Elective c section reasons
Planned or elective caesarean | Pregnancy Birth and Baby
Planned or elective caesarean | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a planned or elective caesarean?
A caesarean section (C-section) is an operation to deliver a baby through a cut in your tummy.
Caesarean sections may be planned before the birth. This is known as an elective caesarean. This may happen if there are pregnancy complications that prevent your baby being born by vaginal birth. In some cases, an elective caesarean is requested by the mother.
There are some important things to think about if you plan to or want to have a caesarean.
Why have a planned caesarean?
About 3 out of every 5 caesarean births in Australia are planned (elective).
Sometimes health problems or pregnancy complications mean that a caesarean birth would be safer than a vaginal birth.
Your doctor might recommend a planned, or elective, caesarean section for the following reasons:
- you have already had one or more caesarean sections
- your baby is in an abnormal position (such as bottom or feet first, or lying sideways)
- you are carrying more than one baby (for example, a twin pregnancy)
- your placenta is covering all or part the cervix (the opening to the uterus) - this is called placenta praevia
- you have a health problem, such as a heart problem, high blood pressure or fibroids (growths in the uterus)
- you have an infection that could be passed to your baby during a vaginal birth
- you or your baby have other medical complications
Some women may prefer a caesarean section to a vaginal birth for non-medical reasons. There are some risks and benefits to this decision for both mother and baby. It can also affect future pregnancies.
It can also affect future pregnancies.
You have a right to be involved in making decisions about the type of birth you will have. If you are having a planned caesarean section, talk with your doctor about the risks and benefits.
A caesarean section is major surgery. Complications are rare but can be serious. It is important to make an informed decision. So, make sure you ask questions and discuss concerns with your doctor and midwife.
How do I prepare for a planned caesarean?
Your doctor or midwife will arrange any tests and medical reviews that may be needed before your surgery. You will be asked to sign a consent form for the operation.
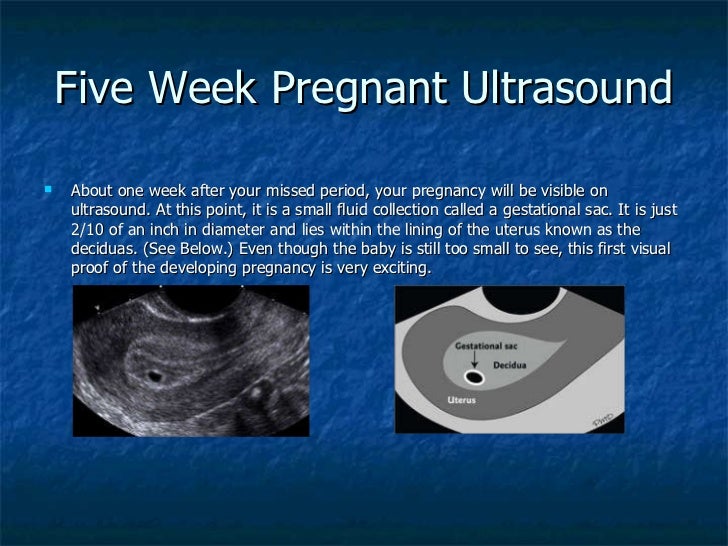
The timing of your caesarean birth will depend on your health, your baby’s health and the caesarean team’s schedule. Where possible, planned caesarean sections are often done at around 39 weeks. If there are problems or if you are having multiple babies (for example, twins), your caesarean may be done earlier than this.
Remember to take a bag for your stay in hospital, containing the things you and your baby will need. If you would like to take photos of the birth, ask your doctor whether it is OK for your partner or support person to bring a camera.
What will happen before a caesarean?
You will need to stop eating and drinking for about 6 hours before the operation.
Before the surgery, your pubic hair may be shaved and your tummy will need to be cleaned with antiseptic wash. You will be fitted with compression stockings on your legs. These help to reduce the risk of blood clots in your legs.
You will then be prepared for the anaesthetic. Many women having an elective caesarean will have an epidural anaesthetic or spinal block.
You will have intravenous (IV) lines put into your arm to give you fluids and medicines.
A doctor will place a catheter (a thin flexible tube) into your bladder. This will likely be removed once sensation returns to your legs and you can sit out of bed and walk.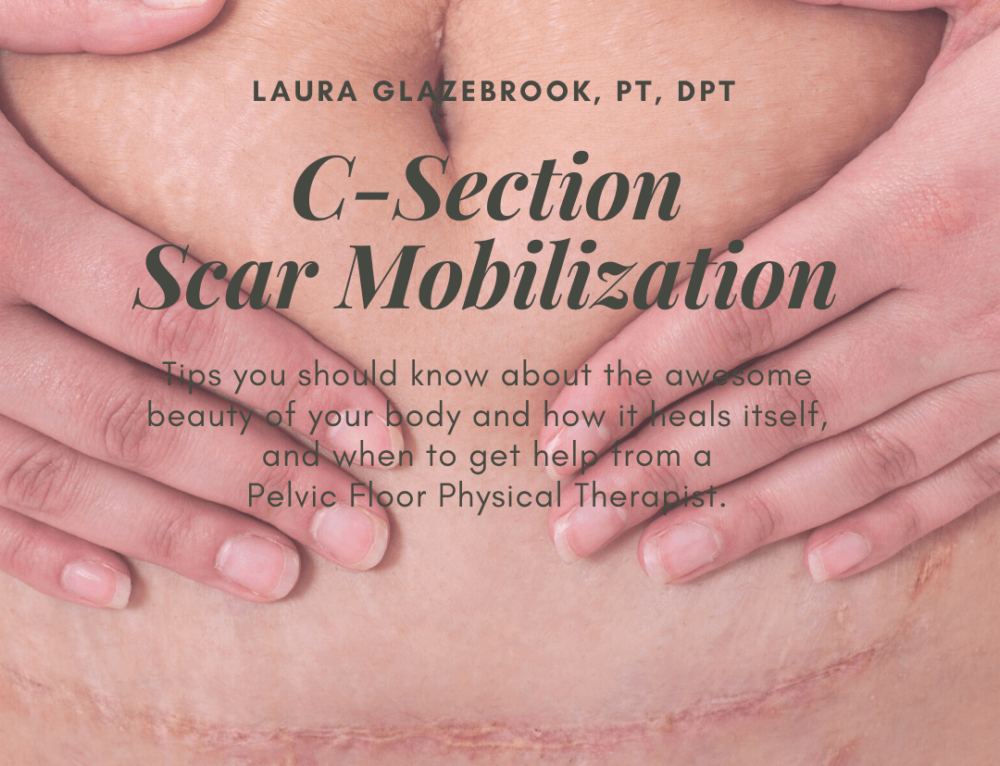
What happens during and after a caesarean?
A screen is usually put across your chest so you cannot see what is happening. Some doctors now offer a ‘maternal assisted caesarean section’ so mothers can help deliver their baby. This is under the guidance of the doctor and is not always possible.
Your partner or support person can usually be with you during your planned caesarean birth. You will also usually have a midwife that stays with you. They will look after you and your baby in the operating theatre and recovery area.
If your baby is well, it is a good idea for you or your partner or support person to hold them straight away after the birth. Skin to skin contact keeps the baby warm and helps with bonding.
If you are choosing to breastfeed, your midwife may be able to assist you to do so once in the recovery room.
Remember that you will need time to recover after a caesarean. If possible, plan to have plenty of help at home in the weeks after the surgery.
What happens if I go into labour first?
About 1 in 10 women whose planned caesareans are scheduled for 39 weeks will go into labour first. That means their waters break or their contractions start. If this happens, you will have an emergency rather than a planned caesarean.
Call your hospital's maternity unit or delivery suite immediately if you are booked to have a planned caesarean and you go into labour.
Sources:
The Royal Women's Hospital (Caesarean birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Caesarean section), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Timing of elective caesarean section at term)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2022
Back To Top
Related pages
- Vaginal birth after caesarean (VBAC)
- Recovery after a caesarean
- Emergency caesarean
Need more information?
Vaginal birth after caesarean (VBAC)
If you've delivered a baby by caesarean (C-section), you may have a choice with your next pregnancy - a vaginal birth after caesarean (VBAC) or a planned (elective) caesarean.
Read more on Pregnancy, Birth & Baby website
Vaginal Birth after Caesarean Section
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Emergency caesarean
Sometimes birth doesn't go as expected. If you or your baby are at risk, there might be a need to do an emergency caesarean.
Read more on Pregnancy, Birth & Baby website
Having a caesarean
A caesarean is an operation to deliver a baby through a cut in the abdomen (tummy) and uterus (womb). It might be planned (elective) or an emergency procedure.
Read more on Pregnancy, Birth & Baby website
Caesarean section - Better Health Channel
A caesarean section is usually performed when it is safer for the mother or the baby than a vaginal birth.
Read more on Better Health Channel website
Recovery after a caesarean
Recovery after a caesarean section - whether it's an emergency or planned - will take several weeks. Find out what to expect after you have had your baby.
Read more on Pregnancy, Birth & Baby website
Elective caesarean birth: what to expect | Raising Children Network
Having a planned or elective caesarean birth? As with any major surgery, it helps to know what to expect during a caesarean section. Our guide explains.
Read more on raisingchildren.net.au website
Caesarean Section - Birth Trauma
Being abdominal surgery, pain in the early months is very common after a caesarean section (C-section) and needs to be managed with rest, pain relief, and
Read more on Australasian Birth Trauma Association website
Your Next Birth after Caesarean Section - Maternal, child and family health
Consumer brochure with information on birth options available to women planning their next birth after caesarean section.
Read more on NSW Health website
VBAC: vaginal birth after caesarean | Raising Children Network
For many women, vaginal birth after caesarean – VBAC – is a safe and positive way to have a baby. Our guide explains VBAC’s possible benefits and risks.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Reasons for a C-Section: Medical and Elective
One of the first major decisions you’ll make as a mom-to-be is how to deliver your baby.
While a vaginal delivery is considered safest, doctors today are performing cesarean deliveries more often.
A cesarean delivery — also called a C-section — is a common but complicated procedure that poses health risks for mom and baby.
Although cesarean deliveries are common and generally safe, they have more risks than delivering a baby vaginally. For this reason, vaginal births are recommended. But it’s possible to schedule a cesarean delivery in advance for medical reasons.
For example, if your baby is breech and doesn’t change position as your due date approaches, your doctor may schedule a cesarean delivery. Additionally, cesarean deliveries are usually scheduled for the medical reasons listed below.
It’s also possible to schedule a cesarean delivery for nonmedical reasons, but this isn’t recommended. A cesarean delivery is major surgery and there’s a greater risk for complications, including:
- blood loss
- organ damage
- allergic reaction to anesthesia
- infections
- blood clots
A scheduled surgery for nonmedical reasons is called an elective cesarean delivery, and your doctor may allow this option. Some women prefer to deliver by surgery because it gives them more control in deciding when their baby is born. It can also reduce some anxiety of waiting for labor to start.
It can also reduce some anxiety of waiting for labor to start.
But just because you’re given the option of an elective cesarean delivery doesn’t mean it comes without risks. There are pros to a scheduled cesarean delivery, but there are also cons. Some health insurance plans also will not cover elective cesarean deliveries.
Pros of an elective C-section
- Lower risk of incontinence and sexual dysfunction after the birth of the baby.
- Lower risk of the baby being deprived of oxygen during delivery.
- Lower risk of the baby experiencing trauma while passing through the birth canal.
Cons of an elective C-section
- You’re more likely to need a repeat cesarean delivery with future pregnancies.
- There’s a higher risk of complications with cesarean deliveries.
- You’ll have a longer hospital stay (up to five days) and a longer recovery period.
A cesarean delivery might be scheduled by your doctor in advance of your due date. Or it may become necessary during labor because of an emergency.
Or it may become necessary during labor because of an emergency.
Below are some of the most common medical reasons for a cesarean.
Prolonged labor
Prolonged labor — also called “failure to progress” or “stalled labor”— is the reason for nearly one-third of cesareans, according to the Centers for Disease Control and Prevention. It happens when a new mom is in labor for 20 hours or more. Or 14 hours or more for moms who’ve given birth before.
Babies that are too large for the birth canal, slow cervical thinning, and carrying multiples can all prolong labor. In these cases, doctors consider a cesarean to avoid complications.
Abnormal positioning
In order to have a successful vaginal birth, babies should be positioned headfirst near the birth canal.
But babies sometimes flip the script. They can position their feet or butt toward the canal, known as a breech birth, or position their shoulder or side first, known as a transverse birth.
A cesarean may be the safest way to deliver in these cases, especially for women carrying multiple babies.
Fetal distress
Your doctor may choose to deliver via emergency cesarean if your baby is not getting enough oxygen.
Birth defects
To reduce delivery complications,doctors will choose to deliver babies diagnosed with certain birth defects, like excess fluid in the brain or congenital heart diseases, through a cesarean to reduce delivery complications.
Repeat cesarean
About 90 percent of women who’ve had a cesarean can deliver vaginally for their next birth, according to the American Pregnancy Association. This is known as vaginal birth after cesarean (VBAC).
Moms-to-be should talk with their physician to decide whether a VBAC or repeat cesarean is the best and safest option.
Chronic health condition
Women may deliver via cesarean if they live with certain chronic health conditions like heart disease, high blood pressure, or gestational diabetes. Vaginal delivery with one of these conditions may be dangerous for mom.
Doctors will also suggest a cesarean if the mom-to-be has HIV, genital herpes, or any other infection that could be transferred to the baby through vaginal delivery.
Cord prolapse
When the umbilical cord slips through the cervix before the baby is born, it’s called a cord prolapse. This can lessen blood flow to the baby, putting the baby’s health at risk.
While rare, a cord prolapse is a serious condition that requires an emergency cesarean delivery.
Cephalopelvic disproportion (CPD)
A CPD is when a mom-to-be’s pelvis is too small to deliver the baby vaginally, or if the baby’s head is too large for the birth canal. In either case, the baby can’t pass through the vagina safely.
Placenta issues
Doctors will perform a cesarean when the low-lying placenta partially or completely covers the cervix (placenta previa). A cesarean is also necessary when the placenta separates from the uterine lining, causing the baby to lose oxygen (placenta abruption).
According to the American Pregnancy Association, placenta previa happens to 1 in every 200 pregnant women. About 1 percent of pregnant women experience placental abruption.
Carrying multiples
Carrying multiples can pose different risks during pregnancy. It can cause prolonged labor, which can put mom in distress. One or more babies may also be in an abnormal position. Either way, a cesarean is often the safest route for delivery.
Since pregnancy and birth can be unpredictable at times, moms-to-be should be prepared in case a cesarean delivery is necessary. Giving birth is a beautiful and miraculous thing, and it’s best to be as prepared for the unexpected as possible.
Q:
Why are so many more women today scheduling elective C-sections? Is this a dangerous trend?
Anonymous patient
A:
The trend in elective cesarean deliveries is growing. One study showed that 8 percent of mothers requested an elective cesarean delivery.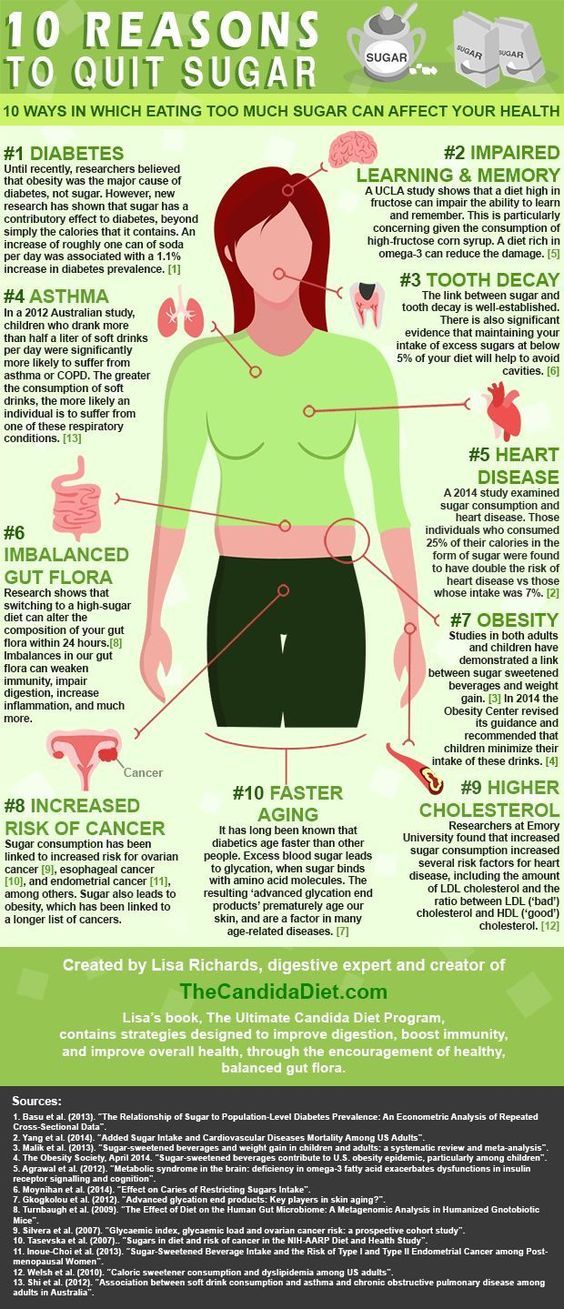 While popular, this trend can have serious complications, including the risk of blood loss, infection, blood clots, and adverse reactions to anesthesia. It’s important to remember that a cesarean delivery is a major abdominal surgery, and typically has a longer recovery than a vaginal delivery. If you’re thinking about scheduling an elective cesarean delivery, you should talk to your doctor more about the risks and benefits.
While popular, this trend can have serious complications, including the risk of blood loss, infection, blood clots, and adverse reactions to anesthesia. It’s important to remember that a cesarean delivery is a major abdominal surgery, and typically has a longer recovery than a vaginal delivery. If you’re thinking about scheduling an elective cesarean delivery, you should talk to your doctor more about the risks and benefits.
Katie Mena, MDAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
WHO: Women in labor and physicians are increasingly opting for caesarean section
Modern surgical approaches, effective pain medications and antibiotics are reported by the World Health Organization to allow the operation to be performed with minimal risk to mother and child. A new WHO study in this area has shown that in countries where at least 10% of women undergo this operation, maternal and child mortality is reduced. However, caesarean section certainly has its downsides. nine0003
However, caesarean section certainly has its downsides. nine0003
“My doctor almost immediately recommended a caesarean section. He explained it by my age. Although this was the second birth for me, but I was already 44 years old. And when I came to the hospital at the appointed time, they said: why, actually, a caesarean? according to what evidence? But my doctor insisted, he didn't want to risk anything. And then, after the birth, he told me that the child had an entanglement of the umbilical cord, and during childbirth this loop could tighten around the child’s neck.
More and more women choose caesarean section as the most painless, quick and safe way to give birth. Caesarean section is especially popular in developed and developing countries. The numbers are impressive. For example, in Brazil, 45% of women choose a caesarean section. In European countries, this figure has increased from 15% to 22% over the past 20 years. WHO spokeswoman Dr. Marlene Temmerman says:
In Brazil, 45% of women opt for a caesarean section.
In European countries, this figure has grown from 15% to 22% over the past 20 years
“In many developing and developed countries, there is a real epidemic of caesarean sections. A cesarean is done even when there is no medical need for it. You may be wondering: so what? If women choose caesarean section and it is safe, why not? Yes, in modern conditions it is really safe. But do not forget that this is still an operation, a surgical intervention.
A caesarean section can cause serious complications for both the baby and the mother. Marlene Temmerman explains:
“Women who have a cesarean are at a higher risk of bleeding. Also, do not forget about the scars that remain from previous births that have passed with the help of surgical intervention. Serious complications may arise. And even in some developed countries, where caesareans are often performed, a higher level of maternal mortality has been reported compared to other developed countries. Of course, this operation is not the main cause of death among women in childbirth, but the connection certainly exists. nine0006
Of course, this operation is not the main cause of death among women in childbirth, but the connection certainly exists. nine0006
However, the preference for caesarean is made, of course, not only by women, but also by doctors. And they are partly understandable. It is better to perform a scheduled operation at a prearranged time than to receive a call from a patient in the middle of the night and then have to deal with this or that unforeseen situation during childbirth:
adjust your schedule. The doctor sees patients at a certain time. He can do two surgeries a day. No unexpected calls, no late night work, no emergencies, no added stress. The quality of life of doctors thanks to caesarean section is significantly improved.” nine0006
At the same time, experts emphasize that in many cases, caesarean section really saves lives. According to WHO, in countries where the number of women who have undergone surgery reaches at least 10% of women, maternal and child mortality is sharply reduced. But, unfortunately, in many regions, women still have no alternative to natural childbirth. Marlin Temmerman speaking:
But, unfortunately, in many regions, women still have no alternative to natural childbirth. Marlin Temmerman speaking:
In a number of countries, women still do not have access to procedures that can ensure safe childbirth. They also cannot opt for a caesarean section as it is not practiced. Women in these countries die during childbirth
“In a number of countries, women still do not have access to procedures that can ensure safe childbirth. They also cannot opt for a caesarean section as it is not practiced. In these countries, women die during childbirth.”
The conclusion reached by the WHO specialists is simple. Doctors should honestly tell expectant mothers about all the pros and cons of a caesarean section, not resort to it too often and only do it when necessary.
Endometriosis of the postoperative scar - article at the LOTOS MC
All articles
Endometriosis is a chronic, progressive, recurrent and hormone-dependent disease in which a benign growth of tissue occurs outside the uterine cavity, similar in morphological and functional properties to the endometrium. In other words, cells that should be located and function inside the uterus migrate to other organs and tissues, while continuing to perform their functions. nine0003
In other words, cells that should be located and function inside the uterus migrate to other organs and tissues, while continuing to perform their functions. nine0003
Symptoms and causes of the disease
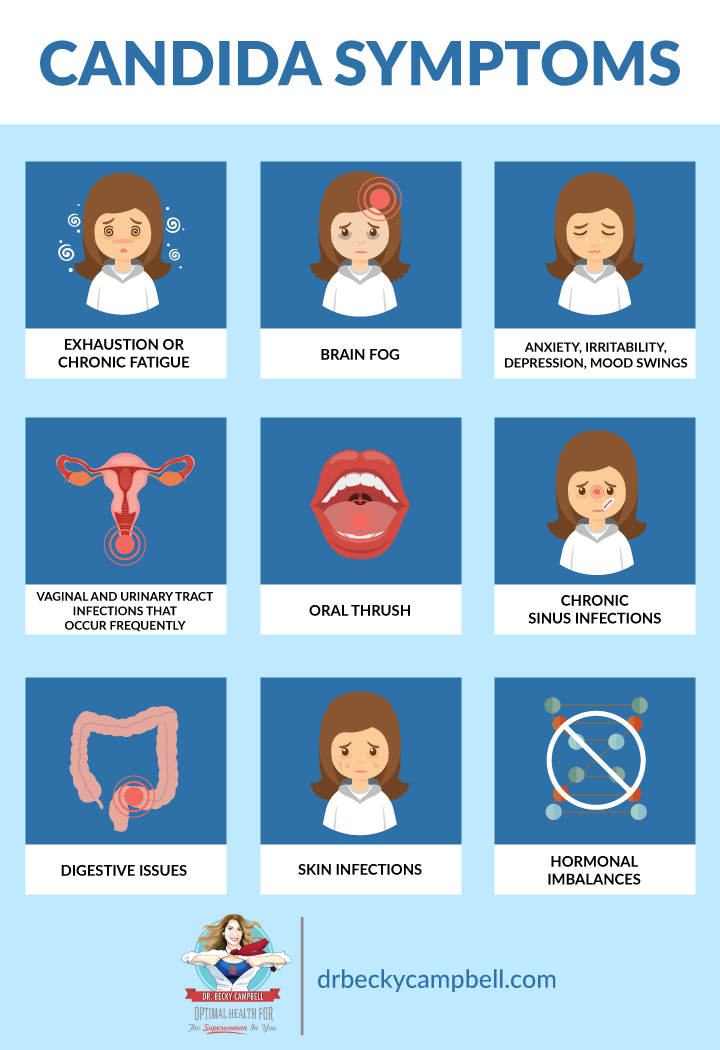
We will consider one of the types of the disease - endometriosis of the postoperative scar. Already from the name it is clear that this type of endometriosis develops after an operation, namely a caesarean section. During the operation, endometrial cells enter the surgical wound and, under certain conditions, continue to function there. Symptoms of the disease usually appear no earlier than 6-12 months after surgery, after the restoration of the menstrual cycle. Sometimes this period lasts long enough and women go to the doctor even after a few years. nine0003
The symptoms of the disease are cyclical. During or before menstruation, local pains appear in the area of the postoperative scar, which become more intense with each cycle. After some time, patients find a seal in the area of the scar, which also becomes larger with each cycle.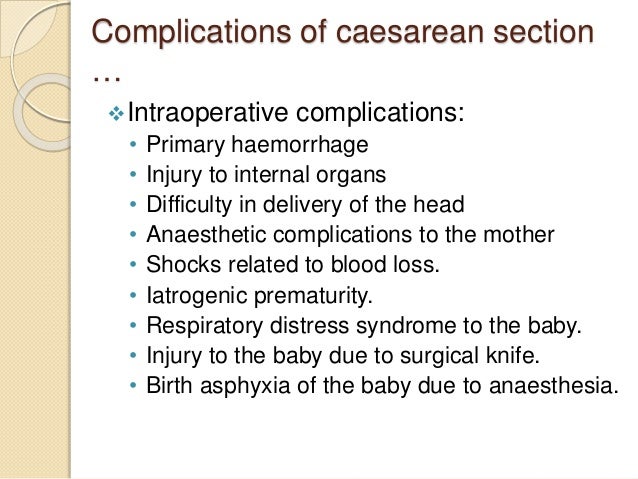 This is usually the reason for going to the doctor.
This is usually the reason for going to the doctor.
Diagnostics
Diagnosis of endometriosis of the scar is usually not difficult. Postponed caesarean section, the presence of an increasing formation in the postoperative scar, which causes pain during menstruation - the combination of these three facts is enough to establish a diagnosis even without additional examination. However, patients are often referred to purulent surgeons, suspecting suppuration of the scar, and even to oncologists, suspecting a malignant process. To clarify the diagnosis, ultrasound of the abdominal wall is used, less often an MRI is required. nine0003
Treatment
Treatment of endometriosis of the postoperative scar is only surgical. It is necessary to completely excise the focus within healthy tissues. But even this cannot 100% guarantee the absence of a recurrence of the disease. In some cases, hormone therapy is prescribed before and after the operation, which is necessary to reduce the focus and reduce the risk of relapse.