When does baby head down
Symptoms of Baby Turning Head Down
Your baby kicks, squirms, and flips all day (and night!). But what exactly are they doing in there?
Well, toward the end of your pregnancy, your baby will likely get into a head-down position so that they can begin their descent into the birth canal. The exact timing of when your baby hits this position is individual. And some babies prefer other positions, like breech (head up) or transverse (side lying).
Regardless, some signs can serve as clues about how baby’s relaxing in there. Here’s more about when your baby will move head down, what the options are if they stay head up or in another position, and what to feel for when trying to determine your baby’s position at home.
Related: What Sleeping Position Will Help Turn My Breech Baby?
Most babies tend to shimmy their way into a cephalic (head-first) presentation before birth.
Fast fact
At 28 weeks, around 25 percent of babies are breech (head up), but this number jumps down to just 3 or 4 percent at term.
Your baby may move all over the place in the first and second trimesters. Their position may change wildly early on in the third trimester as well.
However, if you’re between 32 and 36 weeks, you may notice your baby staying put in a head-down position. Your uterus grows to accommodate their size — but there’s only so much room. As time passes, your baby gets bigger and starts to run out of space to move into different positions.
Related: The Third Trimester of Pregnancy: Concerns and Tips
Being head down is just half of the equation when it comes to birth. There’s also the matter of which way your baby is facing.
Why does this make a difference? It comes down to geometry. Your baby’s head must fit through the pelvis on its way into the vaginal canal for delivery. Some positions make this journey easier than others, especially considering how different parts of your baby’s skull are wider and narrower than others.
- Occiput anterior: This position is the most common.
 It means that your baby is head down with their back against your stomach and their chin tucked into their chest.
It means that your baby is head down with their back against your stomach and their chin tucked into their chest. - Occiput posterior: This position means that your baby is head down but facing the opposite direction. In this position, your baby’s back is at your back.
Anterior is the ideal position for an uncomplicated vaginal delivery. When your baby’s chin is tucked, it helps the narrowest part of their head go through the birth canal. Posterior presentation can mean a longer or potentially more difficult delivery, sometimes requiring a vacuum, forceps, or cesarean section.
If your baby is posterior even in early labor, they may still turn throughout the process as contractions move them around in the womb. Some babies completely spin to an anterior position during labor while others are born posterior.
Related: What Your Baby’s Position in the Womb Means
You may not experience any signs that your baby has flipped into a head-down position. There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
Fortunately, your doctor or midwife is trained to feel for your baby’s position using what are called Leopold’s maneuvers.
With this technique, your provider will feel for what part of your baby is presenting in the pelvis, then for your baby’s back, and then for what part of your baby is in your fundus (up high, near your rib cage). They’ll also feel around for your baby’s cephalic prominence, which simply means which way your baby is facing.
With a head-down presentation:
- baby’s head would be in your pelvis
- baby’s back position would depend on whether baby is anterior/posterior, but generally baby will have either their back to your belly (anterior) or your back (posterior)
- baby’s bottom/legs would be in your fundus
All these findings can also be confirmed via ultrasound to give you the clearest picture.
But how can you figure out your baby’s position at home? Pay close attention to the shapes in your belly, as well as the different movements you feel.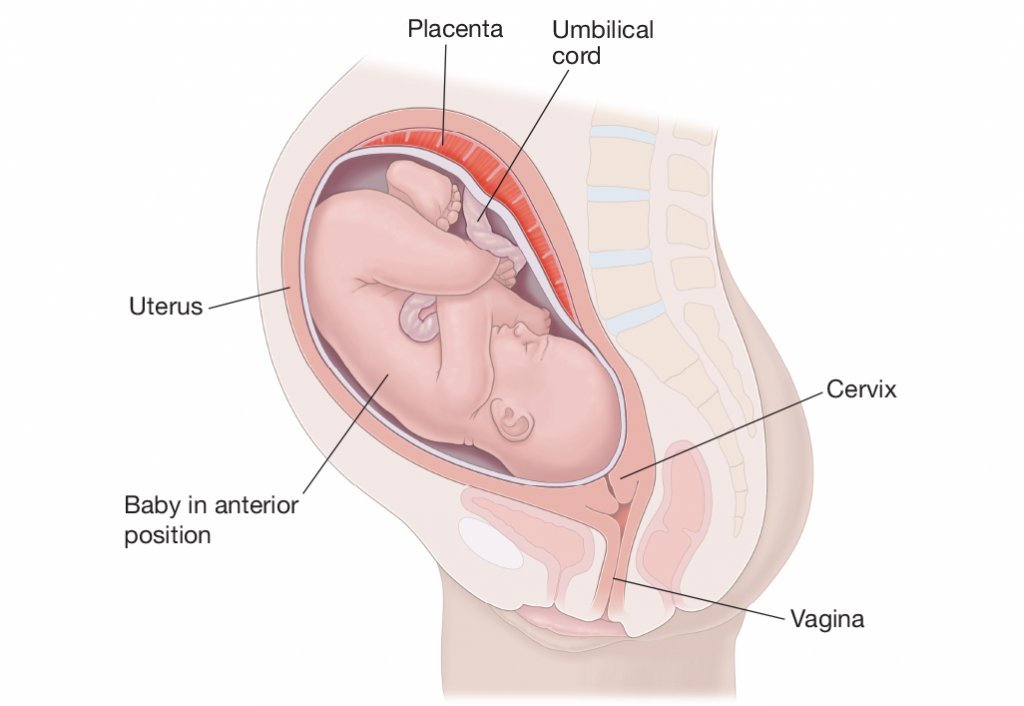
Your baby may be head down if you can:
- feel their head low down in your belly
- feel their bottom or legs above your belly button
- feel larger movements — bottom or legs — higher up toward your rib cage
- feel smaller movements — hands or elbows — low down in your pelvis
- feel hiccups on the lower part of your belly, meaning that their chest is likely lower than their legs
- hear their heartbeat (using an at-home doppler or fetoscope) on the lower part of your belly, meaning that their chest is likely lower than their legs
Belly mapping
It can be difficult to read the different lumps and bumps you feel on your stomach. With practice, you may start to understand what you’re feeling. You might even try belly mapping — a process to estimate baby’s position. It was created by Gaily Tully, certified professional midwife and author of SpinningBabies.com.
To use this technique, wait until you are at least 30 weeks pregnant. You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
Lie down in bed or on the couch. Using a washable marker or finger paint, gently mark where you feel your baby’s head (it feels like a small bowling ball). The arms and hands are likely near the head, and their tiny movements give them away.
Then feel for the back, butt, and legs, as well as larger movements. You may find it helpful to use a baby doll to play with different possible positions. You can then lightly draw or paint your baby on your stomach to help you visualize how they’re lying.
Related: Can You Give Birth with Baby in the Vertex Position?
If you’re in late pregnancy and have concerns about your baby’s positioning, ask your doctor about it at your next prenatal appointment. Chances are that your healthcare provider is making a note of your baby’s position as well.
If your baby is breech or in some other position besides head down, there are several options for delivery. Factors at play here include:
Factors at play here include:
- whether your baby stays in a certain position as you reach term
- any other pregnancy complications you might have
- when you end up going into labor naturally
Wait-and-see approach
Again, your baby’s position isn’t usually a big concern until you reach between 32 and 36 weeks in your pregnancy. Before that point, the fluid in the uterus gives your baby plenty of space to move around. As you get closer to delivery and your baby hasn’t settled head down, they start to run out of room to make the switch.
Your doctor can monitor your baby’s position at your prenatal appointments by feeling your belly for where their head, back, and buttocks are. To confirm, you may also have an ultrasound or pelvic exam.
External cephalic version (ECV)
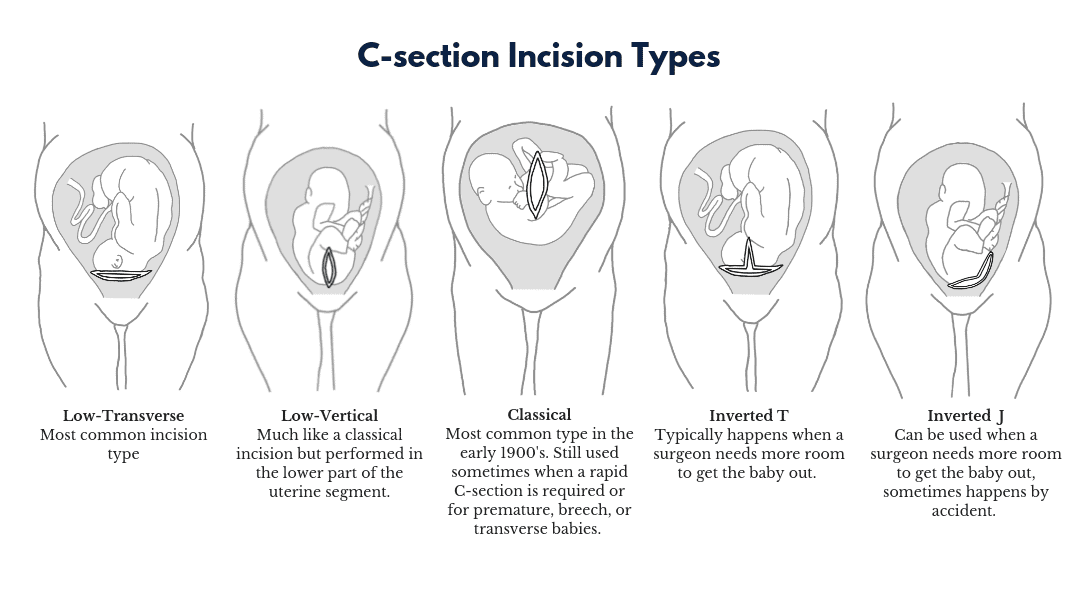
External cephalic version (ECV) is a procedure during which your doctor tries to move your baby into a head-down position to increase the chance you’ll have a vaginal birth. This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
Your provider uses their hands to manually turn the baby head down. If you’ve reached 36 weeks and your baby still isn’t head down, your doctor may suggest an ECV.
The success rate of this procedure is around 58 percent. While that’s not a super impressive statistic, ECV may be worth a try if delivering vaginally is important to you.
It’s also worth noting that some babies that are flipped return to a breech position. You can have a repeat ECV, but space runs out the closer you get to birth, so it may be more difficult the second time.
Cesarean delivery (C-section)
A C-section is another option for delivering babies who aren’t head down. It involves major surgery that you may schedule ahead of time (if you know your baby isn’t head down) or that can be performed in the event you go into labor naturally.
Around 85 percent of breech babies are born via C-section. While this surgery is routine, it involves some risks, including:
While this surgery is routine, it involves some risks, including:
- infection
- postpartum hemorrhage
- blood clots
- issues with future pregnancies, like a risk of placenta previa or uterine rupture
Vaginal birth
The American College of Obstetricians and Gynecologists explains that some women may be candidates for a vaginal birth even if their babies are breech. This possibility is determined on a case-by-case basis and involves a review of your medical history and weighing the benefits of vaginal delivery versus the risks of C-section.
If you choose to go this route, you’ll need to follow any specific guidelines set up by your hospital or birth center.
Related: Midwives Are Growing in Popularity: Here’s What You Need to Know
Your baby moves a lot throughout your pregnancy. As you get closer to your due date, they’ll likely settle into a head-down position as they get ready for birth.
If you have concerns about your baby’s position, don’t hesitate to bring them up at your next prenatal appointment. Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Symptoms of Baby Turning Head Down
Your baby kicks, squirms, and flips all day (and night!). But what exactly are they doing in there?
Well, toward the end of your pregnancy, your baby will likely get into a head-down position so that they can begin their descent into the birth canal. The exact timing of when your baby hits this position is individual. And some babies prefer other positions, like breech (head up) or transverse (side lying).
Regardless, some signs can serve as clues about how baby’s relaxing in there. Here’s more about when your baby will move head down, what the options are if they stay head up or in another position, and what to feel for when trying to determine your baby’s position at home.
Related: What Sleeping Position Will Help Turn My Breech Baby?
Most babies tend to shimmy their way into a cephalic (head-first) presentation before birth.
Fast fact
At 28 weeks, around 25 percent of babies are breech (head up), but this number jumps down to just 3 or 4 percent at term.
Your baby may move all over the place in the first and second trimesters. Their position may change wildly early on in the third trimester as well.
However, if you’re between 32 and 36 weeks, you may notice your baby staying put in a head-down position. Your uterus grows to accommodate their size — but there’s only so much room. As time passes, your baby gets bigger and starts to run out of space to move into different positions.
Related: The Third Trimester of Pregnancy: Concerns and Tips
Being head down is just half of the equation when it comes to birth. There’s also the matter of which way your baby is facing.
Why does this make a difference? It comes down to geometry. Your baby’s head must fit through the pelvis on its way into the vaginal canal for delivery. Some positions make this journey easier than others, especially considering how different parts of your baby’s skull are wider and narrower than others.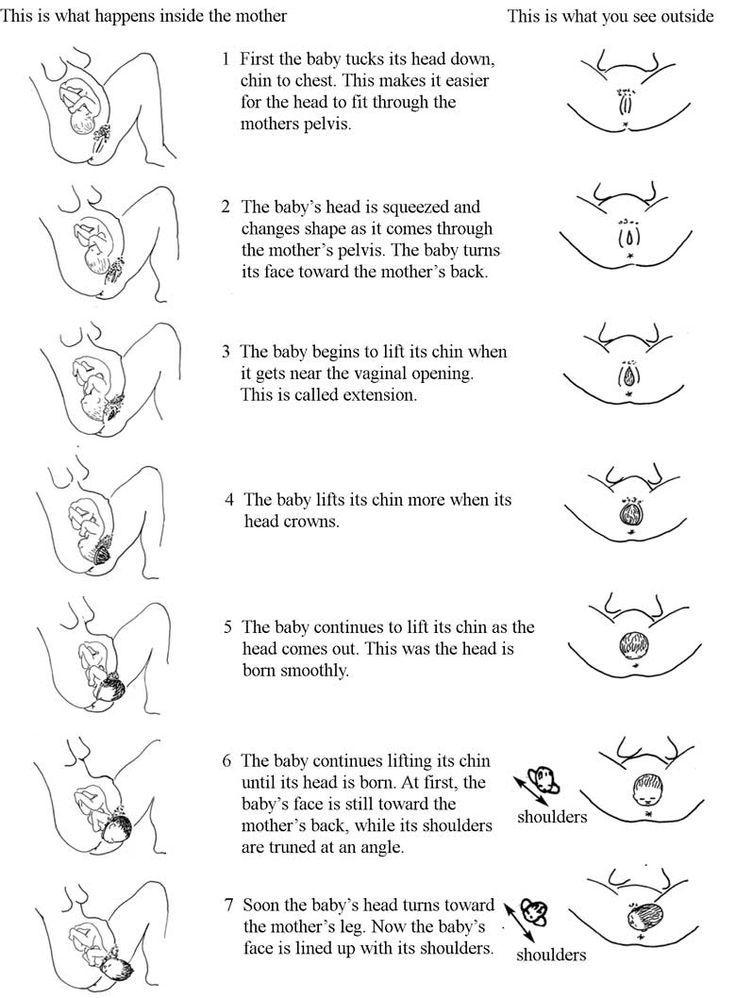
- Occiput anterior: This position is the most common. It means that your baby is head down with their back against your stomach and their chin tucked into their chest.
- Occiput posterior: This position means that your baby is head down but facing the opposite direction. In this position, your baby’s back is at your back.
Anterior is the ideal position for an uncomplicated vaginal delivery. When your baby’s chin is tucked, it helps the narrowest part of their head go through the birth canal. Posterior presentation can mean a longer or potentially more difficult delivery, sometimes requiring a vacuum, forceps, or cesarean section.
If your baby is posterior even in early labor, they may still turn throughout the process as contractions move them around in the womb. Some babies completely spin to an anterior position during labor while others are born posterior.
Related: What Your Baby’s Position in the Womb Means
You may not experience any signs that your baby has flipped into a head-down position. There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
Fortunately, your doctor or midwife is trained to feel for your baby’s position using what are called Leopold’s maneuvers.
With this technique, your provider will feel for what part of your baby is presenting in the pelvis, then for your baby’s back, and then for what part of your baby is in your fundus (up high, near your rib cage). They’ll also feel around for your baby’s cephalic prominence, which simply means which way your baby is facing.
With a head-down presentation:
- baby’s head would be in your pelvis
- baby’s back position would depend on whether baby is anterior/posterior, but generally baby will have either their back to your belly (anterior) or your back (posterior)
- baby’s bottom/legs would be in your fundus
All these findings can also be confirmed via ultrasound to give you the clearest picture.
But how can you figure out your baby’s position at home? Pay close attention to the shapes in your belly, as well as the different movements you feel.
Your baby may be head down if you can:
- feel their head low down in your belly
- feel their bottom or legs above your belly button
- feel larger movements — bottom or legs — higher up toward your rib cage
- feel smaller movements — hands or elbows — low down in your pelvis
- feel hiccups on the lower part of your belly, meaning that their chest is likely lower than their legs
- hear their heartbeat (using an at-home doppler or fetoscope) on the lower part of your belly, meaning that their chest is likely lower than their legs
Belly mapping
It can be difficult to read the different lumps and bumps you feel on your stomach. With practice, you may start to understand what you’re feeling. You might even try belly mapping — a process to estimate baby’s position. It was created by Gaily Tully, certified professional midwife and author of SpinningBabies.com.
To use this technique, wait until you are at least 30 weeks pregnant. You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
Lie down in bed or on the couch. Using a washable marker or finger paint, gently mark where you feel your baby’s head (it feels like a small bowling ball). The arms and hands are likely near the head, and their tiny movements give them away.
Then feel for the back, butt, and legs, as well as larger movements. You may find it helpful to use a baby doll to play with different possible positions. You can then lightly draw or paint your baby on your stomach to help you visualize how they’re lying.
Related: Can You Give Birth with Baby in the Vertex Position?
If you’re in late pregnancy and have concerns about your baby’s positioning, ask your doctor about it at your next prenatal appointment. Chances are that your healthcare provider is making a note of your baby’s position as well.
If your baby is breech or in some other position besides head down, there are several options for delivery. Factors at play here include:
Factors at play here include:
- whether your baby stays in a certain position as you reach term
- any other pregnancy complications you might have
- when you end up going into labor naturally
Wait-and-see approach
Again, your baby’s position isn’t usually a big concern until you reach between 32 and 36 weeks in your pregnancy. Before that point, the fluid in the uterus gives your baby plenty of space to move around. As you get closer to delivery and your baby hasn’t settled head down, they start to run out of room to make the switch.
Your doctor can monitor your baby’s position at your prenatal appointments by feeling your belly for where their head, back, and buttocks are. To confirm, you may also have an ultrasound or pelvic exam.
External cephalic version (ECV)
External cephalic version (ECV) is a procedure during which your doctor tries to move your baby into a head-down position to increase the chance you’ll have a vaginal birth. This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
Your provider uses their hands to manually turn the baby head down. If you’ve reached 36 weeks and your baby still isn’t head down, your doctor may suggest an ECV.
The success rate of this procedure is around 58 percent. While that’s not a super impressive statistic, ECV may be worth a try if delivering vaginally is important to you.
It’s also worth noting that some babies that are flipped return to a breech position. You can have a repeat ECV, but space runs out the closer you get to birth, so it may be more difficult the second time.
Cesarean delivery (C-section)
A C-section is another option for delivering babies who aren’t head down. It involves major surgery that you may schedule ahead of time (if you know your baby isn’t head down) or that can be performed in the event you go into labor naturally.
Around 85 percent of breech babies are born via C-section. While this surgery is routine, it involves some risks, including:
While this surgery is routine, it involves some risks, including:
- infection
- postpartum hemorrhage
- blood clots
- issues with future pregnancies, like a risk of placenta previa or uterine rupture
Vaginal birth
The American College of Obstetricians and Gynecologists explains that some women may be candidates for a vaginal birth even if their babies are breech. This possibility is determined on a case-by-case basis and involves a review of your medical history and weighing the benefits of vaginal delivery versus the risks of C-section.
If you choose to go this route, you’ll need to follow any specific guidelines set up by your hospital or birth center.
Related: Midwives Are Growing in Popularity: Here’s What You Need to Know
Your baby moves a lot throughout your pregnancy. As you get closer to your due date, they’ll likely settle into a head-down position as they get ready for birth.
If you have concerns about your baby’s position, don’t hesitate to bring them up at your next prenatal appointment. Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Scientists named signs of giftedness in children
How to discern a capable child? When is the "golden period" for the development of talents in children? What is the "age of questions"? These and other questions of "RG" are answered by the leading researcher of the laboratory of psychology of giftedness of the Psychological Institute of the Russian Academy of Education Elena Belova.
Elena Sergeevna, a high school student from Yekaterinburg, who memorized and wrote more than 13 thousand numbers after the decimal point from the Pi sign, got into the Russian Book of Records. There are kids who, by the age of 2-3, know the multiplication table, the capitals of all countries. Are they gifted kids?
Elena Belova: Giftedness and learning outcomes, training are two different things. If you show the letters of the alphabet and repeat the names to a two-year-old child every day, in a month or earlier he will know a lot by heart. But it will not be knowledge that will please him, but the approval of adults. A gifted child is ready to give up sweets, walks, and sleep for the sake of a new book, a favorite pastime. The main component of giftedness is a high creative potential. It allows you to think outside the box, unconventional, find original solutions and can manifest itself already in preschool childhood. No wonder the age from 5 to 8 years is called the "golden period" of the development of children's creativity. About 20 percent of today's preschoolers have a high creative potential. However, the disclosure of this potential can be delayed and even ruined at any stage of development.
If you show the letters of the alphabet and repeat the names to a two-year-old child every day, in a month or earlier he will know a lot by heart. But it will not be knowledge that will please him, but the approval of adults. A gifted child is ready to give up sweets, walks, and sleep for the sake of a new book, a favorite pastime. The main component of giftedness is a high creative potential. It allows you to think outside the box, unconventional, find original solutions and can manifest itself already in preschool childhood. No wonder the age from 5 to 8 years is called the "golden period" of the development of children's creativity. About 20 percent of today's preschoolers have a high creative potential. However, the disclosure of this potential can be delayed and even ruined at any stage of development.
How can parents understand whether they have a gifted child or an ordinary one?
Elena Belova: Pay attention to how your child explores the world around them. There is evidence that gifted children in the early stages of development - up to 2-3 years old - have a more persistent and pronounced reaction to a new object, sound, image. New toys delight everyone, but one child will forget about the toy in an hour, and the other will try to study it better - throw it up, twist it, lower it into the water, cover it with a rug ... Speech is the most important indicator of development. Children have a so-called age of questions - from about two and a half to three and a half years. It is difficult to distinguish this age among the gifted. They ask a lot of questions all the time. Topics are deeper, and topics are broader. For example, a child at the age of four may be interested in how a computer or TV works, memorize chess combinations.
There is evidence that gifted children in the early stages of development - up to 2-3 years old - have a more persistent and pronounced reaction to a new object, sound, image. New toys delight everyone, but one child will forget about the toy in an hour, and the other will try to study it better - throw it up, twist it, lower it into the water, cover it with a rug ... Speech is the most important indicator of development. Children have a so-called age of questions - from about two and a half to three and a half years. It is difficult to distinguish this age among the gifted. They ask a lot of questions all the time. Topics are deeper, and topics are broader. For example, a child at the age of four may be interested in how a computer or TV works, memorize chess combinations.
What if you take tests that will tell you whether you have a miracle child or not?
Elena Belova: First, answer the question: why do you need to identify giftedness? To satisfy your own vanity, in order to relieve anxiety (all children are like children, but mine is not like that), for psychological help, in order to create conditions for the development of abilities?
Of course, for the development of abilities!
Elena Belova: Here is the simplest questionnaire for parents and teachers.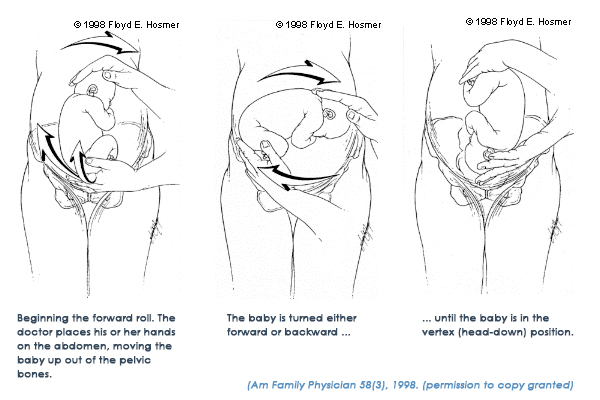 Answer "yes" or "no" to five statements. 1. The child is proactive, lively, mobile. 2. He readily responds to everything new. 3. Curious, loves everything mysterious, incomprehensible. 4. Often needs the support of elders. 5. Shows the ability to concentrate for a longer period of time than peers. Did you answer "yes" to all questions? There are reasons to consider the child capable. The use of serious tests requires professional training, so it is better to contact specialists.
Answer "yes" or "no" to five statements. 1. The child is proactive, lively, mobile. 2. He readily responds to everything new. 3. Curious, loves everything mysterious, incomprehensible. 4. Often needs the support of elders. 5. Shows the ability to concentrate for a longer period of time than peers. Did you answer "yes" to all questions? There are reasons to consider the child capable. The use of serious tests requires professional training, so it is better to contact specialists.
And keep in mind that gifted children can be very sensitive, vulnerable.
8 percent of preschoolers and primary school children admitted that they cannot live without gadgets...
Elena Belova: them fade into the background. We cannot completely remove gadgets, but if we do not develop the creative potential of the child, it will hardly be possible to talk about giftedness. What's in Gadgets? Ready-made instructions, a series of changing sensory impressions instead of independent play, active creativity and communication with close adults. Perhaps gadgets contribute to the development of attention, memory, reaction speed, and the accumulation of visual experience. How useful this will be when initiative and independence are required is a question.
Perhaps gadgets contribute to the development of attention, memory, reaction speed, and the accumulation of visual experience. How useful this will be when initiative and independence are required is a question.
...For your gifted children to grow up financially wealthy as well - read excerpt from Yakov Mirkin's book published in today's issue.
By the way
Considered stupid...
Thomas Alve Edison neighbors, acquaintances, teachers considered mediocre child. He was absent-minded, studied poorly, and in addition had hearing problems. His parents had to pick him up from school.
Photo: Gettyimages
Ilya Mechnikov was known as a loser in his childhood, he endured ridicule from his brothers and their contemptuous attitude. The only place where he was head and shoulders above everyone else was botanism. He paid 2 kopecks to the brothers just for them to listen to him.
Photo: Gettyimages
.
 ..and idolized
..and idolized Sergei Prokofiev was an adored child in the family, his parents became his first teachers in Russian, arithmetic, geography, history. By the age of 6 he had already written three plays.
Photo: Gettyimages
Charles Gounod was multi-talented: he composed sacred music, drew beautifully and wrote talentedly. His parents were also extraordinary people and supported their son.
Photo: Gettyimages
Specifically
How to help reveal your creative abilities
1. Take your child for a walk, even if he is still in a stroller, put your phone in your pocket. Try to talk as much as possible with the child, show and name what surrounds him: "This is a tree, it is big, tall, this is a flower, look how beautiful it is!" The child's vocabulary begins to grow long before the child begins to speak.
2. Read books to your child, saying all the words. Pay attention to the illustrations, details. Ask: "Who is the bunny looking at?", "Where did the fox run?" and so on. The child is silent and does not answer? Give the answer yourself: "The bunny looks at the house (wolf, grove ...)", "The fox runs to the lake (into the forest, on the path ...)".
Ask: "Who is the bunny looking at?", "Where did the fox run?" and so on. The child is silent and does not answer? Give the answer yourself: "The bunny looks at the house (wolf, grove ...)", "The fox runs to the lake (into the forest, on the path ...)".
3. When active speech begins, watch how it develops. Speech disorders are usually very closely related to the functioning of the brain. Remember: gifted children may speak later than usual, but they begin to speak a lot at once and quite correctly. But if there is still no speech at the age of three, perhaps this is a reason to turn to a speech therapist.
4. Preschool age - the age of play. When buying new toys, prioritize those that allow your child to use them creatively.
5. Keep a diary of your child's development; until the age of 7, development proceeds at a gigantic pace. Write down the ideas, sayings, writings of the baby. Be attentive to all his creative manifestations!
Meanwhile
An account in favor of Kamilla
Recently, on one of the TV programs about the unusual abilities of children, Kamilla Aliyeva from Dagestan amazed the presenter. The girl does mental arithmetic and solves two thousand examples in her mind in 20 minutes! How does a 12-year-old girl do all this?
The girl does mental arithmetic and solves two thousand examples in her mind in 20 minutes! How does a 12-year-old girl do all this?
Photo: 1tv.ru
The basis is training with the help of a special counting board (abacus) like the one that all accountants used to have. Abacus is still different from the usual accounting board. For example, there can be 13, 15 or even 17 knitting needles. First, the child learns to count on these accounts, and then simply imagines them in his mind. Teachers recommend starting to do mental arithmetic as early as possible - from 4-5 years old, when the brain is most plastic. It is believed that this helps to develop both hemispheres at once: the child has a photographic memory, the ability to concentrate. But there are also disadvantages. Among them - overload, the desire to do everything as quickly as possible. And most importantly, how do you apply your quick counting skills later? After all, you can't overtake a computer anyway.
A cold in a child: how to treat it correctly
Shcherbakova Alla Anatolievna
Pediatrician
Clinic "Mother and Child" Savelovskaya
Many parents are ready for the fact that babies will pick up common, including seasonal infections, which is typical for childhood. Some parents study the methods of treating SARS and colds in advance, read about it from experienced mothers in blogs and diaries, consult with doctors they know, and watch medical programs. But even despite the fact that the child's body has a powerful immune system from birth, this protection is imperfect. Therefore, no matter how informed the mother is, when the child becomes ill, she has a lot of questions that require qualified answers.
Some parents study the methods of treating SARS and colds in advance, read about it from experienced mothers in blogs and diaries, consult with doctors they know, and watch medical programs. But even despite the fact that the child's body has a powerful immune system from birth, this protection is imperfect. Therefore, no matter how informed the mother is, when the child becomes ill, she has a lot of questions that require qualified answers.
What are acute respiratory infections and SARS
Most often, children experience acute respiratory diseases, abbreviated as acute respiratory infections or colds. This is especially evident when visiting children's groups, where they come into contact with other kids and actually exchange various pathogens. The mothers of "kindergarten" children are very familiar with the phrase: "We go for 2 days, then 2 weeks - on sick leave."
A cold can be both viral and bacterial, even fungal and of a different nature, in 70-80% of cases it is of a viral nature.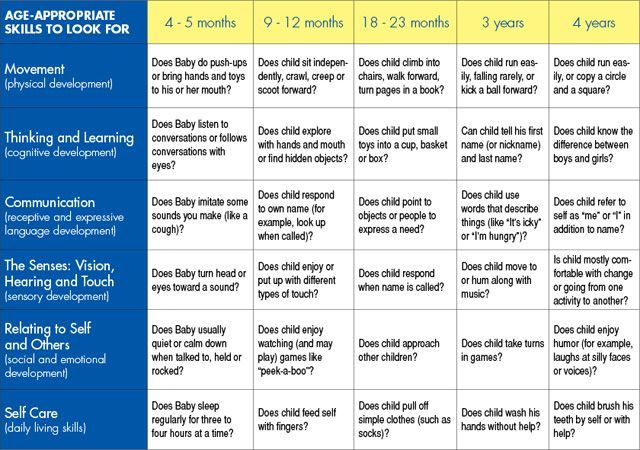 It is impossible to establish the origin of a cold with accuracy on a pediatric examination, as well as "by eye" to distinguish one infection from another. However, there are certain signs that indicate the action of viruses, harmful bacteria and other pathogens. For example, mucous nasal discharge testifies in favor of an acute respiratory viral infection, which usually begins with a slight malaise, loss of appetite, capriciousness, sleep disturbance in a child. This is a prodromal period, it lasts from several hours to 1-2 days. And such a viral infection as the flu begins acutely, immediately with a very high temperature, intoxication, there is almost no prodromal period, dry cough appears in the late stages of the disease. Often ARVI goes away with catarrhal symptoms: nasal congestion, change in tone of voice, "circles", "blue" under the eyes, runny nose, cough, sore throat and swallowing.
It is impossible to establish the origin of a cold with accuracy on a pediatric examination, as well as "by eye" to distinguish one infection from another. However, there are certain signs that indicate the action of viruses, harmful bacteria and other pathogens. For example, mucous nasal discharge testifies in favor of an acute respiratory viral infection, which usually begins with a slight malaise, loss of appetite, capriciousness, sleep disturbance in a child. This is a prodromal period, it lasts from several hours to 1-2 days. And such a viral infection as the flu begins acutely, immediately with a very high temperature, intoxication, there is almost no prodromal period, dry cough appears in the late stages of the disease. Often ARVI goes away with catarrhal symptoms: nasal congestion, change in tone of voice, "circles", "blue" under the eyes, runny nose, cough, sore throat and swallowing.
What to do?
First of all, you need to remember that parents should not panic if the child has a fever and other unpleasant symptoms of a cold. Any mood of the mother is transmitted to the baby. A cold with a competent approach is simply MUST go away in 5-7 days without complications. And it is important to know that the treatment of a cold is complex, which includes the main drugs - antiviral, antibacterial, etc., as well as symptomatic therapy. You should not rely on just one kind of medicine as a panacea, a magic pill from an advertisement or the advice of a pharmacy worker.
Any mood of the mother is transmitted to the baby. A cold with a competent approach is simply MUST go away in 5-7 days without complications. And it is important to know that the treatment of a cold is complex, which includes the main drugs - antiviral, antibacterial, etc., as well as symptomatic therapy. You should not rely on just one kind of medicine as a panacea, a magic pill from an advertisement or the advice of a pharmacy worker.
How to treat?
- Antivirals. Now there is a lot of false information regarding antiviral drugs. They are credited with mythical side effects and actions. If this comes from a doctor, then he must provide data confirming his point of view in official sources, which are state medical institutions, major scientific journals.
- Antibiotics. As for antibiotics, their use is currently limited by very clear indications, contraindications, age of the patient, etc. In addition, antibiotics, especially with uncontrolled, frequent use, contribute to the formation of new strains of harmful bacteria that are difficult to treat.
 Usually, against the background of antibiotic treatment, it is customary to prescribe biological products - live microbes that make up the human intestinal microflora. But there is an opinion that the antibiotic has a detrimental effect on these bacteria, and such therapy does not bring the desired result.
Usually, against the background of antibiotic treatment, it is customary to prescribe biological products - live microbes that make up the human intestinal microflora. But there is an opinion that the antibiotic has a detrimental effect on these bacteria, and such therapy does not bring the desired result. - Auxiliaries. In the treatment of colds of any origin, symptomatic therapy is used, the action of which is directed against the symptoms of the disease. They are called auxiliary, as they help to alleviate the course of a cold. They do not get rid of the cause of SARS, but the child's own antibodies work against viruses.
- How to treat a runny nose? In case of a runny nose, a nasal toilet with saline solutions is performed. The procedure is simple, but requires certain skills and caution. To do this, you should seat the child with his back to him, first clean his nose. For babies, this can be done with cotton buds (for children under six months old, only with ordinary cotton turundas), and at an older age, children can already blow their nose.
 After that, you need to raise your chin, holding the child’s face with your palm in a raised state. Using a pipette, drip a saline solution into both nasal passages, lower the child's head forward. Part of the medicine may spill out of the nose, but the result of such a procedure will still be achieved. If there are no special recommendations from the pediatrician of the sick child, you can use a pipette and normal saline. But it is preferable with a sterile solution based on sea water. It is a delusion to think that washing a child's nose will be addictive or the snot will flow out on its own. Part, of course, can leak out, but if you do not clean your nose, there is a high risk of infection spreading to the underlying airways, the development of complications such as inflammation of the trachea, bronchi, and lungs.
After that, you need to raise your chin, holding the child’s face with your palm in a raised state. Using a pipette, drip a saline solution into both nasal passages, lower the child's head forward. Part of the medicine may spill out of the nose, but the result of such a procedure will still be achieved. If there are no special recommendations from the pediatrician of the sick child, you can use a pipette and normal saline. But it is preferable with a sterile solution based on sea water. It is a delusion to think that washing a child's nose will be addictive or the snot will flow out on its own. Part, of course, can leak out, but if you do not clean your nose, there is a high risk of infection spreading to the underlying airways, the development of complications such as inflammation of the trachea, bronchi, and lungs.
If the runny nose is profuse, watery, painful, accompanied by nasal congestion, vasoconstrictor drugs (based on oxymetazoline, xylometazoline) are used in the form of drops at bedtime, before walking with a child. This helps the baby to have a good rest in a dream without waking up, and on a walk it is normal to breathe through the nose without taking cold air into the mouth. It should not be instilled into the nose of a child in a supine state, since there is a high probability of a change in pressure during such manipulation and there is a risk of otitis media. All instillations must be done while sitting. The use of special preparations in the form of soft (spray with limited jet pressure) should be carried out with great care, since there is also a risk of promoting the spread of infection under pressure.
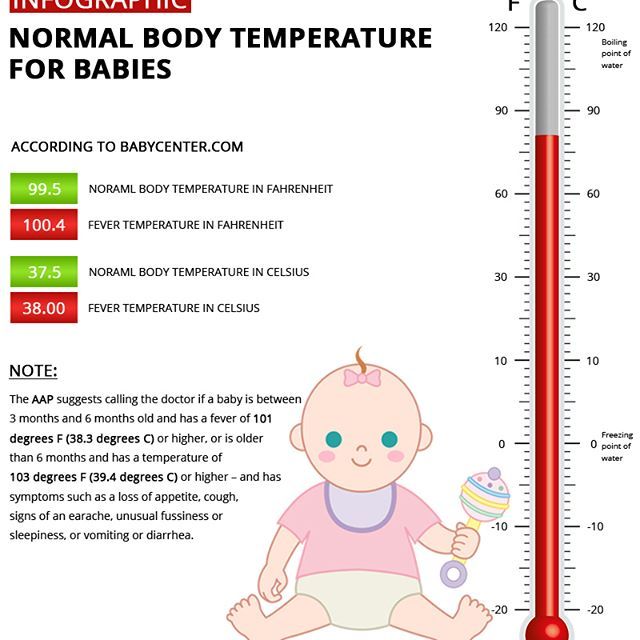
This helps the baby to have a good rest in a dream without waking up, and on a walk it is normal to breathe through the nose without taking cold air into the mouth. It should not be instilled into the nose of a child in a supine state, since there is a high probability of a change in pressure during such manipulation and there is a risk of otitis media. All instillations must be done while sitting. The use of special preparations in the form of soft (spray with limited jet pressure) should be carried out with great care, since there is also a risk of promoting the spread of infection under pressure. - Antipyretics. Often there are questions about the use of antipyretics, for children - these are drugs based on paracetamol or ibuprofen, for babies - in syrup, suppositories. It should be noted that if there are no special recommendations in this regard, it is necessary to reduce the temperature above 38.3-38.5°C. If the child feels well, plays, has an appetite, and, in general, tolerates temperature well, antipyretic drugs can not be used.
 If parents see that the child's condition is bad, he refuses to eat and drink, becomes lethargic, vomiting occurs, headache, the temperature rises further, you can start giving antipyretics even at a low temperature.
If parents see that the child's condition is bad, he refuses to eat and drink, becomes lethargic, vomiting occurs, headache, the temperature rises further, you can start giving antipyretics even at a low temperature. - How to treat a cough? Questions about cough are the most frequent and sometimes the most difficult at a pediatric appointment for SARS. It is best if the doctor dynamically observes the coughing child. In this case, the specialist can distinguish changes in the tone of the voice, a barking component, a dry or wet cough, wheezing, localization of wheezing. If the pediatrician recommends taking an x-ray, you should not refuse such an examination, this will help to make the correct diagnosis and prescribe adequate treatment. Currently, in the treatment of cough, inhalation drugs are widely used - through a special device - an inhaler. This tactic reduces the systemic effect of the drug on the child's body, where the drug reaches the point of its application - large and medium bronchi, and even alveoli.
 Inhalers can be used from the very birth of a child, but it is necessary to pay attention to the type of device, the medicinal substances recommended for it, their dosages and frequency of use.
Inhalers can be used from the very birth of a child, but it is necessary to pay attention to the type of device, the medicinal substances recommended for it, their dosages and frequency of use.
Activities before the doctor arrives
Sometimes, especially during the season of high incidence of influenza and colds, there are difficulties with a doctor's visit, you have to wait for an appointment, the doctor does not have time to come as quickly as parents would like. There are measures that can be taken before the arrival of a specialist. It is necessary to measure the temperature of the child and write down the data on the thermometry carried out in a diary, which is then shown to the doctor. If the temperature is high, do not wrap or even dress the child warmly. At home, you can generally strip to your underwear. Disposable diapers are also recommended to be removed from infants. Do not forget about physical methods of cooling - you can wipe it with cool water, you can put a cloth moistened with water on your head, stomach, places of the main vessels.