Expressing milk during pregnancy
Antenatal expression of colostrum - reasons for, when and how
Antenatal expression of colostrum - reasons for, when and how | Pregnancy Birth and Baby beginning of content5-minute read
Listen
During pregnancy, the breasts produce their first milk, known as colostrum. Colostrum is high in antibodies and protective substances that help to support a newborn baby's immunity. Although not much colostrum is produced, it is very high in energy, protein and fat. Colostrum is also easy for newborns to digest.
There can be benefits to expressing and storing colostrum during pregnancy in case it is needed after birth. If there is a risk of premature birth or of your baby having feeding problems, the person providing your maternity care may recommend you express and store some colostrum.
What is colostrum?
Colostrum is a type of early breast milk, produced by the breasts from around 20 weeks of pregnancy until the first few days after birth. Colostrum is a thick, sticky, yellowish liquid. It can leak from the breasts onto the nipples and cause yellow crusts to form. Sometimes colostrum leaks and absorbent nursing pads need to be worn.
When does colostrum appear?
Many pregnant women notice they are producing colostrum earlier than 20 weeks, especially if they’ve been pregnant before. It’s not always obvious that colostrum is being produced until the woman checks.
What are the benefits of expressing colostrum in pregnancy?
There are several benefits from expressing during pregnancy, including:
- helping to support successful breastfeeding after birth — women who express are generally motivated to do all they can to increase their likelihood of exclusively breastfeeding their baby
- building a supply of colostrum is useful in case the baby needs extra feeds and avoids offering formula
- managing potential feeding problems relating to prematurity or a congenital condition
- managing feeds for babies of diabetic mothers where there is a risk of having problems maintaining a normal blood sugar level
- having a store of colostrum if the baby is likely to need special care and is likely to be separated from their mother
Why might there be a low supply of breast milk?
Sometimes there are reasons why a mother’s breasts do not produce as much milk as their baby needs. Storing a small supply of colostrum means the baby can have access to extra kilojoules. These reasons include:
Storing a small supply of colostrum means the baby can have access to extra kilojoules. These reasons include:
- breast surgery or problems with breast growth during pregnancy
- some medical conditions, such as multiple sclerosis or polycystic ovarian syndrome
- a history of having low milk supply
Are there any reasons not to express colostrum during pregnancy?
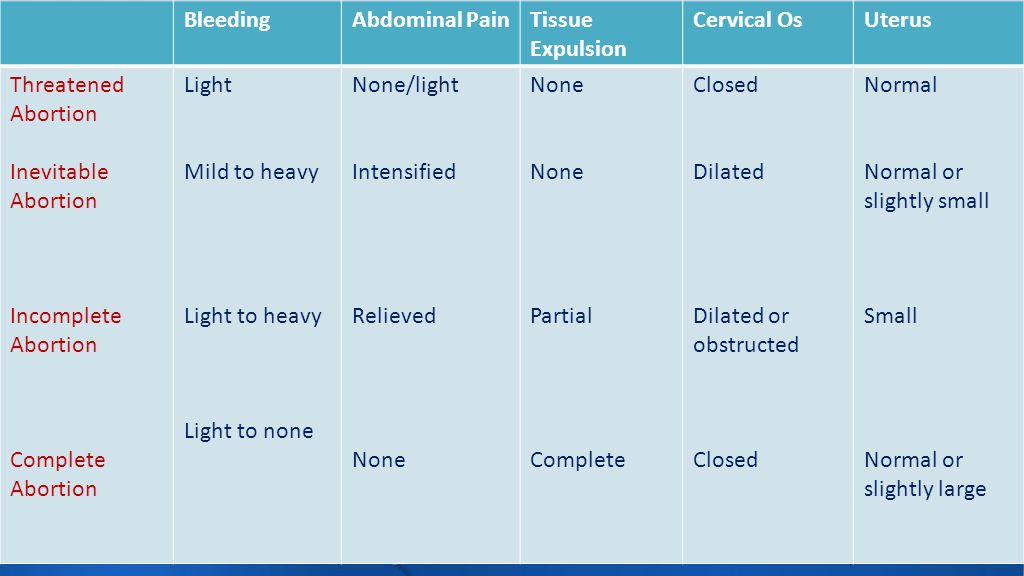
Not all women are keen or able to breastfeed. Some choose to express colostrum and offer this as well as formula after their baby is born. Although there are benefits in expressing colostrum during pregnancy, there are times when it’s not recommended. There is a risk of premature labour by stimulating the breasts.
Don’t express your breasts if you:
- are at risk of, or have had, threatened premature labour
- have had a cervical suture inserted, or been diagnosed with cervical incompetence
- have experienced bleeding during your pregnancy>
- have been diagnosed with placenta praevia
- have been advised by your maternity care provider not to
- cannot store colostrum safely and hygienically
When and how to express your colostrum
Pick a time when you’re relaxed and feeling calm.
- Wash your hands with soap and water and dry well.
- Using your thumb on top of your breast and your forefingers underneath, gently press your fingers towards your chest.
- Compress the breast tissue, hold briefly and then release. Try not to squeeze or pinch the nipple.
- Collect the colostrum in either a sterile syringe or a clean container.
- Express each breast twice during each expression. You can collect colostrum twice a day in each syringe or container. Between expressions, store the colostrum in the fridge. Label with the date, cap the syringe and put in a plastic bag and into the freezer.
Aim to express 2 to 3 times each day from around 36 weeks of pregnancy. Start gently and slowly, eventually building up to 3 to 5 minutes of expressing on each breast twice each day.
How to store colostrum
| Room temperature (26° C or lower) | Fridge (4° C or lower) | Freezer |
|
|
|
Top 5 tips for expressing colostrum
- Start expressing at around 36 weeks into your pregnancy.
 Stop if at any time you start to feel contractions or vaginal bleeding.
Stop if at any time you start to feel contractions or vaginal bleeding. - Remember that any amount of colostrum will be beneficial to your baby. The amount of colostrum women can express varies widely while they are pregnant.
- Be patient as you learn how to express and store the colostrum safely.
- Take the clearly labelled and frozen colostrum with you (in an esky or cooler bag) when you have your baby.
- Only use your hand, not a pump to express your colostrum.
The person who is providing your maternity care — such as your doctor or midwife — will be able to give you more advice about what’s right for you. Some pregnancy-related conditions increase the risk of premature labour and it’s important not to express colostrum if you’re at risk of having your baby early.
Sources:
Mater Mother's Hospital (Antenatal expression of colostrum), National Health and Medical Research Council (Infant Feeding Guidelines Information for Health Workers), Women and Newborn Health Service (Breastfeeding – antenatal expression of colostrum for women with Diabetes), Queensland Government (Expressing breastmilk)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2021
Back To Top
Related pages
- Storing expressed breast milk
- Expressing and storing breast milk
- Breastfeeding your baby
Need more information?
Antenatal expression of colostrum | Australian Breastfeeding Association
Antenatal expressing of colostrum is the hand expression and collection of colostrum during pregnancy. Expressed colostrum is collected and frozen and used to feed a baby after birth, if required.Colostrum
Read more on Australian Breastfeeding Association website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Everything You Need to Know About Expressing and Pumping During Pregnancy
In recent years, expressing during pregnancy has become an increasingly popular topic. Just type in antenatal hand expression into Google and you will see 160,000 results pop up! No wonder so many mums-to-be are talking about it or confused about whether they should be doing it...
Share this content
Some Background About the Way that Breasts Make Milk During Pregnancy
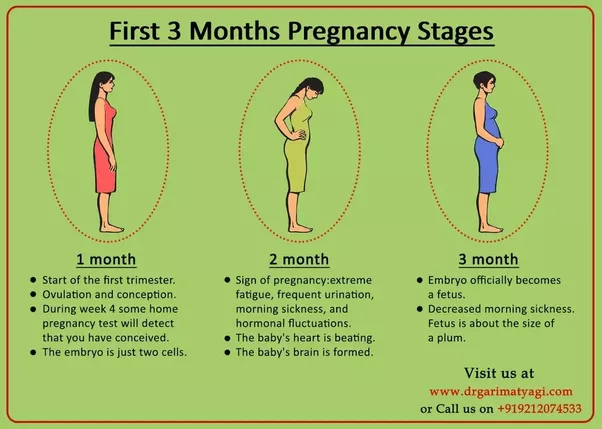
Your breasts start to produce milk (colostrum) from around 16-20 weeks of pregnancy. This is totally normal.
This is totally normal.
Some women will notice this instantly as their nipples start leaking milk. For other women, this will come as a surprise as they have never seen a drop come out.
Do not panic! We are all different and all a variation of “normal.”
But from around the middle to end of the second trimester your breasts can actually make milk; whether you see it or not!
The breasts only make tiny quantities of milk at this stage, as the hormones of pregnancy stop the milk cells from being able to make large volumes of milk until both your baby and the placenta are born.
Why is Everyone Talking About Expressing Milk During Pregnancy?
Research showed an increased risk in a baby developing diabetes later on in life if they were fed formula milk and their mother had diabetes in pregnancy. Babies born from mothers who have diabetes during pregnancy are more likely to have low blood sugar levels soon after the birth. This is known as hypoglycaemia.
Hypoglycaemia can potentially affect whether the baby is able to feed at first. If you’ve ever had low blood sugar you will know that it makes you feel really low on energy, tired, and shaky, among other things. Now, imagine a newborn baby trying to breastfeed when they feel like this, not easy!
And, because a baby may not be able to breastfeed to naturally increase his blood sugar level, the midwives or nurses would often have given the baby formula milk instead.
In order to stop giving so many babies formula milk for low blood sugar levels, midwives have started to advise some mothers to hand express their milk during pregnancy, around 35-36 weeks of pregnancy.
Mothers were instructed to expressed anywhere from twice to six times per day and to collect the milk in tiny syringes and store the milk in the freezer. They would then take this antenatally expressed frozen milk into the hospital when they went into labour. This extra colostrum could then be used instead of formula milk if the baby had low blood sugar levels.
A Few Safety Questions with Antenatal Hand Expression
Since then, this practice has gotten more and more common, with many women being advised to express their milk in pregnancy for lots of different reasons.
Until recently, we have not had any good scientific research which has shown whether this practice is advised and safe. There was a small concern that expressing during pregnancy could lead to preterm labour.
When our babies breastfeed or we express we produce a hormone called oxytocin, which helps muscles contract around the milk cells and push the milk down the ducts to the nipple and baby/pump. This is the same hormone which also makes our uterus contract during labour.
Scientific Research Investigating Antenatal Expression
In 2017, the first and only randomised control trial was published, which investigated whether antenatal expression for women with diabetes in pregnancy is safe.
The researchers stated that the “research showed that not only is expressing breast milk before birth safe, but it increased the proportion of mothers who exclusively breast milk fed their child within the first 24 hours of birth and up to seven days after birth. ”
”
Please note: this research only looked at women with healthy pregnancies, who were hand expressing from 36 weeks of pregnancy (not earlier) and only for two times each day (not more).
Using a Pump During Pregnancy
The research and technique of antenatal expression has only ever been done with women using their hands to express, not with a pump (whether a hand-pump or an electric pump). Therefore, it is not advised to use a pump to antenatally express milk.
If you are pregnant and still breastfeeding or expressing for another child, pumping should not cause preterm labour in a healthy pregnancy. Many mums continue to provide breastmilk for their child while pregnant with their next one.
If you have any concerns it is always best to discuss this with your health care provider.
In Summary
Always discuss antenatal hand expression with your midwife or obstetrician first to check if it is a good option for you and your pregnancy.
Never use a pump during pregnancy.
If you have diabetes, discuss this further with your midwife or obstetrician to create a plan for you and your baby.
If you have been advised to antenatally express your milk, your health care provider will show you how to hand express and provide you with an instruction and collection kit.
Do you have any breastfeeding questions? How would you describe your own breastfeeding journey? Let’s have a chat here or on our Medela Australia Facebook page.
Antenatal (prenatal) colostrum expression
Patient information leaflet * .
Colostrum is a fatty, nutrient-rich substance that is excellent for nourishing and protecting your baby from infections during the first days of life. It is especially rich in immunological factors that promote the growth and development of the infant's immune system and protect it from allergies and various diseases. Colostrum also helps the newborn eliminate meconium (original feces), which helps prevent jaundice.
Colostrum also helps the newborn eliminate meconium (original feces), which helps prevent jaundice.
This first milk begins to be produced at 16-20 weeks of gestation. Some women notice leakage of milk during pregnancy, while others may not. In both cases, this is normal and does not affect a woman's ability to breastfeed successfully.
The importance of exclusive breastfeeding for all newborns has been proven in many studies. Some babies may have difficulty breastfeeding as well as blood sugar regulation in the first few days after birth. By hand expressing and preserving colostrum during pregnancy, your baby will be able to get your milk despite the difficulties. Research data show that colostrum is able to stabilize blood sugar levels in newborns significantly better than formula.
You can start expressing colostrum from the 36th week of pregnancy, although if you notice milk leakage earlier, you can collect it in a sterile syringe. You can discuss this with your midwife or other healthcare provider. They can provide you with tools and guidance to start collecting colostrum.
They can provide you with tools and guidance to start collecting colostrum.
Benefits of collecting colostrum during pregnancy.
If women start harvesting colostrum during pregnancy, studies show that they:
- gain more confidence in how their breasts work even before the baby is born reach “full production” of milk faster
- increase their confidence that they will be able to breastfeed their baby manual pumping skills.
Most women can express during pregnancy, although there are several groups of mothers and children for whom antenatal colostrum expression may be particularly beneficial:
- Infants at risk for hypoglycaemia or possible difficulty sucking
- Children of mothers with diabetes mellitus
- Very small and low birth weight children
cleft lip or palate, or other congenital anomalies such as Down's Syndrome- when it is known during pregnancy that the baby will need special care in the neonatal unit
- Twins or triplets.
There are also women who, due to their common medical or gynecological history, will find it difficult to exclusively breastfeed their babies. Others suffer from certain diseases, such as multiple sclerosis, for which breastfeeding is very beneficial:
- any form of diabetes
- polycystic ovary syndrome
- breast hypoplasia
- previous breast surgery
planned caesarean section
In mothers with diabetes and allergies, as well as a family history of dairy intolerance, inflammatory bowel disease or diabetes, children may also have these diseases more often if they are fed artificial protein-based formulas from the first days of life cow's milk.
It is especially important for mothers with diabetes to completely avoid the use of artificial formulas, or at least not to use them until the baby is 6 months old.
Women with gestational diabetes are less likely to develop the disease after childbirth if they are breastfeeding.
Women with diabetes should monitor their blood sugar levels especially if they express colostrum before giving birth. They may need to adjust their insulin doses and change their diet.
Are there women who should not express colostrum during pregnancy?
There is no scientific evidence that daily hand expression of colostrum activates labor in women who are not at risk for preterm birth.
However, we would advise some women not to actively express colostrum until a sufficient pregnancy is reached: multiple births before 36/40 weeks
- women with cervical sutures to prevent preterm labor
If you feel uterine contractions during pumping, you should stop the procedure. If contractions continue, contact your midwife.
How can I express colostrum during pregnancy?
Preparation.
To prevent cross-infection, please:
- wash your hands thoroughly before pumping
- wash your breasts no more than once a day (avoid using detergents that can irritate or dry out the skin on the nipples, causing soreness ).
Prepare a sterile milk collection container, such as a cup, bottle, wide-mouth container, or syringe (may be best for collecting small amounts of colostrum with minimal wastage). Activation of the release of OXYTOCIN (milk ejection reflex) can facilitate the outflow of milk. Find a quiet, secluded place where you can relax properly. You can gently massage your entire breast before pumping (you can see some of the massage techniques in the picture), be careful not to slide your fingers over the breast, as this can damage the skin. You can gently roll the nipple between your index and thumb. Some women find it helpful to put a warm diaper (soaked in warm water) over their breasts before pumping.
Make gentle circular motions with your fingertips.
Gently roll your clenched fist towards the nipple.
Locate the milk ducts.
Place your thumb on top of your chest with your index finger opposite it underneath. Both fingers are placed as far away from the base of the nipple as you can comfortably do. Gently “walk” your fingers along the chest until you find structures that feel different to the touch.
Gently “walk” your fingers along the chest until you find structures that feel different to the touch.
This means that you have felt the milk ducts (usually they are located 2-3 cm from the nipple).
Expression positions.
It can help if you lean forward slightly. Place your thumb and forefinger in the place where you found changes in the tissue of the gland. The thumb should be at 12 o'clock and the index finger at 6 o'clock, as shown in the picture (your hand is in a C-shape), covering the chest.
Pumping .
Without moving the thumb and forefinger, gently press the chest towards the chest (if the chest is large, it should be lifted first). Without releasing the pressure, roll your fingers towards each other to draw the milk out of the ducts. After that, you should reduce the pressure to allow the ducts to refill with milk. At first, you will be able to get only a few drops, but with practice, the amount of colostrum will increase. You can move your hand in a circle, changing the position of your thumb and forefinger, or change your hand, if necessary, to express milk from the entire breast. Collect drops of your colostrum in a sterile syringe or capped cup if more. You may find it easier to deal with this if your husband or other family members help you. Write your name, date of delivery, time and date of pumping on each syringe. Colostrum is usually produced in small amounts, so don't expect to be able to express a lot right away, although you might get lucky! You can make just 1 or 2 servings, but don't despair...every drop counts, and the more often you pump, the more likely you are to increase your milk production. Hand pumping is generally more effective than using a manual or electric breast pump.
You can move your hand in a circle, changing the position of your thumb and forefinger, or change your hand, if necessary, to express milk from the entire breast. Collect drops of your colostrum in a sterile syringe or capped cup if more. You may find it easier to deal with this if your husband or other family members help you. Write your name, date of delivery, time and date of pumping on each syringe. Colostrum is usually produced in small amounts, so don't expect to be able to express a lot right away, although you might get lucky! You can make just 1 or 2 servings, but don't despair...every drop counts, and the more often you pump, the more likely you are to increase your milk production. Hand pumping is generally more effective than using a manual or electric breast pump.
Colostrum can vary greatly in color from dark orange/brown, yellow/green to pale/clear. Don't worry if your colostrum changes color or consistency after a few pumps. This is fine. Rest assured, the colostrum has not "run out". You continue to produce colostrum until the milk "comes in" (about 3 days after your baby is born). You can pump as often as is comfortable for you.
You continue to produce colostrum until the milk "comes in" (about 3 days after your baby is born). You can pump as often as is comfortable for you.
What if colostrum is not produced?
Don't panic! For some mothers, pumping is not easy. Keep trying, it may take a few days for you to see the first drops of colostrum. If you're ready to continue, try to pump every day. Remember that it is not necessary to pump during pregnancy, however, if you do, it can be very beneficial. Be sure that when your baby is born, you will definitely be able to get colostrum.
Expression Assistance Manual:
- try pumping after a hot bath or shower
- put warm diapers on your chest to improve circulation
- relax!
- Gently massage your breasts before pumping
- Have your baby's ultrasound scan handy
What do you need?
You can ask your midwife for some sterile syringes for your first colostrum. Then you can buy them at a pharmacy or online. 1ml syringes work best.
Then you can buy them at a pharmacy or online. 1ml syringes work best.
How much colostrum should be collected?
As many as you want and can. Remember that a newborn's stomach is the size of a small balloon.
Colostrum storage.
In addition to preparing colostrum for your baby, there are other benefits to expressing your first milk. Many women feel more relaxed and secure knowing they have an "extra reserve" of colostrum in case their newborn needs it.
Put the syringe you used to collect the colostrum back into the package and place it in an airtight plastic container (such as a lunch box or freezer container). Freeze this serving of colostrum immediately.
Transportation of colostrum.
It is best to freeze the colostrum after you have collected it at home and take it to the hospital when needed. Use a cooler bag with ice when transporting colostrum to the hospital and ask medical staff to place it in a special refrigerator as soon as possible after delivery. Once thawed, colostrum should be used within 12 hours, so to avoid wasting colostrum when it is thawed but not used, it is best to defrost a few syringes for each feed.
Once thawed, colostrum should be used within 12 hours, so to avoid wasting colostrum when it is thawed but not used, it is best to defrost a few syringes for each feed.
When the baby is born
Immediately after birth, continuous skin-to-skin contact between mother and baby should be established as early as possible to encourage initiation of breastfeeding (usually within the first 90 minutes after delivery) . Ideally, your baby will suckle well at the breast soon after birth and will latch on frequently, so you won't need the expressed colostrum! However, some babies need regular supplements to keep their blood sugar levels stable, or the baby has some difficulty suckling. In this case, you will be provided with ongoing support to help resolve the difficulties, and in this situation, you can use pre-prepared colostrum. The medical staff will teach you how to feed your newborn with colostrum. You also need to take care to continue expressing colostrum regularly until your baby is able to breastfeed effectively in order to get the milk production back on track and provide the baby with it. We hope you enjoy expressing colostrum during pregnancy, as it will give you extra confidence and an invaluable reserve if you encounter difficulties in establishing breastfeeding. We hope you now know more about how your breasts work and how pumping during pregnancy will help you be more confident when you start breastfeeding your baby!
We hope you enjoy expressing colostrum during pregnancy, as it will give you extra confidence and an invaluable reserve if you encounter difficulties in establishing breastfeeding. We hope you now know more about how your breasts work and how pumping during pregnancy will help you be more confident when you start breastfeeding your baby!
Useful Contact Numbers Breastfeeding Midwife 01296 315799 Community Midwives Office (SMH) 01296 316120 Community Midwives Office (WH) 01494 425172
patients. If you have any comments or suggestions regarding this booklet, please contact us:
Head of Midwifery Women & Children’s Division Buckinghamshire Healthcare NHS Trust Stoke Mandeville Hospital Mandeville Road Aylesbury Buckinghamshire HP21 8AL
How can I help reduce hospital acquired infections?
Infection control is an important part of the well-being of our patients, which is why we have developed local infection control procedures. Frequent hand washing is an effective way to prevent the spread of infection. We ask you and your visitors to use hand sanitizer, which you can find before entering each room, before and after visiting the patient. In some cases, hands need to be washed in the sink with soap and water instead of just hand sanitizer. The hospital staff will let you know if additional hand sanitization is needed.
We ask you and your visitors to use hand sanitizer, which you can find before entering each room, before and after visiting the patient. In some cases, hands need to be washed in the sink with soap and water instead of just hand sanitizer. The hospital staff will let you know if additional hand sanitization is needed.
www.buckshealthcare.nhs.uk Follow us on Twitter @buckshealthcare
Author: L. Randell
Publication date: December 2016
Reissue date: December 2018
9 Leaflet code: n/a Version00 5002: 1
Translation: Tatyana Mamontova
*Attention! Antenatal (prenatal) expression of colostrum should be carried out only when indicated. If you think you need it, be sure to check with a breastfeeding support leader or lactation consultant beforehand
Pumping when the mother needs to go away | Philips Avent
Search Support iconKeywords for searching
Home ›› Milk Expression of Mom from the baby
Home Milk during temporary height of the mother from the baby
↑ Vering
9000
Even if you don't have the opportunity to be near your baby, you can be sure that by pumping, he will receive all the necessary nutrients from breast milk. Perhaps you are already using a breast pump to continue breastfeeding when you go to work, or you just want to have more free time between feedings.
Perhaps you are already using a breast pump to continue breastfeeding when you go to work, or you just want to have more free time between feedings.
3 Philips Avent products to help you pump and store milk comfortably:
Not sure when to start expressing milk or when to start using a breast pump? Don't worry, we've put together a quick guide to help you learn how to express milk and learn about the benefits of using a breast pump. We'll also give you tips on how to express your milk when you're away from home, how to keep it adequate, and how to store it safely.
When should I start expressing milk?
Most women begin to express milk after six months, but there are circumstances that force them to do so sooner.
If you intend to express milk as early as possible, the answer to the question “When can I start expressing milk?” will be: "A few hours after birth." Some mothers find that expressing milk is effective at a very early stage, especially if the baby has latch-on problems, as pumping improves the flow of milk to the breast.
Other mothers start pumping after breastfeeding is established because they want someone in the household to help with feeds while they are away or with feeds after they return to work.
There are no specific rules about when to start pumping, so you can do whatever works best for you. Whatever your needs, you can pump to make your schedule less dependent on feedings.
How to express breast milk: general questions
How long should I express milk? How much milk do I need to express? What equipment do I need for this? Every mother has questions about this topic, however, once she starts expressing milk, she easily adapts to this process.
Most mothers find a breast pump to be the easiest way to express breast milk. The principle of operation of different breast pumps may vary slightly, so read the instructions for use before using the device. Remember that it can take 1-2 minutes for milk to come out of your breast during pumping, so don't worry if you don't see it right away!
Not sure how long to express milk? If you are not in a hurry, try to express milk until you feel that your chest is empty. Due to the individual characteristics of each woman, the pumping time will be different.
Due to the individual characteristics of each woman, the pumping time will be different.
The amount of milk expressed will depend on when you last breastfed and how long you use the pump and are accustomed to using it. Even your internal state and time of day can affect the amount of milk. If you have problems with lactation, check out our tips for increasing your milk supply. Generally, the best time to express is in the morning. During sleep, there is an increase in the level of hormones responsible for the production of milk.
Should breastfeeding be combined with pumping? Wait about an hour between pumping and the next feeding. So you will be sure that the baby will have enough milk! Feed your baby as much as it takes to keep him full and happy. Use a breast pump to fully express milk from your breasts and save excess milk.
How to Express Breast Milk: Practical Tips
Whether you are expressing milk at home (for a night feed) or at work, there are a few key things to keep in mind to help you.
1. Plan ahead. If you have to leave your baby, start using a breast pump a few weeks in advance. This way you will store enough milk for your baby and get used to using a breast pump.
2. Be ready. You may be aware of the so-called "oxytocin reflex", which stimulates the flow of milk due to the release of the hormone oxytocin. Oxytocin increases the secretion of breast milk that can be expressed. The production of the hormone can be caused in many ways, even just by looking at the child. Therefore, many mothers find it effective to look at a photo of their baby while pumping while away from home. After you finish pumping, you can also use bra pads to keep your breasts dry and protect your clothes from milk stains.
3.![]() Make yourself comfortable. The more comfortable you feel, the easier it will be to express milk. Find a quiet, private place and feel free to change the lighting and music to your liking. It is helpful to find a seat with good support so that you can sit comfortably with the pump in front of you.
Make yourself comfortable. The more comfortable you feel, the easier it will be to express milk. Find a quiet, private place and feel free to change the lighting and music to your liking. It is helpful to find a seat with good support so that you can sit comfortably with the pump in front of you.
4. Express as many times as you would like to breastfeed your baby. To maintain the required supply of milk, express it as often as you normally feed your baby. Thus, if the baby usually has three feedings during your absence, then you need to express milk at least three times.
How to choose the best breast pump for expressing milk
There are several different types of breast pumps, each with its own advantages. Choose the one that will help you feel comfortable in your daily life. Perhaps you prefer to have a device that is designed to be used on the go? Or do you need a breast pump that will allow you to express milk quickly?
Storage and preparation of milk after pumping
After you have expressed your milk, remember to freeze it or refrigerate it. Then, before feeding the baby, it must be thawed and warmed up. Here are some tips on how to store breast milk:
Then, before feeding the baby, it must be thawed and warmed up. Here are some tips on how to store breast milk:
- Use sterile milk storage containers or freezer bags to collect and store milk.
- Do not fill the container to the upper limit, because. when frozen, breast milk "expands", the optimal portion for storage is 60-120 ml.
- Label the container with the pumping date or write the pumping date on the container with a permanent marker.
- Store milk in the refrigerator at 2-4°C for up to 24 hours.
- After cooling the expressed milk in the refrigerator for 0.5 hours, the milk can be frozen in the freezer and stored there for 3 months.
- Place the milk closer to the back of the refrigerator or freezer rather than in the door to keep the milk at a constant temperature.
- Thawed milk placed in the refrigerator should be used within 24 hours.
- Do not refreeze thawed milk.
- Transport milk in an insulated container with an ice pack.

Use these tips to prepare your expressed milk for breastfeeding:
- Thaw or warm breast milk under running warm water, in a bain-marie, or with a bottle warmer.
- Do not use a microwave oven to heat milk.
- Do not heat milk to boiling point.
- Shake the milk bottle before feeding until smooth.
- Check milk temperature before feeding. The most optimal temperature is the average between body temperature and room temperature. To check the temperature of milk, you can drop it on your skin.
Advice for first-time moms
If you are just starting to express milk, remember that this process may not be entirely comfortable. The more relaxed you are, the easier it will be to express milk. Sometimes this will be difficult to do, for example if you are trying to express milk during a busy work day or in an unfamiliar place; therefore, it is necessary to practice well at home and show patience.