During pregnancy sugar level
Gestational Diabetes - Symptoms, Treatments
Gestational Diabetes
It can be a scary diagnosis, but it’s one that’s fairly common.
Nearly 10 percent of pregnancies in the U.S. are affected by gestational diabetes every year. So know that you’re not alone.
And know that it doesn’t mean that you had diabetes before you conceived or that you will have diabetes after you give birth. It means that, by working with your doctor, you can have a healthy pregnancy and a healthy baby. No matter what, you have all the support you need for both you and your baby.
We don’t know what causes gestational diabetes...
But we know that you are not alone. It happens to millions of women. We do know that the placenta supports the baby as it grows. Sometimes, these hormones also block the action of the mother’s insulin to her body and it causes a problem called insulin resistance. This insulin resistance makes it hard for the mother’s body to use insulin. And this means that she may need up to three times as much insulin to compensate.
Gestational diabetes can also start when the mother’s body is not able to make and use all the insulin it needs for pregnancy. Without enough insulin, glucose can’t leave the blood and be changed into energy. When glucose builds up in the blood, it’s called hyperglycemia.
Whatever the cause, you can work with your doctor to come up with a plan and maintain a healthy pregnancy through birth. Ask questions. Ask for help. There are many ways to combat gestational diabetes.
How You Can Treat ItThe key is to act quickly. As treatable as it is, gestational diabetes can hurt you and your baby.
Treatment aims to keep your blood glucose (blood sugar) levels normal. It can include special meal plans and regular physical activity. It can also include daily blood glucose testing and insulin injections.
We suggest the following target for women testing blood glucose levels during pregnancy:
- Before a meal: 95 mg/dl or less
- One hour after a meal: 140 mg/dl or less
- Two hours after a meal: 120 mg/dl or less
Always remember that this is treatable—and working with your health care team can help ensure a healthy pregnancy.
As with all forms of diabetes, diet and exercise can help you gain the upper hand. With gestational diabetes, maintaining a balanced diet is integral to your success. Your doctor can help you develop a meal plan that makes sense for you, helping you identify the best foods and quick meal ideas that can help you stay healthy and strong.
Exercise is critical as well. Work with your doctor to determine the level of activity that’s safe for you and your baby throughout your pregnancy. Use our resources as well to stay in touch with ideas for daily activity. The important thing to remember is to take action as quickly as you can, to stay with it, and to stay on top of your condition. It’s treatable. It’s manageable. And it’s a fight that you can win.
Are you depressed?
Nutrition
Fitness
Gestational diabetes - Diagnosis and treatment
Diagnosis
If you're at average risk of gestational diabetes, you'll likely have a screening test during your second trimester — between 24 and 28 weeks of pregnancy.
If you're at high risk of diabetes — for example, if you're overweight or obese before pregnancy; you have a mother, father, sibling or child with diabetes; or you had gestational diabetes during a previous pregnancy — your health care provider may test for diabetes early in pregnancy, likely at your first prenatal visit.
Routine screening for gestational diabetes
Screening tests may vary slightly depending on your health care provider, but generally include:
-
Initial glucose challenge test. You'll drink a syrupy glucose solution. One hour later, you'll have a blood test to measure your blood sugar level. A blood sugar level of 190 milligrams per deciliter (mg/dL), or 10.6 millimoles per liter (mmol/L), indicates gestational diabetes.
A blood sugar level below 140 mg/dL (7.8 mmol/L) is usually considered within the standard range on a glucose challenge test, although this may vary by clinic or lab. If your blood sugar level is higher than expected, you'll need another glucose tolerance test to determine if you have gestational diabetes.
- Follow-up glucose tolerance testing. This test is similar to the initial test — except the sweet solution will have even more sugar and your blood sugar will be checked every hour for three hours. If at least two of the blood sugar readings are higher than expected, you'll be diagnosed with gestational diabetes.
More Information
- Glucose challenge test
- Glucose tolerance test
- Nonstress test
Treatment
Treatment for gestational diabetes includes:
- Lifestyle changes
- Blood sugar monitoring
- Medication, if necessary
Managing your blood sugar levels helps keep you and your baby healthy. Close management can also help you avoid complications during pregnancy and delivery.
Lifestyle changes
Your lifestyle — how you eat and move — is an important part of keeping your blood sugar levels in a healthy range. Health care providers usually don't advise losing weight during pregnancy — your body is working hard to support your growing baby.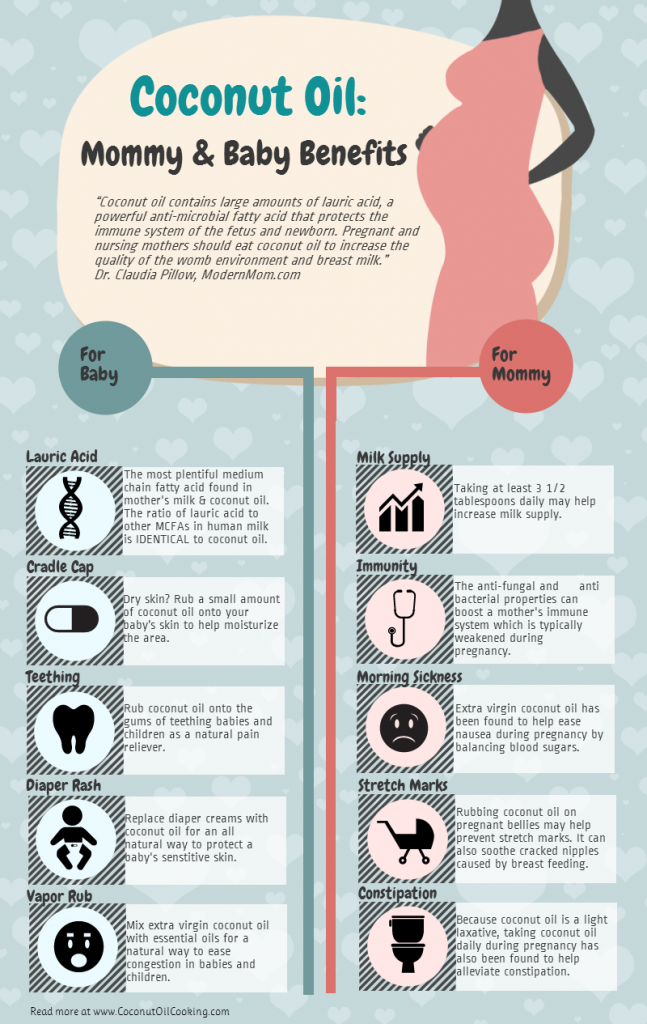 But your health care provider can help you set weight gain goals based on your weight before pregnancy.
But your health care provider can help you set weight gain goals based on your weight before pregnancy.
Lifestyle changes include:
- Healthy diet. A healthy diet focuses on fruits, vegetables, whole grains and lean protein — foods that are high in nutrition and fiber and low in fat and calories — and limits highly refined carbohydrates, including sweets. A registered dietitian or a certified diabetes care and education specialist can help you create a meal plan based on your current weight, pregnancy weight gain goals, blood sugar level, exercise habits, food preferences and budget.
- Staying active. Regular physical activity plays a key role in every wellness plan before, during and after pregnancy. Exercise lowers your blood sugar. As an added bonus, regular exercise can help relieve some common discomforts of pregnancy, including back pain, muscle cramps, swelling, constipation and trouble sleeping.
With your health care provider's OK, aim for 30 minutes of moderate exercise on most days of the week.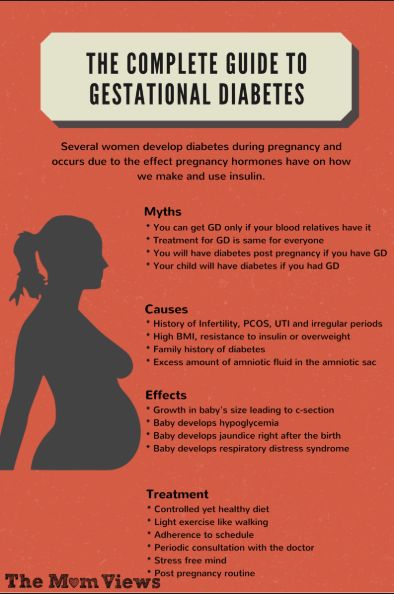 If you haven't been active for a while, start slowly and build up gradually. Walking, cycling and swimming are good choices during pregnancy. Everyday activities such as housework and gardening also count.
If you haven't been active for a while, start slowly and build up gradually. Walking, cycling and swimming are good choices during pregnancy. Everyday activities such as housework and gardening also count.
Blood sugar monitoring
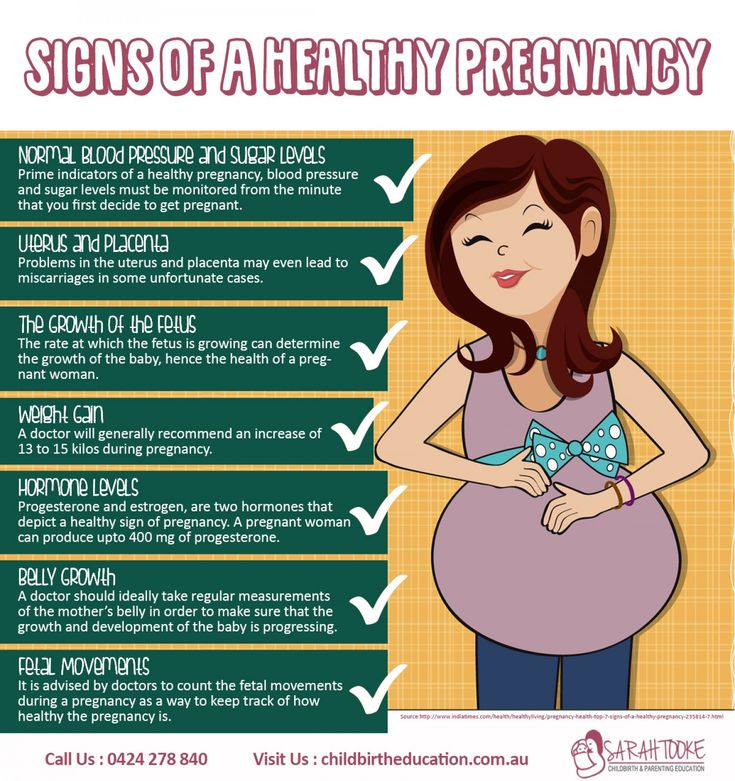
While you're pregnant, your health care team may ask you to check your blood sugar four or more times a day — first thing in the morning and after meals — to make sure your level stays within a healthy range.
Medication
If diet and exercise aren't enough to manage your blood sugar levels, you may need insulin injections to lower your blood sugar. A small number of women with gestational diabetes need insulin to reach their blood sugar goals.
Some health care providers prescribe an oral medication to manage blood sugar levels. Other health care providers believe more research is needed to confirm that oral medications are as safe and as effective as injectable insulin to manage gestational diabetes.
Close monitoring of your baby
An important part of your treatment plan is close observation of your baby. Your health care provider may check your baby's growth and development with repeated ultrasounds or other tests. If you don't go into labor by your due date — or sometimes earlier — your health care provider may induce labor. Delivering after your due date may increase the risk of complications for you and your baby.
Your health care provider may check your baby's growth and development with repeated ultrasounds or other tests. If you don't go into labor by your due date — or sometimes earlier — your health care provider may induce labor. Delivering after your due date may increase the risk of complications for you and your baby.
Follow-up after delivery
Your health care provider will check your blood sugar level after delivery and again in 6 to 12 weeks to make sure that your level has returned to within the standard range. If your tests are back in this range — and most are — you'll need to have your diabetes risk assessed at least every three years.
If future tests indicate type 2 diabetes or prediabetes, talk with your health care provider about increasing your prevention efforts or starting a diabetes management plan.
More Information
- Labor induction
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
It's stressful to know you have a condition that can affect your unborn baby's health. But the steps that will help control your blood sugar level — such as eating healthy foods and exercising regularly — can help relieve stress, nourish your baby and help prevent type 2 diabetes in the future.
You may feel better if you learn as much as you can about gestational diabetes. Talk to your health care team, or read books and articles about gestational diabetes. You may find a support group for people with gestational diabetes helpful. Ask your health care team for suggestions.
Preparing for your appointment
You'll likely find out you have gestational diabetes from routine screening during your pregnancy. Your health care provider may refer you to additional health professionals who specialize in diabetes, such as an endocrinologist, a certified diabetes care and education specialist, or a registered dietitian. One or more of these care providers can help you learn to manage your blood sugar level during your pregnancy.
You may want to take a family member or friend along to your appointment, if possible. Someone who accompanies you may remember something that you missed or forgot.
Here's some information to help you get ready for your appointment and know what to expect from your health care provider.
What you can do
Before your appointment:
- Be aware of pre-appointment restrictions. When you make your appointment, ask if you need to fast for lab tests or do anything else to prepare for diagnostic tests.
- Make a list of symptoms you're having, including those that may seem unrelated to gestational diabetes. You may not have noticeable symptoms, but it's good to keep a log of anything unusual you notice.
- Make a list of key personal information, including major stresses or recent life changes.
- Make a list of all medications, including over-the-counter drugs and vitamins or supplements you're taking.

- Make a list of questions to help make the most of your time with your health care provider.
Some basic questions to ask your health care provider include:
- What can I do to help control my condition?
- Can you recommend a registered dietitian or certified diabetes care and education specialist who can help me plan meals, an exercise program and coping strategies?
- Will I need medication to control my blood sugar?
- What symptoms should prompt me to seek medical attention?
- Are there brochures or other printed materials I can take? What websites do you recommend?
What to expect from your doctor
Your health care provider is also likely to have questions for you, especially if it's your first visit. Questions may include:
- Have you experienced increased thirst or excessive urination? If so, when did these symptoms start? How often do you have them?
- Have you noticed other unusual symptoms?
- Do you have a parent or sibling who's ever been diagnosed with diabetes?
- Have you been pregnant before? Did you have gestational diabetes during your previous pregnancies?
- Did you have other problems in previous pregnancies?
- If you have other children, how much did each weigh at birth?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Gestational diabetes in pregnancy - treatment and diagnosis of diabetes in pregnant women in Moscow, Clinical Hospital on Yauza
Consult a gynecologist
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Contents
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Specialists of the Yauza Clinical Hospital diagnose and treat gestational diabetes and its complications. For a comfortable pregnancy and the safety of the expectant mother and baby, we exercise strict control over the blood sugar level of a pregnant woman, if necessary, prescribe a specially designed diet and medications.
Make an appointment with a gynecologist
- About 7% of pregnant women have manifestations of gestational diabetes. In 50% of cases, the disease is asymptomatic
- Gestational diabetes in pregnancy significantly increases the risk of pregnancy complications for both mother and fetus
- Perinatal mortality increases by 2-3% with a combination of diabetes mellitus and pregnancy
Pregnancy diabetes (gestational diabetes) is an increase in blood glucose that first occurs during pregnancy but is not high enough to warrant a diagnosis of diabetes mellitus.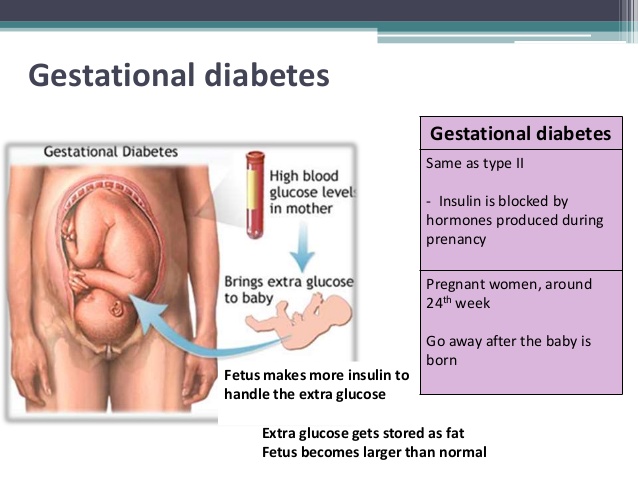 These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus.
These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus.
Pregnant blood glucose norm
During pregnancy, all women experience changes in insulin sensitivity and glucose tolerance. This is fine. The difference between the norm and pathology in the degree of change.
Blood tests for diabetes during pregnancy - norm and pathology
- If the test of venous blood taken on an empty stomach shows a glucose level of more than 5.1 mmol / l, this is the norm for pregnant women.
- From 5.1 to 7.0 mmol / l - gestational diabetes.
- If 7.0 mmol / l or more - diabetes mellitus.
- Testing capillary blood (taken from a fingerstick) for the diagnosis of gestational diabetes mellitus is not recommended.
- If during an oral glucose tolerance test (when 75 g of glucose is taken orally during the study) after an hour the glucose level is more than 10.
 0 mmol/l, and after two hours the blood glucose level is in the range of 7.8-8.5 mmol/l - then for pregnant women this is a normal indicator.
0 mmol/l, and after two hours the blood glucose level is in the range of 7.8-8.5 mmol/l - then for pregnant women this is a normal indicator.
To better understand what gestational diabetes, or diabetes in pregnancy, is, you need to talk a little about hormonal changes in the body in pregnant women.
Causes of gestational diabetes
Hormonal changes that occur during pregnancy are associated with increased production of large amounts of steroid hormones. Some of them, such as cortisol and progesterone, have a significant effect on cell receptors, increasing their resistance to insulin.
This leads to an increase in blood glucose levels and requires a significant increase in insulin production by the pancreas. In cases where the compensatory capacity of the pancreas is not enough, sugar metabolism gets out of control and a condition called gestational diabetes or gestational diabetes develops.
This condition occurs quite often. Between 3 and 10% of pregnant women develop pathological insulin resistance leading to gestational diabetes.
Unlike diabetes mellitus diagnosed before pregnancy, pathological insulin resistance that occurs during pregnancy does not cause fetal malformations and in most cases does not require insulin treatment. But, nevertheless, uncompensated gestational diabetes can significantly complicate the course of pregnancy.
Specialists of the Yauza Clinical Hospital diagnose, treat and prevent diabetes in pregnant women and its complications, such as impaired fetal growth. The doctors of the Clinical Hospital on the Yauza strictly control the blood sugar level of a pregnant woman, if necessary, prescribe a specially designed diet. This ensures a comfortable pregnancy and the safety of the expectant mother and baby.
Pregnancy diabetes - consequences for the child
Large disproportionate fruit. The most important and frequent complication of gestational diabetes is fetal growth failure. Developing in conditions of increased blood glucose levels, which penetrate the fetoplacental barrier, the fetus is forced to compensate for the increased sugar level with its own insulin. Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die.
Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die.
Polyhydramnios or oligohydramnios. In addition, in gestational diabetes, the balance of the amount of amniotic fluid can be disturbed and either polyhydramnios or oligohydramnios develops. This is a serious risk factor for intrauterine fetal death or premature birth.
Underdevelopment of the lungs. In gestational diabetes, the lungs of the fetus mature later, as the production of surfactant (a special lubrication of the inner walls of the alveoli, where oxygen is exchanged in the lungs) is disrupted. Therefore, premature birth in gestational diabetes is especially dangerous.
Hypoglycemia and metabolic disorders in the fetus. Due to the constant increased production of its own insulin during pregnancy, immediately after birth, the child is in a state of hypoglycemia with electrolyte imbalance, which threatens his life.
All this dictates the need for the earliest possible detection of gestational diabetes in pregnant women, the level of sugar in the blood of a pregnant woman and to prevent the development of complications.
.
Diagnosis of diabetes in pregnant women at the Yauza Clinical Hospital
Signs of diabetes in pregnant women
Gestational diabetes in pregnancy is not usually associated with the classic symptoms of diabetes, such as thirst or excessive urination (polyuria).
Pregnancy tests for diabetes mellitus
First phase. At the first visit of a pregnant woman to a doctor at any time, she is tested for glucose levels in venous blood - fasting glucose, regardless of food intake, glycated hemoglobin. This is the first phase of research to detect diabetes mellitus or gestational diabetes in pregnant women. If diabetes mellitus is detected, the patient is referred for observation and treatment to an endocrinologist.
Second phase. For a period of 24-28 weeks, all patients who did not show identified disorders of carbohydrate metabolism at the first study are called for a glucose tolerance test (PGTT) to detect "hidden diabetes". This is done because the occurrence of gestational diabetes is associated with the development of insulin resistance under the influence of hormones produced by the placenta. Therefore, in the vast majority of cases, gestational diabetes develops in the second half of pregnancy after 24 weeks, when there is a peak in the production of placental hormones.
Glucose tolerance test
It is carried out to detect pathological insulin resistance, characteristic of latent diabetes in pregnant women. Pregnant women undergo a two-hour test, only in the laboratory.
During the 3 days leading up to the test, the woman should eat her usual diet, including carbohydrates (>150 g of carbohydrates per day), maintain her usual physical activity. The evening before testing, dinner should include 30-50 grams of carbohydrates.
On the day of the study, before the analysis, you should not smoke and take medications that can affect the level of glucose (vitamins, glucocorticoid hormones, iron preparations, which include carbohydrates, beta-agonists, beta-blockers). You can drink water.
Venous blood is taken on an empty stomach (after 8-14 hours of fasting, usually in the morning, before breakfast).
Then the patient takes a glucose solution (75 g).
And they take blood in an hour and two after the sugar load. Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l.
Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l.
If manifest diabetes mellitus is detected, the patient is referred to an endocrinologist, gestational diabetes mellitus is treated by an obstetrician-gynecologist or therapist.
Glucose tolerance test contraindications
- Strict bed rest for a pregnant woman (until doctor's approval).
- Pronounced toxicosis of pregnant women (with nausea and vomiting).
- Acute infectious or inflammatory disease.
- Exacerbation of chronic pancreatitis.
- Dumping syndrome (syndrome of resected stomach).
Prenatal diabetes monitoring
Blood glucose monitoring, self-monitoring diary
When diagnosing gestational diabetes, it is necessary to establish strict control of sugar levels throughout the subsequent pregnancy and during childbirth. To do this, regularly examine the blood for sugar (glucose). In addition, the patient conducts self-monitoring using a glucometer.
In addition, the patient conducts self-monitoring using a glucometer.
It is recommended that a pregnant woman keep a diary of observations in which to record:
- blood glucose level (normal <5.1 mmol/l),
- the presence of ketone bodies in the urine, which is determined by test strips sold in a pharmacy (normally, ketone bodies are absent),
- blood pressure readings (normal <130|80 mmHg),
- fetal movements,
- body weight,
- diet.
Expert ultrasound
Conducting an expert ultrasound examination reveals signs of intrauterine suffering of the fetus (diabetic fetopathy), polyhydramnios. Most often, this is a sign of chronically elevated blood glucose levels, penetrating into the blood of the fetus. This requires urgent correction of the diet and normalization of the level of glycemia (blood sugar). If necessary, insulin therapy.
Make an appointment
Treatment of gestational diabetes
Diet for gestational diabetes
In most cases, it is sufficient to follow a special diet recommended by a nutritionist based on the body mass index of the pregnant woman and her taste preferences.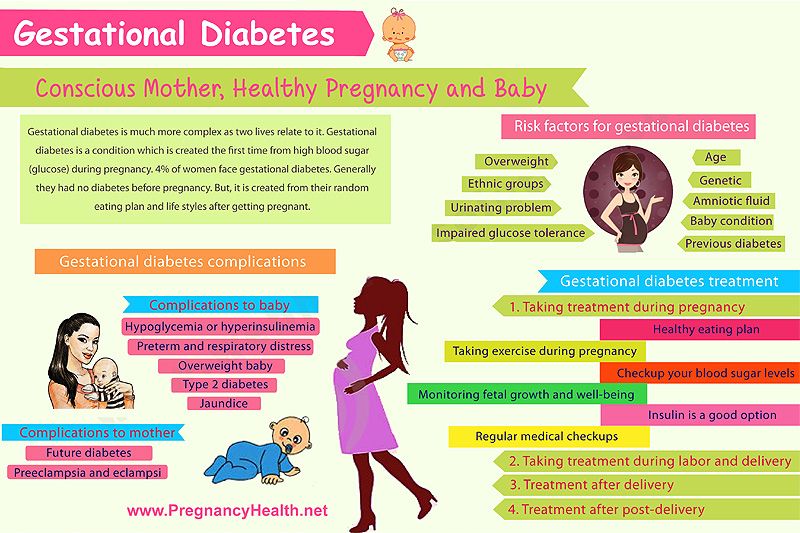 The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
- Avoid simple carbohydrates - sweets, pastries, white bread, honey, sugar, jam, sweet drinks and fruits, ice cream.
- Limit complex carbohydrates - cereals (semolina, rice - exclude), potatoes, corn, legumes, durum wheat pasta. Distribute their intake evenly over several meals throughout the day to eliminate starvation (causes the formation of ketone bodies).
- Eat enough protein - meat, fish, seafood, poultry, mushrooms, eggs, hard cheese, dairy and sour-milk products of medium fat content (3-5%).
- It is necessary to enrich the diet with fiber and vitamins - greens, vegetables (except for boiled carrots and beets), sweet and sour berries (excluding grapes).
- Correctly choose fats, do not exceed their amount recommended by the doctor - vegetable oils (add to ready-made meals), nuts, seeds. Animal fats (butter, sausages) - limit.
- When cooking, boil, stew, steam and bake dishes. Don't fry. Do not deep fry.
A detailed menu for a pregnant woman with gestational diabetes will be compiled by a doctor, taking into account the individual characteristics of each particular woman.
It is not worth using table No. 9 in its pure form for pregnant women with diabetes mellitus due to a significant restriction of its calorie content.
In detail, what you can eat with diabetes in pregnant women will be told by the doctor at an in-person consultation.
Pharmacotherapy
In cases where the diet fails to achieve the desired control of the level of glycemia in the blood, there are signs of a negative effect on the fetus - they resort to prescribing drugs - insulin. In case of diabetes in pregnant women, antidiabetic drugs in tablets should not be used. Insulin therapy is prescribed by an endocrinologist. Pregnant women with diabetes who are on insulin therapy are jointly managed by an endocrinologist, an internist and an obstetrician-gynecologist.
Physical activity
Patients are recommended regular physical activity - walking in the fresh air (at least 150 minutes per week), swimming.
Prenatal diabetes - childbirth
With a compensated course of gestational diabetes, normal development of the fetus and the condition of the woman, childbirth is carried out in time in a natural way. The question of early delivery, caesarean section may arise if there are relevant indications from the mother or fetus.
Specialists of the Yauza Clinical Hospital have included mandatory fetal development screenings and tests to diagnose sugar metabolism disorders in the pregnancy monitoring program. Recommendations are given on a special diet for women with manifestations of gestational diabetes. If necessary, strict glycemic control is carried out throughout pregnancy, ensuring its successful completion and the birth of a healthy child.
Make an appointment
Cost of services
Prices for services you can see in the price list or check by phone listed on the site.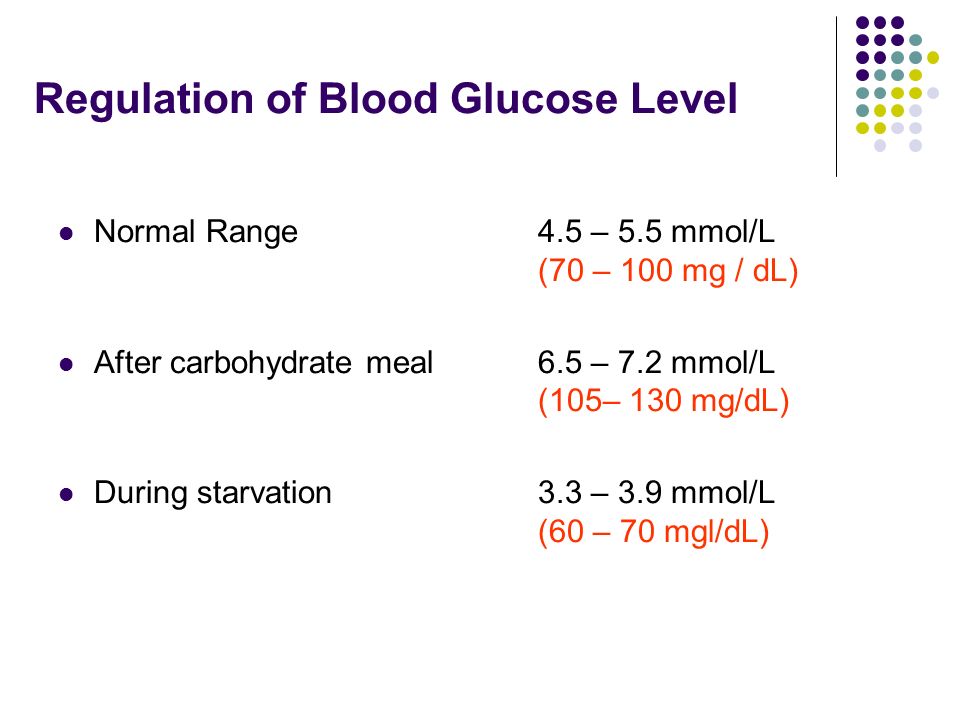
Attention! Website prices may vary.
Please check the current cost with the administrators by phone.
BOOK AN APPOINTMENT. WE WORK WITHOUT DAYS OFF
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Advantages of the clinic
More appears during pregnancy in women who did not have diabetes before.
Outside of pregnancy, blood glucose levels up to and including 6.0 mmol/L are considered normal. But pregnant women are different. The level of sugar becomes lower, due to the costs of the developing fetus, a decrease in the formation of glucose in the liver and other processes. Therefore, the value of glucose in a pregnant woman on an empty stomach of 5.1 mmol / l and higher (but up to 7.0 mmol / l), even with a single determination, indicates gestational diabetes mellitus.
Above 7.0 mmol/l is manifest diabetes, which requires immediate contact with an endocrinologist and initiation of insulin therapy. Often this means that diabetes was before pregnancy, but was not detected.
Often this means that diabetes was before pregnancy, but was not detected.
Gestational diabetes is dangerous because it can cause a number of complications during pregnancy and childbirth, namely: stillbirth, miscarriage, high risk of obesity and the development of diabetes later.
For a woman, this condition is also unsafe: the risks of preeclampsia, the need for a caesarean section and the development of diabetes mellitus after childbirth increase.
Fortunately, all these consequences can be avoided if you consult a doctor and start treatment.
Gestational diabetes is usually asymptomatic, but can sometimes present with excessive fatigue, constant thirst, frequent urination, and blurred vision. All this can be attributed to stress and weather. Therefore, it is possible to accurately diagnose with the help of tests.
After the 6th week of pregnancy, blood glucose is tested from a vein. Normally, the result is up to 5.0 mmol / l inclusive. An increase in sugar to 5.1 mmol / l or more requires intervention - a consultation with an endocrinologist who will talk about the need to change diet, lifestyle, regular self-monitoring of blood sugar, in some cases, insulin treatment is prescribed.
Normally, the result is up to 5.0 mmol / l inclusive. An increase in sugar to 5.1 mmol / l or more requires intervention - a consultation with an endocrinologist who will talk about the need to change diet, lifestyle, regular self-monitoring of blood sugar, in some cases, insulin treatment is prescribed.
At 24-28 weeks, all pregnant women with normal blood glucose are given an oral glucose tolerance test (OGTT) to detect underlying disorders. OGTT is included in the list of examinations that are carried out as part of the MHI.
You can reduce your risk of gestational diabetes by making lifestyle changes. To do this, you need:
- have a BMI less than 25,
- switch to a healthy diet,
- 150 minutes of physical activity per week,
- stop smoking.
Our endocrinologists act within the framework of clinical recommendations, Russian and international, and do not prescribe unnecessary tests and drugs.












