Do you get sick when pregnant
Vomiting and morning sickness - NHS
Nausea and vomiting in pregnancy, often known as morning sickness, is very common in early pregnancy.
It can affect you at any time of the day or night or you may feel sick all day long.
Morning sickness is unpleasant, and can significantly affect your day-to-day life. But it usually clears up by weeks 16 to 20 of your pregnancy and does not put your baby at any increased risk.
There is a chance of developing a severe form of pregnancy sickness called hyperemesis gravidarum. This can be serious, and there's a chance you may not get enough fluids in your body (dehydration) or not get enough nutrients from your diet (malnourishment). You may need specialist treatment, sometimes in hospital.
Sometimes urinary tract infections (UTIs) can also cause nausea and vomiting. A UTI usually affects the bladder, but can spread to the kidneys.
Non-urgent advice: Call your midwife, GP or 111 if:
you're vomiting and:
- have very dark-coloured urine or have not had a pee in more than 8 hours
- are unable to keep food or fluids down for 24 hours
- feel severely weak, dizzy or faint when standing up
- have tummy (abdominal) pain
- have a high temperature
- vomit blood
- have lost weight
Treatments for morning sickness
Unfortunately, there's no hard and fast treatment that will work for everyone’s morning sickness. Every pregnancy will be different.
But there are some changes you can make to your diet and daily life to try to ease the symptoms.
If these do not work for you or you're having more severe symptoms, your doctor or midwife might recommend medicine.
Things you can try yourself
If your morning sickness is not too bad, your GP or midwife will initially recommend you try some lifestyle changes:
- get plenty of rest (tiredness can make nausea worse)
- avoid foods or smells that make you feel sick
- eat something like dry toast or a plain biscuit before you get out of bed
- eat small, frequent meals of plain foods that are high in carbohydrate and low in fat (such as bread, rice, crackers and pasta)
- eat cold foods rather than hot ones if the smell of hot meals makes you feel sick
- drink plenty of fluids, such as water (sipping them little and often may help prevent vomiting)
- eat foods or drinks containing ginger – there's some evidence ginger may help reduce nausea and vomiting (check with your pharmacist before taking ginger supplements during pregnancy)
- try acupressure – there's some evidence that putting pressure on your wrist, using a special band or bracelet on your forearm, may help relieve the symptoms
Find out more about vitamins and supplements in pregnancy
Anti-sickness medicine
If your nausea and vomiting is severe and does not improve after trying the above lifestyle changes, your GP may recommend a short-term course of an anti-sickness medicine, called an antiemetic, that's safe to use in pregnancy.
Often this will be a type of antihistamine, which are usually used to treat allergies but also work as medicines to stop sickness (antiemetic).
Antiemetics will usually be given as tablets for you to swallow.
But if you cannot keep these down, your doctor may suggest an injection or a type of medicine that's inserted into your bottom (suppository).
See your GP if you'd like to talk about getting anti-sickness medication.
Risk factors for morning sickness
It's thought hormonal changes in the first 12 weeks of pregnancy are probably one of the causes of morning sickness.
But you may be more at risk of it if:
- you're having twins or more
- you had severe sickness and vomiting in a previous pregnancy
- you tend to get motion sickness (for example, car sick)
- you have a history of migraine headaches
- morning sickness runs in the family
- you used to feel sick when taking contraceptives containing oestrogen
- it's your first pregnancy
- you're obese (your BMI is 30 or more)
- you're experiencing stress
Visit the pregnancy sickness support site for tips for you and your partner on dealing with morning sickness.
Find maternity services near you
Sign up for pregnancy emails
Sign up for Start4Life's weekly emails for expert advice, videos and tips on pregnancy, birth and beyond.
Video: how can I cope with morning sickness?
In this video, a midwife gives advice on how to deal with morning sickness during your pregnancy.
Media last reviewed: 27 February 2017
Media review due: 27 March 2020
Page last reviewed: 13 April 2021
Next review due: 13 April 2024
Getting Sick While Pregnant | American Pregnancy Association
Getting sick is never fun, but getting sick while pregnant is even worse. It is common for the immune system to weaken while you are pregnant, which makes you more susceptible to getting sick. Obviously, you want to do everything possible to avoid catching something, but don’t be surprised if you do get sick while you are pregnant.
Obviously, you want to do everything possible to avoid catching something, but don’t be surprised if you do get sick while you are pregnant.
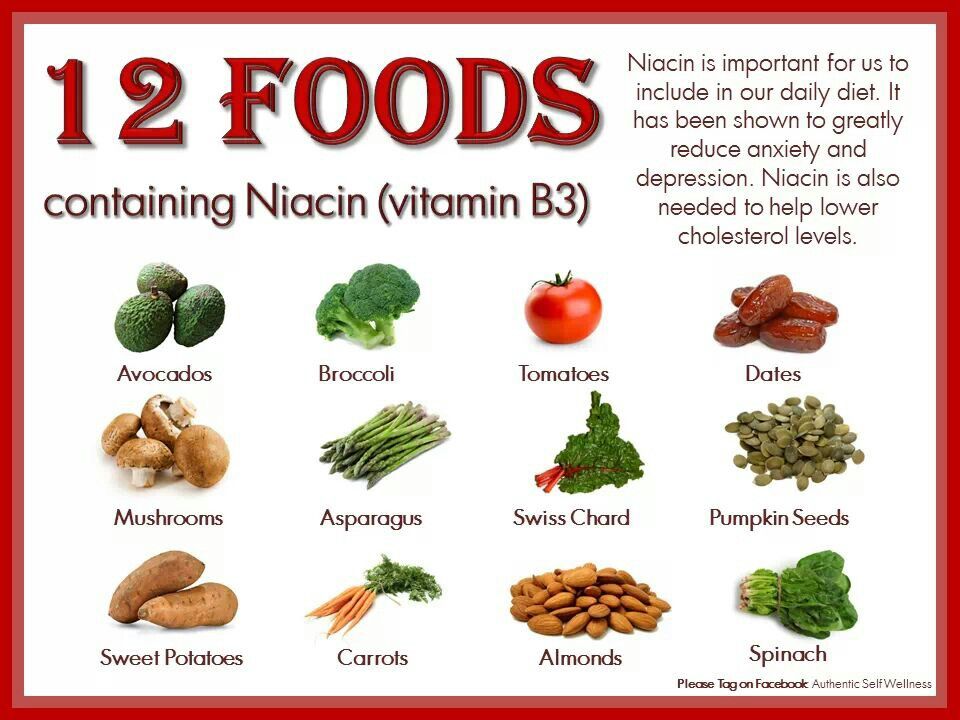
The best way to avoid getting sick while you are pregnant is to take steps to make sure you are healthy. The more you invest in your health, the more likely you will be able to avoid getting sick or speed up your recovery if you do get sick. A healthy body starts with eating healthy. The vitamins and nutrients that you get from a nutritious meal go directly to building up and supporting your immune system. Taking prenatal vitamins and probiotics can further enhance this.
Probiotics occur naturally in foods like yogurt. Eating yogurt and taking probiotic supplements both support your immune system making it easier for your body to fight off bugs. Getting lots of rest is also vital for a healthy body. Try to go bed in a timely fashion, and take naps as necessary. Melatonin, a common sleep aid, is not proven safe during pregnancy and should be avoided at this time. Exercise is also beneficial for your body’s health, and it often makes it easier to get a good night’s sleep.
Exercise is also beneficial for your body’s health, and it often makes it easier to get a good night’s sleep.
One of the best things you can do to avoid getting sick while pregnant is washing your hands regularly. Some of the most common places that you can pick up germs are on doors, which are touched regularly by others going in and out. When you get to the office or back home, make a habit of washing your hands. Using anti-bacterial wipes on grocery baskets or other commonly touched items is another way to protect yourself from picking up germs that may lead to sickness.
How to Get Well If You are Sick While Pregnant
If you are sick while pregnant, there are some steps you can take to get well.
Here are some initial things you should try:
- Rest – As noted above, a rested body helps your immune system work better. A healthy immune system can help shorten your sick period.
- Stay Hydrated – Fluids are also essential to a healthy body.
 Fluids also help wash out your system.
Fluids also help wash out your system. - Take Your Vitamins – Vitamins and supplements contain nutrients that contribute towards a healthy body and a healthy immune system.
The above steps are not magic pills to make your cold go away. However, collectively they give your body the best fighting chance to end the sickness.
There are also some natural steps you can take to alleviate or minimize troublesome symptoms:
- Reduce Congestion – Place a humidifier in your room, keep your head elevated on your pillow while resting, or use nasal strips.
- Alleviate Your Sore Throat – Suck on ice chips, drink warm tea, or gargle with warm saltwater.
You can also talk to the pharmacist or your healthcare provider for over-the-counter (OTC) medication you can take to manage your symptoms if they progress. It is imperative that you read the labels or consult your healthcare team because there are many medications you normally would use to treat the symptoms of your cold that are not safe to take during pregnancy.
The following is a list of medications that pose little risk to your baby during pregnancy; however, it is best to consult with your doctor before taking any medications to relieve your symptoms.
- Acetaminophen (i.e. Tylenol) can be used to alleviate fevers, headaches, and body aches. This should be used sparingly and it is best to consult your obstetrician.
- Anesthetic sore throat lozenges can ease the pain in your throat.
- Codeine and dextromethorphan can often be used as cough suppressants.
When to See Your Doctor if You are Sick While Pregnant
Your healthcare provider is there to help you have the safest and healthiest pregnancy possible. Do not hesitate to contact them with questions if you are sick while pregnant. It is essential to contact your provider if your symptoms cause you to miss meals, lose sleep, or if there is no improvement after a couple of days.
It is also important to consult your physician if you develop a fever that is 102° Fahrenheit or greater. Lastly, if you begin to cough up discolored mucus or if your cough is accompanied by chest pain and/or wheezing, make sure to call your doctor. They may need to prescribe an antibiotic to kill the infection.
Lastly, if you begin to cough up discolored mucus or if your cough is accompanied by chest pain and/or wheezing, make sure to call your doctor. They may need to prescribe an antibiotic to kill the infection.
Want to Know More?
- How to Wash Your Hands Effectively
- Nutrients and Vitamins for Pregnancy
- Pregnancy Nutrition
- Vitamin D and Pregnancy
- Natural Sources of Vitamin B6 During Pregnancy
Compiled using information from the following sources:
1. Yankowitz, Jerome. (2008). Drugs in Pregnancy in Gibbs, Ronald S., Karlan, Beth Y., & Haney, Arthur F., & Nygaard, Ingrid E. (Eds.), Danforth’s Obstetrics and Gynecology, 10th edition (126). Philadelphia, PA: Lippincott Williams & Wilkins.
2. The First Trimester: First 12 weeks in Johnson, Robert V. (Ed.), Mayo Clinic Complete Book of Pregnancy & Baby’s First Year (136). New York, NY: William Morrow and Company, Inc.
New York, NY: William Morrow and Company, Inc.
3. Common concerns and questions of pregnancy in Harms, Roger W. (Ed.), Mayo Clinic Guide to a Healthy Pregnancy (432-3). New York, NY: HarperCollins Publishers Inc.
Coronovirus or COVID-19 and pregnancy
Bookmark this page
Read and download the Coronavirus and Pregnancy Fact Sheet, which answers key questions for women and their families facing COVID-19.
March 28, 2020: Please note that the information provided here is based on a small number of pregnant women who have had this infection. New data is emerging daily. We strongly advise you to speak with your doctor or midwife for the most up-to-date information. nine0008
What is COVID -19?
COVID-19 is an infectious disease caused by the coronovirus. This virus is similar to many other viruses that cause the common cold. The difference is that while most people won't feel the difference in how they feel as if they had a common cold, people with other medical conditions such as lung disease or diabetes are at increased risk and may get sick enough or develop severe pulmonary complications. In people with COVID-19fever and cough or difficulty breathing are common. If the condition worsens, serious breathing problems may occur and admission to a hospital or intensive care unit may be required.
In people with COVID-19fever and cough or difficulty breathing are common. If the condition worsens, serious breathing problems may occur and admission to a hospital or intensive care unit may be required.
How is it distributed?
The COVID-19 virus is spread primarily through contact with someone who is infected or ill, and through contact with objects that the infected or ill have recently touched or sneezed or coughed on. The virus can be found in saliva and nasal discharge from a runny nose. The virus enters the body through contact with the mucous membrane of the mouth, nose or eyes. nine0003
How to prevent infection COVID -19?
Wash your hands regularly after contact with objects outside your home and avoid touching your face with your hands - these are the best ways to prevent infection. Social distancing is also a good way to prevent contagion. Stay at least 2 meters or 6 feet away from others. Stay at home for as long as possible. To prevent transmission of any virus to others, people should cover their mouth when sneezing or coughing with the crook of the arm (the inside of the elbow) and not with the palm of their hand. nine0003
Stay at home for as long as possible. To prevent transmission of any virus to others, people should cover their mouth when sneezing or coughing with the crook of the arm (the inside of the elbow) and not with the palm of their hand. nine0003
Should I avoid going to the hospital or seeing my doctor or midwife?
When you are pregnant, you will have many appointments with doctors or midwives. They are important for the health of you and your baby and should only be discontinued after discussion with your doctor or midwife. Some appointments can be done by phone or video and your doctor or midwife will decide if this is right for you. If you experience complications during your pregnancy, you should not hesitate to contact your doctor or midwife immediately and discuss with them the best way to take care of your health. When you visit a clinic or hospital, wash your hands regularly. If you are touching objects, avoid touching your face with your hands and while waiting for an appointment, try to stay at least 2 meters or 6 feet away from other people. You should also wash your hands after leaving. If you have a cough, put on a mask as soon as you arrive at the clinic or hospital and tell the staff about it as soon as possible, or better, let the staff know about it before the visit so that the staff will expect you and be better prepared to help. If you are sick with COVID-19and you have a regular appointment, contact your doctor or midwife to find out if it's best to come in or reschedule your appointment.
You should also wash your hands after leaving. If you have a cough, put on a mask as soon as you arrive at the clinic or hospital and tell the staff about it as soon as possible, or better, let the staff know about it before the visit so that the staff will expect you and be better prepared to help. If you are sick with COVID-19and you have a regular appointment, contact your doctor or midwife to find out if it's best to come in or reschedule your appointment.
How dangerous is it for me if I contracted COVID -19 during pregnancy?
We don't have much information about pregnant women who have recovered from COVID-19. We know that the best thing is to prevent the disease. But based on the little information we have, it looks like pregnant women are getting COVID-19.no more severe than non-pregnant women of the same age. Women with other health problems, especially those with lung disease, high blood pressure, diabetes, or HIV, are at increased risk when the disease is more severe. If this is your case, and if you are diagnosed with COVID-19, you should be monitored more closely than other pregnant women. Most healthy pregnant women who test positive for corona virus can get sick while staying at home, but you should immediately contact your doctor if the condition worsens. If the condition worsens, emergency medical attention is the best way to prevent serious complications for the mother and fetus. Doctors may suggest x-rays. Sometimes this is necessary in the process of treating patients in a very serious condition. If you know you are pregnant, doctors must take all necessary precautions during x-rays to ensure the safety of you and your baby. Mothers who are in critical condition and require hospitalization also have an increased risk of preterm birth and should be under close obstetric supervision. Acetaminophen or paracetamol are safe drugs during pregnancy if you have a fever. nine0003
If this is your case, and if you are diagnosed with COVID-19, you should be monitored more closely than other pregnant women. Most healthy pregnant women who test positive for corona virus can get sick while staying at home, but you should immediately contact your doctor if the condition worsens. If the condition worsens, emergency medical attention is the best way to prevent serious complications for the mother and fetus. Doctors may suggest x-rays. Sometimes this is necessary in the process of treating patients in a very serious condition. If you know you are pregnant, doctors must take all necessary precautions during x-rays to ensure the safety of you and your baby. Mothers who are in critical condition and require hospitalization also have an increased risk of preterm birth and should be under close obstetric supervision. Acetaminophen or paracetamol are safe drugs during pregnancy if you have a fever. nine0003
How dangerous is it for my baby if I contracted COVID -19 while pregnant?
We do not have much information to know for sure whether the virus is transmitted from mother to fetus during pregnancy. So far, only three newborns have blood tests that show they would have reacted to the virus during pregnancy. Currently, there is no indication that COVID-19 increases the risk of birth defects, but there are only a few cases of infection with the virus in pregnant women at the most vulnerable stages of pregnancy who have already given birth. High fever at 6 weeks pregnant or 4 weeks after conception can increase the risk of spinal and brain problems in the fetus. This is not directly related to COVID-19and can occur when the temperature rises for any reason. The risk remains fairly low. About 2 women in every 1,000 pregnancies who have an early fever may have a child with this kind of problem, compared to 1 in 1,000 pregnant women who do not have a fever during this period. To exclude such problems, it is recommended to undergo an ultrasound examination at 18-22 weeks of pregnancy.
So far, only three newborns have blood tests that show they would have reacted to the virus during pregnancy. Currently, there is no indication that COVID-19 increases the risk of birth defects, but there are only a few cases of infection with the virus in pregnant women at the most vulnerable stages of pregnancy who have already given birth. High fever at 6 weeks pregnant or 4 weeks after conception can increase the risk of spinal and brain problems in the fetus. This is not directly related to COVID-19and can occur when the temperature rises for any reason. The risk remains fairly low. About 2 women in every 1,000 pregnancies who have an early fever may have a child with this kind of problem, compared to 1 in 1,000 pregnant women who do not have a fever during this period. To exclude such problems, it is recommended to undergo an ultrasound examination at 18-22 weeks of pregnancy.
Your baby is most at risk if you become very ill and go into labor much too early, or if your doctors or midwives recommend an early delivery due to the poor condition of the fetus as a result of the severity of your illness. The closer you are to your due date, the lower the risk to your baby. If you have COVID-19and you give birth, your body will not be able to get as much oxygen as it normally does. This, in turn, can weaken the mechanisms of adaptation of the child in childbirth. It is recommended, whenever possible, to give birth in a hospital where the baby can be closely monitored continuously and where a caesarean section can be performed if necessary. At this time, maternal COVID-19 is not an indication for caesarean section unless otherwise indicated. Based on the limited information regarding the situation when the mother is ill with COVID-19at the time of birth, it is estimated that about one in 20 newborns will show symptoms of infection a few days after birth. It is very likely that they became infected during childbirth. We are best aware of three newborns who required treatment and recovered from COVID-19 infection.
The closer you are to your due date, the lower the risk to your baby. If you have COVID-19and you give birth, your body will not be able to get as much oxygen as it normally does. This, in turn, can weaken the mechanisms of adaptation of the child in childbirth. It is recommended, whenever possible, to give birth in a hospital where the baby can be closely monitored continuously and where a caesarean section can be performed if necessary. At this time, maternal COVID-19 is not an indication for caesarean section unless otherwise indicated. Based on the limited information regarding the situation when the mother is ill with COVID-19at the time of birth, it is estimated that about one in 20 newborns will show symptoms of infection a few days after birth. It is very likely that they became infected during childbirth. We are best aware of three newborns who required treatment and recovered from COVID-19 infection.
Some research on these viruses suggests that an infection similar to COVID-19 may slow down fetal growth. Most experts recommend having at least one ultrasound scan 2 to 4 weeks after infection to make sure the fetus is growing normally. Regular follow-up ultrasounds are also recommended at least every 4 weeks throughout pregnancy to assess fetal growth. nine0003
How dangerous is it for my baby if I get COVID -19 shortly after giving birth?
It is not yet clear whether a mother with COVID-19 should be isolated from her children or not. In different regions, people act differently depending on the availability of available funds and the epidemiological situation with COVID-19 on the ground. It is usually advised to stay with the child if you feel well. In some circumstances, it may be necessary to isolate from the child. You should ask your doctor or midwife if this is necessary for you. You must be careful to prevent passing the virus to your baby. First of all, wash your hands before touching the baby, avoid touching the baby's face, avoid sneezing and coughing on the baby, or wear a mask while caring for the baby. When not directly caring for a child (for example, when the child is sleeping), try to stay at least 2 meters or 6 feet away from the child to reduce the risk of infection to the child. nine0003
When not directly caring for a child (for example, when the child is sleeping), try to stay at least 2 meters or 6 feet away from the child to reduce the risk of infection to the child. nine0003
Can I breastfeed if I have COVID -19?
Several women infected with coronovirus tested their breast milk; no signs of the virus were found in the milk. Therefore, it is considered safe to breastfeed your baby even if you are infected with COVID-19. You must be careful to prevent passing the virus to your baby. First of all, wash your hands before touching the baby, avoid touching the baby's face, avoid sneezing and coughing on the baby, and wear a mask when feeding. Another good alternative would be to use a breast pump or manually express breast milk for someone healthy to feed the baby. If you are using a breast pump or manually expressing breast milk, make sure you wash your hands before you do so. nine0003
What to do if after the birth of a child someone in the family has symptoms COVID -19?
If these people are involved in child care, they must be careful to prevent transmission of the virus to the child. Wash hands thoroughly before touching a child, avoid sneezing and coughing on a child, and wear a mask while caring for a child.
Wash hands thoroughly before touching a child, avoid sneezing and coughing on a child, and wear a mask while caring for a child.
If these people do not need to be in close proximity to the child, it is best if they stay at least 2 meters or 6 feet away from the child at all times. Remember to wash your hands when caring for a child, even if you are not sick, as you may have touched objects in the home that have come into contact with the virus. You should also stay 2 meters or 6 feet away from those who get sick and wash your hands regularly to prevent infection. If you have already had COVID-19, recent studies suggest that you can fight the virus and not get sick again. But even then, washing your hands before touching your baby is the best way to prevent transmission of the virus to your baby from those who are sick or through objects they have touched.
| Questions to ask your doctor or midwife as advice may vary around the world:
|
Note:
The data contained [in this document/on our website] is provided for general information only. They are not intended to be used as medical advice on which you should rely. You should seek professional or specialist medical advice regarding your individual situation before taking or refraining from taking any action based on the information contained [in this document/on our website]. While every effort has been made by us to update the information contained [in this document/on our website], we make no warranty that the information contained [in this document/on our website] is accurate, complete and up to date. nine0126
nine0126
Last updated March 28, 2020 Usually, a cold means inflammation of the respiratory tract caused by viruses (ARVI). These infections are contagious and are more common during the cold season. The average person gets infected less than three times a year. If you get sick more often 1 , this indicates health problems. We will tell you what frequent colds are associated with, why they are dangerous, and how to avoid them. nine0003 Permanent SARS usually proceed for a long time and hard. This increases the risk of developing complications that affect the quality of life and threaten health. Among them: ● Spread of infection to the ear (otitis media), paranasal sinuses (sinusitis), larynx and vocal cords (laryngitis), trachea (tracheitis), bronchi (bronchitis), lungs (pneumonia). ● Autoimmune inflammation of the joints (rheumatoid arthritis), heart (rheumatic heart disease), kidneys (glomerulonephritis), connective tissue throughout the body (systemic lupus erythematosus). ● Development of non-atopic bronchial asthma. This is a chronic inflammation of the bronchopulmonary tree caused by an allergy to viral proteins. This form of asthma occurs more often in children older than 10-12 years and adults. ● Exacerbation of chronic diseases of the lower respiratory tract, cardiovascular and urinary systems. Decompensation of diabetes mellitus is likely - the inability to control blood sugar levels. Constant colds are an alarming sign: it is worth taking care of your health and understanding the causes of the development of the disease. This usually indicates a weakening of the immune system. Chronic immunodeficiency over time can trigger dangerous diseases of other organs and systems, including oncology. nine0003 In young children, frequent colds can provoke mental disorders, a delay in general and speech development. The child rarely communicates with peers - this interferes with social adaptation. The work of the immune system is closely connected with the endocrine and nervous systems, metabolic processes in the body. Any violations reduce immune functions. nine0141 2 Common causes of immune suppression: ● Chronic inflammation - infections, allergic and autoimmune non-infectious inflammatory processes. The immune system spends a lot of resources to fight them, so its effectiveness is reduced. ● Metabolic and endocrine diseases: diabetes mellitus, dysfunction of the thyroid gland, adrenal glands, liver, as well as obesity, malnutrition, atherosclerosis. ● Difficulty in nasal breathing. Often associated with a deviated septum or adenoids (in children). Due to pathology, the respiratory tract is often supercooled and irritated, microbes enter the least protected areas of the mucous membranes and inflammation develops. ● Treatment with drugs that suppress the immune system - hormones corticosteroids, anticancer. ● Irrational use of antibiotics and antiseptics. Microorganisms that inhabit the skin and mucous membranes synthesize biologically active substances that affect the regulation of immune processes 3 . If you often take antibiotics and use antiseptics, they will destroy the beneficial microflora. ● Stress. In response to an external stimulus, the body produces the hormone cortisol, which depresses the immune system. The same reaction occurs in the body and hypothermia - cold stress 4 . ● Improper nutrition. A poor diet leads to malnutrition, an excess leads to obesity. A diet that is unbalanced in essential nutrients, vitamins, minerals creates a deficiency of "building material" for the immune system. ● Bad habits and bad ecology - smoke, dust, too dry air. These factors irritate the mucous membranes and create favorable conditions for the reproduction of microbes. Congenital immunodeficiency and acquired immunodeficiency syndrome due to HIV infection occur. nine0003 General recommendations. To avoid frequent colds, follow simple rules. They will help reduce the harm of external factors for the body and strengthen the immune system. ✅ Eat well . Give up fast food and unhealthy snacks in favor of homemade food. Make sure that the diet contains vitamins and vegetable fiber - they maintain a balance of beneficial bacteria in the body. Avoid protein, carbohydrate and other mono-diets. nine0003 ✅ Take vitamins. Even a balanced diet does not completely cover a person's need for vitamins 5 . In winter, anti-cold vitamin-mineral complexes, vitamin D are useful. A doctor will help you choose the right drugs. ✅ Avoid sudden changes in temperature. Avoid hypothermia - wear a scarf and a hat in the cold, do not turn on the air conditioner at full power, turn it off at night. ✅ Exercise, move more . Walking at an average pace for 30-40 minutes a day will improve the blood supply to the body and lung function, and strengthen the immune system. But try to avoid constant overwork, this will reduce immune protection. Start lightly and work your way up to moderate workouts 6 . ✅ Create a safe microclimate in the house. Ventilate the room frequently, but beware of drafts and hypothermia. During the heating period, use a humidifier. A dry environment favors the reproduction of viruses and bacteria, while in humid air they die. nine0003 ✅ Temper yourself. Sunbathe, but avoid overheating and burns. Spend more time outdoors, go barefoot at home. Dousing your feet with cold water for 20-30 seconds every day reduces the frequency of colds. Short-term cooling strengthens the immune defenses 7. ✅ Do not self-medicate. Take your medicines as directed by your doctor. Do not use soaps, body gels with antimicrobial additives. They destroy bacteria that are good for the immune system. nine0003 Therapy. If you lead a healthy lifestyle but still get sick often, get tested. Perhaps the immune system reduces the latent disease. Often the cause of the load on the immune system is: ● caries, sinusitis, chronic tonsillitis and otitis media; ● herpesvirus infections - cytomegalovirus, Epstein-Barr virus, herpesoma type 6 9 ; nine0003 ● Allergy, bronchial asthma; ● Blood glucose level in diabetes mellitus. To accurately determine the cause and prescribe treatment, you will need the help of a therapist and narrow specialists - an immunologist-allergist, an otolaryngologist, an infectious disease specialist, an endocrinologist. Vitamins and drugs. If the examination reveals nothing, the immunologist will assess the immune status and prescribe: ● Vitamins C and E in therapeutic doses. ● Interferons and immunoglobulins are products of the immune system that are not produced enough in immunodeficiencies ● Immunomodulators - depending on the nature of the damage to the immune system. During the rise in the incidence of acute respiratory viral infections, taking the drug Nobasit ® increases the body's resistance to viral infections. According to the instructions for medical use Nobazit, Nobazit Forte ® it is advisable to take the drug with ascorbic acid and other vitamins 10 . The main preventive measure is vaccination . Vaccination "teach" the immune system to produce antibodies to a particular type of microbe. Vaccination reduces the risk of infection, but if you do get infected, you will get the disease with minimal consequences. During a epidemic, limit contact with infected people and avoid large crowds. But if contact with a patient with ARVI nevertheless happened, when the first symptoms appear, it is better to start taking antiviral drugs as soon as possible. A drug with a direct antiviral effect - Nobasit ® - begins to act already 2 hours after taking 10 and reduces the level of virus replication by 100 times already after 4 hours 11 ! The active substance of Nobasit - enisamia iodide - prevents viruses from entering the cells of the body and limits the spread of viruses to neighboring tissues 10 . Practice good personal hygiene : Wash your hands often, use disinfectant wipes. ➢ A person is said to have a frequent cold if they get sick more than four times a year. ➢ It is dangerous to get sick often - this can lead to inflammation of the ENT organs and lower respiratory tract, autoimmune diseases, bronchial asthma, exacerbation of chronic diseases. ➢ The main cause of persistent colds is a weakened immune system. Usually, immunity is suppressed against the background of chronic infectious and non-infectious diseases, unfavorable living conditions, and hereditary factors. nine0003 ➢ To combat frequent colds, follow a healthy lifestyle, strengthen your immune system. Get tested to identify the cause of recurring SARS. 1 Pavlova K.S., Kurbacheva O.M. A difficult patient is a patient with frequent recurrent diseases of the respiratory tract. // Farmateka - No. 6, 2015. 2 M.C. Mammadov Metabolic immunosuppression: mechanisms of development and clinical and pathogenetic significance // Biomedicine - No. 2, 2011. nine0003 3 Chaplin A.V., Rebrikov D.V., Boldyreva N.M. Human microbiome // Bulletin of the Russian State Medical University - No. 2, 2017. 4 Gein S.V., Sharav'eva I.L. Immunomodulatory effects of cold stress // Advances in Modern Biology - V. 138, No. 3, 2018. 5 L.M. Zhitnikova Vitamin-mineral complexes in the prevention of influenza and SARS in adults // Medical business - No. 3, 2012. 6 Bulycheva N.A. The impact of physical education on the immune system // Modern science - No. 6-1, 2021. nine0003 7 Martyniuk N. 8 Gein S.V., Sharavyeva I.L. Immunomodulatory effects of cold stress // Advances in Modern Biology - V. 138, No. 3, 2018. 9 Pavlova K.S., Kurbacheva O.M. A difficult patient is a patient with frequent recurrent diseases of the respiratory tract. // Farmateka - No. 6, 2015. nine0003 10 Instructions for medical use (Nobasit®, film-coated tablets 250 mg; RU: LP-003508 dated 03/16/2016) 11 Activity of enisamium, an isonicotinic acid derivative, against influenza viruses in differentiated normal human bronchial epithelial cells. Boltz D, et al. Antivir Chem Chemother. 2018 Jan-Dec 12 Komarovsky E.O. Influenza and SARS: the simplest instruction // Fundamentals of life safety - No.
Why persistent colds are dangerous
 The complication is often found in children, young people and middle-aged patients. nine0003
The complication is often found in children, young people and middle-aged patients. nine0003 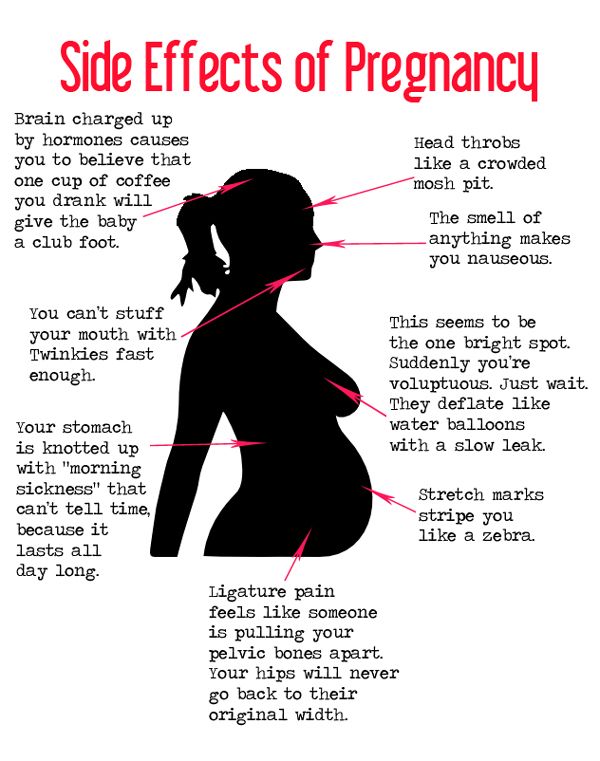 Constant nasal congestion, inflammation of the lymphoid tissue do not allow you to correctly reproduce sounds.
Constant nasal congestion, inflammation of the lymphoid tissue do not allow you to correctly reproduce sounds. Why immunity decreases
 nine0003
nine0003
How to deal with frequent colds
 But try not to get too wrapped up. If you sweat in too warm clothes, even a slight draft will lead to a cold. nine0003
But try not to get too wrapped up. If you sweat in too warm clothes, even a slight draft will lead to a cold. nine0003  8 . Before hardening, be sure to consult a doctor.
8 . Before hardening, be sure to consult a doctor.

Cold prevention
 Today, a flu vaccine is available, and people prone to frequent colds benefit from vaccination against pneumococcal pneumonia, one of the most common complications of SARS. Vaccination should be done only in the absence of signs of a cold and / or after a course of immunomodulatory therapy. nine0003
Today, a flu vaccine is available, and people prone to frequent colds benefit from vaccination against pneumococcal pneumonia, one of the most common complications of SARS. Vaccination should be done only in the absence of signs of a cold and / or after a course of immunomodulatory therapy. nine0003  Try to touch your face less frequently. Moisten your nasal cavity with saline solution. The simplest solution recipe is a teaspoon of salt per liter of boiled water 12 . However, it is more convenient to use ready-made pharmaceutical preparations based on sea salt. nine0003
Try to touch your face less frequently. Moisten your nasal cavity with saline solution. The simplest solution recipe is a teaspoon of salt per liter of boiled water 12 . However, it is more convenient to use ready-made pharmaceutical preparations based on sea salt. nine0003 Briefly about the main
 S., Datskevich I.A. Historical and methodological aspects of the use of water hardening for the improvement of children and adults // Modern health-saving technologies - No. 4, 2017.
S., Datskevich I.A. Historical and methodological aspects of the use of water hardening for the improvement of children and adults // Modern health-saving technologies - No. 4, 2017. 
 Should I take a diagnostic test?
Should I take a diagnostic test?