Bladder leaking after baby
Bladder weakness after birth | Pregnancy Birth and Baby
Bladder weakness after birth | Pregnancy Birth and Baby beginning of content8-minute read
Listen
What is urinary incontinence?
Urinary incontinence describes any accidental or involuntary loss of urine from the bladder. Incontinence can range in severity from a small leak to a complete loss of bladder control. Thankfully, there are ways to improve and even cure urinary incontinence. Seeking help early is recommended.
What causes urinary incontinence?
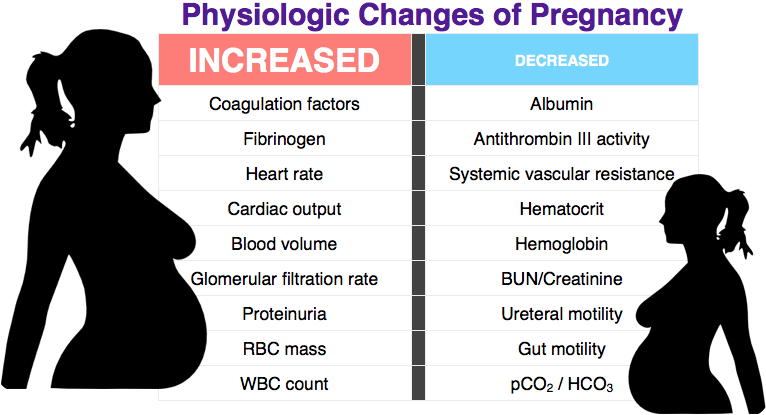
When you are pregnant, you produce hormones that stretch the muscles and tissues that support the bladder, the bowel and the uterus. This group of muscles and tissues is called the pelvic floor.
When your baby moves down through your vagina to be born, your pelvic floor stretches and it remains stretched for some time.
The combination of hormones and stretched muscles means the muscles that control your bladder are weakened. This can lead to an accidental leak of urine.
Diagram showing where the pelvic floor muscle is located in the female body.How common is urinary incontinence?
Leaking urine (called ‘urinary incontinence’) after childbirth is very common. One in 3 women who have had a baby may experience leakage at some point.
Some new mother may leak urine when they laugh, sneezes, coughs or exercises. This is known as stress incontinence.
You are more likely to develop stress incontinence after birth if you:
- have bladder or bowel problems before pregnancy – they are likely to get worse after the birth
- bladder problems during the pregnancy
- are having your first baby
- are having a large baby
- have a long labour, especially a long second stage of labour
- have a difficult delivery, such as needing stitches, tearing, or needing a vacuum cup or forceps during the delivery
Women who have a caesarean can also develop bladder problems. Having a caesarean can reduce the risk of severe incontinence from 10% to 5% for the first baby, but after the third caesarean women are just as likely to develop bladder problems as women who give birth vaginally.
Having a caesarean can reduce the risk of severe incontinence from 10% to 5% for the first baby, but after the third caesarean women are just as likely to develop bladder problems as women who give birth vaginally.
When should I see my doctor?
Most women who leak urine after childbirth find that it goes away in the first few weeks, as the stretched muscles and tissues recover.
However, for some women it can take months while others find their pelvic floor never recovers fully.
If you are experiencing urine leakage, you can talk to your, doctor, maternal and child health nurse, continence nurse or a women’s physiotherapist. Remember dealing with it early can reduce the risk of it becoming a life-long problem.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is urinary incontinence treated?
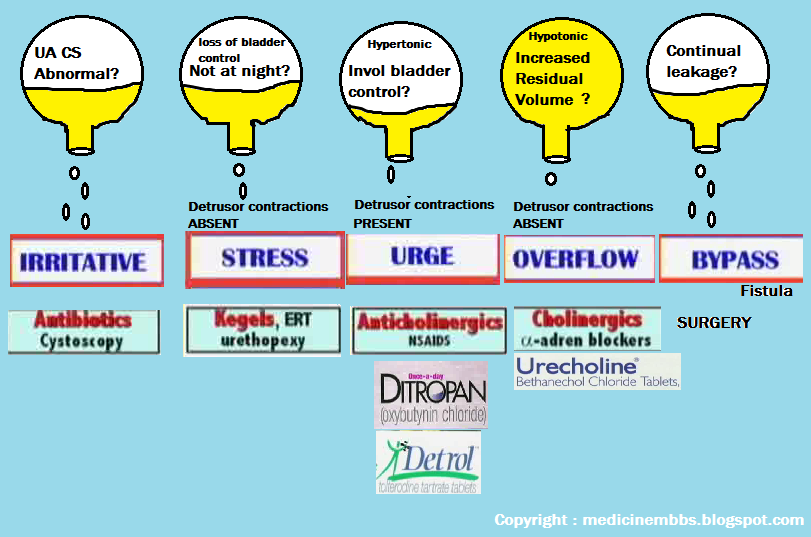
The treatment will depend on what kind of incontinence you have and how severe it is.
Straight after birth, you will need to give the pelvic floor time to recover. Ice the perineal area for the first few days and have plenty of rest.
Then you can start with gentle pelvic floor contractions while you are lying down. Hold for 3 seconds, rest for 15 seconds, and repeat 3 times. Try to build up longer holds when you can. Doing these exercises may help prevent longer term bladder problems.
Simple changes to your lifestyle may also help, such as losing your pregnancy weight, eating more fibre, drinking more water and lifting less.
If your urinary incontinence doesn’t get better, talk to your doctor. They may refer you to another specialist. Longer term treatments for bladder weakness are exercises, medication or surgery.
Pelvic floor exercises
The muscles around the bladder, bowel and uterus can be exercised, toned and trained like any other muscles in the body. Doing this before, during and after pregnancy will help prevent urinary incontinence during pregnancy and after the birth of your baby. They’re easy to do, in any place and at any time.
They’re easy to do, in any place and at any time.
Here’s an example:
- Breathe in and breathe out.
- Pull the pelvic floor muscles up and in as though you are trying to stop yourself from urinating.
- Hold the squeeze for 10 seconds while breathing normally.
- Relax and repeat in 10 seconds.
- Repeat the squeeze and release 10 times.
- Do this exercise 3 times a day.
The Continence Foundation of Australia have produced this video on how to do pelvic floor exercises:
You can also find out more about pelvic floor strength on the Jean Hailes website.
Bladder training
When you’re pregnant, your growing baby puts pressure on your bladder. This causes the bladder to feel full more quickly than usual, meaning you need more frequent trips to the toilet.
After your baby’s birth, it is a good idea to retrain your bladder. You can do this by trying to hold off from going to the toilet, until your bladder is full.
Medication
If you have urge incontinence, or an overactive bladder, medication can help to relax the bladder muscles.
Surgery
If all else fails, surgery might be an option for some women. Talk to your doctor about what's best for you.
Emotional wellbeing
Urinary incontinence can affect not only your physical health but also your emotional health and general wellbeing. For some women this complication may also be linked to an experience of birth trauma. If you find you are experiencing low mood or are concerned, you are not alone. There are service available to support you.
Living with urinary incontinence
Urinary incontinence can, unfortunately, become a long-term problem for some women. Here are some tips that may help if you are living with it:
- use incontinence pads, which are made for urine leakage, rather than sanitary pads
- take a change of underwear or set of clothes when you go out
- know where toilets are located so you can find them quickly (there are smartphone apps to help you do this)
- cross your legs when sneezing or laughing
- modify your exercise routine to avoid high impact exercises such as jumping
What can I do to prevent bladder problems after birth?
There are some simple steps you can take during pregnancy to help prevent incontinence.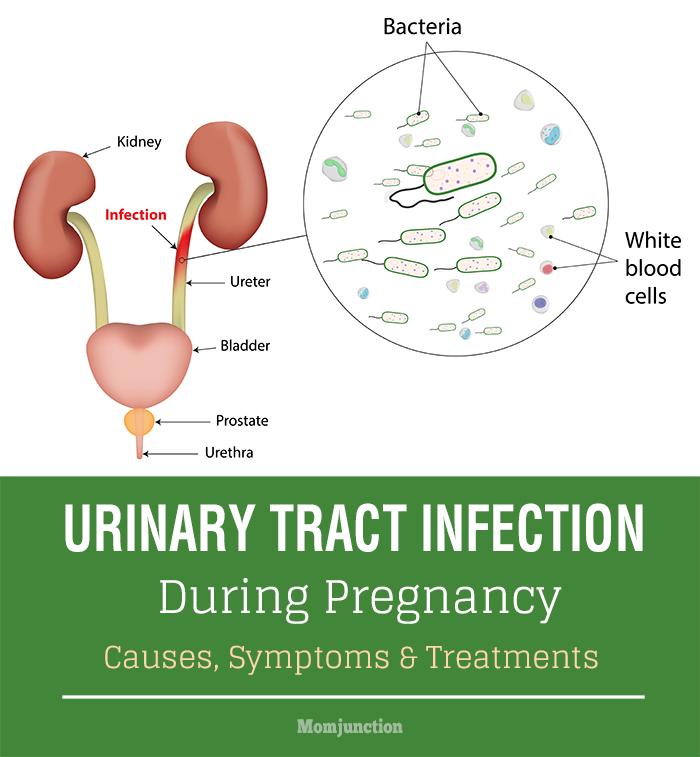
- Drink 6 to 8 cups of fluid a day, unless your doctor tells you otherwise. Avoid drinks containing sugar or caffeine, as these can irritate the bladder.
- Eat a high fibre diet with 2 pieces of fruit, 5 serves of vegetables and 5 serves of cereals/bread per day.
- Make sure you have a healthy weight.
- Stop smoking.
- Exercise for at least 30 minutes most days (see below).
- Do regular pelvic floor exercises.
- Go to the toilet when you have the urge to open your bowels (poo).
- Sit properly on the toilet.
- Avoid constipation, as this strains your pelvic floor muscles.
- Don’t go to the toilet ‘just in case’.
- See your doctor straight away if you have a urinary tract infection.
It’s also important to exercise safely while you are pregnant and after the birth to avoid incontinence. Ideal exercises are walking, low impact aerobics, water aerobics, cycling on a stationary bike, swimming, light weight training or pregnancy exercise classes.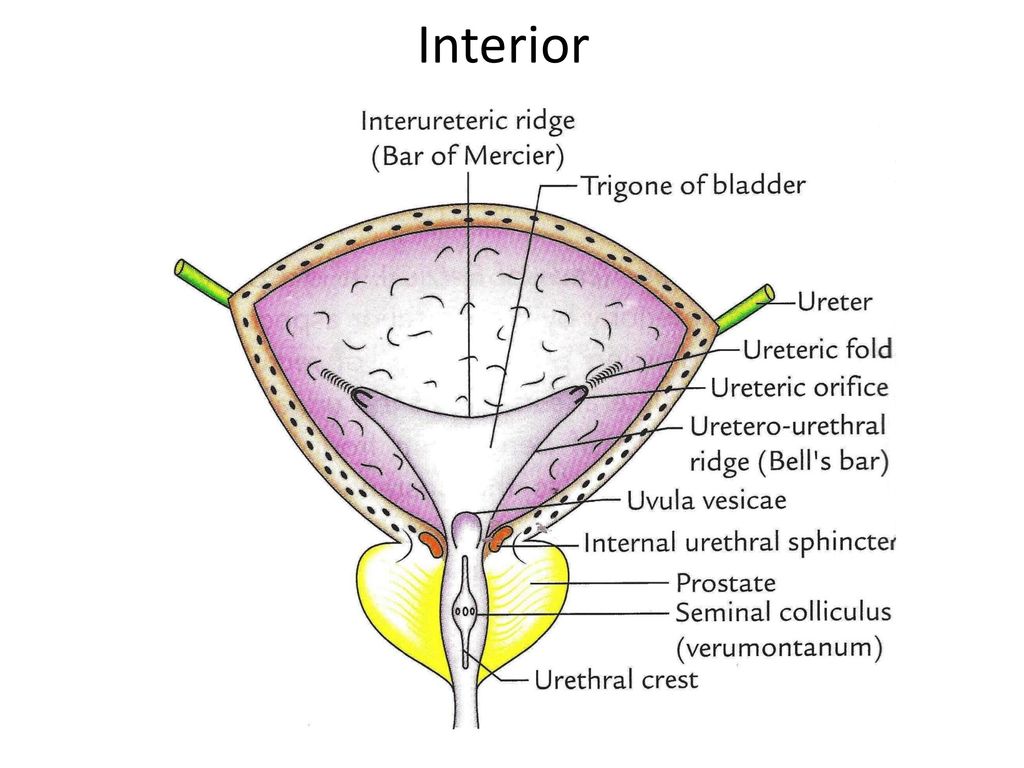 To protect your pelvic floor, avoid:
To protect your pelvic floor, avoid:
- heavy weights
- high impact or jerky movements
- bouncing
- contact sports
- excessive twisting and turning activities
- exercises that require you to hold your breath
- exercises that require sudden changes of direction or intensity
- exercises that make you use one leg more than the other, or lifting your hip while you are on your hands or knees
- exercises that involve standing on one leg for a period of time
- activities involving sudden changes in intensity
- exercises that increase the curve in your lower back
Where can I go for more advice and support?
Speak to your doctor or midwife or call the National Continence Helpline on 1800 33 00 66 for more information and support.
Sources:
Continence Foundation of Australia (Pregnancy and childbirth), The Royal Women's Hospital (Urinary incontinence), Department of Health (One in three women who ever had a baby wet themselves), Jean Hailes for Women's Health (Bladder incontinence), Pelvic Floor First (Exercising during pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Bladder and bowel problems during pregnancy
- Looking after your body after having a baby
- Pelvic floor exercises
- What happens to your body in childbirth
Need more information?
Pelvic Floor Muscle Damage - Birth Trauma
The pelvic floor muscles are a supportive basin of muscle attached to the pelvic bones by connective tissue to support the vagina, uterus, bladder and bowel.
Read more on Australasian Birth Trauma Association website
Pelvic Organ Prolapse (POP) - Birth Trauma
Some women with Pelvic Organ Prolapse do not experience any symptoms. When women do have symptoms they can range from minor changes to completely
Read more on Australasian Birth Trauma Association website
Anatomy of pregnancy and birth - perineum and pelvic floor
The perineum – the skin between the vagina and anus - stretches during childbirth and can sometimes tear. Learn here how to prepare the perineum for the birth.
Learn here how to prepare the perineum for the birth.
Read more on Pregnancy, Birth & Baby website
Pelvic floor exercises
Pelvic floor exercises help to strengthen the muscles of the pelvic floor which come under great strain in pregnancy and childbirth.
Read more on Pregnancy, Birth & Baby website
Pelvic floor - Better Health Channel
Pelvic floor exercises are designed to improve muscle tone and prevent the need for corrective surgery.
Read more on Better Health Channel website
Ever had a baby · Who's at risk · Pelvic Floor First
Pelvic floor muscles take time to get back to their usual state after the birth.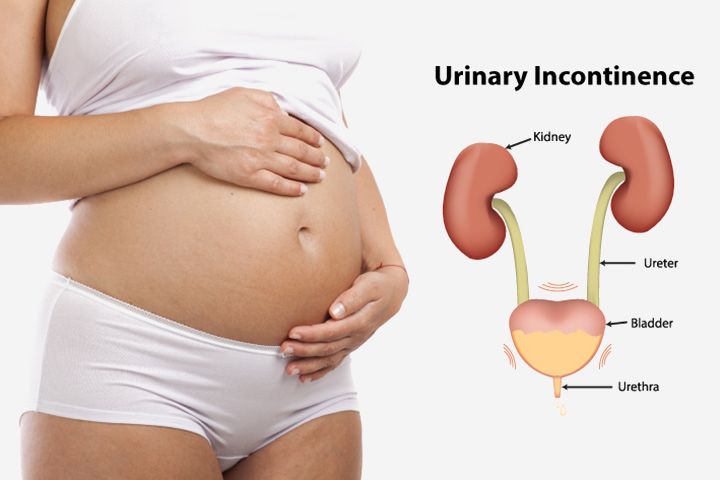
Read more on Continence Foundation of Australia website
Looking after your body after having a baby
Over the last 9 months, your body has had to change to accommodate your growing baby and preparing to give birth.
Read more on Pregnancy, Birth & Baby website
Physiotherapy advice after pregnancy
When you are pregnant, your body changes. Read about simple exercises and healthy habits to help cope with these changes.
Read more on Pregnancy, Birth & Baby website
The pelvic floor and core · The pelvic floor · Pelvic Floor First
The pelvic floor muscles form the base of the group of muscles commonly called the ‘core’.
Read more on Continence Foundation of Australia website
Safe return to exercise after pregnancy
Exercise can help you recover after childbirth, make you stronger and improve mood. Here are some tips on how to exercise safely after a pregnancy.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.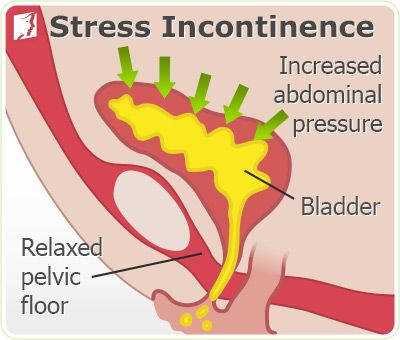
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
How to Handle Urinary Incontinence After Childbirth
Women who expect to leave all the pregnancy aches and pains behind them after childbirth soon find that postpartum symptoms can be almost just as bad.
These effects can take their tole in different ways and can last up to 6 weeks or longer. Soreness, depression, bleeding, fatigue, and constipation are just a few of the unpleasant outcomes women may experience after giving birth. One of the most common complaints from women is how to handle symptoms of urinary incontinence in the weeks following childbirth. Let’s explore some answers.
An Extremely Common Condition
Sorry to report this, but postpartum urinary incontinence is quite common. According to the latest research, women who give birth vaginally are more likely to experience these complications afterward. In some cases, issues of urinary incontinence can last up to a year, and smaller percentages of women are still living symptoms after 5 years.
Contributing factors include the fact that the bladder and pelvis muscles are weakened during childbirth. In addition, the uterus will begin to shrink back to its normal size, which causes repeated compressions on the bladder. Rapid changes in hormones also need to be considered as the body attempts to balance its female sex hormones after a child is born. Women over the age of 35 and those who are obese are also at a greater risk for urinary incontinence following childbirth.
Rapid changes in hormones also need to be considered as the body attempts to balance its female sex hormones after a child is born. Women over the age of 35 and those who are obese are also at a greater risk for urinary incontinence following childbirth.
All together, these influential factors lead women to face a much higher risk for urinary incontinence. The good news is that most women can recover with the proper precautions and effective treatment options recommended by Dedicated to Women.
Simple Lifestyle Changes
There are several ways to address your urinary incontinence without drastically altering your day-to-day routine, including:
- Reduce or completely give up caffeine, carbonated drinks, and alcohol. These beverages, along with spicy foods can cause the bladder to contract much more than what is necessary.
- Losing some weight will ease the pressure on your bladder and pelvic floor.
- Stop smoking if you haven’t done so already. Nicotine causes the muscles of the bladder to spasm, and persistent smoking often leads to a chronic cough that encourages bladder leakage.

- Don’t stop drinking water thinking that it will reduce your urge or need to urinate. You may only end up dehydrated or with a urinary tract infection.
Wear incontinence pads until the problem improves, and contact Dedicated to Women if additional care is needed.
Other Options to Treat Urinary Incontinence After Childbirth
Kegel exercises help to strengthen the pelvic floor muscles and can be performed anywhere. The simplest explanation to this easy exercise is to stop the flow of urine by squeezing the muscles tightly, holding for 5 seconds, and then continuing to urinate. Do these squeezes several times per day for maximum benefit.
A pessary is a small silicone ring inserted into the vagina in the morning and removed each night. This device is designed to stop the flow from a woman’s urethra, and may remain in place all day or only during more strenuous activities if desired.
Sticking to a fixed bathroom schedule will help control your bladder. Try to stretch out the time between trips to the bathroom and build up your tolerance gradually.
Try to stretch out the time between trips to the bathroom and build up your tolerance gradually.
Certain prescription medications can slow down an overactive bladder. Dedicated to Women ObGyn will be able to recommend and prescribe the medications they feel will work best for you and your specific symptoms of urinary incontinence.
There are other treatments that include both non-invasive and surgical methods to help women achieve relief from symptoms of urinary incontinence after childbirth.
Speak with Dedicated to Women if you still are having incontinence issues beyond 6 weeks after the birth of your child.
As always, if you have any further questions or would like to schedule an appointment, please call (302) 674-0223 today!
Urinary incontinence and other health issues after childbirth - Useful articles
There are two types of incontinence: in one case it is associated with an irresistible urge (as they say, "did not reach the toilet"), in the other case, involuntary urination occurs when intra-abdominal pressure increases during exercise , laughing, coughing, sneezing, etc. There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases.
There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases.
The problem in most cases is not resolved by itself, causing physical and psychological inconvenience and suffering (the need to walk around with pads and diapers) and reducing the quality of life, including intimate life. They are embarrassed to talk about it, and compared to how many people are prone to this problem, only a few seek help. Often they simply do not know who exactly to turn to - they go to a gynecologist, and to a therapist, and to a neuropathologist, while this should be done comprehensively and always with the participation of a urologist.
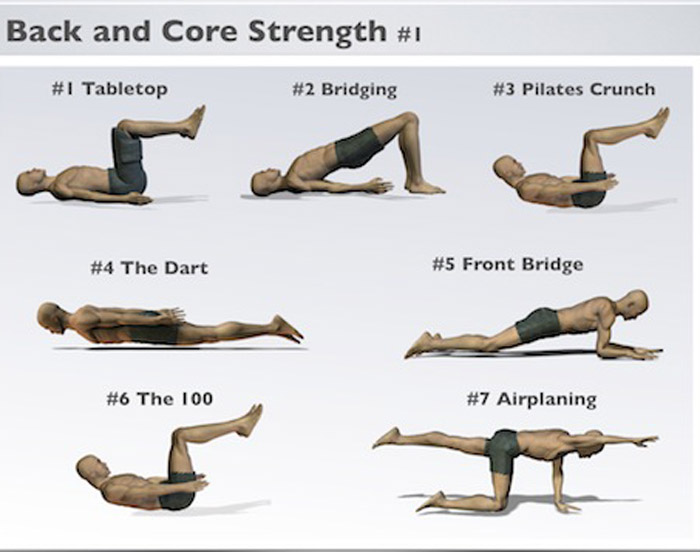
Therapeutic exercise for incontinence
In women after childbirth, disorders of vascular circulation and nervous regulation in the pelvic area are not uncommon.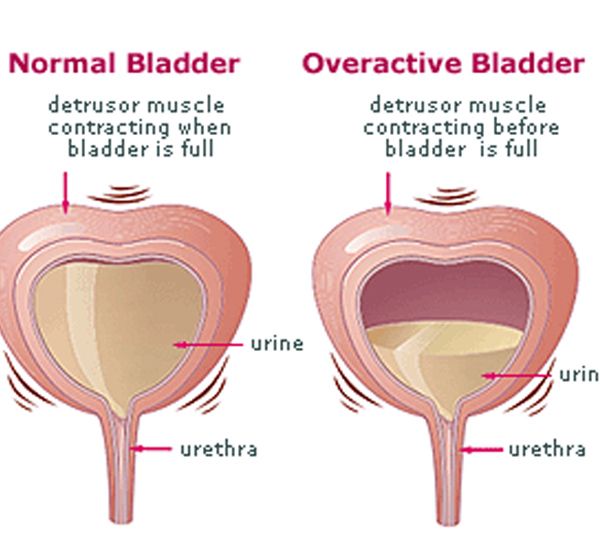 If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions.
If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions.
1. Slow contractions: tighten the muscles as if to stop urination, slowly count to three. Relax.
2. Contractions: tense and relax these same muscles as quickly as possible.
3. Push-ups: tense the perineum and abdominal muscles.
Special therapeutic exercises also help to strengthen the muscles of the small pelvis.
1. I.P. lying on your back. We exhale, draw in the stomach, pull the knees to the chest.
2. I.P. Same. Alternately raise straight legs and make circular movements out and in with full amplitude.
3. From the same position, on exhalation, pull up the chest with bent knees and clasp them with your hands.
4. Now raise the upper body and sit down, wrapping your arms around your knees.
5. At the expense of 1-2-3, lift the upper body and one leg, to which we reach with the same hand. We go down to count 4.
6. Knees bent. At the expense of 1-2-3, we raise the pelvis, squeeze the buttocks, retract the anus. On the count of 4, lower the pelvis and relax.
7. From the same position, we lay bent knees to the right and left of the body.
8. I.P. standing, with support. On the inhale we rise on our toes, on the exhale we squat, holding on to the chair.
9. In the same position, holding onto the support, perform a roll from socks to heels and back.
10. I.P. On knees. Sit on your heels, stretch your arms up.
11. From the same position, alternately straighten the legs and pull them back. Shoulders-back-leg at the same time form one straight line.
12. Standing on all fours, alternately pull opposite arm and leg: straighten on the count of times, hold 2-3, return to the starting position on the count of 4. Be careful not to arch your back.
Be careful not to arch your back.
13. From the same starting position on count 1 stretch one leg back, on count 2-3 take it to the side parallel to the floor, bending at the knee, on count 4 return to the starting position.
14. I.P. hands on the belt, one foot is on the chair. We lean forward and reach for the raised leg, bending it at the knee as much as possible.
There is no need to despair: although treatment is not a simple process due to the large number of components involved in the formation of this syndrome, it is very effective. In all cases, it begins with conservative methods: medicines, physiotherapy and, of course, the therapeutic exercises we have already mentioned. Refrain from activities that increase intra-abdominal pressure. If conservative treatment does not help, low-traumatic surgical methods come to the rescue in the form of imposing various types of loops.
Problems in the perineum
During childbirth, injuries to the soft tissues of the perineum are possible.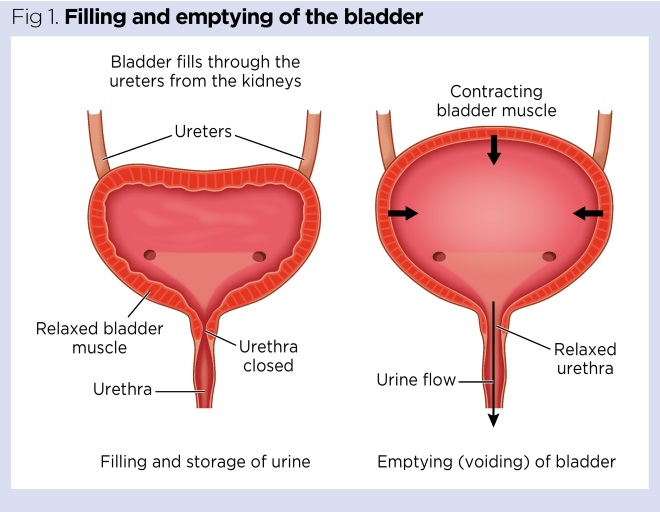 Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life.
Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life.
Sometimes an episiotomy is done for the benefit of the baby and mother. Healing is very fast due to tissue matching and a powerful hormonal explosion. The main task of the mother, if she has stitches, is to keep them clean. This, of course, is hygiene (washing twice a day, from front to back, you can use a decoction of chamomile or a weak solution of potassium permanganate) and ensuring oxygen access. Associated with the latter is the ban on underwear and pads, which causes violent protest among women in maternity hospitals.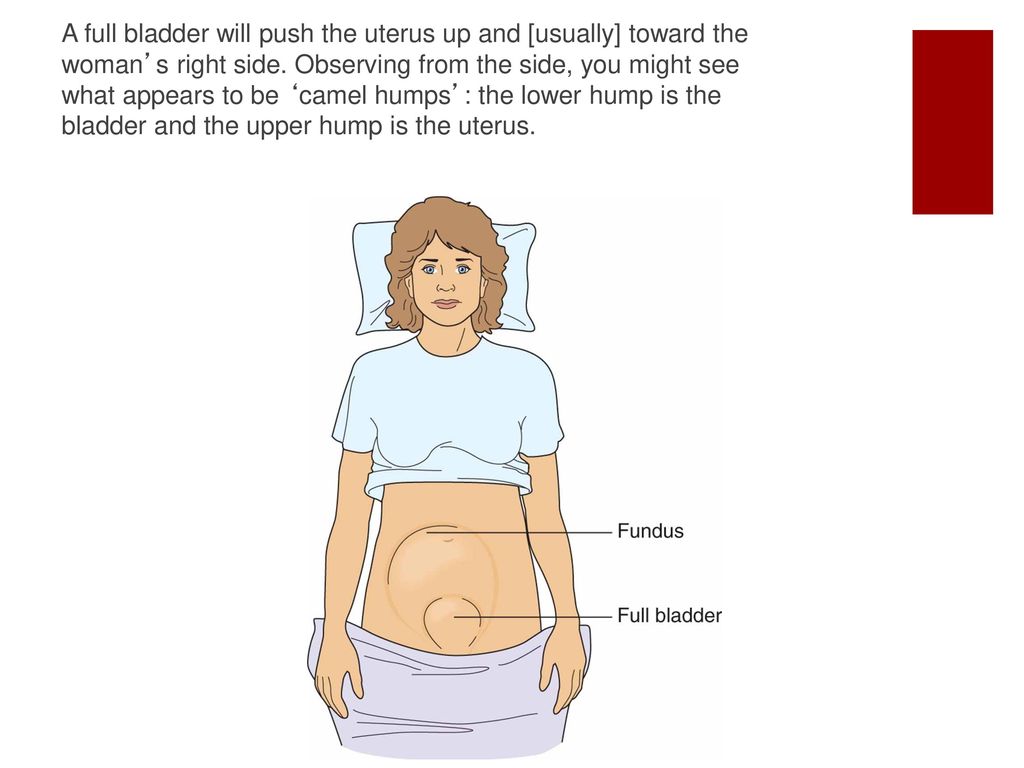
One should not underestimate such an important moment as the normalization of the stool on the third day after childbirth. Defecation does not provoke the divergence of the sutures, on the contrary, this stool retention can lead to trouble, so try to achieve a soft and spontaneous stool by the third day, and upon returning from the hospital, consult a doctor to make sure that the sutures are healing correctly, without divergence and suppuration.
Uterus and vagina
Some women who have recently given birth complain of vaginal gaping, even asking to "sew it up so that it was like before." Bringing the vaginal ring back to normal is really very important, but this process takes some time. During childbirth, the vagina stretches to let the baby through. Closing occurs within six months, which can be accelerated, for example, by the already mentioned Kegel exercise or the mixing-breeding of the legs.
Immediately after delivery, the uterus should empty well, so turn over, give a vertical load.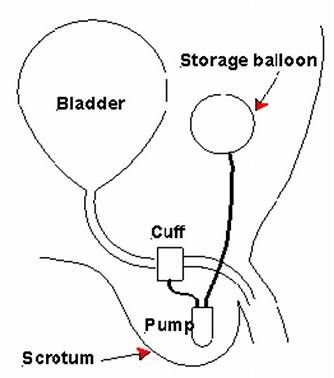 This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down.
This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down.
The return of the tone of the soft tissues of the perineum will also be helped by sexual intercourse, which improves tissue nutrition. Please note: they are allowed when the placental site has been restored in the uterine cavity and there is no longer a risk of inflammation. If you feel pain during intercourse, do not hesitate to tell the doctor about it - he will find out the reason and advise the appropriate position.
Hemorrhoids
Another problem after the birth of a baby is hemorrhoids - a frequent manifestation of varicose veins. If hemorrhoids appear after childbirth, carefully observe them during the first days. Applying cold and topical application of anti-hemorrhoidal agents will help. Remember that the use of drugs after childbirth is limited, so it is necessary to deal with hemorrhoids that have appeared, if necessary, contacting a proctologist.
If hemorrhoids appear after childbirth, carefully observe them during the first days. Applying cold and topical application of anti-hemorrhoidal agents will help. Remember that the use of drugs after childbirth is limited, so it is necessary to deal with hemorrhoids that have appeared, if necessary, contacting a proctologist.
We hope that you will not be at a loss, even if you encounter any of the above troubles and will definitely deal with them as soon as possible. Happy and trouble-free motherhood to you!
Urinary incontinence in women after childbirth.
Article
Ilyina Irina Yuryevna
Akusher-gynecologist, candidate of medical sciences, the Department of Obstetrics and Gynecology of the Moscow Faculty of the RSUMU, Chief Medical Medical Clinic ".
Urinary incontinence in women after childbirth.
The problem of urinary incontinence is one of the most common diseases among women.
The International Society for the Study of Urinary Continence (1974) defined urinary incontinence as a condition in which involuntary loss of urine is a social and hygienic problem and is objectively confirmed.
There are several types of urinary incontinence. In women after childbirth, stress urinary incontinence is most common, another name for this pathology is stress urinary incontinence. This is the involuntary release of urine that occurs when the pressure inside the bladder rises above the pressure in the urethra (urethra).
The cause of stress urinary incontinence is a violation of the function of the sphincter apparatus of the bladder and urethra, which occurs when their normal relationship changes.
Normally, in a standing woman, the bladder neck and the initial section of the urethra are located in the abdominal cavity above the pelvic floor, so the pressure in the urethra is equal to or greater than the pressure in the bladder. With various violations of the normal anatomical relationship between the bladder and the urethra, with an increase in intra-abdominal pressure (when coughing, sneezing, lifting weights), urine leakage is observed.
With various violations of the normal anatomical relationship between the bladder and the urethra, with an increase in intra-abdominal pressure (when coughing, sneezing, lifting weights), urine leakage is observed.
According to the severity of clinical symptoms, three degrees of urinary incontinence are distinguished (Kan D.V., 1986): mild (minimal symptoms of urinary incontinence with significant physical exertion), moderate (involuntary release of urine occurs during laughter, coughing or brisk walking) , severe urinary incontinence (involuntary excretion of urine occurs when changing body position or even during sleep).
The most common cause of this pathology is pathological childbirth (rapid or protracted) - 51.1% - resulting in the development of traumatic and trophic disorders in the walls of the urethra and bladder neck (hematomas, areas of ischemia, tears of muscle fibers), in the future their atrophy and replacement with connective tissue occur, elastic properties are violated. Severe physical activity - 20.6%, associated with a prolonged increase in intra-abdominal pressure, leads to weakening of the ligamentous apparatus of the pelvic floor, disruption of anatomical and functional relationships. However, it should be emphasized that physical overexertion alone rarely leads to urinary incontinence. The disease arises from a number of other reasons, and under the influence of physical activity and inflammatory processes in the genitourinary organs progresses. Hormonal disorders - 15.6% - a decrease in estrogen synthesis that occurs in postmenopause. Operations on the pelvic organs - 12.7% - traumatize muscle formations, develop cicatricial changes in tissues, leading to a shortening of the anatomical and functional length of the urethra.
Severe physical activity - 20.6%, associated with a prolonged increase in intra-abdominal pressure, leads to weakening of the ligamentous apparatus of the pelvic floor, disruption of anatomical and functional relationships. However, it should be emphasized that physical overexertion alone rarely leads to urinary incontinence. The disease arises from a number of other reasons, and under the influence of physical activity and inflammatory processes in the genitourinary organs progresses. Hormonal disorders - 15.6% - a decrease in estrogen synthesis that occurs in postmenopause. Operations on the pelvic organs - 12.7% - traumatize muscle formations, develop cicatricial changes in tissues, leading to a shortening of the anatomical and functional length of the urethra.
Thus, urinary incontinence is a serious medical and social problem that has an extremely negative impact on the psychological state of patients. Studying the psycho-emotional status of women suffering from urinary incontinence, Stanton (2000) noted that more than 38% of patients have a mental disorder of a functional nature.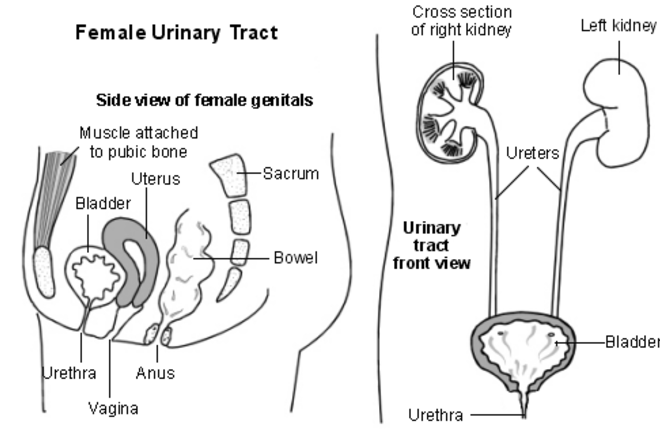 Emotional disturbances were manifested by increased irritability, depression and sexual problems.
Emotional disturbances were manifested by increased irritability, depression and sexual problems.
Many women believe that urinary incontinence develops with age, and almost all experience these symptoms over the years. Indeed, the pelvic floor undergoes significant changes over the years, the urethra-bladder ratio changes, which can lead to the development of symptoms of urinary incontinence, but it is wrong to say that all women are prone to this condition.
Probably, at some stage in the life of every woman there is a change in the pelvic floor, which may be after childbirth, gynecological interventions or during menopause. This leads to changes in the relationship between the bladder and the urethra and it takes some time for the pelvic organs to adapt to the "new" anatomical situation. In the case when this does not happen, the development of symptoms of urinary incontinence is possible.
Among the conditions associated with urinary incontinence, vaginal pelvic organ prolapse has the greatest clinical significance. The problem of prolapse and prolapse of the vagina and uterus continues to be relevant. Prolapse of the uterus is the position of this organ when the cervix is located below the interspinal line. When prolapsed, the uterus goes beyond the genital gap completely (complete prolapse) or partially, sometimes only the cervix (incomplete prolapse).
The problem of prolapse and prolapse of the vagina and uterus continues to be relevant. Prolapse of the uterus is the position of this organ when the cervix is located below the interspinal line. When prolapsed, the uterus goes beyond the genital gap completely (complete prolapse) or partially, sometimes only the cervix (incomplete prolapse).
This disease is caused by congenital or age-related deficiency of the connective tissue, as well as failure of the pelvic floor muscles, which in most cases occurs due to damage to the muscles of the perineum and pelvic diaphragm during childbirth, with a prolonged increase in intra-abdominal pressure due to hard physical work, with chronic lung diseases, constipation . Surgical treatment.
A thorough history and examination is essential in the diagnosis of urinary incontinence. It is important to clarify questions about the duration and severity of incontinence and past attempts to surgically eliminate stress urinary incontinence; it is important to find out the presence of any neurological diseases or diseases of the internal organs that underlie or contribute to urinary incontinence.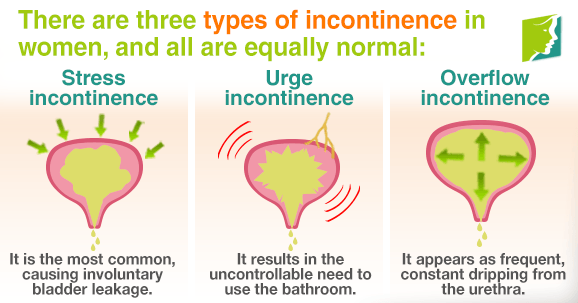
A questionnaire, voiding diary, is used, which is important for quantifying and documenting the amount of urine lost. The diary should record fluid intake and urine output, urination time, and any physical activity associated with episodes of urinary incontinence. A urination diary is kept for 48-72 hours.
| Time of day | Drinking volume (ml) | Excreted volume (ml) | Episodes of urine loss (ml) | What were you doing? |
|
|
|
|
|
|
Urodynamic studies play a significant role in the diagnosis of urination disorders and monitoring the effectiveness of treatment.
Severe to moderate stress urinary incontinence is treated surgically. With a mild degree of urinary incontinence, conservative treatment is possible. Therefore, it is very important to contact a specialist in time in order to start treatment in a timely manner.
The complex of conservative treatment of stress urinary incontinence includes training of the pelvic floor muscles. The key principle of this effect is repeated voluntary contractions of the pelvic floor muscles, which improves their tone, and also facilitates the muscle contraction reflex in response to an increase in intra-abdominal pressure. These exercises in some cases allow you to restore the pelvic muscles and minimize urine loss. The level of success depends on the severity and type of incontinence. The best results are achieved in patients with mild symptoms and well-preserved pelvic floor muscles. Their tone is assessed by a gynecologist during the study quite easily. You can also use specific vaginal cones.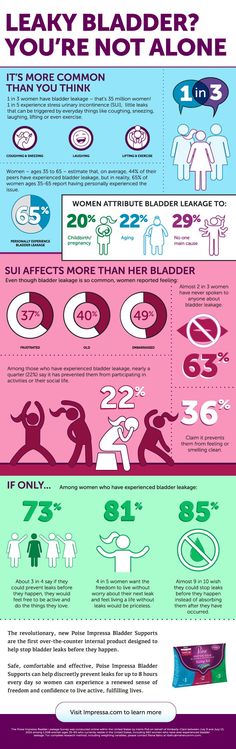 The kit includes several cones of various weights, as certain results of treatment are achieved, the mass of the applied cone gradually increases. Exercises are carried out 10 times for 30 seconds every hour. For an adequate assessment of the effectiveness of treatment, it must be carried out for at least 8-12 weeks. These are the treatments that a woman can independently carry out at home.
The kit includes several cones of various weights, as certain results of treatment are achieved, the mass of the applied cone gradually increases. Exercises are carried out 10 times for 30 seconds every hour. For an adequate assessment of the effectiveness of treatment, it must be carried out for at least 8-12 weeks. These are the treatments that a woman can independently carry out at home.
There are also other conservative treatments such as negative feedback pelvic floor muscle training, electrical stimulation.
Urinary incontinence is a complex medical, hygienic and social problem. Therefore, assistive devices used to correct incontinence play an important role in many situations - in preparation for surgical treatment, as well as during rehabilitation after it, when training the bladder and pelvic floor muscles. They enhance the social adaptation of this category of women and solve most of the hygiene problems caused by the negative effect of urine on the skin.
Modern devices (pessaries, urethral obturators) are effective means of preventing stress urinary incontinence for a long time. They do not have serious side effects and subjective inconveniences. However, there is a small percentage of violations of the integrity of the vaginal epithelium, including erosion and polyps, which can also sometimes lead to infection of the urinary tract.
They do not have serious side effects and subjective inconveniences. However, there is a small percentage of violations of the integrity of the vaginal epithelium, including erosion and polyps, which can also sometimes lead to infection of the urinary tract.
Women rarely turn to specialists because are embarrassed and many of them believe that this phenomenon is quite natural and every woman ever notes the symptoms of urinary incontinence. At the same time, some are skeptical about the possibility of treatment by a specialist, because. do not believe in the effectiveness of the treatment of this pathology. Lots of sick people put off
a visit to the doctor until the manifestations and severity of the disease interfere with their daily lifestyle and work.
Once again, we note that timely access to specialists and the early start of conservative treatment of urinary incontinence largely determines the success of treatment. In order to shorten the examination time and facilitate your first communication with the doctor, we suggest that you fill out the urination diary above and a questionnaire that includes 28 questions reflecting the possible causes of urinary incontinence, the nature of complaints, the duration of the disease, the number of births, their course, the effectiveness of conservative and surgical treatment (if any), the function of the bladder, urethra and rectum.