Do lesbians get pregnant
Lesbian pregnancy options: Choices and considerations
Lesbians who want to get pregnant have a number of options depending on their budget, health, fertility preferences, and personal values. The process often begins with a consultation with a doctor or fertility specialist since this can help with narrowing down options.
A note about sex and gender
Sex and gender exist on spectrums. This article will use the terms “male,” “female,” or both to refer to sex assigned at birth. Click here to learn more.
In this article, we will provide a list of lesbian pregnancy options and note some factors people may want to consider.
Lesbians can use all of the same paths to pregnancy and parenthood that different-sex couples can. But those who wish to avoid sex with a person with a penis may need to use assisted reproductive technologies (ART) such as intrauterine insemination (IUI) or in vitro fertilization (IVF).
These procedures may be an option for lesbian couples who have already undergone various fertility treatment options but are not yet pregnant. People should consider discussing options with a healthcare professional and may need to consult with a knowledgeable reproductive specialist.
The Centers for Disease Control and Prevention (CDC) provide an interactive map that allows people to locate fertility clinics near them in the United States. People can use this to learn about what services they provide, the types of patients they see, and their success rates.
Regardless of the specific path a lesbian couple chooses to take to parenthood, if one partner wants to become pregnant without having sex with a person who has a penis, the couple will need to use a sperm donor.
There are many options for doing this. The couple could ask someone they know to donate sperm. Or they can purchase sperm from a sperm bank, usually with the assistance of a fertility clinic.
Lesbians who use donor sperm can perform the insemination themselves or pursue insemination options at a fertility clinic.
Some lesbian couples may opt to use the egg of one partner and the uterus of the other, which requires the help of a fertility clinic. But if one partner intends to use both their egg and their uterus, it is often possible to get pregnant without specialist help.
But if one partner intends to use both their egg and their uterus, it is often possible to get pregnant without specialist help.
About 6% of married heterosexual women under 45 years old cannot get pregnant after a year of trying. It is likely that a similar number of lesbian women have fertility issues.
Some fertility treatments, such as using medication to induce ovulation, can increase the odds of successfully getting pregnant without additional intervention. Others, such as IVF, require the ongoing assistance of a fertility doctor.
Intrauterine insemination (IUI)
IUI is a type of artificial insemination during which a doctor inserts sperm directly into the cervix or uterus, mimicking the process of fertilization that may occur during penile-vaginal intercourse.
If a couple uses donor sperm, the sperm will be pre-washed and prepared.
In some cases, the person undergoing insemination may take medication to increase the odds of pregnancy. Even without such medication, a doctor will use various monitoring techniques to pinpoint ovulation to ensure the timing is right.
In vitro fertilization (IVF)
IVF is a more complicated technique, in which a doctor fertilizes the egg outside of the body. It requires the doctor to remove eggs from the body first, then fertilize them, then wait for them to grow into embryos. At that time, the doctor implants them back into the uterus.
In most cases, IVF requires about a month of preparation, during which the partner who will be carrying the pregnancy takes various drugs to prepare the body for pregnancy and induce ovulation. The partner whose eggs the couple uses will need to undergo a separate procedure to remove the eggs.
Lesbian couples can choose to undergo reciprocal, or partner IVF. In this scenario, one partner donates eggs that a doctor transfers into the other partner’s uterus.
A lesbian can choose to have sex with a male partner if they are comfortable doing so, attracted to men, or the couple’s budget is very limited. The success of this depends on the timing of intercourse, as well as the fertility of both sexual partners.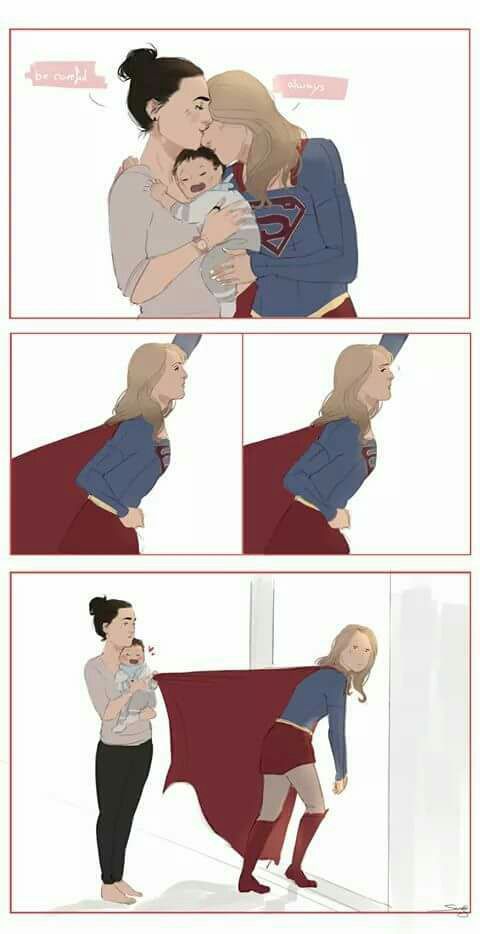
Sex with a partner with a penis may have significant legal complications since the man may have a right to claim the child as his own.
Couples who use IVF sometimes end up with extra embryos they do not use. Some allow third parties to “adopt” these embryos.
This can save some time and money and may also be a good option if neither partner ovulates regularly or if both have other fertility complications. A doctor can then implant the embryos directly into the uterus of the partner who wishes to become pregnant.
Lesbian couples do not have to become pregnant to become parents. They may wish to consider other options such as:
Co-parenting
Lesbians can co-parent one another’s children. For example, a person who has children from a prior relationship may opt to raise them with their new partner.
In some cases, such as if the prior partner renounces their parental rights, the new partner may even adopt the child or children.
Fostering or adoption
Lesbian couples can sign up to be foster parents, either on a temporary basis or with the intention of adopting. Some couples opt to foster children they know, while many enter the foster care system.
Some couples opt to foster children they know, while many enter the foster care system.
Similarly, it may be possible to adopt a child. This could be a child the couple knows who needs a home, such as the orphan of a relative, or by seeking help from an adoption agency.
A popular myth suggests that children need two parents of different sexes. But numerous studies suggest children can thrive in many environments, and there is no evidence that children of lesbians fare worse than other children.
In fact, some research suggests they may actually do better on some measures of well-being.
For example, a 2020 analysis found that children raised by same-sex parents did better in school than peers raised by different-sex parents. A 2016 study found that children of same-sex parents are similarly well-adjusted with similar social skills to children raised by different-sex parents.
Lesbian couples may also have a more equitable distribution of household labor, distributing the load of parenting more evenly.
Lesbian couples may also face some challenges. They include:
- Stigma and discrimination: Lesbian couples may face heterosexism discrimination, making the transition to parenthood more stressful.
- Lack of social support: Some lesbians report less social support, especially if their families of origin reject them because of their sexual orientation.
- Cost: In most cases, lesbian pregnancies incur significant costs, especially when using ART. A 2016 study estimates the average cost of ART in 2012 to be $28,829 per singleton pregnancy. Even when the cost of ART is minimal, lesbians may need to work with lawyers to ensure they are both legal parents of the child.
- Legal concerns: While same-sex marriage has reduced some legal hurdles, some states continue to enact laws that may make it more difficult for two lesbian parents to claim their child, especially if the couple is not married.

- Medical issues: Pregnancies that use ART, especially IVF, have higher rates of complications such as preterm labor, gestational diabetes, and pregnancy loss. But this may be partially due to the fact that people who use ART are more likely to have infertility and related health problems.
- Provider issues: Some lesbian couples may struggle to find non-heterosexist providers, either when trying to become pregnant or for their prenatal care.
- Emotional concerns: Some couples may struggle emotionally with the challenges of lesbian parenting, such as the fact that both parents cannot be a genetic/biological parent, or the rigors of ART.
Lesbian couples, and other members of LGBTQIA+ communities, have many options for becoming parents.
There are many fertility treatments available, such as IUI and IVF, which can help the couple become pregnant. Many reproductive clinics have significant experience supporting lesbian couples on their journey to pregnancy.
Additionally, some couples may instead opt to become parents without pregnancy and consider options such as co-parenting, adopting, or fostering children.
How to Get Pregnant as a Lesbian Couple
In honor of Pride Month, Guest Blogger, Christina Barnes, RN, shares ways to get pregnant as a lesbian couple
Getting pregnant as a lesbian couple may seem complicated, but it all comes down to the three things you need to make a baby: sperm, an egg, and a uterus. You and your partner likely have the eggs and a uterus, but if not, you still have options (such as egg donation and surrogacy). In this post, though, we’re going to cover family creation for two women who have eggs and a uterus. If you have those two, you just need the sperm, which can be acquired through a known donor or a sperm bank. Once you’ve decided whose eggs, uterus, and sperm you’ll be using, you’re almost ready to go!
Before Trying To Conceive
Before one or both of you start trying to conceive, it is important to meet with your primary care doctor or gynecologist. Your doctor will make sure that you do not have any fertility issues and that you are healthy enough to successfully carry a pregnancy. If you do have any issues that might impact your fertility, it’s best to know that before purchasing vials of sperm or undergoing expensive procedures. You can discuss the different methods of family building and insemination with your doctor and decide which one is best for you and your partner.
Your doctor will make sure that you do not have any fertility issues and that you are healthy enough to successfully carry a pregnancy. If you do have any issues that might impact your fertility, it’s best to know that before purchasing vials of sperm or undergoing expensive procedures. You can discuss the different methods of family building and insemination with your doctor and decide which one is best for you and your partner.
This visit is also a great opportunity to discuss genetic testing. With genetic testing, you can find out if you are a carrier of a genetic disease. If you are a carrier of a particular disease, you can look for a donor who is not a carrier and reduce the risk that your child would inherit that disease.
There are many legal implications when same sex couples build their families, and it’s a good idea to understand your state’s laws about conception, pregnancy, birth, and parenting in same sex relationships. Connecting Rainbows is a free legal and fertility resource for the LGBTQ+ community to help start, grow, and protect your family. They can be found at www.connectingrainbows.org.
They can be found at www.connectingrainbows.org.
Intracervical Insemination (ICI)
Intracervical insemination (ICI) can be done at home, and is often referred to as home insemination. ICI is a relatively simple procedure – the woman being inseminated will lay in a comfortable place, and either she or her partner will insert the semen sample in a needless syringe into her vagina. The semen is injected into the area inside the vagina at the cervix. ICI is painless and less expensive than other options for family building, making it a great option for many couples. ICI is, however, less effective than IUI or IVF. Women with no fertility issues who undergo ICI have a 5-10% pregnancy success rate per cycle. One “cycle” is the period of ovulation when a person can get pregnant, regardless of how many times she inseminates with ICI during that period. When doing ICI, the woman must track her menstrual cycle and ovulation to pinpoint her exact fertile window. The ICI is then completed during the fertile window. Some women do ICI only once during the fertile window, and some do it multiple times per window. How often you do ICI during your fertile window is up to you.
Some women do ICI only once during the fertile window, and some do it multiple times per window. How often you do ICI during your fertile window is up to you.
Women who purchase donor sperm for ICI can use either ICI or IUI vials. ICI vials are less expensive than IUI vials, because the ICI vials still contain seminal fluid. In an IUI vial, that seminal fluid is washed away, also known as “pre-washed.” Your medical health provider will recommend which type of vial you should purchase.
Unfortunately, some states have laws that do not allow home insemination. These states may require that the insemination be performed by a physician. Fairfax Cryobank’s client services can help you determine your state’s laws: 800-338-8407.
For more information on ICI and home insemination, check out some stories from families who chose to create their families through ICI:
The Ensign Family: https://fairfaxcryobank.com/blog/how-we-got-pregnant-fast-as-a-lesbian-couple-abbie-and-julia-ensign
The Anderson Family: https://fairfaxcryobank. com/home-insemination
com/home-insemination
Intrauterine Insemination (IUI)
Intrauterine insemination (IUI) is done in a doctor’s office or clinic, and usually takes about 15-20 minutes to complete. A long, flexible tube is inserted through the woman’s cervix directly into the uterus. Sperm is injected through this tube into the uterus, where it has a higher chance of meeting and fertilizing an egg. IUI has a higher pregnancy success rate than ICI – a woman has a 15-20% success rate per cycle of IUI. When comparing ICI versus IUI, IUI may be a better choice for women who are unable to track their cycles with home ovulation predictor kits, as well as women with a history of fertility issues.
While IUI is more effective than ICI, one downside is that it is more expensive. The cost of IUI includes any doctor’s office and procedure fees, any testing or ultrasounds, medications, and the IUI pre-washed sperm sample. It may be possible to purchase an ICI sperm sample if your clinic can pre-wash it for you, but make sure to check with your healthcare provider first.
Check out some of our Fairfax Cryobank families who chose to have their babies through IUI:
The Conrad Family: https://fairfaxcryobank.com/blog/two-moms-and-a-vial-of-sperm
The Mitryk Family: https://fairfaxcryobank.com/blog/fairfax-family-testimonial-krystian-mitryk
In Vitro Fertilization (IVF)
In Vitro Fertilization (IVF) has the highest pregnancy success rate of all available reproductive options, but it is also the most expensive and invasive. IVF involves retrieving eggs from one or both partners, fertilizing them with sperm outside of the body, and then implantation of the fertilized embryos into one or both partners.
IVF can offer lesbian couples unique ways to create their families, allowing couples to choose whose eggs they use, who will carry the baby (or babies), and when the embryos will be implanted. Some couples who use IVF choose to implant embryos together and become pregnant at the same time, some choose to have one woman carry a baby first and the other woman carry a baby from the same embryo batch a few years later. Some couples choose to do reciprocal IVF, where one woman’s eggs are retrieved and fertilized, and then implanted into her partner’s uterus. The baby is carried and birthed by the non-genetic mother, allowing each woman to contribute significantly to the creation and growth of their baby.
Some couples choose to do reciprocal IVF, where one woman’s eggs are retrieved and fertilized, and then implanted into her partner’s uterus. The baby is carried and birthed by the non-genetic mother, allowing each woman to contribute significantly to the creation and growth of their baby.
For some personal stories from lesiban couples who have undergone IVF and reciprocal IVF, check out these posts:
The Lotito Family (IVF): https://fairfaxcryobank.com/blog/donor-sperm/fairfax-families-meet-the-lotito-family
The Jaffe Family (Reciprocal IVF): https://fairfaxcryobank.com/blog/the-jaffes-journey-to-motherhood-with-rivf
90,000 Lesbian couple took turns carrying their baby for the first time 90,001 90,002 In the US, lesbian couples became the first same-sex couple to take turns carrying their baby. This was made possible thanks to the new IVF technology, in which the embryo is placed not in an incubator, but in a woman's body. The boy was born perfectly healthy, and soon another lesbian couple repeated this experience.
A Texas lesbian couple took turns carrying the same baby. This is the first such case in medical practice.0005 ABC .
Ashley, 28, and Bliss Coulter, 36, met six years ago and got married in 2015. They both expected to have a child in the future, while Bliss wanted him to be biologically hers, but the prospect of walking pregnant did not attract her.
Usually, in the case of lesbian couples, donor sperm is used, with which doctors fertilize one of the women, and after the birth of the child, the second adopts him.
But since the eggs were to be taken from Bliss and Ashley was going to carry the baby, this was not an option for them.
From acquaintances they learned about a new IVF method, practiced in only one clinic. Usually, during IVF, fertilized eggs are placed in an incubator for several days, after which they are transferred to the uterine cavity. But reproductologists Kathy and Kevin Doody have developed a new technology - with it, fertilization occurs in a special plastic capsule, which is then immediately placed in the body of the expectant mother. There, the embryo is warm and protected from external influences. Then, after a few days, the embryo is removed from the capsule and transferred to the uterus.
There, the embryo is warm and protected from external influences. Then, after a few days, the embryo is removed from the capsule and transferred to the uterus.
This approach makes it possible to reduce the cost of IVF by more than half, as it eliminates the need for incubation of the embryo in the laboratory. It is necessary, because the embryo does not yet have the internal organs - the liver, kidneys and lungs - necessary for the elimination of toxins.
“It turns out, not surprisingly, that a woman's own body is a very good incubator,” explains Cathy Doody. “We have a liver, kidneys and lungs, so we can provide the same services to the embryo, but in a more natural way.”
The new method has been practiced as recently as 2015. Usually, the same woman becomes both the egg donor and the mother. But in the case of Bliss and Ashley, the capsule was first in Bliss's body, and then the embryo was placed in Ashley's uterus.
“This case is special - two women carried their child together,” says Doody. “Everyone contributed to this pregnancy.”
“Everyone contributed to this pregnancy.”
“When we talked to Doody, she was very confident that she could do it. She gave us hope. It was very exciting,” says Ashley. “The idea that we could both bear a child was hers, she suggested insemination inside Bliss's body. We laughed and I said - wow, so she will carry him too.
Bliss underwent ovarian stimulation, her cells were fertilized with donor sperm and placed in a capsule. The capsule remained in Bliss's body for five days, until the fertilized eggs developed into the blastocyst stage. The embryo was then frozen and Ashley began preparing for the pregnancy. When she began her period, she received hormonal drugs designed to trick the body. The doctors then implanted one embryo into her uterus. And after 10 days, the pregnancy was confirmed from the first time.
“Bliss jokes that she has golden eggs,” Ashley laughs.
9 months later, in June 2018, she gave birth to a healthy boy weighing 3,700. The couple named their son Stetson.
“The moment he was born, I felt like the happiest person in the world because he was perfect,” recalls Ashley. “When I look at him, I see my wife in him. It's priceless".
Although the couple is extremely happy with one child, Ashley hopes that she can talk Bliss into having a second one - they still have two frozen embryos left.
Dr. Doody notes that the method of insemination used allows lesbian couples to have a unique bond with their children and makes pregnancy more natural. Previously, she and her husband practiced it only for heterosexual couples.
“We were talking at home one evening and I said, you know, we could use this for same-sex couples too. And Kevin said yes, I think you're right. I think we can do it."
After Bliss and Ashley, Doody was approached by another couple who went through the same procedure. Their daughter was born shortly after Bliss and Ashley's son.
When the procedures became known, Doody faced criticism from religious adherents who said that science was contrary to their beliefs.
“Well, with all due respect, I disagree,” Cathy replied. - I think that family, relationships, children - this is exactly what should be in our world. Nobody knew it was possible, but it all worked out great.”
ROPA technique MOTHERHOOD IN LESBIAN, BISEXUAL AND TRANSEXUAL COUPLES
Thanks to advanced technology and individually tailored treatments, modern seminal models can achieve pregnancy. For example, the ROPA method allows same-sex female couples to actively participate in the fertilization process. One of them is the genetic mother of the child, and the other is the biological
- Subscribe to newsletter
- I accept the terms of the user agreement and privacy policy
This field is used for verification purposes and should be left unchanged.
What is ROPA technology?
In vitro fertilization ROPA (Use of partner eggs) or the use of female partner oocytes is one of the assisted reproduction techniques that allows married women of the same sex marriage to participate in fertilization and pregnancy.
One provides oocytes, which are inseminated with sperm from anonymous donor , while the other receives embryos and carries a child. As a result, after the provision of prior consent, there is a genetic mother and one who bears a child.
Lesbian motherhood: biological and social changes
Conception requires the interaction within the female reproductive organs of two germ cells: one female and one male. If, due to gender identity or sexual orientation, this path is unacceptable for a woman, it is necessary to resort to artificial reproduction methods, because sexual orientation and the desire to have offspring should not necessarily be associated with these biological characteristics.
Today we meet with different types of families whose situations and desires require individual approach in each case, such as pregnancy between two women.
Instituto Bernabeu always takes into account the special needs of each patient and adapts the medical services and fertility treatment to provide a personalized in vitro fertilization procedure.
Legal aspects of motherhood for lesbian couples in Spain
Under current Spanish law: "A woman may use the methods regulated by this Law, regardless of her marital status and sexual orientation." Therefore, the law enshrines the right to motherhood for all women, and more importantly, not only because of infertility.
Since 2007, Spanish law has allowed the registration of dual motherhood at the registry office. At the same time, children born using the ROPA method in a female same-sex couple are legally owned by both mothers only if their relationship is officially married.
If the women are unmarried, then the genetic mother (who did not bear a child) will have to start the process of adoption or adoption in order to be legally registered as a mother in the Civil Registry.
In the case of embryo freezing with the ROPA method (Use of Partner Oocytes), if there is no medical indication for transfer only to the partner who has already received the embryo/s for the first time, the frozen embryos can be transferred to either of them in the subsequent cycle so how women are married and embryos are shared.
IVF ROPA or dual motherhood (use of female partner's eggs)
), we offer a new alternative to co-motherhood - the ROPA method with partner egg retrieval.
Currently, although this technique is not mandated by law, one can resort to the ROPA (Reception of Oocytes from PArtner) method, or the use of female partner oocytes, which allows two women of the same sex marriage to participate in insemination and pregnancy. One provides oocytes, which are inseminated with sperm from an anonymous donor, and the other receives embryos to conceive. As a result, after the provision of prior consent, there is a genetic mother and one who bears a child. For this purpose, since 2007, Spanish law has allowed the registration of dual motherhood in the Civil Registry in the case of same-sex marriages. In this regard, children born in Spain using the ROPA method will be the children of two mothers from a legal point of view.
One provides oocytes, which are inseminated with sperm from an anonymous donor, and the other receives embryos to conceive. As a result, after the provision of prior consent, there is a genetic mother and one who bears a child. For this purpose, since 2007, Spanish law has allowed the registration of dual motherhood in the Civil Registry in the case of same-sex marriages. In this regard, children born in Spain using the ROPA method will be the children of two mothers from a legal point of view.
How is IVF ROPA carried out?
ROPA is conventional in vitro fertilization (IVF) adapted to the reproductive needs of lesbian families. First of all, it is necessary to examine both patients in order to develop an individually tailored treatment method in accordance with their state of health. Then, the ovaries are stimulated to obtain a sufficient number of embryos and thus increase the chances of conceiving a child. At the same time, the recipient partner goes through the process of preparing the uterus for the transfer and implantation of the embryo. As soon as the maturation of oocytes (oocytes) is established, the cells are punctured and aspirated. After that, the egg is fertilized in the laboratory with the donor's sperm from our sperm bank. And then, we culture the embryos under close supervision and do the transfer on the 5th or 6th day. Thus, we manage to transfer embryos to the blastocyst stage, optimizing the chances of pregnancy. The following months of pregnancy will develop like any other pregnancy, allowing both women to enjoy this happiness.
As soon as the maturation of oocytes (oocytes) is established, the cells are punctured and aspirated. After that, the egg is fertilized in the laboratory with the donor's sperm from our sperm bank. And then, we culture the embryos under close supervision and do the transfer on the 5th or 6th day. Thus, we manage to transfer embryos to the blastocyst stage, optimizing the chances of pregnancy. The following months of pregnancy will develop like any other pregnancy, allowing both women to enjoy this happiness.
In addition, epigenetics has shown that environmental factors and the lifestyle of a pregnant woman marks and determines the expression of the genes of the unborn child. Therefore, it is also genetically involved in the development of the child.
Any method of reproductive treatment (IVF, adoption of embryos or ROPA) has an emotional impact. Therefore, to help our patients walk this path, the Instituto Bernabeu offers, on request and at no extra charge, sessions with a psychologist, with which expectant mothers will be prepared for the possible emotions during each stage of the process and pregnancy.
ROPA Sperm Donors - Strict Selection
To ensure maximum confidence and assurance during ROPA procedures, the selection of the most suitable donor involves comprehensive medical, physical and psychological tests and examinations.
The selection process for the most suitable sperm donor is very rigorous. It corresponds to the responsibility that we take on in connection with the trust of our patients. That is why, when donating, we perform examinations and tests beyond those required by law. Due to the rigorous nature of the tests, only a small percentage of candidates are eligible for inclusion in our sperm bank. Only 9% of candidates undergo strict psychological, genetic and medical mandatory tests.
Modern technological advances allow us to perform additional analyzes providing a high degree of assurance. In addition to the tests provided, when donating, we carry out a study of sexually transmitted diseases, a genetic analysis of the 600 or 3000 most serious diseases that can be transmitted to the child and, among other things, a PCR blood test, which can be used to re-check the serology in the moment of sampling, since the diagnosis is obtained in just a few minutes.