Do meningitis rashes itchy
Meningitis Rash: Pictures, Symptoms, and More
Meningitis is a swelling of the membranes of the brain and spinal cord. It can be due to viral, fungal, or bacterial infection.
The most common cause of meningitis is a viral infection. But bacterial meningitis is one of the most dangerous forms of the disease.
Symptoms generally occur within 1 week after exposure and include:
- fever
- feeling ill
- headache
Not everyone develops every symptom. But they may develop a distinctive skin rash. In this article, we take a closer look at what that skin rash may look like, as well as other notable symptoms.
See a doctor if you think you or a loved one may have developed meningitis. This infection can be life threatening.
A meningitis skin rash is a distinct symptom of this serious illness. However, a skin rash doesn’t always appear in the early stages of meningitis, and when it does, it starts as small pinpricks on the skin before spreading into larger blotches.
Large, dark or purple rashes may indicate a related bloodstream infection called septicemia.
In these images, we show how an early meningitis skin rash begins and what it looks like as the illness progresses.
A meningitis rash may look similar to other skin rashes. However, what sets a meningitis-related rash apart from other skin symptoms is the presence of other symptoms, such as fever and stiff neck.
The glass test
One sign of meningococcal septicemia is that the rash doesn’t fade when you apply pressure to the skin. You can test this by pressing the side of a clear drinking glass against the skin.
If the rash looks like it fades, check periodically for changes. If you can still see the spots clearly through the glass, it may be a sign of septicemia, especially if you also have a fever.
The glass test is a good tool, but it’s not always accurate. Meningitis is a life threatening illness so it’s important to get medical attention if you have any symptoms.
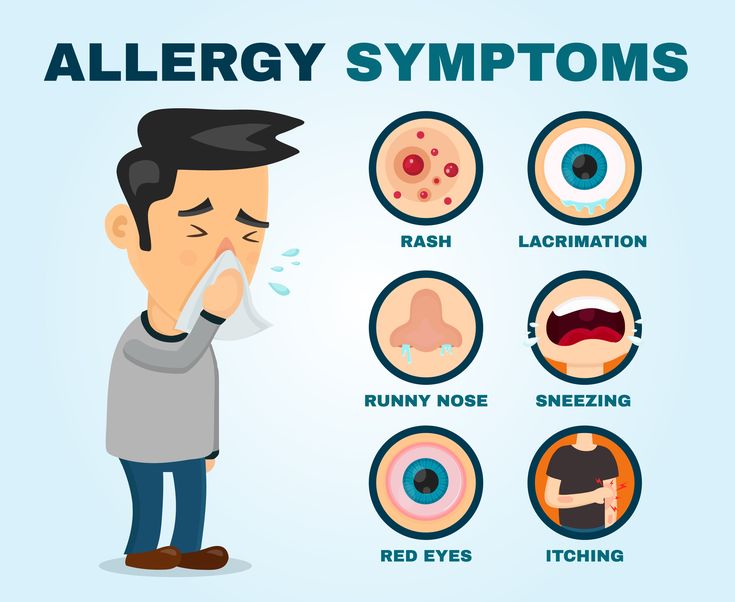
Other causes of skin rashes that appear like pinpricks or large, bruise-like blotches may include:
- Petechial rash. This leads to pinpoints in skin that look like tiny bruises. They’re typically less than 2 millimeters in size. Petechiae may develop on the skin or in mucous membranes from a variety of diseases, including meningitis, leukemia, and idiopathic thrombocytopenia (ITP).
- Vasculitis skin rashes. These rashes can cause petechiae or larger bruises. This rash may also cause itchy hives. Vasculitis is caused by an inflammation in the blood vessels and may also lead to other symptoms, such as fever, fatigue, and muscle pain.
- Purpura. These lesions may look like bruises but are larger than petechiae. Purpura rashes may be caused by a variety of conditions, such as vascular, platelet, and coagulation disorders.
- Hives (urticaria). These pale or dark and often itchy welts are common and may result from allergies, infections, and vascular diseases.
The symptoms of a meningitis infection in children are similar to those in adults. In addition to a possible rash, here’s what you might see during the early and later stages of this illness in children.
Early warning signs
Meningococcal bacteria reproduce in the bloodstream and release poisons (septicemia). As the infection progresses, blood vessels can become damaged.
This can cause a faint skin rash that looks like tiny pinpricks. The spots may be pink, red, or purple. In the early stages, these symptoms may be dismissed as a scratch or mild bruising. The skin may simply look blotchy and can appear anywhere on the body.
In addition to a meningitis rash, other symptoms of a meningococcal infection may include:
- fever
- a stiff neck
- nausea or vomiting
- confusion
- sensitivity to light (photophobia)
A worsening rash
As the infection spreads, the rash becomes more obvious. More bleeding under the skin may cause the spots to turn dark red or deep purple.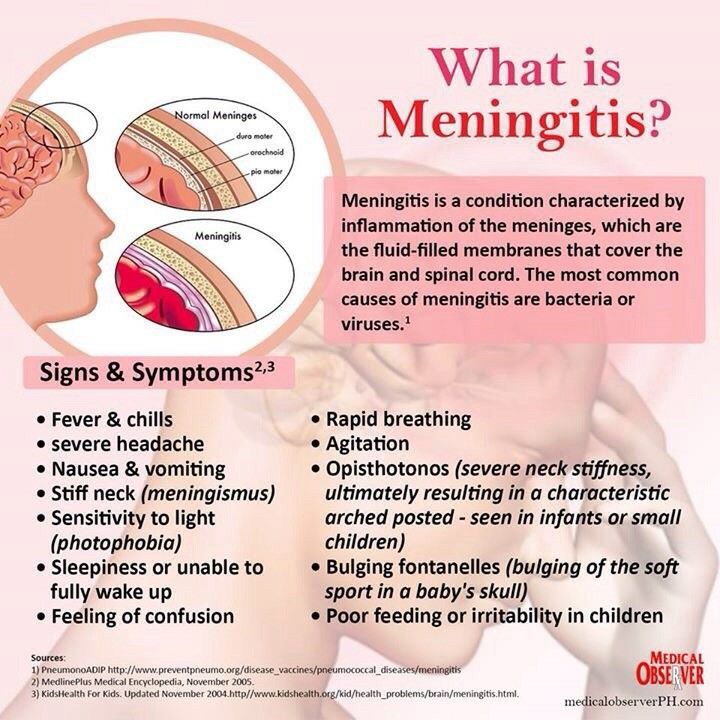 The rash may resemble large bruises.
The rash may resemble large bruises.
It’s harder to see the rash on darker skin. If you suspect meningitis, check lighter areas like the palms, eyelids, and inside the mouth.
Also, not everyone with meningitis develops a rash.
Tissue damage as the rash spreads
As the condition advances, the rash spreads and continues to darken. Blood vessel damage causes blood pressure and circulation to fall.
Because the limbs are at the far reaches of the circulatory system, a system-wide decrease in blood pressure leads to inadequate oxygen delivery, especially in the limbs. This can injure tissue and lead to permanent scarring.
Plastic surgery and skin grafting may be able to improve function after the illness passes. In severe cases, it becomes necessary to amputate fingers, toes, arms, or legs. Rehabilitative services may be helpful in those cases, but recovery could take years.
Anyone can get meningitis, but infants and children are at particular risk because they may not have fully developed immune systems, especially if they come in close contact with other children who have meningitis.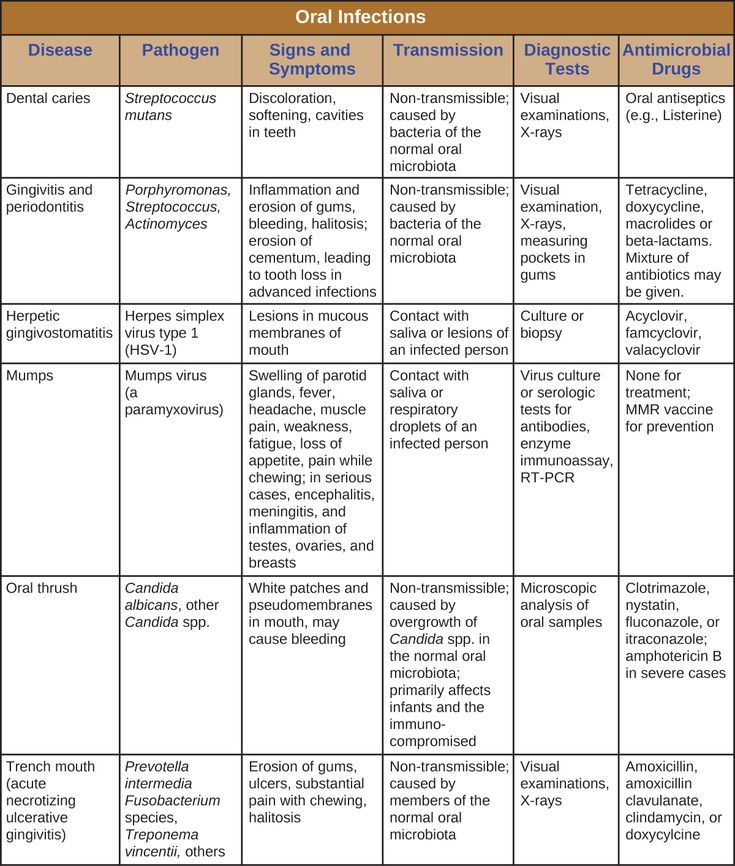
While the symptoms of meningitis are similar to those in adults, this infection may cause different symptoms in infants. Rather than causing the more classic symptoms, babies who have meningitis may display the following.
Abnormal arching in head, neck, and spine
Neck pain and stiffness are common symptoms of meningitis. It can sometimes cause the head, neck, and spine to become rigid and arch backward (opisthotonos). Infants may also exhibit widespread body stiffness and have jerky, or floppy movements.
Skin rash
Early in the course of infection, infants’ skin sometimes develops a yellow, blue, or pale tone. Like adults, they may also develop blotchy skin or a pinprick rash.
As the infection progresses, the rash grows and darkens. Lesions or blood blisters may form. The infection can spread quickly.
Seek medical attention if your infant has a fever with a rash.
Bulging fontanel
Another sign of meningitis concerns the soft spot on top of a baby’s head (fontanel).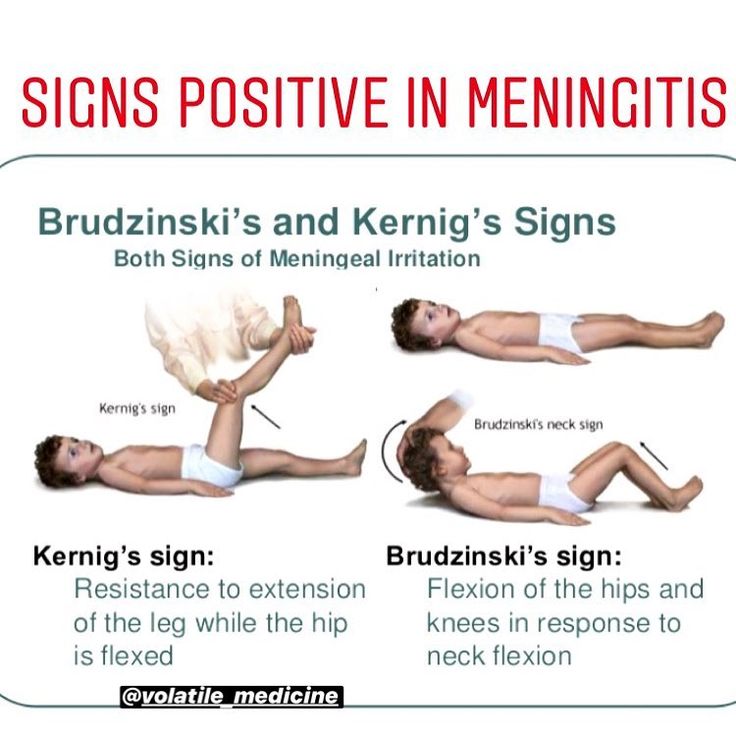 A soft spot that feels tight or forms a bulge could be a sign of swelling in the brain.
A soft spot that feels tight or forms a bulge could be a sign of swelling in the brain.
Always contact your doctor if you see bumps or bulges on your infant’s head. Meningitis can be a very serious illness even if your baby doesn’t develop septicemia.
Other symptoms in infants
In addition to the above symptoms, other signs of meningitis seen in infants may include:
- breathing difficulties
- rapid breathing
- extreme drowsiness
- diarrhea
- extreme shivering
- crying or irritability when being picked up due to pain
- cold hands and feet
- refusing to eat
- vomiting
If your baby exhibits any of these symptoms, it’s important to seek emergency medical help right away. A meningitis infection may spread quickly, and prompt treatment reduces the risk of complications.
Meningitis symptoms in adults are largely the same as those in children.
In addition to the most common symptoms of meningitis, you should look out for signs of septicemia. Seek emergency medical help if you also experience:
Seek emergency medical help if you also experience:
- rash that gets larger
- a fever accompanied by cold hands and feet
- severe muscle pain
- vomiting
- severe headache
- extreme drowsiness
- confusion and irritability
- severe stiff neck
- convulsions or seizures
Meningitis can happen at any age, but infants, children, and young adults are at a higher risk, as well as older adults. The disease is also more likely to spread in areas of close quarters, such as day care centers, nursing homes, and college dorms.
Additionally, having certain medical conditions like HIV may increase your risk of developing a meningitis infection, due to a weakened immune system. Chemotherapy treatments and immunosuppressants may also increase your risk.
Infants younger than 1 month old are also more likely to experience severe illness from an underdeveloped immune system.
Vaccines can help prevent some, but not all, types of meningitis. Early diagnosis and treatment can help you avoid complications and potential long-term effects.
Early diagnosis and treatment can help you avoid complications and potential long-term effects.
While early diagnosis and treatment can help you avoid complications and potential long-term effects, vaccination may also help prevent certain types of meningitis.
Currently, vaccines are available for bacterial meningococcal disease, the most serious type of meningitis. This is a two-dose series, typically administered around age 11 or 12, and then at the age of 16. These vaccines help prevent Neisseria meningitidis bacteria from causing meningitis.
There’s currently no vaccine to help prevent viral meningitis infections. However, the Centers for Disease Control and Prevention (CDC) outlines other types of routine vaccinations may offer some protection against viral meningitis, including those for chickenpox, influenza, and measles.
Besides vaccines, you can help prevent contracting the virus or bacteria that causes meningitis by washing your hands often, regularly disinfecting common surfaces, and avoiding others who may be sick.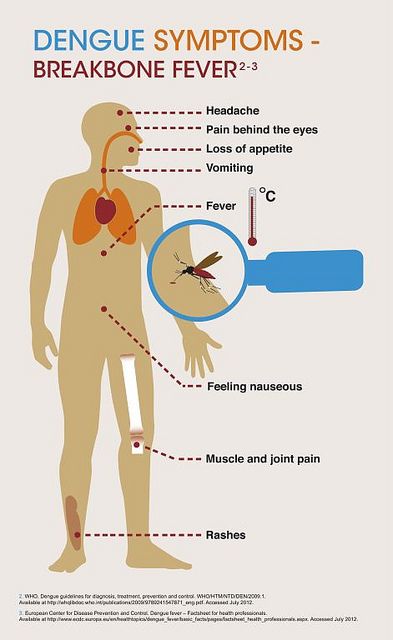
It’s also important to prevent the spread of this illness to others. If you or your child are sick, stay home until your doctor says it’s OK to go back to work or school.
Vaccine recommendations
Children ages 11 or 12 should receive a meningococcal vaccine (MenACWY) vaccine, followed by a booster dose at age 16.
Vaccination is also recommended for teens ages 13 to 18 who did not receive this vaccine when they were younger. Talk with your child’s pediatrician about their recommendations for your child. Children who are at increased risk due to certain medical conditions may need additional boosters.
If you’re unsure whether you received a meningococcal vaccine as a child, talk with your doctor. You may still be able to get vaccinated as an adult to protect yourself against this serious illness.
A meningitis rash is a serious sign that a meningitis infection has developed and possibly spread. This distinct rash may start as small pinpricks but rapidly develop into larger blotches over your entire body.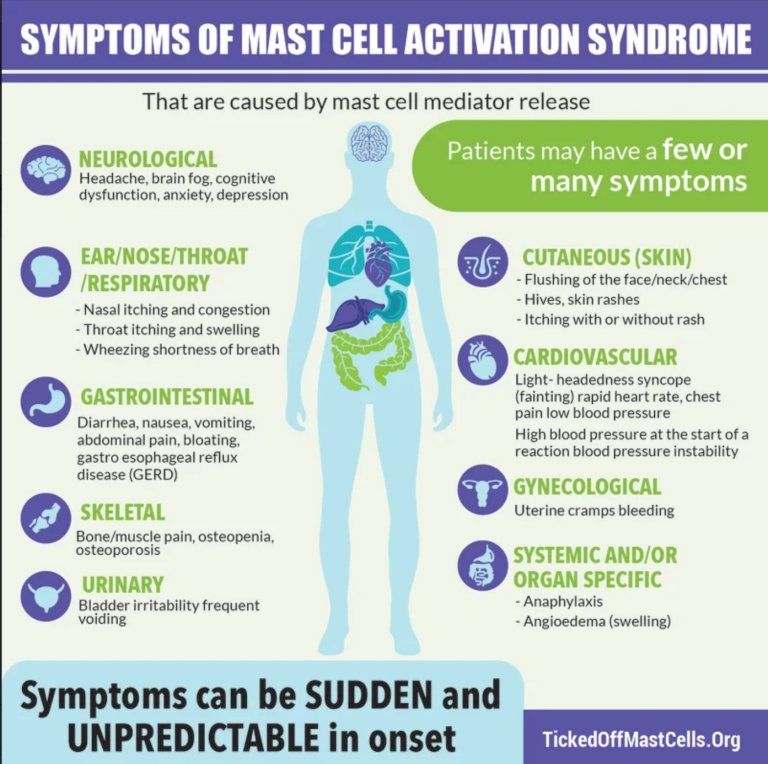 The appearance of the rash is similar across all age groups.
The appearance of the rash is similar across all age groups.
However, not everyone with meningitis experiences a rash. This is why it’s important to pay attention to other possible symptoms of meningitis, such as fever, headache, stiff neck, and photosensitivity.
Infants may also have bulging soft spots on their heads, along with unexplained fussiness and floppy movements.
If you suspect that you or your child has meningitis, seek emergency medical care right away.
Meningitis Rash: Pictures, Symptoms, and More
Meningitis is a swelling of the membranes of the brain and spinal cord. It can be due to viral, fungal, or bacterial infection.
The most common cause of meningitis is a viral infection. But bacterial meningitis is one of the most dangerous forms of the disease.
Symptoms generally occur within 1 week after exposure and include:
- fever
- feeling ill
- headache
Not everyone develops every symptom. But they may develop a distinctive skin rash.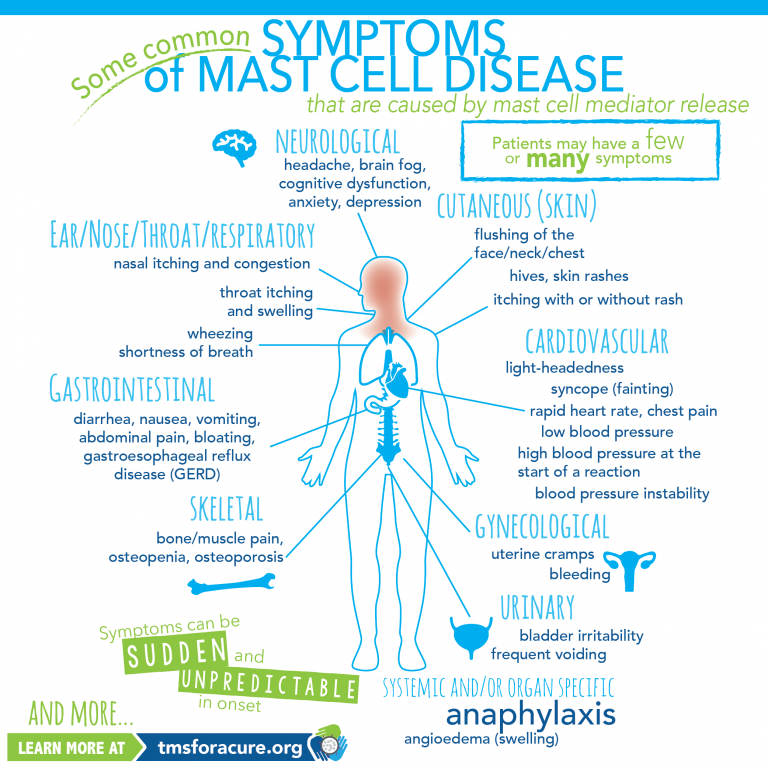 In this article, we take a closer look at what that skin rash may look like, as well as other notable symptoms.
In this article, we take a closer look at what that skin rash may look like, as well as other notable symptoms.
See a doctor if you think you or a loved one may have developed meningitis. This infection can be life threatening.
A meningitis skin rash is a distinct symptom of this serious illness. However, a skin rash doesn’t always appear in the early stages of meningitis, and when it does, it starts as small pinpricks on the skin before spreading into larger blotches.
Large, dark or purple rashes may indicate a related bloodstream infection called septicemia.
In these images, we show how an early meningitis skin rash begins and what it looks like as the illness progresses.
A meningitis rash may look similar to other skin rashes. However, what sets a meningitis-related rash apart from other skin symptoms is the presence of other symptoms, such as fever and stiff neck.
The glass test
One sign of meningococcal septicemia is that the rash doesn’t fade when you apply pressure to the skin.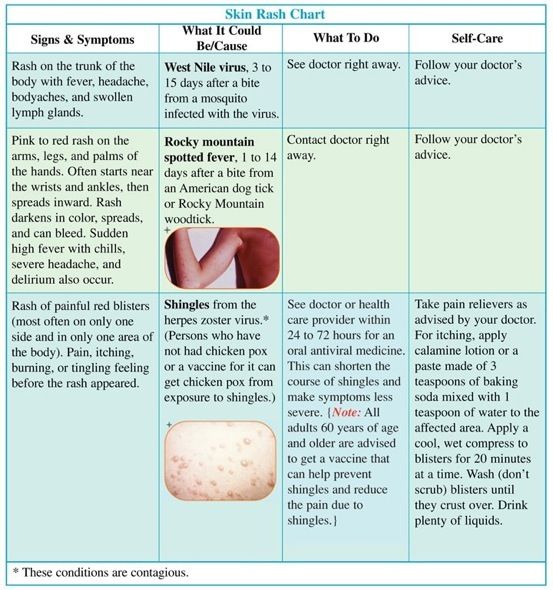 You can test this by pressing the side of a clear drinking glass against the skin.
You can test this by pressing the side of a clear drinking glass against the skin.
If the rash looks like it fades, check periodically for changes. If you can still see the spots clearly through the glass, it may be a sign of septicemia, especially if you also have a fever.
The glass test is a good tool, but it’s not always accurate. Meningitis is a life threatening illness so it’s important to get medical attention if you have any symptoms.
Other causes of skin rashes that appear like pinpricks or large, bruise-like blotches may include:
- Petechial rash. This leads to pinpoints in skin that look like tiny bruises. They’re typically less than 2 millimeters in size. Petechiae may develop on the skin or in mucous membranes from a variety of diseases, including meningitis, leukemia, and idiopathic thrombocytopenia (ITP).
- Vasculitis skin rashes. These rashes can cause petechiae or larger bruises. This rash may also cause itchy hives.
 Vasculitis is caused by an inflammation in the blood vessels and may also lead to other symptoms, such as fever, fatigue, and muscle pain.
Vasculitis is caused by an inflammation in the blood vessels and may also lead to other symptoms, such as fever, fatigue, and muscle pain. - Purpura. These lesions may look like bruises but are larger than petechiae. Purpura rashes may be caused by a variety of conditions, such as vascular, platelet, and coagulation disorders.
- Hives (urticaria). These pale or dark and often itchy welts are common and may result from allergies, infections, and vascular diseases.
The symptoms of a meningitis infection in children are similar to those in adults. In addition to a possible rash, here’s what you might see during the early and later stages of this illness in children.
Early warning signs
Meningococcal bacteria reproduce in the bloodstream and release poisons (septicemia). As the infection progresses, blood vessels can become damaged.
This can cause a faint skin rash that looks like tiny pinpricks. The spots may be pink, red, or purple.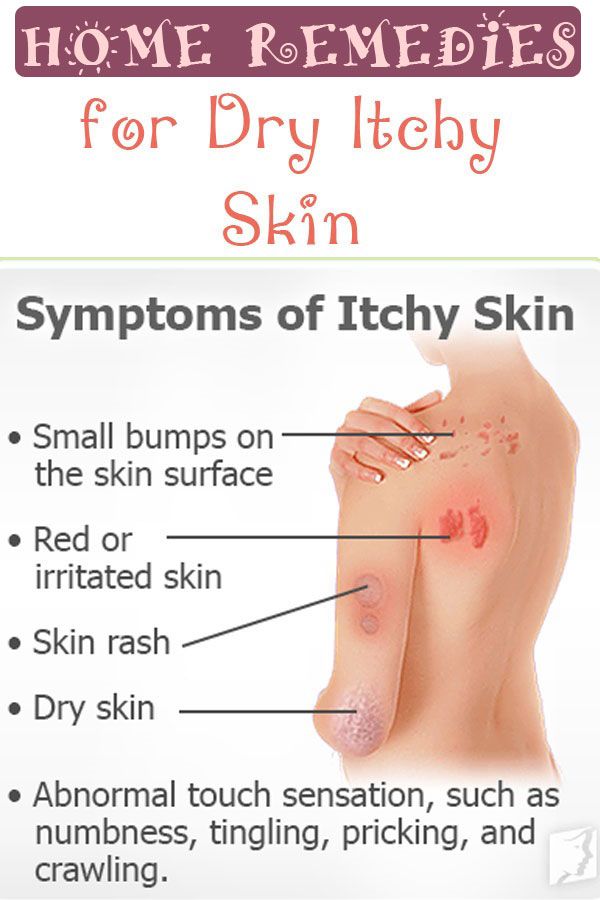 In the early stages, these symptoms may be dismissed as a scratch or mild bruising. The skin may simply look blotchy and can appear anywhere on the body.
In the early stages, these symptoms may be dismissed as a scratch or mild bruising. The skin may simply look blotchy and can appear anywhere on the body.
In addition to a meningitis rash, other symptoms of a meningococcal infection may include:
- fever
- a stiff neck
- nausea or vomiting
- confusion
- sensitivity to light (photophobia)
A worsening rash
As the infection spreads, the rash becomes more obvious. More bleeding under the skin may cause the spots to turn dark red or deep purple. The rash may resemble large bruises.
It’s harder to see the rash on darker skin. If you suspect meningitis, check lighter areas like the palms, eyelids, and inside the mouth.
Also, not everyone with meningitis develops a rash.
Tissue damage as the rash spreads
As the condition advances, the rash spreads and continues to darken. Blood vessel damage causes blood pressure and circulation to fall.
Because the limbs are at the far reaches of the circulatory system, a system-wide decrease in blood pressure leads to inadequate oxygen delivery, especially in the limbs.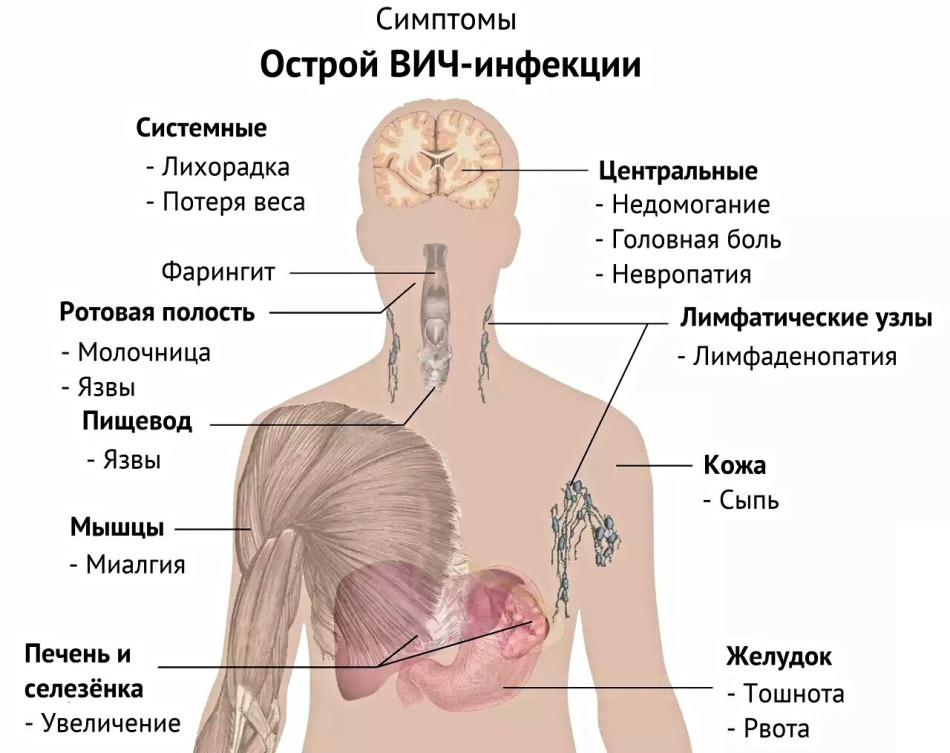 This can injure tissue and lead to permanent scarring.
This can injure tissue and lead to permanent scarring.
Plastic surgery and skin grafting may be able to improve function after the illness passes. In severe cases, it becomes necessary to amputate fingers, toes, arms, or legs. Rehabilitative services may be helpful in those cases, but recovery could take years.
Anyone can get meningitis, but infants and children are at particular risk because they may not have fully developed immune systems, especially if they come in close contact with other children who have meningitis.
While the symptoms of meningitis are similar to those in adults, this infection may cause different symptoms in infants. Rather than causing the more classic symptoms, babies who have meningitis may display the following.
Abnormal arching in head, neck, and spine
Neck pain and stiffness are common symptoms of meningitis. It can sometimes cause the head, neck, and spine to become rigid and arch backward (opisthotonos). Infants may also exhibit widespread body stiffness and have jerky, or floppy movements.
Skin rash
Early in the course of infection, infants’ skin sometimes develops a yellow, blue, or pale tone. Like adults, they may also develop blotchy skin or a pinprick rash.
As the infection progresses, the rash grows and darkens. Lesions or blood blisters may form. The infection can spread quickly.
Seek medical attention if your infant has a fever with a rash.
Bulging fontanel
Another sign of meningitis concerns the soft spot on top of a baby’s head (fontanel). A soft spot that feels tight or forms a bulge could be a sign of swelling in the brain.
Always contact your doctor if you see bumps or bulges on your infant’s head. Meningitis can be a very serious illness even if your baby doesn’t develop septicemia.
Other symptoms in infants
In addition to the above symptoms, other signs of meningitis seen in infants may include:
- breathing difficulties
- rapid breathing
- extreme drowsiness
- diarrhea
- extreme shivering
- crying or irritability when being picked up due to pain
- cold hands and feet
- refusing to eat
- vomiting
If your baby exhibits any of these symptoms, it’s important to seek emergency medical help right away. A meningitis infection may spread quickly, and prompt treatment reduces the risk of complications.
A meningitis infection may spread quickly, and prompt treatment reduces the risk of complications.
Meningitis symptoms in adults are largely the same as those in children.
In addition to the most common symptoms of meningitis, you should look out for signs of septicemia. Seek emergency medical help if you also experience:
- rash that gets larger
- a fever accompanied by cold hands and feet
- severe muscle pain
- vomiting
- severe headache
- extreme drowsiness
- confusion and irritability
- severe stiff neck
- convulsions or seizures
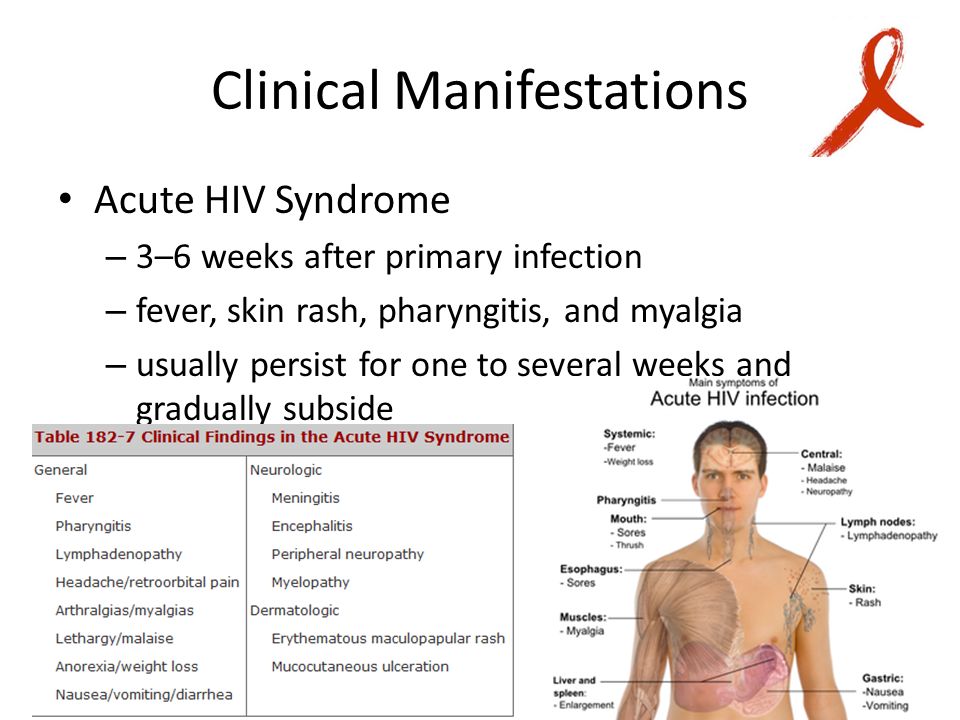
Meningitis can happen at any age, but infants, children, and young adults are at a higher risk, as well as older adults. The disease is also more likely to spread in areas of close quarters, such as day care centers, nursing homes, and college dorms.
Additionally, having certain medical conditions like HIV may increase your risk of developing a meningitis infection, due to a weakened immune system.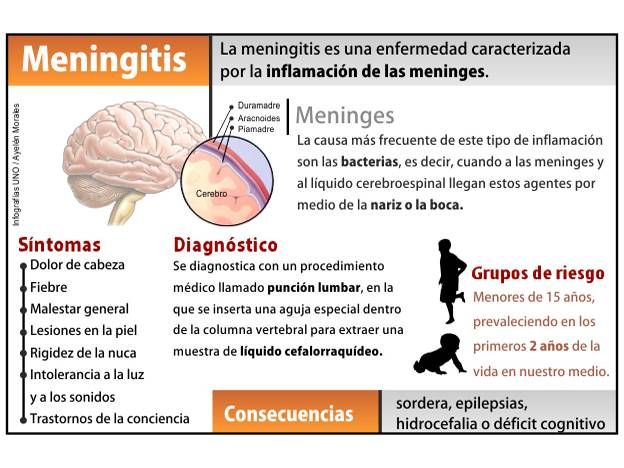 Chemotherapy treatments and immunosuppressants may also increase your risk.
Chemotherapy treatments and immunosuppressants may also increase your risk.
Infants younger than 1 month old are also more likely to experience severe illness from an underdeveloped immune system.
Vaccines can help prevent some, but not all, types of meningitis. Early diagnosis and treatment can help you avoid complications and potential long-term effects.
While early diagnosis and treatment can help you avoid complications and potential long-term effects, vaccination may also help prevent certain types of meningitis.
Currently, vaccines are available for bacterial meningococcal disease, the most serious type of meningitis. This is a two-dose series, typically administered around age 11 or 12, and then at the age of 16. These vaccines help prevent Neisseria meningitidis bacteria from causing meningitis.
There’s currently no vaccine to help prevent viral meningitis infections. However, the Centers for Disease Control and Prevention (CDC) outlines other types of routine vaccinations may offer some protection against viral meningitis, including those for chickenpox, influenza, and measles.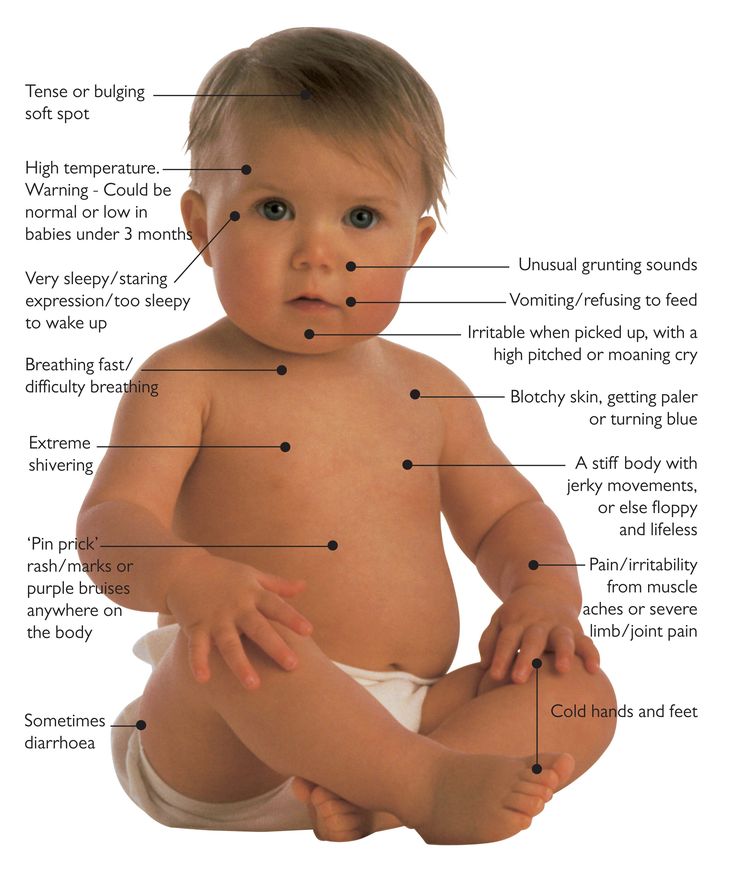
Besides vaccines, you can help prevent contracting the virus or bacteria that causes meningitis by washing your hands often, regularly disinfecting common surfaces, and avoiding others who may be sick.
It’s also important to prevent the spread of this illness to others. If you or your child are sick, stay home until your doctor says it’s OK to go back to work or school.
Vaccine recommendations
Children ages 11 or 12 should receive a meningococcal vaccine (MenACWY) vaccine, followed by a booster dose at age 16.
Vaccination is also recommended for teens ages 13 to 18 who did not receive this vaccine when they were younger. Talk with your child’s pediatrician about their recommendations for your child. Children who are at increased risk due to certain medical conditions may need additional boosters.
If you’re unsure whether you received a meningococcal vaccine as a child, talk with your doctor. You may still be able to get vaccinated as an adult to protect yourself against this serious illness.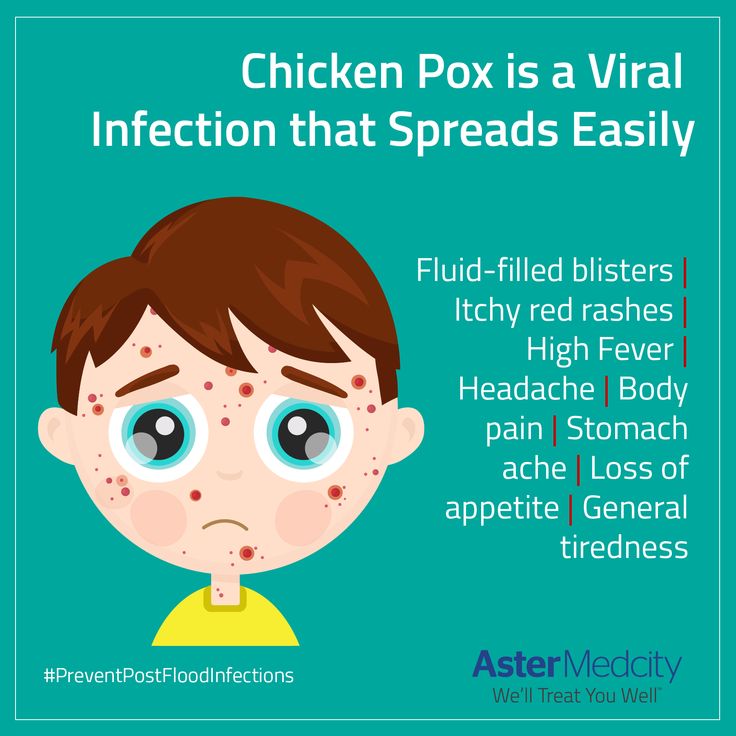
A meningitis rash is a serious sign that a meningitis infection has developed and possibly spread. This distinct rash may start as small pinpricks but rapidly develop into larger blotches over your entire body. The appearance of the rash is similar across all age groups.
However, not everyone with meningitis experiences a rash. This is why it’s important to pay attention to other possible symptoms of meningitis, such as fever, headache, stiff neck, and photosensitivity.
Infants may also have bulging soft spots on their heads, along with unexplained fussiness and floppy movements.
If you suspect that you or your child has meningitis, seek emergency medical care right away.
Meningococcal infection and its prevention
Meningococcal infection occupies an important place in infectious pathology and continues to be relevant for the Republic of Belarus
Meningococcal infection affects only people. The causative agent - meningococcus - is transmitted by airborne droplets, as well as, for example, with the flu. This microbe lives in the nasal cavity and can be transmitted from person to person by sneezing, coughing and even talking. This is a very serious disease that can develop among full health in a matter of hours and minutes. Children are more often ill, and generalized forms of the disease in 80% of cases occur in children under 2 years of age. Sometimes it is not possible to save a sick child.
This microbe lives in the nasal cavity and can be transmitted from person to person by sneezing, coughing and even talking. This is a very serious disease that can develop among full health in a matter of hours and minutes. Children are more often ill, and generalized forms of the disease in 80% of cases occur in children under 2 years of age. Sometimes it is not possible to save a sick child.
The incubation period (the period from the moment meningococcus enters the body until the first signs of the disease appear) can last from several hours to 10 days. It all depends on the age and immune status of the patient.
The microbe itself is relatively unstable in the external environment. Outside of a person, he dies within 30 minutes. Fresh air, direct sunlight, ultraviolet radiation and disinfectants are especially detrimental to meningococcus.
This disease is characterized by a very acute onset, one might say in the midst of full health or after a slight runny nose. The temperature rises sharply to very high numbers, the child complains of a severe headache, at first a single, and then indomitable vomiting appears. Young children, who cannot yet complain, may have regurgitation, lethargy, refusal of the breast.
The temperature rises sharply to very high numbers, the child complains of a severe headache, at first a single, and then indomitable vomiting appears. Young children, who cannot yet complain, may have regurgitation, lethargy, refusal of the breast.
The main symptom of the fulminant form and the appearance of an infectious agent in the blood (meningococcemia) is a rash on the child's skin. Rash with meningitis in children is one of the most characteristic symptoms. Initially, it may be morbilliform in nature - in the form of small red spots and papules. After some time, such a rash disappears and a hemorrhagic rash characteristic of meningococcal infection appears. Pinpoint hemorrhages appear first in the feet and legs of the child, and then spread higher to the trunk and other parts of the body. On pale skin, they resemble a picture of a starry sky.
- Note that meningococcal rash does not go away with pressure. If a rash appears on the face, eyelids, oral mucosa, auricles, or at the very beginning of the disease, this is an unfavorable factor and is typical for severe forms of the disease.
 The rash will increase. And it is precisely in the presence of it that it is necessary to re-call the doctor, since the primary diagnosis before the rash can be set as an acute respiratory disease.
The rash will increase. And it is precisely in the presence of it that it is necessary to re-call the doctor, since the primary diagnosis before the rash can be set as an acute respiratory disease.
This form of meningitis is dangerous because toxic-septic shock can develop due to hemorrhage in vital organs and, above all, in the adrenal glands. This shock causes death in 5-10 percent of patients. Therefore, the sooner parents seek medical help, and the sooner an appropriate diagnosis is made, the greater the chance of saving the patient. But in any case, hospitalization will be required and parents do not need to refuse it.
- What are the preventive measures for meningococcal disease?
You just need to carefully monitor the child's condition and, if warning signs appear, immediately seek medical help.
Oddly enough, the best prevention of meningitis is to strengthen the immune system - walks in the fresh air, rational nutrition and hardening.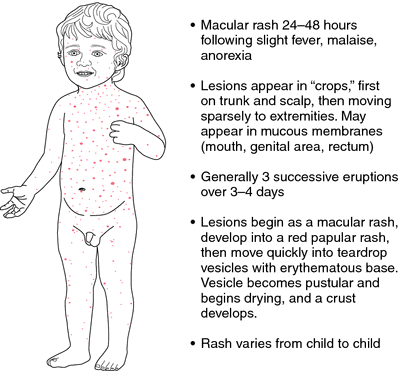 Equally important is personal hygiene. Thorough hand washing is very important to avoid infection. Teach your children to wash their hands frequently, especially before eating, after being in a public place, and after they have touched animals.
Equally important is personal hygiene. Thorough hand washing is very important to avoid infection. Teach your children to wash their hands frequently, especially before eating, after being in a public place, and after they have touched animals.
And most importantly, do not try to treat the baby yourself. In many ways, the results of the treatment of meningitis depend on the time that has passed since the onset of the first symptoms and the start of therapy. Only a specialist is able to correctly assess the situation and select treatment tactics.
Prevention of meningitis in children is primarily the prevention of airborne infection of the child. For children aged 1 to 3 years, the main danger is adults, and first of all, relatives. The most dangerous age for meningitis is up to 5 years, and in many respects the health of the child depends on his parents. If one of the older family members has a cough, runny nose, nasal congestion, think about the child - do not approach him, or put on a four-layer gauze bandage, covering both the nose and mouth.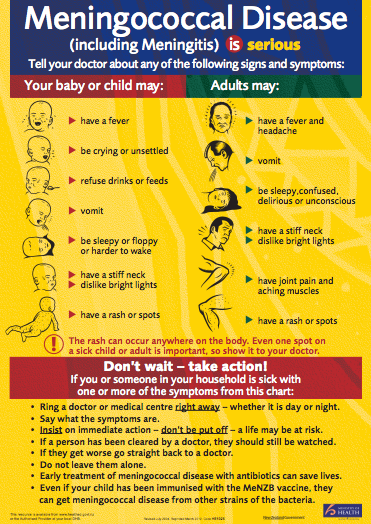
- Meningococcus is one of the weakest microbes, it dies very quickly outside the human body, especially from the action of ultraviolet rays of sunlight. Regular ventilation of the premises and sufficient sunlight can quickly get rid of these microbes in the air. Thus, you need to take care of good lighting in your child's room. The nursery should always be ventilated and washed clean.
Among other preventive measures, it is recommended to have fewer contacts during the period of the seasonal rise in the incidence of influenza and ARVI, to attend social events less frequently. All festive events (christenings) associated with the birth of a child must be carried out outside the apartment where he is.
And most importantly, don't try to treat yourself. The results of treatment of meningococcal infection largely depend on the time interval between the onset of the first symptoms and the start of therapy. Only a specialist can correctly assess the situation and choose the tactics of treatment.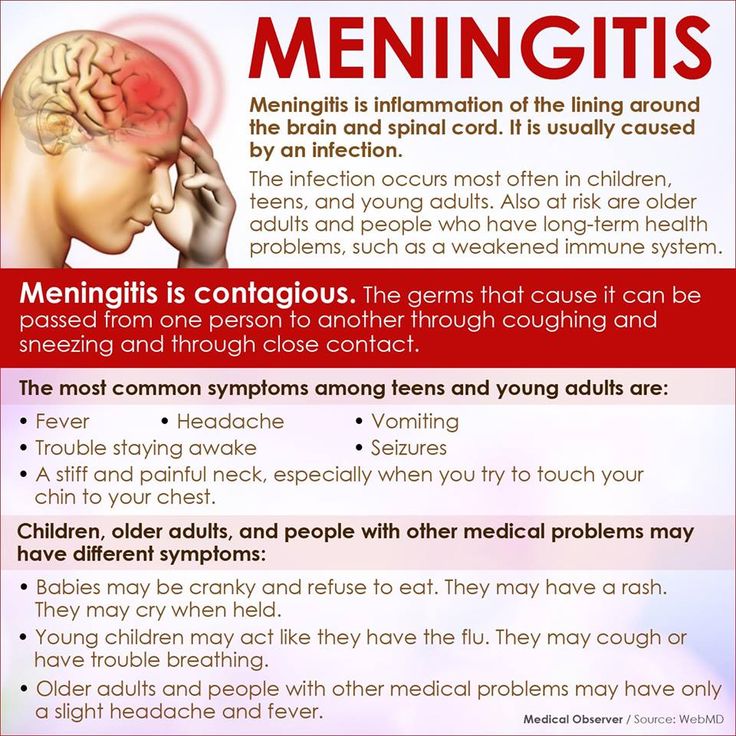
If hospitalization is suggested by a health worker, do not refuse it, your child's life may depend on it.
A complete and balanced diet enriched with vitamins and microelements, playing sports, hardening the body also contribute to the body's resistance to infection. 9Nedved N.V.
what happens, a photo of how it looks in a child and features of the hemorrhagic type
Home → Diseases → Meningitis
Published: 11/27/17
Updated: 11/30/20 Author: Alexandra Ageeva
A rash is an unpleasant symptom that leaves a person with a lot of inconvenience. It can occur for various reasons, one of which is meningitis.
At the same time, diseases for rashes are characterized by certain features, knowing which, you can seek medical help in time and prevent complications. Read more about it in this article.
All information on the site is presented for informational purposes only and does not replace the need for examination by a doctor.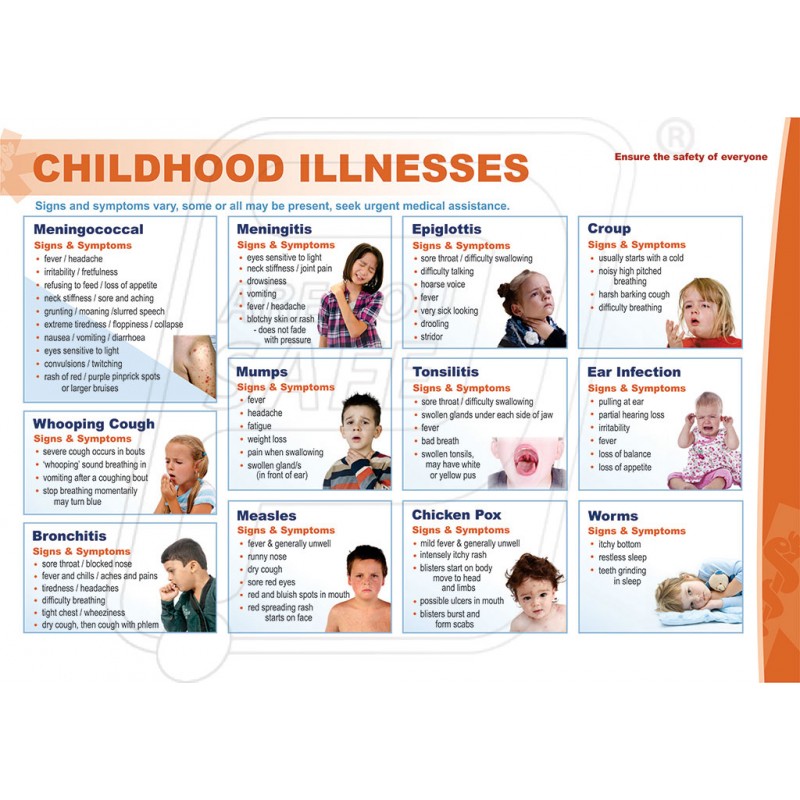 We kindly ask you to contact a medical institution if you have any health problems.
We kindly ask you to contact a medical institution if you have any health problems.
Hide content
- What is this disease?
- Why does this symptom appear and where is it localized?
- What does it look like?
Photo
- Do you itch?
- How to distinguish a dangerous sign from similar ones?
- First aid
- Treatment
- Are hemorrhagic rashes dangerous in this disease?
- Bibliography
What is this disease?
WARNING : Meningitis is a dangerous infectious disease that can be spread through the air or through household items. Most often, the disease is diagnosed in preschool children.
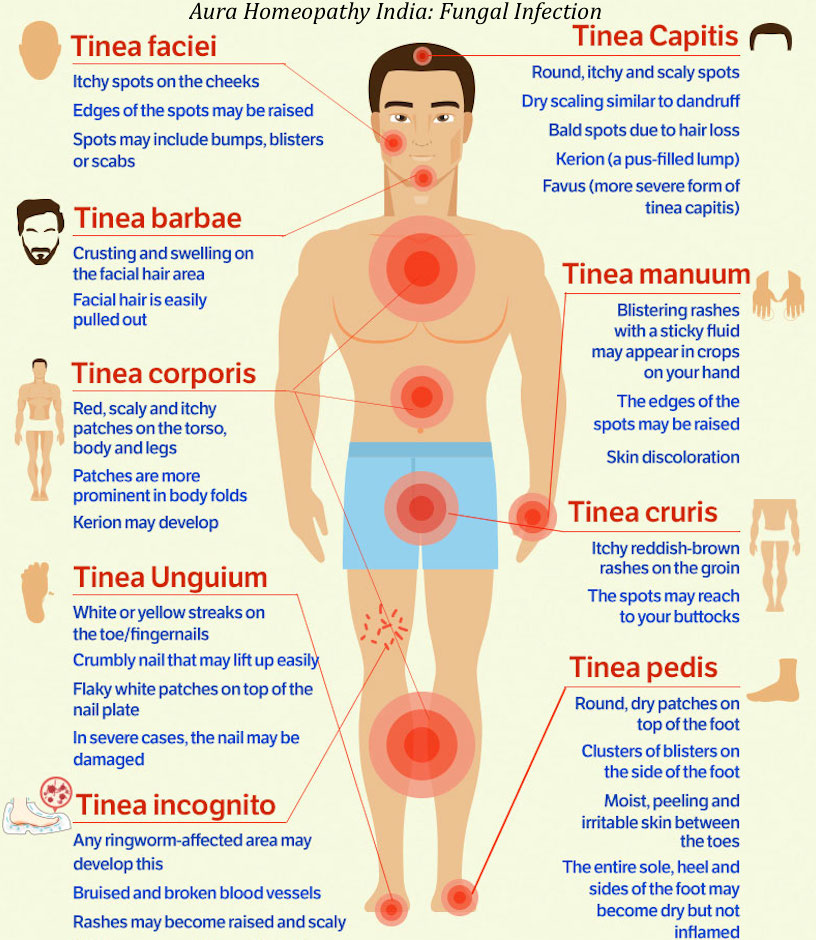
Quite often, the pathological process begins with symptoms of nasopharyngitis, and then vomiting, rash, and headache follow. The rash of meningitis on the first day of illness is very similar to the rash of measles.
Watch a video about the symptoms of meningitis:
Why does this symptom appear and where is it localized?
The causative agent of meningitis produces a toxic substance . It is a poison to the vascular system. The formation of a non-inflammatory rash is associated with the effect of toxins on the blood vessels.
Their walls become extremely permeable. Rashes often form with generalized forms of meningitis immediately after infection.
With meningitis, the rash always forms on the lower and upper limbs, as well as on the sides of the patient.
What does it look like?
In bacterial meningitis, the rash is most often located on the sides and lower extremities of the child. The shape of the rash is irregular, the color can be from red to dark brown, almost purple.
When touched, does not rise above the skin.
Especially dangerous is the appearance of rashes on the head. In order to make sure that the rash is caused by meningitis, you should press on it and hold it. If she does not turn pale, urgent medical attention should be sought.
- As the disease progresses, sepsis may develop.
- The shape is more like "asterisks". With viral meningitis, the rash appears in rare cases, it is not as bright as with a bacterial infection, it can be located on any part of the body, and even on the mucous membranes. It does not have a specific form.
The meningitis rash does not itch, itch, or cause particular discomfort to the child, and cannot be contracted by contact. However, it is important to remember that it is not the rashes themselves that are contagious, but the infection that causes them . Therefore, precautions should be taken when examining a child.
Meningitis is highly contagious and many forms are transmitted by both airborne droplets and contact.
Expert's opinion
Zemlyanukhina Tatyana Vyacheslavovna
Paramedic for emergency and emergency care at Clinical Emergency Hospital #7, Volgograd.
Ask an expert
The disease begins with a small herpetic rash quickly acquiring a large stellate hemorrhagic form, which most often manifests itself together with hemorrhages in the mucous membrane of the eyes as a result of vascular damage. This symptom may last from two hours to two weeks.
Photo
You can see what the meningitis rash looks like in these photos:
Do they itch?
The peculiarity of this rash is that it does not itch or hurt . It is these symptoms that should alert the patient, because with allergies, for example, rashes itch and hurt very much. With meningitis at the initial stage, the rash is small in size.
IMPORTANT : These are small red spots that look like fresh bruises.
But over time, they increase in size, merge and spread over a large area of the body.
How to distinguish a dangerous sign from similar ones?
It is important to remember that not only meningitis is manifested by a skin rash . You need to know how to distinguish a dangerous hemorrhagic rash with meningitis, from rashes with allergies, chickenpox, rubella and others. Common childhood diseases that may cause rashes:
- Chicken pox.
- Measles.
- Mononucleosis.
- Various allergies.
- Rubella.
- Scarlet fever.
- Pyoderma.
- The meningeal rash differs from the chickenpox rash in that it is blistering in smallpox and covers the entire body of the child. It is localized without any pattern, and at first it is small red spots that form papules, and then vesicles containing a clear liquid. After the vesicles burst, crusts form.
In meningitis, the rash is localized in certain parts of the body, has a dark red color, does not have bubbles.
With smallpox, the rash is itchy and itchy, but not with meningitis.
- A distinctive feature of the measles rash is a rapid transition from red or purple to dark, almost black. Forms papules, which is not typical for meningeal. With measles, the rash is on the face. With meningitis, a rash on the face is very rare.
- In mononucleosis rash there is no itching and irritation, as in meningeal, but mononucleosis rashes turn pale when pressed. The spots are reddish in color and clusters can be located on any part of the body.
- An allergic rash, as a rule, does not cause a general infectious syndrome in a patient. Infectious rash, on the contrary, is accompanied by fever, weakness, headache. The main difference between an allergic rash and a meningitis rash is itching.
- In children, rubella spots do not merge into a single whole, and the rash appears some time after the onset of the disease. With meningitis, a rash is one of the first symptoms.
Rubella is accompanied by a runny nose, sore throat, and other symptoms that are not characteristic of meningitis.
- Scarlet fever is caused by streptococci, they can also be the cause of meningitis, but in scarlet fever the rash is accompanied by slight itching, and is often localized in the groin or armpits. The rash is punctate and can cover any skin folds, face, thighs. The meningitis rash does not itch, and looks more like asterisks.
- With pyoderma, the formations spread throughout the body, in the form of vesicles with pus, then they dry up and turn yellow.
First Aid
Since a hemorrhagic rash occurs when blood capillaries break, the first thing to do when it is detected is to limit the child's mobility, and observe bed rest until the doctor arrives.
Important! If a rash and meningitis-like symptoms appear, immediately call an ambulance and take the patient to a hospital.
Only a doctor, after a general examination and examination of the tests, can make a diagnosis and prescribe treatment.
Meningitis is not only a severe disease for the patient himself, but also dangerous for others .
Treatment
If rash manifestations lead to the development of a hyperthermic state, severe pain, then urgent hospitalization and medical assistance are required. If no adequate action is taken in the near future, the consequences can be very sad.
In the treatment of meningeal infection, antibiotic therapy is prescribed. Using antibiotics, it is possible to stop the pathogenic microflora that led to the development of the disease. The patient after hospitalization is placed in the inpatient department of the hospital. Further, his treatment is reduced to the following :
- The doctor prescribes bed rest with a sparing diet to the patient.
- Antibacterial preparations. Prescribe drugs with low, medium and high permeability. The most effective include: Amoxicillin, Cefuroxime, Ketoconazole, Clindamycin. The dosage is determined individually.
But the duration of therapy should not be longer than 7-10 days, as addiction occurs.
- In addition to antibiotic therapy, antiviral drugs are prescribed.
- The combination of desensitizing therapy with anti-inflammatory therapy will alleviate the patient's condition, stop unpleasant symptoms.
The therapeutic course for any age category will be at least 10 days. If there are complicated forms, then the duration of treatment may increase. As soon as the patient is discharged from the hospital, he should prepare for long-term home treatment. For some patients with meningococcal pathology, recovery takes 1 year. Read more about emergency care and nursing care for meningitis in this article.
Meningitis vaccination available . It can prevent the development of this dangerous disease. Vaccination is required in places where a regular outbreak of the disease occurs.
TIP : When a skin rash is accompanied by high fever and severe headache, go to the hospital as soon as possible.
Such a state means that the account of life goes to the clock.
Are hemorrhagic rashes dangerous in this disease?
Complicated variants of the course of the pathological process are often diagnosed. Inflammation that occurs in the meninges almost always goes away. But if the treatment was started at the wrong time or the disease proceeds in a severe form, then this is fraught with the following complications :
- mental retardation of the child;
- mental impairment;
- development of a paretic, paralyzed condition;
- blindness or strabismus;
- hearing loss;
- the patient becomes asthenic, lethargic, his memory decreases and attention is absent.
If you suddenly find such a rash against the background of a high temperature, especially if new elements of the rash appear one by one in a matter of minutes, URGENTLY call an ambulance. Infectious disease specialist Nekrasova E.
S. 21st city polyclinic, Minsk.
Meningitis is a rather dangerous disease. When an infectious process damages the brain, the work of many systems throughout the human body is disrupted. If treatment is not started in time, the consequences can be extremely unfavorable. The most dangerous complication remains the death of the patient.
Bibliography
- Pokrovsky V.I., Favorova L.A., Kostyukova N.N. Meningococcal infection.-M.: Medicine, 1976: 272p.
- Vengerov Yu.Ya., Nagibina M.V., Molotilova T.P., Chentsov V.B. et al. // Clinical and pathogenetic significance of lactic acidosis in purulent meningitis "(I National Conference with international participation on neuroinfection - Moscow- 2007: 13 - 15.
- Koroleva I.S., Beloshitsky. G.V., Spirikina L.V., et al. // Actual problems of meningococcal infection and purulent bacterial meningitis. – Epidemiology and vaccination. – 2009; 1:5-8.
- Harisson L.H., Trotter C.L., Ramsay M.