Red behind baby ear
Rash Behind Ear: Causes, Symptoms, and Treatments
The delicate skin behind the ears is a common source for rashes. But they can be difficult to identify and treat because you can’t see the affected area well yourself.
There are many potential causes of a rash behind the ears, from skin irritation caused by haircare products to fungal infections.
Rashes behind the ears may cause itching, redness, swelling, and skin flaking that may range from irritating to painful. Here are some of the common causes of a rash behind the ears.
Eczema (atopic dermatitis)
Eczema is an itchy skin condition that can impact the area of skin behind the ears, as well as most areas of the ear itself. Symptoms of an eczema rash behind the ears include:
- cracked skin
- redness
- scaling
Most people with ear eczema will notice the skin scaling where the ear lobe meets the skin.
Contact dermatitis
Contact dermatitis occurs when you come in contact with something you’re allergic to or that irritates your skin. The ears are vulnerable to contact dermatitis because you may use skin care or hair care products that irritate the skin. Some perfumes, cosmetics, and earrings (especially those made from nickel) can also cause contact dermatitis.
Symptoms of contact dermatitis behind the ear include:
- dry skin
- red, irritated skin
- skin itching
If you’ve used a new skin care or hair care product and experienced skin irritation, those are likely the cause.
Fungal infection
Fungal infections can affect skin folds, such as those behind the ears. Symptoms include:
- blistering
- burning
- itching
- peeling
- scaling of the skin
Ringworm is another type of fungal infection that can cause a red, circular sore on the skin. Sometimes, a person may have more than one rash-like ring behind the ear.
Seborrheic dermatitis
Also known as dandruff or cradle cap, seborrheic dermatitis is a condition that can cause white or yellow scales to form on the scalp. The backs of the ears may also be affected.
The backs of the ears may also be affected.
Other symptoms include itching, thick crusts on the skin, and sometimes clear to yellow drainage. The crusts may flake off.
Granuloma annulare
Granuloma annulare is a skin condition that can cause red, raised skin patches. It sometimes causes similar symptoms to ringworm. You may have just one or multiple skin patches.
In addition to a red rash, you may also notice deep, rounded lumps in the skin of the affected area if you have granuloma annulare.
Lichen planus
Lichen planus is an autoimmune disorder that can cause skin inflammation, including in and around the ears. Doctors call this otic lichen planus. The condition can even cause hearing loss in some people.
Other symptoms of lichen planus include ringing in the ears, bleeding, pain, and drainage from the ears.
Rosea
Pityriasis rosea is a skin condition that causes a pink, scaly rash that may or may not itch.
Most people with the condition first have a viral-type illness, such as a runny nose, sore throat, and unexplained fatigue. The rash related to rosea can last several months. The condition most commonly affects people ages 10 to 35.
The rash related to rosea can last several months. The condition most commonly affects people ages 10 to 35.
Rubella
Also known as the German measles, rubella is a viral infection that causes a rash that may appear behind the neck and ears. The rash usually causes pink or red spots that may come together in patches. After starting on the face and head, the rash may spread downward.
Other symptoms of rubella include:
- appetite loss
- headache
- itching that lasts up to three days
- joint pain
- joint swelling
- runny nose
- swollen lymph nodes
The invention of the rubella vaccine, including the measles, mumps, rubella (MMR) vaccine, has made rubella a rarer condition. However, it’s still possible to contract the virus.
Lupus
Lupus is an autoimmune disorder that can cause rashes or sores to develop on the skin. Not all people with lupus will have skin-related symptoms.
Lupus can cause a rash that appears on areas of skin the sun hits the most, such as the arms, ears, face, legs, and neck.
A lupus rash usually causes red, scaling skin that has rounded or ring-shaped lesions. Exposure to sunlight typically causes them to get worse.
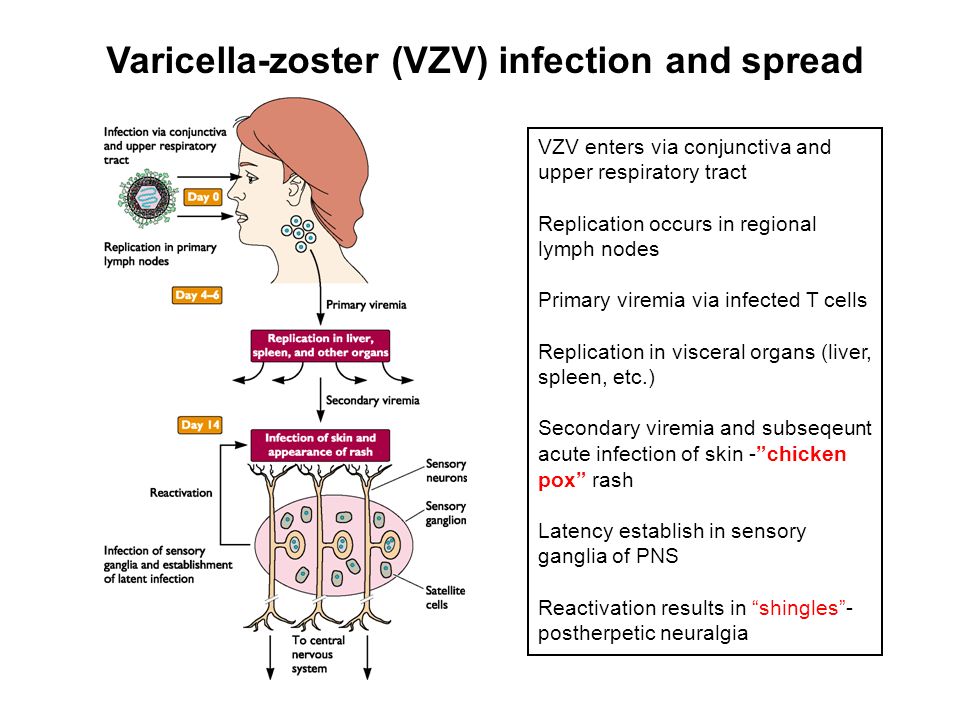
Measles
Measles is a viral infection that can cause a rash that begins on the face and behind the ears before moving to the rest of the body. Measles can be a severe and sometimes deadly infection, especially in children. Although modern vaccines have helped to reduce measles rates in the United States, the condition still affects people worldwide.
Measles causes a skin rash that may appear as flat, red blotches that connect to each other. The condition is highly contagious and can cause symptoms like high fever, sore throat, cough, eye inflammation, and runny nose.
Babies and toddlers can also experience rashes behind the ears due to conditions adults don’t normally get.
One example is intertrigo behind the ears. This skin condition occurs in skin folds, sometimes when a baby’s drool goes behind the ears. The skin can become red, hot to the touch, and sometimes painful.
The skin can become red, hot to the touch, and sometimes painful.
Parents can treat intertrigo by applying zinc creams or other moisture barriers to keep the wetness from damaging the skin.
Another condition that can cause a rash behind the ears is hand, foot, and mouth disease. This condition is common in children in childcare centers and preschools. In addition to a red, blistering rash, a child may have a fever, sore throat, and runny nose.
Seborrheic dermatitis (cradle cap) is another possible condition that affects babies.
Below are some examples of the common sources of rashes behind the ears.
Treatments for rashes behind the ears usually depend on the underlying cause. Keeping the skin clean, dry, and moisturized can often help to treat the rash.
Medical treatment
A doctor may prescribe treatments if a rash behind the ears is due to a fungal or bacterial infection. These include oral or topical antifungal medications or antibiotics. This is especially true if the skin is bleeding and cracking or appears infected.
This is especially true if the skin is bleeding and cracking or appears infected.
Home remedies
If the rash is due to allergic dermatitis, avoiding the substance that caused the rash can help to reduce the rash’s appearance. Here are some other home treatments that may help:
- Clean the affected area with soap and warm water. Always wash your hands before and after touching the rash.
- Apply a fragrance-free anti-itch ointment, or antibiotic skin cream, depending upon your symptoms. Loosely cover the affected area with a bandage, allowing the skin to breathe.
- Refrain from scratching the affected area.
- Apply cloth-covered compresses for swelling skin behind the ears.
A doctor can sometimes diagnose a skin rash by visually examining the affected area and taking a medical history.
If a doctor isn’t certain what may be causing the rash, they may take a swab or scraping of your skin (biopsy) and send it to a laboratory. A laboratory technician can then identify the bacteria, virus, or fungus that may be causing the rash.
See a doctor if your efforts to treat the rash at home aren’t improving its appearance. If the rash is bleeding or weeping (has yellow fluid coming from the rash area), call a doctor.
If you have signs that your rash may be infected, such as a fever, unexplained fatigue, or red and swollen skin, see a doctor.
A rash behind the ears may be a common occurrence, but it can have the potential to become infected. Always call a doctor if the rash appears to be getting worse and spreading to other areas of your skin.
Rubella (german measles) - NHS
Rubella (german measles) is a rare illness that causes a spotty rash. It usually gets better in about a week, but it can be serious if you get it when you're pregnant.
Check if you or your child have rubella
The main symptom of rubella is a spotty rash that starts on the face or behind the ears and spreads to the neck and body.
The rash takes 2 to 3 weeks to appear after getting rubella.
The rash looks red or pink on white skin.Credit:
PR. PH. FRANCESCHINI/CNRI/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/259748/view
It can be harder to see on brown or black skin, but might feel rough or bumpy.Credit:
DR P. MARAZZI/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/259492/view
You might also have lumps (swollen glands) in your neck or behind your ears.Credit:
DR P. MARAZZI/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/259236/view
Rubella can also cause:
- aching fingers, wrists or knees
- a high temperature
- coughs
- sneezing and a runny nose
- headaches
- a sore throat
- sore, red eyes
Information:
It's very unlikely to be rubella if you have had both doses of the MMR vaccine or had rubella before.
See other rashes in children and babies
Non-urgent advice: Call a GP if:
- you or your child have symptoms of rubella
Rubella can spread to others. It's best to call before you go in. The GP may suggest talking over the phone.
How to look after yourself or your child
Rubella usually gets better in about a week.
After getting advice from a GP, you or your child should:
- get plenty of rest
- drink lots of fluids, like water or squash
- take paracetamol or ibuprofen if you're uncomfortable – do not give aspirin to children under 16
How to avoid spreading rubella
Rubella spreads in coughs and sneezes.![]()
It’s infectious from 1 week before the symptoms start and for 5 days after the rash first appears.
It can be serious for some people, so you should try to avoid spreading it to others.
Do
-
stay off nursery, school, or work for 5 days after the rash appears
-
try to avoid close contact with anyone who is pregnant
-
wash your hands often with soap and warm water
-
use tissues when you cough or sneeze
-
throw used tissues in the bin
Don’t
-
do not share cutlery, cups, towels, clothes, or bedding
Rubella in pregnancy
Rubella is very rare in pregnancy.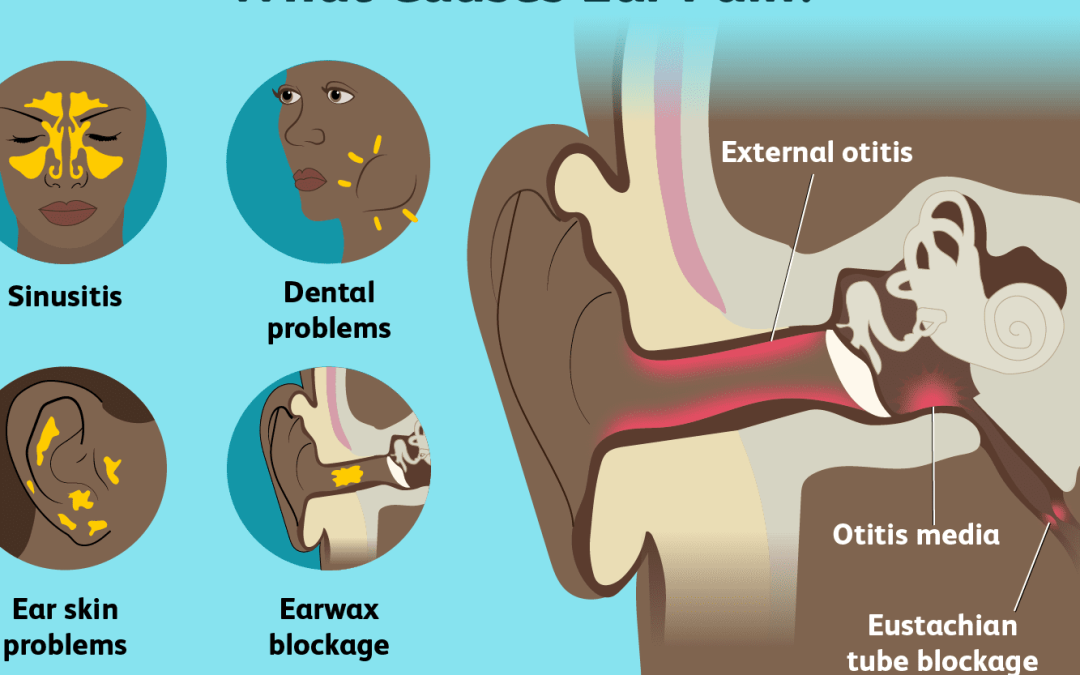 But if you get it when you're pregnant, rubella could harm your baby.
But if you get it when you're pregnant, rubella could harm your baby.
It can cause:
- loss of the baby (miscarriage)
- serious problems after the baby is born – such as problems with their sight, hearing, heart, or brain
The risk is highest if you get rubella early in pregnancy.
There's not thought to be a risk to your baby if you get rubella after week 20 of your pregnancy.
Urgent advice: Call your midwife, maternity unit, or GP immediately if:
You're pregnant and either:
- you have a new rash
- you’ve been in close contact with someone who has rubella
Get vaccinated against rubella
The MMR vaccine can prevent rubella. It also protects you from measles and mumps.
It also protects you from measles and mumps.
The MMR vaccine is offered to all children in the UK. 2 doses can give lifelong protection against measles, mumps, and rubella.
Ask at your GP surgery if you're not sure you or your child have had the vaccine. They can give it for free on the NHS.
Find out more about the MMR vaccine
Page last reviewed: 23 May 2022
Next review due: 23 May 2025
Ear inflammation in a child: how to prevent complications
Otitis media is one of the most common diseases in childhood. According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko. nine0003
nine0003
Why does otitis occur?
Depending on the location of the inflammatory process, otitis can be external, medial or internal. Otitis externa is caused by microbes and fungi, most often manifested by damage to the skin of the ear canal and boils in the auricle.
Acute otitis media is an acute inflammation of the mucous membrane of the middle ear cavity. It develops against the background of respiratory infections. Ear infection occurs through the auditory tube, when mucus from the nasopharynx enters the middle ear and viruses, bacteria, fungal flora freely penetrate from the nasopharynx through the mouth of the auditory tube into the tympanic cavity. nine0003
Due to anatomical features, the smaller the child, the shorter and wider the auditory tube connecting the ear cavity with the nasopharynx. Therefore, in an infant who spends most of his time lying down, and in a younger child who does not know how to clean his nose, mucus can flow at any time. In adolescent children, the auditory tube is a tortuous narrow tube, so the infection from the nasopharynx to the middle ear is less likely to pass.
In adolescent children, the auditory tube is a tortuous narrow tube, so the infection from the nasopharynx to the middle ear is less likely to pass.
Adenoid vegetations also contribute to the development of ear inflammation. This is an overgrowth of the nasopharyngeal tonsil, which is the main focus of bacterial infection in the nasopharynx. nine0003
How does the disease manifest itself?
The main symptom of otitis media is pain in the ear. Children under one year old, as a rule, refuse to eat, because sucking movements cause pain. Babies often touch their ears, rub them, and cry. You can suspect otitis media by pressing on the tragus of the child's auricle.
The key method for diagnosing otitis media is otoscopy - an examination by a doctor of the external auditory canal and eardrum using a special instrument.
How to treat otitis?
If the inflammatory process is at the initial stage, outpatient treatment is carried out. The therapy is selected by a pediatrician or an otorhinolaryngologist depending on the child's condition. Be sure to use vasoconstrictor drops in the nose.
The therapy is selected by a pediatrician or an otorhinolaryngologist depending on the child's condition. Be sure to use vasoconstrictor drops in the nose.
If medical assistance is not provided in a timely manner, the inflammatory process turns into acute catarrhal otitis media, and then into acute purulent otitis media, characterized by the appearance of purulent discharge from the ear. In some cases, with inadequate outflow of contents or its absence, the child in the hospital undergoes paracentesis - an incision in the eardrum. The intervention is performed under anesthesia. Then medical conservative treatment continues. nine0003
Which preventive measures are most effective?
There is an opinion among many parents that otitis media can be prevented by “covering the ears with cotton wool in the street” or “putting a few hats on the child”. Such recommendations will not insure against otitis media.
Due to the fact that ear infection occurs through the auditory tube that communicates with the nasopharynx, it is necessary to carefully care for the nasal cavity if the child has a runny nose. Otherwise, mucus flows from the nasopharynx into the middle ear, which leads to an inflammatory process in the ear. nine0003
Otherwise, mucus flows from the nasopharynx into the middle ear, which leads to an inflammatory process in the ear. nine0003
In case of excessive growth of the nasopharyngeal tonsil, its removal is recommended.
Why does the child get seizures?
Almost every wound in the area of the outer and inner surface of the lips, as well as the corner of the mouth, can be called a bite. The exception is traumatic injuries of the skin and mucous membranes, which are quite common in children. Such wounds, although they resemble seizures, have a completely different origin.
In short, seizures in a child can occur due to infection, allergic reactions, vitamin deficiency. In most cases, seizures in children are caused by streptococci. nine0003
Although according to pediatricians, the most common cause of seizures in a child is a deficiency of riboflavin, which is necessary for healthy skin and normal hair and nail growth. Also, seizures often occur due to a decrease in immunity and certain diseases. Many children suffering from seizures also have a history of chronic tonsillitis, caries, frequent colds and viral diseases. Among the reasons for a seizure in a child, there may also be staphylococci, streptococci, fungal diseases, and helminthic invasions. Timely treatment of such skin lesions helps to get rid of such unpleasant consequences. nine0003
Many children suffering from seizures also have a history of chronic tonsillitis, caries, frequent colds and viral diseases. Among the reasons for a seizure in a child, there may also be staphylococci, streptococci, fungal diseases, and helminthic invasions. Timely treatment of such skin lesions helps to get rid of such unpleasant consequences. nine0003
Several factors play a role in the etiology of true seizures in children. The most important of these are:
- Microbes;
- Allergic reactions;
- Various diseases and pathological abnormalities in the body;
Regardless of the root cause of seizures in children, all the same, its central link is the microbial factor. In this case, ordinary microorganisms that normally live on the surface of the skin become pathogens. But, when the child's body is healthy, such microbes do not cause any manifestations. As soon as there is a decrease in protective forces, they immediately begin to actively multiply, causing inflammation of the skin with the formation of wounds on the lips or in the corners of the mouth (jamming). nine0003
nine0003
With regard to specific types of pathogens that provoke the formation of seizures, the main role belongs to streptococcal and fungal infections. It is these two classes of microbes that live on the surface of the skin in children and are capable of causing an inflammatory lesion of the surface layers of the skin, which ends with the formation of a small ulcerative surface, which is called jamming.
Important! For the occurrence of seizures, a decrease in the immune function of the child's body must occur, against which conditionally pathogenic microflora (fungi and streptococci) is activated. Sometimes a similar condition occurs as a result of infection with these microbes from the environment. nine0072
The following factors can lead to this very decrease in immune surveillance:
- Colds;
- Fever;
- Allergic reactions;
- Food, toys and objects contaminated with pathogenic microbes that the child puts into the mouth;
- Anemia of various types and origins;
- Hypovitaminosis;
- Diseases of the immune system; nine0058 Diseases of the blood system;
- History of chemotherapy.

The most important thing is that seizures in children are not a frequent occurrence. But, if they occur, then, as a rule, they are of a long duration. Most of all, children in transitional age periods (6-8 years and 13-17 years) are prone to their appearance.
Symptoms of seizure in a child
Among the first symptoms of seizure in a child, small bubbles appear in the corners of the mouth, which eventually burst, and erosion forms in their place. The skin of the corners of the lips becomes moist and bleeds, microcracks appear. Erosion heals, then inflames again. Children may experience pain that prevents them from eating and talking. nine0003
Treatment of seizures in a child
Treatment of seizures should be complex. Before starting treatment, laboratory diagnostics is carried out to identify the pathogen and implement more effective treatment. They also do a general blood test, sowing feces for enterobiasis and dysbacteriosis, and examining the thyroid gland. In addition to antibacterial ointments and antiseptic lotions, multivitamins, immunostimulants are prescribed, and dysbacteriosis is treated. Carry out a correction of the diet: increase the consumption of dairy products, vegetables and fruits. nine0003
In addition to antibacterial ointments and antiseptic lotions, multivitamins, immunostimulants are prescribed, and dysbacteriosis is treated. Carry out a correction of the diet: increase the consumption of dairy products, vegetables and fruits. nine0003
If the child does not get seizures
Sometimes it happens that seizures do not respond to topical treatment for a long time. This is possible, even despite the use of different combinations of means, the action of which is aimed at different causes and mechanisms for the development of this problem. This situation clearly indicates a serious weakening of the body's immune and protective resources. Therefore, every mother must take this fact into account. After all, children with such problems are subject to a thorough examination:
- Pediatric examination;
- Dermatological consultation;
- General analysis of blood and urine;
- Biochemical blood tests;
- Inoculation of the microflora and its sensitivity to the action of specific drugs;
This will help determine the true cause of the child's seizures and their resistance to topical treatments.