Ginger and breast feeding
Ginger - Drugs and Lactation Database (LactMed®)
Last Revision: April 18, 2022.
Estimated reading time: 6 minutes
Drug Levels and Effects
Summary of Use during Lactation
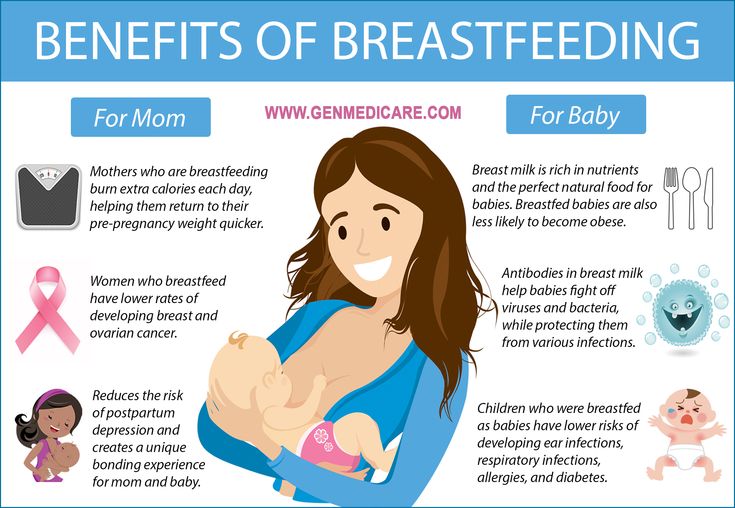
Ginger (Zingiber officinale) root contains the pungent principles or gingerols that are considered to be responsible for its pharmacological activity. Ginger is commonly used for nausea and motion sickness. It has no specific lactation-related uses in Western medicine, but is reportedly used as a galactogogue in Turkey and some parts of Asia.[1,2] Ginger is reportedly used as part of a topical herbal mixture to shorten the time to full lactation and or alone or as part of a topical herbal mixture used for breast engorgement.[3-5] A systemic review of 5 studies on ginger as a galactogogue alone or in combinations with other herbals found weak evidence that ginger may increase milk supply in mothers who had a natural delivery, but not in mothers who had a cesarean section. [6] Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[7,8] Very limited data exist on the safety and efficacy of ginger in nursing mothers or infants. However, ginger has a long history of use as a food and medicine and is "generally recognized as safe" (GRAS) as a food flavoring by the U.S. Food and Drug Administration, including during lactation.[9] When used as a medicinal, ginger is generally well tolerated in adults, but mild side effects such as bad taste, heartburn, abdominal discomfort, weight gain, headache, dry mouth and nausea are reported occasionally.
Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to prove the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does not certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information about dietary supplements is available elsewhere on the LactMed Web site.
A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does not certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information about dietary supplements is available elsewhere on the LactMed Web site.
Drug Levels
Maternal Levels. Relevant published information was not found as of the revision date.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
A woman was treated with a number of Ayruvedic treatments for rheumatoid arthritis postpartum. One of the products used was ginger 250 mg orally twice daily for 3 months. She reportedly breastfed her infant (extent not stated) throughout treatment and the infant had normal growth and development.[10]
In a study of exclusively nursing mothers receiving fenugreek seed 200 mg, turmeric 100 mg and ginger 120 mg (Fenucaps; Herbal Acharn's Home Co. Ltd., Thailand) 3 times daily for 4 weeks, no adverse events were reported in their infants, although the method used to determine this finding were not reported.[11]
Ltd., Thailand) 3 times daily for 4 weeks, no adverse events were reported in their infants, although the method used to determine this finding were not reported.[11]
Effects on Lactation and Breastmilk
A study in Japan compared the use of a mixture of 13 herbs, including ginger, to ergonovine for their effects on lactation and serum prolactin in postpartum women. The herbal mixture, called Xiong-gui-tiao-xue-yin, was given in a randomized fashion to 41 women in a dose of 2 grams of a dried aqueous extract 3 times daily. A comparable group of 41 women were randomized to receive methylergonovine 0.375 mg daily. Therapy was started on the day of delivery, but the duration of therapy was not specified. Plasma oxytocin and prolactin were measured on days 1 and 6; milk volumes were measured daily, although the method of measuring milk volume was not specified. Serum prolactin was higher on days 1 and 6 in the women who received the herbals; plasma oxytocin was lower on day 1 in the women who received the herbal, but not different on day 6. Milk volumes were greater on days 4, 5, and 6 in women who received the herbal mixture.[12] This study has serious flaws that make its interpretation impossible. First, milk volume measurement is subject to considerable variability depending on the measurement method used, but the method was not specified. Second, methylergonovine has caused decreases in serum prolactin and milk production in some studies.[13,14] Because of the lack of a placebo group, the differences found could be a negative effect of methylergonovine rather than a positive effect of the herbal preparation. Because this study used a multi-ingredient combination products in which ginger was only one component, the results might be different from studies in which ginger was used alone.
Milk volumes were greater on days 4, 5, and 6 in women who received the herbal mixture.[12] This study has serious flaws that make its interpretation impossible. First, milk volume measurement is subject to considerable variability depending on the measurement method used, but the method was not specified. Second, methylergonovine has caused decreases in serum prolactin and milk production in some studies.[13,14] Because of the lack of a placebo group, the differences found could be a negative effect of methylergonovine rather than a positive effect of the herbal preparation. Because this study used a multi-ingredient combination products in which ginger was only one component, the results might be different from studies in which ginger was used alone.
Studies of Thai herbal compresses containing ginger, turmeric and camphor have evaluated the effect of application of the compresses to the breasts on lactation. The studies showed that the compresses shortened the time to lactation postpartum compared to routine clinical care for enhancing lactation. [3]
[3]
A randomized, double-blind study in Thailand compared the milk output of mothers taking either dried ginger 500 mg or placebo twice daily starting within 2 hours after delivery. On day 3, mothers receiving ginger produced a statistically significantly greater volume of milk than those receiving placebo, 191 mL per 24 hours compared to 135 mL per 24 hours. On day 7 postpartum, the ginger group produced an average of 80 mL/hour of milk compared to 112 mL/hour in the placebo group, although the difference was not statistically significant. No significant difference in serum prolactin was found between the two groups on day 3 postpartum.[15]
A randomized trial in women with breast engorgement compared warm compresses to warm compresses containing a mixture of dried herbs, including ginger, lemon grass, Stapf leaves and leaf sheaths, Acacia concinna leaves, tamarind leaves, Citrus hystrix (kaffir lime) peels, Blumea balsamifera (sambong) leaves, salt and camphor. Both treatments relived the pain of engorgement, but women who received the compress with herbs (n = 250) had greater pain relief than those who received the warm compress alone. Because of the possible color and odor differences between treatments, the study cannot be considered to be blinded.[4]
Both treatments relived the pain of engorgement, but women who received the compress with herbs (n = 250) had greater pain relief than those who received the warm compress alone. Because of the possible color and odor differences between treatments, the study cannot be considered to be blinded.[4]
Fifty women in Thailand who were 1 month postpartum and exclusively breastfeeding were randomized to receive either a placebo or capsules containing fenugreek seed 200 mg, turmeric 100 mg and ginger 120 mg (Fenucaps; Herbal Acharn's Home Co. Ltd., Thailand) 3 times daily for 4 weeks. Participants pumped milk on 2 days at 0, 2 and 4 weeks of the study. The average milk volumes increased by 49% at 2 weeks and 103% at 4 weeks among participants receiving the active product. The macronutrient composition of the milk did not change in either group over the 4-week period. Growth of infants was not reported.[11]
A randomized, double-bind study of 70 women who delivered by cesarean section in a hospital in Thailand compared 35 who took 5 grams of instant ginger powder in water to 35 who took a placebo with ginger scent, but no ginger.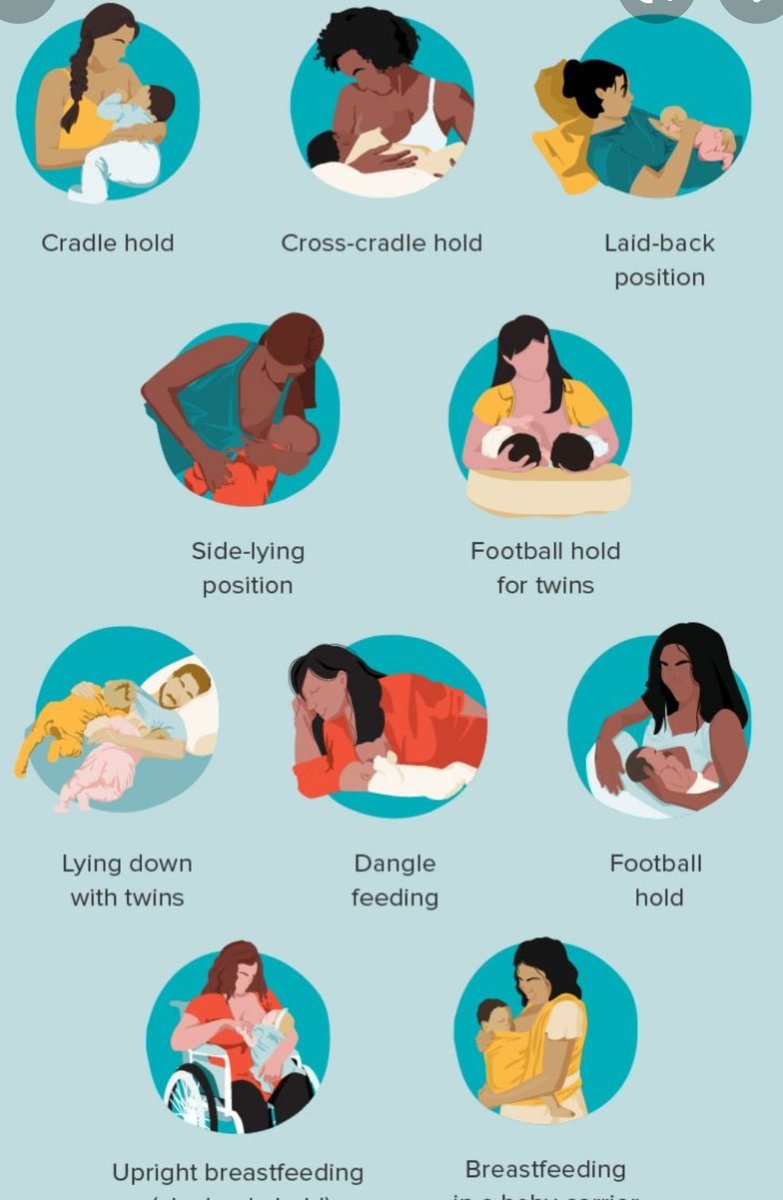 The products were taken every 12 hours up to 72 hours postpartum, starting at 24 hours postpartum. Breastmilk volumes were measured by test weighing of their infants. Total milk volume between 48 and 72 hours postpartum were compared. The median total breast milk volumes during this time were 80 mL in the ginger group and 100 mL in the placebo group. The difference was not statistically significant.[16]
The products were taken every 12 hours up to 72 hours postpartum, starting at 24 hours postpartum. Breastmilk volumes were measured by test weighing of their infants. Total milk volume between 48 and 72 hours postpartum were compared. The median total breast milk volumes during this time were 80 mL in the ginger group and 100 mL in the placebo group. The difference was not statistically significant.[16]
A randomized study compared nursing mothers with breast engorgement who received either a hot compress (n = 38) or hot ginger compress (n = 38) three times daily for 2 days. The women who received the ginger compresses had a greater decrease in breast pain than those who received the hot compresses.[5]
In a survey of nursing mothers in Australia, 52 mothers were taking ginger as a galactogogue. On average, mothers rated ginger as “slightly effective” on a Likert scale. Six percent of mothers taking ginger reported experiencing adverse reactions, such as weight gain, headache, dry mouth and nausea. [17]
[17]
References
- 1.
Lamxay V, de Boer HJ, Bjork L. Traditions and plant use during pregnancy, childbirth and postpartum recovery by the Kry ethnic group in Lao PDR. J Ethnobiol Ethnomed. 2011;7:14. [PMC free article: PMC3120637] [PubMed: 21569234]
- 2.
Kaygusuz M, Gümüştakım RŞ, Kuş C, et al. TCM use in pregnant women and nursing mothers: A study from Turkey. Complement Ther Clin Pract. 2021;42:101300. [PubMed: 33412511]
- 3.
Dhippayom T, Kongkaew C, Chaiyakunapruk N, et al. Clinical effects of Thai herbal compress: A systematic review and meta-analysis. Evid Based Complement Alternat Med. 2015;2015:942378. [PMC free article: PMC4377500] [PubMed: 25861373]
- 4.
Ketsuwan S, Baiya N, Paritakul P, et al. Effect of herbal compresses for maternal breast engorgement at postpartum: A randomized controlled trial. Breastfeed Med. 2018;13:361–5. [PubMed: 29688768]
- 5.
Monazzami M.
 , Yousefzadeh S., Rakhshandeh H., et al. Comparing the effects of hot compress and hot ginger compress on pain associated with breast engorgement. Nursing and Midwifery Studies. 2021;10:73–8. [CrossRef]
, Yousefzadeh S., Rakhshandeh H., et al. Comparing the effects of hot compress and hot ginger compress on pain associated with breast engorgement. Nursing and Midwifery Studies. 2021;10:73–8. [CrossRef]- 6.
Dilokthornsakul W, Rinta A, Dhippayom T, et al. Efficacy and safety of ginger regarding human milk volume and related clinical outcomes: A systematic review of randomized controlled trials. Complement Med Res. 2021;29:67–73. [PubMed: 33789272]
- 7.
Brodribb W. ABM Clinical Protocol #9. Use of galactogogues in initiating or augmenting maternal milk production, second revision 2018. Breastfeed Med. 2018;13:307–14. [PubMed: 29902083]
- 8.
Breastfeeding challenges: ACOG Committee Opinion, Number 820. Obstet Gynecol. 2021;137:e42–e53. [PubMed: 33481531]
- 9.
O'Hara M, Kiefer D, Farrell K, et al. A review of 12 commonly used medicinal herbs. Arch Fam Med. 1998;7:523–36. [PubMed: 9821826]
- 10.

Deshpande SV, Deshpande VS, Potdar SS. Effect of panchakarma and Ayurvedic treatment in postpartum rheumatoid arthritis (amavata): A case study. J Ayurveda Integr Med. 2017;8:42–4. [PMC free article: PMC5377475] [PubMed: 28302414]
- 11.
Bumrungpert A, Somboonpanyakul P, Pavadhgul P, et al. Effects of fenugreek, ginger, and turmeric supplementation on human milk volume and nutrient content in breastfeeding mothers: A randomized double-blind controlled trial. Breastfeed Med. 2018;13:645–50. [PubMed: 30411974]
- 12.
Ushiroyama T, Sakuma K, Souen H, et al. Xiong-gui-tiao-xue-yin (Kyuki-chouketsu-in), a traditional herbal medicine, stimulates lactation with increase in secretion of prolactin but not oxytocin in the postpartum period. Am J Chin Med. 2007;35:195–202. [PubMed: 17436360]
- 13.
Peters F, Lummerich M, Breckwoldt M. Inhibition of prolactin and lactation by methylergometrine hydrogenmaleate. Acta Endocrinol (Copenh).
 1979;91:213–6. [PubMed: 463447]
1979;91:213–6. [PubMed: 463447]- 14.
Arabin B, Ruttgers H, Kubli F. Geburtshilfe Frauenheilkd. 1986;46:215–20. [Effects of routine administration of methylergometrine during puerperium on involution, maternal morbidity and lactation] [PubMed: 3519353]
- 15.
Paritakul P, Ruangrongmorakot K, Laosooksathit W, et al. The effect of ginger on breast milk volume in the early postpartum period: A randomized, double-blind controlled trial. Breastfeed Med. 2016;11:361–5. [PubMed: 27505611]
- 16.
Sassanarakkit S, Kaiwong S, Chittacharoen A. A study on instant ginger drink effect in enhancing postpartum breastfeeding in immediate post cesarean delivery. J Med Assoc Thai. 2019;102:259–63. http://www
.jmatonline.com - 17.
McBride GM, Stevenson R, Zizzo G, et al. Use and experiences of galactagogues while breastfeeding among Australian women. PLoS One. 2021;16:e0254049. [PMC free article: PMC8248610] [PubMed: 34197558]
Substance Identification
Substance Name
Ginger
Scientific Name
Zingiber officinale
Drug Class
Breast Feeding
Lactation
Milk, Human
Complementary Therapies
Phytotherapy
Plants, Medicinal
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment.
 You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
The Effect of Ginger on Breast Milk Volume in the Early Postpartum Period: A Randomized, Double-Blind Controlled Trial
Randomized Controlled Trial
. 2016 Sep;11:361-5.
doi: 10.1089/bfm.2016.0073. Epub 2016 Aug 9.
Panwara Paritakul 1 , Kasem Ruangrongmorakot 1 , Wipada Laosooksathit 1 , Maysita Suksamarnwong 1 , Pawin Puapornpong 1
Affiliations
Affiliation
- 1 Department of Obstetrics and Gynecology, Faculty of Medicine, Srinakharinwirot University , Bangkok, Thailand .
- PMID: 27505611
- DOI: 10.1089/bfm.2016.0073
Randomized Controlled Trial
Panwara Paritakul et al. Breastfeed Med. 2016 Sep.
. 2016 Sep;11:361-5.
doi: 10.1089/bfm.2016.0073. Epub 2016 Aug 9.
Authors
Panwara Paritakul 1 , Kasem Ruangrongmorakot 1 , Wipada Laosooksathit 1 , Maysita Suksamarnwong 1 , Pawin Puapornpong 1
Affiliation
- 1 Department of Obstetrics and Gynecology, Faculty of Medicine, Srinakharinwirot University , Bangkok, Thailand .
- PMID: 27505611
- DOI: 10.1089/bfm.2016.0073
Abstract
Background: In Thailand, ginger is a popular natural galactagogue among breastfeeding women. However, there has never been evidence to support the effectiveness of ginger in increasing the breast milk volume.
Objectives: To compare breast milk volume on the third and seventh day postpartum between lactating mothers who receive 500 mg dried ginger capsules twice daily with those receiving placebo.
Materials and methods: A randomized, double-blind controlled trial was conducted. Women who deliver a term baby were randomly assigned to receive dried ginger or placebo for 7 days postpartum. Breast milk volume was measured on third day postpartum using test weight method for a period of 24 hours and on seventh day postpartum using 1 hour milk production. We also compared the third day serum prolactin level between the two groups.
Women who deliver a term baby were randomly assigned to receive dried ginger or placebo for 7 days postpartum. Breast milk volume was measured on third day postpartum using test weight method for a period of 24 hours and on seventh day postpartum using 1 hour milk production. We also compared the third day serum prolactin level between the two groups.
Results: Data from 63 women were available for analysis, 30 from the ginger group and 33 from the placebo group. The two groups were similar regarding baseline characteristics. Women in the ginger group have higher milk volume than the placebo group (191.0 ± 71.2 mL/day versus 135.0 ± 61.5 mL/day, p < 0.01). However, the seventh day milk volume in the ginger group does not differ from the placebo group (80.0 ± 58.5 mL versus 112.1 ± 91.6 mL, p = 0.24). The mean serum prolactin levels were similar in both groups (321.5 ± 131.8 ng/L in the ginger group, and 331. 4 ± 100.7 ng/L in the placebo group, p = 0.74). No side effect was reported in this study.
4 ± 100.7 ng/L in the placebo group, p = 0.74). No side effect was reported in this study.
Conclusion: Ginger is a promising natural galactagogue to improve breast milk volume in the immediate postpartum period without any notable side effect.
Similar articles
-
The effect of galactagogue herbal tea on breast milk production and short-term catch-up of birth weight in the first week of life.
Turkyılmaz C, Onal E, Hirfanoglu IM, Turan O, Koç E, Ergenekon E, Atalay Y. Turkyılmaz C, et al. J Altern Complement Med. 2011 Feb;17(2):139-42. doi: 10.1089/acm.2010.0090. Epub 2011 Jan 24. J Altern Complement Med. 2011. PMID: 21261516 Clinical Trial.
-
Effect of a galactagogue herbal tea on breast milk production and prolactin secretion by mothers of preterm babies.

Özalkaya E, Aslandoğdu Z, Özkoral A, Topcuoğlu S, Karatekin G. Özalkaya E, et al. Niger J Clin Pract. 2018 Jan;21(1):38-42. doi: 10.4103/1119-3077.224788. Niger J Clin Pract. 2018. PMID: 29411721 Clinical Trial.
-
Efficacy of a galactogogue containing silymarin-phosphatidylserine and galega in mothers of preterm infants: a randomized controlled trial.
Zecca E, Zuppa AA, D'Antuono A, Tiberi E, Giordano L, Pianini T, Romagnoli C. Zecca E, et al. Eur J Clin Nutr. 2016 Oct;70(10):1151-1154. doi: 10.1038/ejcn.2016.86. Epub 2016 Jun 1. Eur J Clin Nutr. 2016. PMID: 27245206 Clinical Trial.
-
Supporting Mothers of Very Preterm Infants and Breast Milk Production: A Review of the Role of Galactogogues.
Asztalos EV. Asztalos EV. Nutrients. 2018 May 12;10(5):600. doi: 10.3390/nu10050600. Nutrients. 2018. PMID: 29757199 Free PMC article. Review.
-
Safety and efficacy of galactogogues: substances that induce, maintain and increase breast milk production.
Zuppa AA, Sindico P, Orchi C, Carducci C, Cardiello V, Romagnoli C. Zuppa AA, et al. J Pharm Pharm Sci. 2010;13(2):162-74. doi: 10.18433/j3ds3r. J Pharm Pharm Sci. 2010. PMID: 20816003 Review.
See all similar articles
Cited by
-
The effect of Moringa oleifera capsule in increasing breast milk volume in early postpartum patients: A double-blind, randomized controlled trial.
Fungtammasan S, Phupong V.
 Fungtammasan S, et al. Eur J Obstet Gynecol Reprod Biol X. 2022 Nov 17;16:100171. doi: 10.1016/j.eurox.2022.100171. eCollection 2022 Dec. Eur J Obstet Gynecol Reprod Biol X. 2022. PMID: 36440058 Free PMC article.
Fungtammasan S, et al. Eur J Obstet Gynecol Reprod Biol X. 2022 Nov 17;16:100171. doi: 10.1016/j.eurox.2022.100171. eCollection 2022 Dec. Eur J Obstet Gynecol Reprod Biol X. 2022. PMID: 36440058 Free PMC article. -
Use of Galactagogues in a Multi-Ethnic Community in Southeast Asia: A Descriptive Study.
Tan ML, Foong SC, Foong WC, Ho JJ. Tan ML, et al. Int J Womens Health. 2022 Sep 22;14:1395-1404. doi: 10.2147/IJWH.S366288. eCollection 2022. Int J Womens Health. 2022. PMID: 36172202 Free PMC article.
-
Infant stimulation reduces weight loss and increases breastfeeding: a randomized controlled trial.
Gualdrón LMV, Villalobos MMD, Camargo NMB. Gualdrón LMV, et al. Invest Educ Enferm. 2022 Mar;40(1):e05.
 doi: 10.17533/udea.iee.v40n1e05. Invest Educ Enferm. 2022. PMID: 35485618 Free PMC article.
doi: 10.17533/udea.iee.v40n1e05. Invest Educ Enferm. 2022. PMID: 35485618 Free PMC article. -
Efficacy of Wang Nam Yen herbal tea on human milk production: A randomized controlled trial.
Saejueng K, Nopsopon T, Wuttikonsammakit P, Khumbun W, Pongpirul K. Saejueng K, et al. PLoS One. 2022 Jan 31;17(1):e0247637. doi: 10.1371/journal.pone.0247637. eCollection 2022. PLoS One. 2022. PMID: 35100251 Free PMC article. Clinical Trial.
-
Herbal Medicines-Are They Effective and Safe during Pregnancy?
Sarecka-Hujar B, Szulc-Musioł B. Sarecka-Hujar B, et al. Pharmaceutics. 2022 Jan 12;14(1):171. doi: 10.3390/pharmaceutics14010171. Pharmaceutics. 2022. PMID: 35057067 Free PMC article. Review.
See all "Cited by" articles
Publication types
MeSH terms
Substances
is it possible for breastfeeding: benefits and harm, reviews
complain
Updated
Content:
You can or not
What ginger to choose
9000
video
Ginger root is useful, but not everyone can use it. Nursing mothers, knowing that the food eaten comes with breast milk to the baby, are interested in: is it possible to ginger while breastfeeding? Or is it still worth abandoning tonic ginger tea and not adding ginger to pastries and meat? In most cases, in moderate doses during lactation, ginger root is allowed. But, before adding the plant to tea or other dishes, you need to consult a doctor. In some conditions, the spice can be harmful.
Nursing mothers, knowing that the food eaten comes with breast milk to the baby, are interested in: is it possible to ginger while breastfeeding? Or is it still worth abandoning tonic ginger tea and not adding ginger to pastries and meat? In most cases, in moderate doses during lactation, ginger root is allowed. But, before adding the plant to tea or other dishes, you need to consult a doctor. In some conditions, the spice can be harmful.
Moderate doses of ginger can be used while breastfeeding
May or may not
Breastfeeding mother can use ginger root during lactation. The plant will help:
- improve the production of breast milk;
- prevent lactostasis;
- increase vitality and get rid of chronic fatigue, which often occurs in a woman when caring for a baby;
- increase resistance to stress;
- strengthen immunity;
- to reduce the weight gained during pregnancy faster.
Ginger also has a positive effect on the baby's body. Studying the reviews of breastfeeding women who drank ginger tea or added spice to food, we can conclude that these women have children who get sick less, sleep better and suffer less from allergies.
Studying the reviews of breastfeeding women who drank ginger tea or added spice to food, we can conclude that these women have children who get sick less, sleep better and suffer less from allergies.
Ginger is good for breastfeeding, but not everyone is allowed to use it. The root is contraindicated in the following cases:
- Diseases of the stomach. The spice irritates the mucous membrane, causing exacerbation of gastritis or peptic ulcer.
- Hemorrhoids. Hemorrhoids often first appear during pregnancy, and childbirth provokes an exacerbation of the pathology. The root can cause hemorrhoids to bleed.
- Early postpartum period. In the first month after the birth of a baby, a woman develops lochia, the placenta heals, the uterus shrinks to normal size. Ginger thins the blood, so taking the root immediately after childbirth can cause uterine bleeding.
A relative contraindication is that the woman has not tried the product before. In this case, she does not know how it will affect the body. To exclude possible adverse reactions, it is better to postpone the test of the spice until the end of breastfeeding.
To exclude possible adverse reactions, it is better to postpone the test of the spice until the end of breastfeeding.
Which ginger to choose
The store offers fresh and pickled ginger, as well as dry ginger seasoning. During lactation, only dried and fresh spices are allowed.
Pickled ginger is banned because pickling adds preservatives to keep the product longer. The use of the root cooked in the marinade is prohibited due to the fact that preservatives enter breast milk and can adversely affect the health of the baby.
If the woman is on medication
Not all women are completely healthy. Some are forced to take medication for life to prevent the progression of the disease. With the joint intake of this spice and some medicines, you can harm the body. Incompatible with ginger:
- Sugar reducing products. You can not use the plant both with insulin injections and when taking antihyperglycemic tablets.

- Antiarrhythmic and cardiac stimulants. The root will enhance the effect of medicines.
- Hypotensive.
- Blood thinners. Ginger affects blood clotting and, when taken together with anticoagulants, can cause internal bleeding.
If medications are taken, a doctor should be consulted about compatibility of medications with ginger spice. In most cases, it is allowed to drink medicines and consume ginger at the same time.
Ginger is good for breastfeeding. The root will improve lactation, help get rid of postpartum depression and increase immunity. But you need to observe the measure and remember that the plant has contraindications and is incompatible with certain drugs. In order not to harm yourself and the baby, you should consult a doctor before using the spice.
Video
Read more: figs while breastfeeding
HeadingNutrition of a nursing mother
Cauliflower during breastfeeding
Is it possible for a nursing mother to drink milk
Media news2
Comments
' + '
' +tooltips[tooltip][0] + '
' +'' +tooltips[tooltip][1] +'' + '
' + 'Discover and participate
Clubs on Baby. ru are a storehouse of useful information
Teacher and student: how to stay “on the same wavelength”? Burn scars in children: how to treat? ?Choose the path of a superheroYour career in the media industryAthletes break recordsTalent can become a professionHistory is the memory of the most importantWho and how manages the country's moneyDo you like to travel?Why is Russia called a treasuryUrbanism of the city takes! Bioengineer – profession of the future studies more precisely All about food technology Ecology: concerns everyone Interested in space Passionate about technology All about prospects in medicine Promising professions here The real riches of Russia The key to the cultural code of Russia You and Russia are tomorrow. Assess the OpportunitiesHow a single mom can get back to work
Can a breastfeeding mother eat ginger?
Valeria Leshchenko
Ginger for toxicosis is an excellent remedy for nausea, but can this product be used while breastfeeding?
Ginger is a spicy spice that can be added to tea, all kinds of pastries, salads, sauces for meat and fish. Ginger root relieves fatigue, improves immunity, warms (which is important in the winter months), improves digestion and calms the nervous system. Despite the useful properties, the product has a number of contraindications that will be relevant not only for those who are breastfeeding.
How to use ginger while breastfeeding?
If you have never used ginger, then the first acquaintance should not be made during lactation. The root has a very rich taste, so it can cause allergies in both mother and child.
- Ginger during breastfeeding can increase lactation, but it is recommended to eat for mom when the baby is 2 months old. It is best to do this before lunch. Serving should be no more than 3 g! After introducing a new product into the diet, observe the reaction of the child's body: if there are rashes, if there is reddening of the cheeks or if the stool is thinned. If the child's body normally accepted ginger, you can increase the amount every day.
- Ginger tea is delicious, but the drink has tonic properties, so it will not benefit the mother of a child with hyperexcitability of the central nervous system.
- Ginger thins the blood and irritates the mucous membranes of the gastrointestinal tract, so it is contraindicated for stomach ulcers, gastritis, and if there is bleeding (for example, hemorrhoids after childbirth).
- Ginger during breastfeeding can be harmful to a mother with hypertension. The fact is that the root can affect the increase in pressure.
Ginger to improve lactation
If you do not have the above problems with the use of ginger, then this spice is a real find for those who need to increase lactation. Experts recommend the following recipe to increase the amount of breast milk:
- Take ginger root, wash, peel and grate.
- Pour 1 tablespoon of ginger into 350 ml of boiling water and let it steep for 10 minutes.
- It is necessary to consume such a drink 30 minutes before feeding, 150 ml each.
NO! This recipe for breastfeeding should be used only after consulting a doctor! Do not self-medicate!
Ginger can also be added to poultry broths and vegetable stews when breastfeeding to add a tangy flavor to dishes.
And remember, what is useful is what is in moderation, so do not abuse this spice, even if there is a result - improved lactation.
There is another useful product for breastfeeding mothers. Pumpkin when breastfeeding effectively fights fatigue.
When should you not use ginger?
- Ginger is a spicy food product that perfectly complements the taste of dishes, but as an independent product it should not be consumed, especially if a new mother has stomach problems (ulcer, gastritis, etc.).
- Ginger has a choleretic effect, so it should be eaten with caution for those who have liver problems and gallstones.
- If a woman has never consumed ginger, then you should not try it during lactation, as this product can cause allergies.
- With increased acidity of the gastrointestinal tract, ginger is not recommended, as it can cause heartburn.
- If the baby is diagnosed with atopic dermatitis, it is necessary to consult with a pediatrician whether it is possible for a nursing mother to consume ginger and in what quantity.