaired placental function. Therefore, the determination of blood flow in the uterine arteries, which is absolutely safe for the fetus, is currently, I believe, an indispensable component in ultrasound screening of the first trimester of pregnancy.
If there is a violation, a decrease in uterine blood flow inside the arteries at this time, we can identify increased risks associated with a number of complications in the second half of pregnancy, even longer. These are intrauterine growth retardation, the risk of preeclampsia, the risk of antenatal fetal death, the risk of prematurity for long periods.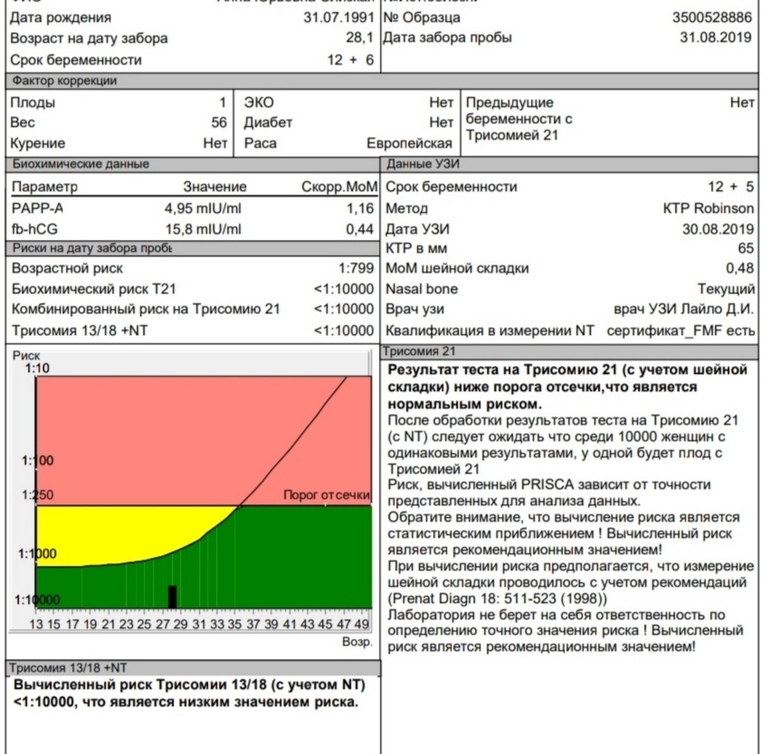
A whole range of these risks can be calculated if we include an additional indicator inside this screening. That is, ultrasound screening includes determining the blood flow of the uterine arteries. This is a very significant moment. We talked about this, but now we are talking about what we need to do in connection with this analysis.
When we evaluate the biochemical risk, we get hCG 3.59. That is, in this case, hCG is 3.6 times higher than the median.
PAPP-A is slightly reduced, 0.75, i.e. 75% of the conditional median.
If we take the direction of all these indicators: an increase in the level of hCG, a slight decrease in the level of PAPP-A, then we have scissors that can be characteristic in their pattern for an increased risk of trisomy 21 pair. But since the risk of trisomy for the 21st pair is a purely algebraic or arithmetic study, that is, several MoMs are laid down: TVP, the presence of a nasal bone, MoM for hCG and MoM for PAPP-A. Accordingly, all this is evaluated together, and we get the total risk - 1 to 244, as if they are telling you that everything is fine, and nothing needs to be done.
It probably is. Because the program thinks so. She thinks stupidly, but this program takes into account the fact that there is a completely normal unaltered structure of the fetus, but it is theoretically possible to assume that there may be a problem associated with some kind of chromosomal anomaly, but there are no heart defects.
And then this ultrasound of normal TP, normal nasal bone, and normal blood circulation can lower the alarm threshold when we get these numbers.
Often the antenatal clinic doctor just looks at the report and says that you are fine, or that you have something. Of course, with such a ratio of indicators, I would simply recommend somehow removing this “worm of doubt” about any problems.
In such a situation, firstly, I would recommend a consultation with a geneticist, and we wrote to you about it. Also, I would still recommend taking, if possible, blood for NIPT. This is exactly the case when NIPT (non-invasive prenatal screening) helps to remove the last “worms of doubt”: what if there is something, some problems regarding chromosomal abnormalities.
With this ratio of indicators, in my opinion, the probability of any chromosomal abnormalities, in particular trisomy 21, has a fairly low risk. But this risk is greater than the average for the population. Your individual risk is 1 in 244, and the population risk could be 1 in 500, 1 in 600. That is, if this individual risk is greater than the population average risk, if you approach this analytically and see what is best to do, I in this case, I would recommend donating blood for NIPT, and if there are no problems with it for the 21st pair, then the issue can be closed. Most likely, everything is fine.
In any case, with such a ratio of indicators, I would recommend an ultrasound examination also at 16 weeks of pregnancy. Just in case, in order to make sure that everything is correctly formed there.
Let's assume that everything will be fine (I'm almost sure that everything will be fine there according to these chromosomal parameters), what else can be associated with a higher than the average for the population figure of hCG?
Why can the level of hCG be 3. 5 times higher?
5 times higher?
Very often the cause is absolutely physiological. Perhaps this is due to the fact that the genes that provide placentation, inherited from the father by the child, work this way. We said in one of our previous conversations that sometimes higher hCG numbers are just a characteristic of some men. Since hCG and the numbers associated with placentation are largely controlled by the genes inherited by the child from his dad. Very often there are higher numbers associated with the fact that the child received such a gene, and is not associated with any chromosomal abnormalities or any other problems.
Our task, the task of the obstetrician-gynecologist, is not to miss the problem. If there are any indicators that can characterize an increase in the risk of problems, it is better to check it. We say that this can be a completely normal option. But what if it could be unrelated to the father's genetics? What other options?
There may also be a situation when there were 2 fertilized eggs.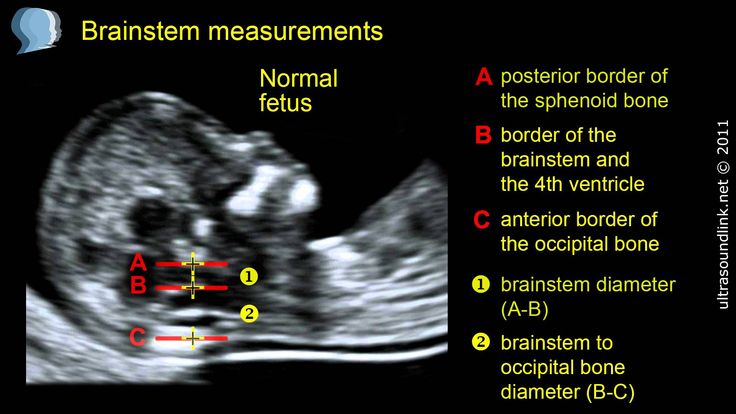 That fertilized egg stopped developing because there was some kind of problem, the second fertilized egg continues to develop. The "vanished twin" may continue to give its increased hCG figure for some time, and this may give an increase to this MoMa. Is it possible.
That fertilized egg stopped developing because there was some kind of problem, the second fertilized egg continues to develop. The "vanished twin" may continue to give its increased hCG figure for some time, and this may give an increase to this MoMa. Is it possible.
It must be remembered that hCG is a human chorionic hormone. During pregnancy, it has its own specific dynamics. It turns out that in the early stages of pregnancy, it begins to be produced literally from the first days of pregnancy. But it begins to enter the mother's blood after implantation after about 7-9 days of pregnancy. At least after 10 days of pregnancy, we already see small positive values. When implantation occurred, there was contact between the mother's body and the child's body, the fetus completely immersed in the uterine mucosa and sent a signal to the mother's body - hCG.
This hormone stops menstruation, causes the corpus luteum (that is, the structure inside the ovary formed after ovulation) to produce progesterone. The first week of pregnancy develops due to the fact that the hormone progesterone, which is very important for it, produced by the corpus luteum inside the ovary, continues to produce progesterone, ensuring the preparation of the uterine mucosa, ensuring the normal development of the fetus in early pregnancy.
The first week of pregnancy develops due to the fact that the hormone progesterone, which is very important for it, produced by the corpus luteum inside the ovary, continues to produce progesterone, ensuring the preparation of the uterine mucosa, ensuring the normal development of the fetus in early pregnancy.
Therefore, as the primary fetal villi develop, when the implantation process is underway, we see a sharp and quite high increase in hCG levels occurring in the first 8-10 weeks of pregnancy. Around this time, it reaches very high values, while ensuring the development of pregnancy.
At the same time, the need for hCG disappears in the baby, because as the placenta forms, the placenta itself begins to produce progesterone.
If we take the concentration of progesterone, then approximately 7-8 weeks of pregnancy is the period when the corpus luteum begins to "lose its ground" and produces less progesterone, and the placenta itself produces more and more progesterone.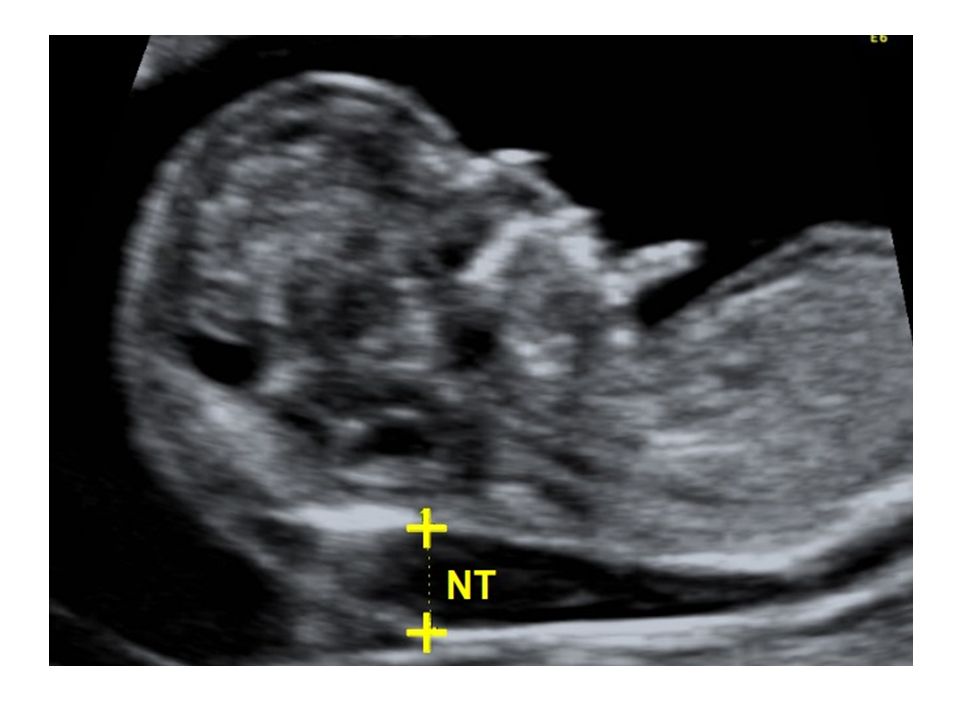 After 11-12 weeks of pregnancy, the production of the corpus luteum does not matter. The placenta produces so much progesterone that there are situations when, for example, some kind of tumor is found on the ovaries and they are removed, and the pregnancy continues to develop normally.
After 11-12 weeks of pregnancy, the production of the corpus luteum does not matter. The placenta produces so much progesterone that there are situations when, for example, some kind of tumor is found on the ovaries and they are removed, and the pregnancy continues to develop normally.
During IVF, when a donor egg is used, when there are no own eggs, that is, the work of the ovary in a woman is completely turned off due to menopause or early menopause, or due to the removal of the ovaries, progesterone support goes up to about 12-13, maybe, 14 weeks. And then this support is not needed, because the child himself, by producing progesterone, fully meets his needs.
And that's why you don't need HCG during these times when you're screening. He starts to fall. If you keep it at higher numbers, then in some cases this is a sign, an “alarm signal”, that something is missing. This is how HCG works.
When we usually evaluate the numbers of such an indicator, we say that it is good that there is a lot of progesterone.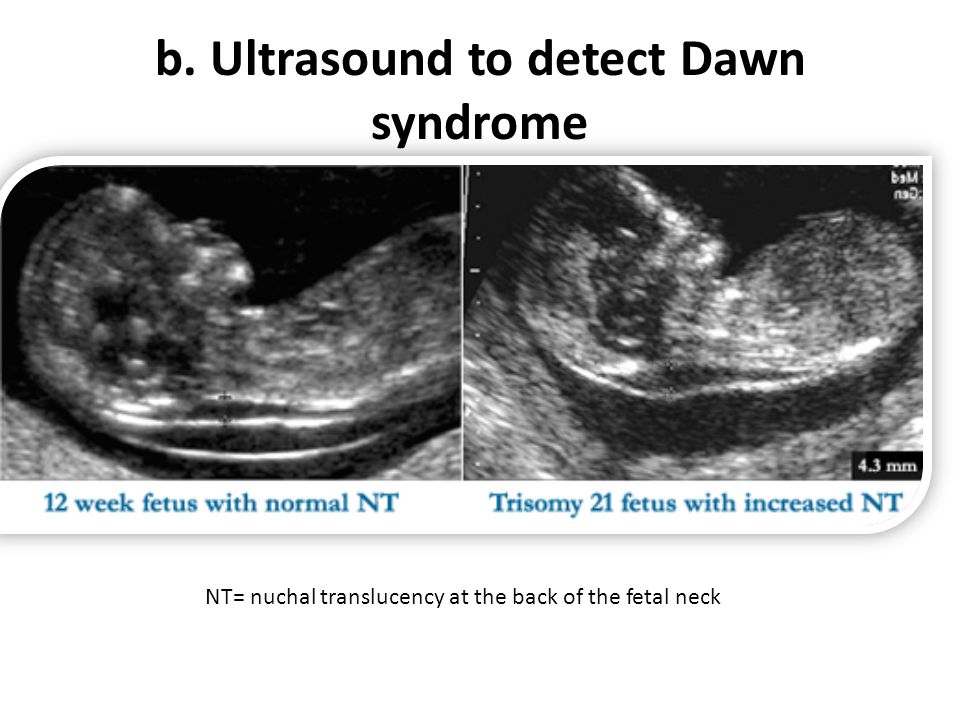 And when there is a lot of hCG, this is often “not healthy”, because the child can give an alarm signal to the mother’s body by giving higher numbers of hCG to the mother’s body.
And when there is a lot of hCG, this is often “not healthy”, because the child can give an alarm signal to the mother’s body by giving higher numbers of hCG to the mother’s body.
I believe that in order for us to be completely sure that everything is going well, it is better to additionally look at the blood flow in the uterine arteries. And look all the same indicator called placental growth factor (PLGF). And then this screening will be complete and complete. And we will not miss the situation, which is typical for an increase in the risk of problems at long stages of pregnancy, we will have time to prescribe the prevention of placental dysfunction. Usually in such cases, low-dose aspirin is prescribed.
This is the standard international practice that I have described. Therefore, I would go this route. And in order to still not guess when the risk of trisomy for the 21st pair is higher than the average risk for the population. Since we now have such a powerful, significant and much more informative study in this regard as NIPT, I would recommend turning it in just in case.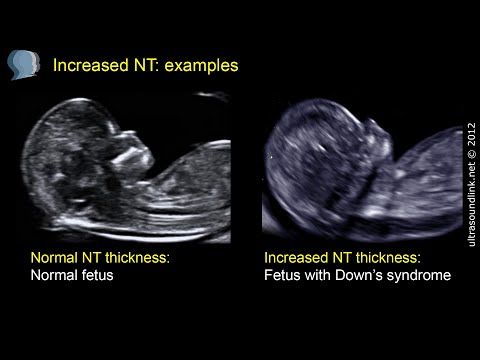 So that you don’t have to constantly think about what happened in the first trimester.
So that you don’t have to constantly think about what happened in the first trimester.
I would recommend doing these things: look at the blood flow in the uterine arteries, get a placental growth factor test, get an NIPT test. Just in order to completely protect you from the risk of all problems, and at the same time predict placental function, do not miss any things.
These are 0.75 MoM according to PAPP-A. PAPP-A is a completely placental indicator that largely characterizes how well the placentation went. It is slightly reduced, but not critically reduced. Usually, if the decrease goes up to 30%, then this fits into the spread of the usual normal values. But still, the "arrow" is rejected downward. Therefore, I did not talk too much on PAPP-A today and did not concentrate your attention. But, in general, here this moment, just in case, also needs to be remembered. I would also arrange for more careful monitoring of placental function.
I showed how, in principle, to analyze this screening.