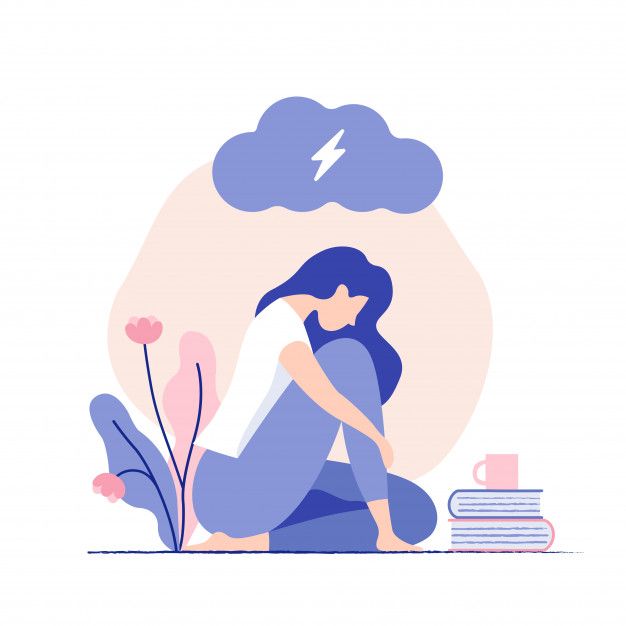
Feeling depressed in pregnancy
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
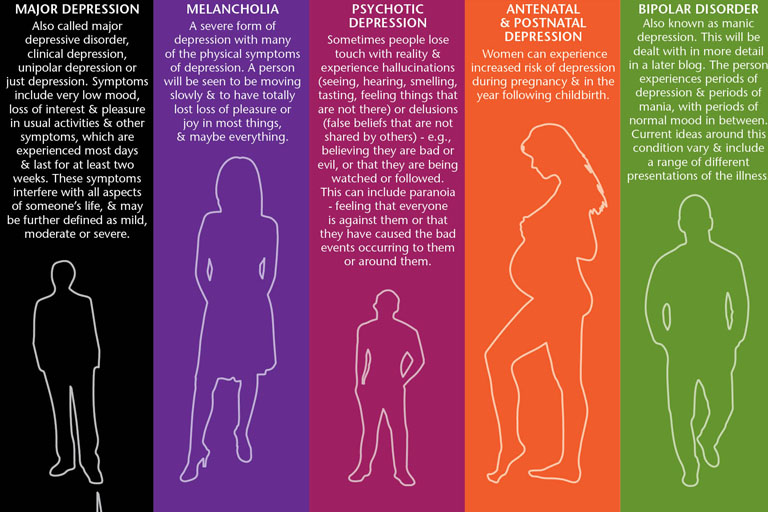
Depression during and after pregnancy: why it occurs
Ekaterina Barskaya
GMS Clinic doctor, perinatal psychologist
When a woman makes a decision for herself that she will be a mother, changes gradually begin in the body both at the physiological and psycho-emotional levels. There is an adaptation to new sensations, roles, status. Their acceptance by a pregnant woman and her reaction to changes will depend on many factors: age, social, religious, personal characteristics and life experience. nine0006
nine0006
Today we will talk about the symptoms of depression and the importance of a stable psychological state of expectant mothers with Ekaterina Sergeevna Barskaya, a GMS Clinic doctor and a perinatal psychologist with 20 years of experience.
Does prenatal depression really happen and why does it occur?
Yes, this really happens. The first pregnancy is exciting in itself. I want everything to be not only correct, but completely perfect. However, the flow of information or someone else's experience, which is often negative, causes a defensive reaction - anxiety, which in turn forms uncertainty in one's thoughts and actions. nine0006
There is such a natural fear as the instinct of self-preservation, and not a single desired pregnancy was without fear for oneself and for the child - this is natural!
Each stage of pregnancy has its own challenges and difficulties. And how sensibly the state and feelings will be accepted depends largely on the woman herself.
- The first trimester is the realization and acceptance of the very fact of future parenthood. There is a reassessment and a change in lifestyle, habits, regimen, taste preferences. The body is rebuilt, new functions appear that were not previously known. Symptoms of toxicosis, irritability and drowsiness are frequent companions of the first period. Here it is important to learn to listen to your body and satisfy the need for rest. nine0021
- In the second trimester there are noticeable changes in the body. Feel the movements of the child. From that moment on, attachment is formed, acceptance of another life inside your body.
- The third trimester is preparation for childbirth. As practice shows, the more anxious a woman feels, the more information about childbirth she tries to find. Sometimes this leads to even more stress and anxiety.
Imagine a person decides to jump with a parachute. He ground himself with theories about the opening mechanism of the dome, about air currents, about the correct grouping, etc. But it's still scary. You can refuse to jump. But childbirth - will be! Knowing about the future is good, but emotions are sometimes stronger than rationality. Therefore, the most important thing is to believe in yourself, in your body, in your child. If you become pregnant, carried a baby, then the body knows what to do next. We must listen to him and support him. nine0006
But it's still scary. You can refuse to jump. But childbirth - will be! Knowing about the future is good, but emotions are sometimes stronger than rationality. Therefore, the most important thing is to believe in yourself, in your body, in your child. If you become pregnant, carried a baby, then the body knows what to do next. We must listen to him and support him. nine0006
Before childbirth, the body concentrates inward, as if accumulating strength. Therefore, expectant mothers become more passive, sleepy, sometimes aloof. This is physiologically understandable - they need a sufficient amount of the hormone oxytocin. And the adrenaline released into the blood during stress destroys it. That is why special attention is paid to the regime, sparing lifestyle and information hygiene.
Are there prerequisites for the onset of prenatal depression?
Unfortunately, the number of depressive states is growing in the modern world. Studies show that women are 3 times more likely to be affected than men. One of the reasons is a brighter psycho-emotional background. nine0006
One of the reasons is a brighter psycho-emotional background. nine0006
Depression in pregnancy can be caused by a variety of factors:
- heredity;
- fear;
- unresolved conflicts;
- internal rejection of future motherhood;
- unwanted pregnancy;
- financial and domestic difficulties;
- excessive demands on oneself, when it is necessary to do everything, control everything and be an ideal mother, wife, employee, etc. nine0021
Prenatal depression is not just a bad mood. This is a persistent, weeks-long state of anxiety, sadness, and pessimism. It can provoke not only psychosomatic diseases, but also premature birth.
Correct and timely diagnosis of the mental state can reduce the risk of developing depressive tendencies during pregnancy, and thus prevent postpartum disorders.
It is important to pay attention to the mood of the expectant mother in time. Of course, patience and care are needed from others. A more trusting and warm relationship will help to avoid difficulties. nine0006
A more trusting and warm relationship will help to avoid difficulties. nine0006
What happens to a woman's emotional state after childbirth?
After childbirth, a woman expects a surge of emotions and tenderness. But this is not always the case. Maternal feelings do not turn on on click. The expectations of others that a young mother is happy, feels and understands the child are often not justified. A woman may experience regret and even guilt. It's okay, it happens!
Even in the maternity hospital, you can experience unpleasant sensations: the so-called "baby blues" or depressive syndrome. 85% of young mothers face it - this is due to hormonal changes in the body, it starts 3-5 days after birth and lasts from 2 days to two weeks. Usually it does not require any intervention and goes away on its own. If, over time, the psychological state of a new mother causes concern, and the process of adapting to a new role is not going as expected, pay attention to the following signs: nine0006
- tearfulness and sadness for no particular reason;
- reduced emotional background;
- irritability;
- apathy;
- lack of emotional reaction to what is happening in life;
- poor sleep, appetite;
- absent-mindedness.

All of these are warning signs. The main burden will fall on the shoulders of the partner, because he plays the role of "first violin", providing the necessary support and attention. After the birth of a child, a crisis often occurs in family relationships, and it will take time to adapt. The passage of this period will depend on how much parents understand and support each other. nine0006
How to help a young mother?
Support and care are different:
- Give mom a chance to rest and sleep.
- Take charge of household and domestic duties.
- Have a weekend - give a young mother the opportunity to get out of the house, go to a manicure, a beauty salon, meet her friends.
- Find an opportunity to communicate. It can be a motherly chat where you can discuss all the complexities and difficulties of motherhood, see that what is happening is normal. nine0021
- Don't give up on your own desires. Remind mom sometimes to do something for herself: let her choose her favorite foods for dinner, do not forget about her TV shows, books and hobbies.
- Listen to the emotional state. Create an environment in which you can cry, complain, or yell into a pillow, for example. It helps to relieve tension and throw out the accumulated negative emotions.
Don't be afraid to ask your mom for help from a specialist. It can be a psychologist, neurologist, psychiatrist. They will be able to provide additional support in difficult times. nine0006
And yet: is depression a physiology or a psychology?
This question is often asked. In my opinion, this is a single system. At the biochemical level, depression looks like an imbalance in the cerebral cortex: serotonin, dopamine and norepinephrine. These are neurotransmitters that transmit impulses to our neurons and are involved in the regulation of mood and behavior. This is physiology.
But when there is a reaction, psychology comes into play. We feel → react → give feedback to what is happening. As the saying goes: "When the soul cries, the body also suffers.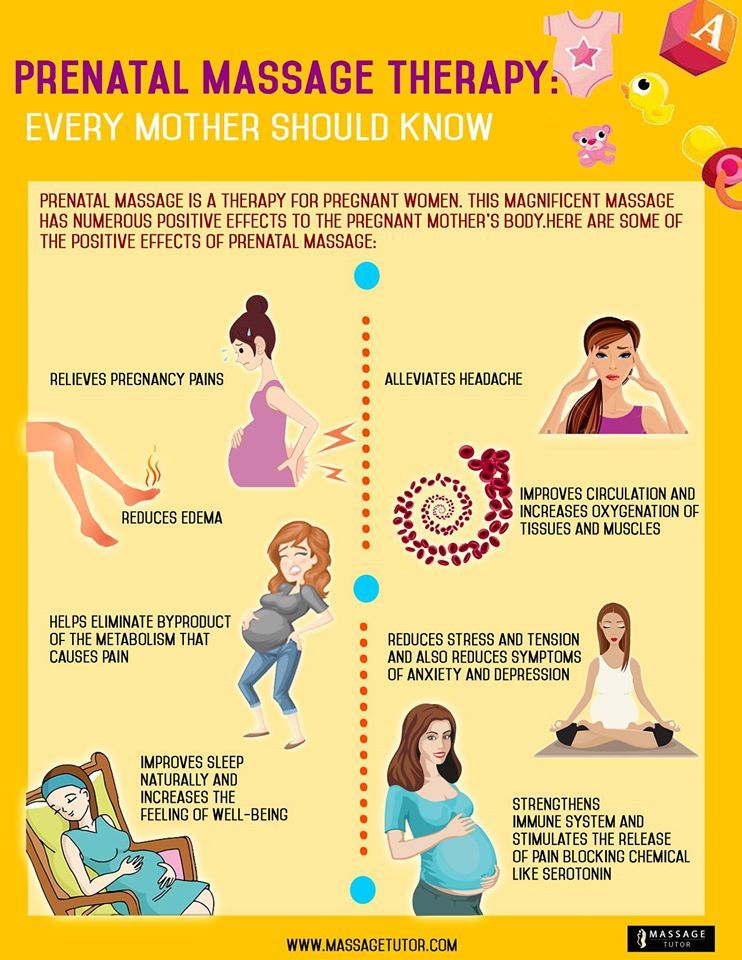 " Everything in our body is interconnected. Both psychology and physiology. Influence can have features of the nervous and endocrine systems, heredity. nine0006
" Everything in our body is interconnected. Both psychology and physiology. Influence can have features of the nervous and endocrine systems, heredity. nine0006
Try to always listen to yourself and do not be too self-critical. When a child is born, it is important for him to see an emotional response from his parents. Especially mothers are the information reading systems of this world. Be supportive of yourself and your child.
Effect of depression on pregnancy
Effect of depression on pregnancySite search nine0006
Preambula Bot
Preambula Bot
Online
List of dialogues
Available dialogues
You can communicate with doctors and ask any questions to the bot nine0006
Log in
in PreAmbula
No questions asked
the administrator is in touch, who knows your medical history
Log in
in PreAmbula
Personal
widget
with appointments, conclusions
and appointments
Log in
in PreAmbula
1
Hello! I want to sign up
Continue
in the telegram bot
it's convenient: we are always online
on your phone
Continue
Preambula Bot
To see dialogues with doctors, you need to log in
Hello. If you need to contact a doctor, sign up for an online consultation:
If you need to contact a doctor, sign up for an online consultation:
Conditions for the consultation nine0006
Sign up for a consultation
five
Effects of depression on pregnancy
Share
Some women develop depression during pregnancy. There may be several reasons: someone feels somehow "not like that", while someone's depression is completely unrelated to the phenomenon of "pregnancy".
Also, during pregnancy there can be psychological and physical stress. All this flows smoothly from depression. If a woman has financial or family problems, as well as health problems, then stress cannot be avoided. nine0006
Depression during pregnancy is similar to that of the average person. For example, a person has a certain emptiness, sadness, depression is also felt, constant fatigue is felt, appetite may disappear or appear. There are also problems with sleep.