Herpes medicine while pregnant
Genital Herpes Suppressive Treatment in Pregnancy
Genital Herpes Suppressive Treatment in PregnancyMedically reviewed by Aleah Rodriguez, PharmD — By the Healthline Medical Network on March 15, 2012
Overview
The primary goal of genital herpes management during pregnancy is to prevent infection in the baby. Women with herpes lesions during delivery are at the highest risk of transmitting the infection to their baby. If you tend to have recurrent herpes lesions, your doctor will most likely discuss the risks and benefits of using suppressive treatment toward the end of your pregnancy. Suppressive treatment can help decrease your risk of recurrent lesions and other symptoms. This can reduce your risk of transmitting genital herpes to your baby during delivery.
Suppressive treatment drugs in pregnancy
Your doctor may recommend suppressive therapy during pregnancy to help reduce your number of herpes outbreaks, especially if you have six or more episodes per year. Long-term suppressive therapy can significantly reduce these outbreaks and is likely safe during pregnancy.
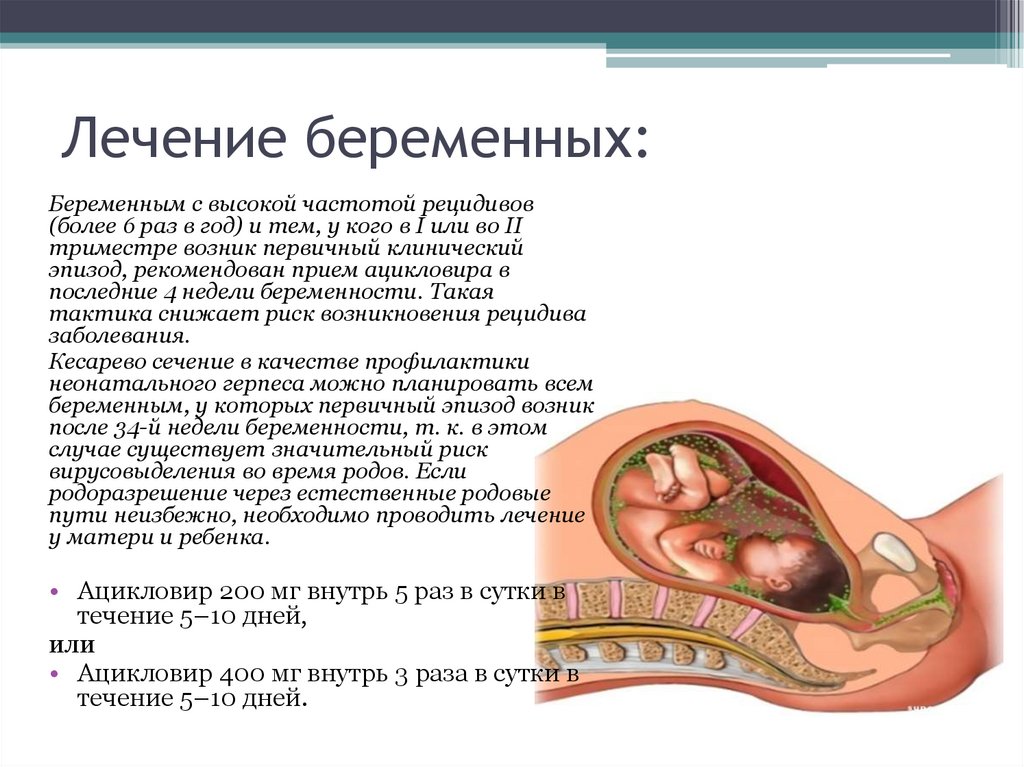
Acyclovir (Zovirax) and valacyclovir (Valtrex) are the drugs most commonly used for herpes outbreak suppression and treatment during pregnancy. These drugs help reduce how active the virus is. They also help speed up lesion healing. They may also decrease the chance of active lesions at the time of labor. In turn, this decreases the likelihood of needing a cesarean delivery to avoid virus transmission.
No evidence links acyclovir or valacyclovir to serious side effects in infants born to mothers who took these drugs during pregnancy.
Treatment with these drugs usually starts around the 36th week of pregnancy. It continues through delivery. Both the American College of Obstetricians and Gynecologists and the Centers for Disease Control and Prevention recommend the following dosages during pregnancy:
- acyclovir: 400-mg doses three times per day
- valacyclovir: 500-mg doses twice per day
Famciclovir (Famvir) has also been approved for treatment of recurrent genital herpes. Famciclovir is as effective as acyclovir or valacyclovir, but it’s also more expensive. However, there is no data on the use of famciclovir during pregnancy, so this drug is used less often.
Famciclovir is as effective as acyclovir or valacyclovir, but it’s also more expensive. However, there is no data on the use of famciclovir during pregnancy, so this drug is used less often.
Transmission prevention during sex
Genital herpes suppressive treatment can also help reduce your risk of transmitting the infection to new sexual partners. Other steps can help ensure that you don’t infect a sexual partner, as well. For example, genital herpes infection can be transmitted through mouth-to-genital contact in addition to genital-to-genital contact, so you should use a condom or dental dam. This is true even when you have no symptoms.
When you have an outbreak of symptoms, you should avoid sexual contact altogether. This includes the period before an outbreak when you may be more sensitive to touch in your genital area. The sensitivity is a warning that an outbreak of herpes lesions is about to occur.
Talk to your doctor
You have options for suppressing your genital herpes during pregnancy. There are several benefits of this, including:
There are several benefits of this, including:
- decreased risk of virus transmission to your baby during delivery
- possible reduction of the need for cesarean delivery
- decreased risk of virus transmission to sexual partners
Talk to your doctor to discuss if one of the suppressive drugs may be a good option for you.
Read more: Symptoms, treatment, and prevention of birth-acquired herpes »
Last medically reviewed on January 26, 2017
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- ACOG Committee on Practice Bulletins.
 (2007, June). ACOG practice bulletin: Clinical management guidelines for obstetrician-gynecologists, No. 82: Management of herpes in pregnancy. The American College of Obstetricians and Gynecologists, 109(6), 1489-98
(2007, June). ACOG practice bulletin: Clinical management guidelines for obstetrician-gynecologists, No. 82: Management of herpes in pregnancy. The American College of Obstetricians and Gynecologists, 109(6), 1489-98
acog.org/Resources_And_Publications/Practice_Bulletins/Committee_on_Practice_Bulletins_Obstetrics/Management_of_Herpes_in_Pregnancy - Dental dam use. (2016, August 12)
cdc.gov/condomeffectiveness/dental-dam-use.html - Edwards, R. K., & Duff, P. (1999). Herpes simplex virus infections in women. In: T. G. Stovall & F. W. Ling FW (eds.), Gynecology for the Primary Care Physician. Current Medicine Group.
- Ready-to-use STD curriculum for clinical educators: Genital herpes simplex virus module. (2014, January)
www2a.cdc.gov/stdtraining/ready-to-use/Manuals/HSV/hsv-notes-2014.pdf - Sexually transmitted diseases treatment guidelines, 2010. (2010, December 17). Morbidity and Mortality Weekly, 59(RR-12)
cdc.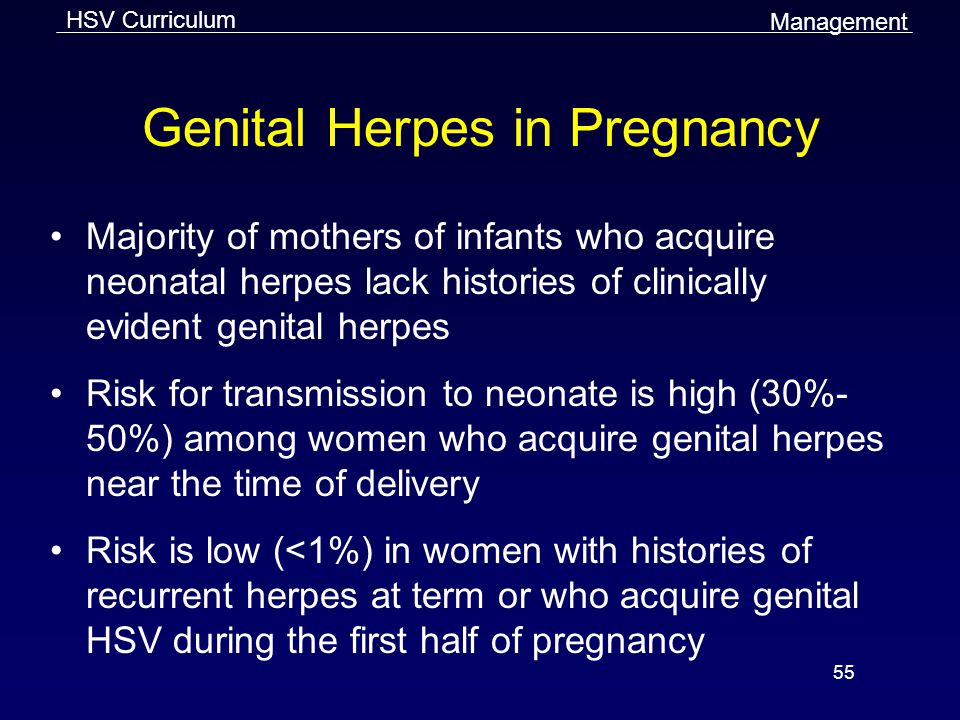 gov/std/treatment/2010/std-treatment-2010-rr5912.pdf
gov/std/treatment/2010/std-treatment-2010-rr5912.pdf
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Aleah Rodriguez, PharmD — By the Healthline Medical Network on March 15, 2012
Read this next
Can You Get Herpes from a Dirty Towel?
Medically reviewed by Cameron White, M.D., MPH
Oral and genital herpes cannot live on porous surfaces, such as a towel. For this reason, you can’t get either type from using someone else’s dirty…
READ MORE
Can You Die from Herpes?
Medically reviewed by Jill Seladi-Schulman, Ph.D.
Herpes is generally mild. You won't die from it. However, there are some complications to keep in mind.
READ MORE
Herpes: Symptoms, Treatments, and Prevention
Medically reviewed by Meredith Goodwin, MD, FAAFP
There are home remedies, over-the-counter medications, and prescription medications for herpes.
 Here’s what you need to know about herpes treatments.
Here’s what you need to know about herpes treatments.READ MORE
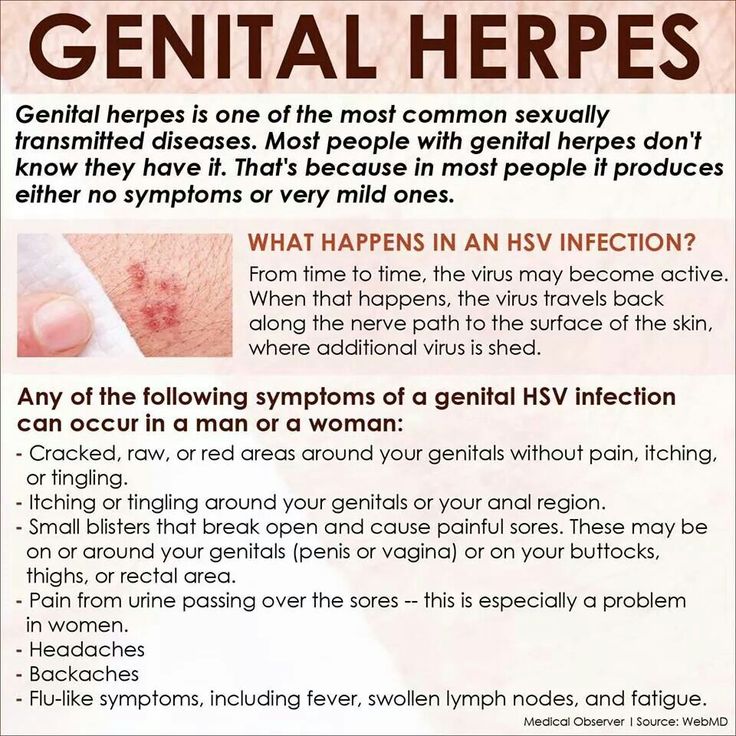
Genital Herpes Causes, Symptoms, and Diagnosis
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Genital herpes is a sexually transmitted infection. It causes herpes sores, which are painful blisters (fluid-filled bumps) that can break open and…
READ MORE
Can You Get Herpes on the Buttocks?
Medically reviewed by Meredith Goodwin, MD, FAAFP
The herpes simplex virus can cause blisters or sores to erupt on various parts of the body, including the buttocks.
READ MORE
A Guide to Genital Herpes Symptoms in Women
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Genital herpes is a common sexually transmitted disease, and the way it looks can vary from person by person and outbreak to outbreak.
READ MORE
Genital Pimples vs. Herpes: How to Identify and Treat Your Symptoms
Medically reviewed by Angela M. Bell, MD, FACP
Genital herpes sores may look similar to pimples, but they require different treatment. Here’s how to differentiate between them and what you can do.
READ MORE
If You’re Wondering What a Herpes Diagnosis Means for Dating or Sex, Read This
Medically reviewed by Janet Brito, Ph.D., LCSW, CST
A genital herpes diagnosis can feel life-altering. And in some ways, it is. But it doesn’t mean that your relationships are doomed or that your sex…
READ MORE
Safety of antiviral medication for the treatment of herpes during pregnancy
Can Fam Physician. 2011 Apr; 57(4): 427–428.
Language: English | French
So-Hee Kang, RPh, Angela Chua-Gocheco, MD, Pina Bozzo, and Adrienne Einarson, RN
Copyright and License information Disclaimer
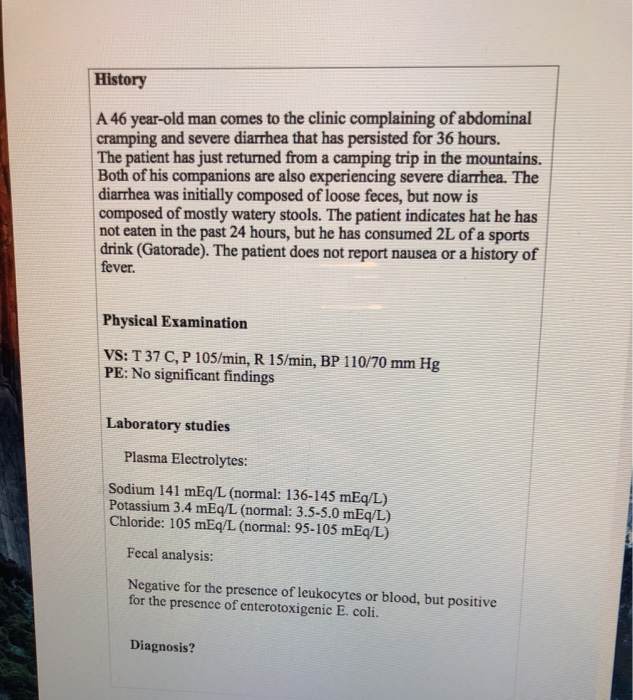
Question One of my patients is a pregnant woman in her first trimester with a history of recurrent genital herpes. She is concerned about whether use of her antiviral medication will adversely affect her baby. What should I tell her?
She is concerned about whether use of her antiviral medication will adversely affect her baby. What should I tell her?
Answer Studies have shown that the use of acyclovir or valacyclovir is not associated with an increase in birth defects. Limited data exist for famciclovir and therefore it would not be considered a first-line choice for treatment of herpes during pregnancy.
Question L’une de mes patientes enceintes en est à son premier trimestre de grossesse et elle a des antécédents d’herpès génital récurrent. Elle se demande si l’utilisation de ses médicaments antiviraux pourrait nuire à son bébé. Que devrais-je lui répondre?
Réponse Des études ont démontré que l’utilisation de l’acyclovir ou du valacyclovir n’est pas associée à une augmentation des anomalies congénitales. Les données concernant le famciclovir sont limitées et ce médicament ne devrait donc pas être considéré comme choix de traitement de première intention pour l’herpès durant la grossesse.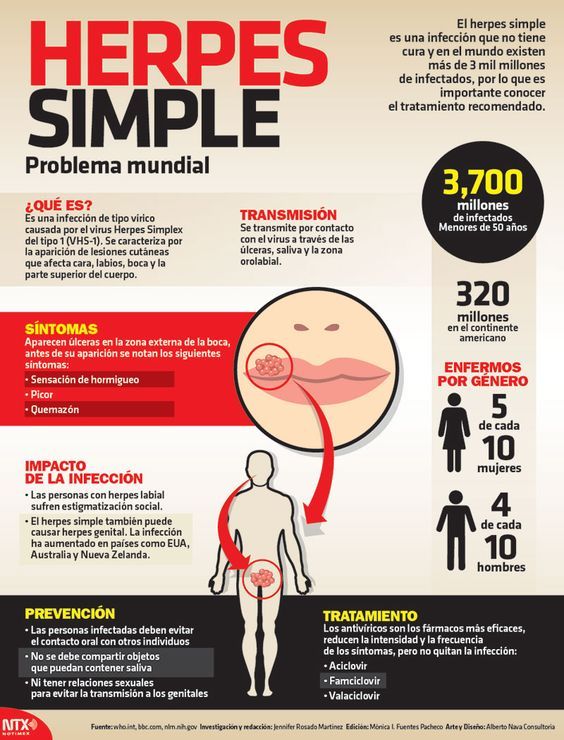
Herpes simplex virus (HSV) infections are common viral infections, with almost 40% of infected patients encountering frequent recurrence within the first year of disease onset.1 In Ontario the seroprevalence for HSV type 1 (HSV-1) and type 2 was 51.1% and 9.1%, respectively.2 A Canadian study revealed HSV type 2 seropositivity in pregnant women to be 17.3%, which raises the concern of potential viral transmission from mother to infant.3 It is also important to note that genital herpes due to HSV-1 infections has increased in frequency and is responsible for up to 30% to 50% of new genital HSV infections.3,4 Recent findings indicate that pregnant women who acquire HSV as a primary infection in the latter half of their pregnancies are at greatest risk of transmission to neonates.5
Neonatal HSV infections are considered more serious compared with adult infections, having consequences that include the following: skin, eye, and mouth infections; central nervous system diseases; disseminated infections; and death. The Canadian neonatal HSV surveillance data indicate that there are 5.9 cases per 100 000 live births, stressing the importance of antiviral treatment during pregnancy to reduce such complications.6 Treatment with antivirals in adults has established their efficacy and safety, but evidence of the safety of acyclovir, famciclovir, and valacyclovir during pregnancy is relatively lacking. It is important to discuss the use of topical antiviral preparations owing to the need to prevent potential orolabial to genital transmission of HSV-1.
The Canadian neonatal HSV surveillance data indicate that there are 5.9 cases per 100 000 live births, stressing the importance of antiviral treatment during pregnancy to reduce such complications.6 Treatment with antivirals in adults has established their efficacy and safety, but evidence of the safety of acyclovir, famciclovir, and valacyclovir during pregnancy is relatively lacking. It is important to discuss the use of topical antiviral preparations owing to the need to prevent potential orolabial to genital transmission of HSV-1.
Valacyclovir is well absorbed after oral administration; absorption of a single dose of 1000 mg is 54% higher than that achieved after single 200- or 800-mg doses of oral acyclovir.7 Valacyclovir is rapidly metabolized to acyclovir, the triphosphorylated form of which selectively inhibits human HSV DNA polymerase, reducing viral DNA replication. Similarly, famciclovir is the oral prodrug of its active form penciclovir; it is more stable than acyclovir triphosphate, as evidenced by longer half-lives intracellularly, which might account for the prolonged in vitro antiviral activity. 8 Acyclovir 5% and penciclovir 1% creams are used to treat orolabial herpes (HSV-1). Penciclovir was not detected in the plasma or urine of healthy volunteers after single or repeated application of the 1% cream.9 Systemic absorption of acyclovir following topical application is minimal or undetectable in adults.10
8 Acyclovir 5% and penciclovir 1% creams are used to treat orolabial herpes (HSV-1). Penciclovir was not detected in the plasma or urine of healthy volunteers after single or repeated application of the 1% cream.9 Systemic absorption of acyclovir following topical application is minimal or undetectable in adults.10
Although controlled studies evaluating the effectiveness of oral antivirals for recurrent HSV outbreaks in the mother and neonatal HSV infections at delivery do exist, they are limited by small sample sizes, the lack of fetal safety outcomes, and variation in timing of exposure.11 However, data on the safety of antiviral drugs during pregnancy have been collected in pregnancy registries, usually established by the manufacturers. The oldest registry (ie, Acyclovir Pregnancy Registry) was open from 1984 to 1998, evaluating the use of oral or intravenous acyclovir in pregnant women. In total, 1234 pregnancies were noted with 1246 outcomes from 24 countries; 756 exposed pregnancies were studied in the first trimester. The risk of birth defects was 3.2% (95% confidence interval 2.0% to 5.0%), which is similar to the baseline risk of birth defects in the general population. No unusual defects or patterns of defects were seen, but the limitation of the results was the high loss to follow-up (27% of registrants).12 During the years 1995 to 1999, the manufacturer of valacyclovir maintained its pregnancy registry, and 110 exposures were reported with 111 known outcomes. Within the first trimester, 1 birth defect was reported out of 28 exposures; 2 of 31 and 1 of 51 exposures resulted in defects in the second and third trimesters, respectively. Prenatal exposures were too limited to provide pregnancy outcomes. According to personal written correspondence from GlaxoSmithKline to Motherisk (January 2010), this registry was limited by the number of registrants and the length of monitoring.
The risk of birth defects was 3.2% (95% confidence interval 2.0% to 5.0%), which is similar to the baseline risk of birth defects in the general population. No unusual defects or patterns of defects were seen, but the limitation of the results was the high loss to follow-up (27% of registrants).12 During the years 1995 to 1999, the manufacturer of valacyclovir maintained its pregnancy registry, and 110 exposures were reported with 111 known outcomes. Within the first trimester, 1 birth defect was reported out of 28 exposures; 2 of 31 and 1 of 51 exposures resulted in defects in the second and third trimesters, respectively. Prenatal exposures were too limited to provide pregnancy outcomes. According to personal written correspondence from GlaxoSmithKline to Motherisk (January 2010), this registry was limited by the number of registrants and the length of monitoring.
A recent Danish population-based retrospective cohort study used data from its nationwide registry to examine live-born infants born between 1996 and 2008 who were exposed to antivirals during pregnancy and the rate of major birth defects within the first year of life. Of the 837 795 enrolled infants, 1804 pregnancies were exposed to acyclovir, valacyclovir, or famciclovir in the first trimester; prevalence odds ratios were considered no different between exposed and unexposed cohorts. Similar results were found when evaluating second and third trimester data. There was also no significant difference in the prevalence of malformations between exposed and unexposed groups when examining exposure during the first trimester to individual antivirals. The rate of malformations was 2.0% for acyclovir (32 of 1561 infants) and 3.1% for valacyclovir (7 of 229 infants). For famciclovir, exposure was uncommon with 1 infant of 26 exposed having a birth defect. As a supplementary analysis, the association between the use of dermatologic acyclovir and penciclovir creams and major birth defects was evaluated. The rate of malformations in those exposed to acyclovir cream and penciclovir cream in the first trimester (2.3%, 65 of 2850 infants, and 4.2%, 5 of 118 infants, respectively) was not different from the unexposed cohort; similar results were found in the second and third trimesters of pregnancy.
Of the 837 795 enrolled infants, 1804 pregnancies were exposed to acyclovir, valacyclovir, or famciclovir in the first trimester; prevalence odds ratios were considered no different between exposed and unexposed cohorts. Similar results were found when evaluating second and third trimester data. There was also no significant difference in the prevalence of malformations between exposed and unexposed groups when examining exposure during the first trimester to individual antivirals. The rate of malformations was 2.0% for acyclovir (32 of 1561 infants) and 3.1% for valacyclovir (7 of 229 infants). For famciclovir, exposure was uncommon with 1 infant of 26 exposed having a birth defect. As a supplementary analysis, the association between the use of dermatologic acyclovir and penciclovir creams and major birth defects was evaluated. The rate of malformations in those exposed to acyclovir cream and penciclovir cream in the first trimester (2.3%, 65 of 2850 infants, and 4.2%, 5 of 118 infants, respectively) was not different from the unexposed cohort; similar results were found in the second and third trimesters of pregnancy.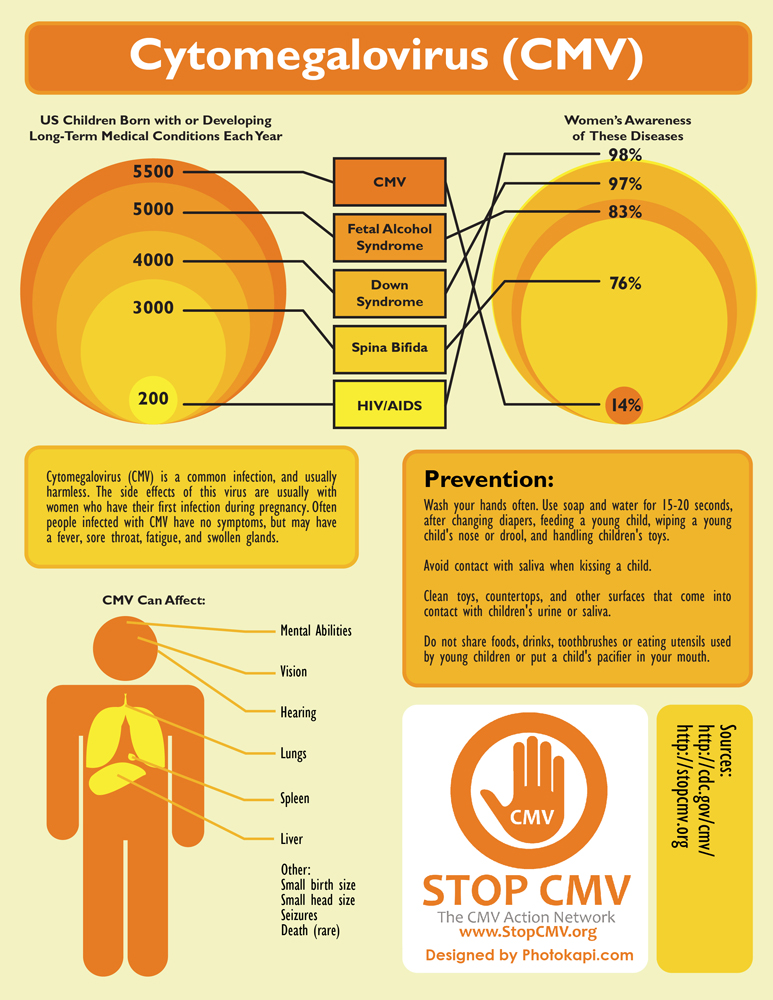 13
13
The accumulated evidence for the safety of oral acyclovir and valacyclovir, established from the manufacturer’s pregnancy registries and as a result of the Danish cohort study, does not demonstrate an increase in the rate of major birth defects when compared with the general population or an unexposed group. Data on the safety of famciclovir’s use during pregnancy is quite limited, and although it might not be expected to increase the risk of major malformations, it should not be the first choice of medication for treatment of HSV during pregnancy. In addition, topical antiviral preparations of acyclovir and penciclovir resulted in no increased rate of major birth defects during pregnancy. Limitations of the safety data on antivirals include a high lost-to-follow-up rate in the registries and the lack of prospective controlled studies. However, these data are reassuring, allowing physicians to offer pregnant patients either acyclovir or valacyclovir for treatment of primary or recurrent HSV infection, which not only treats the mother’s condition, but also reduces the likelihood of transmission to the neonate, without unduly compromising fetal safety.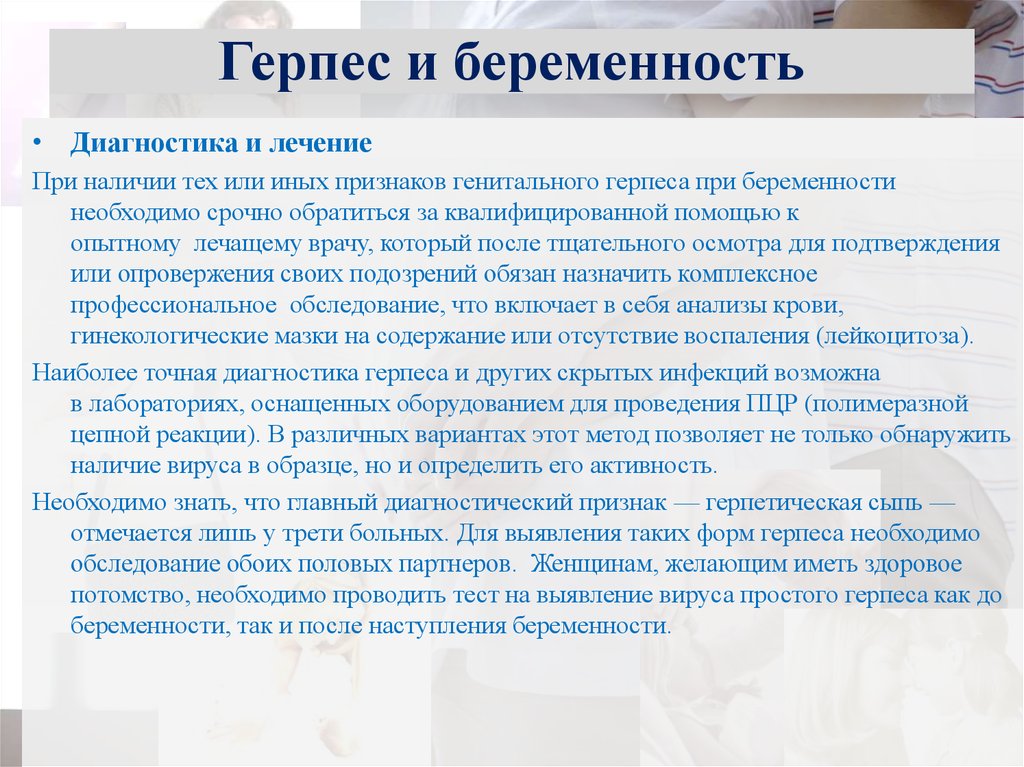
Motherisk
Motherisk questions are prepared by the Motherisk Team at the Hospital for Sick Children in Toronto, Ont. Ms Kang is a doctoral candidate in the Faculty of Pharmacy at the University of Toronto. Dr Chua-Gocheco is a member of the Motherisk Program. At the time this paper was written, Ms Bozzo was a member and Ms Einarson was Assistant Director of the Motherisk Program. Ms Bozzo is now Assistant Director and Ms Einarson has retired but continues to be a member of the Motherisk Program.
Do you have questions about the effects of drugs, chemicals, radiation, or infections in women who are pregnant or breastfeeding? We invite you to submit them to the Motherisk Program by fax at 416 813-7562; they will be addressed in future Motherisk Updates.
Published Motherisk Updates are available on the Canadian Family Physician website (www. cfp.ca) and also on the Motherisk website (www.motherisk.org).
cfp.ca) and also on the Motherisk website (www.motherisk.org).
Competing interests
None declared
1. Benedetti J, Corey L, Ashley R. Recurrence rates in genital herpes after symptomatic first-episode infection. Ann Intern Med. 1994;121(11):847–54. [PubMed] [Google Scholar]
2. Howard M, Sellors JW, Jang D, Robinson NJ, Fearon M, Kaczorowski J, et al. Regional distribution of antibodies to herpes simplex virus type 1 (HSV-1) and HSV-2 in men and women in Ontario, Canada. J Clin Microbiol. 2003;41(1):84–9. [PMC free article] [PubMed] [Google Scholar]
3. Patrick DM, Dawar M, Cook DA, Krajden M, Ng HC, Rekart ML. Antenatal seroprevalence of herpes simplex virus type 2 (HSV-2) in Canadian women: HSV-2 prevalence increases throughout the reproductive years. Sex Transm Dis. 2001;28(7):424–8. [PubMed] [Google Scholar]
4. Xu F, Sternberg MR, Kottiri BJ, McQuillan GM, Lee FK, Nahmias AJ, et al. Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. JAMA. 2006;296(8):964–73. [PubMed] [Google Scholar]
JAMA. 2006;296(8):964–73. [PubMed] [Google Scholar]
5. Anzivino E, Fioriti D, Mischitelli M, Bellizzi A, Barucca V, Chiarini F, et al. Herpes simplex virus infection in pregnancy and in neonate: status of art of epidemiology, diagnosis, therapy and prevention. Virol J. 2009;6:40. [PMC free article] [PubMed] [Google Scholar]
6. Kropp RY, Wong T, Cormier L, Ringrose A, Burton S, Embree JE, et al. Neonatal herpes simplex virus infections in Canada: results of a 3-year national prospective study. Pediatrics. 2006;117(6):1955–62. [PubMed] [Google Scholar]
7. Ormrod D, Scott LJ, Perry CM. Valaciclovir: a review of its long term utility in the management of genital herpes simplex virus and cytomegalovirus infections. Drugs. 2000;59(4):839–63. [PubMed] [Google Scholar]
8. Simpson D, Lyseng-Williamson KA. Famciclovir: a review of its use in herpes zoster and genital and orolabial herpes. Drugs. 2006;66(18):2397–416. [PubMed] [Google Scholar]
9. Denavir cream 1% [package insert] Parsippany, NJ: Novartis Consumer Health, Inc; 2002. [Google Scholar]
[Google Scholar]
10. Zovirax cream 5% [package insert] Research Triangle Park, NC: GlaxoSmithKline; 2002. [Google Scholar]
11. Hollier LM, Wendel GD. Third trimester antiviral prophylaxis for preventing maternal genital herpes simplex virus (HSV) recurrences and neonatal infection. Cochrane Database Syst Rev. 2008;(1):CD004946. [PubMed] [Google Scholar]
12. GlaxoSmithKline . Acyclovir pregnancy registry and valacyclovir pregnancy registry [interim report] Research Triangle Park, NC: Glaxo Wellcome; 1997. [Google Scholar]
13. Pasternak B, Hviid A. Use of acyclovir, valacyclovir, and famciclovir in the first trimester of pregnancy and the risk of birth defects. JAMA. 2010;304(8):859–66. [PubMed] [Google Scholar]
Herpes during pregnancy - consequences of lichen for pregnant women
Herpes viruses are many-sided and very dangerous for humans. Of particular concern is the infection in a woman expecting a baby.
Doctor's consultation
You can get the consultation of the necessary specialist online in the Doctis application
Laboratory
You can undergo a comprehensive examination of all major body systems nine0005
- Genital herpes in early pregnancy
- Genital herpes in late pregnancy
- Pregnancy herpes test
- Chicken pox and herpes zoster during pregnancy
- Prevention of infection of the newborn with chickenpox
- Treatment and prevention of exacerbations of herpes
There is an opinion that if a pregnant woman is infected with the herpes simplex virus, then the unborn danger! But everything is not so scary if the disease does not manifest itself (is in stable remission) or a pregnant woman with an active form of the disease is observed by an infectious disease specialist. Today approaches to maintaining patients with genital herpes changed
Why is herpes dangerous during pregnancy
I am pregnant, short term, and I have genital herpes.
 Does this mean that I need to terminate the pregnancy?
Does this mean that I need to terminate the pregnancy? No way! Genital herpes is not an indication for abortion. Virus crosses the placenta extremely rarely. But for a child, herpes is dangerous if it first appeared a month before birth. or repeated a few days before the birth, since there is a risk of infection of the baby at the time of his passage through the infected birth canal. If infected, the infant will develop severe the disease is neonatal herpes, often occurring with damage to the central nervous system. nine0005
Although during pregnancy the risk of transmission of herpes virus from mother to fetus minimal, tolerate the manifestations of genital herpes and not take antiviral drugs, being afraid the consequences of treatment for the unborn child are not worth it.
After 14 weeks of pregnancy, if genital herpes occurs, treatment with an antiviral drug is possible acyclovir. After 22 weeks, therapy with valaciclovir is possible.
In the vast majority of cases, the herpes simplex virus is transmitted from the mother child during childbirth, so the closer to the end of pregnancy there is a recurrence of genital herpes, the higher the risk of infection of the child and the more relevant the treatment of the disease. nine0037If primary genital herpes or recurrence occurs at or after 36 weeks of gestation, clinicians do not limit treatment to 5-10 days, but continue the entire period until the moment of delivery. As in the case very frequent recurrences of genital herpes during pregnancy (one outbreak in 1-2 months) - at week 36, proactive treatment with acyclovir or its analogues begins and continues until the moment childbirth. The goal of proactive treatment is to prevent recurrence shortly before delivery and to reduce the likelihood of asymptomatic carriage. nine0005
It must be remembered that it is the asymptomatic shedding of the virus from the urogenital tract that can often be cause of infection of the child during childbirth.
 Even when there seems to be no cause for concern, since the manifestations genital herpes are absent in the last months of pregnancy, still at 32-34 weeks pregnancy, it is necessary to conduct a smear (scraping) examination from the cervical canal for the presence of DNA herpes simplex virus types 1 and 2 by PCR. nine0037
Even when there seems to be no cause for concern, since the manifestations genital herpes are absent in the last months of pregnancy, still at 32-34 weeks pregnancy, it is necessary to conduct a smear (scraping) examination from the cervical canal for the presence of DNA herpes simplex virus types 1 and 2 by PCR. nine0037This analysis is necessary for primary genital herpes or its recurrence in the 1st and / or 2nd trimester, relapses genital herpes before pregnancy, relapses of genital herpes in a sexual partner, lesions urogenital tract of unknown cause, antibodies to herpes simplex virus type 1 and type 2 IgM class, detected during a routine examination during pregnancy.
For rashes or virus shedding on Wednesday within 7 days before delivery, especially in the presence of genital herpes by the beginning of childbirth, a caesarean section is performed to reduce the risk of transmission virus from mother to child.nine0037
I'm just planning a pregnancy. And I want to get rid of herpes recurrences that have been haunting me for a long time me. How do you feel about the treatment of genital herpes with interferon inducers and immunomodulators?
Widespread use of immunomodulators and interferon preparations in Russian medical centers (viferon, polyoxidonium, isoprinosine, etc.) for the treatment of herpesvirus infections is completely unreasonable. The so-called "ozone therapy" will not help the patient either. You will not find these methods in international protocols, recommendations for the treatment of viral infections in children and adults, including pregnant women women. Neither in Russia nor abroad have studies been conducted proving the effectiveness of these drugs in accordance with all international regulations. nine0005
An infectious disease specialist, a professional in his field, will never turn to immunomodulators and inducers interferon, but will look for the cause of the disease and prescribe therapy that acts on the pathogen itself - drugs acyclovir, valaciclovir or famaciclovir.With primary genital herpes for 10 days, with relapses diseases - in appropriate doses for 5 days.
Therapy should be started as early as possible at the very first signs of an exacerbation. Application possible antiherpetic drugs as a preventive treatment - 2-3 days before the expected relapse, if the patient is aware of the factors that provoke it, and for the entire period of the risk factor. If genital herpes disturbs a person more than 6 times a year and / or relapses reduce the quality of life of the patient and bring him not only physical, but also serious psychological discomfort, should be discussed with the patient long-term (at least 12 months) daily suppressive antiviral therapy (for example, valaciclovir). The effectiveness of such treatment tactics for the prevention of recurrence of herpes infection has been proven. all international rules. nine0005
Sequelae of chickenpox during pregnancy
How dangerous are chicken pox and shingles for a pregnant woman?
These diseases are caused by the varicella-zoster virus (VZV), which also belongs to the herpesvirus family.
infect women are most often children who easily tolerate the disease. At the same time, chickenpox in an adult can be severe and dangerous to his health.
Infection is transmitted by airborne droplets from person to person already 48 hours before the onset of the rash, during the entire period of the rash and for a week after appearance of the last bubbles. nine0037Expectant mothers who catch chickenpox may develop severe herpes pneumonia. Therefore, when sick chickenpox during pregnancy should be observed by an infectious disease specialist and in most cases of antiviral therapy.
In maternal varicella at 8 to 20 weeks of gestation infection fetus with the varicella-zoster virus can lead to fetal chickenpox with the development of a "syndrome congenital chicken pox" with severe malformations - damage to the brain, eyes, skeletal defects. Therefore, if a woman falls ill with chicken pox in the 1-3rd month of pregnancy, the doctor the woman should be informed about all possible risks of the disease for the fetus and discussed with her the question of a possible termination of pregnancy.
nine0005
Second and third trimesters infectious disease doctor monitors the state of the future mothers. If the infection is severe or the infection occurred in the last month of pregnancy, prescribe antiviral treatment with acyclovir or its analogues. If ultrasound does not detect fetal pathology, pregnancy is not interrupted.
Within 96 hours (preferably within the first 48 hours) after contact a pregnant woman with chickenpox in the absence of IgG class antibodies to VVZ it is possible to introduce a specific VVZ-immunoglobulin as a measure to prevent the development of the disease. Immunity persists for 3-4 weeks, may be re-introduced after 21 days. nine0037If the mother-to-be becomes ill with chicken pox in the last month of pregnancy , then the child may be born with skin rashes. If a woman falls ill in the last few days of pregnancy or in the first days after childbirth in a newborn infected during childbirth, the symptoms of chickenpox appear in the first 11 days of life.
Chickenpox is most severe in infants whose mothers fell ill 5 days before or 2-3 days after delivery. In case of chickenpox in mothers, newborn children are given a specific immunoglobulin to prevent the development of the disease. In case of its severe course - appoint acyclovir for intravenous administration. nine0005
Infection of a child with VVV a few days after birth may manifest as postnatal varicella in the period of 12-28 day of his life. This form of the disease is less severe, it is possible to introduce a specific immunoglobulin with the risk of the disease and the appointment of intravenous acyclovir for destructive skin lesions.
Vaccination against the varicella-zoster virus is not given to pregnant women because this is a live vaccine. Therefore, if a young woman does not have IgG antibodies to VVZ before planning pregnancy, it is advisable to vaccinate against chicken pox. nine0037Herpes zoster ("secondary" VVZ infection) in a pregnant woman is not dangerous for a child.
Contact seronegative pregnant woman with herpes zoster is not desirable, although the threat of her infection There is practically no VVZ.
I'm just planning a pregnancy. And I want to get rid of herpes recurrences that have been haunting me for a long time me. How do you feel about the treatment of genital herpes with interferon inducers and immunomodulators?
nine0002 Widespread use of immunomodulators and interferon preparations in Russian medical centers (viferon, polyoxidonium, isoprinosine, etc.) for the treatment of herpesvirus infections is completely unreasonable. The so-called "ozone therapy" will not help the patient either. You will not find these methods in international protocols, recommendations for the treatment of viral infections in children and adults, including pregnant women women. Neither in Russia nor abroad have studies been conducted proving the effectiveness of these drugs in accordance with all international regulations.nine0005
Infectionist, a professional in his field will never turn to immunomodulators and interferon inducers, but will look for the cause of the disease and prescribe an effective pathogen therapy - drugs acyclovir, valaciclovir or famaciclovir. With primary genital herpes for 10 days, with relapses of the disease - in appropriate doses for 5 days.Therapy should be started as early as possible at the very first signs of an exacerbation. Application possible antiherpetic drugs as a preventive treatment - 2-3 days before the expected relapse, if the patient is aware of the factors that provoke it, and for the entire period of the risk factor. If genital herpes disturbs a person more than 6 times a year and / or relapses reduce the quality of life of the patient and bring him not only physical, but also serious psychological discomfort, should be discussed with the patient long-term (at least 12 months) daily suppressive antiviral therapy (for example, valaciclovir).
The effectiveness of such treatment tactics for the prevention of recurrence of herpes infection has been proven. all international rules. nine0005
If you have any questions, you can ask your doctor obstetrician-gynecologist or infectious disease specialist online at Doctis app.
The author of the article: Vasily Iosifovich Shakhgildyan
Treatment of herpes during pregnancy - BIOFON
Is it necessary to treat herpes during pregnancy? How dangerous is the disease for the normal development of the fetus? These questions concern every woman who is preparing to become a mother. nine0005
Herpes is an infectious disease that can be caused by two types of virus. The first type affects the lips, nose, eyes, the second is localized on the genitals.
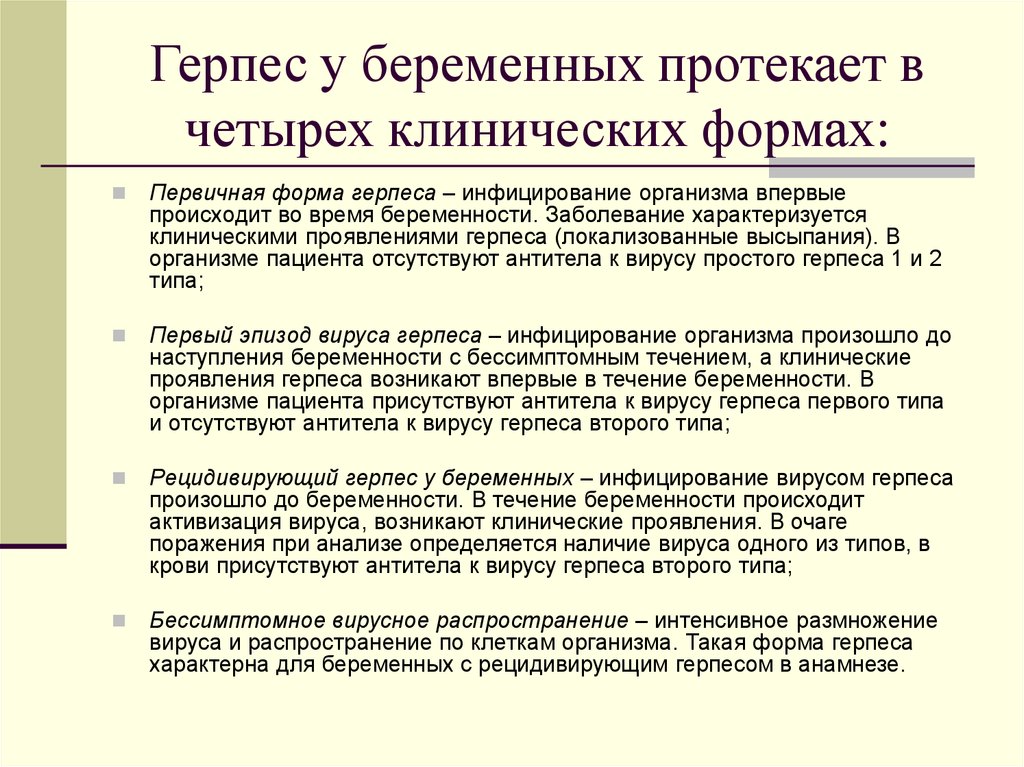
Herpes is primary - when the infectious agent only penetrates into the human body and recurrent - when a person becomes a carrier and the disease develops again.
If a woman develops primary herpes during pregnancy, there is a serious risk to the health of the fetus. nine0072 A child may have various anomalies, deviations in the development of the brain, in some cases a fatal outcome is possible.
With recurrent herpes, the fetus is affected in isolated cases. In the mother's body there are already specific antibodies that reliably protect the child from the infectious agent. Especially dangerous is genital herpes, infection which can occur during childbirth.
Symptoms of herpes during pregnancy:
- general weakness;
- fever; nine0016
- headache;
- rashes on the mucous membranes and skin, in place of which bubbles filled with liquid form after a while;
- general intoxication of the organism.
Herpes is especially dangerous in the second and third trimester of pregnancy, when the placenta is already fully formed, through which the virus can penetrate.
Treatment of herpes during pregnancy
How to quickly eliminate herpes during pregnancy? Treatment with medication will take one to one and a half weeks.
You should not take independent measures and risk the health of your unborn child. Pregnant women should take medications only as directed by a doctor. Pregnant women are prescribed homeopathic and anti-inflammatory ointments for herpes, antiviral drugs. Expectant mothers are categorically contraindicated in antibiotic treatment, which is usually prescribed for a speedy recovery. Oxalin ointment is very popular in the fight against herpes, but it should be used no more than four times a day. nine0005
In the fight against herpes during pregnancy, traditional medicine has long been used, which are absolutely safe for the health of a young mother. This is fir and sea buckthorn oil, which should be used several times a day to lubricate the site of inflammation, warm tea with viburnum and honey. In the case when the treatment of genital herpes during pregnancy did not give the expected effect, the woman is prescribed a caesarean section.
If you are afraid of contracting herpes during pregnancy, it is worth being examined for the presence of antibodies in the body even at the planning stage.
You can completely protect yourself from infection with the help of vaccination. Do not forget about proper nutrition, walking in the fresh air, taking immunostimulating drugs. Be sure to include in the diet food containing lysine - chicken meat, fruits, vegetables. The amino acid prevents the growth of pathogenic bacteria in the body, becoming a reliable protector from infection. nine0005
One of the most reliable modern means to combat herpes is the Uro-Biofon device, which does not have a negative effect on the body of a young mother.
Recommended for the treatment of genital herpes apparatus "Uro-Biofon"
"Uro-Biofon" is an antimicrobial device that acts on the cell membrane of the microbe, damaging it. In the microbial cell, metabolic processes are disturbed, it is inactivated and loses its ability to defend itself. Cells of the immune system capture the defenseless pathogen and lyse (dissolve) it. nine0005
Advantages of "Uro-Biofon":
- According to the results of clinical trials, the effectiveness of treatment with devices of the "Biofon" series ranges from 64 to 100%.
- Works on drug-resistant strains.
- Does not cause side effects, as it acts only on pathogenic microbes and their toxins.
- They can be treated both alone and with the whole family. The range of the device is 1.5 meters.
- Easy to handle.
- "Uro-Biofon" can be used by any age group, as well as by persons suffering from chronic diseases of the gastrointestinal tract, liver, kidneys. nine0016
See for yourself the results of using
Uro-Biofon :“And this is after 22 years of relapses every month.
“I want to thank the creators and manufacturers of Biofon devices and leave a report on my use of these devices. The first device I purchased was Uro-Biofon. Acquired for the treatment of herpes. It was in 2005. By this time, for almost my entire conscious life (from the age of 21 to 43), i.e. For 22 years I tried in every possible way to get rid of this disease.
I tried a lot ... The means allowed me to be treated by different methods, but nothing helped. Genital herpes, as it was, remained. In 2005, I saw an advertisement for Uro-Biofon and decided to try it. There were no particular illusions, but since the manufacturer promised to return the money if the device did not help, it was a win-win option. nine0005
Passed the full course. Surprisingly, there were no recurrences of herpes. Has handed over analyzes, the virus in an organism is not found out. And this is after 22 years of relapses every month with blisters, sores, suppuration, burning! »
Alexey, Moscow, January 24, 2013« Thanks to Biofon, this happened. We are already 21 weeks old! All tests are normal!
Hello again! I wrote my review about a year ago. So, I wrote that we are going to have a baby, but without success for 6 years. Thanks to "Biofon" it happened.