What is gdm in pregnancy
Gestational Diabetes Mellitus (GDM) | Johns Hopkins Medicine
What is gestational diabetes mellitus?
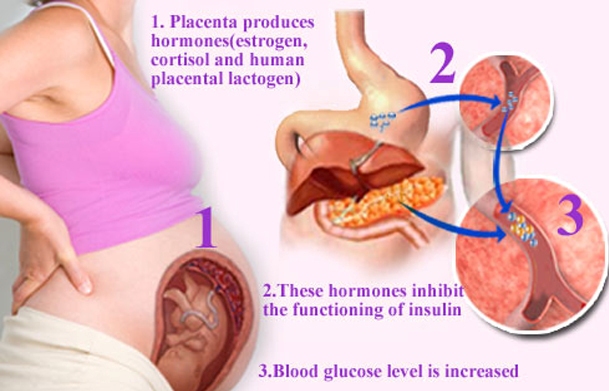
Gestational diabetes mellitus (GDM) is a condition in which a hormone made by the placenta prevents the body from using insulin effectively. Glucose builds up in the blood instead of being absorbed by the cells.
Unlike type 1 diabetes, gestational diabetes is not caused by a lack of insulin, but by other hormones produced during pregnancy that can make insulin less effective, a condition referred to as insulin resistance. Gestational diabetic symptoms disappear following delivery.
Approximately 3 to 8 percent of all pregnant women in the United States are diagnosed with gestational diabetes.
What causes gestational diabetes mellitus?
Although the cause of GDM is not known, there are some theories as to why the condition occurs.
The placenta supplies a growing fetus with nutrients and water, and also produces a variety of hormones to maintain the pregnancy. Some of these hormones (estrogen, cortisol, and human placental lactogen) can have a blocking effect on insulin. This is called contra-insulin effect, which usually begins about 20 to 24 weeks into the pregnancy.
As the placenta grows, more of these hormones are produced, and the risk of insulin resistance becomes greater. Normally, the pancreas is able to make additional insulin to overcome insulin resistance, but when the production of insulin is not enough to overcome the effect of the placental hormones, gestational diabetes results.
What are the risks factors associated with gestational diabetes mellitus?
Although any woman can develop GDM during pregnancy, some of the factors that may increase the risk include the following:
Overweight or obesity
Family history of diabetes
Having given birth previously to an infant weighing greater than 9 pounds
Age (women who are older than 25 are at a greater risk for developing gestational diabetes than younger women)
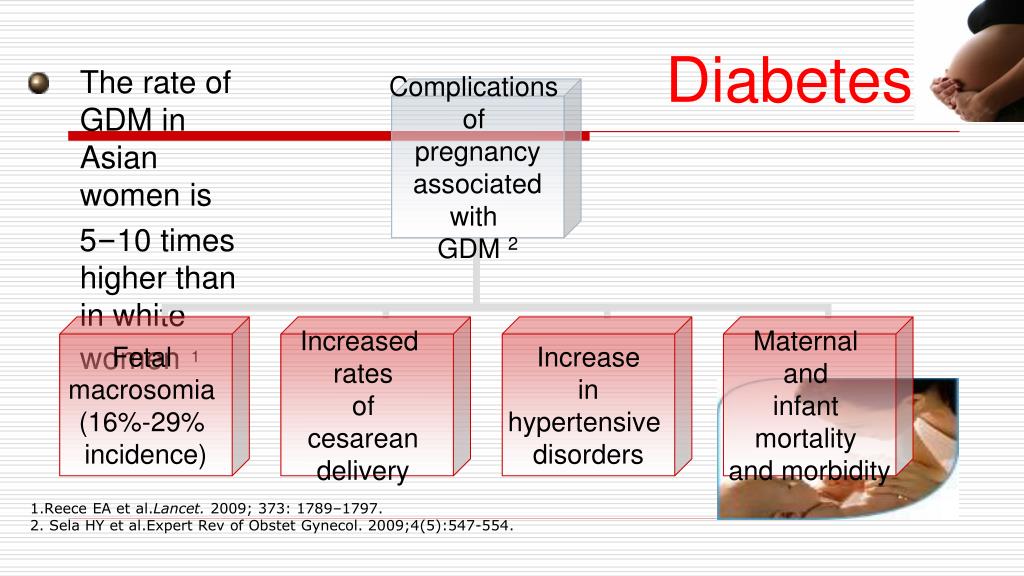
Race (women who are African-American, American Indian, Asian American, Hispanic or Latino, or Pacific Islander have a higher risk)
Prediabetes, also known as impaired glucose tolerance
Although increased glucose in the urine is often included in the list of risk factors, it is not believed to be a reliable indicator for GDM.
How is gestational diabetes mellitus diagnosed?
The American Diabetes Association recommends screening for undiagnosed type 2 diabetes at the first prenatal visit in women with diabetes risk factors. In pregnant women not known to have diabetes, GDM testing should be performed at 24 to 28 weeks of gestation.
In addition, women with diagnosed GDM should be screened for persistent diabetes 6 to 12 weeks postpartum. It is also recommended that women with a history of GDM undergo lifelong screening for the development of diabetes or prediabetes at least every three years.
What is the treatment for gestational diabetes mellitus?
Specific treatment for gestational diabetes will be determined by your doctor based on:
Your age, overall health, and medical history
Extent of the disease
Your tolerance for specific medications, procedures, or therapies
Expectations for the course of the disease
Your opinion or preference
Treatment for gestational diabetes focuses on keeping blood glucose levels in the normal range. Treatment may include:
Treatment may include:
Possible complications for the baby
Unlike type 1 diabetes, gestational diabetes generally occurs too late to cause birth defects. Birth defects usually originate sometime during the first trimester (before the 13th week) of pregnancy. The insulin resistance from the contra-insulin hormones produced by the placenta does not usually occur until approximately the 24th week. Women with gestational diabetes mellitus generally have normal blood sugar levels during the critical first trimester.
The complications of GDM are usually manageable and preventable. The key to prevention is careful control of blood sugar levels just as soon as the diagnosis of diabetes is made.
Infants of mothers with gestational diabetes are vulnerable to several chemical imbalances, such as low serum calcium and low serum magnesium levels, but, in general, there are two major problems of gestational diabetes: macrosomia and hypoglycemia:
Macrosomia.
 Macrosomia refers to a baby who is considerably larger than normal. All of the nutrients the fetus receives come directly from the mother's blood. If the maternal blood has too much glucose, the pancreas of the fetus senses the high glucose levels and produces more insulin in an attempt to use this glucose. The fetus converts the extra glucose to fat. Even when the mother has gestational diabetes, the fetus is able to produce all the insulin it needs. The combination of high blood glucose levels from the mother and high insulin levels in the fetus results in large deposits of fat which causes the fetus to grow excessively large.
Macrosomia refers to a baby who is considerably larger than normal. All of the nutrients the fetus receives come directly from the mother's blood. If the maternal blood has too much glucose, the pancreas of the fetus senses the high glucose levels and produces more insulin in an attempt to use this glucose. The fetus converts the extra glucose to fat. Even when the mother has gestational diabetes, the fetus is able to produce all the insulin it needs. The combination of high blood glucose levels from the mother and high insulin levels in the fetus results in large deposits of fat which causes the fetus to grow excessively large.Hypoglycemia. Hypoglycemia refers to low blood sugar in the baby immediately after delivery. This problem occurs if the mother's blood sugar levels have been consistently high, causing the fetus to have a high level of insulin in its circulation. After delivery, the baby continues to have a high insulin level, but it no longer has the high level of sugar from its mother, resulting in the newborn's blood sugar level becoming very low.
 The baby's blood sugar level is checked after birth, and if the level is too low, it may be necessary to give the baby glucose intravenously.
The baby's blood sugar level is checked after birth, and if the level is too low, it may be necessary to give the baby glucose intravenously.
Blood glucose is monitored very closely during labor. Insulin may be given to keep the mother's blood sugar in a normal range to prevent the baby's blood sugar from dropping excessively after delivery.
Gestational Diabetes | CDC
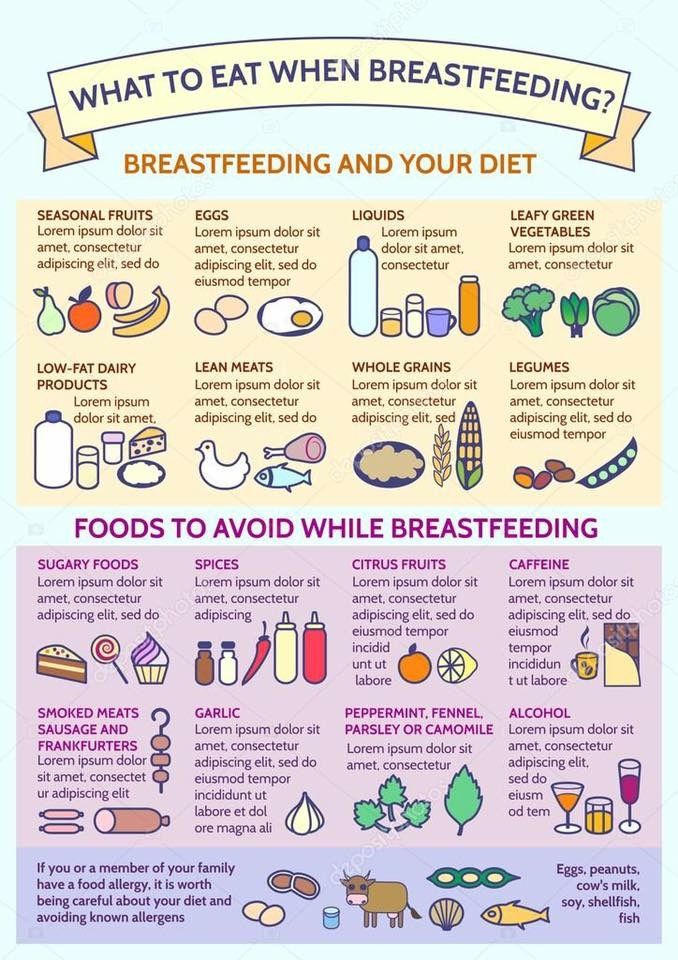
Follow a healthy eating plan to nourish you and your baby.
Gestational diabetes is a type of diabetes that can develop during pregnancy in women who don’t already have diabetes. Every year, 2% to 10% of pregnancies in the United States are affected by gestational diabetes. Managing gestational diabetes will help make sure you have a healthy pregnancy and a healthy baby.
What Causes Gestational Diabetes?
Gestational diabetes occurs when your body can’t make enough insulin during your pregnancy. Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into the cells in your body for use as energy.
During pregnancy, your body makes more hormones and goes through other changes, such as weight gain. These changes cause your body’s cells to use insulin less effectively, a condition called insulin resistance. Insulin resistance increases your body’s need for insulin.
All pregnant women have some insulin resistance during late pregnancy. However, some women have insulin resistance even before they get pregnant. They start pregnancy with an increased need for insulin and are more likely to have gestational diabetes.
About 50% of women with gestational diabetes go on to develop type 2 diabetes, but there are steps you can take to prevent it. Talk to your doctor about how to lower your risk and how often to have your blood sugar checked to make sure you’re on track.
Symptoms and Risk Factors
Gestational diabetes typically doesn’t have any symptoms. Your medical history and whether you have any risk factors may suggest to your doctor that you could have gestational diabetes, but you’ll need to be tested to know for sure.
Related Health Problems
Having gestational diabetes can increase your risk of high blood pressure during pregnancy. It can also increase your risk of having a large baby that needs to be delivered by cesarean section (C-section).
If you have gestational diabetes, your baby is at higher risk of:
- Being very large (9 pounds or more), which can make delivery more difficult
- Being born early, which can cause breathing and other problems
- Having low blood sugar
- Developing type 2 diabetes later in life
Your blood sugar levels will usually return to normal after your baby is born. However, about 50% of women with gestational diabetes go on to develop type 2 diabetes. You can lower your risk by reaching a healthy body weight after delivery. Visit your doctor to have your blood sugar tested 6 to 12 weeks after your baby is born and then every 1 to 3 years to make sure your levels are on target.
Testing for Gestational Diabetes
It’s important to be tested for gestational diabetes so you can begin treatment to protect your health and your baby’s health.
Gestational diabetes usually develops around the 24th week of pregnancy, so you’ll probably be tested between 24 and 28 weeks.
If you’re at higher risk for gestational diabetes, your doctor may test you earlier. Blood sugar that’s higher than normal early in your pregnancy may indicate you have type 1 or type 2 diabetes rather than gestational diabetes.
Prevention
Before you get pregnant, you may be able to prevent gestational diabetes by losing weight if you’re overweight and getting regular physical activity.
Don’t try to lose weight if you’re already pregnant. You’ll need to gain some weight—but not too quickly—for your baby to be healthy. Talk to your doctor about how much weight you should gain for a healthy pregnancy.
Treatment for Gestational Diabetes
You can do a lot to manage your gestational diabetes. Go to all your prenatal appointments and follow your treatment plan, including:
- Checking your blood sugar to make sure your levels stay in a healthy range.

- Eating healthy food in the right amounts at the right times. Follow a healthy eating plan created by your doctor or dietitian.
- Being active. Regular physical activity that’s moderately intense (such as brisk walking) lowers your blood sugar and makes you more sensitive to insulin so your body won’t need as much. Make sure to check with your doctor about what kind of physical activity you can do and if there are any kinds you should avoid.
- Monitoring your baby. Your doctor will check your baby’s growth and development.
If healthy eating and being active aren’t enough to manage your blood sugar, your doctor may prescribe insulin, metformin, or other medication.
- Diabetes During Pregnancy
- Diabetes and Women
- Insulin Resistance
- Diabetes Articles
- Infographics
Diagnosis - Diabetesinformationsportal
"Sugar test" for diagnosing diabetes in pregnant women
Between 24 and 28 weeks of pregnancy, women are routinely screened for gestational diabetes. This is commonly referred to as the "sugar test". Specialists talk about the oral glucose tolerance test (OGTT).
This is commonly referred to as the "sugar test". Specialists talk about the oral glucose tolerance test (OGTT).
While pregnant woman drinks sugar solution . Shortly thereafter, her blood sugar level is checked. The value shows how the body copes with the processing of incoming sugar. As a rule, a two-stage procedure is used, which does not pose any risk to the child. nine0007
Pretest with 50 grams of glucose
First, every pregnant woman is offered a pre-test. A woman drinks a glass of water with 50 grams of glucose (sugar) dissolved in it. This test does not have to be done on an empty stomach. An hour later, blood is taken from her cubital vein and the level of sugar in the blood is determined. If the blood glucose is within the normal range, the test is completed. If after hour your blood glucose is 135 mg/dL (7.5 mmol/L) or more , a second glucose tolerance test is performed. This extended glucose tolerance test is done with 75 grams of glucose.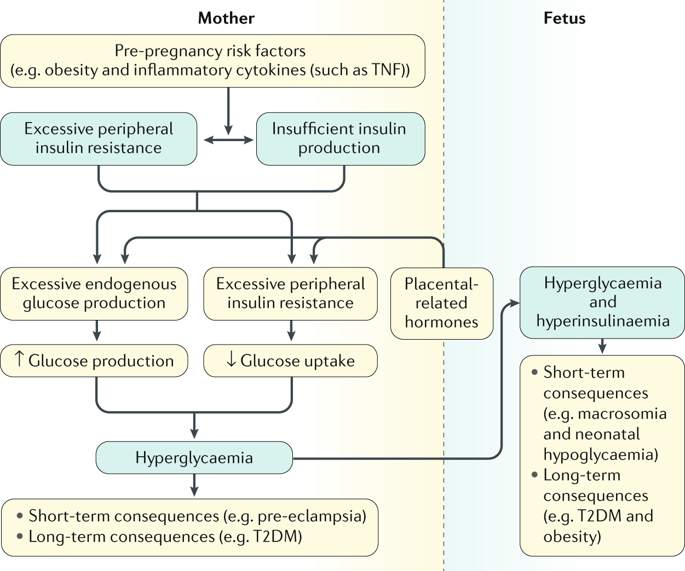 The result of the preliminary test itself is still not a diagnosis of .
The result of the preliminary test itself is still not a diagnosis of .
Diagnostic test with 75 grams of glucose
The so-called diagnostic (extended) glucose tolerance test is performed on an empty stomach. A pregnant woman should not eat anything and should not drink sugary drinks for at least 8 hours before the test. First, blood is taken from her, then she drinks a sugar solution with 75 grams of glucose. After that, blood is taken two more times: one hour and two hours after taking the sugar solution. nine0007
Gestational diabetes is diagnosed when one of the following three blood sugar levels is reached or exceeded.
- Fasting: 92 mg/dL (5.1 mmol/L)
- After 1 hour: 180 mg/dL (10.0 mmol/L)
- After 2 hours: 153 mg/dL (8.5 mmol/L)
If your fasting blood sugar is 126 mg/dL (7.0 mmol/L) or your blood sugar is 200 mg/dL (11.1 mmol/L) two hours later, gestational diabetes is out of the question. It's Diabetes mellitus, first diagnosed during pregnancy. In this case, additional tests are carried out to determine the form of diabetes and individual selection of therapy. This can be, for example, diabetes mellitus type 2, type 1, or juvenile non-insulin dependent diabetes mellitus (MODY).
It's Diabetes mellitus, first diagnosed during pregnancy. In this case, additional tests are carried out to determine the form of diabetes and individual selection of therapy. This can be, for example, diabetes mellitus type 2, type 1, or juvenile non-insulin dependent diabetes mellitus (MODY).
If gestational diabetes is diagnosed, metabolism needs to be adjusted. Usually it is enough just to adjust the diet. Learn more about treating gestational diabetes.
Is the glucose tolerance test covered by the Health Insurance Fund? nine0003
Normally, the Health Insurance Fund only pays for a preliminary test with 50 grams of glucose. If the result of this test exceeds 135 mg/dL, the Health Insurance Fund reimburses the cost of the subsequent diagnostic test with 75 grams of glucose.
How are women at increased risk of developing diabetes tested?
During the pregnancy consultation, the doctor will find out if there is an increased risk of developing diabetes. An increased risk is possible, for example, if the woman is significantly overweight, pregnancy occurs over the age of 35, and if the woman has already had gestational diabetes before. nine0007
An increased risk is possible, for example, if the woman is significantly overweight, pregnancy occurs over the age of 35, and if the woman has already had gestational diabetes before. nine0007
If there is an increased risk, a blood sugar test should be carried out already in the first trimester, i.e. at the very beginning of pregnancy . To do this, a pregnant woman on an empty stomach (you can’t eat anything and drink drinks with a sugar content for at least 8 hours before the test) takes blood from the cubital vein and determines the level of sugar in the blood.
If the fasting blood sugar level exceeds 92 mg/dL (5.1 mmol/L) , remeasure the next day. If the remeasurement result is between 92 to 125 mg/dL (5.1 to 6.9 mmol/L), the diagnosis of gestational diabetes is confirmed. If the value is lower than indicated, then between the 24th and 28th weeks of pregnancy, a sugar test (glucose tolerance test) is again performed.
A value of 126 mg/dL (7.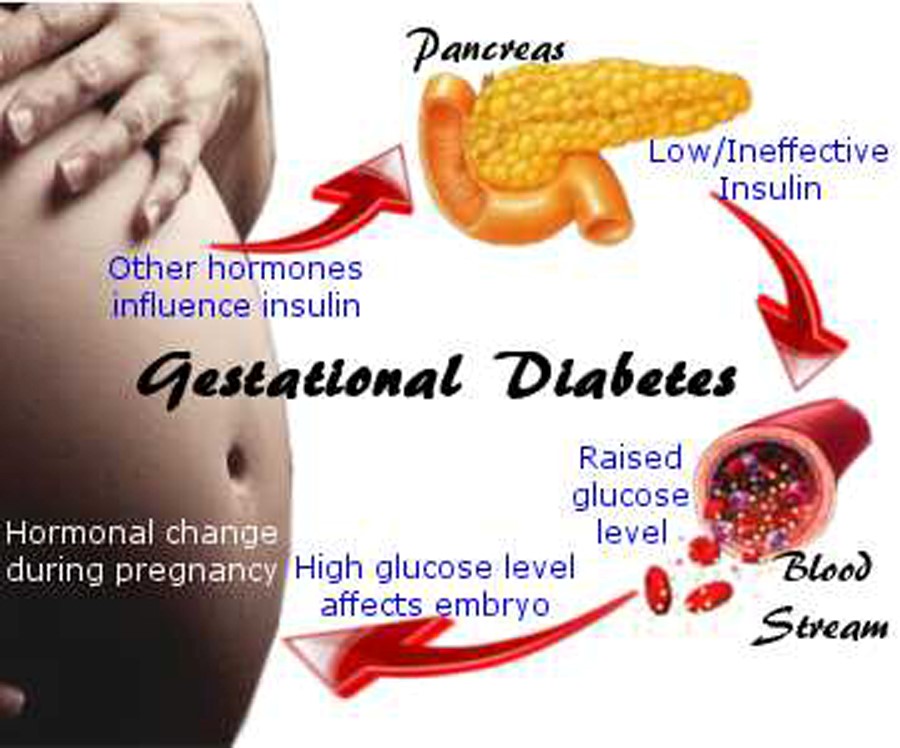 0 mmol/L) or higher indicates that diabetes already existed before pregnancy.
0 mmol/L) or higher indicates that diabetes already existed before pregnancy.
Alternatively, glycated hemoglobin (HbA1c) can be measured. This value shows if your blood sugar has been too high in the past 6-8 weeks. It's like a "long-term memory" of blood sugar. In healthy people without impaired carbohydrate metabolism, it is about 5 percent (31 mmol / mol). nine0007
If the measurement reaches 5.8% (40 mmol/mol), the blood sugar level is re-tested the next day by fasting blood to rule out gestational diabetes. If the repeat measurement is between 92 and 125 mg/dL (5.1 and 6.9 mmol/L), the diagnosis of gestational diabetes is confirmed.
At HbA1c values of 5.9-6.4% (41-46.5 mmol/mol), a glucose tolerance test with 75 grams of glucose is performed to confirm or refute the suspicion of gestational diabetes. nine0007
If the HbA1c value is greater than 6.4% (46.5 mmol/mol), diabetes was already present before pregnancy.
Learn more about risk factors for gestational diabetes.
Gestational Diabetes Questions and Answers - Indevex
Gestational Diabetes Questions and Answers
Gestational diabetes is a form of diabetes that can develop in pregnant women. Gestational diabetes means that the mother has high blood sugar, which may be due to inadequate insulin production. Insulin is a hormone produced by the pancreas and its primary role is to lower blood sugar levels. The hormone "unlocks" the cells so they can receive sugar. Lack of insulin or decreased sensitivity to insulin means that sugar cannot get into the cells. As a result, sugar remains in the blood, causing its level to rise. During pregnancy, a woman's body becomes more sensitive to insulin. This is partly due to
hormonal changes in the placenta. In most cases, as a result of pancreatic insensitivity, more insulin is produced in order to maintain blood glucose at a normal level. However, in some pregnant women, the pancreas cannot adapt to the increased production of needed insulin, resulting in gestational diabetes.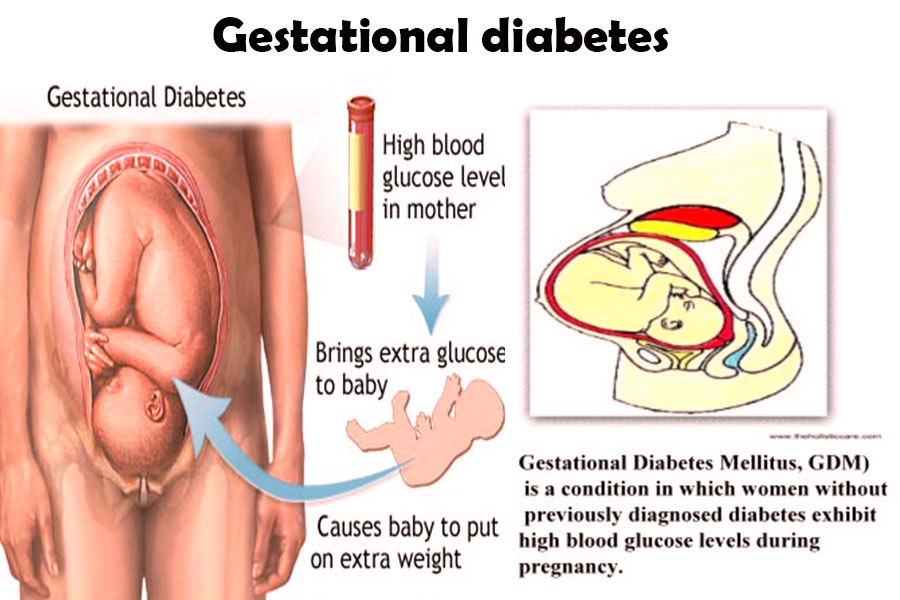 Below you can find answers to questions about how common gestational diabetes is; why it develops in some mothers; what does it affect; what are its symptoms; what are the methods of diagnosis; what are the risks and effects on the intrauterine stage of fetal development. You will also learn about how to avoid and treat gestational diabetes. nine0007
Below you can find answers to questions about how common gestational diabetes is; why it develops in some mothers; what does it affect; what are its symptoms; what are the methods of diagnosis; what are the risks and effects on the intrauterine stage of fetal development. You will also learn about how to avoid and treat gestational diabetes. nine0007
How common is gestational diabetes? What causes gestational diabetes? Who gets gestational diabetes? How can I know if I have gestational diabetes? How is gestational diabetes diagnosed? What are the risks of gestational diabetes? How does gestational diabetes affect the development of a baby in the womb? have I had gestational diabetes before? How can I avoid developing gestational diabetes? What is the treatment for gestational diabetes? What should I do after giving birth?0007
How common is gestational diabetes?
According to numerous studies in Europe and the United States, gestational diabetes develops in about three to five percent of all pregnant women.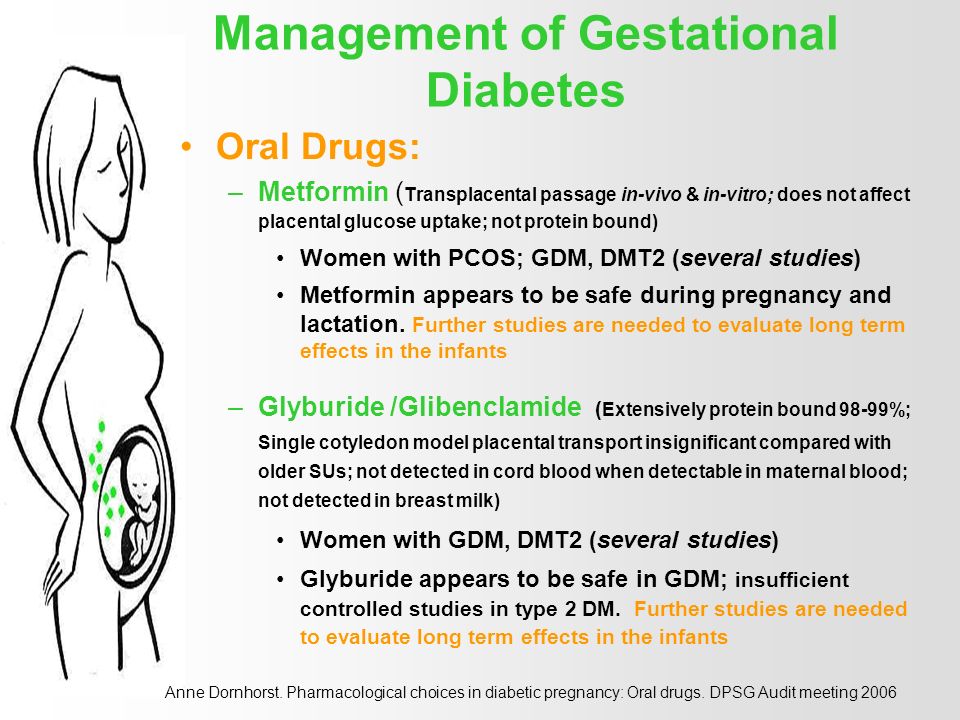 In Sweden, these figures are slightly lower: slightly below three percent. However, new criteria for assessing gestational diabetes could increase the number of women with this diagnosis by two to three times. As a result, more people will be able to receive treatment, which will reduce the risk of the negative impact that high blood sugar has on the expectant mother and her unborn child. nine0007
In Sweden, these figures are slightly lower: slightly below three percent. However, new criteria for assessing gestational diabetes could increase the number of women with this diagnosis by two to three times. As a result, more people will be able to receive treatment, which will reduce the risk of the negative impact that high blood sugar has on the expectant mother and her unborn child. nine0007
What causes gestational diabetes?
The hormone insulin produced by the pancreas lowers blood sugar levels. If you are unable to produce enough insulin, you are at risk of developing gestational diabetes. During pregnancy, especially in the second and third trimesters, insulin sensitivity decreases, which is primarily due to hormones produced in the placenta. This means that the pancreas must increase the production of its own insulin to compensate for the increased need for it. If the pancreas cannot produce more insulin, blood sugar levels rise, leading to gestational diabetes. nine0007
nine0007
Who has gestational diabetes?
There are a number of factors that increase the risk of developing gestational diabetes:
- Family history of diabetes
- The expectant mother was previously diagnosed with gestational diabetes
- Complications from a previous pregnancy such as high birth weight or caesarean section
- Obesity
- Relatively high age of the mother, i.e. over 35 years
- Mother had many pregnancies
- Ethnicity
- Hypertension
- Vitamin D deficiency
There are various theories about why, regardless of the presence of risk factors, some women are more likely to develop gestational diabetes than others.
How can I know if I have gestational diabetes?
It is usually difficult to notice that you have gestational diabetes because the disease rarely develops any obvious symptoms. They are usually mild and not life threatening. nine0007
Most common symptoms:
- Increased thirst
- Frequent urination, large amounts of urine
- Increased appetite
- Fatigue and weakness
- Frequent infections
- Nausea and vomiting
How is gestational diabetes diagnosed?
Because the disease rarely presents with any significant symptoms, gestational diabetes is almost always detected through a blood test performed at the maternity clinic.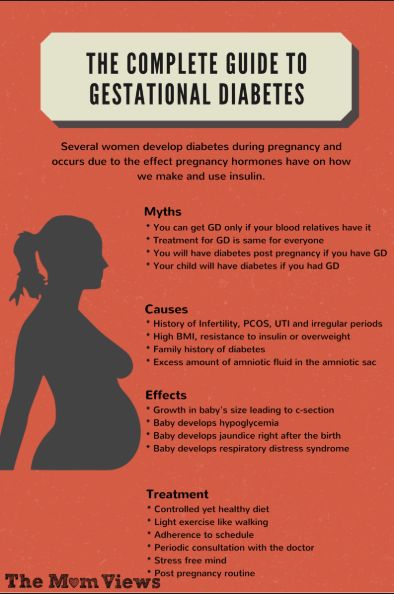 During pregnancy registration, blood sugar levels are checked. If the result is within the normal range, then a similar analysis during pregnancy will be carried out several times. The amount depends on the country of residence. If a blood test shows an elevated level of sugar, a glucose tolerance test is performed, or, as it is often called, a “sugar load”. nine0007
During pregnancy registration, blood sugar levels are checked. If the result is within the normal range, then a similar analysis during pregnancy will be carried out several times. The amount depends on the country of residence. If a blood test shows an elevated level of sugar, a glucose tolerance test is performed, or, as it is often called, a “sugar load”. nine0007
The glucose tolerance test is performed by fasting blood, usually in the morning. No food should be taken 8 hours before the test. Before the test, you should drink a glucose solution, after which the blood sugar level is measured twice over the next two hours. The blood sugar level measured after a meal is referred to in the medical literature as postprandial blood sugar.
If the blood sugar level exceeds the criteria, the person is diagnosed with gestational diabetes. nine0007
What are the risks of gestational diabetes?
Gestational diabetes poses a number of risks during pregnancy for both mother and fetus.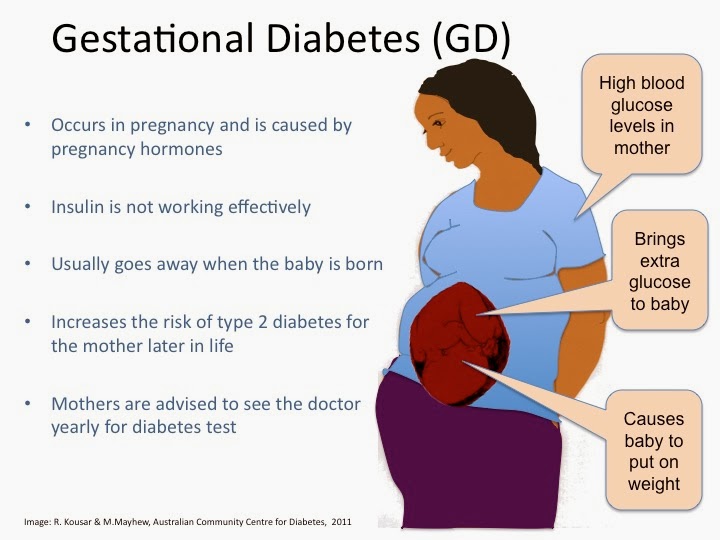
- Large fruit size. Elevated maternal blood sugar leads to increased fetal blood sugar, as glucose is delivered to the fetus through the placenta. To cope with the increase in the amount of sugar (glucose) in the blood, the fetus responds by increasing the production of its own insulin. We can say that the child receives too much too concentrated nutrient solution. As a result, the baby may grow and gain weight too quickly, which in turn can lead to complications during childbirth. nine0032
- Preeclampsia. Gestational diabetes can cause the mother to develop preeclampsia. This condition threatens the life of both mother and fetus.
- Prematurity. Gestational diabetes increases the risk of preterm birth and related complications, which include the infant's need for a breathing machine until the lungs can function on their own.
- Too low blood sugar (hypoglycemia). If a pregnant woman has high blood sugar, this can lead to the fact that the child at birth may suffer from too low blood sugar levels, since the baby's insulin production may be abnormally high (in response to the mother's high blood sugar during pregnancy) .
 Left untreated, this condition can lead to seizures and other complications in the newborn. nine0032
Left untreated, this condition can lead to seizures and other complications in the newborn. nine0032 - Risk of diabetes. Women who have been diagnosed with gestational diabetes in previous pregnancies have a greater risk of developing type 2 diabetes than mothers who did not have gestational diabetes. The child also has an increased risk of developing diabetes and becoming overweight in the future.
How does gestational diabetes affect the development of the baby in the womb?
In most cases, maternal gestational diabetes does not seriously affect the fetus. Elevated blood sugar during the first trimester of pregnancy increases the risk of birth defects in the fetus, but this is rarely associated with gestational diabetes. As a rule, this is due to the fact that the mother had diabetes before pregnancy. nine0007
If blood sugar rises during the last trimester of pregnancy, it can cause abnormal growth of the fetus, which increases the risk of complications during childbirth.
If I have had gestational diabetes before?
The risk increases significantly. This means that already in the early stages of pregnancy you should be supervised in the maternity center. You will receive a referral to them through a regular perinatal center.
How to avoid gestational diabetes? nine0003
Most pregnant women do not develop gestational diabetes, but some women have an increased risk of developing it. Information about risk factors and who gets the condition can be found here.
If certain risk factors apply to you and you would like to be as careful as possible, there are some rules to follow. In particular, avoid excessive weight gain, eat healthy foods, and exercise regularly. One method of controlling blood sugar that can help reduce the risk of gestational diabetes is nutraceutical therapy, which you can read more about here. nine0007
What is the treatment for gestational diabetes?
If your midwife's glucose tolerance test shows you have gestational diabetes, the first step of treatment is to give you advice to change your eating habits and increase your physical activity. This helps to normalize blood sugar levels.
This helps to normalize blood sugar levels.
In general, the general recommendations are:
- Reduce portions and eat more often, evenly spreading meals throughout the day. nine0032
- Food should be rich in fiber and vegetables and contain less "fast" carbohydrates.
- Exercise daily, take long walks.
Ask for an opportunity to speak with a nutritionist. If adjusting your diet and physical activity is not enough to lower your blood sugar, you will need anti-diabetic therapy, which in most cases is done with insulin.
Nutraceutical therapy can lower blood sugar levels without insulin treatment. More information about Preload® Balance can be found here. nine0007
What should be done after childbirth?
In most women diagnosed with gestational diabetes, blood sugar returns to normal soon after giving birth. However, there is an increased risk of developing type 2 diabetes later in life. To reduce this risk, you should avoid excessive weight gain by focusing on a healthy diet and physical activity. Preload® Balance can also be taken post-pregnancy to help you feel full faster, replenish your energy stores regularly, and reduce sugar cravings. nine0007
Preload® Balance can also be taken post-pregnancy to help you feel full faster, replenish your energy stores regularly, and reduce sugar cravings. nine0007
Past research
The Indevex network currently includes a group of experts on nutraceutical therapy during pregnancy and GDM, focusing on collecting information from their own and other research, as well as participating in public debates on women's health and children.
Preload® Balance
The Preload® Balance method is based on the principles of nutraceutical therapy. This treatment contributes to the stabilization of blood sugar in a natural way. This method is the basis of our first product, which contains a combination of natural nutrients derived from pea proteins, egg and milk, apples, rose hips and sugar beet fiber. nine0007
Our product is called Preload® Balance. The drink should be taken 30 minutes before meals (breakfast, lunch and dinner) - it will help you feel full faster and reduce cravings for sweets.