Headache during late pregnancy
Headaches During Pregnancy | American Pregnancy Association
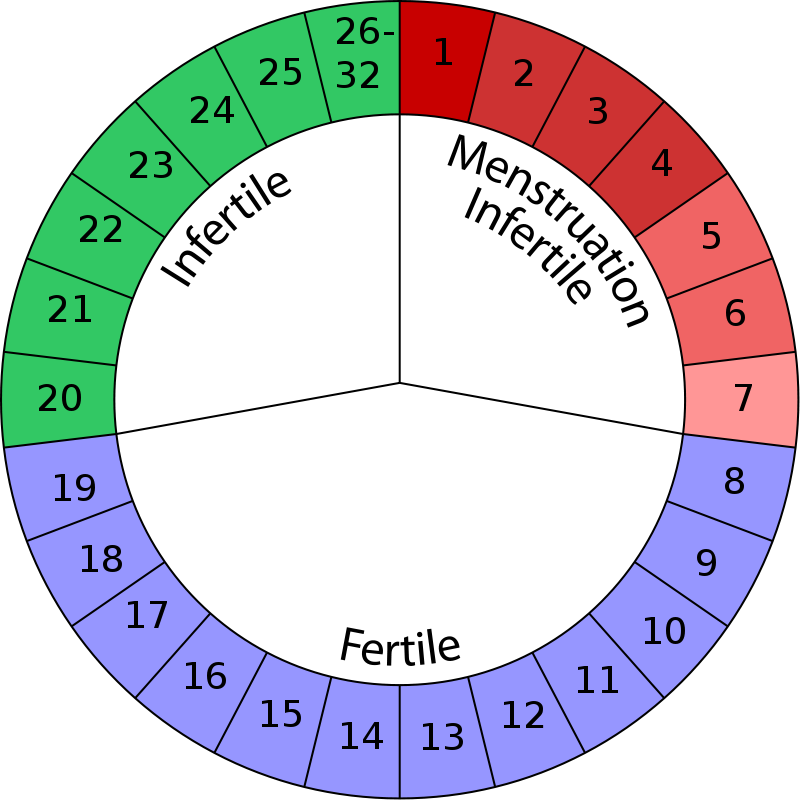
Headaches are one of the most common discomforts experienced during pregnancy and may occur at any time during your pregnancy, but they tend to be most common during the first and third trimesters.
During the first trimester, your body experiences a surge of hormones and an increase in blood volume. These two changes can cause more frequent headaches. These headaches may be further aggravated by stress, poor posture or changes in your vision.
Other causes of headaches during pregnancy may involve one or more of the following:
- Lack of sleep
- Low blood sugar
- Dehydration
- Caffeine withdrawal
- Stress (due to many changes)
Women who have regular migraine headaches may discover that they experience fewer migraines during pregnancy; however, some women may encounter the same number or even more migraine headaches. If you are pregnant, it is important to talk to your health care provider about any medications that you may be taking for headaches.
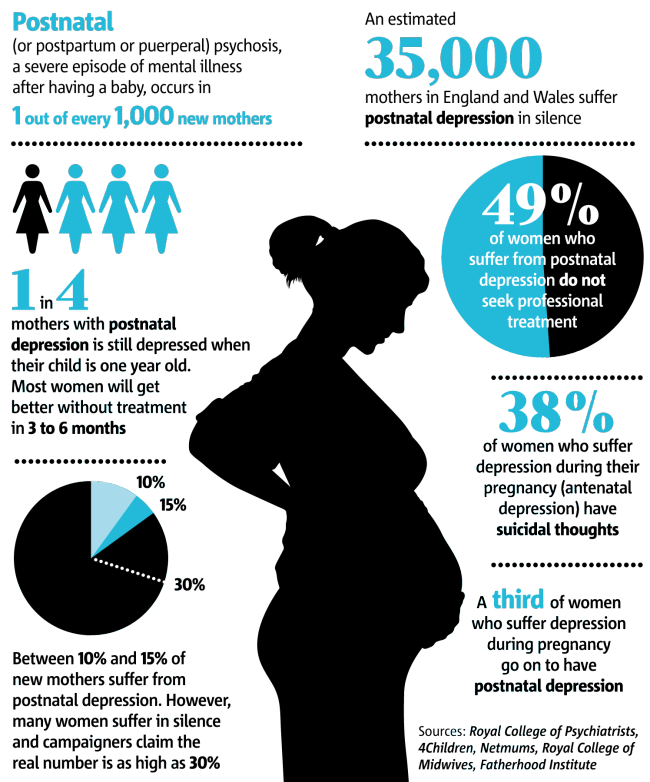
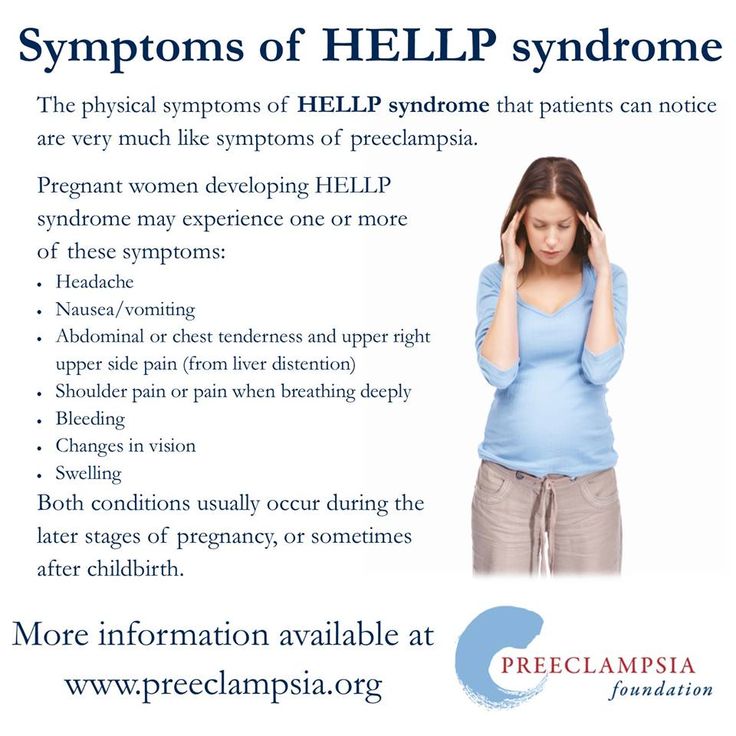
Headaches during the third trimester tend to be related more often to poor posture and tension from carrying extra weight. Headaches during the third trimester may also be caused by a condition called preeclampsia, which is high blood pressure during pregnancy.
How Do I Treat Headaches During Pregnancy?
During pregnancy, you want to try and relieve your headache by natural means if possible, however your health care provider may recommend acetaminophen.
You may want to try to relieve your headache with one or more of the following natural remedies:
- If you have a sinus headache, apply a warm compress around your eyes and nose
- If you have a tension headache, apply a cold compress or ice pack at the base of your neck
- Maintain your blood sugar by eating smaller, more frequent meals – this may also help prevent future headaches
- Get a massage – massaging your shoulders and neck is an effective way to relieve pain
- Rest in a dark room and practice deep breathing
- Take a warm shower or bath
- Practice good posture (especially during the third trimester)
- Get plenty of rest and relaxation
- Exercise
- Eat well-balanced meals
You may also reduce the likelihood of migraine headaches by avoiding common triggers of migraine headaches:
- Chocolate
- Alcohol
- Yogurt
- Aged cheese
- Peanuts
- Bread with fresh yeast
- Preserved meats
- Sour cream
When Should I Contact My Doctor?
- Before taking any medications
- If you do not experience any relief from the remedies above
- Your headaches get worse or more persistent
- You experience headaches that are different than normal
- Your headaches are accompanied by blurry vision, sudden weight gain, pain in the upper right abdomen, and swelling in the hands and face
Want to Know More?
- 7 Common Discomforts of Pregnancy
- Treating Muscle Cramps Naturally During Pregnancy
- Pregnancy and Leg Cramps
Compiled using information from the following sources:
1. Williams Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 55.
Williams Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 55.
2. National Headache Foundation.
https://www.headaches.org
3. Mayo Clinic Guide To A Healthy Pregnancy Harms, Roger W., M.D., et al, Part 3.
Pregnancy and Headaches: When Should I Worry?
Pregnancy is a beautiful thing to be celebrated, but few people fill you in on the not-so-great symptoms that may occur during the journey. Namely, heartburn, gas, constipation and, for some pregnant mamas, headaches.
While headaches can be just another normal symptom of pregnancy, should they ever be a cause for concern?
“Headaches are common in women both in and outside of pregnancy,” said Kelley Saunders, MD, an OBGYN with Banner – University Medicine Women’s Institute. “But whether they are normal or not should always be discussed with your doctor."
Here is some insight into what causes headaches during pregnancy, some remedies to treat them and why your doctor should be kept in the loop.
Is it a headache or something else?
It isn’t always easy to tell what kind of headache you’re having, but the most common types of headaches during pregnancy are tension-type headaches, migraines and cluster headaches.
Tension headaches are the most common kind of headache in pregnant women. It can feel like someone is trying to squish your head like a watermelon. If you carry your stress in your shoulders and neck, you may be more susceptible to this kind of headache.
Migraines are a particular type of headache that occur on one side of the head. For some women, migraines can get worse the first few months and then improve in later stages of pregnancy. For others, they may experience no change, decrease or difference in their migraines.
Cluster headaches are less common but can occur during pregnancy. You’ll suddenly have severe pain around your eyes or temples usually about the same time every day.
The good news is that there are plenty of pregnancy-safe things you can do to prevent and relieve the most common pregnancy headaches.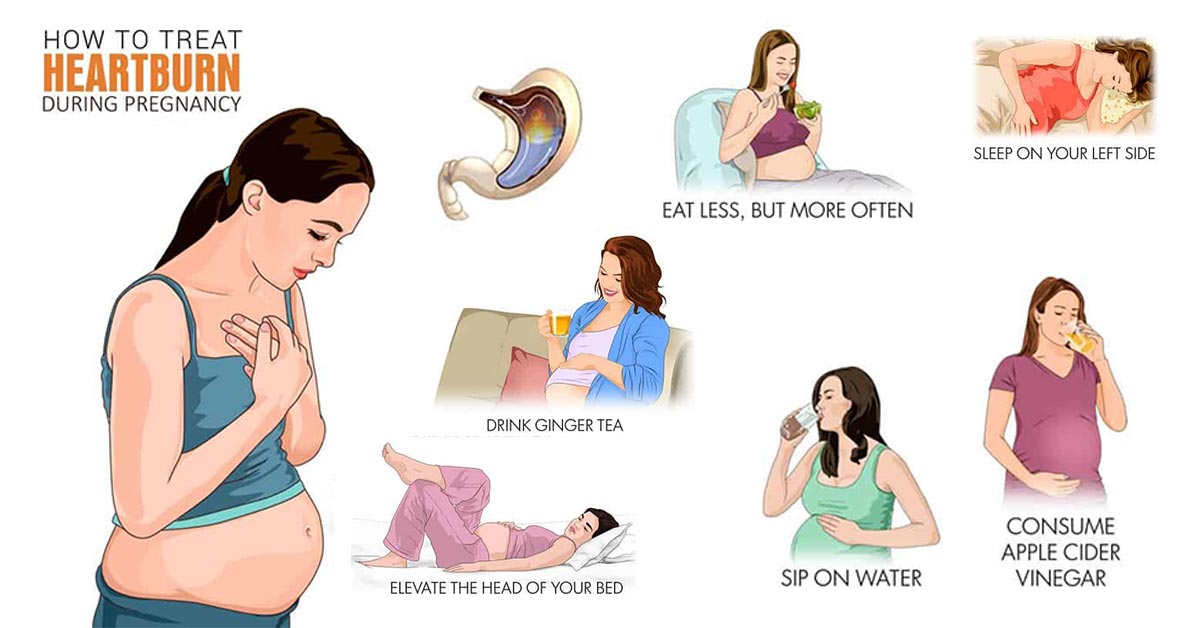
Tips for relieving mild headaches
- Get plenty of rest. Sleep is especially hard later in your pregnancy but is so important to physical and mental health. Find yourself a comfy prenatal pillow and snuggle away.
- Drink plenty of water. Pregnant moms require more water than the average person. While you may want to avoid extra trips to the bathroom, adequate fluid intake is important for you and baby.
- Eat regular, well-balanced meals. To prevent low blood sugar, eat small meals throughout the day. Avoid sugar, like soda and candy.
- Get a prenatal massage. A full-body massage can release tension in the muscles of your neck, shoulders and back.
- Use warm compresses on head, neck and shoulders.
- Avoid triggers. Keep a journal to help identify specific triggers so you can learn what to avoid. Some common headache triggers include strong odors and nitrites or nitrates.

- Try exercise and relaxation techniques. There’s evidence that regular exercise can reduce stress and boost overall mood. Check with your doctor first before starting any new fitness routines.
- Take acetaminophen to relieve symptoms (as approved by doctor).
- Take caffeine in doses less than 200mg in a day (as approved by doctor).
If you have a history of migraines, however, your doctor may treat them differently during pregnancy. Discuss with your doctor what medications are safe to take during pregnancy.
Is my headache a cause for concern?
Sometimes. Headaches tend to be more common in the first and third trimesters, but they can occur in the second trimester as well. While there are common causes for headaches during pregnancy, it’s important to note that headaches during the second and third trimester can also be due to high blood pressure, called preeclampsia.
“Preeclampsia is a pregnancy-related condition that requires prompt evaluation and management with an obstetrician or maternal fetal medicine specialist,” Dr. Saunders said. “Elevated blood pressure prior to pregnancy puts a woman at increased risk for preeclampsia.”
Saunders said. “Elevated blood pressure prior to pregnancy puts a woman at increased risk for preeclampsia.”
When should I call my doctor?
Whether you experience headaches or not, it’s always important to discuss your pre-pregnancy history, obstetrical history and concerns with your doctor for an individualized assessment and management plan. However, if none of the above treatments resolve your mild headache or your headaches become more frequent and severe, talk to your doctor to determine the cause.
“This includes new headaches that present after 20 weeks, a sudden onset of severe headaches, headaches associated with a fever, mental health changes, elevated blood pressure and vision changes,” Dr. Saunders said. “It’s important to keep an open line of communication with your physician and let them know about any changes in your health so they can rule out anything serious."
Got questions? We can help!
If a headache is keeping you up at night and your doctor isn’t available, call the Banner Nurse Now line, a free health care service that offers advice 24-hours a day, seven days a week.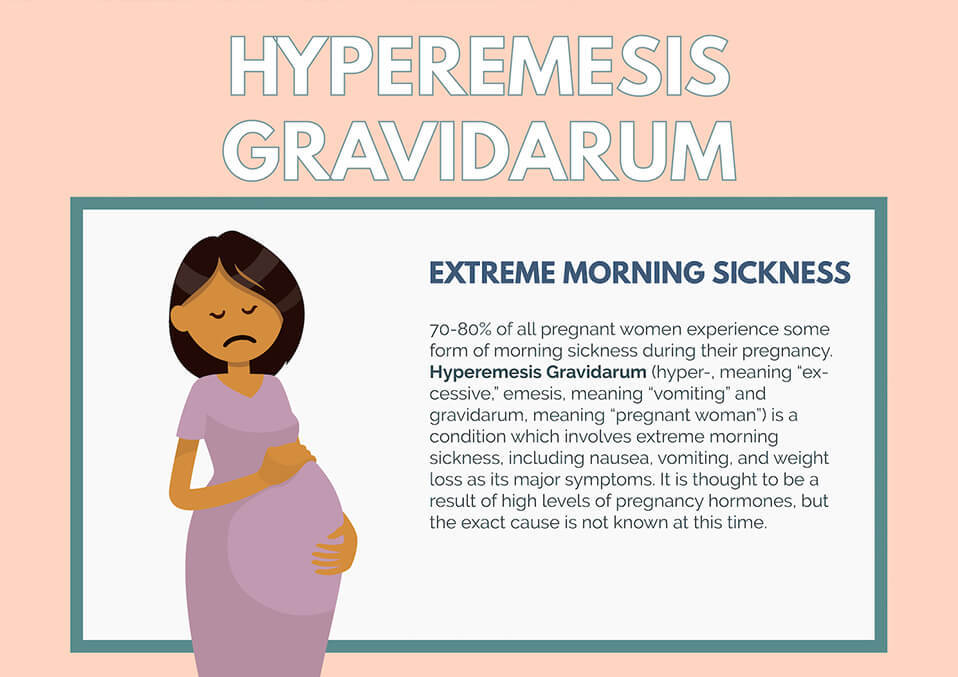 Call 844-259-9494.
Call 844-259-9494.
Check out other pregnancy articles on our Banner Health blog
Pregnancy is an exciting, but also a bit scary time (especially if this is your first baby). Here are some other reads to help guide you through the trimesters and welcoming baby:
- 5 Tips for Having a Happy, Healthy Pregnancy
- Expect the Unexpected: How Your Body Changes During Pregnancy
- What To Expect In The Second Trimester
- Understanding Pulmonary Embolism Risk During Pregnancy
Women's Health Pregnancy
Join the Conversation
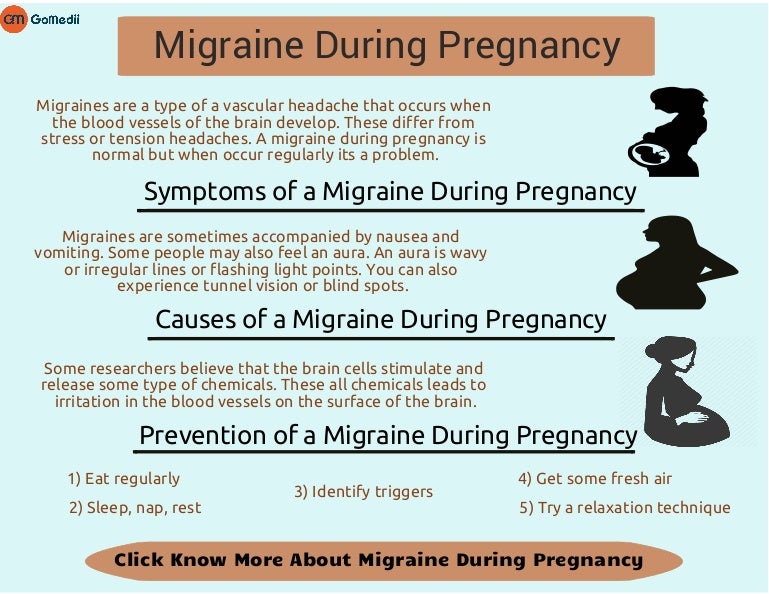
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, because:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.
 nine0003
nine0003
Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop. nine0003
In other women, migraines during pregnancy either remain unchanged or worsen. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman throughout the entire period of pregnancy and after childbirth too.
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help. nine0003
-
Follow lifestyle advice:
-
get enough sleep;
-
drink enough fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations. This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make attacks less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods.
 Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfering with your life, then under the supervision of a specialist, you can resort to drug therapy. nine0003
PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences; nine0003
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted.
 However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription. nine0003
When to see a doctor:
-
migraine occurred for the first time during pregnancy;
-
if migraine attacks suddenly become more frequent and stronger;
-
if the aura became longer or appeared for the first time;
-
if the headache is rapidly increasing and has an unusual character;
-
if the pressure rises during the headache.
Follow our Instagram to read the latest materials on the diagnosis and treatment of headaches!
cluster headache.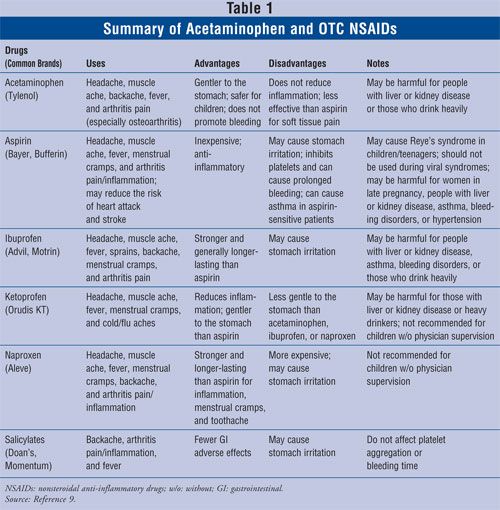 Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh. nine0003
Rare but painful Holidays without headaches. Real holidays Something about osteochondrosis. An excerpt from the book of Kirill Skorobogatykh. nine0003
Migraine during pregnancy: description of the disease, causes, symptoms, cost of treatment in Moscow
Migraine during pregnancy is a fairly common phenomenon that should not be ignored and treated. There are many reasons for the appearance of the problem during this period. After childbirth, the disease usually disappears completely. In the next pregnancy, there is a risk of recurrence of the violation, but it will not necessarily appear again. Since the pain negatively affects not only the condition of the woman, but also the child, it is necessary to take drugs to eliminate the attack, but only those that are allowed for pregnant women. nine0003
Migraine in pregnant women occurs not infrequently, since, in addition to hormonal changes in the body, there are also changes in the psycho-emotional state, which often also act as a trigger for the development of pathology.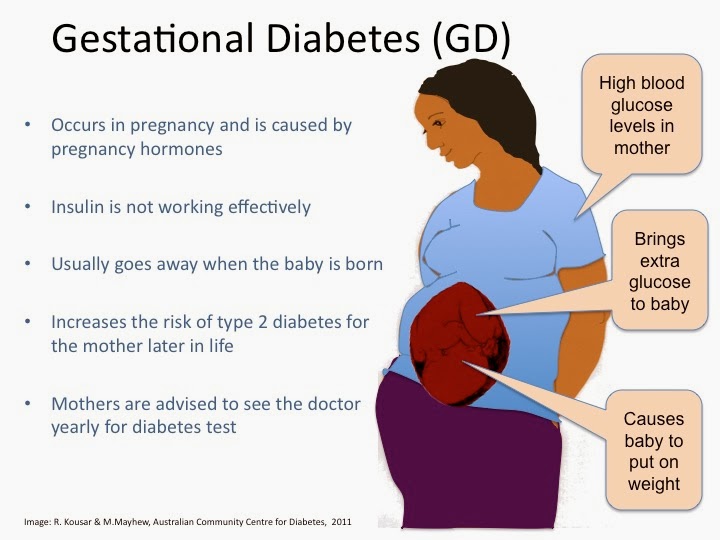 Depending on the duration of pregnancy, a woman's well-being may improve or worsen. The peak of migraines in most cases occurs in the first trimester of pregnancy, when a woman's body undergoes especially rapid hormonal changes. In the later stages, headaches may begin to disturb due to changes in the spine that appear against the background of a shift in the center of gravity. nine0003
Depending on the duration of pregnancy, a woman's well-being may improve or worsen. The peak of migraines in most cases occurs in the first trimester of pregnancy, when a woman's body undergoes especially rapid hormonal changes. In the later stages, headaches may begin to disturb due to changes in the spine that appear against the background of a shift in the center of gravity. nine0003
Reasons
Migraine attacks during pregnancy are usually triggered by specific factors. Migraines during early pregnancy can be caused by the following reasons:
-
specific stresses for the body, which are associated with the process of implantation of the egg and the beginning of the development of the embryo;
-
a sharp change in hormonal levels;
-
dehydration due to changes in metabolic processes in the body and a woman's lack of attention to herself; nine0003
-
the appearance of food intolerance against the background of early toxicosis.
Also, a number of women in the first trimester of pregnancy often experience migraine-provoking nervous strain due to constant concern about their condition, the development of the child and the upcoming birth.
In the second trimester, a woman has a significant improvement in her condition. The frequency of seizures is reduced, and because of the ability to use more drugs, they become less painful. The main provocateurs of the appearance of headaches in this period are the following factors: nine0003
-
physical overload - it occurs if a woman does not reduce physical activity, continuing to lead the same lifestyle as before pregnancy. As a result, an attack occurs as a protest of the body against what is happening;
-
strong emotional experience;
-
sudden changes in the weather - they affect a woman if she suffered from meteorological dependence before pregnancy; nine0003
-
inhalation of very sweet heavy odours.

In the third trimester of pregnancy, the intensity of migraine increases. Due to the ongoing changes in the spine, blood circulation begins to deteriorate to a large extent, due to which even a slight vascular spasm is enough for a migraine attack. The main reasons that can cause it are:
-
drinking a large amount of liquid at once - in order not to provoke an attack, you need to drink often, but little by little, thereby not causing a sharp influx of water into the blood; nine0003
-
staying in an uncomfortable position, which significantly worsens blood circulation in the lower extremities;
-
prolonged stay in the supine position, which also worsens blood circulation;
-
eating spicy or spicy foods;
-
great excitement or prolonged nervous tension. nine0003
Migraines may persist for some time after childbirth due to hormonal changes in the body. However, this phenomenon is not always the case and is considered the exception rather than the rule for migraine during pregnancy.
However, this phenomenon is not always the case and is considered the exception rather than the rule for migraine during pregnancy.
Is an aura possible
Migraine with aura occurs in pregnant women with the same frequency as the classical one. In a quarter of cases, a few minutes before an attack or a maximum of an hour before it, a woman develops previous neurological disorders. If they do not appear strongly, then the patient has time to take medications, thereby relieving an attack, or to return home. When the symptoms of the aura are strong, they can cause no less torment than the pain attack itself. nine0003
You can talk about the presence of an aura in a woman if any of the following symptoms are present before a migraine attack:
-
visual disturbances - these may cause loss of visual fields, temporary loss of vision in one or both eyes, flickering flies before the eyes or flashes of light;
-
severe weakness - it can spread to the whole body, but more often it is felt only in the limbs of the side from which the head will hurt in the future.
 The opposite side of the body suffers much less often; nine0003
The opposite side of the body suffers much less often; nine0003 -
tingling in the limbs and upper half of the body, even affecting the tongue and lips;
-
goosebumps;
-
complete loss or significant reduction in the sensation of limbs;
-
various speech disorders such as confusion or slurring.
Quite often, in pregnant women with migraine with aura, such a phenomenon is noted that if during this period the effect of the negative factor is eliminated, a further attack does not develop, even if medications are not taken. Because of this, in such a situation, a woman needs to fix as accurately as possible what caused the deterioration. nine0003
Is an attack dangerous for the fetus
Today, thanks to numerous studies, doctors have been able to find out whether a migraine attack affects the fetus. The unborn child is able to feel the emotions of the mother and her pain, which is why there is a negative change in his condition at the time of the attack.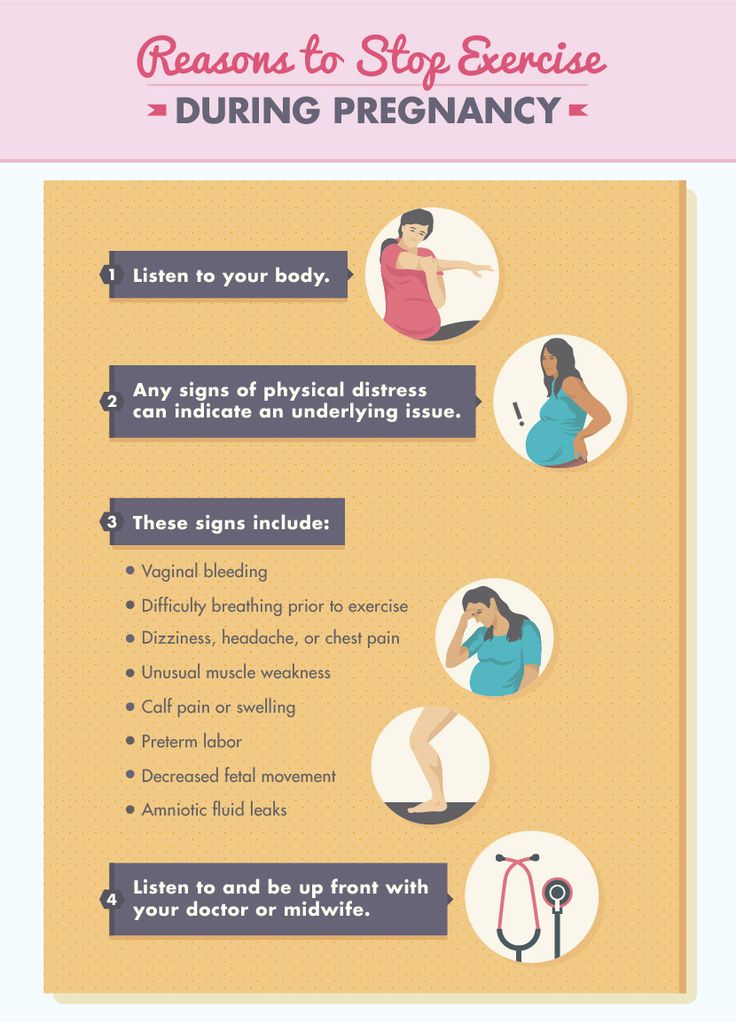 Also, against the background of pain, a spasm of the vessels supplying the placenta often occurs. As a result, the fetus begins to receive significantly less oxygen, which causes hypoxia in it, which, with frequent repetitions of migraine attacks, can cause mental development disorders against the background of brain damage. nine0003
Also, against the background of pain, a spasm of the vessels supplying the placenta often occurs. As a result, the fetus begins to receive significantly less oxygen, which causes hypoxia in it, which, with frequent repetitions of migraine attacks, can cause mental development disorders against the background of brain damage. nine0003
Medicines prescribed for pregnant women must be taken during an attack without fail. They will not harm the child, as they do not penetrate the placental barrier and effectively relieve pain, eliminating its negative impact. It is unacceptable to prescribe such funds on your own, since mistakes can be too dangerous for the fetus. All drugs are correctly selected taking into account the duration of pregnancy only by a doctor.
Prophylaxis
Preventive measures against migraine during pregnancy greatly help to reduce the risk of this problem. Additionally, it will help improve well-being and a proper lifestyle. The main preventive measures during pregnancy include: nine0003
-
full sleep at least 9 hours a day;
-
taking light sedatives when nervous tension appears;
-
providing a comfortable temperature in the room;
-
drinking frequently and in small amounts;
-
eating food that does not cause a burning sensation in the mouth.