Signs of uti while pregnant
Urinary tract infections (UTIs) in pregnancy - symptoms, causes
Urinary tract infections (UTIs) in pregnancy - symptoms, causes | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a urinary tract infection?
A urinary tract infection (UTI) is an infection of the urinary system. UTIs are the most common bacterial infection that women develop during pregnancy. They can occur in different parts of the urinary tract, including the bladder (cystitis), urethra (urethritis) or kidneys (pyelonephritis). Sometimes when a UTI develops and bacteria are detected in the urinary tract, you may not have any symptoms of an infection. This is known as asymptomatic bacteriuria.
While anyone can get a UTI, they are much more common in women than men and they are also more likely to occur in the very young and the elderly.
What are the symptoms of UTIs during pregnancy?
Common symptoms of a UTI during pregnancy are similar to those that you might experience at any other time, and include:
- a burning sensation when you pass urine
- feeling the urge to urinate more often than usual
- urinating before you reach the toilet (‘leaking’ or incontinence)
- feeling like your bladder is full, even after you have urinated
- urine that looks cloudy, bloody or is very smelly
- pain above the pubic bone
- fever
Sometimes the first sign of an infection is a faint prickly sensation when you pass urine. If the infection is more advanced and has moved up to the kidneys, you may also experience fever with a particularly high temperature, back pain and vomiting.
What are the common causes of UTIs?
Your urinary tract is normally free of bacteria. If bacteria enter the tract and multiply, they can cause a UTI. There are several factors that increase the risk of developing an infection:
- Infection with common bacteria in your gut, usually from faeces (poo) can contaminate your urinary tract
- Being sexually active increases the risk of bacteria moving around the genital area and entering the urinary tract
- If you have weak pelvic floor muscles your bladder might not empty completely, which can lead to an infection
- Women with diabetes are at increased risk of developing a UTI since the sugar in their urine may cause bacteria to multiply
Are UTIs a risk during pregnancy?
During pregnancy, many changes occur in your body that increase your risk of developing a UTI, including changes to the make-up of your urine and immune system. As your baby grows, there is also an increase in the pressure on your bladder, which can reduce the flow of your urine and lead to an infection.
As your baby grows, there is also an increase in the pressure on your bladder, which can reduce the flow of your urine and lead to an infection.
UTIs can affect women whether they are pregnant or not. However, pregnant women are more likely to develop repeated or more severe infections. Up to 1 in 10 pregnant women will have a UTI but not have any symptoms at all.
Is there a risk to my baby?
Having a UTI during pregnancy can increase your risk of developing high blood pressure, and your baby may be born early and smaller than usual. For this reason, even if you don’t have any symptoms, it is important to treat a UTI as soon as possible.
How are UTIs diagnosed?
UTIs are diagnosed by taking a urine sample which is checked in a laboratory for bacteria. Your doctor may also perform a physical examination if they think you have an infection.
All pregnant women are offered a urine test, usually at their first antenatal visit or soon after. You may need to repeat the urine test if you have a history of UTIs; have symptoms of a UTI; have a contaminated sample or if your doctor thinks you are at high risk of developing a UTI. If you have frequent UTIs, you may also need additional tests such as an ultrasound of your kidneys.
If you have frequent UTIs, you may also need additional tests such as an ultrasound of your kidneys.
How are UTIs treated during pregnancy?
When you have a UTI, it is important to drink plenty of water to flush out the urinary tract. UTIs are treated with antibiotics that are safe in pregnancy. Your doctor will select the right antibiotic, based on your infection and the type of bacteria found in your urine sample.
Can I prevent UTIs?
You can lower your risk of developing a UTI during pregnancy by:
- drinking plenty of fluids, especially water
- quickly treating any vaginal infection that may occur, including thrush or a sexually transmitted infection
- avoiding becoming constipated
Some women have also found the following tips helpful:
- urinate immediately after sex
- don’t delay going to the toilet — go as soon as you feel the need
- wipe from the front to the back after going to the toilet
- wear cotton underwear
When should I see my doctor?
See your midwife or doctor if you have any symptoms of a UTI. It’s important not to delay treatment since infections develop quickly, and can affect both you and your baby.
It’s important not to delay treatment since infections develop quickly, and can affect both you and your baby.
More information
UTIs are very common during pregnancy, and are best treated early. If you notice the symptoms of an infection, seek medical advice from your doctor, midwife or pharmacist.
For more information on UTIs, visit the Kidney Health Australia page on UTIs.
Sources:
Government of South Australia (Urinary Tract Infection in Pregnancy), Jean Hailes (Urinary Tract Infections), Kidney Health Australia (Factsheet: Urinary Tract Infections), Government of Western Australia North Metropolitan Health Service (Urinary Tract Infection in Pregnant Women)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2021
Back To Top
Related pages
- Incontinence during pregnancy
- Frequent urination during pregnancy
Need more information?
Urinary tract infection (UTI) - MyDr.
 com.au
com.au Urinary tract infection occurs when part of the urinary tract becomes infected. UTIs are usually caused by bacteria and generally clear up with a course of antibiotics.
Read more on myDr website
Urinary tract infection (UTI) | SA Health
Urinary tract infection (UTI) is an infection of the urinary system. Infection may occur in the kidneys, bladder or urethra.
Read more on SA Health website
Urinary tract infections (UTIs) explained - NPS MedicineWise
Learn about the causes & treatments for urinary tract infections (UTIs).
Read more on NPS MedicineWise website
Urinary Tract Infections (UTIs) | Jean Hailes
A comprehensive guide to urinary tract infections. Everything you should know about UTIs including causes, symptoms, management and treatment.
Everything you should know about UTIs including causes, symptoms, management and treatment.
Read more on Jean Hailes for Women's Health website
Incontinence & Bladder Weakness | Jean Hailes
What makes a normal bladder. Types of incontinence. Causes and symptoms. Diagnosis and treatment. Prevention and management.
Read more on Jean Hailes for Women's Health website
Pyelonephritis
Infection of the kidneys.
Read more on Queensland Health website
Check-ups, tests and scans available during your pregnancy
Antenatal care includes several check-ups, tests and scans, some of which are offered to women as a normal part of antenatal care in Australia. Learn more here.
Learn more here.
Read more on Pregnancy, Birth & Baby website
Thrush | SA Health
Thrush or Candidiasis is a common vaginal infection, caused by an overgrowth of yeasts and is not considered to be a sexually transmitted infection
Read more on SA Health website
Pregnancy at week 9
Your baby is now the size of a peanut. You won't be showing just yet, but you may have put on a little weight.
Read more on Pregnancy, Birth & Baby website
Your first antenatal visit
Find out what will happen and what you can learn during your first antenatal care visit with your GP or midwife.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Urinary Tract Infections (UTI) During Pregnancy
Written by WebMD Editorial Contributors
Medically Reviewed by Nivin Todd, MD on September 04, 2022
In this Article
- UTI Symptoms
- Why Are UTIs More Common During Pregnancy?
- UTI Diagnosis
- UTI Treatment During Pregnancy
- UTI Complications During Pregnancy
- UTI Prevention
A urinary tract infection (UTI) is an infection of some part of your body's urinary system, which includes your:
- Kidneys
- Ureters (tubes that carries urine from your kidneys to your bladder)
- Bladder
- Urethra (a short tube that carries urine from your bladder to outside your body)
Bacteria cause most UTIs. Anyone can get one, but they're most common in women, and they can be extra concerning if you're pregnant.
Anyone can get one, but they're most common in women, and they can be extra concerning if you're pregnant.
If you think you might have a UTI, tell your doctor. With proper care, you and your baby should be fine.
Usually, these infections are in the bladder and urethra. But sometimes they can lead to kidney infections. If they do, UTIs may lead to preterm labor (giving birth too early) and low birth weight.
UTI Symptoms
If you have a UTI, you may have:
- An urgent need to pee, or peeing more often
- Trouble with peeing
- A burning sensation or cramps in your lower back or lower belly
- A burning feeling when you pee
- Urine that looks cloudy or has an odor
- Blood in your pee, which can turn it red, bright pink, or cola-colored
If you have a kidney infection, you may have:
- Fever
- Nausea
- Vomiting
- Upper back pain, often on just one side
If you have symptoms of a kidney infection, see your doctor right away. Without treatment, the infection can spread into your bloodstream and cause life-threatening conditions.
Without treatment, the infection can spread into your bloodstream and cause life-threatening conditions.
Why Are UTIs More Common During Pregnancy?
Hormones are one reason. In pregnancy, they cause changes in the urinary tract, and that makes women more likely to get infections. Changes in hormones can also lead to vesicoureteral reflux, a condition in which your pee flows back up from your bladder to your kidneys. This can cause UTIs.
When you’re pregnant, your pee has more sugar, protein, and hormones in it. These changes also put you at higher risk for a UTI.
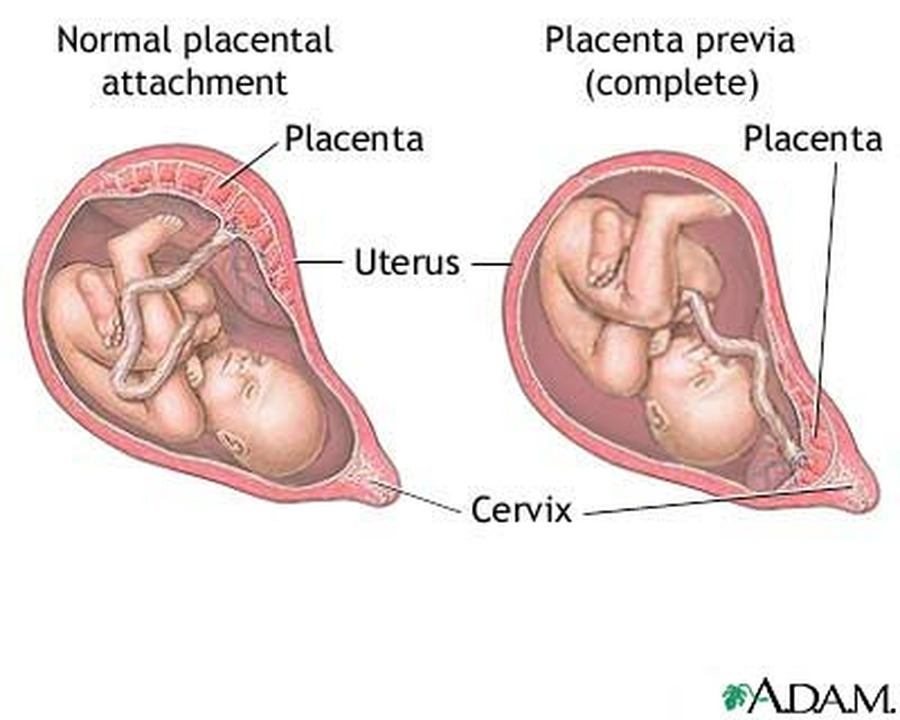
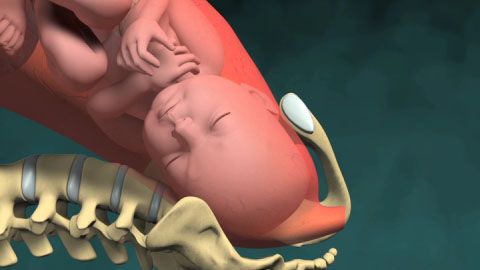
Because you’re pregnant, your growing uterus presses on your bladder. That makes it hard for you to let out all the urine in your bladder. Leftover urine can be a source of infection.
Other causes of UTIs include:
Escherichia coli and other bacteria from your poop. E. Coli is the most common cause of UTIs and can move from your rectum to your urethra if you don’t wipe from front to back.
Sexual activity. Fingers, your partner’s penis, or devices can move bacteria near your vagina into your urethra.
Group B streptococcus. Many women have this bacteria in their colon and vagina. It can cause UTIs and women can pass it to their newborns. Your doctor will test you for this bacteria around weeks 36 to 37 of pregnancy. If you’re positive for group B strep, your doctor will give you IV antibiotics during labor.
UTI Diagnosis
You’ll take a urine test. Your doctor will test it for bacteria and red and white blood cells. A urine culture may also be checked. It shows what kind of bacteria are in the urine.
UTI Treatment During Pregnancy
You’ll take antibiotics for 3 to 7 days or as your doctor recommends. If your infection makes you feel uncomfortable, your doctor will probably start your treatment before you get your urine test results.
Your symptoms should go away in 3 days. Take all of your medication on schedule anyway. Don’t stop it early, even if your symptoms fade.
Don’t stop it early, even if your symptoms fade.
Many common antibiotics -- amoxicillin, erythromycin, and penicillin, for example -- are considered safe for pregnant women. Your doctor wouldn’t prescribe others, such as ciprofloxacin (Cipro), sulfamethoxazole, tetracycline, or trimethoprim (Primsol, Proloprim, Trimpex), that can affect your baby’s development.
UTI Complications During Pregnancy
Pyelonephritis is a UTI that affects the kidneys. If you’re pregnant it can cause:
- Preterm labor
- Severe infection
- Adult respiratory distress syndrome
- Anemia
- Long-term infection
UTI Prevention
To try to avoid getting a UTI:
- Drink at least eight glasses of water a day.
- Wipe yourself from front to back when you go to the bathroom.
- Empty your bladder shortly before and after sex.
- If you need a lubricant when you have sex, choose a water-based one.
- Don't douche.
- Avoid strong feminine deodorants or soaps that cause irritation.

- Wash your genital area with warm water before sex.
- Wear cotton underwear.
- Take showers instead of baths.
- Don’t wear pants that are too tight.
- Pee often.
- Avoid alcohol, citrus juices, spicy food, and caffeinated drinks, which can irritate your bladder.
Women's Health Guide
- Screening & Tests
- Diet & Exercise
- Rest & Relaxation
- Reproductive Health
- Head to Toe
Early pregnancy | Shchelkovsky perinatal center
Pregnancy is a wonderful period! However, the changes taking place in the body at this time can greatly frighten you. The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
1. Frequent urination.
Frequent urination.
Frequent, painless (!) urge to urinate is one of the signs of pregnancy. This is due to increased secretion of progesterone (pregnancy hormone), changes in metabolism and pressure from the growing uterus on the bladder. nine0005
Be sure to see a doctor if:
- painful urination (this may be a sign of an infection)
- urine of strange color (stained with blood, brown)
- the amount of urine excreted per day is much less than the liquid drunk per day
Life hack! Under no circumstances should fluid intake be restricted! To alleviate the condition and reduce the frequent urge to urinate, it is necessary to exclude products that have a diuretic effect: tea, coffee, zucchini, watermelon; as well as salty, spicy and fried foods. It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen. nine0005
2. Nausea, vomiting, heartburn, increased susceptibility to smells.
Nausea, vomiting, heartburn, increased susceptibility to smells.
Nausea is one of the common symptoms of early pregnancy. The range of issues related to nausea and vomiting during pregnancy is quite wide. From "it's good, I don't even feel sick" (with relief), "I don't feel sick, what's wrong with me?" (with anxiety) to "when will this nausea pass" (with hope). Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy. nine0005
Life hack! For nausea, eat before feeling hungry. Solid, non-hot food and drinks at a cool temperature are best. With heartburn, you should eat small portions of food and often, and most importantly, sit, stand or walk for at least 30 minutes after eating, but do not lie down.
You should definitely consult a doctor if:
- vomiting occurs even after drinking water
- vomiting is exhausting, accompanied by dizziness, weakness
- dryness, jaundice and flaking of the skin appear
- Nausea and vomiting interfere with proper nutrition, accompanied by weight loss
To reduce nausea and vomiting in the morning, try eating something before you get out of bed. It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea. nine0005
It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea. nine0005
3. Pain or cramps in the lower abdomen, constipation, pain in the lumbar region.
The simplest and most easily controlled cause of pain is delayed and incomplete bowel movements. An increase in the concentration of progesterone relaxes the smooth muscles, which are located not only in the uterus, but also in other hollow organs. In this case, the correction of the diet and the restoration of the passage of feces will help. If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment. nine0005
If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment. nine0005
You should definitely consult a doctor if:
- pain is accompanied by spotting bloody discharge from the external genitalia
- increasing duration and intensity of pain
- abdominal pain accompanied by dizziness, fever, loss of consciousness
Life hack! To normalize bowel movements, eat more vegetables and fruits, drink water and move more during the day. Try to eat often and in small portions. nine0005
Try to eat often and in small portions. nine0005
4. Enlargement and soreness of the mammary glands.
Hormonal restructuring of the body during gestation is accompanied, among other things, by an increase in the size of the mammary glands and an increase in their sensitivity. By the end of the first trimester, the soreness usually disappears, no additional methods of treatment are needed.
Life hack! Choose comfortable supportive underwear (it should not leave marks on the skin at the end of the day). You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day. nine0005
You should definitely see a doctor if:
- the pain is intense
- mammary glands are very dense with redness and body temperature is increased
- discharge from the nipples appears (purulent, bloody)
5. Increased body temperature.
In early pregnancy, an increase in body temperature to 37.5 ° C is not necessary, but is possible due to the peculiarities of the action of progesterone. Because of this, it is difficult for pregnant women to endure stuffy, hot rooms. Self-medication is dangerous: an attempt to bring down the temperature even with a seemingly harmless folk method - tea with raspberries - can mask the true cause of hyperthermia and delay the diagnosis. Due to the increased body temperature, pregnant women should dress in layers and avoid stuffy and hot rooms and spaces so that they can always “adjust” their temperature on their own. nine0005
- temperature above 37.5 °C
- along with fever, any pain occurs
- runny nose, cough, body aches appear
6. Nasal congestion, difficulty breathing, nosebleeds.
These symptoms can be explained by the individual reaction of the vascular system to the increase in blood volume that occurs during pregnancy. Another possible reason is dry air in the room, the operation of central heating batteries. nine0005
Another possible reason is dry air in the room, the operation of central heating batteries. nine0005
Life hack! The easiest way to deal with nasal congestion is to use a humidifier. If you don't have one, you can put a damp towel on the battery - less effective, but better than nothing. It is possible to use sprays with sea salt, but you need to carefully read the instructions and especially the "Indications" section, it should contain information about the safety of the product during pregnancy.
You should definitely see a doctor if:
- symptoms of a cold occur
- nasal congestion accompanied by ear congestion
- These symptoms appeared after exposure to the allergen known to you
7. Blood pressure fluctuations.
An ideal option for the course of any pregnancy is the stability of the blood pressure throughout the gestation. However, this is extremely rare. A small (up to 10 units) increase in pressure from the usual reference may be due to an increase in the load on the cardiovascular system as a result of changes in body weight, hormonal changes, and uterine pressure on the vessels. Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130-139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits. Of the completely exotic for our days, but no less significant - the prevention of stress.
A small (up to 10 units) increase in pressure from the usual reference may be due to an increase in the load on the cardiovascular system as a result of changes in body weight, hormonal changes, and uterine pressure on the vessels. Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130-139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits. Of the completely exotic for our days, but no less significant - the prevention of stress. nine0005
nine0005
Life hack! If you first discovered that you have high normal pressure, repeat the measurement after 15 minutes. If the pressure remains elevated, see a doctor.
Be sure to see a doctor if:
- your blood pressure is above 140/90 mmHg.
- pressure increased by more than 10 mm Hg. relative to your regular
- an increase in the pressure indicator is accompanied by edema, the appearance of "flies" before the eyes
NB! You should also pay attention to lowering blood pressure. Numbers less than 90/60 mmHg - an excuse to see a doctor.
Life hack! Keep a blood pressure diary, especially if you are prone to hypertension. Show your diary to your doctor at every appointment.
8. Heaviness and pain in the legs.
Heaviness and pain in the legs, especially in the evening, are frequent companions of pregnancy. There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body. nine0005
nine0005
Life hack! Ask your partner/husband to give you a foot massage, relax with your limbs elevated (not too much!) A therapeutic pedicure, dousing the legs with cool water, a contrast shower, a cream or gel for legs with cooling components (menthol, essential oils), as well as compression stockings or stockings of the lightest degree of compression will help.
You should always see a doctor if:
- one or both legs are very swollen or discolored
- previously diagnosed varicose veins, family history of thrombosis
9. Skin changes.
During pregnancy, you may notice dark spots on your skin. Especially often such darkening (hyperpigmentation) is observed in the nipple area, along the white line of the abdomen. Stretch marks (stretch marks) may appear on the skin of the abdomen and thighs. These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks. nine0005
Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks. nine0005
Life hack! Oils and moisturizing creams to increase skin elasticity, contrast showers, massage with a hard brush will help reduce the likelihood of skin changes.
You should definitely consult a doctor if:
- along with itching there are areas of redness, spots, peeling
- itching increases
10. Bleeding gums.
Changes in the characteristics of blood circulation in the body of a pregnant woman can cause bleeding gums. The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist. nine0005
If you find it difficult to assess your own condition, consult a specialist. nine0005
You should definitely consult a doctor if:
- you have loose teeth, sore gums, bad breath
- bleeding in the gum area increases
11. Fatigue, mood instability.
Tearfulness, lack of strength, forgetfulness, distraction, the whole palette of feelings "here and now"... The list can be continued, and there is only one explanation for this - pregnancy. The most common early symptom is severe fatigue. There is no universal recipe, just as there is no single picture of these states. The main recommendation for all pregnant women is to rest often, relax and even sleep during the day. Most importantly, you need to remember: pregnancy is not a disease, but a great time to prepare for motherhood. nine0005
Polyhydramnios during pregnancy. What is polyhydramnios during pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Polyhydramnios during pregnancy is a condition characterized by an increase in the amount of amniotic fluid in the amnion. Pathology manifests itself at different stages of embryogenesis, accompanied by a deterioration in general well-being, fluctuation, swelling and severe toxicosis. It is possible to diagnose polyhydramnios during pregnancy on the basis of data from an objective examination and ultrasound. Treatment of pathology involves hospitalization in the obstetric department, where antibiotics, drugs that improve blood flow in the placenta, and vitamins are prescribed. Depending on the severity of the patient's condition, expectant management or emergency delivery may be used. nine0005
- Causes of polyhydramnios during pregnancy
- Classification and symptoms of polyhydramnios during pregnancy
- Symptoms of polyhydramnios during pregnancy
- Diagnosis of polyhydramnios during pregnancy
- Treatment of polyhydramnios during pregnancy
- Prognosis and prevention of polyhydramnios during pregnancy
- Prices for treatment
General
Polyhydramnios during pregnancy is an obstetric anomaly, accompanied by a gradual or rapid deviation of the level of OPV from normal values towards an increase. Another name for this pathological condition is polyhydramnios. Normally, the volume of OPV depends on the gestational age: at 10 weeks - 30 ml, after 21 days - 100 ml, at 18 weeks - 400 ml, closer to childbirth - 800-1500 ml. Polyhydramnios is diagnosed in approximately 1% of patients at different stages of gestation, most often the pathology occurs in the 2nd-3rd trimester. The danger of polyhydramnios during pregnancy lies in provoking multiple negative consequences for the woman and the child. In 36% of all cases, this condition causes severe toxicosis at any stage of embryogenesis and contributes to a significant deterioration in the patient's condition. nine0005
Another name for this pathological condition is polyhydramnios. Normally, the volume of OPV depends on the gestational age: at 10 weeks - 30 ml, after 21 days - 100 ml, at 18 weeks - 400 ml, closer to childbirth - 800-1500 ml. Polyhydramnios is diagnosed in approximately 1% of patients at different stages of gestation, most often the pathology occurs in the 2nd-3rd trimester. The danger of polyhydramnios during pregnancy lies in provoking multiple negative consequences for the woman and the child. In 36% of all cases, this condition causes severe toxicosis at any stage of embryogenesis and contributes to a significant deterioration in the patient's condition. nine0005
A third of cases of polyhydramnios during pregnancy ends with spontaneous interruptions. The fetal membranes do not withstand the increased pressure of the OPV and are damaged, which is accompanied by the death of the fetus. Polyhydramnios during pregnancy is fraught with an incorrect location of the fetus in the uterus due to the presence of a large space for its movements. Such a violation occurs in about 6-7% of cases. The danger of polyhydramnios during pregnancy also lies in the fact that in every second case it provokes the development of postpartum hemorrhage, premature outflow of amniotic fluid, placental abruption. nine0005
Such a violation occurs in about 6-7% of cases. The danger of polyhydramnios during pregnancy also lies in the fact that in every second case it provokes the development of postpartum hemorrhage, premature outflow of amniotic fluid, placental abruption. nine0005
Polyhydramnios during pregnancy
Causes of polyhydramnios during pregnancy
The pathogenesis of polyhydramnios during pregnancy may consist in two opposite mechanisms: a violation of the secretory activity of the villi of the membranes and a pathological increase in the volume of OPV due to malabsorption. Normally, the absorption of amniotic fluid is carried out through the lungs and intestines of the baby, as well as directly by the amniotic membrane itself. Polyhydramnios during pregnancy can also develop in case of impaired swallowing activity of the fetus. At the same time, a normal volume of OPV is released, but the waters do not have time to go through the absorption cycle (normally, the amniotic fluid is updated every 3 hours, and the child swallows up to 4 liters per day). nine0005
nine0005
So far, it has not been possible to finally find out the causes of polyhydramnios during pregnancy. Doctors believe that the risk of developing obstetric pathology increases significantly if a woman has metabolic disorders, in particular, diabetes. Polyhydramnios during pregnancy often occurs due to diseases of the kidneys, the cardiovascular system. The probability of polyhydramnios increases against the background of the Rhesus conflict. Another common cause of polyhydramnios during pregnancy is infection, and in this case there is a threat of intrauterine infection of the fetus. The most dangerous pathogens are rubella and herpes, toxoplasma and cytomegalovirus. nine0005
Polyhydramnios during pregnancy can be triggered by disorders in the development of the fetus. According to statistics, an obstetric anomaly is more often diagnosed if there are abnormalities associated with chromosomal mutations. Polyhydramnios during pregnancy often occurs in the presence of malformations of the kidneys, intestines, lungs, central nervous system, heart. The risk group for the formation of this pathology includes women who, after conception, suffered viral and bacterial infections, including influenza, SARS. A certain role in the development of polyhydramnios during pregnancy is played by the impact of negative factors: smoking, drug and alcohol use, work in hazardous enterprises, insufficient intake of nutrients. nine0005
The risk group for the formation of this pathology includes women who, after conception, suffered viral and bacterial infections, including influenza, SARS. A certain role in the development of polyhydramnios during pregnancy is played by the impact of negative factors: smoking, drug and alcohol use, work in hazardous enterprises, insufficient intake of nutrients. nine0005
Classification and symptoms of polyhydramnios during pregnancy
Depending on the rate of increase in the volume of amniotic fluid in obstetrics, two types of this condition are distinguished:
- Chronic polyhydramnios during pregnancy is the most favorable variant of the course of the pathology, in which there is a high probability of carrying the fetus before the expected date of birth. In this case, polyhydramnios during pregnancy develops gradually, is accompanied by minor clinical manifestations and responds well to conservative treatment. nine0018
- Acute polyhydramnios during pregnancy is a severe form characterized by a rapid increase in the volume of OPV (in just a few hours).
 More often, such a pathology develops at 16-18 weeks of gestation, leading to a serious condition of the mother and baby. This form causes spontaneous abortion in the later stages, severe congenital anomalies, stillbirth and provokes serious complications on the part of the patient.
More often, such a pathology develops at 16-18 weeks of gestation, leading to a serious condition of the mother and baby. This form causes spontaneous abortion in the later stages, severe congenital anomalies, stillbirth and provokes serious complications on the part of the patient.
The severity of polyhydramnios during pregnancy is determined by the amount of amniotic fluid: mild - OPV volume up to 3 liters, moderate - from 3 to 5 liters, severe - over 5 liters. nine0005
Symptoms of polyhydramnios during pregnancy
Polyhydramnios during pregnancy can manifest itself in different ways, the clinical picture depends on the severity and rate of progression of the pathology. The most characteristic sign of an obstetric anomaly is late toxicosis, accompanied not only by intense bouts of nausea, but also by severe vomiting. In a woman suffering from polyhydramnios during pregnancy, swelling of the anterior abdominal wall is observed, and accumulation of fluid in the subcutaneous fatty tissue of the lower extremities is also possible. Almost every patient has fluctuation - "squishing" of the amniotic fluid, which increases with movement. nine0005
Almost every patient has fluctuation - "squishing" of the amniotic fluid, which increases with movement. nine0005
Polyhydramnios during pregnancy is always accompanied by a significant deterioration in the general condition of the woman. Due to the pressure of the bottom of the uterus on the diaphragm, shortness of breath is noted, sometimes the work of the heart is disturbed, tachycardia is detected. With polyhydramnios, a pregnant woman is worried about pain in the abdomen, lower back and inguinal region, and increased fatigue. Against the background of strong overstretching of tissues, multiple coarse stretch marks appear on the anterior abdominal wall. On the part of the fetus, polyhydramnios during pregnancy is usually accompanied by signs of hypoxia, breech presentation and cord entanglement are also possible due to sufficient space for motor activity. nine0005
Diagnosis of polyhydramnios during pregnancy
An obstetrician-gynecologist can already suspect polyhydramnios during pregnancy on the basis of an objective examination and complaints of the patient. In addition to the deterioration of the general condition of a woman, a characteristic feature is an increase in the standing of the fundus of the uterus, which does not correspond to the gestational age. Also, a significant increase in the circumference of the abdomen indicates polyhydramnios during pregnancy, the indicators sometimes exceed 100-120 cm. Palpation can determine the pathological position of the fetus in the uterine cavity - oblique, transverse or pelvic. If polyhydramnios is suspected during pregnancy, a woman is assigned laboratory diagnostics: general blood and urine tests, a smear from the genital tract for microflora in order to detect infections. nine0005
In addition to the deterioration of the general condition of a woman, a characteristic feature is an increase in the standing of the fundus of the uterus, which does not correspond to the gestational age. Also, a significant increase in the circumference of the abdomen indicates polyhydramnios during pregnancy, the indicators sometimes exceed 100-120 cm. Palpation can determine the pathological position of the fetus in the uterine cavity - oblique, transverse or pelvic. If polyhydramnios is suspected during pregnancy, a woman is assigned laboratory diagnostics: general blood and urine tests, a smear from the genital tract for microflora in order to detect infections. nine0005
If polyhydramnios during pregnancy is caused by a Rh conflict, a study is indicated to determine the amount of antibodies. The diagnosis is finally established after an ultrasound. During the procedure, it is possible to measure the amount of OPV, as well as to assess the functionality of the placenta and the well-being of the fetus. In rare cases, amniocentesis is performed. Polyhydramnios during pregnancy requires careful monitoring of the baby. For this purpose, CTG and uteroplacental dopplerography are performed, which allow assessing the degree of hypoxia, heart function, physical activity, the level of blood flow in the vessels of the umbilical cord and determining further medical tactics. nine0005
In rare cases, amniocentesis is performed. Polyhydramnios during pregnancy requires careful monitoring of the baby. For this purpose, CTG and uteroplacental dopplerography are performed, which allow assessing the degree of hypoxia, heart function, physical activity, the level of blood flow in the vessels of the umbilical cord and determining further medical tactics. nine0005
Treatment of polyhydramnios during pregnancy
Polyhydramnios during pregnancy requires hospitalization in an obstetric hospital and careful monitoring of the condition of the woman and the fetus. Complete rest is prescribed, it is important to exclude stress factors and physical activity. Drug treatment of polyhydramnios during pregnancy depends on the cause of this condition. Be sure to carry out the therapy of the underlying disease, which contributed to the development of a pathological increase in the volume of OPV. If the etiology of polyhydramnios during pregnancy is not established, the classical scheme is used - antibiotic therapy in order to prevent the introduction of intrauterine infection. nine0005
nine0005
Conservative treatment of polyhydramnios during pregnancy also involves the use of drugs to improve uteroplacental blood flow, vitamin complexes, diuretic drugs. In the case of acute polyhydramnios during pregnancy and a significant deterioration in the patient's condition, associated with a threat to her life, depending on the period of embryogenesis, interruption or premature delivery by caesarean section is indicated. If a conservative approach gives a positive trend, pregnancy management is continued until 37-38 weeks. nine0005
Delivery in the case of polyhydramnios during pregnancy is carried out using a planned caesarean section. It is important to prevent spontaneous opening of the fetal bladder. Due to the large volume of amniotic fluid, its rapid outflow can lead to the loss of small parts of the fetus, as well as weakness of labor. If a decision is made to perform a natural birth against the background of polyhydramnios during pregnancy, an amniotomy is required. This further stimulates contractions. nine0005
This further stimulates contractions. nine0005
Prognosis and prevention of polyhydramnios during pregnancy
In general, the prognosis for polyhydramnios during pregnancy is favorable. Early diagnosis and treatment make it possible to prolong gestation until the expected date of birth and keep the baby healthy. However, this condition is often complicated by birth and postpartum hemorrhage, intrauterine hypoxia, and premature placental abruption. Acute polyhydramnios during pregnancy in most cases leads to fetal death. To prevent the development of obstetric anomalies, conception should be planned, foci of infection should be treated in a timely manner and a consultation with an obstetrician-gynecologist should be made. Prevention of oligohydramnios during pregnancy also consists in moderate physical activity and proper nutrition. A woman during the gestation period should avoid stress and bad habits, be in the fresh air a lot. nine0005
You can share your medical history, what helped you in the treatment of polyhydramnios during pregnancy.