Women give milk
Causes & How It Works
Overview
Lactation is the process of making human milk. It's driven by hormones and results in milk coming from your nipple.What is lactation?
Lactation is the process of producing and releasing milk from the mammary glands in your breasts. Lactation begins in pregnancy when hormonal changes signal the mammary glands to make milk in preparation for the birth of your baby. It’s also possible to induce lactation without a pregnancy using the same hormones that your body makes during pregnancy. Lactation ends once your body stops producing milk.
Feeding your baby directly from your breasts is called breastfeeding (or sometimes chestfeeding) or nursing. You can also feed your baby milk that you have expressed or pumped from your breast and saved in a bottle.
Where does human milk come from?
Human milk comes from your mammary glands inside your breasts. These glands have several parts that work together to produce and secrete milk:
- Alveoli: These tiny, grape-like sacs produce and store milk.
A cluster of alveoli is called lobules, and each lobule connects to a lobe.
- Milk ducts: Each lobe connects to a milk duct. You can have up to 20 lobes, with one milk duct for every lobe. Milk ducts carry milk from the lobules of alveoli to your nipples.
- Areola: The dark area surrounding your nipple, which has sensitive nerve endings that lets your body know when to release milk. To release milk, the entire areola needs stimulation.
- Nipple: Your nipple contains several tiny pores (up to about 20) that secrete milk. Nerves on your nipple respond to suckling (either by a baby, your hands or a breast pump). This stimulation tells your brain to release milk from the alveoli through the milk ducts and out of your nipple.
It helps to think of the lactation system as a large tree. Your nipple is the trunk of the tree. The milk ducts are the branches. The leaves are the alveoli.
Why do people lactate?
The primary reason people lactate is to feed a baby. Lactation is a biological, hormonal response that occurs during and after pregnancy to feed a newborn baby. Your body triggers specific hormones to initiate milk production and ejection (releasing of milk). All mammals lactate for this purpose and it’s possible to induce lactation in men and in non-pregnant women using the right hormone medications.
Lactation is a biological, hormonal response that occurs during and after pregnancy to feed a newborn baby. Your body triggers specific hormones to initiate milk production and ejection (releasing of milk). All mammals lactate for this purpose and it’s possible to induce lactation in men and in non-pregnant women using the right hormone medications.
Function
What triggers lactation?
A series of hormonal events, which begin when you’re pregnant, trigger the lactation process. That process is called lactogenesis.
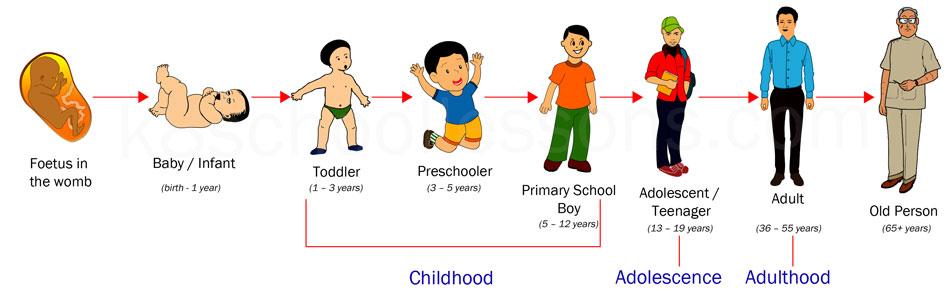
Stage one lactogenesis: This begins around the 16th week of pregnancy and lasts until a few days after you give birth.
- Estrogen and progesterone rise and cause your milk ducts to grow in number and size. This causes your breasts to become fuller. Your mammary glands begin to prepare for milk production.
- Your nipples darken and your areolas become larger.
- Your Montgomery glands (small bumps on the areola) secrete oil to lubricate your nipple.

- Your body begins making colostrum. It’s highly nutritious and filling and serves as your baby’s first milk.
Stage two lactogenesis: This stage starts about two or three days postpartum (after giving birth). It’s when milk production intensifies.
- Once your baby and placenta are delivered, a sudden drop in your estrogen and progesterone causes the hormone prolactin to take over.
- Prolactin is the hormone that produces milk.
- You’ll notice your milk production increases dramatically at this stage. It’s often referred to as milk “coming in.”
- Your breasts are often engorged (or overly full of milk) to the point where they feel sore, painful or tender.
Stage three lactogenesis: This describes the rest of the time you lactate.
- Lactation generally continues as long as milk is removed from your breast.
- The more milk that’s removed, the more milk your body makes to replace it. Frequent feeding or pumping will cause your body to make more milk.

Hormones for lactation
The hormone prolactin controls the amount of milk you produce, and your body begins producing prolactin early in pregnancy. At first, the high levels of estrogen, progesterone and other pregnancy hormones suppress prolactin. Once you deliver the placenta, those pregnancy hormones drop and prolactin takes charge.
When your baby suckles, it stimulates nerves that tell your body to release prolactin and oxytocin. Prolactin causes the alveoli to make milk and oxytocin causes muscle contractions that push out of the alveoli and through the milk ducts.
When milk is released, it’s called a “letdown,” and it takes about 30 seconds of suckling before the letdown occurs. Because you can’t control which breast receives the hormones, the letdown can cause milk to drip from both nipples.
Inducing lactation in people who aren’t pregnant requires medication that mimics hormones your body makes during pregnancy. Suckling from the nipple can initiate lactation, either with a breast pump or by a baby. This is a complex process that involves working closely with a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
This is a complex process that involves working closely with a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
When do you lactate during pregnancy?
Lactation begins as early as a few weeks into the second trimester of your pregnancy. As estrogen and progesterone levels rise, your body prepares for lactation by increasing the number of milk ducts in your breasts, and those milk ducts will transport milk from the alveoli to your nipples. About midway through pregnancy, your body creates colostrum, which is your baby’s first milk.
Can you lactate when you’re not pregnant?
Yes, it’s possible to lactate if you’re not pregnant. Inducing lactation is a complex process that usually involves using hormone-mimicking drugs for several months to produce milk. The second part of lactation is expressing the milk through your nipple. Stimulation from infant suckling, pumping with a breast pump or hand-expressing signals the brain to release the milk. It’s common for people in this situation to receive assistance from a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
It’s common for people in this situation to receive assistance from a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
How do you stop lactation?
There are many reasons why you might need to stop producing milk, and you can stop lactating either naturally or with the help of hormonal drugs.
Natural milk suppression
Lactation is a supply-and-demand process. Your milk supply gradually goes down as your baby relies less on breast milk, or as you reduce the number of times you nurse or pump. Generally, if you decrease the volume of milk removed from your breasts, your body will slow milk production.
Suppressing your milk can feel uncomfortable and most people will become engorged (the term for overfilled breasts). You may also leak milk or develop a clogged milk duct. However, you can treat that pain by taking an over-the-counter pain reliever, wearing a firm bra or using an ice pack on your breasts.
Medication suppression
Medications can also be an option if you need to stop producing milk. Your healthcare provider can explain more about lactation-suppressing drugs, as well as the benefits and possible side effects.
Anatomy
Where are the mammary glands located?
Mammary glands are commonly called breasts and both genders have them. They are located on your chest and are composed of connective tissue, fat and special glandular tissue that makes milk. A woman’s glandular tissue is slightly different because it contains the alveoli and lobules necessary for producing milk. Women also have much more glandular tissue.
Conditions and Disorders
What are common conditions that affect your ability to lactate?
The ability to lactate and the length of time you’re able to produce milk varies. Some can produce milk for years, while others have trouble producing enough milk for their baby.
Some common factors that can impact lactation or breastfeeding are:
- Hormonal levels and conditions.

- Medications.
- Undergoing radiation therapy in the past.
- Trauma to your breast or nipples.
- Breast augmentation, reconstruction or other breast surgeries.
- Other medical conditions like HIV infection.
- Use of drugs and alcohol.
If you’re nursing or pumping your milk to bottle-feed your baby, you should always consult with your healthcare provider before starting any new medications or treatments. Many medications can pass to your baby through breast milk, which may have dangerous effects on your baby.
What is lactational amenorrhea?
Lactation amenorrhea (ah-men-oh-re-uh) means you aren’t menstruating (getting a period) due to lactation. When you’re lactating, your body produces prolactin, the hormone that produces milk. Prolactin reduces the amount of luteinizing hormone (LH) in your body, which helps trigger the release of an egg during ovulation. If you aren’t producing enough LH, you can’t ovulate or get your period.![]() The length of time you can be amenorrheic due to lactation varies from a few months or until you’re completely done lactating.
The length of time you can be amenorrheic due to lactation varies from a few months or until you’re completely done lactating.
Does lactation reduce my risk of any diseases?
Studies have shown that breastfeeding reduces a woman’s risk of ovarian and breast cancers. It can also lower your risk for Type 2 diabetes and high blood pressure.
Care
How do you maintain milk production?
Maintaining lactation is mostly based on supply and demand. The more your baby breastfeeds or the more milk you express with a breast pump, the more your body will make. There are ways to suppress lactation with hormones or oral contraceptives. If you wish to maintain lactation, some things you should do are:
- Continue nursing on-demand or pump milk frequently (approximately every four hours).
- Eat a healthy diet with enough calories. Low-calorie diets can decrease milk supply.
- Drink plenty of water to stay hydrated. Human milk is primarily water.
- Avoid smoking, drugs or alcohol.
 These can reduce your supply and transfer to your milk.
These can reduce your supply and transfer to your milk.
Frequently Asked Questions
What is the difference between lactation and colostrum?
Lactation describes the process of making and secreting milk from your breast. Colostrum is the first milk your breasts create during lactation and the first milk your baby drinks. It’s thick, yellow and commonly called “liquid gold.” Colostrum is high in protein, minerals, vitamins and antibodies.
What is hormone therapy for inducing lactation?
Couples or families who wish to induce lactation, maybe because of adoption, surrogacy or other reasons, can try hormone therapy. Induced lactation means you’re creating a milk supply without being pregnant. It’s a process that involves taking estrogen and progesterone for several months to make your body believe it’s pregnant. This helps prepare your breasts for lactation. Some medications and herbs are believed to help establish a milk supply, too.
Several weeks before your baby arrives, begin pumping your breasts with a breast pump. This encourages your body to release prolactin, which produces milk. Ideally, you express your milk several times a day, just like you would if you had a baby. This helps establish a supply. You can also freeze any milk you produce for use once your baby arrives.
This encourages your body to release prolactin, which produces milk. Ideally, you express your milk several times a day, just like you would if you had a baby. This helps establish a supply. You can also freeze any milk you produce for use once your baby arrives.
If you’re considering this as an option, you should talk to your healthcare provider about your desire to feed your baby with human milk. Induced lactation works for many people, but not all.
A note from Cleveland Clinic
If you want to feed your baby human milk, it’s helpful to understand the process of lactation so you know what to expect. Talk to your healthcare provider about how to best prepare for nursing or expressing milk. Remember, lactation can look different for everyone depending on your circumstances and health history. If you struggle with lactation at any point, you may feel embarrassed or even ashamed. But struggling with lactation is very common, and lactation specialists and other healthcare providers can help you as you try to overcome these difficulties.
Causes & How It Works
Overview
Lactation is the process of making human milk. It's driven by hormones and results in milk coming from your nipple.What is lactation?
Lactation is the process of producing and releasing milk from the mammary glands in your breasts. Lactation begins in pregnancy when hormonal changes signal the mammary glands to make milk in preparation for the birth of your baby. It’s also possible to induce lactation without a pregnancy using the same hormones that your body makes during pregnancy. Lactation ends once your body stops producing milk.
Feeding your baby directly from your breasts is called breastfeeding (or sometimes chestfeeding) or nursing. You can also feed your baby milk that you have expressed or pumped from your breast and saved in a bottle.
Where does human milk come from?
Human milk comes from your mammary glands inside your breasts. These glands have several parts that work together to produce and secrete milk:
- Alveoli: These tiny, grape-like sacs produce and store milk.
 A cluster of alveoli is called lobules, and each lobule connects to a lobe.
A cluster of alveoli is called lobules, and each lobule connects to a lobe. - Milk ducts: Each lobe connects to a milk duct. You can have up to 20 lobes, with one milk duct for every lobe. Milk ducts carry milk from the lobules of alveoli to your nipples.
- Areola: The dark area surrounding your nipple, which has sensitive nerve endings that lets your body know when to release milk. To release milk, the entire areola needs stimulation.
- Nipple: Your nipple contains several tiny pores (up to about 20) that secrete milk. Nerves on your nipple respond to suckling (either by a baby, your hands or a breast pump). This stimulation tells your brain to release milk from the alveoli through the milk ducts and out of your nipple.
It helps to think of the lactation system as a large tree. Your nipple is the trunk of the tree. The milk ducts are the branches. The leaves are the alveoli.
Why do people lactate?
The primary reason people lactate is to feed a baby. Lactation is a biological, hormonal response that occurs during and after pregnancy to feed a newborn baby. Your body triggers specific hormones to initiate milk production and ejection (releasing of milk). All mammals lactate for this purpose and it’s possible to induce lactation in men and in non-pregnant women using the right hormone medications.
Lactation is a biological, hormonal response that occurs during and after pregnancy to feed a newborn baby. Your body triggers specific hormones to initiate milk production and ejection (releasing of milk). All mammals lactate for this purpose and it’s possible to induce lactation in men and in non-pregnant women using the right hormone medications.
Function
What triggers lactation?
A series of hormonal events, which begin when you’re pregnant, trigger the lactation process. That process is called lactogenesis.
Stage one lactogenesis: This begins around the 16th week of pregnancy and lasts until a few days after you give birth.
- Estrogen and progesterone rise and cause your milk ducts to grow in number and size. This causes your breasts to become fuller. Your mammary glands begin to prepare for milk production.
- Your nipples darken and your areolas become larger.
- Your Montgomery glands (small bumps on the areola) secrete oil to lubricate your nipple.
- Your body begins making colostrum. It’s highly nutritious and filling and serves as your baby’s first milk.
Stage two lactogenesis: This stage starts about two or three days postpartum (after giving birth). It’s when milk production intensifies.
- Once your baby and placenta are delivered, a sudden drop in your estrogen and progesterone causes the hormone prolactin to take over.
- Prolactin is the hormone that produces milk.
- You’ll notice your milk production increases dramatically at this stage. It’s often referred to as milk “coming in.”
- Your breasts are often engorged (or overly full of milk) to the point where they feel sore, painful or tender.
Stage three lactogenesis: This describes the rest of the time you lactate.
- Lactation generally continues as long as milk is removed from your breast.
- The more milk that’s removed, the more milk your body makes to replace it. Frequent feeding or pumping will cause your body to make more milk.

Hormones for lactation
The hormone prolactin controls the amount of milk you produce, and your body begins producing prolactin early in pregnancy. At first, the high levels of estrogen, progesterone and other pregnancy hormones suppress prolactin. Once you deliver the placenta, those pregnancy hormones drop and prolactin takes charge.
When your baby suckles, it stimulates nerves that tell your body to release prolactin and oxytocin. Prolactin causes the alveoli to make milk and oxytocin causes muscle contractions that push out of the alveoli and through the milk ducts.
When milk is released, it’s called a “letdown,” and it takes about 30 seconds of suckling before the letdown occurs. Because you can’t control which breast receives the hormones, the letdown can cause milk to drip from both nipples.
Inducing lactation in people who aren’t pregnant requires medication that mimics hormones your body makes during pregnancy. Suckling from the nipple can initiate lactation, either with a breast pump or by a baby. This is a complex process that involves working closely with a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
This is a complex process that involves working closely with a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
When do you lactate during pregnancy?
Lactation begins as early as a few weeks into the second trimester of your pregnancy. As estrogen and progesterone levels rise, your body prepares for lactation by increasing the number of milk ducts in your breasts, and those milk ducts will transport milk from the alveoli to your nipples. About midway through pregnancy, your body creates colostrum, which is your baby’s first milk.
Can you lactate when you’re not pregnant?
Yes, it’s possible to lactate if you’re not pregnant. Inducing lactation is a complex process that usually involves using hormone-mimicking drugs for several months to produce milk. The second part of lactation is expressing the milk through your nipple. Stimulation from infant suckling, pumping with a breast pump or hand-expressing signals the brain to release the milk. It’s common for people in this situation to receive assistance from a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
It’s common for people in this situation to receive assistance from a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
How do you stop lactation?
There are many reasons why you might need to stop producing milk, and you can stop lactating either naturally or with the help of hormonal drugs.
Natural milk suppression
Lactation is a supply-and-demand process. Your milk supply gradually goes down as your baby relies less on breast milk, or as you reduce the number of times you nurse or pump. Generally, if you decrease the volume of milk removed from your breasts, your body will slow milk production.
Suppressing your milk can feel uncomfortable and most people will become engorged (the term for overfilled breasts). You may also leak milk or develop a clogged milk duct. However, you can treat that pain by taking an over-the-counter pain reliever, wearing a firm bra or using an ice pack on your breasts.
Medication suppression
Medications can also be an option if you need to stop producing milk. Your healthcare provider can explain more about lactation-suppressing drugs, as well as the benefits and possible side effects.
Anatomy
Where are the mammary glands located?
Mammary glands are commonly called breasts and both genders have them. They are located on your chest and are composed of connective tissue, fat and special glandular tissue that makes milk. A woman’s glandular tissue is slightly different because it contains the alveoli and lobules necessary for producing milk. Women also have much more glandular tissue.
Conditions and Disorders
What are common conditions that affect your ability to lactate?
The ability to lactate and the length of time you’re able to produce milk varies. Some can produce milk for years, while others have trouble producing enough milk for their baby.
Some common factors that can impact lactation or breastfeeding are:
- Hormonal levels and conditions.

- Medications.
- Undergoing radiation therapy in the past.
- Trauma to your breast or nipples.
- Breast augmentation, reconstruction or other breast surgeries.
- Other medical conditions like HIV infection.
- Use of drugs and alcohol.
If you’re nursing or pumping your milk to bottle-feed your baby, you should always consult with your healthcare provider before starting any new medications or treatments. Many medications can pass to your baby through breast milk, which may have dangerous effects on your baby.
What is lactational amenorrhea?
Lactation amenorrhea (ah-men-oh-re-uh) means you aren’t menstruating (getting a period) due to lactation. When you’re lactating, your body produces prolactin, the hormone that produces milk. Prolactin reduces the amount of luteinizing hormone (LH) in your body, which helps trigger the release of an egg during ovulation. If you aren’t producing enough LH, you can’t ovulate or get your period. The length of time you can be amenorrheic due to lactation varies from a few months or until you’re completely done lactating.
The length of time you can be amenorrheic due to lactation varies from a few months or until you’re completely done lactating.
Does lactation reduce my risk of any diseases?
Studies have shown that breastfeeding reduces a woman’s risk of ovarian and breast cancers. It can also lower your risk for Type 2 diabetes and high blood pressure.
Care
How do you maintain milk production?
Maintaining lactation is mostly based on supply and demand. The more your baby breastfeeds or the more milk you express with a breast pump, the more your body will make. There are ways to suppress lactation with hormones or oral contraceptives. If you wish to maintain lactation, some things you should do are:
- Continue nursing on-demand or pump milk frequently (approximately every four hours).
- Eat a healthy diet with enough calories. Low-calorie diets can decrease milk supply.
- Drink plenty of water to stay hydrated. Human milk is primarily water.
- Avoid smoking, drugs or alcohol.
 These can reduce your supply and transfer to your milk.
These can reduce your supply and transfer to your milk.
Frequently Asked Questions
What is the difference between lactation and colostrum?
Lactation describes the process of making and secreting milk from your breast. Colostrum is the first milk your breasts create during lactation and the first milk your baby drinks. It’s thick, yellow and commonly called “liquid gold.” Colostrum is high in protein, minerals, vitamins and antibodies.
What is hormone therapy for inducing lactation?
Couples or families who wish to induce lactation, maybe because of adoption, surrogacy or other reasons, can try hormone therapy. Induced lactation means you’re creating a milk supply without being pregnant. It’s a process that involves taking estrogen and progesterone for several months to make your body believe it’s pregnant. This helps prepare your breasts for lactation. Some medications and herbs are believed to help establish a milk supply, too.
Several weeks before your baby arrives, begin pumping your breasts with a breast pump. This encourages your body to release prolactin, which produces milk. Ideally, you express your milk several times a day, just like you would if you had a baby. This helps establish a supply. You can also freeze any milk you produce for use once your baby arrives.
This encourages your body to release prolactin, which produces milk. Ideally, you express your milk several times a day, just like you would if you had a baby. This helps establish a supply. You can also freeze any milk you produce for use once your baby arrives.
If you’re considering this as an option, you should talk to your healthcare provider about your desire to feed your baby with human milk. Induced lactation works for many people, but not all.
A note from Cleveland Clinic
If you want to feed your baby human milk, it’s helpful to understand the process of lactation so you know what to expect. Talk to your healthcare provider about how to best prepare for nursing or expressing milk. Remember, lactation can look different for everyone depending on your circumstances and health history. If you struggle with lactation at any point, you may feel embarrassed or even ashamed. But struggling with lactation is very common, and lactation specialists and other healthcare providers can help you as you try to overcome these difficulties.
Colostrum during pregnancy | Medela
Colostrum is sometimes called liquid gold, and not only because of its color. We will tell you why this first food is so important for a newborn baby.
Share this information
Colostrum, the first milk produced at the start of breastfeeding, is the ideal nutrition for a newborn. It is very concentrated and rich in proteins and nutrients, so even in small quantities it saturates the tiny tummy of a newborn for a long time. Colostrum is low in fat and easy to digest, yet provides the baby with all the essential ingredients for an optimal developmental start. And perhaps most importantly, it plays a decisive role in the formation of the baby's immune system. nine0003
Colostrum looks thicker and yellower than mature milk. Its composition also differs in accordance with the special needs of the newborn.
Colostrum fights infections
Almost two-thirds of the cells in colostrum are white blood cells, which not only protect the baby's body from infections, but also teach them to fight them themselves. 1 “White blood cells are very important for the development of immunity. They provide protection and counteract pathogenic microbes,” says Professor Peter Hartmann of the University of Western Australia, a leading lactation expert. nine0003
1 “White blood cells are very important for the development of immunity. They provide protection and counteract pathogenic microbes,” says Professor Peter Hartmann of the University of Western Australia, a leading lactation expert. nine0003
After giving birth, your body no longer protects the baby, and he must confront the new dangers of the world on his own. The white blood cells found in colostrum produce antibodies that can neutralize bacteria and viruses. These antibodies are especially good at dealing with indigestion and diarrhea, which is very important for very young children, whose intestines are not yet fully developed.
Colostrum supports the child's immune system and intestinal function
Colostrum is especially rich in secretory immunoglobulin A -
is the most important antibody that protects the child from diseases, but not through the circulatory system, but as a protective coating of the mucous membrane of the gastrointestinal tract. 2 “Molecules that provide a mother's immune defenses enter the mother's bloodstream into the breast, where they combine to form secretory immunoglobulin A, which is then transferred to the baby along with colostrum,” explains Professor Hartmann. “Secretory immunoglobulin A accumulates on the mucous membranes of the intestines and respiratory system of the child and protects him from diseases that the mother has already had.” nine0003
2 “Molecules that provide a mother's immune defenses enter the mother's bloodstream into the breast, where they combine to form secretory immunoglobulin A, which is then transferred to the baby along with colostrum,” explains Professor Hartmann. “Secretory immunoglobulin A accumulates on the mucous membranes of the intestines and respiratory system of the child and protects him from diseases that the mother has already had.” nine0003
Colostrum also contains many other immunological components and growth factors that stimulate the development of protective mucous membranes in the intestines of the child, and the prebiotics contained in it contribute to the formation of beneficial microflora. 3
Colostrum prevents jaundice
Colostrum not only protects against indigestion, but also has a laxative effect. This helps newborns to empty the intestines frequently, removing from it everything that was digested there in the prenatal state, in the form of meconium - dark and viscous feces. nine0003
nine0003
Frequent stools in newborns also reduce the risk of jaundice. A baby is born with a high level of red blood cells that absorb oxygen from the air. As these cells break down, the liver helps to process them, producing a by-product called bilirubin. If the child's liver is not yet sufficiently formed to process it, bilirubin begins to be deposited in the body, causing jaundice. 4 The laxative properties of colostrum help the baby to remove bilirubin from the body along with the stool. nine0003
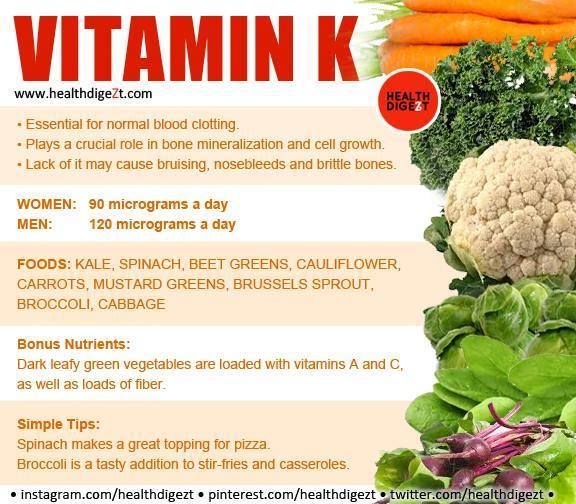
Colostrum contains vitamins and minerals
Carotenoids and vitamin A give colostrum its characteristic yellow color. . 7 Babies are usually born with a low supply of vitamin A, 8 and colostrum helps to replenish it.
"The first three days are especially important for establishing breastfeeding"
In addition, colostrum is rich in minerals, such as magnesium, which is good for the baby's heart and bones, and copper and zinc, which are involved in the development of the immune system. 9.10 Zinc also contributes to the development of the brain, and there is almost four times more zinc in colostrum than in mature milk, 10 because the brain of a newborn must develop rapidly.
9.10 Zinc also contributes to the development of the brain, and there is almost four times more zinc in colostrum than in mature milk, 10 because the brain of a newborn must develop rapidly.
Colostrum helps your baby grow and develop
Colostrum contains many other ingredients that help your baby grow and develop. The role of some of them is still unknown to scientists. nine0003
“Colostrum retains its composition for about 30 hours after the baby is born,” says Prof. Hartmann. - It contains quite a lot of proteins, because all the antibodies in its composition are essentially proteins. It is relatively low in lactose [milk sugar] and has a different fat composition than mature milk.”
In addition, colostrum is close in composition to the amniotic fluid that your baby swallowed and excreted while in the womb, making it ideal for adapting to the outside world. nine0015 11
Transition from colostrum to mature milk
Breast milk usually begins to arrive two to four days after birth. The breasts become firmer and fuller, and instead of colostrum, transitional milk is excreted, which is whiter in color and more creamy in consistency.
The breasts become firmer and fuller, and instead of colostrum, transitional milk is excreted, which is whiter in color and more creamy in consistency.
“The first three days are especially important for establishing breastfeeding,” says Prof. Hartmann. “If everything is done correctly during this period, lactation is likely to be good, and the baby will be able to grow normally.” nine0003
It seems unbelievable now, but in just one year your baby will be able to walk and maybe even talk. Colostrum is produced for only a few days, but makes an invaluable contribution to the development of the baby during the first 12 months, and the resulting benefits remain with him for life.
Want to know more? Read our free e-book Surprising Breast Milk Facts and article What is Transitional Milk?.
Literature
1 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. 2 Pribylova J et al. Colostrum of healthy mothers contains broad spectrum of secretory IgA autoantibodies. nine0081 J Clin Immunol. 2012;32(6):1372-1380. - Pribylova J. et al., "Healthy mother's colostrum contains a broad spectrum of secretory autoimmune antibodies to immunoglobulin A". W Clean Immunol. 2012;32(6):1372-1380. 3 Bode L. Human milk oligosaccharides: every baby needs a sugar mama. Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." nine0081 Glycobiology (Glycobiology). 2012;22(9):1147-1162. 4 Mitra S, Rennie J. 5 Patton S et al. Carotenoids of human colostrum. Lipids. nine0081 1990;25(3):159-165. - Patton S. et al., Carotenoids in Maternal Colostrum Lipidz. 1990;25(3):159-165. 6 Gilbert C , Foster Childhood blindness in the context of VISION 2020--the right to sight. Bull World Health Organ. 2001;79(3):227-232. - Gilbert S., Foster A., "Childhood Blindness in Context VISION 2020 - the right to see". Bull World Health Organ. 2001;79(3):227-232. 7 Bates CJ. Vitamin A. Lancet. 1995;345(8941):31-35. 8 World Health Organization. e-Library of Evidence for Nutrition Actions (eLENA) [Internet]. Geneva , Switzerland : WHO ; 2018 [ Accessed : 05/14/2018]. Available from Evidence E-Library for WHO nutrition activities ( eLENA ) [Internet]. Geneva, Switzerland: WHO; 2018 [visited 14 May 2018] Article at: [ www.who.int/elena/titles/vitamina_infants/en/ ] 9 Kulski JK, Hartmann PE. Changes in human milk composition during the initiation of lactation. AUST J EXP Biol  Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl Immunology. 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.  Neonatal jaundice: aetiology, diagnosis and treatment. Br J Hosp Med (Lond). 20172;78(12):699-704. - Mitra S, Rennie J, Neonatal Jaundice: Etiology, Diagnosis, Treatment. Br J Hosp Med (Lond). 20172;78(12):699-704.
Neonatal jaundice: aetiology, diagnosis and treatment. Br J Hosp Med (Lond). 20172;78(12):699-704. - Mitra S, Rennie J, Neonatal Jaundice: Etiology, Diagnosis, Treatment. Br J Hosp Med (Lond). 20172;78(12):699-704.  — Bates S.J., "Vitamin A". Lancet (Lancet) 1995;345(8941):31-35.
— Bates S.J., "Vitamin A". Lancet (Lancet) 1995;345(8941):31-35.  Aust Zh Exp Biol Med Sai. 1981;59(1):101-114. nine0081
Aust Zh Exp Biol Med Sai. 1981;59(1):101-114. nine0081
10 Casey CE Studies in human lactation: zinc, copper, manganese and chromium in human milk in the first month of lactation. Am J Clin Nutr 1985;41(6):1193-1200. - Casey S.I. et al., Female Lactation Study: Zinc, Copper, Magnesium, and Chromium in Breast Milk in the Early Months of Lactation. nine0081 Am J Clean Nutr. 1985;41(6):1193-1200.
11 Marlier L et al. Neonatal responsiveness to the odor of amniotic and lacteal fluids: a test of perinatal chemosensory continuity. Child Dev . 1998;69(3):611-623. - Marlier L. et al., "Newborn responses to amniotic and milk odors: testing perinatal chemosensory continuity. Child Dev. 1998;69(3):611-623.
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. nine0015 1 It's not for nothing that this time is called the “magic hour”!
nine0015 1 It's not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ” nine0003
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK. nine0003
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions. In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a cesarean section or other complications during childbirth,
You can still establish skin-to-skin contact with your baby and breastfeed him in the first hours after birth. nine0003
nine0003
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding.” nine0003
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. However, all of them later successfully switched to breastfeeding,” says Kathy. nine0003
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital. nine0003
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
- There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. nine0015 6
“If the baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable. There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently. "
"
How often should a newborn be fed? nine0013
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy. nine0003
Milk usually arrives on the second or fourth day after birth. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise." nine0003
Camille, a mother from Australia, experienced this. “For the first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable. nine0003
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional. ” nine0003
” nine0003
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. nine0015 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.
- Colour: greenish black. nine0426
- Texture: sticky like tar.
Day two
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases. nine0015 11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that your baby is not getting enough milk. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends. nine0003
nine0003
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. A doctor should also be consulted if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the feces, and also if the weight recorded at birth has not recovered within two weeks. 11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J9 Mammary Gland Biol Neoplasia . 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." nine0081 Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." nine0081 G Egypt Public Health Assoc. 2004;79(1-2):1-2.
J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." nine0081 G Egypt Public Health Assoc. 2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding. " F Midwifery Women Health. 2007;52(6):638-642.
" F Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208.