When is miscarriage stage over
Miscarriage | NHS inform
A miscarriage is the loss of your baby before 24 weeks. Early miscarriages happen in the first 12 weeks of pregnancy. Late miscarriages happen between 12 and 24 weeks.
Most of the time there’s no clear reason why it happens, but it’s very unlikely to be caused by anything you did or didn’t do.
About 1 out of 5 pregnancies miscarry. Since many miscarriages aren't recorded the figure might be higher.
What causes a miscarriage?
Doctors think most miscarriages are caused when the building blocks controlling the development of a baby (the chromosomes) aren’t right. Babies with too many or not enough chromosomes won't develop properly. This leads to a miscarriage.
Miscarriages can also be caused by:
- issues with your placenta
- cervical weakness - when your cervix (neck of your womb) starts to open
Early miscarriages
An early miscarriage happens in the first 12 weeks of pregnancy. Most women who miscarry do so in the first 12 weeks of their pregnancy.
Many women have a miscarriage before they even know they’re pregnant. If this happens it can feel like a late period with heavy bleeding.
Symptoms of an early miscarriage
You might be having an early miscarriage if:
- you're bleeding from your vagina
- you've cramps in your lower abdomen – these can feel like bad period pains
- there's fluid or tissue coming from your vagina
- your breasts are no longer tender and any morning sickness has passed
Bleeding
Having some light bleeding's fairly common in the first 12 weeks of pregnancy and doesn't necessarily mean you're having a miscarriage.
If you start bleeding, you should always contact your GP or midwife and get advice about what to do.
What happens during an early miscarriage
If you’re in the early weeks of pregnancy:
- you’ll probably be asked to go to the early pregnancy unit at your local hospital straight away
- you’ll have some tests and usually an ultrasound scan
- your body usually completes the miscarriage naturally
Depending on your stage of pregnancy, you may deliver a small baby.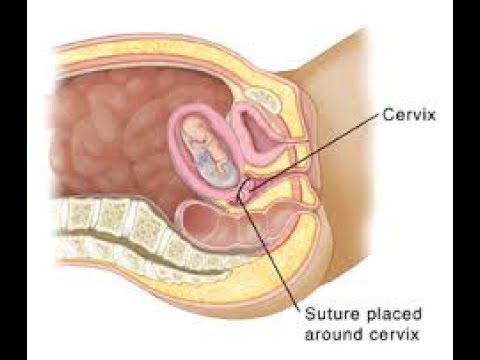 That can be a shock and is an understandably upsetting time.
That can be a shock and is an understandably upsetting time.
Late miscarriages
A late miscarriage happens after 12 weeks and before 24 weeks.
For many parents who lose their baby after a late miscarriage, the word ‘miscarriage’ doesn't properly express the impact of their loss. The loss of a baby at any time's a terrible shock and a late miscarriage can be especially hard.
Symptoms of a late miscarriage
You might be having a late miscarriage if:
- you're bleeding from your vagina – this can be heavy and you might have blood clots
- you've strong, cramping pains
Always get medical help if:
- you're bleeding
- your baby’s movements have changed or you haven’t felt any movements for a while.
- your waters break and your baby's born very quickly
Contact your midwife or local maternity unit if you’re registered with them. If you’re not registered, contact your GP or phone the NHS 24 111 service.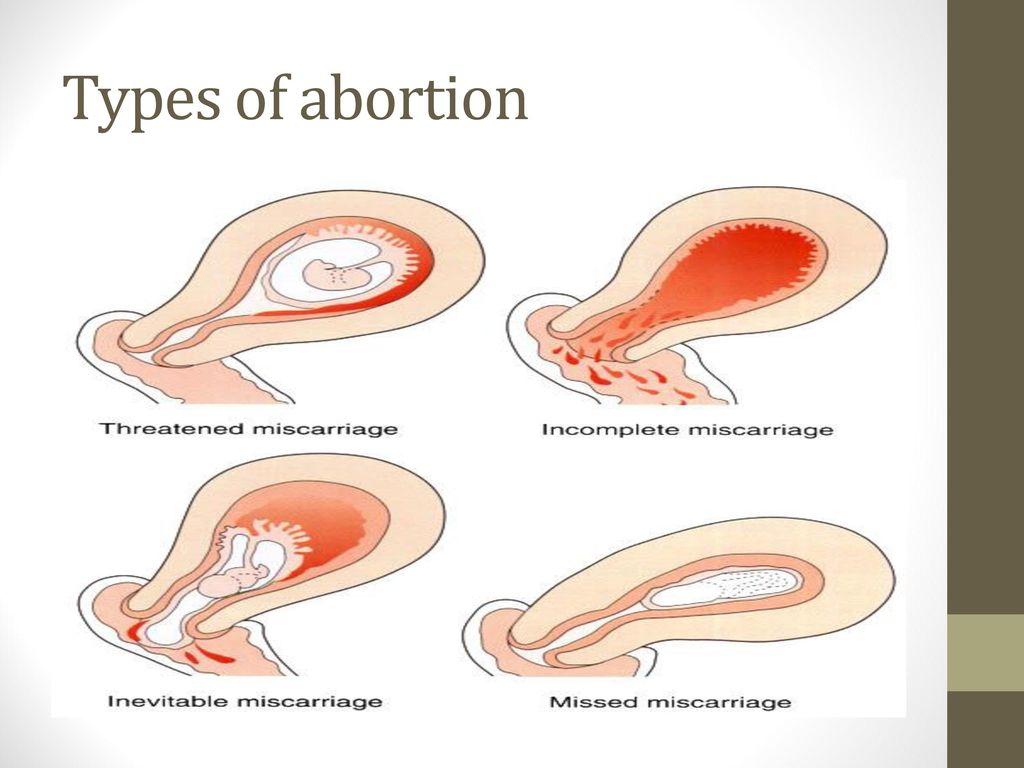
What happens during a late miscarriage
If you’re later on in pregnancy:
- you may be asked to go to the maternity ward
- you’ll have some tests and usually an ultrasound scan
- you're likely to go through labour in hospital and might have your labour induced
While you deliver your baby you're likely to have heavier bleeding and labour-like pains.
Making difficult decisions
If you're having a miscarriage, your doctor or midwife will:
- talk to you about what will happen next
- help you, and your partner if you have one, decide what you’d like to do
You may have many difficult decisions to make at this time and will have overwhelming emotions. Take your time. Your midwife or doctor can help, and there are many organisations that can support you, your baby’s father and your family.
Get support from SANDS
Get support from SiMBA
After a miscarriage
Depending on your circumstances and stage of pregnancy, your midwife or doctor may ask if you'd like to see or hold your baby.
Some parents decide they don't want to see their baby, and others choose not to for faith or cultural reasons. This is a decision only you can make. It can be very hard when you're feeling overwhelmed. Whatever you decide is okay.
If you’re worried about what your baby looks like, your midwife or doctor can describe them to help you decide.
If your symptoms continue
You’ll probably have some bleeding for a week or two. If you continue to have symptoms after your miscarriage, it may mean that some of the pregnancy tissue's still in your womb.
Some women may need medicine or a short operation to treat this.
If you’re worried about seeking treatment, maybe a friend can come with you. Having support's really important at this difficult time.
Taking time off work
Many women will want to take time off work after having a miscarriage.
If you have a miscarriage before the end of the 24th week, you’re entitled to:
- take sick leave
- any sick pay you'd normally qualify for
If you lose your baby after the end of the 24th week, you’re entitled to:
- take maternity leave
- any maternity pay you qualify for
Speak to your employer about which choices may be right for you and your family.
Working Families has more about your rights at work after a miscarriage
Repeated miscarriages
Most women go on to have a successful pregnancy and a healthy baby after a miscarriage. But unfortunately, some women have repeated miscarriages.
If you've had:
- 1 or 2 miscarriages - you're not more likely than anyone else to have another one
- 3 or more miscarriages - your GP can refer you to a specialist to see whether there’s a specific cause
Miscarriage Rates by Week: Causes and Risks
Miscarriage Rates by Week: Causes and RisksMedically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
Overview
Miscarriage is a word used to describe the early loss of a pregnancy before 20 weeks of pregnancy. It usually happens in the first trimester.
Unfortunately, between 10 and 15 percent of known pregnancies end in miscarriage.
You may have heard of couples waiting to announce a pregnancy until the risk of having a miscarriage is lower. The further you are into the pregnancy, the less likely you are to miscarry.
The further you are into the pregnancy, the less likely you are to miscarry.
Read on to learn about what causes miscarriages and the risk for miscarriage during pregnancy.
Causes
Dr. Kaylen Silverberg, a Texas-based fertility specialist, says miscarriages are very common.
“Women think that when they have one miscarriage, they are doomed to miscarry again,” he says. However, the likelihood of having recurrent miscarriages (at least 2 or 3) is low, only occurring in about 1 percent of women.
Studies have shown an increased risk for miscarriage in women who have had recurrent miscarriages in the past. Conversely, some studies indicate that having a successful pregnancy before a current pregnancy may decrease the risk for miscarriage in the current pregnancy.
Several factors have to be accounted for in these cases, however. This includes maternal age and other medical conditions present. Most doctors will begin to investigate for a cause after you have had two to three losses. This will include reviewing your medical history in detail and performing certain tests.
This will include reviewing your medical history in detail and performing certain tests.
Here are the five most common miscarriage causes.
Genetics
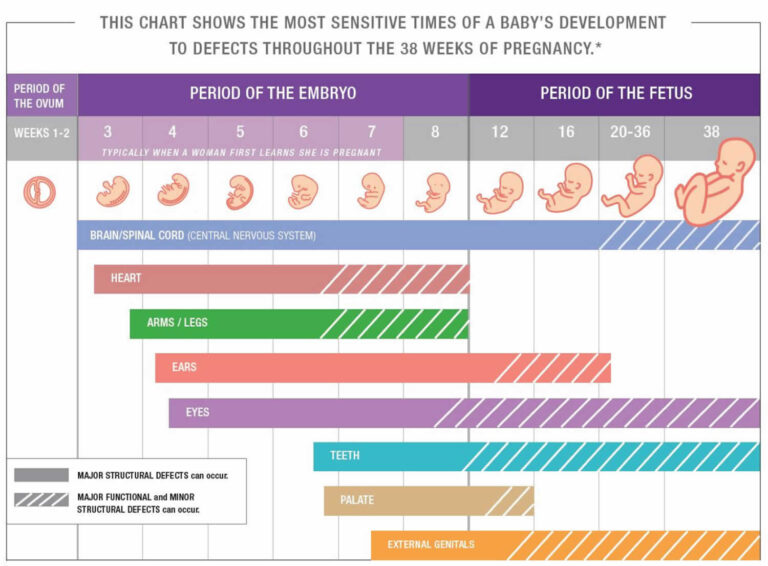
When the sperm and egg meet, the cells come together. They then begin to divide to start forming the genetic material that makes up a person.
Each of us is supposed to have 46 total chromosomes. That’s 23 from one parent and 23 from the other. If something goes wrong when the cells are dividing, a chromosome may be missing or repeated.
About 50 percent of all first trimester miscarriages are because of chromosomal abnormalities. This can occur more frequently in women who are considered advanced maternal age, or greater than 35 years old at pregnancy term.
Infections
Uterus or cervix infections can be dangerous to a developing baby and lead to miscarriage. Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Some of these infections include:
- listeria
- parvovirus B19
- toxoplasma gondii
- rubella
- herpes simplex
- cytomegalovirus
Anatomic problems
This refers to defects of the uterus cavity.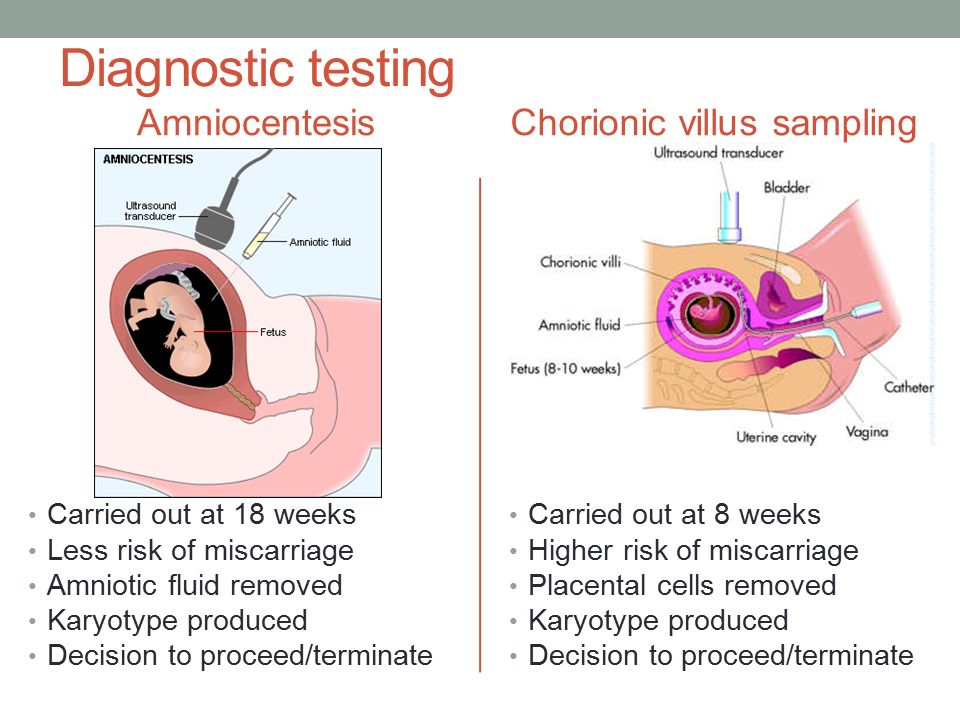 If a woman’s uterus didn’t form correctly when she was developing, it may be unable to support a healthy pregnancy.
If a woman’s uterus didn’t form correctly when she was developing, it may be unable to support a healthy pregnancy.
Clotting disorders
Clotting disorders are conditions that cause your body to form more blood clots than normal. Examples include lupus anticoagulant and antiphospholipid syndrome.
In the case of pregnancy, blood clots can form in the placenta. This prevents nutrition and oxygen from getting to the baby-to-be, and prevents waste from being carried away.
Risk rates
The first trimester of pregnancy is considered weeks 0 to 13. About 80 percent of miscarriages happen in the first trimester. Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Weeks 0 to 6
These early weeks mark the highest risk of miscarriage. A woman can have a miscarriage in the first week or two without realizing she’s pregnant. It may even seem like a late period.
Age plays a role in a woman’s risk factor. One study indicated that compared to women younger than 35:
One study indicated that compared to women younger than 35:
- Women ages 35 to 39 have a 75 percent increase in risk
- Women ages 40 and older are at 5 times the risk
Weeks 6 to 12
Once a pregnancy makes it to 6 weeks and has confirmed viability with a heartbeat, the risk of having a miscarriage drops to 10 percent. According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
Weeks 13 to 20
By week 12, the risk may fall to 5 percent. But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
Signs and symptoms
The most common signs of a miscarriage are bleeding and cramping that are felt in the abdomen, pelvis, or lower back.
Some women have spotting (light bleeding) during pregnancy. A few drops or light flow of brown or dark red doesn’t necessarily mean trouble.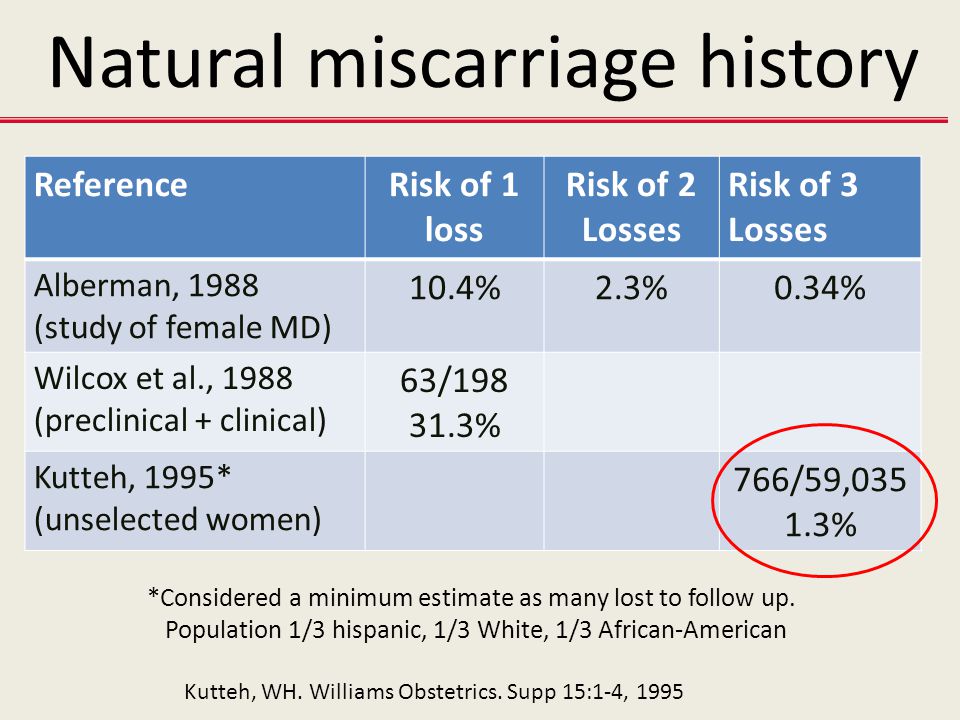 But call your doctor right away if you see bright red blood, particularly in large amounts.
But call your doctor right away if you see bright red blood, particularly in large amounts.
Cramping can also happen in normal pregnancies. But if it’s severe or occurring more on one side of the pelvis, you should call your doctor.
Prevention
The majority of miscarriages are the result of genetic abnormalities or other health factors that are beyond our control. For that reason, there isn’t a whole lot you can do for prevention.
The best thing you can do is to keep yourself as healthy as possible before trying to conceive and throughout your pregnancy. Here are some tips to staying healthy during pregnancy:
- Eat a well-balanced diet.
- Exercise regularly.
- Avoid alcohol, recreational drugs, and cigarette smoking.
- Reduce caffeine to 200 mg or less per day.
- Get regular prenatal visits.
If you’re worried about your risk of having a pregnancy affected by chromosomal issues, you can speak to your doctor about genetic testing before trying to conceive.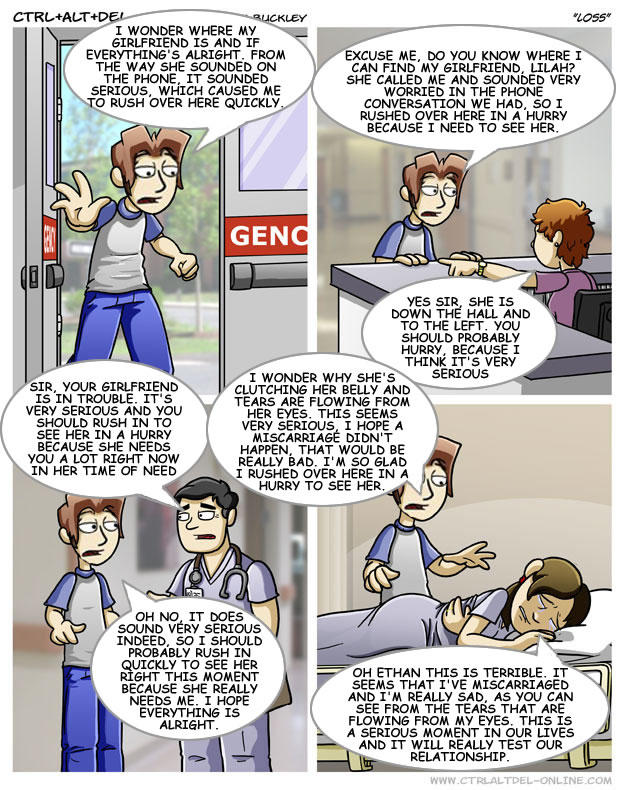 A blood sample will be taken from one or both partners, and then sent to a laboratory to be evaluated for major genetic disorders. This testing and other evaluation are generally done after someone has recurrent losses.
A blood sample will be taken from one or both partners, and then sent to a laboratory to be evaluated for major genetic disorders. This testing and other evaluation are generally done after someone has recurrent losses.
The takeaway
The experience of a miscarriage can be physically and emotionally painful. But it’s important to remember that it’s not your fault. Talk to trusted friends and family, and ask for help when you need it.
Your doctor may be able to recommend a support group or therapist in your area. There are also many online organizations and support groups like March of Dimes that offer a safe place to share your story and grieve with others.
Share on Pinterest
Rena Goldman is a journalist and editor who lives in Los Angeles. She writes about health, wellness, interior design, small business, and the grassroots movement for campaign finance reform. When she’s not glued to a computer screen, Rena likes to explore new hiking spots in Southern California. She also enjoys walking in her neighborhood with her dachshund, Charlie, and admiring the landscaping and architecture of LA homes she can’t afford. Follow her on Twitter: @ReeRee_writes
She also enjoys walking in her neighborhood with her dachshund, Charlie, and admiring the landscaping and architecture of LA homes she can’t afford. Follow her on Twitter: @ReeRee_writes
Last medically reviewed on October 3, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chromosomal conditions. (2018).
marchofdimes.org/baby/chromosomal-conditions.aspx - Early pregnancy loss: FAQs. (2015).
acog.org/Patients/FAQs/Early-Pregnancy-Loss - Early pregnancy loss: Practice bulletin. (2015).
acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Early-Pregnancy-Loss - Ford HB, et al.
 (2009). Recurrent pregnancy loss: Etiology, diagnosis, and therapy.
(2009). Recurrent pregnancy loss: Etiology, diagnosis, and therapy.
ncbi.nlm.nih.gov/pmc/articles/PMC2709325/ - Maconochie N, et al. (2007). Risk factors for first-trimester miscarriage—results from a UK-population-based case-control study.
obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.2006.01193.x - Miscarriage. (2017).
marchofdimes.org/complications/miscarriage.aspx - Regan L, et al. (1989). Influence of past reproductive performance on risk of spontaneous abortion.
uptodate.com/contents/definition-and-etiology-of-recurrent-pregnancy-loss/abstract/19 - Repeated miscarriages. (2016).
acog.org/Patients/FAQs/Repeated-Miscarriages - Tong S, et al. (2008). Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit.
ncbi.nlm.nih.gov/pubmed/18310375 - Tulandi T. (2018). Patient information: Miscarriage (beyond the basics).

uptodate.com/contents/miscarriage-beyond-the-basics
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Rena Goldman
Medically Reviewed By
Holly Ernst, PA-C
Share this article
Medically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
related stories
How to Tell if You’re Having a Miscarriage Without Bleeding
When Is the Best Time to Announce Your Pregnancy?
What’s a Chemical Pregnancy?
How Long Does a Miscarriage Last?
Late Miscarriage: Symptoms and Finding Support
Read this next
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
A miscarriage is also known as a pregnancy loss.
 These are the symptoms, causes, and a look at how to move forward.
These are the symptoms, causes, and a look at how to move forward.READ MORE
When Is the Best Time to Announce Your Pregnancy?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
If you’re expecting, you might be wondering when it’ll be safe to tell family and friends. Here’s how to decide when to share the news of your…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
A chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
Late Miscarriage: Symptoms and Finding Support
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
It can be devastating to experience a miscarriage in your second trimester. Find support and information here.
READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
Threatened Abortion (Threatened Miscarriage)
Threatened abortion refers to vaginal bleeding during the first 20 weeks of pregnancy. Learn about its symptoms, risk factors, and diagnosis.

READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
An obstetrician-gynecologist at the SM-Clinic Center for Reproductive Health spoke about whether it is possible not to notice a miscarriage
Unfortunately, the loss of a child at an early stage of pregnancy is quite common. After the first miscarriage, a woman lives in constant fear and is afraid that the second attempt to become a mother will turn into a tragedy.
After the first miscarriage, a woman lives in constant fear and is afraid that the second attempt to become a mother will turn into a tragedy.
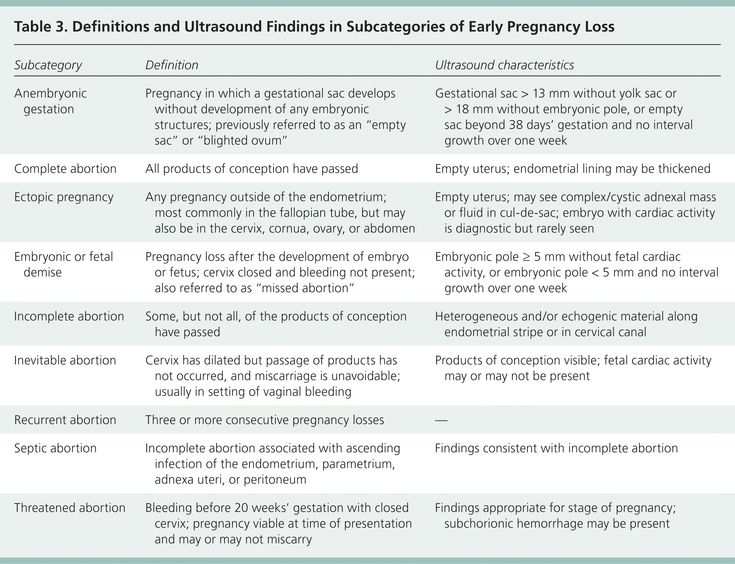
“A miscarriage is the spontaneous termination of a pregnancy before the fetus reaches a viable term. A fetus weighing up to 500 g is considered viable, which corresponds to a period of less than 22 weeks of pregnancy. Many women face this diagnosis. About 80 percent of miscarriages occur before 12 weeks of pregnancy." nine0007
Causes of miscarriage
Approximately half of early miscarriages occur due to genetic pathologies in the development of the fetus, that is, from defects in the number and composition of chromosomes. It is in the first weeks that the formation of the baby's organs begins, which requires 23 normal chromosomes from each of the future parents. When at least one abnormal changes occur, there is a risk of losing a child.
At 8–11 weeks, the rate of such miscarriages is 41–50 percent, at 16–19 weeksweeks of pregnancy, the frequency of miscarriages caused by chromosomal defects drops to 10 to 20 percent.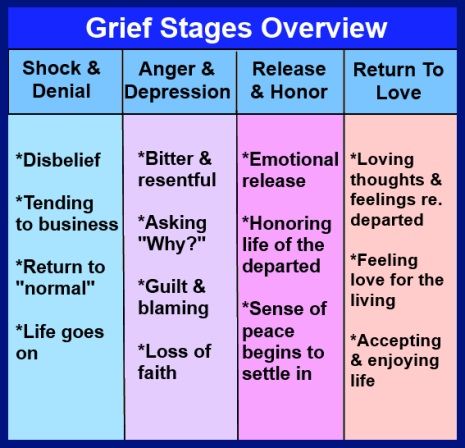
There are other causes of miscarriage. Among them:
- Congenital and acquired disorders of the anatomy of the genital organs If there are fibroids, polyps in the uterus, this can cause abnormal development of the embryo. The threat of miscarriage may be in women with an abnormal development of the uterus.
- Infectious causes Numerous studies have shown that the risk of miscarriage increases in the presence of sexually transmitted infections. Dangerous for a pregnant woman are measles, rubella, cytomegalovirus, as well as diseases that occur with an increase in body temperature. Intoxication of the body often leads to the loss of a child.
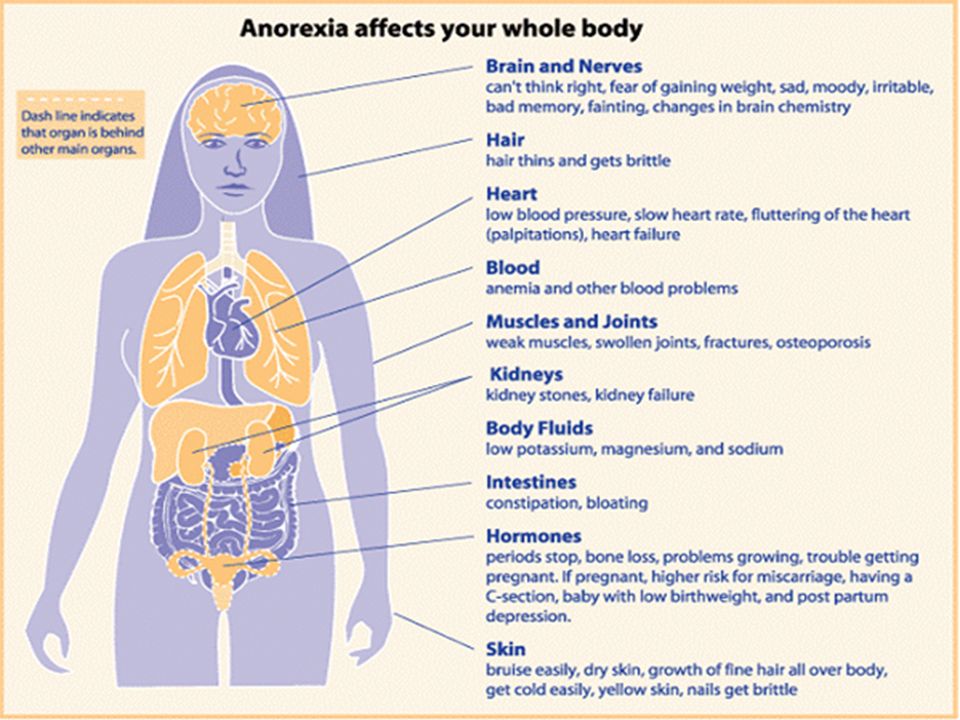
- Endocrine causes Problems with gestation occur with diabetes, thyroid diseases, disorders of the adrenal glands.
- Unfavorable ecology, exposure
- Blood clotting disorder (thrombosis, antiphospholipid syndrome) APS (antiphospholipid syndrome) is a disease in which the human body produces a lot of antibodies to phospholipids, the chemical structures that make up parts of cells.
 The body mistakenly perceives its own phospholipids as foreign and begins to defend itself against them: it produces antibodies to them that damage blood components. Blood clotting increases, microthrombi appear in small vessels that feed the fetal egg and placenta. Blood circulation in the fetal egg is disturbed. As a result, the pregnancy stops or the growth of the fetus slows down. Both of these lead to miscarriage. All this is due to the hormonal background that has changed during pregnancy. nine0018 Lifestyle and bad habits Nicotine addiction, alcohol use, obesity.
The body mistakenly perceives its own phospholipids as foreign and begins to defend itself against them: it produces antibodies to them that damage blood components. Blood clotting increases, microthrombi appear in small vessels that feed the fetal egg and placenta. Blood circulation in the fetal egg is disturbed. As a result, the pregnancy stops or the growth of the fetus slows down. Both of these lead to miscarriage. All this is due to the hormonal background that has changed during pregnancy. nine0018 Lifestyle and bad habits Nicotine addiction, alcohol use, obesity. Is it possible not to notice a miscarriage
Sometimes women mistake a miscarriage for normal menstruation. This occurs during the so-called biochemical pregnancy, when there is a violation of the implantation of the embryo at a very early stage and menstruation begins. But before the appearance of spotting, the test will show two strips.
The classic variant is when a miscarriage is manifested by bleeding against the background of a long delay in menstruation, which rarely stops on its own.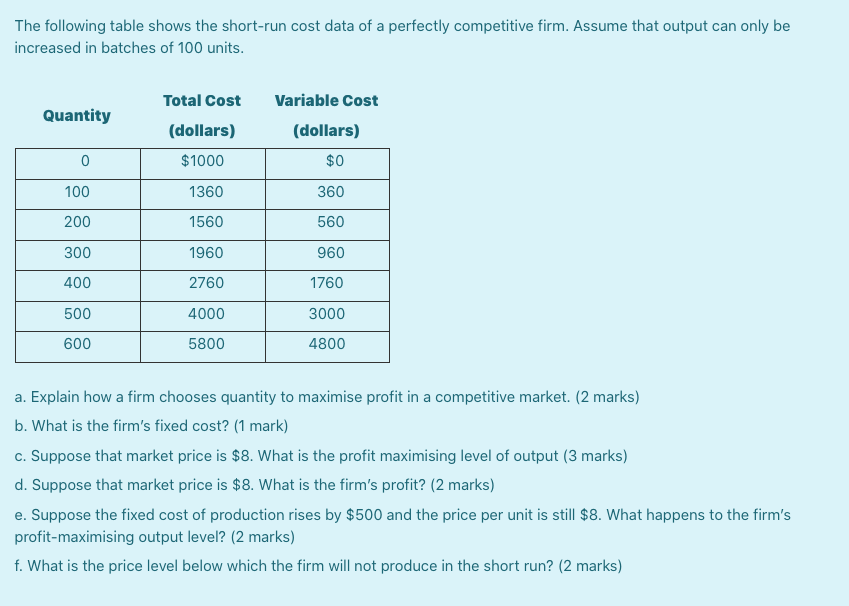 Therefore, even if a woman does not follow the menstrual cycle, the signs of an interrupted pregnancy will be immediately noticed by the doctor during examination and ultrasound. nine0007
Therefore, even if a woman does not follow the menstrual cycle, the signs of an interrupted pregnancy will be immediately noticed by the doctor during examination and ultrasound. nine0007
Alarm
The symptoms of a miscarriage can be completely different, and depending on them, as a rule, it is possible to predict the likelihood of maintaining and successfully continuing this pregnancy.
For the threat of miscarriage is characterized by pulling pains in the lower abdomen and lumbar region, scanty bloody discharge from the genital tract. Ultrasound signs: the tone of the uterus is increased, the cervix is not shortened and closed, the body of the uterus corresponds to the gestational age, the fetal heartbeat is recorded. nine0003
Started miscarriage - pain and discharge from the genital tract are more pronounced, the cervix is ajar.
Miscarriage in progress - cramping pain in the lower abdomen, copious bloody discharge from the genital tract. On examination, as a rule, the uterus does not correspond to the gestational age, the cervix is open, the elements of the fetal egg are in the cervix or in the vagina.
Incomplete miscarriage - the pregnancy was interrupted, but there are delayed elements of the fetal egg in the uterine cavity. This is manifested by ongoing bleeding due to the lack of a full contraction of the uterus. nine0003
Non-progressive pregnancy - the death of an embryo (up to 9 weeks) or a fetus up to 22 weeks of gestation in the absence of any signs of termination of pregnancy.
Important!
Severe abdominal pain and spotting at any stage of pregnancy is a reason for an urgent appeal to an obstetrician-gynecologist with a solution to the issue of hospitalization in a gynecological hospital.
Is it possible to avoid miscarriage
“Today, there are no methods for preventing miscarriages,” the doctor says. “Therefore, it is very important to comprehensively prepare for pregnancy before it occurs by visiting an obstetrician-gynecologist and following all the necessary recommendations for examination and taking the necessary drugs.”
“Therefore, it is very important to comprehensively prepare for pregnancy before it occurs by visiting an obstetrician-gynecologist and following all the necessary recommendations for examination and taking the necessary drugs.”
But if, nevertheless, the pregnancy could not be maintained, then the birth of a child can be planned again no earlier than 3-6 months after the miscarriage. This time is needed to figure out, together with the attending physician, what are the causes of miscarriage and whether it is possible to avoid them in the future. nine0003
By the way, a common misconception for both women and men is that only the woman is to blame for the loss of pregnancy, but this is far from being the case.
“A man is also responsible, which is why future dads are required to perform a study - a spermogram and be tested for genital infections, since with a pathology of spermatozoa, the likelihood of miscarriage due to genetic abnormalities increases many times,” emphasizes our expert.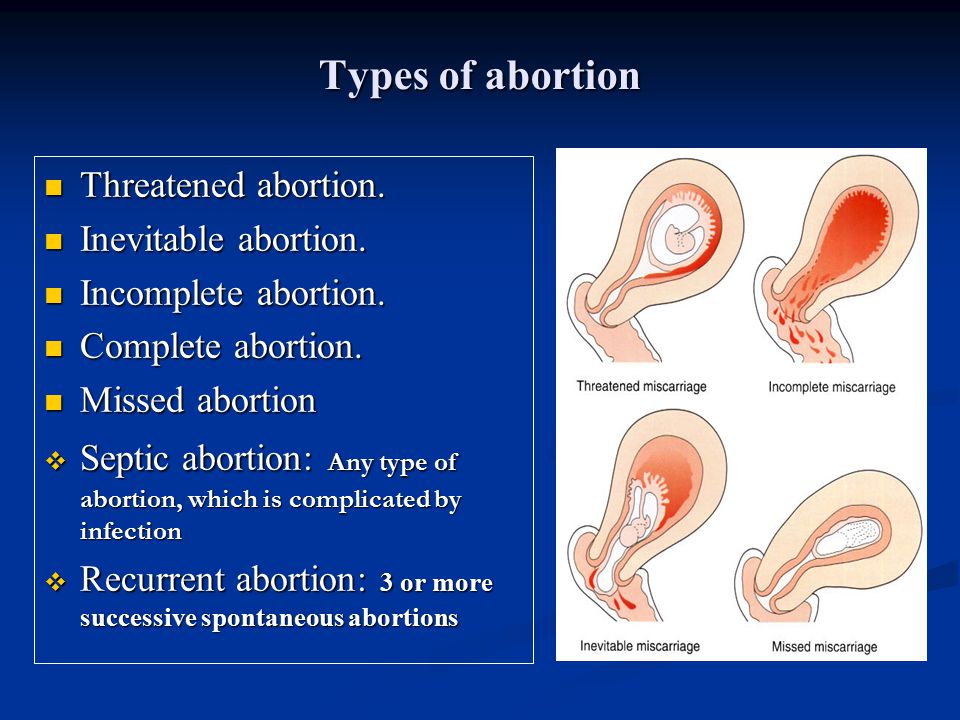
There is always a chance
Most women whose first pregnancy ends in a miscarriage, when examined before pregnancy and the causes are eliminated, have a high chance of a successful next pregnancy (about 85 percent). “A woman who has lost a child needs the support of her family and friends. Sometimes words are unnecessary, just be there. Duty phrases from the series “You will definitely give birth”, “It was just an embryo” hurt very much. The best consolation is to advise you to see a doctor,” says Natalia Kalinina. nine0003
Published on the portal wday.ru
Miscarriage during missed pregnancy | Articles by EMC doctors about diseases, diagnosis and treatment
What is a miscarriage?
According to medical statistics, miscarriage is the most common complication during pregnancy. About 10-20% of all recorded pregnancies end in miscarriage. Miscarriage is a sporadic, sudden, termination of pregnancy, which is accompanied by complete or partial emptying of the uterus.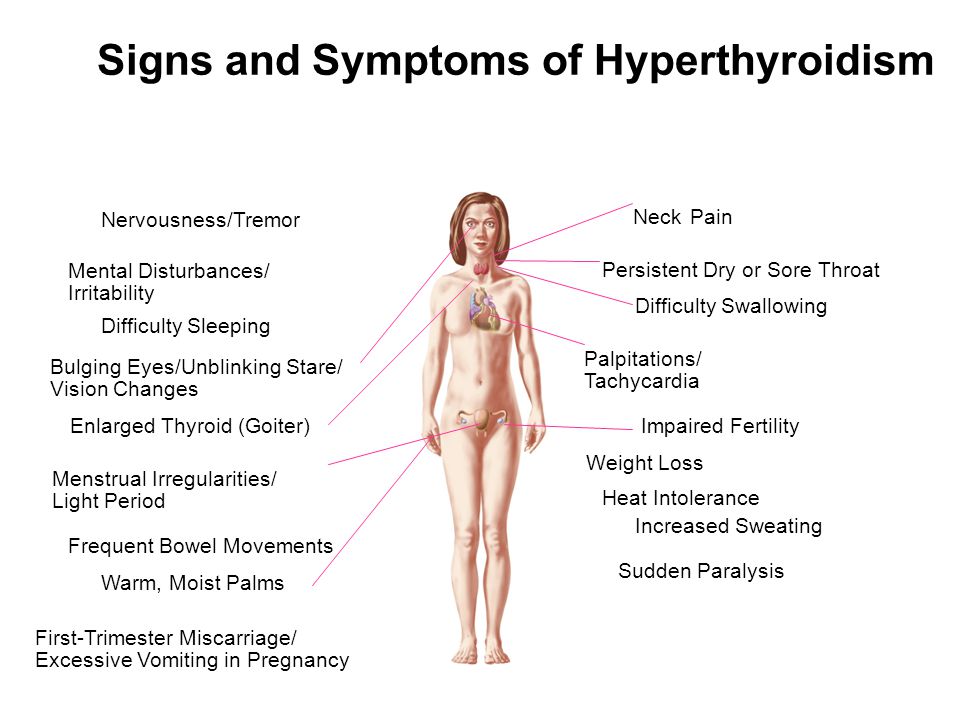 nine0003
nine0003
Missed pregnancy loss (MP) can be seen on ultrasound. It consists in confirming the non-viability of the fetus without bleeding. The ST can end in a miscarriage, when the body gets rid of the dead fetus on its own, or in a medical abortion, when medical or surgical manipulations are used to clean the uterine cavity.
Causes of miscarriage and miscarriage
80% of miscarriages occur in the first trimester before 12 weeks. In 50% of cases, this occurs due to genetic defects in the fetus. The threat of miscarriage due to chromosomal abnormalities decreases with the course of pregnancy: by 20 weeks it is 10-20% versus 41-50% in the first trimester. The main cause of genetically determined early miscarriages are autonomous trisomies - when three homologous chromosomes are present in the cells instead of two. Such defects occur at the time of conception and are not subject to correction. They lead to miscarriage or to the development of severe genetic diseases.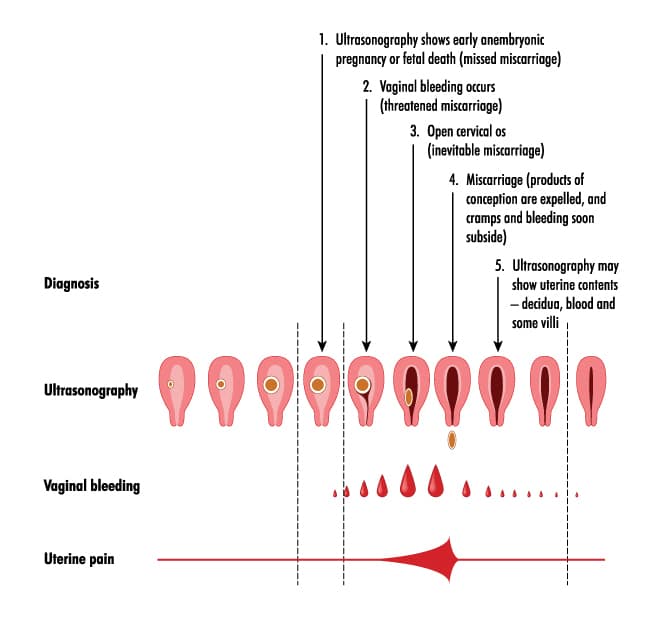 In addition to genetics, immunological, endocrine and infectious causes are distinguished. nine0003
In addition to genetics, immunological, endocrine and infectious causes are distinguished. nine0003
In the second trimester, various diseases and disorders in the mother's body become the main cause of miscarriage.
There is a list of factors that can trigger early pregnancy loss:
-
woman's age. At the age of 20-30 years, the risk of spontaneous miscarriage is 9-17%, at 35-40 years old - 20%, at 40-45 - 40%;
-
alcohol abuse;
nine0023 -
abuse of caffeine;
-
smoking;
-
drug use;
-
chronic diseases of the mother;
-
maternal infections;
-
use of medications incompatible with pregnancy;
- nine0004 history of spontaneous abortion. The risk of subsequent pregnancy loss in women with one miscarriage in history is 18-20%, with two - 30%, with three - 43%.
Symptoms and signs of miscarriage
You can suspect a miscarriage by sudden spotting and sharp pain in the lower abdomen. If these symptoms appear, seek immediate medical attention. The doctor must conduct an ultrasound diagnosis. Transvaginal scanning (TVS) is considered the gold standard for diagnostics - when the sensor is inserted into the uterus through the vagina. If TVS is not available, a transabdominal scan can be applied - through the anterior abdominal wall. nine0003
If these symptoms appear, seek immediate medical attention. The doctor must conduct an ultrasound diagnosis. Transvaginal scanning (TVS) is considered the gold standard for diagnostics - when the sensor is inserted into the uterus through the vagina. If TVS is not available, a transabdominal scan can be applied - through the anterior abdominal wall. nine0003
Missed pregnancy may be asymptomatic and not manifest until the next scheduled ultrasound.
How does a miscarriage happen?
The miscarriage process has four stages. This does not happen overnight and lasts from several hours to several days.
The first stage - the threat of miscarriage. Among the symptoms: pulling pains in the lower abdomen, scanty blood discharge, increased uterine tone. The process of detachment of the placenta from the place of attachment in the uterus begins. The internal os is closed. The main thing is to seek help in time, then with proper therapy if there is a chance to stop the miscarriage and save the pregnancy. nine0003
nine0003
The second stage - the beginning of a miscarriage. Strong discharge, the cervical canal is ajar, the doctor diagnoses the final detachment of the placenta.
The third stage is a miscarriage in progress. You can feel the regular contractions of the uterus, the outcome of the fetus, placenta and uterine contents, profuse blood discharge has begun.
The last fourth stage is a complete miscarriage. The pregnancy is interrupted, the uterine cavity does not contain the fetus and products of conception.
nine0009 How to determine the ST?It should be remembered that a miscarriage can be diagnosed only during an ultrasound examination. Home tests will not give reliable results. Ultrasound will show the presence or absence of a heartbeat in the fetus.
Treatment of miscarriage and miscarriage
Due to the fact that the vast majority of spontaneously terminated pregnancies are due to genetic abnormalities (non-viability) of the fetus, then, speaking about the treatment of miscarriage, it is worth talking about ensuring complete and safe cleansing of the uterus, preventing infection and preventing bruising.