Headaches during pregnancy 12 weeks
You and Baby at 12 Weeks Pregnant
Key Takeaways at 12 Weeks Pregnant
- Those overwhelming first-trimester symptoms may begin to wane. That means morning sickness may start fading soon and the outrageous exhaustion-fog may lift. Hope is on the horizon!
- Have you bought maternity pants yet? If not, it’s time to loosen your purse strings—and your belt. Your belly is expanding and a budding bump is probably visible at this point.
- Baby continues to develop by leaps and bounds every day. Their fingers and toes are no longer webbed, and their eyes, nose and fingernails are forming—so cool!
- Getting a 12-week ultrasound? Your tech might be able to determine the sex of baby at this point, but it’s not guaranteed, nor is it foolproof.
Things are changing fast at 12 weeks pregnant. You’re reaching the home stretch of the first trimester (we know, finally!), which means your hormones are likely to tone things down a bit. It also means you may be ready to share your pregnancy news with family and friends. So exciting!
Baby at Week 12
Your 12-week fetus is almost done developing their body’s important systems and parts, which means it’s all about getting bigger and more mature from here on out. Yep, baby's about to enter the growth and maturation stage, in which organs and tissues will grow and develop rapidly.
Baby at 12 weeks is opening and closing their fingers and curling their toes, and their brain is developing fast!
Baby is now developing reflexes—if you poke your 12-week pregnant belly while looking at baby on an ultrasound, you'll likely see movement. If you’re 12 weeks pregnant with twins, your twosome is developing at a similar rate as singleton babies at 12 weeks. Later on, they’ll have a slightly slower rate of growth.
How big is baby at 12 weeks?
At 12 weeks pregnant, baby is as big as a plum. The average 12-week fetus is about 2.1 inches long and .49 ounces. Now that baby's got pretty much all of their important organs, their main job is to keep on growing. Go, baby, go!
Go, baby, go!
12 weeks pregnant is how many months?
At 12 weeks pregnant, you’re about three months pregnant. Remember, pregnancy is 40 weeks long, which doesn't break down cleanly into nine months. Just two more weeks until you can officially put your first trimester behind you!
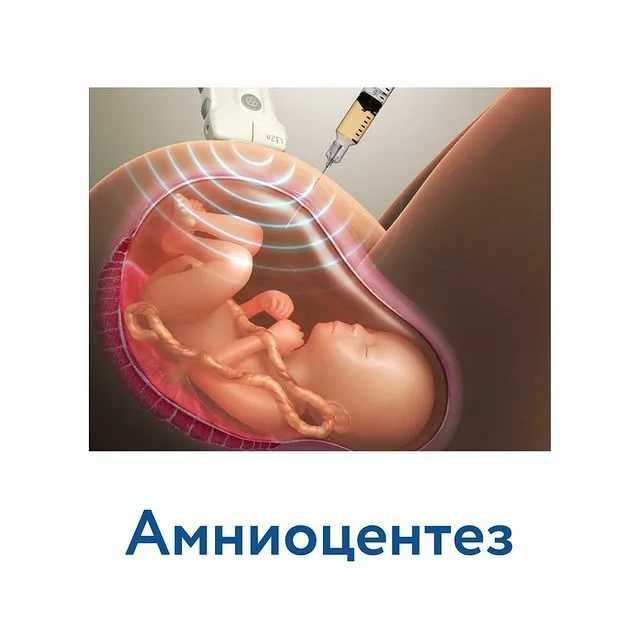
12 week ultrasound
You may have one more prenatal checkup before the end of your first trimester. Whether or not you have a 12-week ultrasound may depend on your doctor’s preference and maybe also on what your insurance covers. If you do get an ultrasound at this time, you’ll notice that you can see your 12-week fetus more clearly this time around, which may make you want to start spreading the news that you’re expecting.
Itching to find out if it’s a boy or a girl? We hate to be the bearers of bad news, but on a 12 weeks pregnant ultrasound, the sex isn’t usually revealed. Between 12 and 13 weeks is the very earliest a boy or girl could possibly be seen on an ultrasound, and the anatomy is still difficult to make out with any certainty. Your OB or technician is much more likely to be able to see baby’s sex at the mid-pregnancy anatomy scan, which will happen around week 20. However, if you received DNA blood testing for chromosomal disorders, you may find out baby’s sex when you get those results—if you want to know, that is!
Your OB or technician is much more likely to be able to see baby’s sex at the mid-pregnancy anatomy scan, which will happen around week 20. However, if you received DNA blood testing for chromosomal disorders, you may find out baby’s sex when you get those results—if you want to know, that is!
Around week 12, you might want to know more about baby’s health, so you may have genetic testing done to determine the risk of birth defects or other problems. This can be a little scary—and confusing—so be sure to ask your OB plenty of questions, and know that it’s much more likely that baby is a-okay than anything else.
What does a 12-week fetus look like?
With the first trimester almost done, you may be wondering, “what does a 12-week fetus look like?” New and exciting changes are happening for baby at 12 weeks! The eyes and nose take shape, fingers and toes lose their connective webbing, fingernails develop, teeth buds crop up and organs such as the kidneys and intestines keep growing.
3D Views: My Baby, My Body
See their progress for yourself with our 3D interactive tool.
See My Baby in 3D
See My Body in 3D
Pregnancy Symptoms at Week 12
Here’s the good news about 12 weeks pregnant symptoms: Morning sickness and fatigue may start to fade a bit soon as your hormones start to calm down. The bad? Headaches and dizziness may replace them. We’ll take that trade-off. Here’s more info about what’s happening to your body at 12 weeks pregnant:
Increased discharge
This clear discharge might seem weird, but it’s normal and has an important purpose: to protect your vagina from infection. But if you have yellow, greenish, pink or brown discharge during pregnancy week 12, call your doctor right away. Those colors could be a sign of infection or even miscarriage.
Spotting
Spotting or bleeding during pregnancy at 12 weeks could be worrisome—or it could be nothing at all. For example, your cervix is more sensitive during pregnancy, so simply having sex could cause light bleeding that’s harmless. If you’re spotting or bleeding, definitely tell your doctor. If the bleeding is accompanied by cramping or the flow is heavy, it’s an urgent call.
For example, your cervix is more sensitive during pregnancy, so simply having sex could cause light bleeding that’s harmless. If you’re spotting or bleeding, definitely tell your doctor. If the bleeding is accompanied by cramping or the flow is heavy, it’s an urgent call.
Headaches
These may start to intensify around week 12 of pregnancy. Headaches may be caused by hormonal shifts, drops in blood sugar, dehydration, lack of sleep or stress. To deal, pay attention to what might be triggering your headaches and try to avoid those culprits. If you notice a drastic increase in headaches or a type of headache you’ve never experienced before (such as a migraine), or if your headaches are accompanied by other weird symptoms, let your OB know.
Dizziness
Whoa! Hormone shifts and blood pressure changes could cause dizzy spells around pregnancy week 12 (and sometimes even earlier!). You can help prevent dizziness by snacking regularly, avoid becoming overheated and drinking plenty of water..jpg) Sit or lie down if you’re feeling dizzy or lightheaded and let your doctor know about any severe bouts.
Sit or lie down if you’re feeling dizzy or lightheaded and let your doctor know about any severe bouts.
If you’re 12 weeks pregnant with twins, you may still be experiencing morning sickness, while your singleton mom-to-be counterparts are likely starting to see the light at the end of the nausea tunnel. Know that things will likely improve soon.
What should I be feeling at 12 weeks pregnant?
Your body is working hard, and you may wonder, “what should I be feeling at 12 weeks pregnant?” You may not be showing much on the outside yet, but on the inside everything feels like it’s changing! In addition to typical 12 weeks pregnant symptoms, you may start to feel shifts with morning sickness and fatigue. One day you might be exhausted, and another you may feel a burst of energy, while nausea comes and goes. Hang tight—you're getting closer to the second trimester! Make sure you get plenty of fluids and healthy foods for those days when morning sickness makes it rough to keep anything down.
Your Pregnant Belly at 12 Weeks
At 12 weeks, your pregnant belly is probably getting noticeable now. This is one reason many moms-to-be start to tell others they’re expecting around 12 weeks. (Of course, if you’re 12 weeks pregnant with twins, you may have been showing for weeks now, obviously because you’ve got double the babies in there!)
If you haven’t already, start taking photos of your pregnant belly at 12 weeks. Trust us, after pregnancy you’ll want a memento of how much your body changed throughout.
How does your stomach feel at 12 weeks pregnant?
You may already feel the waistband of your clothes getting tighter as your stomach begins to round out. When baby is at 12 weeks, your uterus is expanding to make room for your growing little one. This can also cause a tight feeling in your stomach itself as the stretching uterus puts pressure on the surrounding tissues of your body. Gas or constipation are other common causes of tummy troubles.
“You are moving for two!… Going for a walk, doing your favorite workout or dancing to music, creates better weight management, cognitive development, cardiovascular health and beneficial health outcomes for baby. Remind yourself on your exhausted days that exercising through your pregnancy is going to make this journey easier for you and set your baby up for a lifetime of better health!” - Joanie Johnson Rubin, pre- and postnatal fitness expert and founder of Strong Mom Society
Tips for 12 Weeks Pregnant
Here’s some advice for living your best pregnant life as you finish up your first trimester and move into your second.
Give sore breasts some TLC
Your body’s hormones are getting you ready for breastfeeding, which can make breasts sore or tender. Soothe pain by wearing comfortable clothes that don’t irritate the body, trading in underwire bras for maternity or nursing bras with soft support or using ice packs for temporary relief.
Wear sun protection
One 12 weeks pregnant symptom that can occur for many women is melasma, or the “mask of pregnancy,” where dark spots appear on the face. It’s caused by those active hormones, but melasma can be made worse with sun exposure. Protect your skin with a mineral-based sunblock and a wide-brimmed hat, and stay in the shade or indoors during the day whenever possible.
Don’t give into junk food temptations
If your appetite starts to return as morning sickness fades, don’t feed it with lots of sugar, fats or processed foods. Healthy eating is good for you and baby, and it also helps you achieve a healthy weight gain moving forward. While it’s totally normal to not gain any weight in the first trimester (or even lose a few pounds), women of normal pre-pregnancy weight should plan on adding a pound or two a week during the second trimester
Think about getting physical
Pretty soon, you’ll have more energy, so make sure to talk with your OB about a safe exercise plan for the rest of your pregnancy. Regular workouts may help manage weight gain, make your heart and lungs strong, decrease pain and potentially reduce risk of issues such as gestational diabetes.
Regular workouts may help manage weight gain, make your heart and lungs strong, decrease pain and potentially reduce risk of issues such as gestational diabetes.
ADVERTISEMENT
Pregnancy Checklist at 12 Weeks Pregnant
Reminders for the week:
save article
PREVIOUS
Week 11Pregnancy
NEXT
Week 13Pregnancy
ADVERTISEMENT
Watch These Videos Next:
Article saved.Go to My Saved Articles
Article removed.
Headaches during pregnancy | Pregnancy Birth and Baby
Headaches during pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Headaches in women can often be triggered by a change in hormones during pregnancy. Expectant mothers may experience an increase or decrease in the number of headaches. Unexplained, frequent headaches later in your pregnancy could be a sign of a more serious condition called pre-eclampsia, so tell your doctor if this is the case.
Unexplained, frequent headaches later in your pregnancy could be a sign of a more serious condition called pre-eclampsia, so tell your doctor if this is the case.
Causes of headache during pregnancy
Many women experience headaches during pregnancy, especially in the first and third trimesters. If you're pregnant, you may notice an increase in the number of headaches you have at around week 9 of your pregnancy.
As well as hormonal changes, headaches in the early stages of pregnancy can be caused by an increase in the volume of blood your body is producing.
Other causes of headaches during pregnancy can include:
- not getting enough sleep
- withdrawal from caffeine (e.g. in coffee, tea or cola drinks)
- low blood sugar
- dehydration
- feeling stressed
- poor posture, particularly as your baby gets bigger
- having depression or anxiety
Migraine
Migraine is a particular type of headache that mostly occurs on one side of the head – it can be either moderate or very painful. People who experience migraine can also feel sick or vomit, and be sensitive to light or sound.
People who experience migraine can also feel sick or vomit, and be sensitive to light or sound.
In pregnancy, migraine may get worse for the first few months, but for many women it can improve in the later stages of their pregnancy when the level of the hormone oestrogen stabilises. Other women may experience no change or a decrease in the number of migraine headaches while pregnant. Some women may experience differences in migraine during different pregnancies.
Treatment
It’s not advisable for pregnant women with migraine to use migraine medicine. For other headaches it's also recommended that you try to treat your headache without medicine.
You could try:
- getting more sleep or rest and relaxation
- pregnancy yoga classes or other exercise
- practising good posture, particularly later in your pregnancy
- eating regular, well-balanced meals
- putting a warm facecloth on your eye and nose area, if it is a sinus headache
- putting a cold pack on the back of your neck, taking a bath or using a heat pack, if it is a tension headache
- neck and shoulders massage
Pregnant women who experience migraine should avoid things that may trigger their migraine. This may include:
This may include:
- chocolate
- yoghurt
- peanuts
- bread
- sour cream
- preserved meats
- aged cheese
- monosodium glutamate (MSG)
- caffeine (withdrawal from)
- bright or flickering lights
- strong smells
- loud sounds
- computer or movie screens
- sudden or excessive exercise
- emotional triggers such as arguments or stress
If you do take medicine for your headache or migraine you should check with your doctor, pharmacist or midwife first. Paracetamol, with or without codeine, is generally considered safe for pregnant women to use but you should avoid using other pain medicine such as aspirin or ibuprofen.
When to contact your doctor
If you experience frequent headaches that don't go away with paracetamol, it could be a sign of a more serious medical condition called pre-eclampsia. This usually involves an increase in the pregnant woman's blood pressure and problems with her kidneys. There are also other serious risks for both you and your baby. Pre-eclampsia mostly occurs in the second half of pregnancy.
There are also other serious risks for both you and your baby. Pre-eclampsia mostly occurs in the second half of pregnancy.
Contact your doctor, particularly if, along with your headaches, you have a pain below your ribs, feel like you have heartburn, you suddenly swell in your face, hands or feet, or you have problems with your eyesight.
Further information
- Speak with your doctor or midwife, particularly if you have any concerns about pre-eclampsia
- Phone Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse.
- For more information about headaches during pregnancy, visit Headache Australia.
- For more information about medication during pregnancy, see your doctor or pharmacist, or visit NPS MedicineWise.
Sources:
Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Pre-eclampsia and high blood pressure during pregnancy), Headache Australia (Migraine), Women's and Children's Health Network (Medicines during pregnancy), Headache Australia (Adults and headache), Headache Australia (Migraine – A common and distressing disorder), Raising Children Network (9 weeks pregnant), Raising Children Network (34 weeks pregnant), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Perinatal Anxiety and Depression), American Pregnancy Association (Pregnancy and Headaches), NPS Medicinewise (Taking medicines in pregnancy), Australian and New Zealand College of Obstetricians and Gynaecologists (Is paracetamol safe to use in pregnancy?)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2020
Back To Top
Related pages
- Common discomforts during pregnancy
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, because:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.

Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraines during pregnancy either remain unchanged or worsen. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman throughout the entire period of pregnancy and after childbirth too.
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink enough fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations. This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make seizures less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods.
 Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfere with your life, then under the supervision of a specialist, you can resort to drug therapy.
PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted.
 However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.
When to see a doctor:
-
migraine occurred for the first time during pregnancy;
-
if migraine attacks suddenly become more frequent and stronger;
-
if the aura became longer or appeared for the first time;
-
if the headache is rapidly increasing and has an unusual character;
-
if the pressure rises during the headache.
Follow our Instagram to read the latest materials on the diagnosis and treatment of headaches!
cluster headache. Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh.
Headache during pregnancy: where does it come from and how to get rid of it
Share
0When to call an ambulance
Call 103 or 112 urgently if you experience the following symptoms:
- sudden and severe headache;
- consciousness becomes confused or completely lost;
- pain worsens over 5 minutes;
- flies, spots flash in the eyes;
- throbbing and noisy in the ears;
- speech has become slurred, words are drawn out;
- arms and legs weaken, convulsions set in;
- the muscles of the neck are very stiff, it is impossible to reach the chest with the chin;
- temperature rises to 39 °C or more;
- increased heart rate at rest;
- severe shortness of breath;
- the child pushes without stopping or stops abruptly;
- leaking water or blood;
- pain in the lower abdomen, as if contractions had begun.

Why pregnant women can get headaches
Pregnancy headaches are not always life threatening. But the doctor needs to be told about it in any case. If the symptom appeared for the first time and does not hurt much, postpone the conversation until a scheduled visit. If your headache is recurring or gets worse, it's best to make an appointment as soon as possible. The gynecologist will decide what needs to be done or refer you to another doctor.
There are many causes of headaches. Scientists have found that in pregnant women in 57% of cases it is primary, that is, not associated with other diseases. The most common are migraines and tension headaches.
Everything else is a secondary headache caused by various pathologies. Usually it is high blood pressure and infections. But there are also more dangerous reasons.
1. Stress and fatigue
A pregnant woman's body experiences increased stress, because it has to work for two. If at the same time the expectant mother is exposed to stress, strong feelings or sleeps little, she develops a tension headache.
Discomfort lasts from 30 minutes to several days. The head hurts in the forehead, occiput, both temples. But there is no feeling that they put on a tight hoop or helmet. The pain does not get worse when bending over, walking, or climbing stairs, bright lights, or sounds.
What to do
Tension headache can go away on its own: just get some fresh air or sleep. Sometimes pleasant emotions help, which distract from experiences.
If the pain persists for 2-3 consecutive days, see a doctor. He will select painkillers that are safe for the child.
2. Taking medications
Any medication that enters the stomach or blood can cause headaches even if the dosage is correct. In pregnant women, this often occurs due to drugs for high blood pressure, heart disease, antibiotics, anticonvulsants.
Long-term use of non-steroidal anti-inflammatory drugs for headaches may cause the opposite effect: the pills do not remove, but provoke symptoms.
What to do
If your head hurts a few hours after taking the medicine, you need to see a doctor to change the medicine. Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
3. Love or refusal to coffee
Coffee can cause headaches during pregnancy. Unpleasant symptoms occur if you drink more than 3-4 cups a day.
Abrupt refusal of coffee is also harmful. It is worth finding out about pregnancy and stopping brewing a fragrant drink, and after 1-2 days, aching pain will appear in the temples and the back of the head.
What to do
Coffee is best avoided during pregnancy. If a headache occurs a day after this, you can drink a small cup of the drink and wait a day again. Gradually, the dependence on coffee will pass.
Coffee drinkers can reduce their drink intake to 1-2 cups per day.
4. Infection with fever
Acute viral (usually SARS) or bacterial (eg, streptococcal tonsillitis) infections cause fever and headache. This is a normal reaction to foreign microorganisms.
But any infection is dangerous for pregnant women. It can cause fetal defects, growth retardation and even miscarriage. And with meningitis, especially listeriosis, there is a threat to the life of the mother.
What to do
If you have a headache with fever, call your doctor. He will prescribe safe medications or give you a referral to the hospital if a serious infection is suspected. In this case, you need strong antibiotics, droppers to maintain the body and sometimes hormones.
5. Preeclampsia and preeclampsia
After 20 weeks, preeclampsia may develop in pregnant women. This is a disease in which one of three symptoms or a combination of them may appear: high blood pressure, edema, and protein in the urine.
Without proper treatment, preeclampsia turns into preeclampsia. The pressure rises sharply, the head and lower abdomen hurt unbearably, the baby pushes unusually hard or, on the contrary, suddenly calms down. Preeclampsia can lead to placental abruption, damage to the liver and other organs, bleeding, and even seizures. Without urgent medical care, the fetus and mother die.
Without urgent medical care, the fetus and mother die.
What to do
When the first signs of preeclampsia appear, the pregnant woman is hospitalized to find treatment. After that, she is discharged home under the supervision of her gynecologist.
But if her health worsens, the doctor again sends the woman to the hospital, where she is prescribed medicines to reduce pressure, special droppers to keep her body functioning. If improvement does not occur within a day, a caesarean section is performed.
6. Migraine
One of the causes of migraine is a change in estrogen levels. But the disease very rarely appears due to pregnancy. On the contrary, in 70% of women, the symptoms subside dramatically after conception. Nevertheless, migraines torment many.
It may begin with an aura: flashes of light, spots before the eyes, tingling in the hands or numbness of half of the face, sometimes tinnitus. Each symptom can last from 20 minutes to an hour.
A migraine attack develops after the aura. In this case, one side of the head hurts and throbs, nausea or vomiting appears. A woman is irritated by bright lights, loud noises, smells. They make the pain worse.
Seizures last from a few hours to a week or more. After a migraine, there is a feeling of severe fatigue, exhaustion, and an awkward turn of the head can return the pain.
What to do
Any medication for migraine during pregnancy must be prescribed by a doctor. In some cases, drugs from the group of beta-blockers are used.
Studies have shown that frequent migraine in pregnancy is associated with a lack of magnesium. The doctor will help you choose the appropriate type of vitamin and mineral complex and its dosage.
7. Cerebral vascular disease
Hormone problems in some pregnant women increase blood clotting, which increases the risk of thrombosis, stroke, or bleeding in the meninges. These conditions are very dangerous: a woman can die within a few minutes or remain disabled.
Vascular involvement is always accompanied by several symptoms:
- severe headache on one side;
- nausea and vomiting;
- blurred vision;
- loss of consciousness;
- convulsions.
What to do
Urgently call an ambulance. The pregnant woman must be laid or seated so that she does not hit when she falls. You can't give medicine! You can only open the window so that there is more air in the room.
Which treatment the doctor prescribes depends on the specific disease. These can be drugs that reduce blood clotting and dissolve blood clots. In some cases, urgent surgery is needed.
8. Brain tumors
Studies show that progesterone and estrogen during pregnancy can trigger or accelerate the growth of tumors in the brain. Symptoms of the disease appear slowly, over several months, and depend on the size and location of the tumor.
Headache may gradually increase, then vision, speech, hearing deteriorate, limbs go numb and convulsions appear. Sometimes it is difficult for a woman to keep her balance.
Sometimes it is difficult for a woman to keep her balance.
What to do
If a pregnant woman often has a headache or she forgets what she wanted to buy in the store and how to cook her favorite borscht, confuses her way home, you need to go to a neurologist. First, he will prescribe standard treatment, simple and safe medicines, rest, good sleep.
If this does not help, the symptoms persist or worsen, a deep examination is required. The pregnant woman will be sent for an MRI of the brain. This procedure is safe for the fetus. If the diagnosis is confirmed, surgery may be required.
What to do if the doctor cannot find the cause of the pain
If you have been examined and the doctor cannot tell you why your head hurts and diagnoses you with vascular dystonia, this is a reason to be wary. There is no such disease.
Look for another doctor. Perhaps he uses new diagnostic methods that will help to deal with the problem and choose a treatment.